In the presence of danger, pain, extreme distress, or injury, a number of profound physiological changes ready the body for survival. To understand the core dilemmas of a child experiencing trauma, it is useful to have knowledge of the body’s communication and memory systems and of its survival and adaptive mechanisms. For readers who may not be familiar with the basic ways the body organizes, regulates, and remembers its experiences, Section I of this chapter provides a summary of the structure and function of the nervous and endocrine systems and of the memory system. Much of what we present is a simplification of complex functions, but it nevertheless offers an overall template from which to orient our understanding of the physiological organization upon which psychological experience is built. Section II presents an overview of the responses that occur in the face of threat, and Section III discusses the impact of trauma on early life.
There is no doubt that scientific expansion of our knowledge about the brain and body has opened new options for developing more effective clinical treatments. However, it is important to keep a balanced view that takes into account what we know against what we do not yet know. The body is extremely complex and research, as impressive as it is, is limited by available technology. For example, much is known about certain areas of the brain, not necessarily because they are more important but because they are more readily accessible given current research technology.
Even as NARM builds upon physiological and psychological knowledge already gained, it also makes room, through mindfulness, for the body’s innate intelligence and its surprising adaptive creativity, which can seemingly miraculously take us beyond what we can consciously and intellectually understand. It is an important NARM value to remain respectful of the body’s wisdom, knowing that it goes far beyond what is currently known. It is with this caution in mind that we look into the physiological basis of the foundations of self.
The billions of cells in our human body communicate with each other primarily through two systems: the nervous system and the endocrine system. These two systems are closely allied and cooperate to monitor and regulate the body’s many functions. For example, in digestion the nervous system manages the muscular aspects of the process while the endocrine system directly organizes the absorption of nutrients, establishes the secretion and assimilation activities of the cells, and influences the exchanges that take place between the various tissues. The nervous and endocrine systems are the great communicators and regulators of the body and are responsible for maintaining the body’s physiological stability or homeostasis.
There is a growing medical realization that most illnesses and diseases are the result of dysregulation and disorganization within the neuroendocrine communication network. NARM’s primary principles of tracking connection/disconnection, organization/disorganization, and somatic mindfulness work directly with the dysregulated physiology and the disorganizing repercussions a dysregulated nervous system has on the emotional and psychological self.
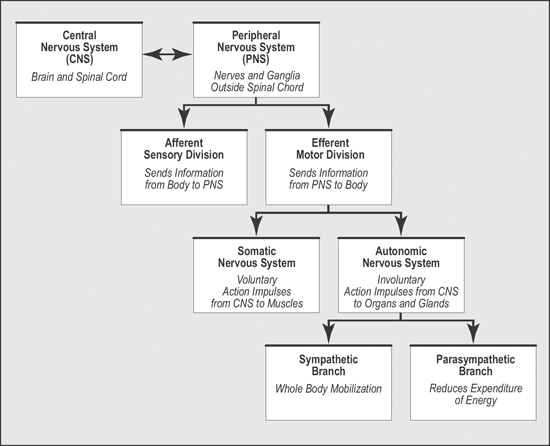
Although there is actually only one nervous system, it can be separated into several divisions based on structure and function. Structurally, the nervous system is seen as having two divisions: the central and peripheral nervous systems. Functionally, it has three roles: to detect information received by our senses and internal organs, to organize that information, and to activate appropriate responses.
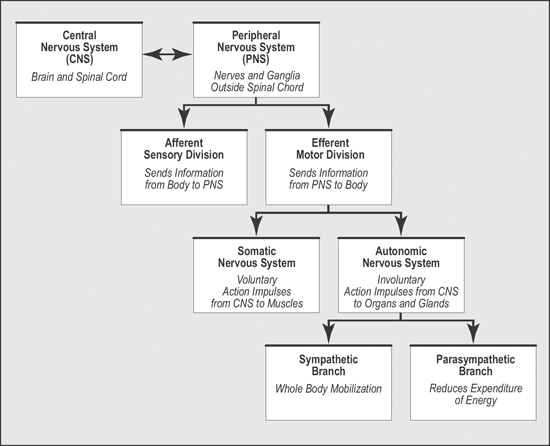
FIGURE 7.1: Schema of the Nervous System
In this section, we first present a short overview of the divisions of the nervous system in order to orient the reader to its complex organization. We then specifically focus on the role of the sympathetic and parasympathetic branches of the autonomic nervous system because of the important role they play in maintaining a regulated physiology and because of the devastating dysregulation that trauma has on their balanced interaction.
The central nervous system consists of the brain and spinal cord. Among its many functions, the central nervous system regulates our body’s responses to the intuitive gut feelings we have in relation to other human beings. It is interesting to note that only recently has the role of the central nervous system as mediator of our capacity to empathically perceive the emotional states of other human beings become clear.
The peripheral nervous system consists of the nerves and ganglia outside the brain and spinal cord. Its main function is to connect the limbs and organs to the brain and spinal cord in the central nervous system. Functionally, the peripheral nervous system comprises two divisions:
• The afferent sensory division is responsible for the detection of information in our external environment and internal organs. This division relays the detected information to the central nervous system. The brain then integrates and organizes that information in preparation for appropriate action.
• The efferent motor division sends motor information from the central nervous system to various areas of the body so that we can take action. This motor division has two subdivisions:
• The somatic nervous system, whose voluntary motor functions are under conscious control. This system relays impulses for action from the central nervous system to the skeletal muscles and skin.
• The autonomic nervous system, whose involuntary motor functions cannot be consciously controlled. It oversees largely unconscious bodily functions, such as heart rate and respiration, and it mediates, through the vagus system, our capacity for social engagement, trust, and intimacy. This system also relays impulses from the central nervous system to the smooth muscles, cardiac muscle, and glands. Its two divisions, the sympathetic and parasympathetic branches, respond extremely rapidly to the signals they receive from the central nervous system.
