CHAPTER 174
Bacterial Infections
Bacteria are microscopic, single-celled organisms. There are thousands of different kinds, and they live in every conceivable environment all over the world. They live in soil, seawater, and deep within the earth’s crust. Some bacteria have been reported even to live in radioactive waste. Some bacteria live in the bodies of people and animals—on the skin and in the airways, mouth, and digestive, reproductive, and urinary tracts—often without causing any harm.
Only a few kinds of bacteria cause disease. They are called pathogens. Sometimes bacteria that normally reside harmlessly in the body cause disease. Bacteria can cause disease by producing harmful substances (toxins), invading tissues, or doing both.
Classification
Bacteria can be classified in several ways:
 Scientific names: Bacteria, like other living things, are classified by genus (based on having one or several similar characteristics) and, within the genus, by species. Their scientific name is genus followed by species (for example, Clostridium botulinum). Within a species, there may be different types, called strains. Strains differ in genetic makeup and chemical components. Sometimes certain drugs and vaccines are effective only against certain strains.
Scientific names: Bacteria, like other living things, are classified by genus (based on having one or several similar characteristics) and, within the genus, by species. Their scientific name is genus followed by species (for example, Clostridium botulinum). Within a species, there may be different types, called strains. Strains differ in genetic makeup and chemical components. Sometimes certain drugs and vaccines are effective only against certain strains.
 Staining: Bacteria may be classified by the color they turn after certain chemicals (stains) are applied to them. A commonly used stain is the Gram stain. Some bacteria stain blue. They are called gram-positive. Others stain pink. They are called gram-negative. Gram-positive and gram-negative bacteria stain differently because their cell walls are different. They also cause different types of infections, and different types of antibiotics are effective against them.
Staining: Bacteria may be classified by the color they turn after certain chemicals (stains) are applied to them. A commonly used stain is the Gram stain. Some bacteria stain blue. They are called gram-positive. Others stain pink. They are called gram-negative. Gram-positive and gram-negative bacteria stain differently because their cell walls are different. They also cause different types of infections, and different types of antibiotics are effective against them.
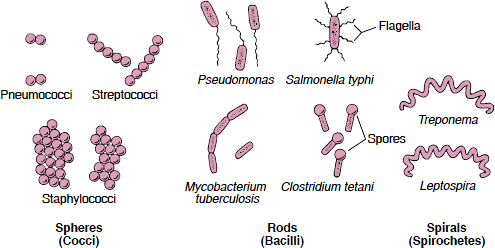
 Shapes: All bacteria may be classified as one of three basic shapes: spheres (cocci), rods (bacilli), and spirals or helixes (spirochetes).
Shapes: All bacteria may be classified as one of three basic shapes: spheres (cocci), rods (bacilli), and spirals or helixes (spirochetes).
 Need for oxygen: Bacteria are also classified by whether they need oxygen to live and grow. Those that need oxygen are called aerobes. Those that have trouble living or growing when oxygen is present are called anaerobes. Some bacteria, called facultative bacteria, can live and grow with or without oxygen.
Need for oxygen: Bacteria are also classified by whether they need oxygen to live and grow. Those that need oxygen are called aerobes. Those that have trouble living or growing when oxygen is present are called anaerobes. Some bacteria, called facultative bacteria, can live and grow with or without oxygen.
Bacterial Defenses
Bacteria have many ways of defending themselves.
Biofilm: Some bacteria secrete a substance that helps them attach to other bacteria, cells, or objects. This substance combines with the bacteria to form a sticky layer called biofilm. For example, certain bacteria form a biofilm on teeth (called dental plaque). The biofilm traps food particles, which the bacteria process and use, and in this process, they probably cause tooth decay. Biofilms also help protect bacteria from antibiotics.
Capsules: Some bacteria are enclosed in a protective capsule. This capsule helps prevent white blood cells, which fight infection, from ingesting the bacteria. Such bacteria are described as encapsulated.
Outer Membrane: Under the capsule, gram-negative bacteria have an outer membrane that protects them against certain antibiotics. When disrupted, this membrane releases toxic substances called endotoxins. Endotoxins contribute to the severity of symptoms during infections with gram-negative bacteria.
Spores: Some bacteria produce spores, which are an inactive (dormant) form. Spores can enable bacteria to survive when environmental conditions are difficult. When conditions are favorable, each spore germinates into an active bacterium.
Flagella: Flagella are long, thin filaments that protrude from the cell surface and enable bacteria to move. Bacteria without flagella cannot move on their own.
Antibiotic Resistance: Bacteria develop resistance to drugs because they acquire genes from other bacteria that have become resistant or because their genes mutate. For example, soon after the drug penicillin was introduced in the mid-1940s, a few individual Staphylococcus aureus bacteria acquired genes that made penicillin ineffective against them. The strains that possessed these special genes had a survival advantage when penicillin was commonly used to treat infections. Strains of Staphylococcus aureus that lacked these new genes were killed by penicillin, allowing the remaining penicillin-resistant bacteria to reproduce and over time become dominant. Chemists then altered the penicillin molecule, making a different but similar drug, methicillin, which could kill the penicillin-resistant bacteria. Soon after methicillin was introduced, strains of Staphylococcus aureus developed genes that made them resistant to methicillin and related drugs. These strains are called methicillinresistant Staphylococcus aureus (MRSA). The genes that encode for drug resistance can be passed to following generations of bacteria or sometimes even to other species of bacteria.
How Bacteria Shape Up
The more often antibiotics are used, the more likely resistant bacteria are to develop. Therefore, doctors try to use antibiotics only when they are necessary. Giving antibiotics to people who probably do not have a bacterial infection, such as those who have cough and cold symptoms, does not make people better but does help create resistant bacteria. Because antibiotics have been so widely used (and misused), many bacteria are resistant to certain antibiotics.
Resistant bacteria can spread from person to person. Because international travel is so common, resistant bacteria can spread to many parts of the world in a short time. Spread of these bacteria in hospitals is a particular concern. Resistant bacteria are common in hospitals because antibiotics are so often necessary and hospital personnel and visitors may spread the bacteria if they do not strictly follow appropriate sanitary procedures. Also, many hospitalized patients have a weakened immune system, making them more susceptible to infection.
 Did You Know…
Did You Know…
Botulinum toxin, produced by clostridial bacteria, can cause food poisoning and muscle paralysis but can also be used to reduce wrinkles and to treat muscle spasms.
Resistant bacteria can also spread to people from animals. Resistant bacteria are common among farm animals because antibiotics are often routinely given to healthy animals to prevent infections that can impair growth or cause illness.
Actinomycosis
Actinomycosis is a chronic infection caused mainly by Actinomyces israelii, anaerobic bacteria that normally reside on the enamel of teeth, gums, tonsils, and membranes lining the intestines and vagina.
 Infection occurs only when tissue is broken, enabling the bacteria to enter deeper tissues.
Infection occurs only when tissue is broken, enabling the bacteria to enter deeper tissues.
 Abscesses form in various areas, such as the intestine or face, causing pain, fever, and other symptoms.
Abscesses form in various areas, such as the intestine or face, causing pain, fever, and other symptoms.
 Symptoms suggest the diagnosis, and doctors confirm it by taking x-rays and identifying the bacteria in a sample of infected tissue.
Symptoms suggest the diagnosis, and doctors confirm it by taking x-rays and identifying the bacteria in a sample of infected tissue.
 Abscesses are drained, and antibiotics are given.
Abscesses are drained, and antibiotics are given.
 With treatment, most people recover fully.
With treatment, most people recover fully.
These bacteria cause infection only when the surface of the tissue on which they reside is broken, enabling them to enter other, deeper tissues, which have no defenses against them. As the infection spreads, scar tissue and abnormal channels (called fistulas or tracts) form. After months to years, fistulas may eventually reach the skin and allow pus to drain. Pockets of pus (abscesses) may develop in the chest, abdomen, face, or neck.
Men are affected most often, but actinomycosis occasionally develops in women who use an intrauterine device (IUD).
Symptoms
Actinomycosis has several forms. All cause abscesses.
Abdominal: The bacteria infect the intestine, usually the area near the appendix, and the lining of the abdominal cavity (peritoneum). Chronic abdominal pain, fever, vomiting, diarrhea or constipation, and severe weight loss are common symptoms. Fistulas may form from the interior of the abdomen to the skin above it and between the intestine and other organs.
Pelvic: The bacteria spread to the uterus, usually from an IUD that has been in place for years. Abscesses and scar tissue may form in the fallopian tubes, ovaries, and nearby organs such as the bladder and ureters. Fistulas may form between these organs. Symptoms include chronic abdominal or pelvic pain, fever, weight loss, and vaginal bleeding and discharge.
Cervicofacial: Usually, small, hard, sometimes painful swellings develop in the mouth and on the face, neck, or skin below the jaw (lumpy jaw). These swellings may soften and discharge pus that contains small, round, yellowish granules. The infection may extend to the cheek, tongue, throat, salivary glands, skull, bones of the neck (cervical vertebrae) and face, brain, or the space within the tissues covering the brain (meninges).
Thoracic: This form affects the chest (thorax). People have chronic chest pain and fever. They lose weight and cough, sometimes bringing up sputum. People probably become infected when they inhale fluids that contain bacteria from their mouth. Abscesses may form in the lungs and eventually spread to the membrane between the lungs and chest wall (pleura). There, abscesses cause irritation (pleuritis), and infected fluid collects (called an empyema). Fistulas may form, enabling the infection to spread to the ribs, skin of the chest, and spine.
Generalized: Rarely, the bacteria are carried in the bloodstream to infect other organs, such as the brain, lungs, liver, kidneys, and heart valves.
Diagnosis
Doctors suspect the infection in people who have typical symptoms. Then, x-rays are taken, and samples of pus or tissue are obtained and checked for Actinomyces israelii. Often, a needle is inserted through the skin to take a sample from an abscess or infected tissue. Sometimes computed tomography (CT) or ultrasonography is used to help doctors place the needle in the infected area. Sometimes surgery is necessary to remove a sample.
Characteristic x-ray findings and identification of the bacteria in a sample confirm the diagnosis.
Treatment
Treatment consists of draining abscesses with a needle (usually inserted through the skin) and giving high doses of antibiotics such as penicillin or tetracycline. Antibiotics may be needed for as long as 6 to 12 months.
Bacteria in the Body
The body normally contains several hundred different species of bacteria but many trillions of individual bacteria. The bacteria outnumber the cells of the body by about 10 to 1. Most of these bacteria reside on the skin and teeth, in the spaces between teeth and gums, and in the mucous membranes that line the throat, intestine, and vagina. The species differ at each site, reflecting the different environment at each site. Many of them are anaerobes—that is, they do not require oxygen.
Usually, these anaerobes do not cause disease. Many have useful functions, such as helping break down food in the intestine. However, these bacteria can cause disease if the mucous membranes are damaged. Then, bacteria can enter tissues that are usually off-limits to them and that have no defenses against them. The bacteria may infect nearby structures (such as the sinuses, middle ear, lungs, brain, abdomen, pelvis, and skin) or enter the bloodstream and spread.
What Are Clostridia?
Clostridia are bacteria that normally reside in the intestine of 3 to 8% of healthy adults and even more newborns. Clostridia also reside in animals, soil, and decaying vegetation. These bacteria do not require oxygen to live. That is, they are anaerobes.
Clostridia cause disease in different ways, depending on the species:
 They may produce a toxin in food, which is then consumed, as occurs in foodborne botulism.
They may produce a toxin in food, which is then consumed, as occurs in foodborne botulism.
 They may produce a toxin after they are in the body if circumstances enable them to multiply excessively (overgrow), as occurs in tetanus, Clostridium perfringens food poisoning, and a type of antibiotic-associated diarrhea and colitis called Clostridium difficile-induced diarrhea and colitis.
They may produce a toxin after they are in the body if circumstances enable them to multiply excessively (overgrow), as occurs in tetanus, Clostridium perfringens food poisoning, and a type of antibiotic-associated diarrhea and colitis called Clostridium difficile-induced diarrhea and colitis.
 They may produce a toxin and invade tissue, causing infection, as occurs in gas gangrene.
They may produce a toxin and invade tissue, causing infection, as occurs in gas gangrene.
Clostridia can infect the gallbladder, colon, and female reproductive organs. Rarely, one species, Clostridium sordellii, causes toxic shock syndrome in women who have infections of the reproductive organs.
Clostridia may also spread to the blood (causing bacteremia). Widespread bacteremia (sepsis) can cause fever and serious symptoms such as low blood pressure, jaundice, and anemia. Sepsis can develop after a clostridial infection and be rapidly fatal.
Foodborne botulism can develop when people eat food that contains botulinum toxin, produced by Clostridium botulinum. Usually, botulism results from eating uncooked or undercooked food because heat (cooking) destroys the toxin. Botulinum toxin enters the bloodstream from the small intestine and is carried to nerves. This toxin prevents nerves from sending impulses to muscles. About 18 to 36 hours after consuming the toxin, people become tired and dizzy. Their mouth becomes dry. They may feel nauseated and vomit. The abdomen may swell (distend), and constipation may develop. Muscles of the face become slack or paralyzed, causing the eyelids and face to droop and vision to blur. Swallowing and talking become difficult. The muscle weakness then spreads to the upper torso and downward. The muscles involved in breathing may weaken—a problem that may become life threatening.
Clostridium perfringens food poisoning can develop when people eat food (usually beef) that contains bacteria (rather than the bacteria’s toxin). The bacteria develop from spores, which are inactive (dormant) forms of the bacteria that can survive the heat of cooking. If food that contains spores is not eaten soon after it is cooked, the spores develop into bacteria, which then multiply in the food. If the food is served without adequate reheating, the bacteria are consumed. They multiply in the small intestine and produce a toxin that causes watery diarrhea and abdominal cramping. This type of food poisoning is usually mild but can cause serious problems in older people. Rarely, certain strains of these bacteria produce a toxin that damages the intestine and causes an infection called necrotizing enteritis, which is often fatal.
Clostridium difficile-induced diarrhea and colitis (inflammation of the colon) can develop after antibiotics are taken to treat an infection (see page 176). Antibiotics may destroy some of the bacteria that normally reside in the intestine. If enough are destroyed, Clostridium difficile may overgrow. These bacteria may already be present in the intestine. Or people may get them from other people, pets, or the environment. Being very young or very old, staying in a hospital or nursing home, or having one or more severe disorders increases the risk of this disorder. When the bacteria overgrow, they release two toxins. One causes the intestine to produce fluids and abnormal membranes to form. The other damages the lining of the large intestine.
CT or magnetic resonance imaging (MRI) may be used to determine whether abscesses are resolving. Surgery, with or without antibiotics, may be necessary, particularly if the infection affects critical areas such as the spine.
If actinomycosis is diagnosed early and treated appropriately, most people recover fully.
Anthrax
Anthrax is a potentially fatal infection with Bacillus anthracis, which may affect the skin, the lungs, or, rarely, the digestive (gastrointestinal) tract.
 Infection in people usually results from skin contact but can result from inhaling spores or eating contaminated meat.
Infection in people usually results from skin contact but can result from inhaling spores or eating contaminated meat.
 Symptoms include bumps and blisters (after skin contact), difficulty breathing and chest pain (after inhaling spores), and abdominal pain and bloody diarrhea (after eating contaminated meat).
Symptoms include bumps and blisters (after skin contact), difficulty breathing and chest pain (after inhaling spores), and abdominal pain and bloody diarrhea (after eating contaminated meat).
 Symptoms suggest the infection, and identifying the bacteria in samples taken from infected tissue confirms the diagnosis.
Symptoms suggest the infection, and identifying the bacteria in samples taken from infected tissue confirms the diagnosis.
 People at high risk of being exposed to anthrax are vaccinated.
People at high risk of being exposed to anthrax are vaccinated.
 Antibiotics must be given soon after exposure to reduce the risk of dying.
Antibiotics must be given soon after exposure to reduce the risk of dying.
Anthrax can occur in wild and domestic animals that graze, such as cattle, sheep, and goats. Anthrax bacteria produce spores that can live for years in soil. Grazing animals become infected when they have contact with or consume the spores. Usually, anthrax is transmitted to people when they have contact with infected animals or animal products (such as wool, hides, and hair). Spores may remain in animal products for decades and are not easily killed by cold or heat. Even minimal contact is likely to result in infection. Although infection in people usually occurs through the skin, it can also result from inhaling spores or eating contaminated, undercooked meat. Anthrax cannot spread from person to person.
Anthrax is a potential biological weapon because anthrax spores can be spread through the air and inhaled.
Anthrax bacteria produce several toxins, which cause many of the symptoms.
Symptoms
Symptoms vary depending on how the infection is acquired: through the skin, through inhalation, or through the gastrointestinal tract.
Skin Anthrax: More than 95% of cases involve the skin. A painless, itchy, red-brown bump appears 1 to 12 days after exposure. The bump forms a blister, which eventually breaks open and forms a black scab (eschar), with swelling around it. Nearby lymph nodes may swell, and people may feel ill—sometimes with muscle aches, headache, fever, nausea, and vomiting. About 20% of untreated people die, but with treatment, death is rare.
Inhalation Anthrax (Woolsorter’s Disease): This form is the most serious. It results from inhaling anthrax spores. Spores may stay in the lungs for weeks but eventually enter white blood cells, where they germinate, and the resulting bacteria multiply and spread to lymph nodes in the chest. The bacteria produce toxins that make the lymph nodes swell, break down, and bleed, spreading the infection to nearby structures. Infected fluid accumulates in the space between the lungs and the chest wall.
