CHAPTER 146
Pituitary Gland Disorders
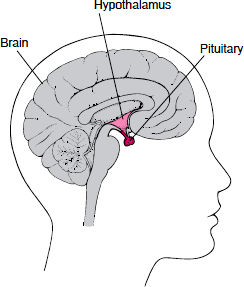
The pituitary is a pea-sized gland that is housed within a bony structure (sella turcica) at the base of the brain. The sella turcica protects the pituitary but allows very little room for expansion.
The pituitary controls the function of most other endocrine glands and is therefore sometimes called the master gland. In turn, the pituitary is controlled in large part by the hypothalamus, a region of the brain that lies just above the pituitary. By detecting the levels of hormones produced by glands under the pituitary’s control (target glands), the hypothalamus or the pituitary can determine how much stimulation the target glands need.
The pituitary has two distinct parts: the front (anterior) lobe, which accounts for 80% of the pituitary gland’s weight, and the back (posterior) lobe. The lobes are connected to the hypothalamus by a stalk that contains blood vessels and nerve cell projections (nerve fibers, or axons). The hypothalamus controls the anterior lobe by releasing hormones through the connecting blood vessels. It controls the posterior lobe through nerve impulses.
The anterior lobe of the pituitary produces and releases (secretes) six main hormones:
 Growth hormone, which regulates growth and physical development and has important effects on body shape by stimulating muscle formation and reducing fat tissue
Growth hormone, which regulates growth and physical development and has important effects on body shape by stimulating muscle formation and reducing fat tissue
 Thyroid-stimulating hormone, which stimulates the thyroid gland to produce thyroid hormones
Thyroid-stimulating hormone, which stimulates the thyroid gland to produce thyroid hormones
 Adrenocorticotropic hormone (ACTH, also called corticotropin), which stimulates the adrenal glands to produce cortisol and other hormones
Adrenocorticotropic hormone (ACTH, also called corticotropin), which stimulates the adrenal glands to produce cortisol and other hormones
 Follicle-stimulating hormone and luteinizing hormone (the gonadotropins), which stimulate the testes to produce sperm, the ovaries to produce eggs, and the sex organs to produce sex hormones (testosterone and estrogen)
Follicle-stimulating hormone and luteinizing hormone (the gonadotropins), which stimulate the testes to produce sperm, the ovaries to produce eggs, and the sex organs to produce sex hormones (testosterone and estrogen)
 Prolactin, which stimulates the mammary glands of the breasts to produce milk
Prolactin, which stimulates the mammary glands of the breasts to produce milk
The anterior lobe also produces several other hormones, including one that causes the skin to darken (beta-melanocyte-stimulating hormone) and ones that inhibit pain sensations and help control the immune system (endorphins).
The posterior lobe of the pituitary produces only two hormones: antidiuretic hormone and oxytocin. Antidiuretic hormone (also called vasopressin) regulates the amount of water excreted by the kidneys and is therefore important in maintaining water balance in the body (see page 969). Oxytocin causes the uterus to contract during childbirth and immediately after delivery to prevent excessive bleeding. Oxytocin also stimulates contractions of the milk ducts in the breast, which move milk to the nipple (the let-down) in lactating women.
The hormones produced by the pituitary are not all produced continuously. Most are released in bursts every 1 to 3 hours, with alternating periods of activity and inactivity. Some of the hormones, such as ACTH, growth hormone, and prolactin, follow a circadian rhythm: The levels rise and fall predictably during the day, usually peaking just before awakening and dropping to their lowest levels just before sleep. The levels of other hormones vary according to other factors. For example, in women, the levels of luteinizing hormone and follicle-stimulating hormone, which control reproductive functions, vary during the menstrual cycle.
The pituitary gland can malfunction in several ways, usually as a result of developing a noncancerous tumor (adenoma). The tumor may overproduce one or more pituitary hormones, or the tumor may press on the normal pituitary cells, causing underproduction of one or more pituitary hormones. The tumor may also cause enlargement of the pituitary gland, with or without disturbing hormone production. Sometimes there is overproduction of one hormone by a pituitary tumor and underproduction of another at the same time due to pressure. Too little or too much of a pituitary hormone results in a wide variety of symptoms.
