CHAPTER 252
Normal Pregnancy
Pregnancy begins when an egg is fertilized by a sperm. For about 9 months, a pregnant woman’s body provides a protective, nourishing environment in which the fertilized egg can develop into a fetus. Pregnancy ends at delivery, when a baby is born.
Detecting and Dating a Pregnancy
If a menstrual period is a week or more late in a woman who usually has regular menstrual periods, she may be pregnant. Sometimes a woman may guess she is pregnant because she has typical symptoms. They include the following:
 Enlarged and tender breasts
Enlarged and tender breasts
 Nausea with occasional vomiting
Nausea with occasional vomiting
 A need to urinate frequently
A need to urinate frequently
 Unusual fatigue
Unusual fatigue
 Changes in appetite
Changes in appetite
When a menstrual period is late, a woman may use a home pregnancy test to determine whether she is pregnant. Home pregnancy tests detect human chorionic gonadotropin (hCG) in urine. Human chorionic gonadotropin is a hormone produced by the placenta. Results of home pregnancy tests are accurate about 97% of the time. If results are negative but the woman still suspects she is pregnant, she should repeat the home pregnancy test a few days later. The first test may have been done too early (before the next menstrual period is expected to start). If results are positive, the woman should contact her doctor, who may do another pregnancy test to confirm the results.
 Did You Know…
Did You Know…
Results of home pregnancy tests are accurate about 97% of the time.
Doctors test a sample of blood or urine from the woman to determine whether she is pregnant. These tests are more than 99% accurate. One of these tests, called an enzyme-linked immunosorbent assay (ELISA), can quickly and easily detect even a low level of human chorionic gonadotropin in urine. Some tests can detect the very low level that is present several days after fertilization (before a menstrual period is missed). Results may be available in about half an hour. During the first 60 days of a normal pregnancy with one fetus, the level of human chorionic gonadotropin in the blood approximately doubles about every 2 days. These levels can be measured during the pregnancy to determine whether the pregnancy is progressing normally.
When Is the Baby Due?
Pregnancies are conventionally dated in weeks, starting from the first day of the last menstrual period.
After pregnancy is confirmed, the woman’s doctor asks her when her last menstrual period was. The doctor calculates the approximate date of delivery by counting back 3 calendar months from the first day of the last menstrual period and adding 1 year and 7 days. For example, if the last menstrual period was January 1, the doctor counts back 3 months to October 1, then adds 1 year and 7 days. The calculated due date is October 8 the next year. Only 10% or fewer of pregnant women give birth on the calculated date, but 50% give birth within 1 week and almost 90% give birth within 2 weeks (before or after the date). Delivery between 3 weeks before and 2 weeks after the calculated date is considered normal.
Ovulation usually occurs about 2 weeks after a woman’s menstrual period starts, and fertilization usually occurs shortly after ovulation. Consequently, the embryo is about 2 weeks younger than the number of weeks traditionally assigned to the pregnancy. In other words, a woman who is 4 weeks pregnant is carrying a 2-week-old embryo. If a woman’s periods are irregular, the actual difference may be more or less than 2 weeks.
Pregnancy lasts an average of 266 days (38 weeks) from the date of fertilization (conception) or 280 days (40 weeks) from the first day of the last menstrual period if the woman has regular 28-day periods. Pregnancy is divided into three 3-month periods, based on the date of the last menstrual period:
 1st trimester: 0 to 12 weeks of pregnancy
1st trimester: 0 to 12 weeks of pregnancy
 2nd trimester: 13 to 24 weeks
2nd trimester: 13 to 24 weeks
 3rd trimester: 25 weeks to delivery
3rd trimester: 25 weeks to delivery
The most accurate way to determine when a baby is due is ultrasonography, particularly if it is done during the first 12 weeks.
From Egg to Embryo
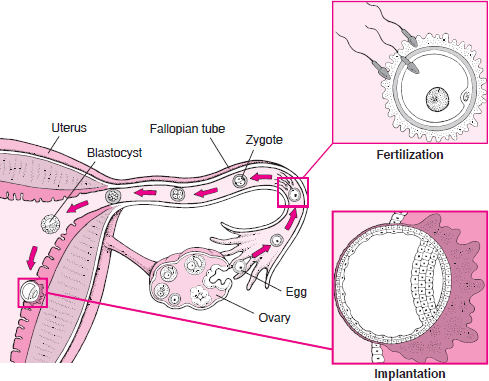
Once a month, an egg is released from an ovary into a fallopian tube. After sexual intercourse, sperm move from the vagina through the cervix and uterus to the fallopian tubes, where one sperm fertilizes the egg. The fertilized egg (zygote) divides repeatedly as it moves down the fallopian tube to the uterus. First, the zygote becomes a solid ball of cells. Then it becomes a hollow ball of cells called a blastocyst.
Inside the uterus, the blastocyst implants in the wall of the uterus, where it develops into an embryo attached to a placenta and surrounded by fluid-filled membranes.