Symptoms develop 1 to 43 days after exposure. Initially, they are vague and similar to those of influenza, with mild muscle aches, a low fever, chest discomfort, and a dry cough. After a few days, breathing suddenly becomes very difficult, and people have chest pain and a high fever with sweating. Blood pressure rapidly becomes dangerously low (causing shock), followed by coma. These severe symptoms probably result from a massive release of toxins. Infection of the brain and the fluid around the meninges (an infection called meningoencephalitis) frequently develops. Many people die 24 to 36 hours after severe symptoms start, even with early treatment. Without treatment, all people with inhalation anthrax die. In the 2001 outbreak in the United States, 5 of the 11 people treated for inhalation anthrax died.
Gastrointestinal Anthrax: Gastrointestinal anthrax is rare. When people eat contaminated meat, the bacteria grow in the mouth, throat, or intestine and release toxins that cause extensive bleeding and tissue death. People have a fever, a sore throat, a swollen neck, abdominal pain, and bloody diarrhea. They also vomit blood. At least half of untreated people with gastrointestinal anthrax die. With treatment, about half of people die.
 Did You Know…
Did You Know…
Anthrax spores are not easily killed by cold or heat and can survive for decades.
Over 1.25 million people have received the anthrax vaccine without having a serious adverse reaction.
Diagnosis
Doctors suspect skin anthrax based on its typical appearance. Knowing that people have had contact with animals or animal products or were in an area where other people developed anthrax supports the diagnosis. If inhalation anthrax is suspected, chest x-ray and computed tomography (CT) are done.
Samples from infected skin, fluids around the lungs, or stool are removed and examined with a microscope or cultured (enabling bacteria, if present, to multiply). Anthrax bacteria, if present, can be readily identified. If people have inhalation anthrax, doctors may also take samples of the sputum or blood or do a spinal tap (lumbar puncture) to obtain a sample of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid). The samples are examined and analyzed. Blood tests may be done to check for fragments of the bacteria’s genetic material or antibodies to the toxins produced by the bacteria.
Prevention and Treatment
A vaccine against anthrax can be given to people at high risk of infection. Because of anthrax’s potential as a biological weapon, most members of the armed forces have been vaccinated. To be effective, the vaccine must be given in six doses. Despite widely publicized anxiety, over 1.25 million people have received the anthrax vaccine without having serious adverse reactions.
People who are exposed to anthrax may be given an antibiotic by mouth, usually ciprofloxacin or doxycycline or, if they cannot take these antibiotics, amoxicillin. The antibiotic is continued for 60 days to prevent the infection from developing. People may not need to take the antibiotic as long if they are also given several doses of anthrax vaccine.
OTHER BACTERIAL INFECTIONS

The longer treatment is delayed, the greater the risk of death. Thus, treatment is usually started as soon as anthrax is first suspected:
 Skin anthrax is treated with ciprofloxacin or doxycycline given by mouth.
Skin anthrax is treated with ciprofloxacin or doxycycline given by mouth.
 Inhalation or gastrointestinal anthrax is treated with a combination of antibiotics, including intravenous ciprofloxacin or doxycycline plus clindamycin, with or without rifampin. Corticosteroids may help relieve symptoms of inhalational anthrax.
Inhalation or gastrointestinal anthrax is treated with a combination of antibiotics, including intravenous ciprofloxacin or doxycycline plus clindamycin, with or without rifampin. Corticosteroids may help relieve symptoms of inhalational anthrax.
Bejel, Yaws, and Pinta
Bejel, yaws (frambesia), and pinta are infections caused by bacteria (called treponemal spirochetes) that are closely related to Treponema pallidum, which causes the sexually transmitted disease syphilis.
 These very contagious infections are usually spread in areas where hygiene is poor.
These very contagious infections are usually spread in areas where hygiene is poor.
 Bejel causes mouth sores and destructive lumps in bone, yaws causes skin sores and disfiguring growths on the legs and around the nose and mouth, and pinta causes itchy patches on the skin.
Bejel causes mouth sores and destructive lumps in bone, yaws causes skin sores and disfiguring growths on the legs and around the nose and mouth, and pinta causes itchy patches on the skin.
 Doctors diagnose these infections when people have typical symptoms and have spent time in areas where the infections are common.
Doctors diagnose these infections when people have typical symptoms and have spent time in areas where the infections are common.
 One injection of penicillin kills the bacteria.
One injection of penicillin kills the bacteria.
Bejel, yaws, and pinta are treponematoses, as is syphilis. Unlike syphilis, these infections are transmitted by nonsexual contact—chiefly between children living in conditions of poor hygiene. Bejel may be spread when eating utensils are shared.
Bejel occurs mainly in the hot arid countries of the eastern Mediterranean region and Saharan West Africa. Yaws occurs in humid equatorial countries. Pinta is common among the natives of Mexico, Central America, and South America. Bejel, yaws, and pinta rarely occur in the United States, except among immigrants from areas of the world where these diseases are common.
Symptoms
Yaws and pinta, like syphilis, begin with skin symptoms. Bejel begins with mouth sores. These symptoms subside, and after a period with few or no symptoms, new symptoms develop.
Bejel affects the mucous membranes of the mouth, then the skin and bones. The initial mouth sore may not be noticed. Moist patches then develop in the mouth. They resolve over a period of months to years. During this time, people have few or no symptoms. Then, lumps develop in long bones, mainly leg bones, and in the tissues around the mouth, nose, and roof of the mouth (palate). These lumps destroy tissue, causing bones to be deformed and disfiguring the face.
Yaws also affects the skin and bones. Several weeks after exposure to Treponema, yaws begins as a slightly raised sore at the site of infection, usually on a leg. The sore heals, but soft nodules (granulomas) form, then break open on the face, arms, legs, and buttocks. The granulomas heal slowly and may recur. Painful open sores on the soles of the feet (crab yaws) may develop, making walking difficult. Later, areas of the shinbones may be destroyed, and many other destructive, disfiguring growths (gangosa), especially around the nose, mouth, and palate, may develop.
Pinta affects only the skin. It begins as flat, itchy, reddened areas on the hands, feet, legs, arms, face, or neck. After several months, slate-blue patches develop in the same areas on both sides of the body. They develop where bones are close to skin, for example, on the elbow. Later, the patches lose their color. The affected skin on the palms and soles may thicken.
Diagnosis
Doctors make the diagnosis when typical symptoms appear in people who live in or have visited an area where such infections are common. Because the bacteria that cause these infections and the bacteria that cause syphilis are so similar, people who have one of these infections test positive for syphilis.
Treatment
A single injection of penicillin kills the bacteria. Then, the skin can heal. However, some scarring may remain, particularly if a lot of tissue has been destroyed. People who are allergic to penicillin are given tetracycline if they are 8 years old or older or erythromycin if they are pregnant or under 8 years old. These drugs are given by mouth.
Because the infections are very contagious, public health officials try to identify and treat infected people and their close contacts.
Campylobacter Infections
Several species of Campylobacter (most commonly Campylobacter jejuni) can infect the digestive tract, often causing diarrhea.
 People can be infected when they consume contaminated food or drink or have contact with infected people or animals.
People can be infected when they consume contaminated food or drink or have contact with infected people or animals.
 These infections cause diarrhea, abdominal pain, and fever.
These infections cause diarrhea, abdominal pain, and fever.
 Identifying the bacteria in a stool sample confirms the diagnosis.
Identifying the bacteria in a stool sample confirms the diagnosis.
 For some people, replacing lost fluids is all that is needed, but if symptoms are severe, antibiotics are also needed.
For some people, replacing lost fluids is all that is needed, but if symptoms are severe, antibiotics are also needed.
Campylobacter bacteria normally inhabit the digestive tract of many farm animals (including cattle, sheep, pigs, and fowl). The feces of these animals may contaminate water in lakes and streams. Meat (usually poultry) and unpasteurized milk may also be contaminated. People may be infected in several ways:
 Eating or drinking contaminated (untreated) water, unpasteurized milk, undercooked meat (usually poultry), or food prepared on kitchen surfaces touched by contaminated meat
Eating or drinking contaminated (untreated) water, unpasteurized milk, undercooked meat (usually poultry), or food prepared on kitchen surfaces touched by contaminated meat
 Contact with an infected person (particularly oral-anal sexual contact)
Contact with an infected person (particularly oral-anal sexual contact)
 Contact with an infected animal
Contact with an infected animal
Campylobacter bacteria cause inflammation of the colon (colitis) that results in fever and diarrhea. These bacteria are a common cause of infectious diarrhea in the United States and among people who travel to countries where food or water may be contaminated. Infections are most commonly caused by Campylobacter jejuni.
Symptoms
Symptoms usually develop 2 to 5 days after exposure and continue for about 1 week. Symptoms of Campylobacter colitis include diarrhea, abdominal pain, and cramps, which may be severe. The diarrhea may be bloody and can be accompanied by nausea, vomiting, and fever ranging from 100 to 104° F (38 to 40° C).
In some people with colitis, the bloodstream is temporarily infected (called bacteremia). This infection usually causes no symptoms or complications. However, the bloodstream is repeatedly or continuously infected in a few people. This type of bacteremia usually develops in people with a disorder that weakens the immune system, such as AIDS, diabetes, or cancer. This infection causes a long-lasting or recurring fever. Other symptoms develop as the bloodstream carries the infection to other structures, such as the following:
 The space within the tissues covering the brain and spinal cord (causing meningitis)
The space within the tissues covering the brain and spinal cord (causing meningitis)
 Bones (causing osteomyelitis)
Bones (causing osteomyelitis)
 Joints (causing infectious arthritis)
Joints (causing infectious arthritis)
 Rarely, heart valves (causing endocarditis)
Rarely, heart valves (causing endocarditis)
Guillain-Barré syndrome (see page 828) develops in about 1 of 1,000 of people with Campylobacter colitis. Guillain-Barré syndrome causes weakness or paralysis. Most people recover, but muscles may be greatly weakened. People may have difficulty breathing and need to use a mechanical ventilator. Weakness does not always completely resolve. Campylobacter colitis is thought to trigger about 20 to 40% of all cases of Guillain-Barré syndrome.
Weeks to months after the diarrhea resolves, reactive arthritis may develop. Usually, the disorder causes inflammation and pain in the knees, hips, and Achilles tendon.
Diagnosis
Doctors may take a sample of stool and send it to a laboratory to grow (culture) the bacteria. However, stool is not always tested. Stool cultures take days to complete, and doctors do not usually need to know which bacteria caused the diarrhea to effectively treat it. If the bacteria are identified, they are tested to see which antibiotics are effective (a process called susceptibility testing).
If doctors suspect that the bloodstream is infected, they take a sample of blood to be cultured.
Treatment
Many people get better in a week or so without specific treatment. Some people require extra fluids intravenously or by mouth. People who have a high fever, bloody or severe diarrhea, or worsening symptoms may need to take azithromycin for 3 days or erythromycin for 5 days. Both drugs are taken by mouth. If the bloodstream is infected, antibiotics such as imipenem, gentamicin, or azithromycin are required for 2 to 4 weeks.
Cholera
Cholera is a serious infection of the intestine that is caused by the bacteria Vibrio cholerae and that causes severe diarrhea.
 People are infected when they consume contaminated food, often seafood, or water.
People are infected when they consume contaminated food, often seafood, or water.
 Cholera is rare except in areas where sanitation is inadequate.
Cholera is rare except in areas where sanitation is inadequate.
 People have watery diarrhea and vomit, usually with no fever.
People have watery diarrhea and vomit, usually with no fever.
 Identifying the bacteria in a stool sample confirms the diagnosis.
Identifying the bacteria in a stool sample confirms the diagnosis.
 Replacing lost fluids and giving antibiotics treat the infection effectively.
Replacing lost fluids and giving antibiotics treat the infection effectively.
Several species of Vibrio bacteria cause diarrhea (see page 149). The most serious illness, cholera, is caused by Vibrio cholerae. Cholera may occur in large outbreaks.
Vibrio cholerae normally lives in aquatic environments along the coast. People acquire the infection by consuming contaminated water, seafood, or other foods. Once infected, people excrete the bacteria in stool. Thus, the infection can spread rapidly, particularly in areas where human waste is untreated.
Once common throughout the world, cholera is now largely confined to developing countries in the tropics and subtropics. It is common (endemic) in parts of Asia, the Middle East, Africa, and South and Central America. Small outbreaks have occurred in Europe, Japan, and Australia. In the United States, cholera can occur along the coast of the Gulf of Mexico.
In endemic areas, outbreaks usually occur when war or civil unrest disrupts public sanitation services. Infection is most common during warm months and among children. In newly affected areas, outbreaks may occur during any season and affect all ages equally.
For infection to develop, many bacteria must be consumed. Then, there may be too many for stomach acid to kill, and some bacteria can reach the small intestine, where they grow and produce a toxin. The toxin causes the small intestine to secrete enormous amounts of salt and water. The body loses this fluid as watery diarrhea. It is the loss of water and salt that causes death. The bacteria remain in the small intestine and do not invade tissues.
Because stomach acid kills the bacteria, people who produce less stomach acid are more likely to get cholera. Such people include young children, older people, and people taking drugs that reduce stomach acid, including proton pump inhibitors (such as omeprazole) and histamine-2 (H2) blockers (such as ranitidine). People living in endemic areas gradually acquire some immunity.
Symptoms
Most infected people have no symptoms. When symptoms occur, they begin 1 to 3 days after exposure, usually with sudden, painless, watery diarrhea and vomiting. Usually, fever is absent.
 Did You Know…
Did You Know…
Without treatment, more than one half of people with severe cholera die.
Diarrhea and vomiting may be mild to severe. In severe infections, more than 1 quart of water and salts is lost per hour. The stool looks gray and has flecks of mucus in it. Within hours, dehydration can become severe, causing intense thirst, muscle cramps, and weakness. Very little urine is produced. The eyes may become sunken, and the skin on the fingers may become very wrinkled. If dehydration is not treated, loss of water and salts can lead to kidney failure, shock, coma, and death.
In people who survive, symptoms usually subside in 3 to 6 days. Most people are free of the bacteria in 2 weeks. The bacteria remain in a few people indefinitely without causing symptoms. Such people are called carriers.
Diagnosis
Doctors take a sample of stool or use a swab to obtain a sample from the rectum. It is sent to a laboratory where bacteria can be grown (cultured). Identifying Vibrio cholerae in the sample confirms the diagnosis.
Blood and urine tests to evaluate dehydration and kidney function are done.
Prevention
Purification of water supplies and appropriate disposal of human waste are essential. Other precautions include using boiled or chlorinated water and avoiding uncooked vegetables and undercooked fish and shellfish. Shellfish tend to carry other forms of Vibrio as well.
Several vaccines for cholera are available outside the United States. These vaccines provide only partial protection for a limited time and therefore are not generally recommended. New vaccines are currently being tested.
Treatment
Rapid replacement of lost body water and salts is lifesaving. Most people can be treated effectively with a solution given by mouth. These solutions are designed to replace the fluids the body has lost. For severely dehydrated people who cannot drink, a salt solution is given intravenously. In epidemics, if the intravenous solution is not available, people are sometimes given a salt solution through a tube inserted through the nose into the stomach. After enough fluids are replaced to relieve symptoms, people should drink at least enough of the salt solution to replace the fluids they have lost through diarrhea and vomiting. Solid foods can be eaten after vomiting stops and appetite returns.
People are usually given an antibiotic to reduce the severity of diarrhea and make it stop sooner. Also, people who take an antibiotic are slightly less likely to spread the infection during an outbreak. Tetracycline or doxycycline is effective in adults, unless the bacteria in the area are resistant to tetracycline. Then, ciprofloxacin can be used. Because tetracycline and doxycycline discolor the teeth in children under 8 years old, azithromycin, erythromycin, or trimethoprim-sulfamethoxazole is used instead.
More than 50% of untreated people with severe cholera die. Less than 1% of people who receive prompt, adequate fluid replacement die.
Gas Gangrene
Gas gangrene (clostridial myonecrosis) is a life-threatening infection of muscle tissue caused mainly by the anaerobic bacteria Clostridium perfringens and several other species of clostridia.
 Gas gangrene can develop after certain types of surgery or injuries.
Gas gangrene can develop after certain types of surgery or injuries.
 Blisters with gas bubbles form near the infected area, and the heartbeat and breathing become rapid.
Blisters with gas bubbles form near the infected area, and the heartbeat and breathing become rapid.
 Symptoms suggest the diagnosis, and imaging tests or culture of a sample taken from infected tissue is usually done.
Symptoms suggest the diagnosis, and imaging tests or culture of a sample taken from infected tissue is usually done.
 Treatment involves high doses of antibiotics and surgical removal of dead or infected tissue.
Treatment involves high doses of antibiotics and surgical removal of dead or infected tissue.
Gas gangrene is a fast-spreading clostridial infection of muscle tissue that, if untreated, quickly leads to death. The bacteria produce gas that becomes trapped in the infected tissue. Several thousand cases occur in the United States every year. Gas gangrene usually develops after injuries or surgery. High-risk injuries include wounds that
 Are deep and severe
Are deep and severe
 Involve muscle
Involve muscle
 Are contaminated with dirt, decaying vegetable matter, or the person’s stool
Are contaminated with dirt, decaying vegetable matter, or the person’s stool
 Contain crushed or dead tissue
Contain crushed or dead tissue
High-risk surgery includes operations on the colon or gallbladder.