Is it good or bad? Is it familiar or unfamiliar? Is it safe or dangerous? The autonomic nervous system evaluates events and people for their survival significance and prepares the body to take appropriate action. Under ideal conditions, the sympathetic branch of the autonomic nervous system initiates whole-body mobilization to get us ready for action. When individuals are under stress, the sympathetic branch of the nervous system prepares them to manage stressful or threatening situations: it initiates the reactions required for aggressive or defensive behavior known as fight-flight responses. It rapidly mobilizes the physiological resources needed to move into action, stimulating involuntary muscular activity and increasing glandular secretions. It elevates blood sugar to increase energy and quickens the heart rate to increase blood supply to the muscles. It dilates the bronchii to increase the breathing rate; dilates the pupils; increases sweating; speeds up mental activity; all actions that ready us to respond to threat.
The parasympathetic branch of the autonomic nervous system modulates sympathetic arousal by reducing the body’s expenditure of energy in order to conserve it. It help us rest and regenerate by maintaining the various organs at levels of activity that are most efficient to preserve the body’s internal homeostasis. For example, it slows down the heart rate; lowers blood pressure; allows for breathing to return to normal; increases digestion, bowel, and bladder activities; and re-establishes immune functions.
With few exceptions, the organs of the body are innervated by both the sympathetic and parasympathetic branches of the autonomic nervous system. When the sympathetic and parasympathetic branches move in a flowing, reciprocal manner, the body’s internal state is said to be regulated. In the relaxed state of autonomic balance, we experience ourselves as steady, strong, present, and at ease. Table 7.1 summarizes the functions of the sympathetic and parasympathetic branches of the autonomic nervous system.
There is more complexity to the autonomic nervous system than simply the paired opposition of its sympathetic and parasympathetic branches. The Polyvagal Theory, developed by Stephen Porges, PhD, expands our understanding of the autonomic nervous system by showing how the evolutionary, layered development of our brain and nervous system contributes to our capacity to switch between defensive strategies and a socially engaged sense of safety and connection.
| AREA OF THE BODY | SYMPATHETIC STIMULATION | PARASYMPATHETIC STIMULATION |
| Heart | Increased rate and force of contraction | Decreased rate |
| Smooth Muscles Arrector pili muscles Digestive tract Lungs Urinary bladder Eye: Iris Ciliary muscle |
Contraction Decreased peristalsis Dilation of bronchioles Relaxation Dilation of pupil No innervation |
No innervation Increased peristalsis Constriction of bronchioles Contraction Contraction of pupil Contraction to assist near vision |
| Blood Vessels of Salivary glands Skin Skeletal muscles Viscera External genitalia |
Constriction Constriction Dilation Constriction Constriction |
Dilation No innervation No innervation Dilation Dilation |
| Glands Salivary Digestive tract Pancreas Adrenal medulla Sweat glands Liver |
Viscous secretion / low enzyme content Inhibition Inhibition Secretion Secretion Increased release of glucose |
Thin secretion / high enzyme content Stimulation of secretion Stimulation of secretion No innervation No innervation No innervation |
TABLE 7.1: Sympathetically and Parasympathetically Driven Changes that Occur in the Body in Response to Stress or Threat
To grasp the evolutionary dimension of the Polyvagal Theory, as well as the importance of working therapeutically bottom-up and top-down, it is useful to remember that the human brain evolved from the bottom up, with the higher centers developing as elaborations of lower, more ancient parts. Newer brain structures that perform more adaptive functions were built on older structures, keeping those areas that had proved useful and slowly adding complexity and sophistication. The human brain and nervous system thus retain features of our reptile, mammal, and primate ancestors. In spite of its layered evolutionary architecture, the healthy brain and nervous system largely operate as an integrated whole.
• First came the brainstem, which surrounds the top of the spinal cord and is preprogrammed to regulate bodily processes and vital functions such as the sleep-wake cycle, heartbeat, respiration, and body temperature. The capacity for self-regulation and self-soothing starts at the level of the brainstem, in the dorsal branch of the vagal system.
• Next, our reptilian ancestors developed the basal ganglia, responsible for behavioral-motor routines learned from repeated behaviors, which then become automatic. This portion of the brain makes it possible for us to ride a bicycle or play the piano.
• With the emergence of mammals came a ringlike section surrounding the brainstem called the limbic (Latin for ring) system. Also called the emotional brain, it is from the limbic system that emotion and the mammalian behaviors of nursing, parental care, and play evolved. The limbic system added powerful tools to upgrade the organism’s capacity to adapt to the changing demands of the environment: learning, memory, and the beginning of socialization. In the simplest terms, the emotional limbic system uses pleasurable and unpleasurable stimuli to organize and guide how we respond to the events of our lives. The limbic system impacts the encoding of memory in that personally relevant and emotionally arousing events are more likely to be remembered.
• Finally, the cortex, considered the most highly evolved part of the brain, brings in rational thought and the ability to strategize and plan long term in order to fine-tune the subcortical functions of the limbic system and brainstem. With its capacity to plan for the future, direct attention to a task, regulate affect, and control voluntary movement, the executive prefrontal cortex is the most developed area of the cortex. From a cortical perspective, putting our emotional and sensory experiences into words—creating a narrative for the nonverbal subcortical signals as they arise, bottom-up, into awareness—teaches the cortex new ways to relate and respond to sensations and emotions.
A useful metaphor to illustrate the hierarchy of the brain and nervous system is the organization of a company. In the highly organized “company” that is our body, the working sensory neurons gather information and bring it to the managers in the brainstem and limbic systems, who sort it, store it, and send it on to the appropriate executives in the cortical offices. The executives interpret the incoming information and formulate a plan of action. Once the plan of action is made, the executives send it back to management, who discusses how the plan will be carried out and assigns specific tasks to the working action neurons. This is perhaps an oversimplification, but it serves to illustrate the importance of using both a bottom-up and top-down perspective when working to repair a breakdown in neural communication.