Stages of Development
A baby goes through several stages of development, beginning as a fertilized egg. The egg develops into a blastocyst, an embryo, then a fetus.
Fertilization
During each normal menstrual cycle, one egg (ovum) is usually released from one of the ovaries, about 14 days before the next menstrual period. Release of the egg is called ovulation. The egg is swept into the funnel-shaped end of one of the fallopian tubes.
At ovulation, the mucus in the cervix becomes more fluid and more elastic, allowing sperm to enter the uterus rapidly. Within 5 minutes, sperm may move from the vagina, through the cervix into the uterus, and to the funnel-shaped end of a fallopian tube—the usual site of fertilization. The cells lining the fallopian tube facilitate fertilization.
If a sperm penetrates the egg, fertilization results. Tiny hairlike cilia lining the fallopian tube propel the fertilized egg (zygote) through the tube toward the uterus. The cells of the zygote divide repeatedly as the zygote moves down the fallopian tube. The zygote enters the uterus in 3 to 5 days. In the uterus, the cells continue to divide, becoming a hollow ball of cells called a blastocyst. If fertilization does not occur, the egg degenerates and passes through the uterus with the next menstrual period.
If more than one egg is released and fertilized, the pregnancy involves more than one fetus, usually two (twins). Such twins are fraternal. Identical twins result when one fertilized egg separates into two embryos after it has begun to divide.
Placenta and Embryo at 8 Weeks
At 8 weeks of pregnancy, the placenta and fetus have been developing for 6 weeks. The placenta forms tiny hairlike projections (villi) that extend into the wall of the uterus. Blood vessels from the embryo, which pass through the umbilical cord to the placenta, develop in the villi. A thin membrane separates the embryo’s blood in the villi from the mother’s blood that flows through the space surrounding the villi (intervillous space). This arrangement allows materials to be exchanged between the blood of the mother and that of the embryo. It also prevents the mother’s immune system from attacking the embryo because the mother’s antibodies are too large to pass through the membrane.
The embryo floats in fluid (amniotic fluid), which is contained in a sac (amniotic sac). The amniotic fluid provides a space in which the embryo can grow freely. The fluid also helps protect the embryo from injury. The amniotic sac is strong and resilient.

Development of the Blastocyst
Between 5 and 8 days after fertilization, the blastocyst attaches to the lining of the uterus, usually near the top. This process, called implantation, is completed by day 9 or 10.
The wall of the blastocyst is one cell thick except in one area, where it is three to four cells thick. The inner cells in the thickened area develop into the embryo, and the outer cells burrow into the wall of the uterus and develop into the placenta. The placenta produces several hormones that help maintain the pregnancy. For example, the placenta produces human chorionic gonadotropin, which prevents the ovaries from releasing eggs and stimulates the ovaries to produce estrogen and progesterone continuously. The placenta also carries oxygen and nutrients from mother to fetus and waste materials from fetus to mother.
Some of the cells from the placenta develop into an outer layer of membranes (chorion) surrounding the embryo. An inner layer of membranes (amnion) develops by about day 10 to 12, forming the amniotic sac. The amniotic sac fills with a clear liquid (amniotic fluid) and expands to envelop the developing embryo, which floats within it.
Development of the Embryo
The next stage in development is the embryo, which develops under the lining of the uterus on one side. This stage is characterized by the formation of most internal organs and external body structures. Organ formation begins about 3 weeks after fertilization, when the embryo elongates, first suggesting a human shape. Shortly thereafter, the area that will become the brain and spinal cord (neural tube) begins to develop. The heart and major blood vessels begin to develop by about day 16 or 17. The heart begins to pump fluid through blood vessels by day 20, and the first red blood cells appear the next day. Blood vessels continue to develop in the embryo and placenta.
Almost all organs are completely formed by about 8 weeks after fertilization (which equals 10 weeks of pregnancy). The exceptions are the brain and spinal cord, which continue to mature throughout pregnancy. Most malformations (birth defects) occur during the period when organs are forming. During this period, the embryo is most vulnerable to the effects of drugs, radiation, and viruses. Therefore, a pregnant woman should not be given any live-virus vaccinations or take any drugs during this period unless they are considered essential to protect her health (see page 1636).
Development of the Fetus and Placenta
At the end of the 8th week after fertilization (10 weeks of pregnancy), the embryo is considered a fetus. During this stage, the structures that have already formed grow and develop. The following are markers during pregnancy:
 By 12 weeks of pregnancy: The fetus fills the entire uterus.
By 12 weeks of pregnancy: The fetus fills the entire uterus.
 By about 14 weeks: The sex can be identified.
By about 14 weeks: The sex can be identified.
 By about 16 to 20 weeks: Typically, the pregnant woman can feel the fetus moving. Women who have been pregnant before typically feel movements about 2 weeks earlier than women who are pregnant for the first time.
By about 16 to 20 weeks: Typically, the pregnant woman can feel the fetus moving. Women who have been pregnant before typically feel movements about 2 weeks earlier than women who are pregnant for the first time.