Gas gangrene can occur when there is no injury or surgery—usually in people with colon cancer. People with open fractures and frostbite are also susceptible to gas gangrene. Gas gangrene may develop when a contaminated needle is used to inject an illegal drug into a muscle.
Symptoms
Gas gangrene causes severe pain in the infected area. Initially, the area is swollen and pale but eventually turns red, then bronze, and finally blackish green. Large blisters often form. Gas bubbles may be visible within the blister or may be felt under the skin, usually after the infection progresses. Fluids draining from the wound smell rotten (putrid).
People quickly become sweaty and very anxious. They may vomit. Heart rate and breathing often become rapid. In some people, the skin turns yellow, indicating jaundice. These effects are caused by toxins produced by the bacteria. Typically, people remain alert until late in the illness, when dangerously low blood pressure (shock) and coma develop. Kidney failure and death rapidly follow.
Without treatment, death occurs within 48 hours. Even with treatment, about one of eight people with an infected limb and about two of three people with infection in the torso die.
Diagnosis
The initial diagnosis is based on symptoms and results of a physical examination. X-rays are taken to check for gas bubbles in muscle tissue, or computed tomography (CT) or magnetic resonance imaging (MRI) is done to check for signs of muscle involvement. These findings support the diagnosis. However, gas bubbles may also occur in other anaerobic infections.
Fluids from the wound are examined under a microscope to check for clostridia, and cultures are done to confirm their presence. However, not all people with clostridia have gas gangrene. Confirmation of the diagnosis may require exploratory surgery or removal of a tissue sample for examination under a microscope (biopsy) to check for characteristic changes in muscle.
Prevention and Treatment
Doctors do the following to prevent gas gangrene:
 Clean wounds thoroughly
Clean wounds thoroughly
 Remove foreign objects and dead tissue from wounds
Remove foreign objects and dead tissue from wounds
 Give antibiotics intravenously before, during, and after abdominal surgery to prevent infection
Give antibiotics intravenously before, during, and after abdominal surgery to prevent infection
No vaccine can prevent clostridial infection.
If gas gangrene is suspected, treatment must begin immediately. High doses of antibiotics, typically penicillin and clindamycin, are given, and all dead and infected tissue is removed surgically. About one of five people with gas gangrene in a limb requires amputation. Treatment in a high-pressure oxygen (hyperbaric oxygen) chamber is of uncertain value, and such chambers are not always readily available.
Klebsiella, Enterobacter, and Serratia Infections
Klebsiella, Enterobacter, and Serratia are closely related gram-negative bacteria that occasionally infect people in hospitals or in long-term care facilities.
 These bacteria may infect the urinary or respiratory tract, intravenous catheters used to give drugs or fluids, burns, wounds made during surgery, or the bloodstream.
These bacteria may infect the urinary or respiratory tract, intravenous catheters used to give drugs or fluids, burns, wounds made during surgery, or the bloodstream.
 Identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
Identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
 If the infection is acquired in the community, antibiotics can cure it, but if it is acquired in a health care facility, it is difficult to treat because bacteria tend to be resistant.
If the infection is acquired in the community, antibiotics can cure it, but if it is acquired in a health care facility, it is difficult to treat because bacteria tend to be resistant.
Klebsiella bacteria reside in the intestine of up to one third of healthy people. Enterobacter and Serratia bacteria usually reside outside the body, often in hospitals and long-term care facilities. People in such places can become infected.
These bacteria may infect different areas:
 Urinary or respiratory tract
Urinary or respiratory tract
 Catheters inserted into a vein (intravenous catheter), used to administer drugs or fluids
Catheters inserted into a vein (intravenous catheter), used to administer drugs or fluids
 Burns
Burns
 Wounds made during surgery
Wounds made during surgery
 Bloodstream
Bloodstream
Rarely, Klebsiella bacteria cause pneumonia in people who live outside a health care facility (in the community), usually in alcoholics, older people, people with diabetes, or people with a weakened immune system. Typically, this severe infection causes cough, bringing up a sticky, dark brown or dark red sputum, and collections of pus (abscesses) in the lung or in the membrane between the lungs and chest wall (empyema).
One species of Klebsiella can cause inflammation of the colon (colitis) after antibiotics are taken. This disorder is called antibiotic-associated colitis. The antibiotics kill bacteria that normally reside in the intestine. Then Klebsiella bacteria are able to multiply and cause problems. However, this type of colitis usually results from toxins produced by Clostridium difficile (see page 176).
Diagnosis
Doctors suspect one of these infections in people at high risk of getting one, such as people who live in a long-term care facility or in a place when there was an outbreak. To confirm the diagnosis, doctors take a sample of sputum, lung secretions (obtained through a bronchoscope), blood, urine, or infected tissue. The sample is stained with Gram stain, cultured, and examined under a microscope. These bacteria can be readily identified.
Other tests depend on the type of infection. They may include imaging tests, such as ultrasonography, x-rays, and computed tomography (CT).
Bacteria identified in samples are tested to determine which antibiotics are likely to be effective (a process called susceptibility testing).
Treatment
If Klebsiella pneumonia is acquired in the community, antibiotics, usually a cephalosporin (such as ceftriaxone) or fluoroquinolone (such as levofloxacin), given intravenously, can cure it.
If an infection with any of these three bacteria is acquired in a health care facility, the infection is difficult to treat because bacteria acquired in such facilities are usually resistant to many antibiotics.
Escherichia coli Infections
Escherichia coli (E. coli) is a group of gram-negative bacteria that normally reside in the intestine of healthy people, but some strains can cause infection.
 People develop intestinal E. coli infections by eating contaminated food, touching infected animals, or swallowing contaminated water in a pool.
People develop intestinal E. coli infections by eating contaminated food, touching infected animals, or swallowing contaminated water in a pool.
 Intestinal infections can cause diarrhea, sometimes severe or bloody, and abdominal pain.
Intestinal infections can cause diarrhea, sometimes severe or bloody, and abdominal pain.
 Antibiotics can effectively treat E. coli infections outside the digestive tract and most intestinal infections but are not used to treat intestinal infections by one strain of these bacteria.
Antibiotics can effectively treat E. coli infections outside the digestive tract and most intestinal infections but are not used to treat intestinal infections by one strain of these bacteria.
Some strains of E. coli normally inhabit the digestive tract of healthy people. However, some strains of E. coli cause infection in the digestive tract and in other parts of the body, most commonly the urinary tract. E. coli is the most common cause of bladder infection in women. These bacteria can also cause infection of the prostate gland (prostatitis), gallbladder infection, infections that develop after appendicitis and diverticulitis, wound infections (including wounds made during surgery), infections in pressure sores, foot infections in people with diabetes, pneumonia, meningitis in newborns, and bloodstream infections. Many E. coli infections affecting areas outside the digestive tract develop in people who are debilitated, who are staying in a health care facility, or who have taken antibiotics.
One strain produces a toxin that causes brief watery diarrhea. This disorder (called traveler’s diarrhea—see page 152) usually occurs in travelers who consume contaminated food or water in areas where water is not adequately purified.
Another strain (E. coli O157:H7) produces a toxin that damages the colon and causes inflammation (colitis). People are usually infected with this strain by doing the following:
 Eating contaminated ground beef that is not cooked thoroughly (one of the most common sources)
Eating contaminated ground beef that is not cooked thoroughly (one of the most common sources)
 Going to a petting zoo and touching animals that carry the bacteria in their digestive tract
Going to a petting zoo and touching animals that carry the bacteria in their digestive tract
 Eating ready-to-eat food (such as produce at salad bars) that was washed with contaminated water or contaminated by cattle manure
Eating ready-to-eat food (such as produce at salad bars) that was washed with contaminated water or contaminated by cattle manure
 Swallowing inadequately chlorinated water that has been contaminated by the stool of infected people in swimming or wading pools
Swallowing inadequately chlorinated water that has been contaminated by the stool of infected people in swimming or wading pools
Inadequate hygiene, particularly common among young children in diapers, can easily spread the bacteria from person to person.
Symptoms
Symptoms depend on the part of the body affected and the strain of E. coli causing the infection.
In infections due to E. coli O157:H7, diarrhea begins about 3 days after exposure. Diarrhea becomes bloody about 1 to 3 days later. (This disease is sometimes called hemorrhagic colitis.) People usually have severe abdominal pain and diarrhea many times a day. They also often feel an urge to defecate but may not be able to. Most people do not have a fever. Because the infection is easily spread, people must often be hospitalized and isolated.
The diarrhea resolves on its own in 85% of people. However, in about 15% of children and fewer older people, red blood cells are destroyed and kidney failure occurs about 1 week after symptoms begin. This complication (called hemolytic-uremic syndrome—see page 1042) is a common cause of chronic kidney disease in children.
 Did You Know…
Did You Know…
E. coli is the most common cause of bladder infection in women.
Diagnosis
Samples of blood, stool, sometimes urine, or other infected material are taken and sent to a laboratory to grow (culture) the bacteria. Identifying the bacteria in the sample confirms the diagnosis. If the bacteria are identified, they may be tested to see which antibiotics are effective (a process called susceptibility testing).
If E. coli O157:H7 is detected, blood tests must be done frequently to check for hemolytic-uremic syndrome.
Treatment
For traveler’s diarrhea, loperamide can be given to slow movement of food through the intestine and thus help control diarrhea. Antibiotics (such as azithromycin, ciprofloxacin, or rifaximin) can also be given to end symptoms more quickly.
Many people with diarrhea due to E. coli O157:H7 need to be given fluids containing salts intravenously. This infection is not treated with loperamide or antibiotics. Antibiotics may make diarrhea worse and increase the risk of hemolytic-uremic syndrome. If hemolytic-uremic syndrome develops, people are admitted to an intensive care unit and may require hemodialysis.
Many other E. coli infections, usually bladder or other urinary tract infections, are treated with antibiotics, such as trimethoprim-sulfamethoxazole or a fluoroquinolone. However, many bacteria, particularly those acquired in a health care facility, are resistant to these antibiotics. For more serious infections, antibiotics that are effective against many different bacteria (broad-spectrum antibiotics) may be used. Several antibiotics may be used together until doctors get the test results indicating which antibiotics are likely to be effective.
Haemophilus influenzae Infections
Haemophilus influenzae can cause infection in the respiratory tract, which can spread to other organs.
 Infection is spread through sneezing, coughing, or touching.
Infection is spread through sneezing, coughing, or touching.
 The bacteria can cause middle ear infections, sinusitis, and more serious infections, including meningitis and epiglottitis.
The bacteria can cause middle ear infections, sinusitis, and more serious infections, including meningitis and epiglottitis.
 Identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
Identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
 Children are routinely given a vaccine that effectively prevents infections due to Haemophilus influenzae type b.
Children are routinely given a vaccine that effectively prevents infections due to Haemophilus influenzae type b.
 Infections are treated with antibiotics given by mouth or, for serious infections, intravenously.
Infections are treated with antibiotics given by mouth or, for serious infections, intravenously.
Many species of Haemophilus normally reside in the upper airways of children and adults and rarely cause disease. One species causes chancroid, a sexually transmitted disease. Other species cause infections of heart valves (endocarditis) and, rarely, collections of pus (abscesses) in the brain, lungs, and liver. The species responsible for the most infections is Haemophilus influenzae.
Haemophilus influenzae can cause infections in children and sometimes in adults who have a chronic lung disorder or a weakened immune system. Infection is spread by sneezing, coughing, or touching infected people. One type of Haemophilus influenzae, called type b, is more likely to cause serious infections.
In children, Haemophilus influenzae type b (Hib) can spread through the bloodstream (causing bacteremia) and infect the joints, bones, lungs, skin of the face and neck, eyes, urinary tract, and other organs. The bacteria may cause two severe, often fatal infections: meningitis and epiglottitis (infection of the flap of tissue over the voice box). Some strains cause infection of the middle ear in children, the sinuses in children and adults, and the lungs in adults, especially those with chronic obstructive pulmonary disease (COPD) or AIDS.
Symptoms and Diagnosis
Symptoms vary depending on the part of the body affected.
To diagnose the infection, doctors take a sample of blood, pus, or other body fluids and send it to a laboratory to grow (culture) the bacteria. If people have symptoms of meningitis, doctors do a spinal tap (lumbar puncture) to obtain a sample of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid). Identifying the bacteria in a sample confirms the diagnosis.
Prevention and Treatment
Children are routinely vaccinated against Haemophilus influenzae type b. The vaccine is very effective, especially in preventing meningitis, epiglottitis, and bacteremia.
Treatment of meningitis must begin as soon as possible. An antibiotic—usually, ceftriaxone or cefotaxime—is given intravenously. Corticosteroids may help prevent brain damage.
Epiglottitis must also be treated as soon as possible. People may need help breathing. An artificial airway, such as a breathing tube, may be inserted, or rarely, an opening may be made in the windpipe (a procedure called tracheostomy). The antibiotic rifampin is used because it can eradicate the bacteria from the throat. People are given this antibiotic before they are discharged from the hospital.
If the household of a person with a serious Haemophilus influenzae type b infection includes a child who is under 4 years old and is not fully immunized against Haemophilus influenzae type b, the child should be vaccinated. Also, all members of the household, except pregnant women, should be given an antibiotic, such as rifampin, by mouth to prevent infection.
Other Haemophilus influenzae infections are treated with various antibiotics given by mouth. They include amoxicillin-clavulanate, azithromycin, cephalosporins, clarithromycin, fluoroquinolones, and trimethoprim-sulfamethoxazole.
Leptospirosis
Leptospirosis is a potentially serious disorder caused by Leptospira bacteria.
 Most people are infected through contact with contaminated soil or water during outdoor activities.
Most people are infected through contact with contaminated soil or water during outdoor activities.
 Fever, headache, and other symptoms occur in two phases, separated by a few days.
Fever, headache, and other symptoms occur in two phases, separated by a few days.
 A severe, potentially fatal form damages many organs, including the liver and kidneys.
A severe, potentially fatal form damages many organs, including the liver and kidneys.
 Detecting antibodies against the bacteria in blood or identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
Detecting antibodies against the bacteria in blood or identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
 Antibiotics and sometimes fluids containing salts are given, but people with the severe form may require transfusions and hemodialysis.
Antibiotics and sometimes fluids containing salts are given, but people with the severe form may require transfusions and hemodialysis.
Leptospirosis occurs in many wild and domestic animals. Some animals act as carriers and pass the bacteria in their urine. Others become ill and die. People acquire these infections directly through infected animals or indirectly through soil or water contaminated by urine from an infected animal.
Leptospirosis is an occupational disease of farmers and sewer and slaughterhouse workers. However, most people become infected during outdoor activities when they come in contact with contaminated soil or water, particularly while swimming or wading. The 40 to 100 infections reported every year in the United States occur mainly in the late summer and early fall. Because mild leptospirosis typically causes vague, flu-like symptoms that go away on their own, many infections are probably unreported.
Symptoms
In about 90% of infected people, symptoms are mild. In the rest, the disorder involves many organs. This potentially fatal form of leptospirosis is called Weil’s syndrome.
Leptospirosis usually occurs in two phases:
 First phase: About 2 to 20 days after infection occurs, fever, headache, nausea, vomiting, severe muscle aches in the calves and back, and chills occur suddenly. The eyes usually become very red on the third or fourth day. Some people cough, occasionally bringing up blood, and have chest pain. Most people recover within 1 week.
First phase: About 2 to 20 days after infection occurs, fever, headache, nausea, vomiting, severe muscle aches in the calves and back, and chills occur suddenly. The eyes usually become very red on the third or fourth day. Some people cough, occasionally bringing up blood, and have chest pain. Most people recover within 1 week.
 Second (immune) phase: In some people, symptoms recur a few days later. They result from inflammation caused by the immune system as it eliminates the bacteria from the body. The fever returns, and the space within the tissues covering the brain and spinal cord (meninges) often becomes inflamed. This inflammation (meningitis) causes a stiff neck and headache.
Second (immune) phase: In some people, symptoms recur a few days later. They result from inflammation caused by the immune system as it eliminates the bacteria from the body. The fever returns, and the space within the tissues covering the brain and spinal cord (meninges) often becomes inflamed. This inflammation (meningitis) causes a stiff neck and headache.
Weil’s Syndrome: This form can occur during the second phase. It causes jaundice (yellowish discoloration of the skin and whites of the eyes), kidney failure, and a tendency to bleed. People may have nosebleeds or cough up blood, or bleeding may occur within tissues in the skin, lungs, and, less commonly, digestive tract. Anemia can develop. Several organs such as the heart, lungs, and kidneys may stop functioning.
Most people who do not develop jaundice recover. About 5 to 10% of people with jaundice (which indicates liver damage) die. The death rate is probably higher in people with Weil’s syndrome and people over 60. If leptospirosis develops during early pregnancy, the risk of miscarriage is increased.
Diagnosis
To confirm the diagnosis, doctors take a sample of blood and urine. These samples are analyzed. If people have symptoms of meningitis, doctors do a spinal tap (lumbar puncture) to obtain a sample of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid). Usually, several samples are taken over several weeks. These samples are sent to a laboratory to grow (culture) the bacteria.
Identifying the bacteria in cultures or, more commonly, detecting antibodies against the bacteria in blood confirms the diagnosis.