In his groundbreaking work on the autonomic nervous system, Porges emphasizes the phylogenetic emergence of two vagal systems: (1) an older circuit originating in the brainstem involved in the defensive strategies of immobilization such as fainting and dissociation and (2) a newer limbic circuit linking the heart to the face that is involved in both social engagement behaviors and in dampening reactivity in the sympathetic nervous system. These two aspects of the polyvagal system are respectively referred to as the dorsal vagus and the ventral vagus, and each supports a different adaptive function.
• The dorsal vagus is a more primitive, early-developing “reptilian” or “vegetative” structure that oversees our primary defensive survival strategies and drives the freeze response. The dorsal vagus activates the impulse to hide or feign death. It shuts down metabolic activity during immobilization due to extreme terror.
• The ventral vagus is a later-developing “mammalian” limbic-based system that modulates sympathetic arousal through social engagement, with the goal of defusing aggression and tension. It provides safety through connection. The ventral vagus supports the ability to communicate via eye contact, facial expressions, tone of voice, and the ability to listen, all of which play important roles in our capacity for social engagement. The ventral vagus also calms the heart: the term vagal tone refers to the regulation of our heart rate. As the heartbeat slows, we feel calmer and become more available for connection.
The Polyvagal Theory gives insight into the adaptive nature of our physiology. Porges sees the two branches of the vagal system as hierarchical. First, when social engagement is a possible choice, the newer ventral vagus directs our responses. If, however, safety through loving connection is not possible, as is the case with depressed, anxious, or dissociated mothers, the system falls back on the dorsal vagus: vagal tone decreases and the heart rate rises in preparation for survival.
The Polyvagal Theory is particularly useful to help us understand the Connection Survival Style. When there is early trauma, the older dorsal vagal defensive strategies of immobilization dominate, leading to freeze, collapse, and ultimately to dissociation. As a result, the ventral vagus fails to adequately develop and social development is impaired. Consequently, traumatized infants favor freeze and withdrawal over social engagement as a way of managing states of arousal. This pattern has lifelong implications. On the physiological level, since the vagus nerve innervates the larynx, pharynx, heart, lungs, and the enteric nervous system (gut), the impact of early trauma on these organ systems leads to a variety of physical symptoms. On the psychological and behavioral level, the capacity for social engagement is severely compromised, leading to self-isolation and withdrawal from contact with others, as well as to the many psychological symptoms detailed in Chapters 2 and 8.
Within the brain are some 100 billion neurons, each capable of synaptic connection with 60,000 to 100,000 other neurons—a tremendous organization of neuronal networks with an almost infinite potential. When new information enters the nervous system, whether of internal or external origin, it activates unique patterns of interconnection, or neural assemblies, that are governed by specific laws. Since much of the work in NARM addresses the regulation of the nervous system, it is helpful to know some of the laws by which the nervous system grows, organizes, regulates, and changes.
This law is simple: cells that fire together, wire together. If two neurons are electrically active at the same time, they will automatically form a connection. If they are already weakly connected, the synapse between them will be strengthened. Neural firings gather all aspects of an experience together into a neural assembly that is encoded in memory. Indeed, it is believed that the firing is the memory.
This activity-dependent wiring together is the basic mechanism of all learning and adaptation. With new learning comes the growth of new neurons and the branching of dendrites that allow the brain to change and expand the established connections among existing neurons. We can conclude that at the physiological level, supporting growth and healing involves tapping into the processes that build and modify the cells of the nervous system and the firing patterns of neural assemblies. By working bottom-up—by specifically slowing down the pacing of a session in order to give attention to sensations and emotional responses as they are experienced in the moment—a NARM therapist makes room for new learning opportunities that can directly contribute to changing neural connections and building new networks.
We are born with an overabundance of synapses, which represents the potential connections among neurons that infants might need in order to create internal maps and models of the world. In the neonatal period a pruning process begins: because the development of neural circuits depends on our experience, neural paths that are activated remain, whereas those that are not activated and incorporated into a developing structure are eliminated, leaving only the more adaptive synaptic configurations—a “use it or lose it” rule.
The nervous system is shaped by experience—either pruned or reinforced in response to safety and stress. When stress levels are consistently high, neural pathways connecting the limbic system to the cortex are pruned, while other circuits that are more adaptive to distressing interactions, are formed and strengthened. As a result, the neural landscape becomes vulnerable to emotional and social dysregulation. Adults whose brain and nervous system were patterned by distress at the beginning of life often feel helpless in the face of their symptoms; they do not have the neural circuits to imagine a different way of being. Thankfully, the brain is constantly changing. It is the goal of a resource-based therapy to stimulate and nurture the development of neural circuits that contribute to connection and stability.
Contrary to popular belief, the brain does not operate like a camera that takes in a whole scene. It is more like a feature detector that detects individual stimuli, (for example, edges, contours, line orientation, color, form, pitch, volume, and movement) and processes them in separate regions of the brain. The term quale (plural qualia) refers to discreet attributes of reality such as green, round, or hot; the experience of a quale (say, green) is generally never in isolation of other attributes (long, sharp, cool). Given the absence of a computer-like central processor in the brain, each quale is processed in its own separate region of the brain and has its own neural networks. The experience of qualia is based in the wiring and activity of an individual’s nervous system. Each and every perception is actively constructed from the building blocks of individual sensory cues under the guidance and influence of emotion, motivation, and prior experience. How a person experiences qualia is therefore highly personal and is believed to be a large part of what shapes individual consciousness.
Through a process known as reentry, the brain weaves together the information entering in different regions to create a full picture of what is happening. For example, information entering the visual cortex (dark, red) is automatically connected to information in the auditory cortex (loud, sudden) and vice versa: what we see influences what we hear, and what we hear influences what we see. The attention we give to qualia and our brain’s capacity to blend them together comprise our perception of reality. It is believed that reentry could be the unique, single-most-important feature of higher brain organization, the vital component of integrated, complex cognitive tasks.
