CHAPTER 242
Vaginal Infections
 Vaginal infections are caused by microorganisms, but women can take precautions, such as wearing loose, absorbent underwear, to reduce their risk of getting infections.
Vaginal infections are caused by microorganisms, but women can take precautions, such as wearing loose, absorbent underwear, to reduce their risk of getting infections.
 Infections usually cause a discharge with itching, redness, and sometimes burning and soreness.
Infections usually cause a discharge with itching, redness, and sometimes burning and soreness.
 Doctors examine a sample of fluids from the vagina or cervix to check for microorganisms that can cause infections.
Doctors examine a sample of fluids from the vagina or cervix to check for microorganisms that can cause infections.
 Treatment depends on the cause, but a sitz bath and antihistamines taken by mouth can help relieve itching.
Treatment depends on the cause, but a sitz bath and antihistamines taken by mouth can help relieve itching.
In the United States, vaginal infections are one of the most common reasons women see their doctor, accounting for more than 10 million visits each year. Vaginal infections can cause discomfort, discharge, and vaginal odor. However, these symptoms do not necessarily indicate an infection. Instead, they may result from irritation of the vagina by chemicals or other materials such as hygiene products, bubble bath, laundry detergents, contraceptive foams and jellies, and synthetic underwear. The inflammation that results is called noninfectious vaginitis.
 Did You Know…
Did You Know…
Children may get a vaginal infection when they move bacteria from the anus to the vagina by wiping from back to front.
Vaginal discharge may not be caused by a vaginal infection. A discharge can result from certain sexually transmitted diseases such as chlamydial infection (see page 1266) or gonorrhea (see page 1269). These diseases affect other reproductive organs, such as the cervix or uterus. Genital herpes (see page 1245), which can cause blisters on the vulva, in the vagina, and on the cervix, can also cause a vaginal discharge.
Causes
Vaginal infections may be caused by bacteria, yeast, and other microorganisms.
Certain conditions make infection more likely:
 Reduced acidity (increased pH) in the vagina: When acidity in the vagina is reduced, the number of protective bacteria that normally live in the vagina decreases, and the number of bacteria that can cause infection increases (see page 1539).
Reduced acidity (increased pH) in the vagina: When acidity in the vagina is reduced, the number of protective bacteria that normally live in the vagina decreases, and the number of bacteria that can cause infection increases (see page 1539).
 Poor hygiene: When the genital area is not kept clean, the number of bacteria increases, making bacterial infections more likely.
Poor hygiene: When the genital area is not kept clean, the number of bacteria increases, making bacterial infections more likely.
 Tight, nonabsorbent underwear: This type of underwear may trap moisture, which encourages the growth of bacteria and yeast.
Tight, nonabsorbent underwear: This type of underwear may trap moisture, which encourages the growth of bacteria and yeast.
 Tissue damage: If tissues in the pelvis are damaged, the body’s natural defenses are weakened. Damage can result from tumors, surgery, radiation therapy, or structural abnormalities such as birth defects or fistulas. Fistulas are abnormal connections between organs, which may, for example, allow the intestine’s contents to enter the vagina.
Tissue damage: If tissues in the pelvis are damaged, the body’s natural defenses are weakened. Damage can result from tumors, surgery, radiation therapy, or structural abnormalities such as birth defects or fistulas. Fistulas are abnormal connections between organs, which may, for example, allow the intestine’s contents to enter the vagina.
 Irritation: Irritation of vaginal tissues can lead to cracks or sores, which provide access to the bloodstream for bacteria and yeast.
Irritation: Irritation of vaginal tissues can lead to cracks or sores, which provide access to the bloodstream for bacteria and yeast.
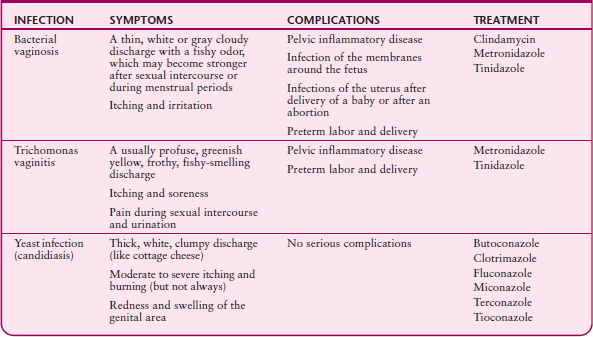
SOME VAGINAL INFECTIONS
Some specific causes of infection are more common among certain age groups.