Prevention and Treatment
The antibiotic doxycycline can prevent leptospirosis. It is given to people who were exposed to the bacteria at the same time as people who have been infected.
Mild infections are treated with antibiotics such as amoxicillin or doxycycline, given by mouth. For severe infections, antibiotics such as penicillin, doxycycline, or erythromycin may be given intravenously. Fluids containing salts may also be given. People with the infection do not have to be isolated, but care must be taken when handling and disposing of their urine.
People with Weil’s syndrome may need blood transfusions and hemodialysis.
Listeriosis
Listeriosis is infection caused by the gram-positive bacteria Listeria monocytogenes.
 People may consume the bacteria in commercially prepared foods that require no further cooking.
People may consume the bacteria in commercially prepared foods that require no further cooking.
 People have fever, chills, and muscle aches plus nausea, vomiting, and diarrhea.
People have fever, chills, and muscle aches plus nausea, vomiting, and diarrhea.
 Identifying the bacteria in a sample of blood or cerebrospinal fluid confirms the diagnosis.
Identifying the bacteria in a sample of blood or cerebrospinal fluid confirms the diagnosis.
 Antibiotics can cure the infection.
Antibiotics can cure the infection.
Listeria monocytogenes resides in the intestine of many animals worldwide. Most cases of listeriosis result from eating contaminated food. The bacteria grow in food at refrigerator temperatures and survive in the freezer. Pasteurization of dairy products destroys the bacteria unless many bacteria are present. Adequate cooking or reheating of food kills the bacteria. However, they can reside in food-filled cracks and inaccessible areas in commercial food preparation facilities and recontaminate food. If the food requires no further cooking once purchased, the bacteria that remain are consumed with the food. They can grow in a refrigerated, packaged, ready-to-eat product without changing the food’s taste or smell. Foods involved in previous outbreaks of listerosis include soft cheeses (such as Latin American white cheeses, feta, Brie, and Camembert), delicatessen salads (such as cole slaw), unpasteurized milk, cold cuts, turkey franks, other hot dogs, shrimp, and undercooked chicken.
The bacteria sometimes enter the bloodstream from the intestine and spread, causing invasive listeriosis. Bacteria may spread to the space within the tissues covering the brain and spinal cord (causing meningitis), the eyes, heart valves (causing endocarditis), or, in pregnant women, the uterus. Collections of pus (abscesses) may form in the brain and spinal cord. In the United States, invasive listeriosis develops in only about 2,500 people each year but is fatal in 20 to 30%. It is more common among pregnant women, newborns, people aged 60 or older, and people with a weakened immune system, such as those with human immunodeficiency (HIV) infection. About one third of cases occur in pregnant women.
 Did You Know…
Did You Know…
Pregnant women are particularly susceptible to listeriosis, which can harm the fetus.
Symptoms
People typically have chills, fever, and muscle aches (resembling the flu), with nausea, vomiting, and diarrhea. Usually, symptoms resolve in 5 to 10 days.
If invasive listeriosis develops, symptoms vary depending on the area infected. If meningitis develops, people have a headache and a stiff neck. They may become confused and lose their balance. If the uterus or placenta is infected in a pregnant woman, spontaneous abortion or stillbirth may result. Or the newborn may have a bloodstream infection (sepsis) or meningitis. About one half of newborns infected near or at the end of the pregnancy die.
Diagnosis
A sample of blood is withdrawn. If people have symptoms of meningitis, a spinal tap (lumbar puncture) is done to obtain a sample of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid). The samples are sent to a laboratory to grow (culture) the bacteria. Identifying the bacteria in the sample confirms the diagnosis.
Treatment
The antibiotic ampicillin or, for people who are allergic to penicillin, trimethoprim-sulfamethoxazole usually cures listeriosis. These antibiotics are given intravenously. If the heart valves are infected, a second antibiotic (such as gentamicin) may be given at the same time.
Eye infections can be treated with erythromycin, given by mouth, or trimethoprim-sulfamethoxazole, given intravenously.
Lyme Disease
Lyme disease is caused by the bacteria Borrelia burgdorferi, which is usually transmitted to people by deer ticks.
 Most people are infected when they go outdoors in wooded areas where the disease is common.
Most people are infected when they go outdoors in wooded areas where the disease is common.
 Typically, a large, red spot appears at the site of the bite and slowly enlarges, often surrounded by several red rings.
Typically, a large, red spot appears at the site of the bite and slowly enlarges, often surrounded by several red rings.
 Untreated, the disease can cause fever, muscle aches, swollen joints, and eventually problems related to brain and nerve malfunction.
Untreated, the disease can cause fever, muscle aches, swollen joints, and eventually problems related to brain and nerve malfunction.
 The diagnosis is based on typical symptoms, opportunity for exposure, and blood tests to detect antibodies to the bacteria.
The diagnosis is based on typical symptoms, opportunity for exposure, and blood tests to detect antibodies to the bacteria.
 Taking antibiotics usually cures the disease, but some symptoms, such as joint pain, may persist.
Taking antibiotics usually cures the disease, but some symptoms, such as joint pain, may persist.
Lyme disease was recognized and named in 1975 when a cluster of cases occurred in Lyme, Connecticut. It is now the most common insect-borne infection in the United States. It occurs in 49 states. About 80% of the cases occur along the northeastern coast from Massachusetts to Maryland. Most of the remaining reported cases occur in Wisconsin, Minnesota, and the coastal regions of northern California and Oregon. Lyme disease also occurs in Europe, China, Japan, Australia, and the former Soviet Union.
Usually, people get Lyme disease in the summer and early fall. Children and young adults who live in wooded areas are most often infected.
The bacteria that cause Lyme disease are transmitted by the deer tick (Ixodes), so named because the adult ticks often feed on the blood of deer. Young deer ticks (larvae and nymphs) feed on the blood of rodents, particularly the white-footed mouse, which is a carrier of Lyme disease bacteria. Ticks are usually in the nymph stage when they infect people. Deer do not carry or transmit Lyme disease bacteria. They are only a source of blood for adult ticks.
Preventing Tick Bites
People can reduce their chances of picking up or being bitten by a tick by doing the following:
 Staying on paths and trails when walking in wooded areas
Staying on paths and trails when walking in wooded areas
 Walking in the center of trails to avoid brushing up against bushes and weeds
Walking in the center of trails to avoid brushing up against bushes and weeds
 Not sitting on the ground or on stone walls
Not sitting on the ground or on stone walls
 Wearing long-sleeved shirts
Wearing long-sleeved shirts
 Wearing long pants and tucking them into boots or socks
Wearing long pants and tucking them into boots or socks
 Wearing light-colored clothing, which makes ticks easier to see
Wearing light-colored clothing, which makes ticks easier to see
 Applying an insect repellent containing diethyltoluamide (DEET) to the skin
Applying an insect repellent containing diethyltoluamide (DEET) to the skin
 Applying an insect repellent containing permethrin to clothing
Applying an insect repellent containing permethrin to clothing
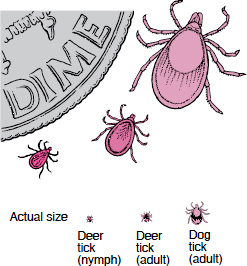
Usually, Lyme disease is transmitted by young deer ticks (nymphs), which are very small, much smaller than dog ticks. So people who may have been exposed to ticks should check the whole body very carefully, especially hairy areas, every day. Inspection is effective because ticks must be attached for more than a day to transmit Lyme disease.
To remove a tick, people should use fine-pointed tweezers to grasp the tick by the head or mouthparts right where they enter the skin and should gradually pull the tick straight off. The tick’s body should not be grasped or squeezed. Petroleum jelly, alcohol, lit matches, or any other irritants should not be used.
The bacteria that cause Lyme disease are transmitted to people when an infected tick bites and stays attached for one or two days. Brief periods of attachment rarely transmit disease. At first, the bacteria multiply at the site of the tick bite. After 3 to 32 days, the bacteria migrate from the site of the bite into the surrounding skin, causing a rash (erythema migrans). The bacteria enter the bloodstream and spread to other organs, such as the skin in other areas of the body and the heart, nervous system, and joints.
 Did You Know…
Did You Know…
Usually, people get Lyme disease only if a tick remains attached to them for at least a day.
Symptoms
Lyme disease has three stages: early localized, early disseminated (widespread), and late. The early and late stages are usually separated by a period without symptoms.
Early-Localized Stage: Typically, a large, raised, red spot (erythema migrans) appears at the site of the bite, usually on the thigh, buttock, or trunk or in the armpit. Usually, the spot slowly expands to a diameter of 6 inches (15 centimeters), often clearing in the center, resulting in several concentric red rings. Although erythema migrans does not itch or hurt, it may be warm to the touch. The spot usually disappears after about 3 to 4 weeks. About 25% of infected people never develop—or at least never notice—the characteristic red spot.
Early-Disseminated Stage: This stage begins when the bacteria spread through the body. Fatigue, chills, fever, headaches, stiff neck, muscle aches, and painful, swollen joints are common. In nearly half of people, more, usually smaller erythema migrans spots appear on other parts of the body. Less commonly, people have a backache, nausea, vomiting, sore throat, swollen lymph nodes, and an enlarged spleen. Although most symptoms come and go, feelings of illness and fatigue may persist for weeks. These symptoms are often mistaken for influenza or common viral infections, especially if erythema migrans is not present.
Sometimes more serious symptoms develop. The nervous system is affected in about 15% of people. The most common problems are headache, stiff neck, meningitis, and Bell’s palsy, which causes weakness on one or occasionally both sides of the face. These problems may last for months. Nerve pain and weakness may develop in other areas and persist longer. About 8% of infected people have irregular heartbeats (arrhythmias) and inflammation of heart tissue (myocarditis) and the sac around the heart (pericarditis) with chest pain. Irregular heartbeats may cause palpitations, light-headedness, or fainting.
Late Stage: If the initial infection is untreated, other problems develop months to years later. Arthritis develops in more than half of people, usually within several months. Swelling and pain typically recur in a few large joints, especially the knee, for several years. The knees are commonly more swollen than painful, often hot to the touch, and, rarely, red. Cysts may develop and rupture behind the knees, suddenly increasing the pain. In about 10% of people with arthritis, knee problems last longer than 6 months.
A few people develop abnormalities related to brain and nerve malfunction. Mood, speech, memory, and sleep may be affected. Some people have numbness or shooting pains in the back, legs, and arms.
Diagnosis
The diagnosis is usually based on typical symptoms (particularly erythema migrans), opportunity for exposure (living in or visiting an area where Lyme disease is common), and test results.
Usually, doctors use tests that measure antibodies to the bacteria in blood. However, antibodies may be absent if the test is done during the first several weeks of infection or if antibiotics are given before antibodies develop. Antibodies develop in more than 95% of people who have had the infection for at least a month, particularly if they have not taken antibiotics. Once antibodies develop, they persist permanently. Thus, antibodies may be present after Lyme disease has resolved.
Interpreting the results of blood tests is difficult. The uncertainty causes several problems. For example, in areas where Lyme disease is common, many people who have painful joints, trouble concentrating, or persistent fatigue worry that they have late-stage Lyme disease, even though they never had a rash or any other symptoms of early-stage Lyme disease. Usually, Lyme disease is not the cause. But they may have antibodies for the bacteria because they were infected years before and the antibodies persist indefinitely. Thus, if a doctor treats people based solely on results of antibody tests, many people who do not have Lyme disease are treated with long, useless courses of antibiotics.
Cultures are not helpful because Borrelia burg-dorferi is difficult to grow in the laboratory.
Sometimes doctors insert a needle into a joint to take a sample of joint fluid or do a spinal tap (lumbar puncture) to take a sample of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid). Fragments of the bacteria’s genetic material may be present.
Treatment
If people are bitten by a tick but have no rash or other symptoms, antibiotics are usually used only if they can be given within 72 hours after an engorged tick is found attached. These people may be given one dose of doxycycline by mouth to prevent Lyme disease from developing.
Although all stages of Lyme disease respond to antibiotics, early treatment is more likely to prevent complications. Antibiotics such as doxycycline, amoxicillin, cefuroxime, or azithromycin, taken by mouth for 2 weeks, are effective during the early stages of the disease. They can also help treat a type of arrhythmia called first-degree heart block and probably Bell’s palsy. Doxycycline is not given to children under 9 years old or to pregnant women.
For arthritis, antibiotics such as amoxicillin or doxycycline are given by mouth for 30 to 60 days, or ceftriaxone or penicillin is given intravenously for 2 to 4 weeks.
For most neurologic abnormalities (except possibly Bell’s palsy) and more severe (third-degree) heart block, ceftriaxone or penicillin is given intravenously for 2 to 4 weeks.
Antibiotics eradicate the bacteria and, in most people, relieve arthritis. However, arthritis sometimes persists even after all the bacteria are gone because inflammation continues. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen, may relieve the pain of swollen joints. Fluid that collects in affected joints may be drained. Using crutches may help.
Antibiotics do not appear to relieve the chronic fatigue.
A vaccine that was only moderately effective against Lyme disease was removed from the market because it was not widely used.
Meningococcal Infections
Meningococcal infections are caused by Neisseria meningitidis (meningococci) and include meningitis and bloodstream infections.
 Infection is spread by direct contact with nasal and throat secretions.
Infection is spread by direct contact with nasal and throat secretions.
 People feel generally ill and have other, often serious symptoms, depending on the area infected.
People feel generally ill and have other, often serious symptoms, depending on the area infected.
 Identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
Identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
 Antibiotics and fluids must be given intravenously as soon as possible.
Antibiotics and fluids must be given intravenously as soon as possible.
More than 90% of meningococcal infections are infections of the space within the tissues covering the brain and spinal cord (meningitis—see page 750) or of the bloodstream (sepsis—see page 1186). Infections of the lungs, joints, and heart are less common.
In temperate climates, most meningococcal infections occur during winter and spring. Local outbreaks can occur, most often in sub-Saharan Africa between Senegal and Ethiopia. This area is known as the meningitis belt.
Meningococci reside in the throat and nose of some people without causing symptoms. Such people are called carriers. People often become carriers after outbreaks. Infection usually occurs in people who have been exposed to meningococci rather than in carriers. Infection is spread by direct contact with nasal and throat secretions.
Children aged 6 months to 3 years are most commonly infected. Infections are also common among adolescents, military recruits, college freshmen living in dormitories, people with certain immune system disorders, and microbiologists working with meningococci.
Symptoms
Most people feel very ill.
Meningitis can cause fever, headache, red rash, and a stiff neck and, in infants, feeding problems, a weak cry, and sluggishness.
Bloodstream infections may cause a rash of red or purple spots. A severe infection may cause low blood pressure, a tendency to bleed, and dysfunction (failure) of many organs (such as the kidneys and liver).
Overall, 10 to 15% of people who are treated die of meningococcal infections. More than half of people with severe bloodstream infections die. Of people who recover, 10 to 20% have serious complications, such as permanent hearing loss, mental retardation, or loss of fingers or toes.
Rarely, infection develops more slowly and causes more gradual, mild symptoms.
Diagnosis
Doctors suspect meningococcal infection in people who have typical symptoms, particularly if symptoms occur during an outbreak. To confirm the diagnosis, they take samples of blood or other infected tissues or do a spinal tap (lumbar puncture) to obtain a sample of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid). The samples are examined under a microscope to check for and identify bacteria. The samples are also sent to a laboratory, where the bacteria can be grown (cultured) and identified. The polymerase chain reaction (PCR) technique, which produces many copies of a gene, may be used to identify the bacteria’s unique genetic material (DNA).
The bacteria may also be tested to determine which antibiotics are effective (a process called susceptibility testing).
Prevention
A meningococcal vaccine is available in the United States. Vaccination is recommended for the following:
 People living in an area affected by an epidemic (to control the epidemic)
People living in an area affected by an epidemic (to control the epidemic)
 Military recruits
Military recruits
 All children aged 11 to 19 years
All children aged 11 to 19 years
 College students who live in dormitories or who are freshmen
College students who live in dormitories or who are freshmen
 Travelers to areas where these infections are common, such as sub-Saharan Africa during the dry season from December to June and Saudi Arabia to attend the Hajj
Travelers to areas where these infections are common, such as sub-Saharan Africa during the dry season from December to June and Saudi Arabia to attend the Hajj
 People who work with meningococci in laboratories or industry
People who work with meningococci in laboratories or industry
 People who are aged 2 years and older and have an immune system disorder, particularly those whose spleen has been removed or damaged (as can occur in people with sickle cell disease)
People who are aged 2 years and older and have an immune system disorder, particularly those whose spleen has been removed or damaged (as can occur in people with sickle cell disease)
Family members, medical personnel, and other people in close contact with people who have a meningococcal infection should be given an antibiotic by mouth (such as a few doses of rifampin or one dose of ciprofloxacin or levofloxacin) or by injection (such as one dose of ceftriaxone) to prevent infection from developing. Meningococcal vaccine is also given (in addition to antibiotics) to people in close contact with a person who has a meningococcal infection.
Treatment
People are usually admitted to an intensive care unit and given antibiotics and fluids intravenously as soon as possible. Corticosteroids may be given to children or adults who have meningitis.
Plague
Plague is a severe infection caused by the gram-negative bacteria Yersinia pestis.
 The bacteria are spread by the rat flea.
The bacteria are spread by the rat flea.