Under normal circumstances, all the aspects of an experience come together into one coherent whole. One of the markers of trauma is the failure to integrate the sensory imprints associated with an event into a coherent whole—a failure of the reentry function. When reentrant interactions are blocked, as they often are with trauma, unprocessed sensory information remains in disconnected fragments. For example, a client may be triggered by the color blue but have no other associations as to why this particular color triggers a stress response. As a result, incomplete memory fragments surface that do not allow sufficient recall for full processing. For a traumatized individual, missing qualia interfere with the capacity to put together a coherent narrative, and certain features of an event may become so prominent as to distort recall.
A number of somatically based interventions address the fragmentation caused by trauma. For example, a simple question such as “What else do you notice?” or “What is happening right now as you talk about this past experience?” encourages clients to open themselves to what may be missing in their recall and to bring back in connection what has been fragmented.
With every new experience, the brain searches for a match between the incoming pattern of neuronal activity and patterns already stored in memory. This pattern-matching quest gives us the sense of recognition and familiarity. In essence, perception happens through a comparison of past and present.
Because perception evolved to facilitate adaptive and survival behaviors, economy and speed of processing are critical. The faster the brain detects food, foes, and mates, the better our chances of survival. This need for efficiency prompted the development of a split perceptual system within the brain’s architecture.
• For quick survival-based responses, pattern-matching from minimal environmental cues uses the shortest possible route to transmit sensory stimuli directly to the amygdala, which is poised, like an alarm, to activate the body’s fight-or-flight hormones. This quick-response emergency route bypasses the executive cortex, sacrificing accuracy and discrimination for speed. In a prey-predator world, this can make the difference between life and death.
• The second perceptual path seeks out detailed features for pattern-matching and is consequently much slower. Moving through the more complex executive cortex and on to the hippocampus, this pathway provides the sensory discrimination that allows us to assess, regulate, and inhibit behaviors that, in the “hands” of the amygdala, are automatic responses based on summary information. This mechanism suggests that conscious awareness helps diminish fear and fight-flight-freeze responses.
The split perceptual system follows a pattern-matching protocol: (1) To minimize effort, the brain makes a quick assessment with just enough detail for a “good-enough” match. If danger is assessed, the amygdala responds to this minimal information. (2) If no match is found, the brain proceeds to seek more information until a match is found. (3) If still no match is found, a new category of experience is generated, the pattern of which is stored in memory for later matching.
Pattern-matching suggests an explanation for people’s tendencies to confuse events in the present with events from the past or to repeat past painful experiences. Because the brain initially looks for a good-enough match between past and present events, we tend to jump to conclusions prematurely. We tend to “see” what we have seen before or predict that it will happen again. Neurologically, it is not so much that we repeat the same experience but that we interpret current situations with a bias toward what has occurred in the past. For example, a child, seeing an animal never previously encountered, such as a raccoon, might say “cat” because it fits the general pattern of “furry animal” already stored in memory. However, with conscious focus on detail, a new category of animal will be generated. Greater perceptual accuracy develops by encouraging conscious attention to details in order to create new categories of experience.
It follows that psychotherapy could be conceptualized as a method of treatment that pays conscious attention to increasingly specific details in order to develop greater perceptual accuracy, separate past from present, and, when necessary, generate new categories of experience.
The traumatized, hypervigilant brain forges ahead with pattern-matching before all the data have been gathered. Traumatized individuals respond to triggering events as if they were being re-exposed to the original trauma, reacting to reminders of the trauma in a physiological way as if they were still living in the past. By mindfully focusing on the present moment, NARM interrupts the quick fight-flight-driven pattern-matching responses and challenges the accuracy of the client’s predictive perceptions. By slowing the pace of a client’s recall, interventions encourage sensory discrimination that supports a return to the present and a re-evaluation of identifications based on the past.
The development of normal perception requires the brain to receive specific kinds of stimulation within particular time frames. For example, during the first year of life, there is a window of sensitivity for the development of attachment that mediates the capacity for self-regulation. Although in early life the brain has specific sensitive periods of development, its growth is thankfully not exclusively limited to these windows. Studies have shown that throughout our lives, repeated new stimuli trigger genes to transcribe and translate new proteins and stimulate the growth of new synapses. Over the life span, every part of the nerve cell can be altered by our ongoing experiences. This “plasticity” suggests that since the receptive properties of the brain and nervous system are clearly not fixed but open to change, providing a stimulus-rich environment is critical to healing. In NARM, the focus on accessing positive resources, supporting inquiry and open curiosity, and tracking the movement of connection, expansion, and aliveness cultivate positive affect and empowering cognitive states that support reconnection with the generative drive of the life force.
It appears that the brain strikes a balance between circuit permanence and circuit plasticity. The brain’s plasticity is an essential feature of our capacity for learning, change, and adaptation—that is, the solutions we develop to meet the problems posed by our needs.
For functions such as the learning of math facts or new vocabulary, the brain exhibits a lot of plasticity, thus facilitating new learning. However, in the emotional limbic circuits, the brain exhibits more circuit permanence and less plasticity, which stabilizes psychological development. It is because of circuit permanence that children develop long-lasting attachments and that we, as adults, continue to seek out and strongly respond to familiar sources of relational comfort and safety. The brain’s plasticity is an essential feature of our capacity to learn and change, and its permanence stabilizes our psychological development, allowing us to establish long-lasting attachments. The brain is a malleable organ whose development and capacity for improvement and change are continuous and lifelong. We are not prisoners of our genes or of our environment, a hopeful message for anyone struggling with the effects of trauma.
The endocrine glands produce a chemical network of signals that keeps the entire body under balanced control and regulates vital metabolic activities. The endocrine system balances the delicate equilibrium, growth, and ongoing breakdown and regeneration of cells in the body by regulating the assimilation of nutrients and the elimination of waste. In other words, the maintenance of our health depends on the good function of the endocrine system. Its function is so closely associated with the nervous system that these two systems are often referred to as one: the neuroendocrine system.