Doctors can diagnose pituitary gland malfunction using several tests. Imaging tests, such as a computed tomography (CT) or magnetic resonance imaging (MRI) scan, can show whether the pituitary has enlarged or shrunk. Such scans can usually determine whether a tumor exists in the gland.
Doctors can measure the levels of pituitary hormones, usually by a simple blood test. Doctors select which pituitary hormone levels they want to measure depending on the person’s symptoms. Sometimes, levels of pituitary hormones are not easy to interpret because the levels vary greatly during the day and according to the body’s needs. For these hormones, measuring a random blood sample does not provide useful information.
For some of those hormones, doctors give a substance that would normally affect hormone production and then they measure the level of the hormone. For example, if a doctor injects insulin, the levels of ACTH, growth hormone, and prolactin should increase. Rather than measuring growth hormone levels directly, doctors often measure another hormone, insulin-like growth factor 1 (IGF-1). Growth hormone is produced in bursts and its levels quickly fall, but IGF-1 levels reflect the overall daily production of growth hormone. For all of these reasons, interpreting the results of blood tests for pituitary hormones is complex.
Pituitary: The Master Gland
The pituitary, a pea-sized gland at the base of the brain, produces a number of hormones. Each of these hormones affects a specific part of the body (a target organ or tissue). Because the pituitary controls the function of most other endocrine glands, it is often called the master gland.
| Hormone | Target Organ or Tissue |
| Adrenocorticotropic hormone (ACTH) | Adrenal glands |
| Antidiuretic hormone | Kidneys |
| Beta-melanocyte-stimulating hormone | Skin |
| Endorphins | Brain and immune system |
| Enkephalins | Brain |
| Follicle-stimulating hormone | Ovaries or testes |
| Growth hormone | Muscles and bones |
| Luteinizing hormone | Ovaries or testes |
| Oxytocin | Uterus and mammary glands |
| Prolactin | Mammary glands |
| Thyroid-stimulating hormone | Thyroid gland |
Enlargement of the Pituitary Gland
Enlargement of the pituitary gland is usually due to a tumor but may be due to bleeding into the gland or involvement by some other disease, such as tuberculosis or sarcoidosis. An enlarged pituitary gland may produce symptoms such as headaches. Because the growing gland often presses on the optic nerve, which passes above the pituitary gland, loss of vision may occur. Vision loss often initially affects only the upper, outermost fields of vision in both eyes. Underproduction or overproduction of pituitary hormones may also occur. Treatment depends on the cause of the enlargement.
Hypopituitarism
Hypopituitarism is an underactive pituitary gland that results in deficiency of one or more pituitary hormones.
 Hypopituitarism can be caused by several factors, including certain inflammatory diseases, a tumor of the pituitary gland, or an insufficient blood supply to the pituitary gland.
Hypopituitarism can be caused by several factors, including certain inflammatory diseases, a tumor of the pituitary gland, or an insufficient blood supply to the pituitary gland.
 Symptoms depend on what hormone is deficient and may include short height, infertility, intolerance to cold, fatigue, and an inability to produce breast milk.
Symptoms depend on what hormone is deficient and may include short height, infertility, intolerance to cold, fatigue, and an inability to produce breast milk.
 The diagnosis is based on measuring the blood levels of hormones produced by the pituitary gland and on imaging tests performed on the pituitary gland.
The diagnosis is based on measuring the blood levels of hormones produced by the pituitary gland and on imaging tests performed on the pituitary gland.
 Treatment focuses on replacing deficient hormones with synthetic ones but sometimes includes surgical removal or irradiation of any pituitary tumors.
Treatment focuses on replacing deficient hormones with synthetic ones but sometimes includes surgical removal or irradiation of any pituitary tumors.
Hypopituitarism, an uncommon disorder, can be caused by a number of factors, including a pituitary tumor or an insufficient blood supply to the pituitary gland.
Symptoms and Complications
Although symptoms sometimes begin suddenly and dramatically, they usually begin gradually and may go unrecognized for a long time. Symptoms depend on which pituitary hormones are deficient. In some cases, the pituitary gland’s production of a single hormone decreases. More typically, the levels of several hormones decrease at the same time (panhypopituitarism). Production of growth hormone, luteinizing hormone, and follicle-stimulating hormone often decreases before that of thyroid-stimulating hormone and adrenocorticotropic hormone.