 Depending on the form, plague can cause fever, chills, swollen lymph nodes, headache, a rapid heartbeat, cough, difficulty breathing, vomiting, and diarrhea.
Depending on the form, plague can cause fever, chills, swollen lymph nodes, headache, a rapid heartbeat, cough, difficulty breathing, vomiting, and diarrhea.
 Identifying the bacteria in samples of blood, sputum, or pus from lymph nodes confirms the diagnosis.
Identifying the bacteria in samples of blood, sputum, or pus from lymph nodes confirms the diagnosis.
 Antibiotics can reduce the risk of death, and isolating infected people helps prevent spread of plague.
Antibiotics can reduce the risk of death, and isolating infected people helps prevent spread of plague.
In the past, massive plague epidemics, such as the black death of the Middle Ages, killed many people. The main contributing factors were large numbers of rodents, urban crowding, and poor sanitation. Plague now occurs mostly in rural areas. In the United States, more than 90% of infections occur in southwestern states such as Arizona, California, Colorado, and New Mexico, particularly among campers. Each year, plague affects about 10 to 15 people in the United States and 1,000 to 3,000 people worldwide.
The bacteria that cause plague usually infect wild rodents, such as rats and prairie dogs. The bacteria are spread by the rat flea. When wild rats die, the fleas may move to rats that live close to people, then to household pets, especially cats. The rat fleas may then bite people and transmit infection. Rarely, the infection is spread from person to person by coughing or sneezing. The bacteria lodge in the lungs and cause a type of pneumonia (pneumonic plague). Spread between people usually happens only when people live with or care for a person with pneumonic plague.
Plague can also be acquired by handling infected animals (for example, by hunters) or eating under-cooked meat from infected animals.
Plague bacteria is a potential biological weapon. The bacteria can be spread through the air and inhaled. The size of the airborne particle determines where the bacteria lodge in the respiratory tract. Small particles lodge in the lungs, causing pneumonic plague.
Symptoms
Plague has several forms: bubonic, pestis minor, pneumonic, or septicemic. Symptoms vary depending on the form of plague.
Bubonic plague is the most common form. Symptoms may appear a few hours to 12 days after exposure (typically, after 2 to 5 days). Chills and fever of up to 106° F (41° C) occur suddenly. The heartbeat becomes rapid and weak, and blood pressure may drop. Many people become delirious. Shortly before the fever or at the same time, lymph nodes in the groin, armpits, or neck usually swell. They are firm, red, warm, and very tender. During the second week, pus may drain from the lymph nodes. The liver and spleen may enlarge. More than 60% of untreated people die, usually between the third and fifth day.
Pestis minor is a mild form of bubonic plague. Its symptoms—swollen lymph nodes, fever, headache, and exhaustion—disappear within a week.
Pneumonic plague is infection of the lungs. Symptoms begin abruptly 2 or 3 days after exposure to the bacteria. People have a high fever, chills, a rapid heartbeat, and often a severe headache. Within 24 hours, they develop a cough that brings up clear sputum, which soon becomes flecked with blood. Then the sputum becomes pink or bright red (resembling raspberry syrup) and foamy. Breathing is rapid and labored. Most untreated people die within 48 hours after symptoms start.
Septicemic plague is infection that spreads into the blood. About 40% of people have nausea, vomiting, diarrhea, and abdominal pain. Without treatment, many organs malfunction, often causing death.
Diagnosis
To diagnose plague, doctors take samples of blood, sputum, or pus from lymph nodes. Samples are examined under a microscope and sent to a laboratory to grow (culture) bacteria. The blood sample is also tested for antibodies to the bacteria. Tests that rapidly detect the bacteria or its genetic material (DNA), such as polymerase chain reaction (PCR), may be done.
Prevention
Controlling rodents and using repellents to prevent fleabites can help. The vaccine against plague is no longer available in the United States. People who are traveling to locations with a plague outbreak may take an antibiotic such as doxycycline, trimethoprim-sulfamethoxazole, or ciprofloxacin.
Treatment
Treatment begins immediately and reduces the risk of death to less than 15%. Streptomycin is given by injection for 7 to 10 days. Other antibiotics such as gentamicin, doxycycline, and ciprofloxacin are also effective.
People with pneumonic plague must be isolated so that they do not spread the bacteria through the air—called respiratory isolation. It includes the following:
 Limiting access to the room
Limiting access to the room
 Requiring people who work within about 6 1/2 feet (2 meters) of the infected person to wear a mask, eye protection, a gown, and gloves
Requiring people who work within about 6 1/2 feet (2 meters) of the infected person to wear a mask, eye protection, a gown, and gloves
Anyone who has had unprotected contact with a person or animal (such as a domestic cat) with pneumonic plague must take doxycycline or ciprofloxacin for 7 days.
Pneumococcal Infections
Pneumococcal infections are caused by the gram-positive bacteria Streptococcus pneumoniae (pneumococcus).
 Bacteria are dispersed in the air when infected people cough or sneeze.
Bacteria are dispersed in the air when infected people cough or sneeze.
 The most common infections are pneumonia, meningitis, sinusitis, and middle ear infection (otitis media).
The most common infections are pneumonia, meningitis, sinusitis, and middle ear infection (otitis media).
 These infections usually cause fever and a general feeling of illness, with other symptoms depending on which part of the body is infected.
These infections usually cause fever and a general feeling of illness, with other symptoms depending on which part of the body is infected.
 Diagnosis may be based on symptoms, x-ray findings, or identification of the bacteria in samples of infected material.
Diagnosis may be based on symptoms, x-ray findings, or identification of the bacteria in samples of infected material.
 Young children are routinely vaccinated against these infections, and vaccination is recommended for all people at high risk.
Young children are routinely vaccinated against these infections, and vaccination is recommended for all people at high risk.
 Penicillin or another antibiotic is usually effective treatment.
Penicillin or another antibiotic is usually effective treatment.
Pneumococci commonly reside in the upper respiratory tract of healthy people, their natural host, particularly during the winter and early spring. The bacteria spread to other people when they inhale infected droplets dispersed by sneezing or coughing. Spread is more likely among self-contained groups of people, such as people who live, stay, or work in nursing homes, prisons, military bases, shelters for the homeless, or day care centers.
Certain conditions make people more likely to develop these infections, and vaccination is recommended for such people. Older people, even if healthy, tend to have more severe symptoms and complications when they get a pneumococcal infection.
Most pneumococcal infections occur in the lungs (pneumonia), middle ear (otitis media, which is common among children), or sinuses (sinusitis). Pneumonia may develop after influenza, which damages the lining of the respiratory tract.
The bacteria may also spread to and through the bloodstream (causing bacteremia). Infections may occur in the space within the tissues covering the brain and spinal cord (meningitis) or, less often, in heart valves, bones, joints, or the abdominal cavity.
Symptoms and Diagnosis
Symptoms vary depending on the site of the infection.
Pneumococcal Pneumonia: Often, symptoms begin suddenly. People have fever, chills, a general feeling of illness (malaise), shortness of breath, and a cough. The cough brings up sputum that becomes rust-colored.
Commonly, sharp, stabbing chest pains occur on one side. Deep breathing and coughing make the pains worse. This pain is called pleurisy.
Chest x-rays are taken to look for signs of pneumonia. Doctors take a sample of sputum and examine it under a microscope. A sample of sputum, pus, or blood may be sent to a laboratory to grow (culture) bacteria. However, these tests do not always enable doctors to identify the bacteria.
Pneumococcal Meningitis: People have fever, headache, and a general feeling of illness (malaise). Moving the neck becomes painful and difficult, but this problem is not always obvious early in the disease. Infants may only be reluctant to eat and be irritable or sluggish.
The diagnosis requires a spinal tap (lumbar puncture) to obtain a sample of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid). The sample is checked for signs of infection, such as white blood cells and bacteria.
Pneumococcal Otitis Media: These infections cause ear pain and a red, bulging eardrum or pus behind the eardrum.
The diagnosis is usually based on symptoms and results of a physical examination. Cultures and other diagnostic tests are usually not done.
Prevention
Two types of pneumococcal vaccines are available.
Conjugate vaccine is the only one that works in children under 2 years old. It is routinely given to children starting at age 2 months but can be started at age 6 weeks. Three doses are given at 2-month intervals, followed by a fourth dose, usually at age 12 to 15 months (see box on page 1685). Because of this vaccine, serious pneumococcal infections—pneumonia, otitis media, and meningitis—are much less common among children.
Nonconjugate polysaccharide vaccine is recommended for people who are at high risk of pneumococcal infections or complications after a pneumococcal infection. These people include the following:
 All adults aged 65 years or older
All adults aged 65 years or older
 Native Alaskans and American Indians
Native Alaskans and American Indians
 People with a chronic disorder such as certain heart or lung disorders (except asthma), kidney failure, nephrotic syndrome, liver dysfunction (including cirrhosis), sickle cell disease, diabetes, or leakage of spinal fluid
People with a chronic disorder such as certain heart or lung disorders (except asthma), kidney failure, nephrotic syndrome, liver dysfunction (including cirrhosis), sickle cell disease, diabetes, or leakage of spinal fluid
 Alcoholics
Alcoholics
 People with a disorder that weakens the immune system, such as some cancers and human immunodeficiency virus (HIV) infection
People with a disorder that weakens the immune system, such as some cancers and human immunodeficiency virus (HIV) infection
 People who take corticosteroids or drugs to suppress the immune system, such as those used to prevent rejection of an organ transplant or to treat cancer
People who take corticosteroids or drugs to suppress the immune system, such as those used to prevent rejection of an organ transplant or to treat cancer
 People who do not have a functioning spleen
People who do not have a functioning spleen
The nonconjugate vaccine is effective against many more types of pneumococci than the conjugate vaccine. Thus, children at high risk, such as those with sickle cell anemia or AIDS, are given one dose of the nonconjugate vaccine at age 2 years (but at least 2 months after the last dose of conjugate vaccine), even if they have had the conjugate vaccine.
Treatment
Penicillin (or the related drugs, ampicillin and amoxicillin) is used for most pneumococcal infections. It is usually taken by mouth but, if the infection is severe, may be given intravenously.
Pneumococci that are resistant to penicillin are becoming more common. Thus, other antibiotics, such as ceftriaxone, cefotaxime, fluoroquinolones, or vancomycin, are often used.
Pseudomonas Infections
Pseudomonas infections are caused by any of several types of the gram-negative bacteria Pseudomonas, especially Pseudomonas aeruginosa.
 Infections range from mild external ones (affecting the ear or hair follicles) to serious internal infections (affecting the lungs, bloodstream, or heart valves).
Infections range from mild external ones (affecting the ear or hair follicles) to serious internal infections (affecting the lungs, bloodstream, or heart valves).
 Symptoms vary depending on which area of the body is infected.
Symptoms vary depending on which area of the body is infected.
 Identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
Identifying the bacteria in a sample taken from infected tissue confirms the diagnosis.
 Antibiotics are applied externally for external infections or given intravenously for more serious, internal infections.
Antibiotics are applied externally for external infections or given intravenously for more serious, internal infections.
Pseudomonas bacteria, including Pseudomonas aeruginosa, are present throughout the world in soil and water. These bacteria favor moist areas, such as sinks, toilets, inadequately chlorinated swimming pools and hot tubs, and outdated or inactivated antiseptic solutions. These bacteria may temporarily reside in the skin, ears, and intestine of healthy people.
Pseudomonas aeruginosa infections range from minor external infections to serious, life-threatening disorders. Infections occur more often and tend to be more severe in people who
 Are weakened (debilitated) by certain severe disorders
Are weakened (debilitated) by certain severe disorders
 Have diabetes or cystic fibrosis
Have diabetes or cystic fibrosis
 Are hospitalized
Are hospitalized
 Have a disorder that weakens the immune system, such as human immunodeficiency virus (HIV) infection
Have a disorder that weakens the immune system, such as human immunodeficiency virus (HIV) infection
 Take drugs that suppress the immune system, such as those used to treat cancer or to prevent rejection of transplanted organs
Take drugs that suppress the immune system, such as those used to treat cancer or to prevent rejection of transplanted organs
These bacteria can infect the blood, skin, bones, ears, eyes, urinary tract, heart valves, and lungs, as well as wounds (such as burns, injuries, or wounds made during surgery). Use of medical devices, such as catheters inserted into the bladder or a vein, breathing tubes, and mechanical ventilators, increase the risk of Pseudomonas aeruginosa infections. These infections are commonly acquired in hospitals.
Symptoms
Pseudomonas aeruginosa causes several different infections.
Swimmer’s ear (external otitis) is a mild external infection that can occur in otherwise healthy people. Water containing the bacteria can enter the ear during swimming. Swimmer’s ear causes pain and a discharge from the ear (see page 1385).
Hot-tub folliculitis is another mild external infection. Hair roots (follicles) become infected in people who use hot tubs or whirlpools, particularly if the hot tubs and whirlpools are inadequately chlorinated. Spending a lot of time in the water softens the follicles, making them easier for bacteria to invade. An itchy skin rash consisting of tiny pimples develops. Pimples may have a drop of pus in their center.
Malignant external otitis is a deep ear infection. It is most common among people with diabetes. Tissues become swollen and inflamed, partly or completely closing the ear canal. Symptoms may include fever, loss of hearing, inflammation of tissues around the infected ear, severe ear pain, a foul-smelling discharge from the ear, and nerve damage.
Eye infections due to these bacteria may damage the cornea, often permanently. Enzymes produced by the bacteria can rapidly destroy the eye. Infections may result from contamination of contact lenses or contact lens solution.
Soft-tissue infections include those in muscle, tendons, ligaments, fat, and skin. These infections can occur in deep puncture wounds, especially in the feet of children who are wearing sneakers and step on a nail. These bacteria can also infect pressure sores, burns, and wounds due to injuries or surgery. When these bacteria grow in soiled dressings, the dressings turn green and smell like newly mowed grass.
Severe pneumonia can develop in hospitalized people, especially those who need to use a breathing tube and a mechanical ventilator.
Urinary tract infections usually develop after a procedure involving the urinary tract is done, when the urinary tract is blocked, or when a catheter must remain in the bladder a long time.
Bloodstream infections (bacteremia) often result when the following occur:
 Bacteria enter the bloodstream from an infected organ (such as the urinary tract).
Bacteria enter the bloodstream from an infected organ (such as the urinary tract).
 A contaminated illegal drug is injected into a vein.
A contaminated illegal drug is injected into a vein.
 A contaminated needle or syringe is used to inject illegal drugs.
A contaminated needle or syringe is used to inject illegal drugs.
Sometimes the source of the bacteria is unknown, as may occur in people who have too few white blood cells after cancer chemotherapy. Purple-black spots surrounded by a red rim on the skin often develop in the armpits and groin. Without treatment, infection can lead to shock and death.
Bone and joint infections usually occur in the spine and the joint between the collar bone and breastbone. The bacteria usually spread to bones and joints from the bloodstream but may spread from nearby soft tissues that have been infected after an injury or surgery.
Heart valve infections are rare. They usually occur in people who inject intravenous drugs and in people with artificial heart valves. The bacteria usually spread to heart valves from the bloodstream.
Diagnosis
Doctors diagnose Pseudomonas aeruginosa infections by taking a sample of blood or other body fluids and growing the bacteria in cultures. Tests to determine which antibiotics are likely to be effective (susceptibility tests) are also done.
Prevention and Treatment
To prevent swimmer’s ear, people who have had it should irrigate their ears with an acetic acid solution before and after swimming. Acetic acid drops with or without corticosteroids are usually effective for treatment.
Hot-tub folliculitis usually resolves without treatment.
Eye infections are treated with highly concentrated antibiotic drops, applied frequently at first. Sometimes antibiotics must be injected directly into the eye.
Serious Pseudomonas aeruginosa infections are difficult to treat. Malignant external otitis, internal infections (such as pneumonia or heart valve infection), and blood infections require weeks of antibiotics given intravenously. Usually, a combination of antibiotics is required because many strains, particularly those acquired in health care facilities, are resistant to many antibiotics. Doctors choose an antibiotic that is usually effective in their geographic area. They may change the antibiotics after test results indicate which antibiotics are likely to be effective.
For heart valve infections, open-heart surgery to replace the valve plus antibiotic therapy is usually needed (see box on page 381).
Salmonella Infections
Salmonella infections are caused by the gram-negative bacteria Salmonella.
 People are usually infected when they eat contaminated food, such as undercooked chicken or eggs.
People are usually infected when they eat contaminated food, such as undercooked chicken or eggs.
 The bacteria usually infect the digestive tract but can travel through the bloodstream and infect other parts of the body.
The bacteria usually infect the digestive tract but can travel through the bloodstream and infect other parts of the body.
 People have nausea and crampy abdominal pain, followed by watery diarrhea, fever, and vomiting.
People have nausea and crampy abdominal pain, followed by watery diarrhea, fever, and vomiting.
 Identifying the bacteria in a sample, usually of stool, confirms the diagnosis.
Identifying the bacteria in a sample, usually of stool, confirms the diagnosis.
 Lost fluids are replaced, and antibiotics are usually not helpful for salmonellal intestinal infections.
Lost fluids are replaced, and antibiotics are usually not helpful for salmonellal intestinal infections.
Two species of Salmonella cause typhoid fever: Salmonella typhi and Salmonella paratyphi. Salmonella typhi resides only in people. Salmonella paratyphi resides mainly in people but sometimes in domestic animals. Other species of Salmonella normally reside in the digestive tract of many wild and domestic animals, such as cattle, sheep, pigs, fowl, and reptiles (including snakes, lizards, and turtles). Many of these can cause infections in people. One species, Salmonella enteritidis, causes most Salmonella infections in the United States.