Within the endocrine system are major glands located in different areas of the body: the pineal, hypothalamus, pituitary, thyroid and parathyroid, thymus, adrenals, pancreas, testes and ovaries. These glands produce hormones, chemical messengers that travel via the bloodstream to targeted organs carrying information vital to their good function. Each hormone is destined for a specific type of cell, which has a distinctly shaped receptor in which it can “dock.” The cell waits for the delivery of the hormone’s message to know what to do. If the hormone does not arrive, the cell remains inactive. When a hormone delivers its message, a chain reaction happens inside the cell that allows it to carry on its metabolic functions.
Hans Selye, MD, PhD, first described the stress response in the 1950s. He introduced the General Adaptation Syndrome model describing how the body responds to external sources of stress and how psychological stress influences physical illness. Selye developed the theory that stress is a major cause of disease because of the long-term hormonal changes stress causes in the body. He determined that the body has a limited supply of adaptive energy with which to deal with stress and that this amount declines with continuous exposure. When there has been trauma, stress levels are chronically high and the body loses its capacity to adapt or recover, leading to adrenal fatigue and exhaustion.
Selye also found that the effects of stress depend not only on the magnitude and duration of the stressor, but also on the strategies individuals adopt to cope with it. This is particularly important to take into account in cases of early developmental trauma, where coping strategies often have not developed beyond those used by a helpless child.
Additionally there is now evidence that when at an early age, individuals become locked in the frozen, parasympathetically dominant state of conservation-withdrawal, the capacity for DNA repair is negatively affected and the vulnerability to illness is increased.
Selye’s research clarified the biological consequences of the repeated activation of what has since become known as the hypothalamic-pituitary-adrenal (HPA) axis. He believed that the HPA system is at the core of the stress response.
The HPA axis manages the interaction between the nervous system and the endocrine system. It is useful to understand its function in trauma, since its wide range of functions affect almost every organ and tissue of the body, including the brain. The HPA axis is involved in the neurobiology of mood disorders and many illnesses, including anxiety disorder, bipolar disorder, insomnia, posttraumatic stress disorder, borderline personality disorder, attention-deficit/hyperactivity disorder (ADHD), major depressive episodes, burnout, chronic fatigue, fibromyalgia, irritable bowel syndrome, and alcoholism.
The HPA axis consists of a complex set of interactions among the hypothalamus (responsible for linking the nervous system to the pituitary), the pituitary gland (which secretes nine hormones that regulate homeostasis), and the adrenal glands (small, conical organs on top of the kidneys that release stress hormones). The HPA axis is critical to regulation: it helps regulate body temperature, digestion, the immune system, tissue function, growth and development, mood, sexuality, and energy usage.
In cases of developmental trauma, as neglect and abuse intensify, and as streams of stress hormones signal ongoing danger, the dysregulation of the HPA axis spirals. In a young child’s vulnerable brain, not only does the continuous flood of stress hormones have a tragic dysregulating effect, it also deprives the body of the all-important wash of opioids that supports bonding and the feeling that all is well.
The mechanisms of the sympathetic-adrenal-medullary (SAM) system prepare the body for the massive output of energy that is required for the fight-flight response. In addition, the SAM response sets in motion the changes necessary for survival should there be injury.
The SAM response triggers a number of far-reaching changes in the body. The adrenal medulla (the center of the adrenal gland) releases the hormones adrenaline (epinephrine) and noradrenaline (norepinephrine) into the bloodstream. These two hormones, which are potent stimulators of the sympathetic nervous system, are responsible for key changes in the body’s homeostasis. Adrenaline and noradrenaline accelerate heart rate and respiration, increase the level of tension in the muscles, constrict blood vessels, divert blood away from the viscera into the muscles, increase blood pressure and blood sugar levels, and reduce gastrointestinal peristalsis. They also trigger pupil dilation, muscle twitching, and trembling; erect the hairs on the skin; and stop the flow of saliva. In anticipation of possible injury, elevated levels of adrenaline in the bloodstream release fibrinogen to speed up blood clotting and signal the brain to release endorphins and other endogenous opioids that are the body’s natural painkillers.
These massive fluctuations in the HPA axis and SAM response are often accompanied by strong emotions: rage, disgust, terror or joy and the feeling that all is well. When NARM therapists support tracking changes in body sensations, they are encouraging clients to be present to, and not identified with, the effects of the fluctuations within the endocrine system.
The functions of the internal body, more particularly the operation of the viscera—respiration, digestion, blood pressure, temperature control, reproduction, etc., which are all responsible for the maintenance of life—are of critical consequence to the world of subjective emotional experience. There is very little conscious control in the autonomic innervation of the viscera, yet visceral experience is at the core of our sense of identity and our ability to adapt. Infants react to negative emotional arousal by instinctively contracting. They manage high-intensity activation though deep contraction of the viscera and joints and through tension in the eyes, ears, and base of the skull. Adults who developed these patterns in childhood are habituated to them and continue to use these same patterns of muscular tension and visceral contraction throughout life.
Emotional arousal, or when an event overpowers our sense of safety, causes a variety of brain alterations; high levels of emotions, as well as lack of emotion, lead to physical changes that contribute to autonomic dysregulation and psychosomatic disorders.
• In response to external danger, emotional processing shifts away from the frontal cortex, which is responsible for focused attention, motivation, and monitoring of goals, to the posterior cortex, responsible for vigilance.
• Intense emotion and stress-related illness are often accompanied by cognitive complaints such as impaired memory, diminished concentration, and difficulty thinking coherently. Reduced frontal activity seems to contribute to the apathy and lack of concentration associated with disorders such as major depression.
• In chronic states of high autonomic arousal, constant elevated levels of cortisol can impair the immune system, contribute to ulcer formations, lead to diminished activity or even atrophy of hippocampal cells, and cause damage to body tissues in the viscera and cardiovascular system.
• High emotional arousal can also trigger the physical symptoms of anxiety and panic, such as muscle tension, heart palpitation, increased blood pressure, and difficulty breathing; in turn, the autonomic dysregulation of the lungs and intestinal function may play a role in such conditions as asthma and irritable bowel syndrome.