Growth Hormone Deficiency: A lack of growth hormone typically leads to poor overall growth and short height (dwarfism) if it occurs in childhood. In adults, growth hormone deficiency does not affect height, because the bones have finished growing, but it can cause increased fat and reduced muscle tissue, thinning of bones, and reduced energy and quality of life.
Deficiency of Gonadotropins (Follicle-Stimulating Hormone and Luteinizing Hormone): In premenopausal women, deficiencies of these hormones cause menstrual periods to stop (amenorrhea), infertility, vaginal dryness, and loss of some female sexual characteristics. In men, deficiencies of these hormones result in wasting away (atrophy) of the testes, decreased sperm production and consequent infertility, and loss of some male sexual characteristics. Deficiencies of luteinizing hormone and follicle-stimulating hormone can also occur in Kallmann’s syndrome, in which people may also have a cleft lip or palate, are color-blind, and are unable to sense smells.
Thyroid-Stimulating Hormone Deficiency: Thyroid-stimulating hormone deficiency leads to an underactive thyroid gland (hypothyroidism), which results in such symptoms as confusion, intolerance to cold, weight gain, constipation, and dry skin (see page 995). Most cases of hypothyroidism, however, are due to a problem originating in the thyroid gland itself, not to low levels of pituitary hormones.
Adrenocorticotropic Hormone Deficiency: Adrenocorticotropic hormone (ACTH) deficiency leads to an underactive adr enal gland, which results in fatigue, low blood pressure, low levels of sugar in the blood, and low tolerance for stress. This is the most serious pituitary hormone deficiency. If the body is unable to make any ACTH, the person may die.
Prolactin Deficiency: Prolactin deficiency reduces or eliminates a woman’s ability to produce breast milk after childbirth. One cause of low prolactin levels and deficiency of other pituitary hormones is Sheehan’s syndrome, a rare complication of childbirth. Sheehan’s syndrome typically develops because of excessive blood loss and shock during childbirth, which results in partial destruction of the pituitary gland. Symptoms include fatigue, loss of pubic and underarm hair, and inability to produce breast milk. Prolactin deficiency has no known ill effects in men.
What Causes an Underactive Pituitary?
CAUSES AFFECTING PRIMARILY THE PITUITARY
 Pituitary tumors
Pituitary tumors
 Inadequate blood supply to the pituitary (due to severe bleeding, blood clots, anemia, or other conditions)
Inadequate blood supply to the pituitary (due to severe bleeding, blood clots, anemia, or other conditions)
 Infections and inflammatory diseases
Infections and inflammatory diseases
 Sarcoidosis or amyloidosis (unusual diseases)
Sarcoidosis or amyloidosis (unusual diseases)
 Irradiation (as for a brain tumor)
Irradiation (as for a brain tumor)
 Surgical removal of pituitary tissue
Surgical removal of pituitary tissue
 Autoimmune disease
Autoimmune disease
CAUSES AFFECTING PRIMARILY THE HYPOTHALAMUS, WHICH THEN AFFECTS THE PITUITARY
 Tumors of the hypothalamus
Tumors of the hypothalamus
 Inflammatory diseases
Inflammatory diseases
 Head injuries
Head injuries
 Surgical damage to the pituitary or to the blood vessels or nerves leading to it
Surgical damage to the pituitary or to the blood vessels or nerves leading to it
Diagnosis
Because the pituitary gland stimulates other glands, a deficiency in pituitary hormones often reduces the amount of hormones those other glands produce. Therefore, a doctor considers the possibility of pituitary malfunction when investigating a deficiency in another gland, such as the thyroid or adrenal gland. When symptoms suggest that several glands are underactive, a doctor may suspect hypopituitarism or a polyglandular deficiency syndrome.
An evaluation usually begins by measuring levels of the hormones that the pituitary gland produces and at the same time measuring levels of the hormone produced by the target organ. For example, a person with hypothyroidism due to failure of the pituitary gland has low levels of thyroid hormone and low or inappropriately normal levels of thyroid-stimulating hormone, which is produced by the pituitary gland. In contrast, a person with hypothyroidism due to failure of the thyroid gland itself has low levels of thyroid hormone and high levels of thyroid-stimulating hormone.