Salmonella bacteria are excreted in the feces of infected animals and people, leading to contamination. In the United States during the 1970s, many infections were spread by pet turtles, so their sale was prohibited, resulting in fewer infections. Recently, the legal and illegal sale of pet reptiles has increased. Up to 90% of pet reptiles are infected with Salmonella.
People are infected usually by eating undercooked poultry or eggs but sometimes by eating under-cooked beef and pork, unpasteurized dairy products, or contaminated seafood or fresh produce. Salmonella bacteria can infect the ovaries of hens and thus infect the egg before the egg is laid. Other foods may be contaminated by animal feces (for example, in slaughterhouses) or by infected food handlers who do not adequately wash their hands after using a toilet.
Because stomach acid tends to destroy Salmonella, a large number of these bacteria must be consumed for infection to develop, unless people have a deficiency of stomach acid. Such a deficiency may occur in children under 1 year old, in older people, and in people taking antacids or drugs that inhibit stomach acid production, including hista-mine-2 (H2) blockers (such as ranitidine) or proton pump inhibitors (such as omeprazole).
The bacteria cause inflammation of the intestine (gastroenteritis) and thus are a common cause of diarrhea. Sometimes the bacteria enter the bloodstream (causing bacteremia) and spread, causing infections or collections of pus (abscesses) at distant sites, such as the bones, joints, urinary tract, and lungs. Bacteria may collect and cause infection on artificial (prosthetic) joints or heart valves, on a blood vessel graft, or on tumors. The lining of arteries, usually the aorta (the largest artery in the body), may be infected. Abscesses and infected arteries can cause chronic bacteremia. The infection is more likely to spread through the bloodstream in the following:
 Infants
Infants
 Older people
Older people
 People with disorders that affect red blood cells such as sickle cell anemia or malaria
People with disorders that affect red blood cells such as sickle cell anemia or malaria
 People with a disorder that weakens the immune system, such as human immunodeficiency virus (HIV) infection
People with a disorder that weakens the immune system, such as human immunodeficiency virus (HIV) infection
 People who take drugs that suppress the immune system, such as those used to treat cancer or prevent rejection of an organ transplant
People who take drugs that suppress the immune system, such as those used to treat cancer or prevent rejection of an organ transplant
Symptoms
When the intestine is infected, symptoms usually start 12 to 48 hours after the bacteria are ingested. Nausea and crampy abdominal pain occur, soon followed by watery diarrhea, fever, and vomiting. Symptoms resolve within a week. Long after symptoms are gone, a few people continue to excrete the bacteria in their stool. Such people are called carriers.
Up to about 30% of adults develop reactive arthritis weeks to months after diarrhea stops. This disorder causes pain and swelling, usually in the hips, knees, and Achilles tendon (which connects the heel bone and calf muscle).
Other symptoms may develop if bacteremia develops and infection spreads. For example, if a bone is infected, the area over it is often tender or painful. If a heart valve is infected, people may feel short of breath. If the aorta is infected, the back and abdomen may be painful.
 Did You Know…
Did You Know…
In the United States, up to 90% of pet reptiles are infected with Salmonella.
Diagnosis
Doctors take a sample of stool, pus, or blood or use a swab to obtain a sample from the rectum. The sample is sent to a laboratory where bacteria can be grown (cultured). Identifying the bacteria in the sample confirms the diagnosis.
Treatment
The intestinal infection is treated with fluids given by mouth or, for severe infection, intravenously.
Antibiotics do not shorten recovery time and may result in bacteria being excreted in the stool longer. Therefore, antibiotics are usually not given. However, people at risk of bacteremia and people with implanted devices or materials (such as an artificial joint or heart valve or a blood vessel graft) are given antibiotics. They may be given ciprofloxacin or azithromycin for 1 week. Antibiotics are given to people who continue to excrete the bacteria in the stool after symptoms are gone.
People with bacteremia are given ciprofloxacin or ceftriaxone intravenously for 2 weeks.
Abscesses are drained surgically, and antibiotics are given for 4 weeks.
If the aorta, a heart valve, or other areas (such as joints) are infected, surgery is usually required, and antibiotics are given for weeks or months.
TYPHOID FEVER
Typhoid fever (enteric fever) is caused by the bacteria Salmonella typhi or the related bacteria, Salmonella paratyphi.
 Typhoid fever can be spread by consuming food or water contaminated with the stool or urine of an infected person.
Typhoid fever can be spread by consuming food or water contaminated with the stool or urine of an infected person.
 People have flu-like symptoms, sometimes followed by delirium, cough, exhaustion, occasionally rash, and diarrhea.
People have flu-like symptoms, sometimes followed by delirium, cough, exhaustion, occasionally rash, and diarrhea.
 Samples of blood, stool, other body fluids, or tissues are sent to a laboratory to grow (culture) the bacteria.
Samples of blood, stool, other body fluids, or tissues are sent to a laboratory to grow (culture) the bacteria.
 To prevent infection, people traveling to areas where typhoid fever is common should be vaccinated and, when there, should avoid certain foods and not drink unbottled water.
To prevent infection, people traveling to areas where typhoid fever is common should be vaccinated and, when there, should avoid certain foods and not drink unbottled water.
 Infected people with or without symptoms are treated with antibiotics.
Infected people with or without symptoms are treated with antibiotics.
Typhoid fever is common in developing countries (mostly in the Indian subcontinent, the Philippines, and Latin America) where sanitary conditions are poor. Most cases in the United States are acquired while traveling in these countries.
Salmonella typhi is present only in people. People who are infected excrete the bacteria in stool and, rarely, in urine. A few infected people develop chronic infection of the gallbladder or urinary tract. They continue to excrete the bacteria in stool or urine, even though they no longer have any symptoms. Such people are called carriers. Thus, they do not know they can spread the infection. During the early 20th century, one such woman, a cook named Mary Mallon, spread typhoid fever to many people and became known as Typhoid Mary.
The bacteria may contaminate food or drink when hands are inadequately washed after defecation or urination. Water supplies may be contaminated when sewage is inadequately treated. Flies may spread the bacteria directly from stool to food.
Like all Salmonella bacteria, many of these bacteria must be consumed for infection to develop, unless the immune system is impaired or people have a deficiency of stomach acid.
The bacteria spread from the digestive tract to the bloodstream (causing bacteremia) and may infect distant organs such as the liver, spleen, gallbladder, lungs (causing pneumonia), joints (causing infectious arthritis), kidneys (causing pyelonephritis), heart valves (causing endocarditis), genital tract, the space within the tissues covering the brain and spinal cord (causing meningitis), and bone (causing osteomyelitis).
 Did You Know…
Did You Know…
Mary Mallon, so-called Typhoid Mary, was a cook who spread typhoid fever to many people during the early 20th century.
Symptoms
Typically, a flu-like illness begins about 8 to 14 days (up to 30 days) after infection. People may have a fever, headache, muscle and joint pains, abdominal pains, and a dry cough. They may lose their appetite. After a few days, the temperature peaks at about 103° to 104° F (39° to 40° C). Often the heartbeat is slow, and people feel exhausted and sometimes become delirious. During the second week, a rash of flat, rose-colored spots develops in about 10% of people. People may be constipated at first, but after 2 weeks, diarrhea may occur. In less than 5% of people, the intestine is torn (perforated) or bleeds. If infection spreads to other organs, symptoms of those infections may also develop.
Without treatment, people may have fever for 3 to 4 weeks. Up to 20% may relapse after initial recovery, and up to 20% may die. Most people who die are malnourished, very young, or very old. Stupor (unresponsiveness that requires vigorous stimulation to be aroused), coma, and shock are signs of severe infection and a poor prognosis.
Diagnosis
To confirm the diagnosis, doctors take samples of blood, stool, other body fluids, or tissues and send them to a laboratory where the bacteria can be grown (cultured). The samples are examined and tested to determine whether the bacteria are present.
Prevention
People who travel to areas where typhoid fever is common should avoid eating raw vegetables and other foods served or stored at room temperature. Generally, people can safely consume foods that are served very hot immediately after cooking, bottled or canned beverages that are sealed, hot tea or coffee, and fruit that they have peeled themselves. People should assume that ice and water (unless it is boiled or chlorinated before use) are unsafe. Sealed bottled water should be used for brushing teeth.
A vaccine given by mouth and a polysaccharide vaccine given by injection can help prevent typhoid fever. Both vaccines have few side effects. Vaccination is recommended for
 Travelers to regions where typhoid fever is common
Travelers to regions where typhoid fever is common
 People who live in a household with carriers
People who live in a household with carriers
 Laboratory workers who work with the bacteria
Laboratory workers who work with the bacteria
People are usually protected for at least 2 years after vaccination by injection and for 5 years after taking the vaccine by mouth. However, they can be infected if many bacteria are ingested. In the United States, 75% of cases of typhoid fever occur in travelers who were not vaccinated or who did not keep their vaccinations up to date.
Treatment
When antibiotics are used, fever lasts only 3 to 5 days, rather than 3 to 4 weeks, and the risk of death is reduced to less than 1%. Complete recovery may take weeks or months.
The antibiotic chloramphenicol is used worldwide. However, it can damage cells in bone marrow that make blood cells. Also, Salmonella typhi bacteria are becoming increasingly resistant to it. Thus, other antibiotics (such as ceftriaxone, ciprofloxacin, or azithromycin) are often used. People who are delirious, comatose, or in shock may also be given corticosteroids.
In 10 to 20% of people given antibiotics, the infection recurs, typically about 1 week after treatment is stopped. This infection is milder than the initial illness and is treated the same way.
Carriers must report to the local health department and are prohibited from working with food. Taking antibiotics for 4 to 6 weeks may eradicate the bacteria in many carriers. However, if carriers have abnormalities of the biliary or urinary tract (for example, kidney or gallbladder stones), surgery to correct these abnormalities is needed before bacteria can be eradicated.
Shigellosis
Shigellosis is infection that is caused by the gram-negative bacteria Shigella and that results in watery diarrhea or dysentery (the frequent and often painful passage of small amounts of stool that contains blood, pus, and mucus).
 The bacteria are excreted in stool and can be easily spread when hygiene or sanitation is inadequate.
The bacteria are excreted in stool and can be easily spread when hygiene or sanitation is inadequate.
 People may have watery diarrhea, sometimes leading to severe dehydration.
People may have watery diarrhea, sometimes leading to severe dehydration.
 Identifying the bacteria in a sample of stool can confirm the diagnosis.
Identifying the bacteria in a sample of stool can confirm the diagnosis.
 For people with shigellosis and people who care for them, meticulous hygiene is necessary to avoid spreading the infection.
For people with shigellosis and people who care for them, meticulous hygiene is necessary to avoid spreading the infection.
 Fluids are given by mouth or, if the infection is severe, intravenously.
Fluids are given by mouth or, if the infection is severe, intravenously.
 Antibiotics are used.
Antibiotics are used.
Shigella bacteria are a common cause of dysentery throughout the world. Probably about a quarter of a million people in the United States develop shigellosis each year.
Because stomach acid does not easily destroy these bacteria, ingesting even a small number of them causes infection. In the large intestine, the bacteria cause inflammation and are then excreted in stool. As a result, infection spreads easily from person to person when hands are soiled. Infection is also spread through the following:
 Oral-anal sex
Oral-anal sex
 Food contaminated by infected food handlers who do not wash their hands with soap after using a toilet
Food contaminated by infected food handlers who do not wash their hands with soap after using a toilet
 Water contaminated with human waste
Water contaminated with human waste
 Swimming and wading pools that are inadequately chlorinated
Swimming and wading pools that are inadequately chlorinated
Infection easily spreads among people who live together. Outbreaks also occur in places that are overcrowded and have inadequate sanitation, such as
 Day-care centers for children
Day-care centers for children
 Long-term care facilities
Long-term care facilities
 Refugee camps
Refugee camps
 Institutions for the intellectually disabled (mentally retarded)
Institutions for the intellectually disabled (mentally retarded)
 Cruise ships
Cruise ships
 Military camps
Military camps
 Developing countries
Developing countries
Children are more likely to become infected and to have severe symptoms, such as seizures.
There are four species of Shigella. All cause diarrhea. However, one—Shigella dysenteriae—is more likely to cause severe diarrhea, dysentery, and complications.
Symptoms
Mild infections cause low-grade fever (about 100.4 to 102° F [38 to 38.9° C]) and watery diarrhea 1 to 2 days after people ingest the bacteria. Abdominal cramps and a frequent urge to defecate are common with more severe infections. Severe infections may cause low-grade or moderate fever and watery diarrhea that progresses to dysentery. In dysentery, bowel movements are frequent and contain blood, pus, and mucus.
Children, particularly young children, are most likely to have severe complications:
 High fever (up to 106° F [41° C]), sometimes with delirium
High fever (up to 106° F [41° C]), sometimes with delirium
 Severe dehydration with weight loss
Severe dehydration with weight loss
 Up to 20 bowel movements a day
Up to 20 bowel movements a day
 With severe diarrhea, protrusion of part of the rectum out of the body (rectal prolapse)
With severe diarrhea, protrusion of part of the rectum out of the body (rectal prolapse)
 Rarely, marked swelling of the intestine and tearing (perforation) of the large intestine
Rarely, marked swelling of the intestine and tearing (perforation) of the large intestine
 Hemolytic-uremic syndrome if the infection is due to Shigella dysenteriae
Hemolytic-uremic syndrome if the infection is due to Shigella dysenteriae
Severe dehydration can lead to shock and death, mainly in chronically ill, malnourished, or debilitated children and in older people. In hemolytic-uremic syndrome, red blood cells are destroyed, causing anemia with fatigue, weakness, and lightheadedness. Blood clots abnormally, causing the kidneys to stop functioning. Seizures or strokes can also occur.
Some adults develop eye inflammation, painful urination, and reactive arthritis (see page 570) weeks to months after the diarrhea.
Diagnosis
A doctor suspects shigellosis based on the typical symptoms of pain, fever, and watery or bloody diarrhea in people who are likely to have been exposed to the bacteria. To confirm the diagnosis, doctors may take a sample of stool and send it to a laboratory to grow (culture) the bacteria.
Prevention
Prevention includes the following:
 Infected people should not prepare food for others.
Infected people should not prepare food for others.
 After using the toilet, infected people should wash their hands, and someone should clean and disinfect the toilet before it is used again.
After using the toilet, infected people should wash their hands, and someone should clean and disinfect the toilet before it is used again.
 People caring for people with shigellosis should wash their hands with soap and water, particularly before they touch other people or handle food.
People caring for people with shigellosis should wash their hands with soap and water, particularly before they touch other people or handle food.
 Infected children with symptoms should not have contact with uninfected children.
Infected children with symptoms should not have contact with uninfected children.
 Diapers of infected children should be disposed of in a sealed garbage can, and the area used to change diapers should be wiped with disinfectant after each use.
Diapers of infected children should be disposed of in a sealed garbage can, and the area used to change diapers should be wiped with disinfectant after each use.
 Stool that contaminates clothing and bedclothes of infected people should be flushed away in running water, and the soiled clothing and bedclothes should be washed in a washing machine using the hot water cycle. When finished, surfaces of the sink, toilet, and washing machine should be wiped down with a disinfectant, such as diluted chlorine bleach.
Stool that contaminates clothing and bedclothes of infected people should be flushed away in running water, and the soiled clothing and bedclothes should be washed in a washing machine using the hot water cycle. When finished, surfaces of the sink, toilet, and washing machine should be wiped down with a disinfectant, such as diluted chlorine bleach.
Currently, no vaccine is available.
Treatment
Water and salts lost because of diarrhea are replaced, usually by mouth. Symptoms typically resolve within 4 to 8 days. Antibiotics are not routinely required for mild infections.
Severe infections may last 3 to 6 weeks and require hospitalization so that fluids containing salts can be given intravenously and complications, such as hemolytic-uremic syndrome, can be treated. Antibiotics, such as azithromycin, ciprofloxacin, or trimethoprim-sulfamethoxazole, are given, particularly when people are very young or very old, when the infection is severe, or when the infection is likely to spread to other people. Antibiotics reduce the severity of symptoms and the length of time the bacteria are excreted in stool.
Drugs to stop diarrhea (such as diphenoxylate or loperamide) may prolong the infection and should not be used.
Staphylococcus aureus Infections
Staphylococcus aureus is the most dangerous of all of the many common staphylococcal bacteria.
 These bacteria are spread by having direct contact with an infected person, by using a contaminated object, or by inhaling infected droplets dispersed by sneezing or coughing.
These bacteria are spread by having direct contact with an infected person, by using a contaminated object, or by inhaling infected droplets dispersed by sneezing or coughing.
 Skin infections are common, but the bacteria can spread through the bloodstream and infect distant organs.
Skin infections are common, but the bacteria can spread through the bloodstream and infect distant organs.
 Skin infections may cause blisters, abscesses, and redness and swelling in the infected area.
Skin infections may cause blisters, abscesses, and redness and swelling in the infected area.
 The diagnosis is based on the appearance of the skin or identification of the bacteria in a sample of the infected material.
The diagnosis is based on the appearance of the skin or identification of the bacteria in a sample of the infected material.
 Thoroughly washing the hands can help prevent spread of infection.