 By about 24 weeks: The fetus has a chance of survival outside the uterus.
By about 24 weeks: The fetus has a chance of survival outside the uterus.
The lungs continue to mature until near the time of delivery. The brain accumulates new cells throughout pregnancy and the first year of life after birth.
As the placenta develops, it extends tiny hairlike projections (villi) into the wall of the uterus. The projections branch and rebranch in a complicated treelike arrangement. This arrangement greatly increases the area of contact between the wall of the uterus and the placenta, so that more nutrients and waste materials can be exchanged. The placenta is fully formed by 18 to 20 weeks but continues to grow throughout pregnancy. At delivery, it weighs about 1 pound.
Physical Changes
Pregnancy causes many changes in a woman’s body. Most of them disappear after delivery. These changes cause some symptoms, which are normal. However, certain disorders, such as gestational diabetes (see page 1630), develop during pregnancy, and some symptoms may indicate such a disorder.
Symptoms that should be immediately reported to a doctor if they occur during pregnancy include the following:
 Persistent or unusual headaches
Persistent or unusual headaches
 Persistent nausea and vomiting
Persistent nausea and vomiting
 Dizziness
Dizziness
 Disturbances of eyesight
Disturbances of eyesight
 Pain or cramps in the lower abdomen
Pain or cramps in the lower abdomen
 Contractions
Contractions
 Vaginal bleeding
Vaginal bleeding
 Leakage of amniotic fluid (described as “the water breaks”)
Leakage of amniotic fluid (described as “the water breaks”)
 Swelling of the hands or feet
Swelling of the hands or feet
 Decreased urine production
Decreased urine production
 Any illness or infection
Any illness or infection
 Tremor (shaking of the hands, feet, or both)
Tremor (shaking of the hands, feet, or both)
 Seizures
Seizures
 Rapid heart rate
Rapid heart rate
 Decreased movement of the fetus
Decreased movement of the fetus
General Health: Fatigue is common, especially in the first 12 weeks and again in late pregnancy. The woman may need to get more rest than usual.
Reproductive Tract: By 12 weeks of pregnancy, the enlarging uterus may cause the woman’s abdomen to protrude slightly. The uterus continues to enlarge throughout pregnancy. The enlarging uterus extends to the level of the navel by 20 weeks and to the lower edge of the rib cage by 36 weeks.
The amount of normal vaginal discharge, which is clear or whitish, commonly increases. This increase is usually normal. However, if the discharge has an unusual color or smell or is accompanied by vaginal itching and burning, a woman should see her doctor. Such symptoms may indicate a vaginal infection. Some vaginal infections, such as trichomoniasis (a protozoan infection—see page 1539) and candidiasis (a yeast infection—see page 1540), are common during pregnancy and can be treated.
Breasts: The breasts tend to enlarge because hormones (mainly estrogen) are preparing the breasts for milk production. The glands that produce milk gradually increase in number and become able to produce milk. The breasts may feel firm and tender. Wearing a bra that fits properly and provides support may help.
During the last weeks of pregnancy, the breasts may produce a thin, yellowish or milky discharge (colostrum). Colostrum is also produced during the first few days after delivery, before breast milk is produced. This fluid, which is rich in minerals and antibodies, is the breastfed baby’s first food.
Heart and Blood Flow: During pregnancy, the woman’s heart must work harder because as the fetus grows, the heart must pump more blood to the uterus. By the end of pregnancy, the uterus is receiving one fifth of the woman’s prepregnancy blood supply. During pregnancy, the amount of blood pumped by the heart (cardiac output) increases by 30 to 50%. As cardiac output increases, the heart rate at rest speeds up from a normal prepregnancy rate of about 70 beats per minute to 80 or 90 beats per minute. During exercise, cardiac output and heart rate increase more when a woman is pregnant than when she is not. During labor, cardiac output increases by an additional 10%. After delivery, cardiac output decreases rapidly at first, then more slowly. It returns to the prepregnancy level about 6 weeks after delivery.
Certain heart murmurs and irregularities in heart rhythm may appear because the heart is working harder. Sometimes a pregnant woman may feel these irregularities. Such changes are normal during pregnancy. However, other abnormal heart sounds and rhythms (for example, diastolic murmurs and tachyarrythmias), which occur more often in pregnant women, may require treatment.
Blood pressure usually decreases during the 2nd trimester but may return to a normal prepregnancy level in the 3rd trimester.
The volume of blood increases by 50% during pregnancy. The amount of fluid in the blood increases more than the number of red blood cells (which carry oxygen). Thus, even though there are more red blood cells, blood tests indicate mild anemia, which is normal. For reasons not clearly understood, the number of white blood cells (which fight infection) increases slightly during pregnancy and markedly during labor and the first few days after delivery.