The list of dysfunctions caused by visceral/emotional dysregulation continues to grow. Obsessions and compulsions seem to be caused by a fixed neural switch in a brain area that monitors the environment for danger; addictions, eating disorders, and alcoholism stem from dysfunction in the brain’s reward system. Disorders on the anxiety spectrum (anxiety, panic, phobias), disorders of affect regulation (bipolar, dysthymic), borderline personality disorder, and many others are increasingly seen as rooted in the neurobiologically induced affective chaos that may have its origins in early failures of attachment or breakdowns of the environment. These internal body imbalances draw an individual’s attention to his or her internal world and override, sometimes dangerously, his or her ability to tend to the external world.
Much of what we take for granted as “the way the world is,” is in fact the world as we remember it. Remembering is a reconstructive process, and every time we recall a memory, it is received in the brain as new information. Since a retrieved memory is not an exact replica of the past, retelling painful memories from a safe and resourced place opens opportunities to reduce their associated pain. Appropriate titration in the safe context of the present moment and in the presence of an empathic therapist initiates new neural firings that add positive associations into the old memories. These new firings encode feelings of safety and comfort into the traumatic recall, thereby creating opportunities for the modification and transformation of our trauma responses.
We do not have to be conscious of a memory in order for it to actively influence our thinking, feeling, and behavior. Our long-term memory is divided into two main branches: explicit, or consciously processed memory, and implicit, or unconsciously processed memory.
• Explicit Memory. Usually, when we think of memory, we think of the explicit branch, which holds all the sights, sounds, smells, conversations, as well as thoughts and images of which we are conscious. It holds personal and general facts that underlie our knowledge of the world—date of birth, who is president—and the autobiographical memory of specific personal events that uniquely define our lives—yesterday’s visit to a friend, last year’s birthday celebration. Explicit memory is readily made conscious through images and words.
• Implicit Memory. The implicit branch stores information that is out of our conscious awareness and verbal experience. Consequently, even though it constantly influences our current functioning, it does not feel like memory to us. It feels more like who we are. Stored in implicit memory are the memory of shapes and forms; the bodily memory of motor skills, habits, and routines; and the memory of our emotional and relational responses. Because implicit memory is non-conceptual and nonlinguistic, it is difficult to investigate its content with verbal methods. Techniques that use a bottom-up approach and make room for empathic resonance are better suited to explore experiences encoded in implicit memory.
Most authors who address issues of somatization agree that they are rooted in failures of infant-caregiver attunement and that these failures are imprinted in implicit memory. The fundamental relationship between the brain-mind-body, particularly when it comes to the processes that establish the underlying capacity for self-regulation, occur rapidly and autonomously, beneath conscious awareness. It is by facilitating a felt sense awareness that nonverbal experiences can become known, thereby developing the capacity for self-knowledge and organization.
How is it that we instinctively recognize a safe person, and how is it that we know, at a “gut level,” the authenticity or falseness of a new acquaintance? Infant observation studies suggest that infants are born with a great deal of relational knowing. They show anticipation of contact and are upset with violations of expected loving connection. These types of relational patterns are seen to be true in all infants. This universal human experience is anchored in what is now called implicit relational knowing. As adults, we experience a visceral recognition and sense of heartful expansion during authentic person-to-person connection and a visceral distress when connection fails. The joy that rises in moments of authentic meeting, of meaningful connection, is recognized by all humans as central to the feelings of aliveness that infuse our desire to live. Much of adults’ memories of relational trauma involve stories of the outrage they experienced in the face of what they viscerally knew to be a violation of natural goodness.
Transforming what we see, hear, feel, and think into memory is directly related to the degree of attention we give to the information we receive. This degree of attention is in relation to the pleasure or aversion we feel in a given situation. When retrieving a memory, the richness or paucity of the emotions associated with that memory affects the content and quality of what we remember. To grasp the potent hold of emotions on our thoughts, we must remember that the rational cortex is rooted in the earlier emotional limbic system; cortical and limbic brains are inseparably intertwined. In effect, we have two minds—one that thinks and one that feels—the classic duality of the rational head and emotional heart. The emotional brain is the foundation upon which the thinking brain is built.
Although emotional arousal normally enhances our capacity to remember, excessively high levels of emotional arousal impair memory. In the case of severe trauma and posttraumatic stress disorder, high levels of circulating cortisol can cause cell damage or even complete shutdown in the hippocampal system, precipitating impairments in explicit memory. In such cases, traumatized individuals cannot express what happened to them in words, and their memories manifest implicitly as dissociative behaviors, startle responses, nightmares, and visual and somatic flashbacks.
It has been clearly demonstrated that an experience learned in one context, either inner (mood and emotions) or outer (environment, location), is more easily recalled when we are in a similar inner-outer environment. We are, for example, more likely to recall an event that was encoded in a sad mood if we are feeling sad. The closer the similarity between a memory and the state we are in at the moment of recall, the more the memory is enhanced and the greater the chance that the memory will be relived rather than recalled. This close relationship between the state we are in at the time of encoding and the one at the time of remembering is called state-dependent learning and memory.
When working with trauma, in order to avoid harmful regressions and traumatizing reliving of past experiences, managing state-dependent memory is particularly important. This is why in NARM, the focus on working with the dual awareness of past and present is an important tool to avoid the danger of reliving rather than remembering a trauma.
In the face of threat, there are predictable biological responses that are shared by humans and animals alike. Here, we describe four major responses that are particularly relevant to developmental trauma: the defensive-orienting response, hypervigilance, the fight-flight-freeze response, and the exploratory-orienting response.
The defensive-orienting response is nature’s first reaction to threat. The following short, guided fantasy, adapted from Somatic Experiencing, helps access the direct experience of the defensive-orienting response. As you go through the exercise, it is important to track your bodily experience and reactions:
Imagine you are home alone, relaxed in bed, reading a book. You are not expecting anyone. Suddenly you hear a very loud noise. What is the first thing that you notice in your body?