Thoroughly washing the hands can help prevent spread of infection.
 Antibiotics are chosen based on whether they are likely to be effective against the strain causing the infection.
Antibiotics are chosen based on whether they are likely to be effective against the strain causing the infection.
Staphylococcus aureus is present in the nose of adults (temporarily in 60% and permanently in 20 to 30%) and sometimes on the skin. People who have the bacteria but do not have any symptoms caused by the bacteria are called carriers. People most likely to be carriers include those whose skin is repeatedly punctured or broken, such as the following:
 People who have diabetes mellitus and have to regularly inject insulin
People who have diabetes mellitus and have to regularly inject insulin
 People who inject illegal drugs
People who inject illegal drugs
 People who are being treated with hemodialysis or chronic ambulatory peritoneal dialysis
People who are being treated with hemodialysis or chronic ambulatory peritoneal dialysis
 People with skin infections, AIDS, or previous staphylococcal bloodstream infections
People with skin infections, AIDS, or previous staphylococcal bloodstream infections
People can move the bacteria from their nose to other body parts with their hands, sometimes leading to infection. Carriers can develop infection if they have surgery, are treated with hemodialysis or chronic ambulatory peritoneal dialysis, or have AIDS.
The bacteria can spread from person to person by direct contact, through contaminated objects (such as telephones, door knobs, television remote controls, or elevator buttons), or, less often, by inhalation of infected droplets dispersed by sneezing or coughing.
Staphylococcus aureus infections range from mild to life threatening. The bacteria tend to infect the skin (see page 1315), often causing abscesses. However, the bacteria can travel through the bloodstream (causing bacteremia) and infect almost any site in the body, particularly heart valves (endocarditis—see page 386) and bones (osteomyelitis—see page 556). The bacteria also tend to accumulate on medical devices in the body, such as artificial heart valves or joints, heart pacemakers, and tubes (catheters) inserted through the skin into blood vessels.
Certain staphylococcal infections are more likely in certain situations:
 Endocarditis: When people inject illegal drugs, have an infected blood vessel catheter, or have an artificial heart valve
Endocarditis: When people inject illegal drugs, have an infected blood vessel catheter, or have an artificial heart valve
 Osteomyelitis: If Staphylococcus aureus spreads to the bone from infection in the bloodstream or from infection in adjacent soft tissue, as may occur in deep pressure sores or foot sores due to diabetes
Osteomyelitis: If Staphylococcus aureus spreads to the bone from infection in the bloodstream or from infection in adjacent soft tissue, as may occur in deep pressure sores or foot sores due to diabetes
 Lung infection (pneumonia): When people have had influenza (particularly) or a bloodstream infection or when they are hospitalized because they need tracheal intubation and mechanical ventilation (see page 527)
Lung infection (pneumonia): When people have had influenza (particularly) or a bloodstream infection or when they are hospitalized because they need tracheal intubation and mechanical ventilation (see page 527)
There are many strains of Staphylococcus aureus. Some strains produce toxins that can cause the symptoms of staphylococcal food poisoning (see page 151), toxic shock syndrome (see page 1182), and scalded skin syndrome (see page 1319).
Many strains have developed resistance to the effects of antibiotics. If carriers take antibiotics, the antibiotics kill the strains that are not resistant, leaving mainly the resistant strains. These bacteria may then multiply, and if they cause infection, the infection is more difficult to treat. Whether the bacteria are resistant and which antibiotics they resist often depend on where people got the infection: in a hospital or other health care facility or outside of such a facility (in the community).
Methicillin-Resistant Staphylococcus aureus (MRSA): Because antibiotics are widely used in hospitals, hospital staff members commonly carry resistant strains. When people are infected in a health care facility, the bacteria are usually resistant to several types of antibiotics, including all antibiotics that are related to penicillin (called beta-lactam antibiotics). Strains of bacteria that are resistant to beta-lactam antibiotics are called methicillin-resistant Staphylococcus aureus (MRSA). MRSA strains are common if infection is acquired in a health care facility, and more and more infections acquired in the community, including mild abscesses and skin infections, are caused by MRSA strains.
 Did You Know…
Did You Know…
Staphylococcal infections may be difficult to treat because many of the bacteria have developed resistance to antibiotics.
Symptoms
Skin infections due to Staphylococcus aureus can include the following:
 Folliculitis is the least serious. A hair root (follicle) is infected, causing a slightly painful, tiny pimple at the base of a hair.
Folliculitis is the least serious. A hair root (follicle) is infected, causing a slightly painful, tiny pimple at the base of a hair.
 Impetigo consists of shallow, fluid-filled blisters that rupture, leaving honey-colored crusts. Impetigo may itch or hurt.
Impetigo consists of shallow, fluid-filled blisters that rupture, leaving honey-colored crusts. Impetigo may itch or hurt.
 Abscesses (boils or furuncles) are warm, painful collections of pus just below the skin.
Abscesses (boils or furuncles) are warm, painful collections of pus just below the skin.
 Cellulitis is infection of skin and the tissue just under it. Cellulitis spreads, causing pain and redness.
Cellulitis is infection of skin and the tissue just under it. Cellulitis spreads, causing pain and redness.
 Toxic epidermal necrolysis and, in newborns, scalded skin syndrome are serious infections. Both lead to large-scale peeling of skin.
Toxic epidermal necrolysis and, in newborns, scalded skin syndrome are serious infections. Both lead to large-scale peeling of skin.
All staphylococcal skin infections are very contagious.
Breast infections (mastitis), which may include cellulitis and abscesses, can develop 1 to 4 weeks after delivery. The area around the nipple is red and painful. Abscesses often release large numbers of bacteria into the mother’s milk. The bacteria may then infect the nursing infant.
Pneumonia often causes a high fever, shortness of breath, and a cough with sputum that may be tinged with blood. Lung abscesses may develop. They sometimes enlarge and involve the membranes around the lungs (causing pleurisy) and sometimes cause pus to collect (called an empyema). These problems make breathing even more difficult.
Bloodstream infection is a common cause of death in people with severe burns. Symptoms typically include a persistent high fever and sometimes shock.
Endocarditis can quickly damage heart valves, leading to heart failure (with difficulty breathing) and possibly death.
Osteomyelitis causes chills, fever, and bone pain. The skin and soft tissues over the infected bone become red and swollen, and fluid may accumulate in nearby joints.
Diagnosis
Skin infections are usually diagnosed based on their appearance. Other infections require samples of blood or infected fluids, which are sent to a laboratory to grow (culture) the bacteria. Laboratory results confirm the diagnosis and determine which antibiotics can kill the staphylococci (called susceptibility testing).
If a doctor suspects osteomyelitis, x-rays, computed tomography (CT), magnetic resonance imaging (MRI), or a combination is also done. These tests can show where the damage is and help determine how severe it is.
Prevention
People can help prevent the spread of these bacteria by always thoroughly washing their hands with soap and water or with antibacterial hand sanitizer gels. The bacteria can be eliminated from the nose by applying the antibiotic mupirocin inside the nostrils. However, because overusing mupirocin can lead to mupirocin resistance, this antibiotic is used only when people are likely to get an infection. For example, it is given to people before certain operations or to people who live in a household in which the skin infection is spreading.
Treatment
Infections due to Staphylococcus aureus are treated with antibiotics. Doctors try to determine whether the bacteria are resistant to antibiotics and, if so, to which antibiotics.
Infection that is acquired in a hospital is treated with antibiotics that are effective against methicillinresistant Staphylococcus aureus (MRSA): ceftobiprole, vancomycin, linezolid, quinupristin plus dalfopristin, or daptomycin. If results of testing later indicate that the strain is susceptible to methicillin and the person is not allergic to penicillin, a drug related to methicillin, such as nafcillin, is used. Depending on how severe the infection is, antibiotics may be given for weeks.
MRSA infection can be acquired outside of a health care facility. The community-acquired MRSA strains are usually susceptible to other antibiotics, such as trimethoprim-sulfamethoxazole, clindamycin, minocycline, or doxycycline, as well as to the antibiotics used to treat MRSA infections acquired in the hospital. Mild skin infections due to MRSA, such as folliculitis, are usually treated with an ointment, such as one that contains bacitracin, neomycin, and polymyxin B (available without a prescription) or mupirocin (available by prescription only). If more than an ointment is required, antibiotics effective against MRSA are given by mouth or intravenously. Which antibiotic is used depends on the severity of the infection and the results of susceptibility testing.
If an infection involves bone or foreign material in the body (such as heart pacemakers, artificial heart valves and joints, and blood vessel grafts), rifampin is sometimes added to the antibiotic regimen. Usually, infected bone and foreign material has to be removed surgically to cure the infection.
Abscesses, if present, are usually drained.
OTHER STAPHYLOCOCCAL INFECTIONS
Staphylococcus aureus produces an enzyme called coagulase. Other species of staphylococci do not and thus are called coagulase-negative staphylococci. These bacteria normally reside in the skin of all healthy people.
These bacteria, although less dangerous than Staphylococcus aureus, can cause serious infections, usually when acquired in a hospital. The bacteria may infect catheters inserted through the skin into a blood vessel or implanted medical devices (such as pacemakers or artificial heart valves and joints).
These bacteria are often resistant to many antibiotics. Vancomycin, which is effective against many resistant bacteria, is used, sometimes with rifampin. Medical devices, if infected, often must be removed.
Streptococcal Infections
Streptococcal infections are caused by any one of several species of Streptococcus.
 Different groups of these bacteria are spread in different ways—for example, through coughing or sneezing, through contact with infected wounds or sores, or during vaginal delivery (from mother to child).
Different groups of these bacteria are spread in different ways—for example, through coughing or sneezing, through contact with infected wounds or sores, or during vaginal delivery (from mother to child).
 These infections affect various areas of the body, including the throat, middle ear, sinuses, lungs, skin, tissue under the skin, heart valves, and bloodstream.
These infections affect various areas of the body, including the throat, middle ear, sinuses, lungs, skin, tissue under the skin, heart valves, and bloodstream.
 Symptoms may include red and painful swollen tissues, scabby sores, sore (strep) throat, and a rash, depending on the area affected.
Symptoms may include red and painful swollen tissues, scabby sores, sore (strep) throat, and a rash, depending on the area affected.
 Doctors may be able to diagnose the infection based on symptoms and can confirm the diagnosis by identifying the bacteria in a sample of infected tissue, sometimes supplemented with imaging tests.
Doctors may be able to diagnose the infection based on symptoms and can confirm the diagnosis by identifying the bacteria in a sample of infected tissue, sometimes supplemented with imaging tests.
 Antibiotics are given by mouth or, for serious infections, intravenously.
Antibiotics are given by mouth or, for serious infections, intravenously.
Many species of streptococci live harmlessly in and on the body. Some species that can cause infection are also present in some healthy people but cause no symptoms. These people are called carriers.
Types of Streptococci: The species that cause disease are divided into groups based on their appearance when grown in the laboratory and on their different chemical components. Each group tends to produce specific infections. Groups include group A, group B, and viridans.
Spread: Group A streptococci, as well as Streptococcus pneumoniae, are spread through inhalation of droplets of secretions from the nose or throat, dispersed when an infected person coughs or sneezes, or through contact with infected wounds or sores on the skin. Usually, the bacteria are not spread through casual contact, but they may spread in crowded environments such as dormitories, schools, and military barracks. After 24 hours of antibiotic treatment, people no longer can spread the bacteria to others.
Group B streptococci can be spread to newborns through vaginal secretions during vaginal delivery.
Viridans streptococci inhabit the mouth of healthy people but can invade the bloodstream, especially in people with periodontal inflammation, and infect heart valves (causing endocarditis).
 Did You Know…
Did You Know…
The bacteria that cause a particularly dangerous streptococcal infection called necrotizing fasciitis are sometimes described as flesh eating.
Symptoms
Symptoms vary, depending on where the infection is:
STREPTOCOCCI AND SOME DISORDERS THEY CAUSE
| SPECIES | CIRCUMSTANCES | DISORDERS |
| Group A | ||
| Streptococcus pyogenes | Ears, nose, and throat | Middle ear infection (otitis media) Sinusitis Sore throat (pharyngitis, called strep throat) |
| Skin | Cellulitis (infection of tissues just under the skin) Erysipelas (a superficial form of cellulitis) Impetigo (a skin infection) Wound infections |
|
| Other | Infection of heart valves (endocarditis) Necrotizing fasciitis Pleurisy Pneumonia Scarlet fever (no longer common) Streptococcal toxic shock syndrome |
|
| Disorders that develop after streptococcal infections | Glomerulonephritis (kidney inflammation) Rheumatic fever |
|
| Group B | ||
| Streptococcus agalactiae | In adults, especially those with diabetes mellitus | Abscesses Cellulitis Wound infections |
| In newborns | Bloodstream infections (sepsis) Meningitis Pneumonia |
|
| In women after delivery of a baby | Bloodstream infections Infection of the uterus (endometritis) |
|
| Viridans | ||
| Various species | — | Dental cavities Infection of heart valves (endocarditis) that have been damaged by a disorder such as a congenital heart disorder or rheumatic fever |
| Streptococcus pneumoniae | — | Meningitis Middle ear infection (otitis media) Pneumonia acquired outside of health care facilities (in the community) Sinusitis |
 Cellulitis: The infected skin becomes red, and the tissue under it swells, causing pain.
Cellulitis: The infected skin becomes red, and the tissue under it swells, causing pain.
 Impetigo: Usually, scabby, yellow-crusted sores form (see page 1317).
Impetigo: Usually, scabby, yellow-crusted sores form (see page 1317).
 Necrotizing fasciitis: The connective tissue that covers muscle (fascia) is infected. People have sudden chills, fever, and severe pain and tenderness in the affected area. The skin may appear normal until infection is severe (see page 1318).
Necrotizing fasciitis: The connective tissue that covers muscle (fascia) is infected. People have sudden chills, fever, and severe pain and tenderness in the affected area. The skin may appear normal until infection is severe (see page 1318).
 Strep throat (pharyngitis): This infection usually occurs in children 5 to 15 years old. Children under 3 years old seldom get strep throat. Symptoms often appear suddenly. The throat becomes sore. Children may also have chills, fever, headache, nausea, vomiting, and a general feeling of illness (malaise). The throat is beefy red, and the tonsils are swollen, with or without patches of pus. Lymph nodes in the neck are usually enlarged and tender. However, children under 3 years old may not have these symptoms. They may have only a runny nose. If people with a sore throat have a cough, red eyes, hoarseness, diarrhea, or a stuffy nose, the cause is probably a viral infection, not a streptococcal infection.
Strep throat (pharyngitis): This infection usually occurs in children 5 to 15 years old. Children under 3 years old seldom get strep throat. Symptoms often appear suddenly. The throat becomes sore. Children may also have chills, fever, headache, nausea, vomiting, and a general feeling of illness (malaise). The throat is beefy red, and the tonsils are swollen, with or without patches of pus. Lymph nodes in the neck are usually enlarged and tender. However, children under 3 years old may not have these symptoms. They may have only a runny nose. If people with a sore throat have a cough, red eyes, hoarseness, diarrhea, or a stuffy nose, the cause is probably a viral infection, not a streptococcal infection.
 Scarlet fever: A rash appears first on the face, then spreads to the trunk and limbs. The rash feels like coarse sandpaper. The rash is worse in skinfolds, such as the crease between the legs and the trunk. As the rash fades, the skin peels. Red bumps develop on the tongue, which is coated with a yellowish white film. The film then peels, and the tongue appears beefy red (strawberry tongue).
Scarlet fever: A rash appears first on the face, then spreads to the trunk and limbs. The rash feels like coarse sandpaper. The rash is worse in skinfolds, such as the crease between the legs and the trunk. As the rash fades, the skin peels. Red bumps develop on the tongue, which is coated with a yellowish white film. The film then peels, and the tongue appears beefy red (strawberry tongue).
Diagnosis
Doctors suspect strep throat based on the following:
 Fever
Fever
 Enlarged and tender lymph nodes in the neck
Enlarged and tender lymph nodes in the neck
 Pus in or on the tonsils
Pus in or on the tonsils
 Absence of cough
Absence of cough
The main reason for diagnosing strep throat is to reduce the chance of developing complications, such as infection of the sinuses, middle ear, or mastoid bone or rheumatic fever, by using antibiotics. However, because symptoms of group A strep throat are often similar to those of throat infection due to a virus, testing with a throat culture or another test is necessary to confirm the diagnosis. Several diagnostic tests (called rapid tests) can be completed in minutes. For these tests, a swab is used to take a sample from the throat. If these results indicate infection (positive results), the diagnosis of strep throat is confirmed, and a throat culture, which takes longer to process, is not needed. However, results of rapid tests sometimes indicate no infection when infection is present (called false-negative results). If results are negative in children and adolescents, culture is needed. A sample taken from the throat with a swab is sent to a laboratory so that group A streptococci, if present, can be grown (cultured) overnight. In adults, negative results do not require confirmation by culture because the incidence of streptococcal infection and risk of rheumatic fever in adults is so low.
If group A streptococci are identified, they may be tested to see which antibiotics are effective (a process called susceptibility testing).
Cellulitis and impetigo can often be diagnosed based on symptoms, although culture of a sample taken from impetigo sores can often help doctors identify other microorganisms that may be the cause, such as Staphylococcus aureus.
To diagnose necrotizing fasciitis, doctors frequently use x-rays, computed tomography (CT), or magnetic resonance imaging (MRI) and culture. Exploratory surgery is often required to confirm the diagnosis.