Growth hormone production by the pituitary is difficult to evaluate because no test accurately measures it. The body produces growth hormone in several bursts each day, and the hormone is quickly used. Thus, the blood level at any given moment does not indicate whether production is normal over the course of a day. Instead, doctors measure the levels of insulin-like growth factor 1 (IGF-1) in the blood. Production of IGF-1 is controlled by growth hormone, and the level of IGF-1 tends to change slowly in proportion to the overall amount of growth hormone produced by the pituitary. In infants and young children, doctors may instead measure levels of a similar substance, IGF-binding protein type 3.
Polyglandular Deficiency Syndromes
Polyglandular deficiency syndromes are hereditary disorders in which several endocrine glands malfunction simultaneously. The actual cause of the malfunction may be related to an autoimmune reaction in which the body’s immune defenses mistakenly attack the body’s own cells. Polyglandular deficiency syndromes are classified into three types:
Type 1: In this type, which develops in children, the parathyroid and adrenal glands are underactive, which can lead to diabetes, hepatitis, malabsorption of nutrients and weight loss, and hair loss. Affected children are prone to chronic yeast infections as well.
Type 2: In this type, which develops in adults, the adrenal and thyroid glands are underactive, although the thyroid gland sometimes becomes overactive. People with type 2 polyglandular deficiency also develop diabetes.
Type 3: This type is very similar to type 2, except that the adrenal glands remain normal.
Because the levels of luteinizing hormone and follicle-stimulating hormone fluctuate with the menstrual cycle, their measurement in women may be difficult to interpret. However, in postmenopausal women who are not taking estrogen, luteinizing hormone and follicle-stimulating hormone levels normally are high.
Production of ACTH is usually measured by assessing the response of its target hormone (cortisol) to stimuli, such as a low level of sugar in the blood after an insulin injection. If the level of cortisol does not change and the level of ACTH in the blood is normal or low, a deficiency of ACTH production is confirmed.
Once hypopituitarism is established by blood tests, the pituitary gland is usually evaluated with a computed tomography (CT) or magnetic resonance imaging (MRI) scan to identify structural problems. CT or MRI scans help reveal individual (localized) areas of abnormal tissue growth as well as general enlargement or shrinkage of the pituitary gland. The blood vessels that supply the pituitary can be examined with cerebral angiography (see page 2036).
Treatment
When possible, treatment is aimed at removing the cause of the pituitary hormone deficiency, such as a tumor. Surgical removal of a tumor is often the most appropriate first treatment, and removal also usually reduces any pressure symptoms and vision problems caused by the tumor. For all but the largest tumors, surgery can usually be done through the nose (transphenoidal).
Supervoltage or proton beam irradiation of the pituitary gland can be used to destroy a tumor. Large tumors and those that have extended beyond the sella turcica may be impossible to remove with surgery alone. If so, doctors use supervoltage irradiation after surgery to kill the remaining tumor cells. Irradiation of the pituitary gland tends to cause a slow loss of pituitary function. The loss may be partial or complete. Therefore, the function of the target glands is generally evaluated every 3 to 6 months for the first year and yearly thereafter. Tumors that produce prolactin can be treated with drugs that act like dopamine, such as bromocriptine or cabergoline. These drugs shrink the tumor while also lowering prolactin levels.
When it is not possible to remove the cause of the hormone deficiency, such as an insufficient blood supply to the pituitary gland, treatment focuses on replacing the deficient hormones, usually by replacing the target hormones. For example, people deficient in thyroid-stimulating hormone are given thyroid hormone. Those deficient in ACTH are given adrenocortical hormones such as hydrocortisone. Those deficient in luteinizing hormone and follicle-stimulating hormone are given estrogen, progesterone, or testosterone.
Growth hormone is the one pituitary hormone that is replaced. Growth hormone treatment must be given by injection. When given to children who have growth hormone deficiency before the growth plates in their bones close, replacement growth hormone prevents them from being exceptionally short. Growth hormone is now also being used to treat some adults with growth hormone deficiency to improve body composition, increase bone density, and enhance quality of life.