The enlarging uterus interferes with the return of blood from the legs and the pelvic area to the heart. As a result, swelling (edema) is common, especially in the legs. Varicose veins commonly develop in the legs and in the area around the vaginal opening (vulva). They sometimes cause discomfort. Clothing that is loose around the waist and legs is more comfortable and does not restrict blood flow. Some measures not only ease the discomfort but may also reduce leg swelling and make varicose veins more likely to disappear after delivery:
 Wearing elastic support hose
Wearing elastic support hose
 Resting frequently with the legs elevated
Resting frequently with the legs elevated
 Lying on the left side
Lying on the left side
Urinary Tract: Like the heart, the kidneys work harder throughout pregnancy. They filter the increasing volume of blood. The volume of blood filtered by the kidneys reaches a maximum between 16 and 24 weeks and remains at the maximum until immediately before delivery. Then, pressure from the enlarging uterus may slightly decrease the blood supply to the kidneys.
Activity of the kidneys normally increases when a person lies down and decreases when a person stands. This difference is amplified during pregnancy—one reason a pregnant woman needs to urinate frequently while trying to sleep. Late in pregnancy, lying on the side, particularly the left side, increases kidney activity more than lying on the back. Lying on the left side relieves the pressure that the enlarged uterus puts on the main vein that carries blood from the legs. As a result, blood flow improves and kidney activity increases.
The uterus presses on the bladder, reducing its size so that it fills with urine more quickly than usual. This pressure also makes a pregnant woman need to urinate more often and more urgently.
Respiratory Tract: The high level of progesterone, a hormone produced continuously during pregnancy, signals the brain to lower the level of carbon dioxide in the blood. As a result, a pregnant woman breathes slightly faster and more deeply to exhale more carbon dioxide and keep the carbon dioxide level low. She may breathe deeper and faster also because the enlarging uterus limits how much the lungs can expand when she breathes in. The circumference of the woman’s chest enlarges slightly.
Virtually every pregnant woman becomes somewhat more out of breath when she exerts herself, especially toward the end of pregnancy. During exercise, the breathing rate increases more when a woman is pregnant than when she is not.
Because more blood is being pumped, the lining of the airways receives more blood and swells somewhat, narrowing the airways. As a result, the nose occasionally feels stuffy, and the eustachian tubes (which connect the middle ear and back of the nose) may become blocked. These effects can slightly change the tone and quality of the woman’s voice.
Digestive Tract: Nausea and vomiting, particularly in the mornings (morning sickness), are common. They may be caused by the high levels of estrogen and human chorionic gonadotropin, two hormones that help maintain the pregnancy. Nausea and vomiting may be relieved by changing the diet or patterns of eating. For example, drinking and eating small portions frequently, eating before getting hungry, and eating bland foods (such as bouillon, consommé, rice, and pasta) may help. Eating plain soda crackers and sipping a carbonated drink may relieve nausea. Keeping crackers by the bed and eating one or two before getting up may relieve morning sickness. No drugs specifically designed to treat morning sickness are currently available. If nausea and vomiting are so intense or persistent that dehydration, weight loss, or other problems develop, a woman may need to be treated with drugs that relieve nausea (antiemetic drugs) or to be hospitalized temporarily and given fluids intravenously (see page 1645).
Heartburn and belching are common, possibly because food remains in the stomach longer and because the ringlike muscle (sphincter) at the lower end of the esophagus tends to relax, allowing the stomach’s contents to flow backward into the esophagus. Several measures can help relieve heartburn:
 Eating smaller meals
Eating smaller meals
 Not bending or lying flat for several hours after eating
Not bending or lying flat for several hours after eating
 Avoiding caffeine, tobacco, alcohol, and aspirin and related drugs (salicylates)
Avoiding caffeine, tobacco, alcohol, and aspirin and related drugs (salicylates)
 Taking liquid antacids, but not antacids that contain sodium bicarbonate because they contain so much salt (sodium)
Taking liquid antacids, but not antacids that contain sodium bicarbonate because they contain so much salt (sodium)
Heartburn during the night can be relieved by the following:
 Not eating for several hours before going to bed
Not eating for several hours before going to bed
 Raising the head of the bed or using pillows to raise the head and shoulders
Raising the head of the bed or using pillows to raise the head and shoulders
The stomach produces less acid during pregnancy. Consequently, stomach ulcers rarely develop during pregnancy, and those that already exist often start to heal.
As pregnancy progresses, pressure from the enlarging uterus on the rectum and the lower part of the intestine may cause constipation. Constipation may be worsened because the high level of progesterone during pregnancy slows the automatic waves of muscular contractions in the intestine, which normally move food along. Eating a high-fiber diet, drinking plenty of fluids, and exercising regularly can help prevent constipation.
Hemorrhoids, a common problem, may result from pressure of the enlarging uterus or from constipation. Stool softeners, an anesthetic gel, or warm soaks can be used if hemorrhoids hurt.
Pica, a craving for strange foods or nonfoods (such as starch or clay), may develop.
Occasionally, pregnant women, usually those who also have morning sickness, have excess saliva. This symptom may be distressing but is harmless.