Treatment
Strep throat usually resolves within 1 to 2 weeks, even without treatment. Antibiotics reduce the severity of symptoms but shorten their duration by only about 1 day. Nevertheless, antibiotics are given to help prevent the spread of the infection to the middle ear, sinuses, and mastoid bone, as well as to prevent spread to other people. Antibiotic therapy also helps prevent rheumatic fever, although it may not prevent kidney inflammation (glomerulonephritis). Usually, antibiotics need not be started immediately. Waiting up to 9 days for culture results before starting antibiotics does not increase the risk of rheumatic fever. An exception is when a family member has or has had rheumatic fever. Then, every streptococcal infection in any family member should be treated as soon as possible.
Usually, penicillin or amoxicillin is given by mouth for 10 days. One injection of a long-acting penicillin (benzathine) can be given instead. People who cannot take penicillin can be given erythromycin, clarithromycin, or clindamycin by mouth for 10 days or azithromycin for 5 days. Usually, the bacteria that cause strep throat are not resistant to penicillin. In the United States, about 5 to 10% of these bacteria are resistant to erythromycin and related drugs (azithromycin and clarithromycin), but in some countries, more than 10% are resistant.
Fever, headache, and sore throat can be treated with acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), which reduce pain and fever. Neither bed rest nor isolation is necessary.
Serious streptococcal infections (such as necrotizing fasciitis, endocarditis, and severe cellulitis) require penicillin, given intravenously, sometimes with other antibiotics. In necrotizing fasciitis, dead, infected tissue must be surgically removed.
Tetanus
Tetanus (lockjaw) results from a toxin produced by the anaerobic bacteria Clostridium tetani. The toxin makes muscles become rigid and contract involuntarily (spasm).
 Tetanus is rare in the United States but is common in developing countries.
Tetanus is rare in the United States but is common in developing countries.
 Diagnosis is based on symptoms
Diagnosis is based on symptoms
 Vaccination and wound care can prevent tetanus.
Vaccination and wound care can prevent tetanus.
 Treatment focuses on treating symptoms until they resolve.
Treatment focuses on treating symptoms until they resolve.
AFTER A WOUND: WHO NEEDS A TETANUS SHOT?

Although rare in the United States, tetanus kills up to 500,000 people each year, mainly in developing countries.
Clostridium tetani is present in soil and animal feces. Tetanus bacteria may enter the body through wounds contaminated with soil or feces (especially if the wound is not adequately cleaned) and skin punctures by nonsterile needles (such as those used to inject illegal drugs or to tattoo or do body piercing). Sometimes the injury is so small that people do not even go to a doctor. Injuries that involve dead skin (such as burns, frostbite, gangrene, or crush injuries) are more likely to cause tetanus. When oxygen is absent in dead tissue, tetanus spores reproduce and produce a toxin that travels through the body and prevents nerves from sending signals to other nerves. Occasionally, tetanus results when the uterus is damaged during an induced abortion or childbirth. In developing countries, soil contamination of the stump of the umbilical cord can cause tetanus in newborns.
Vaccination during childhood plus booster doses every 10 years during adulthood can prevent tetanus. Thus, the infection occurs mainly in people who have not been vaccinated or not kept their vaccinations up to date. This situation is more common in developing countries. In the United States, tetanus is a risk for people who inject drugs. The risk is also higher for older people but usually only if they have never been vaccinated.
Symptoms
Symptoms usually begin about 5 to 10 days after the injury. Muscles contract involuntarily (spasm) and become rigid. Spasms usually begin in the jaw (causing lockjaw) and throat (making swallowing difficult), followed by the neck, shoulder, face, and then the abdomen and limbs. Back muscles contract, making the back arch. Spasms of sphincter muscles can lead to constipation and difficulty urinating. People may have a rapid heart beat, profuse sweating, and a high fever. Slight disturbances—such as noise, a draft, or the bed being jarred—can trigger painful muscle spasms throughout the body. Such spasms may interfere with breathing, sometimes so much that people turn blue. Rarely, muscle spasms may be limited to muscle groups near the wound. Such localized tetanus may persist for weeks. Even when the illness is severe, people remain fully conscious.
Worldwide, about 50% of people who have tetanus die. But in the United States, only about 10 to 15% die if the disorder is treated appropriately. People who inject drugs, the very young, and the very old are more likely to die of tetanus.
 Did You Know…
Did You Know…
Promptly and thoroughly cleaning dirty wounds can help prevent tetanus.
Diagnosis
A doctor suspects tetanus when certain muscles (commonly, jaw and back muscles) become rigid or spasms occur, particularly in people who have a wound. The bacteria can sometimes be grown (cultured) from a sample taken from the wound. Detecting the bacteria in cultures confirms the diagnosis, but tetanus is possible even if no bacteria are detected.
Prevention
Preventing tetanus is far better than treating tetanus. Tetanus rarely develops in people who have completed a primary series of tetanus vaccinations (three or more injections into a muscle) and had vaccinations every 10 years, as recommended. The tetanus vaccine stimulates the body to produce antibodies that neutralize the toxin. But neutralization can take weeks. In young children, the tetanus vaccine is given as part of a series that includes the diphtheria and pertussis (whooping cough) vaccines. Adults who have completed the primary series of tetanus vaccination should get tetanus boosters every 10 years.
When people are injured, they can help prevent tetanus by promptly and thoroughly cleaning wounds. People who have wounds may be given tetanus vaccine to prevent tetanus from developing. Because the vaccine takes weeks to be effective, tetanus immune globulin is sometimes given in addition. It provides antibodies that neutralize the toxin immediately.
Treatment
People with tetanus are admitted to an intensive care unit. The room is kept quiet to prevent disturbances that could trigger muscle spasms. Wounds are cleaned thoroughly, and dead tissue and foreign material are removed.
Antibiotics (usually metronidazole) are given intravenously to kill the bacteria and thus stop the production of toxin. However, antibiotics have no effect on toxin that has already been produced. Tetanus immune globulin is usually given to neutralize the toxin already produced. Tetanus vaccine is given unless vaccinations are known to be up to date.
Sedatives, such as the benzodiazepine diazepam, may be given to control muscle spasms, to help relax rigid muscles, and to relieve pain and anxiety. If muscle rigidity interferes with breathing, an opening may be made in the windpipe (called tracheostomy). Sometimes mechanical ventilation is also needed. If swallowing is difficult, nutrition and fluids are given intravenously or, less often, through a tube inserted through the nose and into the stomach.
After people recover, they are given the full series of vaccinations to prevent future episodes of tetanus.
Toxic Shock Syndrome
Toxic shock syndrome is a group of rapidly progressive and severe symptoms that include fever, rash, dangerously low blood pressure, and failure of several organs. It is caused by toxins produced by Staphylococcus aureus or group A streptococci.
 Using superabsorbent tampons or having an infection caused by Staphylococcus aureus or group A streptococci increases the risk of this syndrome.
Using superabsorbent tampons or having an infection caused by Staphylococcus aureus or group A streptococci increases the risk of this syndrome.
 The syndrome can be fatal, particularly when caused by streptococci.
The syndrome can be fatal, particularly when caused by streptococci.
 Changing tampons frequently and not using superabsorbent tampons can help reduce the risk of the syndrome.
Changing tampons frequently and not using superabsorbent tampons can help reduce the risk of the syndrome.
 Treatment focuses on relieving symptoms and preventing production of more toxin.
Treatment focuses on relieving symptoms and preventing production of more toxin.
Toxic shock syndrome results from toxins produced by Staphylococcus aureus or group A streptococci. It may occur when Staphylococcus aureus infects tissue (for example, in a wound) or is simply growing on a tampon (especially the superabsorbent type) in the vagina. Exactly why superabsorbent tampons increase the risk of this syndrome is unknown. Leaving a diaphragm in the vagina for more than 24 hours also increases the risk slightly. This syndrome may also occur in the following situations:
 When a surgical incision is infected, even when the infection seems minor
When a surgical incision is infected, even when the infection seems minor
 When the uterus becomes infected after delivery of a baby
When the uterus becomes infected after delivery of a baby
 After nose surgery if bandages are used to pack the nose
After nose surgery if bandages are used to pack the nose
 In otherwise healthy people who have a group A streptococcal tissue infection, usually of the skin
In otherwise healthy people who have a group A streptococcal tissue infection, usually of the skin
Symptoms
If staphylococci or streptococci are the cause, symptoms develop suddenly and worsen rapidly over a few days. People may have a high fever, a red and sore throat, red eyes, diarrhea, and muscle aches. A rash that resembles sunburn covers the entire body, including the palms and soles. Then, the skin peels. Blood pressure falls to dangerously low levels, and people become delirious. Fluid accumulates in tissues, causing swelling (edema). Blood does not clot normally, making bleeding more likely and more severe. Several organs such as the kidneys, liver, heart, and lungs may malfunction or stop functioning.
In streptococcal toxic shock syndrome, the wound is painful. Gangrene may develop around the wound.
When streptococci are involved, up to 70% of people die. When staphylococci are involved, 5% of people die if the syndrome is related to menstruation, and 15% die if it is not. If people survive, recovery is usually complete.
When the source is a tampon infected by staphylococci, the syndrome may recur, usually within 4 months of the first episode. Occasionally, the syndrome recurs more than once. Each episode tends to be milder. To reduce the risk of recurrences, women who have had the syndrome should not use tampons or diaphragms.
Diagnosis
The diagnosis is usually based on the symptoms and results of a physical examination and routine blood tests. Samples of blood and infected tissue are sent to a laboratory where bacteria can be grown (cultured).
Prevention
Women who use tampons can take several measures to prevent infection:
 Not using superabsorbent tampons
Not using superabsorbent tampons
 Using the least absorbent tampons needed
Using the least absorbent tampons needed
 Alternating use of tampons and pads
Alternating use of tampons and pads
 Changing tampons every 4 to 8 hours
Changing tampons every 4 to 8 hours
Otherwise, there are no recommendations for preventing toxic shock syndrome.
Treatment
If toxic shock syndrome is suspected, people are hospitalized, usually in an intensive care unit. Fluids that contain salts and often drugs to increase blood pressure to normal levels are given intravenously. Many people need help with breathing, usually with a mechanical ventilator. Tampons, diaphragms, and other foreign objects are removed from the vagina promptly. Antibiotics and, for severe cases, immune globulin (which can neutralize the toxin) are given intravenously. Areas that could contain the bacteria, such as surgical wounds and the vagina, are flushed out with water (irrigated).
If wounds are infected, surgery may be needed to clean them out further, to remove infected tissue, or sometimes, if gangrene has developed, to remove a limb.
Tularemia
Tularemia (rabbit fever, deer fly fever) is infection that is caused by the bacteria Francisella tularensis, which is acquired from wild animals, usually rabbits.
 Handling carcasses, being bitten by a tick, inhaling infected sprayed particles, and eating or drinking infected material can cause infection.
Handling carcasses, being bitten by a tick, inhaling infected sprayed particles, and eating or drinking infected material can cause infection.
 Symptoms can include fever, sores, and swollen lymph nodes.
Symptoms can include fever, sores, and swollen lymph nodes.
 Cultures of tissue samples or blood help doctors make the diagnosis.
Cultures of tissue samples or blood help doctors make the diagnosis.
 Injections of antibiotics are almost always effective.
Injections of antibiotics are almost always effective.
 Preventing tick bites, handling carcasses carefully, and disinfecting water can reduce the risk of tularemia.
Preventing tick bites, handling carcasses carefully, and disinfecting water can reduce the risk of tularemia.
Francisella tularensis is normally present in animals, especially rodents, rabbits, and hares. People may be infected by doing the following:
 Handling infected animal carcasses (as when hunters skin rabbits or when butchers, farmers, fur handlers, and laboratory workers handle animals or animal products)
Handling infected animal carcasses (as when hunters skin rabbits or when butchers, farmers, fur handlers, and laboratory workers handle animals or animal products)
 Being bitten by an infected tick, deerfly, or other insect, usually during the summer (particularly for children)
Being bitten by an infected tick, deerfly, or other insect, usually during the summer (particularly for children)
 Eating or drinking contaminated food (such as undercooked rabbit meat) or water
Eating or drinking contaminated food (such as undercooked rabbit meat) or water
 Inhaling airborne particles that contain the bacteria (as when grass is mowed or brush is cut or when people are working with the bacteria in a laboratory)
Inhaling airborne particles that contain the bacteria (as when grass is mowed or brush is cut or when people are working with the bacteria in a laboratory)
Francisella tularensis is a potential biological weapon. It can be spread through the air and be inhaled. The size of the airborne particles determines where they lodge in the respiratory tract. Small particles lodge in air sacs of the lungs and cause pneumonia.
Tularemia is not spread from person to person.
Symptoms
Different types of tularemia affect different parts of the body and thus cause different symptoms. Symptoms usually appear 3 to 5 days after exposure to the bacteria but can take up to 14 days.
Sores may develop near the scratch or bite that started the infection. Lymph nodes near the infected area may swell and become painful. A fever up to 104° F (40° C) may appear suddenly, with chills, drenching sweats, and muscle aches. People may have a general feeling of illness (malaise) and feel nauseated. They may vomit and lose weight. A rash may appear at any time. Sometimes pus collects, forming an abscess.
Overall, without treatment, 5 to 15% of people with tularemia die. However, with certain types of tularemia (typhoidal or pneumonic), 30 to 60% die. With appropriate treatment, fewer than 1% die. Death usually results from overwhelming infection, pneumonia, meningitis, or infection of the lining of the abdominal cavity (peritonitis).
Relapses are uncommon but can occur if treatment is inadequate. People who have had tularemia are immune to reinfection.
Types of Tularemia
There are several types of tularemia.
Ulceroglandular: This type is the most common. Open painful sores develop where the bacteria entered the skin: through a break in the skin, usually on the hands and fingers, or a tick bite, usually in the groin, armpit, or trunk. The bacteria travel to nearby lymph nodes, making them swollen and painful. Occasionally, the skin around the lymph nodes breaks down, and pus may drain from them.
Glandular: The lymph nodes become swollen and painful, but sores do not form.
Oculoglandular: An eye becomes painful, swollen, and red, and pus often oozes from it. Nearby lymph nodes become swollen and painful. This type probably results from touching the eye with a contaminated finger or from having infected fluid splashed into the eye.
Oropharyngeal: The throat (pharynx) is sore, and lymph nodes in the neck are swollen. Some people also have abdominal pain, nausea, vomiting, and diarrhea. This type is usually caused by eating under-cooked contaminated meat.
Typhoidal: Chills, high fever, and abdominal pain develop, but no sores form and lymph nodes do not swell. This type develops when the bloodstream is infected. Sometimes the source of infection is unknown.
Pneumonic: The lungs are infected. People may have a dry cough, be short of breath, and have chest pain. This type is caused by inhaling the bacteria or spread of the bacteria through the bloodstream to the lungs. This type develops in 10 to 15% of people with ulceroglandular tularemia and in 50% of people with typhoidal tularemia.
Diagnosis
A doctor suspects tularemia in people who develop sudden fever, swollen lymph nodes, and characteristic sores after having been exposed to ticks or deer flies or after having even slight contact with a wild mammal (especially a rabbit).
Samples of infected material, such as blood, fluids from a lymph node, pus from sores, or sputum, are taken. They are sent to a laboratory where the bacteria can be grown (cultured). Blood may also be tested for antibodies to the bacteria.
Prevention
If people are visiting areas where tularemia is common, they should do all of the following:
 Apply insect repellent containing 25 to 30% diethyltoluamide (DEET) to exposed skin
Apply insect repellent containing 25 to 30% diethyltoluamide (DEET) to exposed skin
 Wear clothing treated with a repellent containing permethrin
Wear clothing treated with a repellent containing permethrin
 Stay on paths and trails when walking in wooded areas
Stay on paths and trails when walking in wooded areas
 Walk in the center of trails to avoid brushing against bushes and weeds
Walk in the center of trails to avoid brushing against bushes and weeds
 Wear long pants and tuck them into socks and boots
Wear long pants and tuck them into socks and boots
 Thoroughly search their clothing, themselves, family members, and pets for ticks
Thoroughly search their clothing, themselves, family members, and pets for ticks
 Not drink or bathe, swim or work in untreated water, which may be contaminated
Not drink or bathe, swim or work in untreated water, which may be contaminated
Promptly searching for ticks can help prevent the infection because transmission of infection usually requires that ticks be attached for 4 or more hours. If found, ticks should be removed immediately (see box on page 1166).
When handling rabbits and rodents, people should wear protective clothing (such as rubber gloves and face masks) because bacteria may be present. Wild birds and game should be thoroughly cooked before they are eaten.
A vaccine is available, but it is given only to people whose occupation puts them at risk, mainly laboratory workers. After exposure to the bacteria (for example, after a laboratory accident), people are given doxycycline or ciprofloxacin to prevent the infection from developing.
Treatment
People who have tularemia do not need to be isolated. Tularemia is usually treated with injections of gentamicin or streptomycin for 7 to 14 days. Other antibiotics, including fluoroquinolones (such as ciprofloxacin and levofloxacin) and tetracyclines (such as minocycline and doxycycline), are also effective.
Rarely, large abscesses must be drained surgically. Applying warm compresses to an affected eye, wearing dark glasses, and using prescription eye drops may help. People with intense headaches are usually treated with opioids, such as oxycodone.