Central Diabetes Insipidus
Central diabetes insipidus is a lack of antidiuretic hormone that causes excessive production of very dilute urine (polyuria).
 Central diabetes insipidus has several causes, including a brain tumor, tuberculosis, a brain injury or surgery, and some forms of other diseases.
Central diabetes insipidus has several causes, including a brain tumor, tuberculosis, a brain injury or surgery, and some forms of other diseases.
 The main symptoms are excessive thirst and excessive urine production.
The main symptoms are excessive thirst and excessive urine production.
 The diagnosis is based on urine tests, blood tests, and a water deprivation test.
The diagnosis is based on urine tests, blood tests, and a water deprivation test.
 People with central diabetes insipidus usually are given the drugs vasopressin or desmopressin as a nasal spray.
People with central diabetes insipidus usually are given the drugs vasopressin or desmopressin as a nasal spray.
Causes
Central diabetes insipidus usually results from the decreased production of antidiuretic hormone (vasopressin), the hormone that helps regulate the amount of water in the body (see box on page 970). Antidiuretic hormone is unique in that it is produced in the hypothalamus but is then stored and released into the bloodstream by the pituitary gland.
Central diabetes insipidus may be caused by insufficient production of antidiuretic hormone by the hypothalamus. Alternatively, the disorder may be caused by failure of the pituitary gland to release antidiuretic hormone into the bloodstream. Other causes of central diabetes insipidus include damage done during surgery on the hypothalamus or pituitary gland; a brain injury, particularly a fracture of the base of the skull; a tumor; sarcoidosis or tuberculosis; an aneurysm (a bulge in the wall of an artery) or blockage in the arteries leading to the brain; some forms of encephalitis or meningitis; and the rare disease Langerhans’ cell histiocytosis. Another type of diabetes insipidus, nephrogenic diabetes insipidus, may be caused by abnormalities in the kidneys (see page 285).
Symptoms and Diagnosis
Symptoms may begin gradually or suddenly at any age. Often the only symptoms are excessive thirst and excessive urine production. A person may drink huge amounts of fluid—4 to 40 quarts (3 to 30 liters) a day—to compensate for the fluid lost in urine. Ice-cold water is often the preferred drink. When compensation is not possible, dehydration can quickly follow, resulting in low blood pressure and shock. The person continues to urinate large quantities of dilute urine, and this excessive urination is particularly noticeable during the night.
Doctors suspect diabetes insipidus in people who produce large amounts of urine. They first test the urine for sugar to rule out diabetes mellitus. Blood tests show abnormal levels of many electrolytes, including a high level of sodium. The best test is a water deprivation test, in which urine production, blood electrolyte levels, and weight are measured regularly for a period of about 12 hours, during which the person is not allowed to drink. A doctor monitors the person’s condition throughout the course of the test. At the end of the 12 hours—or sooner if the person’s blood pressure falls or heart rate increases or if he loses more than 5% of his body weight—the doctor stops the test and injects antidiuretic hormone. The diagnosis of central diabetes insipidus is confirmed if, in response to antidiuretic hormone, the person’s excessive urination stops, the urine becomes more concentrated, the blood pressure rises, and the heart beats more normally. The diagnosis of nephrogenic diabetes insipidus is made if, after the injection, the excessive urination continues, the urine remains dilute, and blood pressure and heart rate do not change.
Treatment
Vasopressin or desmopressin (a modified form of vasopressin) may be taken as a nasal spray several times a day. The dose is adjusted to maintain the body’s water balance and a normal urine output. Taking too much of these drugs can lead to fluid retention, swelling, and other problems. People with central diabetes insipidus who are undergoing surgery or are unconscious are generally given injections of vasopressin.
Sometimes central diabetes insipidus can be controlled with drugs that stimulate production of antidiuretic hormone, such as chlorpropamide, carbamazepine, clofibrate, and thiazide diuretics. These drugs are unlikely to relieve symptoms completely in people whose diabetes insipidus is severe.
Acromegaly and Gigantism
Overproduction of growth hormone causes excessive growth. In children, the condition is called gigantism. In adults, it is called acromegaly.
