CHAPTER 154
Symptoms and Diagnosis of Blood Disorders
Disorders that affect the cells in the blood (blood cells) or proteins in the blood clotting or immune systems are called blood disorders or hematologic disorders. Laboratory tests to detect blood disorders generally begin with examination of the blood, which is easily obtained from a vein with a needle and syringe or sometimes from the fingertip by a needle prick. However, evaluation may require examination of the bone marrow, because that is where blood cells develop.
Symptoms
Symptoms of blood disorders are often vague and nonspecific, that is, they could indicate a disorder of almost any part of the body. However, although no single symptom unmistakably indicates a blood disorder, certain groups of symptoms suggest the possibility. Such groups of symptoms most commonly relate to decreases in blood cells, such as a reduced number of red blood cells (anemia), a reduced number of white blood cells (leukopenia), or a reduced number of platelets (thrombocytopenia). For example, a person who has fatigue, weakness, and shortness of breath may have anemia. A person who has fever and infection may have too few white blood cells. A person who bleeds or bruises easily may have too few platelets.
Occasionally, symptoms may relate to increased numbers of blood cells. For example, people with thickened (more viscous) blood due to increased numbers of red blood cells (polycythemia) or white blood cells may experience symptoms such as shortness of breath, headaches, dizziness, and confusion. Blood can also become thickened because of an increased production of immune-related proteins, as in multiple myeloma.
Finally, disorders of substances (factors) responsible for normal blood clotting may result in insufficient blood clotting (manifesting as excessive bruising or bleeding or as small red or purple spots on the skin) or in the formation of abnormal blood clots (producing warm, painful areas in the legs or sudden shortness of breath, chest pain, or both). These problems may arise because the body does not produce enough of these factors, the factors are abnormal, or the body is using up the factors too quickly.
Diagnosis
Laboratory Blood Tests
Doctors depend on many different laboratory tests of blood samples to diagnose and monitor diseases. Because the liquid portion of the blood (plasma) carries so many substances essential to the body’s functioning, blood tests can be used to find out what is happening in many parts of the body.
Testing blood is easier than obtaining a tissue sample from a specific organ. For example, thyroid function can be evaluated more easily by measuring the level of thyroid hormones in the blood than by directly sampling the thyroid. Likewise, measuring liver enzymes and proteins in the blood (see box on page 212) is easier than sampling the liver. However, certain blood tests are used to measure the components and function of the blood itself. These are the tests that are mostly used to diagnose blood disorders.
Complete Blood Count: The most commonly performed blood test is the complete blood count (CBC), which is an evaluation of all the cellular components (red blood cells, white blood cells, and platelets). Automated machines perform this test in less than 1 minute on a small drop of blood. The CBC is supplemented in some instances by examination of blood cells under a microscope.
The CBC determines the number of red blood cells and the amount of hemoglobin (the oxygen-carrying protein in red blood cells) in the blood. In addition, the average size, degree of variability of size, and hemoglobin content of red blood cells is assessed by a CBC and can alert laboratory workers to the presence of abnormal red blood cells (which may then be further characterized by microscopic examination). Abnormal red blood cells may be fragmented or shaped like teardrops, crescents, needles, or a variety of other forms. Knowing the specific shape and size of red blood cells can help a doctor diagnose a particular cause of anemia. For example, sickle-shaped cells are characteristic of sickle cell disease, small cells containing insufficient amounts of hemoglobin are likely due to iron deficiency anemia, and large oval cells suggest anemia due to a deficiency of folate (folic acid) or vitamin B12.
The CBC also determines the number of white blood cells. The specific types of white blood cells (see page 1022) can be counted (differential white blood cell count) when a doctor needs more information. If the total number of white blood cells or the number of one of the specific types of white blood cells is above or below normal, the doctor can examine these cells under a microscope. The microscopic examination can identify features that are characteristic of certain diseases. For example, large numbers of white blood cells that have a very immature appearance (blasts) may indicate leukemia (cancer of the white blood cells).
Platelets are usually also counted as part of a CBC. The number of platelets is an important measure of the blood’s protective mechanisms for stopping bleeding (clotting). A high number of platelets (thrombocytosis or thrombocythemia) can lead to blood clots in small blood vessels, especially those in the heart or brain. In some disorders, a high number of platelets may paradoxically result in excess bleeding.
Reticulocyte Count: The reticulocyte count measures the number of newly formed (young) red blood cells (reticulocytes) in a specified volume of blood. Reticulocytes normally make up about 1% of the total number of red blood cells. When the body needs more red blood cells, as in anemia, the bone marrow normally responds by producing more reticulocytes. Thus, the reticulocyte count is a measure of the capacity of the bone marrow to make new red blood cells.
Special Tests of Blood Cells: Once a doctor determines that something is wrong with one or more of the cell types in the blood, many additional tests are available to shed more light on the problem. Doctors can measure the proportion of the different types of white blood cells and can determine subtypes of these cells by assessing certain markers on the surface of the cells. Tests are available to measure the ability of white blood cells to fight infection, to assess the functioning of platelets and their ability to clot, and to measure the contents of red blood cells to help determine the cause of anemia or why the cells are not functioning properly. Most of these tests are done on samples of blood, but some require a sample from the bone marrow.