Most people report contraction and arousal. This is the startle-arrest response. When faced with possible or actual threat, the body goes into an arrest response: we hold our breath, we become completely still, all extraneous activities stop. We focus attention on our senses, particularly vision and hearing. Usual comments to this exercise are: “I perk my ears up” or “I begin to scan.” Why would we do that?
Obviously, we are hardwired to identify the nature of the threat. We want to know what it is and where it is coming from. We use our eyes and ears to orient ourselves to the source of the threat. Primarily using our senses of vision and hearing, we search for the source of the real or possible danger. Why is this important?
Identifying the nature of the threat leads to one of three reactions: fight, flight, or freeze. If actual danger is located, there are three available strategies: fighting the danger, running away from it, or remaining completely still so as to be invisible.
Imagine now that you identify the source of the threat as merely the wind banging a tree limb against the window. What happens in your body now?
You begin to relax. Bodily tension, particularly in your neck, shoulders, and eyes, dissipates. When we realize that there is no threat, there is a return to a state of relaxation.
When the defensive-orienting response remains incomplete in the nervous system, individuals live with a continual sense of threat. In a reaction of hypervigilance, they are constantly looking for danger. Until the defense-orienting response is completed, people can spend their entire lives in this state.
When individuals are stuck in an unresolved, persistent defensive-orienting response, they continue to scan the environment for danger even when the external threat is no longer present. This continuous scanning, traditionally called hypervigilance, is the result of an attempt to locate danger, not realizing that the source of the danger no longer exists externally. It is, however, still driven internally by undischarged high arousal in the nervous system. (The related symptom of hypovigilance, which consists of a diminished and inadequate awareness of threat, is discussed later under dissociative reactions.) Individuals with early developmental trauma are more vulnerable to later traumas because of their narrowed range of resiliency and lack of access to their aggression, including the fight-flight response. The more extreme the early trauma, the less resilient they are likely to be, and the more severe their symptoms.
Essentially, the goal of the fight-flight response is to prepare us to defend ourselves in a situation of threat or to run away if we cannot defend ourselves. The fight-flight response is mediated by high arousal in the sympathetic branch of the autonomic nervous system as it prepares the body for self-protection and survival. The freeze response is mediated by the parasympathetic branch of the autonomic nervous system. There are two aspects to the freeze response: (1) freeze as a highly charged but immobile defensive maneuver and protective reaction, which is used by all animals, including humans, to avoid being noticed by a predator and (2) freeze as a collapsed fallback position when fight-flight is not possible.
A common metaphor used to explain fight-flight-freeze is to compare the sympathetic branch of the autonomic nervous system to the gas pedal of a car and the parasympathetic branch to the brakes. In trauma, the sympathetic branch is fully engaged (that is, our foot is pressing the gas pedal to the floor) to mobilize massive amounts of fight-flight survival energy. At the same time, the parasympathetic branch is applying the brakes in an attempt to modulate the dangerously high sympathetic arousal. In essence, both the gas pedal and the brakes are simultaneously pressed to the floorboard. The result is high tonus in both branches of the autonomic nervous system: the engine is turning at high speed but the brakes are fully engaged, leaving the car at a standstill. This standstill involving high tonus in both branches of the autonomic nervous system is a particular type of freeze response called tonic immobility. The state of tonic immobility should not be confused with a collapse response, which is a type of freeze in which the parasympathetic branch of the autonomic nervous system is dominant.
In the presence of safety, all animals, including humans, return to what is called the exploratory-orienting response. Curiosity is the non-traumatized body’s natural movement outward as it is motivated by the desire to explore its surroundings when there is no threat or sense of threat. To see the exploratory-orienting response in action, simply observe any healthy toddler, puppy, or kitten. The world is their oyster: they are curious about everything, and their exploration is joyful and full of discovery. This state of open curiosity is the normal non-traumatized state. It becomes available again when a person completes the biological sequence of the defensive-orienting response.
Early trauma is overwhelming, disorganizing, and painful. It creates high levels of systemic arousal and stress that, when ongoing and undischarged, are managed in the body through visceral dysregulation, muscular contraction, and the dissociative processes of numbing, splitting, and fragmentation.
Shock trauma—the impact of acute, devastating incidents that leave an individual frozen in fear and frozen in time—is clinically recognized and treated under the diagnosis of posttraumatic stress disorder (PTSD). In single-event shock trauma, the defensive-orienting response is overwhelmed, completion of fight-flight is not possible, and individuals stay stuck in an incomplete defensive-orienting response. The goal of therapy is to help individuals come out of freeze and complete the fight-flight responses.
Developmental trauma causes ongoing autonomic activation that forms chronic patterns that lead to physiological and psychological developmental deficits. In developmental trauma—which can include specific shock traumas at an early age, profound ongoing misattunement such as in attachment trauma, as well as ongoing abuse and/or neglect—the physiological response may be similar to that in shock trauma, but the dynamics of the trauma itself are quite different. Commonly, with developmental trauma, there is no single traumatizing event, but rather, ongoing experiences of neglect, abuse, and misattunement. The early nature and chronicity of developmental trauma, along with the relational element when parents are the perpetrators, create the therapeutic challenges that are addressed in this book.
Current studies in developmental traumatology show that the cumulative effects of chronic early abuse and neglect adversely influence brain development and negatively impact the nervous system, endocrine system, and memory. Many studies show that trauma of a relational nature is more impactful than trauma from nonhuman or inanimate sources. In fact, it is now believed that severe relational trauma can be so powerful as to override every aspect of an individual’s capacity to cope.