Children: In children, vaginal infections are usually caused by bacteria from the anus. These bacteria may be moved to the vagina when girls, particularly those aged 2 to 6 years, wipe from back to front or do not adequately clean the genital area after bowel movements. Fingering the genital area, particularly if girls do not wash their hands after bowel movements, may also move these bacteria to the vagina. Fingering is often a response to itching.
Putting an object (such as a toy or toilet tissue) in the vagina is another common cause of vaginal infections. Pinworms may also cause vaginal infections.
Women of Reproductive Age: Hormonal changes shortly before and during menstrual periods or during pregnancy can reduce acidity in the vagina, as can frequent douching, use of spermicides, and semen. Reduced acidity encourages the growth of bacteria that cause disease.
Leaving tampons in too long can lead to infection, possibly because tampons provide a warm, moist environment where bacteria can thrive and because they can irritate the vagina.
Postmenopausal Women: After menopause, estrogen levels decrease. As a result, tissues in the vagina become thinner, drier, and more fragile. Cracks or sores may form, providing access for bacteria or yeast. Also, acidity in the vagina decreases.
Women who have urinary incontinence or are confined to bed may have difficulty keeping the genital area clean. Irritation from urine and stool can lead to infection.
 Did You Know…
Did You Know…
Douching often can remove normal, protective bacteria from the vagina, increasing the risk of infection.
Symptoms
Typically, vaginal infections produce a vaginal discharge. This discharge differs from a normal one because it is accompanied by itching, redness, and sometimes burning or soreness in the genital area. A discharge may have a fishy odor. The appearance and amount of the discharge tend to vary depending on the cause. However, different disorders sometimes cause similar discharges.
Nearby Infections: Vulvitis and Bartholinitis
The vulva is the area surrounding the opening of the vagina and containing the external female genital organs. Bartholin’s glands, which are external genital organs, are located on either side of the opening of the vagina.
Vulvitis: Vulvitis is inflammation of the vulva. When both the vulva and vagina are inflamed, the disorder is called vulvovaginitis. Vulvitis may result from allergic reactions to substances that come in contact with the vulva (such as soaps, bubble bath, fabrics, and perfumes), from skin disorders (such as dermatitis), or from infections, including yeast infections and sexually transmitted diseases (such as herpes). The vulva may be infested by pubic lice—a disorder called pediculosis pubis.
In children, infections of the vagina may also affect the vulva. These infections may be due to bacteria from the anus or other bacteria.
Urine or stool, if it remains in contact with the vulva, can irritate it and cause ongoing (chronic) vulvitis. Women who have incontinence or are confined to bed may have this problem.
Vulvitis causes itching, soreness, and redness. Rarely, the folds of skin around the vaginal and urethral openings (labia) become stuck together. Chronic vulvitis may result in sore, scaly, thickened, or whitish patches on the vulva. If chronic vulvitis does not respond to treatment, doctors usually do a biopsy to look for the cause, including skin disorders of the vulva (vulvar dystrophies, such as lichen sclerosus or squamous cell hyperplasia) or cancer.
Bartholinitis: Bartholinitis—infection of one or both glands or their ducts—may develop when bacteria from the vagina enter the glands. Rarely, bartholinitis is due to a sexually transmitted disease. Pus can accumulate in the gland, causing a painful, swollen abscess.
If the ducts to the gland become blocked, the gland may swell without causing pain—a disorder called Bartholin’s cyst. A cyst may become infected.
Doctors can diagnose Bartholin’s cyst and bartholinitis during a physical examination. In women 40 and older, a cyst is usually biopsied.