Clotting Tests: One measure of the body’s ability to stop bleeding is the count of the number of platelets.
COMPLETE BLOOD COUNT (CBC)
| TEST | WHAT IT MEASURES | NORMAL VALUES |
| Hemoglobin | Amount of this oxygen-carrying protein within red blood cells | Men: 12.7 to 13.7 grams per deciliter Women: 11.5 to 12.2 grams per deciliter |
| Hematocrit | Proportion of total blood volume made up of red blood cells | Men: 42 to 50% Women: 36 to 45% |
| Mean corpuscular volume | Average volume of individual red blood cells | 86 to 98 femtoliters |
| Mean corpuscular hemoglobin concentration | Average concentration of hemoglobin within red blood cells | 33.4 to 35.5 grams per deciliter |
| White blood cell count | Number of white blood cells in a specified volume of blood | 4,500 to 10,500 per microliter |
| Differential white blood cell count | Percentages of the different types of white blood cells | Segmented neutrophils: 34 to 75% Band neutrophils: 0 to 8% Lymphocytes: 12 to 50% Monocytes: 2 to 9% Eosinophils: 0 to 5% Basophils: 0 to 3% |
| Platelet count | Number of platelets in a specified volume of blood | 140,000 to 450,000 per microliter |
Sometimes doctors need to test how well the platelets function. Other tests can measure the overall function of the many proteins needed for normal blood clotting (clotting factors). The most common of these tests are the prothrombin time (PT) and the partial thromboplastin time (PTT). The levels of individual clotting factors can also be determined.
Proteins and Other Substances: Some blood cells produce proteins that can be measured in the blood or urine. Doctors may measure these proteins to determine if the cells are abnormal. For example, a blood disorder in which certain red blood cells, called plasma cells, become cancerous produces unusual proteins (Bence Jones proteins) that can be measured in blood and urine. Certain abnormal white blood cells produce unusual antibodies.
Erythropoietin is a protein made in the kidneys that stimulates the bone marrow to produce red blood cells. The level of this protein and several others that affect red blood cell production can be measured in the blood. Levels of iron and certain vitamins that are necessary for the production of healthy blood cells also can be measured.
Other Blood Tests: Specialized blood tests can be used to determine whether uncommon blood disorders are present. For example, on rare occasions, doctors must measure the total volume of blood or the total number of certain blood cells in the body. These measurements can be done using radioactive isotopes that mix in the blood or attach to blood cells.
Blood Typing: Blood type, which is determined by the presence of certain proteins on the surface of red blood cells, can be identified by measuring the reaction of a small sample of a person’s blood to certain antibodies. Blood typing requires evaluation of both the plasma and red blood cells. Blood typing must be done before blood can be transfused (see box on page 1027).
Bone Marrow Examination
Sometimes a sample of bone marrow must be examined to determine why blood cells are abnormal or why there are too few or too many of any kind of blood cell. A doctor can take two different types of bone marrow samples: a bone marrow aspirate and a bone marrow core biopsy. Both types are usually taken from the hipbone (iliac crest), although aspirates are rarely taken from the breastbone (sternum). In very young children, bone marrow samples are occasionally taken from one of the bones in the lower leg (tibia).
When both types of samples are needed, they are taken at the same time. After the skin and tissue over the bone are numbed with a local anesthetic, the sharp needle of a syringe is inserted into the
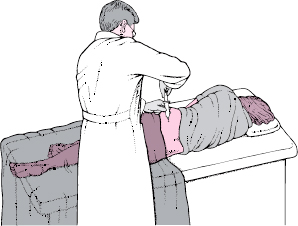
Taking a Bone Marrow Sample
Bone marrow samples are usually taken from the hipbone (iliac crest). The person may lie on one side, facing away from the doctor, with the knee of the top leg bent. After numbing the skin and tissue over the bone with a local anesthetic, the doctor inserts a needle into the bone and withdraws the marrow.
bone. For a bone marrow aspirate, the doctor pulls back on the plunger of the syringe and draws out a small amount of the soft bone marrow, which can be spread on a slide and examined under a microscope. Special tests, such as cultures for bacteria, fungi, or viruses, chromosomal analysis, and analysis of cell surface proteins (flow cytometry), can be performed on the sample. Although the aspirate often provides enough information for a diagnosis to be made, the process of drawing the marrow into the syringe breaks up the fragile bone marrow. As a result, determining the original arrangement of the cells is difficult.
When the exact anatomic relationships of cells must be determined and the structure of the tissues evaluated, the doctor also performs a core biopsy. A small core of intact bone marrow is removed with an internal coring device. This core is preserved and sliced into thin sections that are examined under a microscope.
A bone marrow sampling generally involves a slight jolt of pain, followed by minimal discomfort. The procedure takes a few minutes.