 Excessive growth hormone is almost always caused by a noncancerous (benign) pituitary tumor.
Excessive growth hormone is almost always caused by a noncancerous (benign) pituitary tumor.
 Children develop great stature; adults develop deformed bones but do not grow taller.
Children develop great stature; adults develop deformed bones but do not grow taller.
 Heart failure, weakness, and vision problems are common.
Heart failure, weakness, and vision problems are common.
 The diagnosis is based on blood tests and x-rays of the skull and hands.
The diagnosis is based on blood tests and x-rays of the skull and hands.
 Other imaging tests are done to look for the cause.
Other imaging tests are done to look for the cause.
 A combination of surgery, radiation therapy, and drug therapy is used to treat the overproduction of growth hormone.
A combination of surgery, radiation therapy, and drug therapy is used to treat the overproduction of growth hormone.
Growth hormone stimulates the growth of bones, muscles, and many internal organs. Excessive growth hormone, therefore, leads to abnormally robust growth of all of these tissues. Overproduction of growth hormone is almost always caused by a noncancerous (benign) pituitary tumor (adenoma). Certain rare tumors of the pancreas and lungs also can produce hormones that stimulate the pituitary to produce excessive amounts of growth hormone, with similar consequences.
Symptoms
If excessive growth hormone production starts before the growth plates have closed (that is, in children), the condition produces gigantism. The long bones grow enormously. A person grows to unusually great stature, and the arms and legs lengthen. Puberty may be delayed, and the genitals may not develop fully.
In most cases, excessive production of growth hormone begins between the ages of 30 and 50, long after the growth plates of the bones have closed. Increased growth hormone in adults produces acromegaly, in which the bones become deformed rather than elongated. Because changes occur slowly, they are usually not recognized for years.
The person’s facial features become coarse, and the hands and feet swell. Larger rings, gloves, shoes, and hats are needed. Overgrowth of the jawbone (mandible) can cause the jaw to protrude (prognathism). Cartilage in the voice box (larynx) may thicken, making the voice deep and husky. The ribs may thicken, creating a barrel chest. Joint pain is common; after many years, crippling degenerative arthritis may occur.
In both gigantism and acromegaly, the tongue may enlarge and become more furrowed. Coarse body hair, which typically darkens, increases as the skin thickens. The sebaceous and sweat glands in the skin enlarge, producing excessive perspiration and often an offensive body odor. The heart usually enlarges, and its function may be so severely impaired that heart failure occurs. Sometimes a person feels disturbing sensations and weakness in the arms and legs as enlarging tissues compress the nerves. Nerves that carry messages from the eyes to the brain may also be compressed, causing loss of vision, particularly in the outer visual fields. The pressure on the brain may also cause severe headaches.
Nearly all women with acromegaly have irregular menstrual cycles. Some women produce breast milk even though they are not breastfeeding (galactorrhea) because of either too much growth hormone or a related increase in prolactin. About one third of men who have acromegaly develop erectile dysfunction. There is also an increased likelihood of developing diabetes mellitus, high blood pressure (hypertension), heart failure, sleep apnea, and certain tumors, particularly affecting the large intestine, which may become cancerous. Life expectancy is reduced in people with untreated acromegaly.
Diagnosis
In children, rapid growth may not seem abnormal at first. Eventually, however, the abnormality of the extreme growth becomes clear.
In adults, because the changes induced by high levels of growth hormone occur slowly, acromegaly often is not diagnosed until many years after the first symptoms appear. Serial photographs (those taken over many years) may help a doctor establish the diagnosis. An x-ray of the skull may show thickening of the bones and enlargement of the nasal sinuses. X-rays of the hands show thickening of the bones under the fingertips and swelling of the tissue around the bones. Blood sugar levels and blood pressure may be high.
The diagnosis is confirmed by blood tests, which usually show high levels of both growth hormone and insulin-like growth factor 1 (IGF-1). Because growth hormone is released in short bursts and the levels of growth hormone often fluctuate dramatically even in people without acromegaly, a single high level of growth hormone in the blood is insufficient to make the diagnosis. Doctors must give something that would normally suppress growth hormone levels, most commonly a glucose drink (the oral glucose tolerance test), and show that normal suppression does not occur. This test is not necessary when the clinical features of acromegaly are obvious, the IGF-1 level is high, or a tumor is seen in the pituitary on scanning.