Skin: Mask of pregnancy (melasma) is a blotchy, brownish pigment that may appear on the skin of the forehead and cheeks. The skin surrounding the nipples (areolae) may also darken. A dark line commonly appears down the middle of the abdomen. These changes may occur because the placenta produces a hormone that stimulates melanocytes, the cells that make a dark brown skin pigment (melanin).
Pink stretch marks sometimes appear on the abdomen. This change probably results from rapid growth of the uterus and an increase in levels of adrenal hormones.
Small blood vessels may form a red spiderlike pattern on the skin, usually above the waist. These formations are called spider angiomas. Thin-walled, dilated capillaries may become visible, especially in the lower legs.
Hormones: Pregnancy affects virtually all hormones in the body, mostly because of the effects of hormones produced by the placenta. For example, the placenta produces a hormone that stimulates the woman’s thyroid gland to become more active and produce larger amounts of thyroid hormones. When the thyroid gland becomes more active, the heart may beat faster, causing the woman to become aware of her heartbeat (have palpitations). Perspiration may increase, mood swings may occur, and the thyroid gland may enlarge. However, the disorder hyperthyroidism, in which the thyroid gland malfunctions and is overactive, develops in fewer than 0.1% of pregnancies.
Levels of estrogen and progesterone increase early during pregnancy because human chorionic gonadotropin, the main hormone the placenta produces, stimulates the ovaries to continuously produce them. After 9 to 10 weeks of pregnancy, the placenta itself produces large amounts of estrogen and progesterone. Estrogen and progesterone help maintain the pregnancy.
Skin Rashes During Pregnancy
Two intensely itchy rashes occur only during pregnancy.
Pruritic urticarial papules and plaques of pregnancy (urticaria of pregnancy): This rash is common. The cause is unknown.
Red, irregularly shaped, flat or slightly raised patches appear on the abdomen. The patches sometimes have tiny fluid-filled blisters in the center. Often, the skin around them is pale. The rash spreads to the thighs, buttocks, and occasionally the arms. Hundreds of itchy patches may develop. Itching is bothersome enough to keep the woman awake at night.
Typically, the rash appears during the last 2 to 3 weeks of pregnancy and occasionally during the last few days. However, it may occur at any time after the 24th week. Usually, the rash clears up promptly after delivery and does not recur during subsequent pregnancies.
Doctors may have difficulty making a definite diagnosis.
Herpes gestationis: The cause is thought to be abnormal antibodies that attack the body’s own tissues— an autoimmune reaction.
The rash can begin as flat or raised red spots that often form on the abdomen first. Then blisters develop and the rash spreads. The blisters are small or large, irregularly shaped, and fluid-filled.
The rash can appear any time after the 12th week of pregnancy or immediately after delivery. Typically, the rash worsens soon after delivery and disappears within a few weeks or months. It often reappears during subsequent pregnancies and sometimes reappears if the woman later takes oral contraceptives. The baby may be born with a similar rash, which usually disappears without treatment within a few weeks.
This rash is diagnosed by removing a tiny piece of affected skin and testing it for abnormal antibodies.
Treatment: For either rash, applying a corticosteroid cream (such as triamcinolone acetonide) directly to the skin often helps. For more widespread rashes, a corticosteroid (such as prednisone) is given by mouth.
The placenta stimulates the adrenal glands to produce more aldosterone and cortisol (which help regulate how much fluid the kidneys excrete). As a result, more fluids are retained.
During pregnancy, changes in hormone levels affect how the body handles sugar. Early in pregnancy, the sugar (glucose) level in the blood may decrease slightly. But in the last half of pregnancy, the level may increase. More insulin (which controls the sugar level in the blood) is needed and is produced by the pancreas. Consequently, diabetes, if already present, may worsen during pregnancy. Diabetes can also begin during pregnancy. This disorder is called gestational diabetes (see page 1630).
Joints and Muscles: The joints and ligaments (fibrous cords and cartilage that connect bones) in the woman’s pelvis loosen and become more flexible. This change helps make room for the enlarging uterus and prepare the woman for delivery of the baby. As a result, the woman’s posture changes somewhat.
Backache in varying degrees is common because the spine curves more to balance the weight of the enlarging uterus. Avoiding heavy lifting, bending the knees (not the waist) to pick things up, and maintaining good posture can help. Wearing flat shoes with good support or a lightweight maternity girdle may reduce strain on the back.
Medical Care
Ideally, a couple who is thinking of having a baby should see a doctor or other health care practitioner to discuss whether pregnancy is advisable. Usually, pregnancy is very safe. However, some disorders can become severe during pregnancy. Also, for some couples, the risk of having a baby with a hereditary disorder is increased.