Cysts that cause no symptoms do not require treatment. Infections are treated with an antibiotic, which usually clears the infection in a few days if there is no abscess. However, the infection may recur. Analgesics may be taken to relieve pain.
Abscesses are usually drained.
Itching may interfere with sleep. Some infections can make sexual intercourse painful and make urination painful and more frequent. Rarely, the folds of skin around the vaginal and urethral openings become stuck together. However, sometimes symptoms are mild or do not occur.
Diagnosis
Girls or women who have a vaginal discharge with itching or who have other vaginal symptoms should see a doctor. To determine the cause, the doctor asks questions about the discharge (if present), about possible causes of the symptoms, and about hygiene. Questions may include the following:
 Have lotions or creams (including home remedies) been used to try to relieve the symptoms?
Have lotions or creams (including home remedies) been used to try to relieve the symptoms?
 When did the discharge begin?
When did the discharge begin?
 Was the discharge accompanied by itching, burning, pain, or a sore in the genital area?
Was the discharge accompanied by itching, burning, pain, or a sore in the genital area?
 When do symptoms occur in relation to the menstrual period?
When do symptoms occur in relation to the menstrual period?
 Does the discharge come and go, or is it always present?
Does the discharge come and go, or is it always present?
 Has an abnormal discharge occurred before, and if so, how did it respond to treatment?
Has an abnormal discharge occurred before, and if so, how did it respond to treatment?
 What kind of birth control has been and is being used?
What kind of birth control has been and is being used?
 Is pain felt during sexual intercourse?
Is pain felt during sexual intercourse?
 Has the woman had previous vaginal infections?
Has the woman had previous vaginal infections?
 Does the sex partner have symptoms?
Does the sex partner have symptoms?
The doctor also asks about the possibility of sexually transmitted diseases. This information helps the doctor determine whether other people require treatment.
A pelvic examination is done. While examining the vagina, the doctor takes a sample of the discharge (if present) with a cotton-tipped swab. The sample is examined under a microscope. With this information, the doctor can usually determine whether the cause is bacterial vaginosis, trichomonas vaginitis, or a yeast infection. Usually, the doctor also uses a swab to take a sample of fluid from the cervix. The sample is tested for sexually transmitted diseases.
To determine whether there are other infections in the pelvis, the doctor checks the uterus and ovaries by inserting the index and middle fingers of one gloved hand into the vagina and pressing on the outside of the lower abdomen with the other hand. If this maneuver causes substantial pain or if a fever is present, other infections may be present.
Prevention
Keeping the genital area clean and dry can help prevent infections. Washing every day with a mild, nonscented soap (such as glycerin soap) and rinsing and drying thoroughly are recommended. Wiping from front to back after urinating or defecating prevents bacteria from the anus from being moved to the vagina. Young girls should be taught good hygiene.
Wearing loose, absorbent clothing, such as cotton or cotton-lined underpants, allows air to circulate and helps keep the genital area dry. Douching frequently and using medicated douches are discouraged. Douching can remove normal, protective bacteria from the vagina and reduce the acidity of the vagina, making infections, including pelvic inflammatory disease, more likely. Practicing sex safe and limiting the number of sex partners are important preventive measures.
Treatment
Measures used for prevention, such as keeping the genital area clean and dry, also help treat infections. Strong or scented soaps and unnecessary topical products (such as feminine hygiene sprays) should be avoided. Occasionally placing ice packs on the genital area, applying cool compresses, or sitting in a cool sitz bath (with or without baking soda or Epsom salts) may reduce soreness and itching. A sitz bath is taken in the sitting position with the water covering only the genital and rectal area. Flushing the genital area with lukewarm water squeezed from a water bottle may also provide relief.
If these measures do not relieve symptoms, drugs may be needed. For itching, a corticosteroid cream (such as hydrocortisone) can sometimes be applied to the vulva but not in the vagina. Antihistamines taken by mouth help relieve itching. They also cause drowsiness and may be useful if symptoms interfere with sleep.
Specific treatment depends on the cause.
Bacterial Vaginosis
Bacterial vaginosis is a vaginal infection that occurs when the balance of bacteria in the vagina is altered.