 Did You Know…
Did You Know…
A woman with acromegaly can produce breast milk even if she is not breastfeeding.
A computed tomography (CT) or magnetic resonance imaging (MRI) scan is usually done to look for abnormal growths in the pituitary gland. Because acromegaly is usually present for some years before being diagnosed, a tumor is seen on these scans in most people.
Treatment
Stopping or reducing the overproduction of growth hormone is not easy; thus, doctors may need to use a combination of surgery, radiation therapy, and drug therapy.
Surgery by an experienced surgeon is currently regarded as the best first treatment for most people with acromegaly caused by a tumor. It results in an immediate reduction in tumor size and growth hormone production, most often without causing deficiency of other pituitary hormones. Unfortunately, tumors are often large by the time they are found, and surgery alone does not usually produce a cure. Radiation therapy is often used as a follow-up treatment, particularly if a substantial amount of the tumor remains after surgery and acromegaly persists.
Radiation therapy involves the use of supervoltage irradiation, which is less traumatic than surgery. This treatment may take several years to have its full effect, however, and often results in later deficiencies of other pituitary hormones, as normal tissue is often also affected. More directed radiation therapy, such as stereotactic radiosurgery, is being tried to speed results and spare the normal pituitary tissue.
Drug therapy can also be used to lower growth hormone levels. Occasionally, bromocriptine and other drugs that act like dopamine are of some benefit. The most effective drugs, however, are those that are forms of somatostatin, the hormone that normally blocks growth hormone production and secretion. These drugs include octreotide and its newer long-acting analogs, which only have to be given about once a month. These drugs are effective in controlling acromegaly in many people as long as they continue to be taken (they do not provide a cure). Their use has been limited by the need to inject them and by their high cost. This may change as such drugs become longer acting and more readily available. Several new growth hormone blocker drugs, such as pegvisomant, are now available and may be useful for people who do not respond to somatostatin-type drugs.
Galactorrhea
Galactorrhea is the production of breast milk in men or in women who are not breastfeeding.
 The most common cause of galactorrhea is a tumor in the pituitary gland.
The most common cause of galactorrhea is a tumor in the pituitary gland.
 Galactorrhea can cause unexpected milk production and infertility in both men and women.
Galactorrhea can cause unexpected milk production and infertility in both men and women.
 The diagnosis is based on measuring the blood levels of the hormone prolactin.
The diagnosis is based on measuring the blood levels of the hormone prolactin.
 Imaging tests may be done to look for a cause.
Imaging tests may be done to look for a cause.
 When drugs alone do not stop prolactin production or shrink the tumor, surgery and sometimes radiation therapy may be done.
When drugs alone do not stop prolactin production or shrink the tumor, surgery and sometimes radiation therapy may be done.
In both sexes, the most common cause of galactorrhea is a prolactin-secreting tumor (prolactinoma) in the pituitary gland. Prolactinomas usually are very small when first diagnosed. They tend to be larger in men than in women, probably because they come to attention later. Overproduction of prolactin and the development of galactorrhea may also be induced by drugs, including phenothiazines, certain drugs given for high blood pressure (especially methyldopa), opioids, and birth control pills. There are other causes of galactorrhea that do not involve high levels of prolactin, such as an underactive thyroid gland (hypothyroidism).
 Did You Know…
Did You Know…
Galactorrhea can occur in both women and men.
Symptoms
Although unexpected breast milk production may be the only symptom of a prolactinoma, many women also stop menstruating (amenorrhea) or have less frequent menstrual periods. Women with prolactinomas often have low levels of estrogen, which can produce vaginal dryness, and thus discomfort with sexual intercourse. About two thirds of men with prolactinomas lose interest in sex (reduced libido) and have erectile dysfunction. A high prolactin level can cause infertility in both men and women.
When a prolactinoma is large, it may press on the nerves of the brain that are located just above the pituitary gland, causing the person to have headaches or to become blind in specific visual fields (see box on page 1460).