If the couple decides to try to have a baby, they and the doctor discuss ways to make the pregnancy as healthy as possible. The woman should ask the doctor about factors that could impair her health or the health of the developing fetus. Factors or situations to avoid include the following:
Stages of Pregnancy
Although pregnancy involves a continuous process, it is divided into three 3-month periods called trimesters (weeks 0 to 12, 13 to 24, and 25 to delivery).
| EVENTS | WEEKS OF PREGNANCY |
| 1st Trimester | |
| The woman’s last period before fertilization occurs. | 0 |
| Fertilization occurs. The fertilized egg (zygote) begins to develop into a hollow ball of cells called the blastocyst. |
2 |
| The blastocyst implants in the wall of uterus. The amniotic sac begins to form. |
3 |
| The area that will become the brain and spinal cord (neural tube) begins to develop. | 5 |
| The heart and major blood vessels are developing. The beating heart can be seen during ultrasonography. | 6 |
| The beginnings of arms and legs appear. | 7 |
| Bones and muscles form. The face and neck develop. Brain waves can be detected. The skeleton is formed. Fingers and toes are fully defined. |
9 |
| The kidneys begin to function. Almost all organs are completely formed. The fetus can move and respond to touch (when prodded through the woman’s abdomen). The woman has gained some weight, and her abdomen may be slightly enlarged. |
10 |
| 2nd Trimester | |
| The fetus’s sex can be identified. The fetus can hear. |
14 |
| The fetus’s fingers can grasp. The fetus moves more vigorously, so that the mother can feel it. The fetus’s body begins to fill out as fat is deposited beneath the skin. Hair appears on the head and skin. Eyebrows and eyelashes are present. |
16 |
| The placenta is fully formed. | 20 |
| The fetus has a chance of survival outside the uterus. The woman begins to gain weight more rapidly. |
24 |
| 3rd Trimester | |
| The fetus is active, changing positions often. The lungs continue to mature. The fetus’s head moves into position for delivery. On average, the fetus is about 20 inches long and weighs about 7 pounds. The woman’s enlarged abdomen causes the navel to bulge. |
25 |
| Delivery | 37-42 |


 Using tobacco or alcohol
Using tobacco or alcohol
 Being exposed to secondhand smoke, which may harm the fetus
Being exposed to secondhand smoke, which may harm the fetus
 Having contact with cat litter or cat feces unless the cats are strictly confined to the home and are not exposed to other cats (such contact can transmit toxoplasmosis, an infection by a protozoan that can damage the fetus’s brain)
Having contact with cat litter or cat feces unless the cats are strictly confined to the home and are not exposed to other cats (such contact can transmit toxoplasmosis, an infection by a protozoan that can damage the fetus’s brain)
 Having contact with people who have rubella (German measles) and some other infections, which can cause birth defects
Having contact with people who have rubella (German measles) and some other infections, which can cause birth defects
 Having contact with people who have chickenpox or shingles unless the woman has had a test that shows she has had chickenpox and is immune to it
Having contact with people who have chickenpox or shingles unless the woman has had a test that shows she has had chickenpox and is immune to it
Chickenpox and shingles are caused by herpes viruses. During delivery, these viruses can be spread to the fetus and cause severe illness. The virus can also cause pneumonia, which is occasionally severe, in the woman.
Knowing about and dealing with such factors before pregnancy may help reduce the risk of problems during pregnancy (see page 1626). In addition, the woman can discuss her diet and her social, emotional, and medical concerns with the doctor.
When a woman sees a doctor or another health care practitioner before she is pregnant, she can be given any needed vaccines, such as the rubella vaccine. She can also start taking prenatal multivitamins containing folate (folic acid). If needed, genetic screening can be done to determine whether the woman and her partner are at increased risk of having a baby with a hereditary genetic disorder (see page 1609).
First Examination: After pregnancy is confirmed, the woman should have a physical examination, preferably between 6 and 8 weeks of pregnancy. At this time, the length of the pregnancy can be estimated and the date of delivery can be predicted as accurately as possible.
The first physical examination during pregnancy is very thorough. It includes the following:
 Measurement of weight, height, and blood pressure
Measurement of weight, height, and blood pressure
 Pelvic examination: During this examination, the doctor notes the size and position of the uterus.
Pelvic examination: During this examination, the doctor notes the size and position of the uterus.
 Blood tests: A sample of blood is taken and analyzed. Analysis includes a complete blood cell count, tests for infectious diseases (such as syphilis, hepatitis, and human immunodeficiency virus [HIV]), and tests for evidence of immunity to rubella. Blood type, including Rh factor status (positive or negative), is determined.
Blood tests: A sample of blood is taken and analyzed. Analysis includes a complete blood cell count, tests for infectious diseases (such as syphilis, hepatitis, and human immunodeficiency virus [HIV]), and tests for evidence of immunity to rubella. Blood type, including Rh factor status (positive or negative), is determined.
 Urine tests: A sample of urine is taken, cultured, and analyzed.
Urine tests: A sample of urine is taken, cultured, and analyzed.
 Papanicolaou (Pap) test or a variation of it: Samples of tissue from the cervix are taken to check for cancer of the cervix.