 Women who have a sexually transmitted disease, who have several sex partners, or who use an intrauterine device are more likely to get bacterial vaginosis.
Women who have a sexually transmitted disease, who have several sex partners, or who use an intrauterine device are more likely to get bacterial vaginosis.
 The thin, gray or white discharge may be profuse, smell fishy, and be accompanied by itching.
The thin, gray or white discharge may be profuse, smell fishy, and be accompanied by itching.
 Antibiotics applied as gels or creams or taken by mouth are effective.
Antibiotics applied as gels or creams or taken by mouth are effective.
 Bacterial vaginosis commonly recurs.
Bacterial vaginosis commonly recurs.
Causes
Many bacteria normally reside in the vagina. One type, called lactobacilli, maintains the normal acidity of the vagina. By doing so, lactobacilli help keep the lining of the vagina healthy and prevent the growth of certain bacteria that cause infections. Bacterial vaginosis, the most common vaginal infection, results when the number of protective lactobacilli decreases and the number of other bacteria that are normally present (such as Gardnerella vaginalis and Peptostreptococcus species) increases. Why these changes occur and whether the disorder is sexually transmitted are unknown. What is known is that bacterial vaginosis is more common among women who have a sexually transmitted disease, who have several sex partners, or who use an intrauterine device (IUD).
Symptoms
The vaginal discharge may be gray or white, thin, itchy, and profuse. Usually, the discharge has a fishy odor. The odor may become stronger after sexual intercourse and during menstrual periods.
The infection can lead to serious complications, such as pelvic inflammatory disease and, for pregnant women, infection of the membranes around the fetus, preterm labor and delivery, and infections of the uterus after delivery or after an abortion.
 Did You Know…
Did You Know…
Some antibiotic creams used to treat vaginosis weaken latex condoms and diaphragms.
Treatment
Bacterial vaginosis is treated with an antibiotic (such as metronidazole or clindamycin) applied as a vaginal gel or cream. Metronidazole or tinidazole taken by mouth is also effective but may have body-wide side effects. Women who use clindamycin cream cannot rely on latex products (condoms or diaphragms) for birth control because the drug weakens latex.
Bacterial vaginosis usually resolves in a few days but commonly recurs. If it recurs often, antibiotics may have to be taken for a long time.
Trichomonas Vaginitis
Trichomonas vaginitis is a vaginal infection due to the protozoa Trichomonas vaginalis.
 The infection is usually sexually transmitted.
The infection is usually sexually transmitted.
 The green or yellow discharge may be profuse, smell fishy, and be accompanied by itching.
The green or yellow discharge may be profuse, smell fishy, and be accompanied by itching.
 Always using a condom can prevent this infection.
Always using a condom can prevent this infection.
 One dose of metronidazole or tinidazole taken by mouth cures most women.
One dose of metronidazole or tinidazole taken by mouth cures most women.
The protozoa Trichomonas vaginalis can cause symptoms soon after they enter the vagina, or they can remain in the vagina or on the cervix for weeks or months without causing any symptoms. The bladder may also be infected. In men, the protozoa usually remain for only for a few days or weeks and may cause no symptoms.
Causes
Trichomonas genital infections (trichomoniasis— see page 1273) are almost always sexually transmitted. Women can be infected through sexual contact with men or women. But men can be infected through sexual contact only with women, not with men. Many people who have this infection have other sexually transmitted diseases. Because the protozoa can remain in women for a long time without causing symptoms, determining when the infection was acquired and thus from whom can be difficult or impossible.
This infection may occur in children. If it does, the cause may be sexual abuse.
Symptoms
Women may have a green or yellow vaginal discharge that is sometimes frothy, profuse, or both. It may smell fishy. The genital area may itch, and the vagina may be red and tender. As a result, sexual intercourse may be painful. Urination may also be painful if the bladder becomes infected.
The infection can lead to pelvic inflammatory disease and, in pregnant women, preterm labor and delivery.
Prevention and Treatment
Always using a condom during sexual intercourse can help prevent this infection from being transmitted.