Diagnosis
The diagnosis is usually suspected in women when menstrual periods are reduced or absent or when breast milk is unexpectedly produced. It is also suspected in men with reduced libido and decreased levels of testosterone in the blood who are producing breast milk. It is confirmed by finding a high level of prolactin in the blood. Computed tomography (CT) or magnetic resonance imaging (MRI) scans are done to search for a prolactinoma. If no tumor is detected and there is no other apparent cause of the high prolactin level (such as a drug), a pituitary tumor is still the most likely cause, particularly in women. In this case, the tumor is probably too small to be seen on the scan.
If a prolactinoma is large on imaging studies, an ophthalmologist tests the person’s visual fields for possible effects on vision.
Treatment
Drugs can be given to stimulate dopamine, the chemical in the brain that blocks prolactin production. They include bromocriptine and cabergoline. These drugs are taken by mouth and are effective only as long as they are used. They seldom result in cure of the tumor. In most people, they lower prolactin levels enough to restore menstrual periods (in women), stop galactorrhea, and increase estrogen levels in women and testosterone levels in men, and they are often able to restore fertility. They also usually shrink the tumor and improve any vision problems. Surgery is also effective for treating small prolactinomas but is not usually used first because drug treatment is safe, effective, and easy to use.
When a person’s prolactin levels are not extraordinarily high and a CT or MRI scan shows only a small prolactinoma or none at all, a doctor may not recommend treatment. This is probably appropriate in women who are not having problems getting pregnant as a result of the high prolactin level, whose menstrual periods remain regular, and who are not troubled by galactorrhea, and in men whose testosterone level is not low. Low estrogen levels usually accompany amenorrhea and increase the risk of osteoporosis in women. Low testosterone levels increase the risk of osteoporosis in men.
To overcome the effects of low estrogen levels caused by a prolactinoma, estrogen or oral contraceptives that contain estrogen may be given to women with small prolactinomas who do not want to become pregnant. Although estrogen treatment has not been shown to stimulate the growth of small prolactinomas, most experts recommend a CT or MRI scan every year for at least 2 years to be sure the tumor is not enlarging substantially.
Doctors generally treat people who have larger tumors with drugs to stimulate dopamine (dopamine agonists—for example, bromocriptine or cabergoline) or with surgery. If drugs reduce the prolactin levels and symptoms disappear, surgery may not be necessary. These drugs are generally safe, but heart valve fibrosis and leakage have been reported recently when they were used to treat Parkinson’s disease in much higher doses than they are used to treat increased prolactin levels. Even when surgery is necessary, dopamine agonists may be prescribed to help shrink the tumor before the operation. They are often given after surgery, because a large prolactin-secreting tumor is unlikely to be cured with surgery. Occasionally, prolactinomas subside so the dopamine agonists can be stopped without the prolactin level rising again. This is more common with small tumors and after pregnancy.
Radiation therapy is sometimes needed, as for other pituitary tumors, when the tumor does not respond to medical or surgical treatment.
Empty Sella Syndrome
In empty sella syndrome, the sella turcica (the bony structure at the base of the brain that houses the pituitary gland) enlarges, but the pituitary remains normal-sized or shrinks.
People with empty sella syndrome have a defect in the tissue barrier that normally keeps the cerebrospinal fluid around the brain separate from the sella turcica. As a result, cerebrospinal fluid puts increased pressure on the pituitary gland and the walls of the sella turcica. The sella turcica may enlarge, and the pituitary gland may shrink.
Empty sella syndrome occurs most often in middle-aged women who are overweight and who have high blood pressure. Less commonly, the condition occurs after pituitary surgery, radiation therapy, or infarction (death) of a pituitary tumor.
The empty sella syndrome may produce no symptoms at all and seldom produces serious symptoms. About half of those affected have headaches, and some people have high blood pressure as well. In rare cases, there is leaking of the cerebrospinal fluid from the nose or problems with vision.
The empty sella syndrome can be diagnosed by computed tomography (CT) or magnetic resonance imaging (MRI) scanning. Pituitary function is checked to rule out hormone excess or deficiency, but it is almost always normal.
Treatment is indicated only for overproduction or underproduction of pituitary hormones and is seldom needed.