Papanicolaou (Pap) test or a variation of it: Samples of tissue from the cervix are taken to check for cancer of the cervix.
 Test for sexually transmitted diseases: Immediately after the Pap test, another sample of tissue from the cervix is taken to test for sexually transmitted diseases, such as gonorrhea and chlamydial infection.
Test for sexually transmitted diseases: Immediately after the Pap test, another sample of tissue from the cervix is taken to test for sexually transmitted diseases, such as gonorrhea and chlamydial infection.
Other tests may be done, depending on the woman’s situation. If the woman has Rh-negative blood, it is tested for antibodies to the Rh factor (see page 1650). Having Rh antibodies can cause severe problems (even death) for a fetus that has Rh-positive blood. If antibodies in a pregnant woman’s blood are detected early, the doctor can take measures to protect the fetus.
 Did You Know…
Did You Know…
Things to avoid during pregnancy include tobacco, second-hand smoke, drugs, alcohol, cats, and contact with people who may have chickenpox or shingles.
During the flu season, all pregnant women should get a flu shot.
Women of African descent are tested for sickle cell trait or disease if they have not been tested previously. Skin tests for tuberculosis are advisable for all women. X-rays are not routinely taken during pregnancy, but they can be taken safely when necessary. If an x-ray is required, the fetus is shielded by placing a lead-filled garment over the woman’s lower abdomen to cover the uterus.
Follow-up Examinations: After the first examination, a pregnant woman should see her doctor every 4 weeks until 28 weeks of pregnancy, then every 2 weeks until 36 weeks, then once a week until delivery. At each examination, the woman’s weight and blood pressure are usually recorded, and the size of the uterus is noted to determine whether the fetus is growing normally. The heartbeat of the fetus is also checked to determine whether it is normal. The woman’s ankles are examined for swelling.
At each visit, urine is tested for sugar. Sugar in the urine may indicate diabetes. If the urine contains sugar, a blood test to check for diabetes is done as soon as possible. This test is also done as soon as possible and preferably before 20 weeks for women who
 Are severely overweight (> 250 pounds)
Are severely overweight (> 250 pounds)
 Have had a history of gestational diabetes
Have had a history of gestational diabetes
 Have polycystic ovary syndrome with insulin resistance (see page 1528)
Have polycystic ovary syndrome with insulin resistance (see page 1528)
If the initial test is negative, these women should be retested at 26 to 30 weeks. All other women should have a screening blood test for diabetes at around 28 weeks of pregnancy.
At each visit, the urine is also tested for protein. Protein in urine may indicate preeclampsia (a type of high blood pressure that develops during pregnancy (see page 1649).
If women have a high risk of conceiving a baby with a genetic disorder, prenatal diagnostic testing can be done (see page 1611).
Most doctors believe that ultrasonography (see page 2044), the safest imaging procedure, should be done at least once during a pregnancy to make sure the fetus is normally formed and to verify the expected date of delivery. For the procedure, a device that produces sound waves (transducer) is placed on the woman’s abdomen. The sound waves are processed to form an image that is displayed on a monitor. Sometimes, particularly during early pregnancy, the doctor uses an ultrasound device that can be inserted in the vagina. Ultrasonography produces high-quality images, including live-action images that show the fetus in motion. These images provide the doctor with useful information and can reassure a pregnant woman.
Ultrasonography can show the fetus’s beating heart at 6 weeks of pregnancy and thus can confirm that the fetus is alive. Doctors may periodically use an ultrasound device to listen to the fetus’s heartbeat. Or they may use a stethoscope designed to listen to a fetus’s heartbeat (fetoscope). The fetoscope can detect the heartbeat as early as 18 to 20 weeks of pregnancy.
Ultrasonography can also be used to do the following:
 Identify the sex of the fetus at 14 weeks of pregnancy
Identify the sex of the fetus at 14 weeks of pregnancy
 See whether a woman is carrying more than one fetus
See whether a woman is carrying more than one fetus
 Identify abnormalities, such as a mislocated placenta (placenta previa) or an abnormal position of the fetus
Identify abnormalities, such as a mislocated placenta (placenta previa) or an abnormal position of the fetus
 Date the pregnancy and thus help determine whether the pregnancy is progressing normally
Date the pregnancy and thus help determine whether the pregnancy is progressing normally
 Identify birth defects (sometimes)
Identify birth defects (sometimes)
 Guide the placement of instruments during certain procedures, such as prenatal diagnostic testing
Guide the placement of instruments during certain procedures, such as prenatal diagnostic testing
Toward the end of pregnancy, ultrasonography may be used to identify premature rupture of the fluid-filled membranes containing the fetus. Ultrasonography can provide information that helps doctors decide whether a cesarean delivery is needed.
Experts recommend that all pregnant women be vaccinated against the influenza virus during the influenza (flu) season.
Self-Care
There is much a pregnant woman can do to take care of herself during pregnancy. If she has any questions about diet, the use of drugs or nutritional supplements, physical activity, and sexual intercourse during pregnancy, she can talk with her doctor.