A single dose of metronidazole or tinidazole taken by mouth cures up to 95% of women. Sex partners should be treated at the same time. People should not drink alcohol for at least 72 hours after they take metronidazole or tinidazole. Drinking alcohol while taking either drug can cause nausea, vomiting, cramps, flushing, and headaches.
During sexual intercourse, condoms should be used until the infection resolves to prevent transmission of the infection.
Yeast Infection
 The vagina may be infected by a yeast called Candida, usually Candida albicans, resulting in a yeast infection called candidiasis. Being pregnant or overweight or having diabetes or a weakened immune system increases the risk of yeast infections.
The vagina may be infected by a yeast called Candida, usually Candida albicans, resulting in a yeast infection called candidiasis. Being pregnant or overweight or having diabetes or a weakened immune system increases the risk of yeast infections.
 The vagina and vulva itch, and women often have a thick, white, discharge resembling cottage cheese.
The vagina and vulva itch, and women often have a thick, white, discharge resembling cottage cheese.
 Antifungal drugs—creams, vaginal suppositories, tablets, or capsules—are effective.
Antifungal drugs—creams, vaginal suppositories, tablets, or capsules—are effective.
Causes
In women of reproductive age, yeast infections due to Candida albicans are particularly common. This yeast normally resides on the skin or in the intestine. From these areas, it can spread to the vagina. Yeast infections are not transmitted sexually. They are common among pregnant women, overweight women, and women who have diabetes. Yeast infections are more likely to occur just before menstrual periods. Yeast infections are also more likely to develop if the immune system is weakened— suppressed by drugs (such as corticosteroids or chemotherapy drugs) or impaired by a disorder (such as AIDS).
Antibiotics taken by mouth tend to kill the bacteria that normally reside in the vagina and that prevent yeast from growing. Thus, using antibiotics increases the risk of developing a yeast infection.
After menopause, yeast infections are uncommon except in women who take hormone therapy.
Symptoms
The vagina and vulva may itch or burn, particularly during intercourse. The genital area may become red and swollen. Women may have a white discharge, often thick and resembling cottage cheese. Symptoms may worsen the week before a menstrual period begins.
 Did You Know…
Did You Know…
Yeast infections are not sexually transmitted.
Taking antibiotics increases the risk of yeast infections.
Prevention
Women who are at high risk of a yeast infection may need to take an antifungal drug by mouth to help prevent yeast infections. Such women include those with the following:
 A weakened immune system
A weakened immune system
 Diabetes
Diabetes
 A need to take antibiotics for a long time
A need to take antibiotics for a long time
 Repeated yeast infections
Repeated yeast infections
Treatment
Yeast infections are treated with antifungal drugs. They may be applied as a cream to the affected area, inserted into the vagina as a suppository, or taken by mouth. Butoconazole, clotrimazole, miconazole, and tioconazole are available without a prescription. Oils in these creams and ointments weaken latex-based condoms (but not diaphragms), so women cannot rely on condoms for birth control.
 DRUGS USED TO TREAT VAGINAL YEAST INFECTIONS
DRUGS USED TO TREAT VAGINAL YEAST INFECTIONS
| DRUG | DOSAGE |
| Creams or gels, available without a prescription | |
| Butoconazole | Applied as a cream once a day for 3 days Also available as a sustained-release cream that is applied once |
| Clotrimazole | Applied as a cream once a day for 7 to 14 days Also available as a vaginal tablet inserted once a day for 7 days or for 3 days or inserted only once, depending on the dose (number of milligrams per tablet) |
| Miconazole | Applied as a cream once a day for 7 days Also available as a vaginal suppository inserted once a day for 7 days or for 3 days, depending on the dose |
| Tioconazole | Applied as an ointment only once |
| Drugs taken by mouth, available by prescription | |
| Fluconazole | One tablet taken only once |
| Itraconazole | Available as a capsule, once or twice a day for up to 6 months |
Antifungal drugs (such as fluconazole and itraconazole) taken by mouth require a prescription. A single dose of fluconazole is as effective as the creams and ointments. However, if infections recur often, women may need to take several doses.