Diet and Weight: During pregnancy, the woman’s diet should be adequate and nutritious. If she does not consume enough nutrients for herself and the fetus, nutrients first go to nourish the fetus. However, adding about 250 calories to the daily diet is usually enough to provide nourishment for both. Most of the extra calories should be protein. The diet should be well balanced and include fresh fruits, grains, and vegetables. Cereals that are high in fiber and low in sugar are a good choice.
In the United States, most women get enough salt in their diet, without adding salt to their food at the table. Commercially prepared foods often contain excessive amounts of salt and should be consumed sparingly.
Dieting to lose weight during pregnancy is not recommended, even for obese women, because some weight gain is essential for the fetus to develop normally. Dieting reduces the supply of nutrients to the fetus.
An average-size woman should gain about 25 to 30 pounds during pregnancy. Gaining more than 30 to 35 pounds puts fat on the woman and the fetus. Because controlling weight gain is more difficult later in pregnancy, a woman should try to avoid gaining too much weight during the first months. On the other hand, not gaining weight can hinder the growth and development of the fetus. A woman should try to gain between 2 and 3 pounds each month during early pregnancy.
Sometimes a pregnant woman gains weight because she is retaining fluid. Fluid may be retained because when she lies flat, the enlarging uterus interferes with blood flow from the legs back to the heart. Lying on one side, preferably the left side, for 30 to 45 minutes 2 or 3 times a day may relieve this problem. Wearing elastic support stockings may also help.
Drugs and Dietary Supplements: Generally, avoiding drugs during pregnancy is best. However, drugs must sometimes be used (see page 1636). A pregnant woman should check with her doctor before taking any drug—including nonprescription (over-the-counter) drugs, such as aspirin, or medicinal herbs—particularly during the first 3 months.
Pregnancy doubles the amount of iron needed. Most pregnant women need an iron supplement because the average woman does not absorb enough iron from food to meet the requirements of pregnancy. If a woman has anemia or develops anemia during pregnancy, she may need to take a larger dose of iron than other pregnant women. Iron supplements may cause mild stomach upset and constipation.
All pregnant women should take a folate (folic acid) supplement (usually included in prenatal vitamins) daily. Ideally, the folate supplement is begun before pregnancy. A deficiency of folate increases the risk of having a baby with a birth defect of the brain or spinal cord, such as spina bifida. Women who have had a baby with spina bifida should start taking a high dose of folate before they become pregnant. For some other women who may have a folate deficiency, the amount of folate in a standard prenatal vitamin is sufficient, even if the risk is somewhat increased. For example, women who are exposed to excessive ultraviolet (UV) light, particularly fair-skinned women, may have decreased folate levels. Also, women who have taken oral contraceptives within several months before conception are more likely to develop a folate deficiency, but there is no proof that they are more likely to have a baby with spina bifida.
 Did You Know…
Did You Know…
Usually, exercise and sexual intercourse do not jeopardize a pregnancy.
When traveling, pregnant women should always wear seat belts.
If the diet is adequate, other vitamin supplements may not be needed, although most doctors recommend that pregnant women take a prenatal multivitamin containing iron and folate daily.
Physical Activity: Many pregnant women are concerned about moderating their activities. However, most women can continue their usual activities and exercises throughout pregnancy. Mildly strenuous sports, such as swimming and brisk walking, are good choices. Vigorous activities, such as running and horseback riding, are also possible if done cautiously, to avoid injury, particularly to the abdomen. Contact sports should be avoided.
Sexual Intercourse: Sexual desire may increase or decrease during pregnancy. Sexual intercourse is safe throughout pregnancy unless a woman has vaginal bleeding, pain, leakage of amniotic fluid, or uterine contractions. In such cases, sexual intercourse should be avoided.
Preparing for Breastfeeding: Women who are planning to breastfeed do not need to do anything to prepare their nipples for breastfeeding during pregnancy (see page 1679). Expressing fluids from the breast manually before delivery may lead to an infection of the breast (mastitis) or even early labor. The body prepares the areola and nipple for breastfeeding by secreting a lubricant to protect the surface. This lubricant should not be rubbed off. Observing and talking with women who have breastfed successfully may be instructive and encouraging.
Travel During Pregnancy: The safest time to travel during pregnancy is between 14 and 28 weeks. Travel time should not exceed 6 hours a day. Women can obtain useful tips and information about travel from their doctor, so discussing their travel plans with the doctor is a good idea.
When traveling in a car, airplane, or other vehicle, pregnant women should always wear a seat belt. Placing the lap belt across the hips and under the expanding abdomen and placing the shoulder belt between the breasts can help make wearing seat belts more comfortable. The belts should be snug but not uncomfortably tight.
During any kind of travel, pregnant women should stretch and straighten their legs and ankles periodically.
Travel on airplanes is safe until about 36 weeks. The primary reason for this restriction at 36 weeks is the risk of labor and delivery in an unfamiliar environment.