Because of the lifelong psychological and physiological deficits that result from relational abuse, neglect, and dysregulated attachment, a new differential diagnosis of developmental trauma is being considered. In a call for this new diagnostic category, Bessel van der Kolk, MD, and others have shown that trauma has its most pervasive impact during the first decade of life. Abused infants and children often experience a broad spectrum of developmental delays, including cognitive, language, motor, and socialization skills. The diagnostic criteria for PTSD is not sensitive to developmental issues and therefore does not adequately describe the effect of ongoing early trauma, abuse, and neglect on child development. Chronic family stressors and relational trauma, particularly early in life, increase the risk for psychological, social, and physiological disturbances whose symptoms and treatment differ significantly from the traditional clinical approach to PTSD. The newly proposed diagnosis of developmental trauma addresses several key aspects unique to ongoing trauma occurring early in life. As we demonstrate in this book, developmental trauma can lead to long-lasting changes in neurobiology, behavior, development, and physical health, resulting in identity distortions and systemic dysregulation.
Developmental trauma may well be one of the most important public health issues in the world today. It is estimated that in the United States alone it affects nearly three million children yearly. Because PTSD does not factor in developmental issues, and because developmental trauma is not a recognized diagnosis, children are often misdiagnosed with ADHD and bipolar disorder. Large populations of children who could benefit from treatment are missed, mislabeled, or treated incorrectly based on an inaccurate diagnosis. A recognized diagnosis would open needed avenues of funding for the research and development of appropriate treatments for this critical area of human development.
One of the strategies used by animals in response to threat is to run for safety. Animals run to their burrows, flee to their caves or to any other safe place. When infants or small children experience early shock or attachment trauma, the threat is inescapable. Whether the threat is intrauterine or takes place at birth or later in life, there is no possible safety independent of that provided by the caregivers. Infants are completely dependent, and when their caregivers, for whatever reason, are unable to provide safety or are the source of the threat, infants experience the only home they have as unsafe. This sets up a pattern for a lifelong sense that the world is unsafe. The earlier the trauma, the more global the impact on the physiology and psychology.
When there has been early trauma and developmental wounding, a person may become “stuck” in the defensive-orienting response. The problem for human beings is that the high arousal that gears us up for fight-flight, when not discharged, creates a sense of threat that triggers more defensive-orienting and sets up an ongoing distress cycle that affects all of the body’s systems. Strategies to resolve the sense of threat once real threat has passed, must address the source of the threat that is now in the nervous system itself as well as held in memory and in every cell of the body.
When threat is chronic, when danger never goes away and there is no possible resolution, as is the case in abusive families, the entire organism remains in a defensive-orienting response and the nervous system remains locked in a state of high sympathetic arousal and vigilance. In cases of early or severe trauma, when infants cannot run from threat or fight back, arousal levels can be so dangerously high that they threaten to overload the nervous system, and often do so. Locked in perpetual, painful high arousal, the only alternative, the fallback position, is to go into a freeze state, which infants and small children accomplish by numbing themselves. Until the defensive-orienting response is completed and the high levels of arousal are discharged from the nervous system, the environment continues to feel unsafe even when the actual threat is gone. Being locked in an unresolved defensive-orienting and freeze response can become a lifelong state, as we see in individuals with the Connection Survival Style.
As Peter Levine, PhD, has documented, tonic immobility and other kinds of freeze responses are intended to be time-limited. When the threat has passed, animals return to normal functioning by allowing their bodies to tremble in order to shake off the high sympathetic arousal. In the face of chronic threat, however, when a fetus, infant, or child remains in a persistent freeze state, he or she is living in a parasympathetically dominant state of collapse. When collapse and threat continue, individuals seek comfort from this unbearable state by detaching their consciousness from their ongoing painful experience. They disconnect from bodily experience and from the threatening environment. This disconnection is the beginning of what can become a lifelong dissociative pattern.
In Somatic Experiencing®, the term range of resiliency is used to describe an individual’s overall capacity to cope. Included in that definition is a person’s capacity to self-regulate and self-soothe. In NARM, range of resiliency also includes a person’s access to his or her core energy or basic life force.
High levels of arousal, freeze, and dissociation held in the body foreclose a person’s access to his or her life force and create a diminished range of resiliency. The tragedy of early trauma is that when babies resort to freeze and dissociation before the brain and nervous system have fully developed, their range of resiliency becomes drastically narrowed. In addition to the normal challenges of childhood, meeting later developmental tasks becomes that much more difficult. Being stuck in freeze-dissociation, these individuals have less access to healthy aggression, including the fight-flight response. In addition, their capacity for social engagement is strongly impaired, leaving them much more vulnerable and less able to cope with life challenges and later trauma.
Coherence refers to how each part of a system behaves in relationship to the others and to the whole. Coherence is a reflection of the positive cooperation within a system and between systems, and is experienced as a sense of ease, organization, and unity throughout the whole body. Coherence is the result of the smooth interplay between various systems of the body and often results from the integration of internal and external resources.
In the context of development, external resources are those elements of our early environment that are experienced as supportive, that help us learn to self-regulate, that provide a sense of safety, meaning, and continuity to our life. Inborn internal resources involve genetic resiliency and general hardiness. Additional internal resources develop as a result of supportive positive life experiences.
As children develop, internal resources and the availability of ongoing external resources progressively support coherency and organization on all levels of being. Individuals who are unable to integrate their traumatic experiences often lose their capacity to assimilate new experiences, and their development stops at a certain point. The psychological consequence of trauma is the breakdown of the adaptive processes that normally lead to the maintenance of an integrated coherent, continuous, and unified sense of self.
Traditional psychology focuses on the importance of a coherent narrative. Understanding that a coherent narrative is a reflection of somatic coherence helps develop a positive healing cycle in which increasing somatic coherency supports an increasingly coherent narrative bottom-up, and an increasingly coherent narrative reinforces somatic coherency top-down.
| COHERENCE | ACTIVATION |
Breath is slow and deep |
Breath is rapid and strained |
No bracing in muscles |
Muscles are braced or slack |
Breath moves through whole body in steady rhythmic wave |
Breath is disconnected and does not flow between body areas |
TABLE 7.2: Some Physiological Markers of the Differences between Coherence and Activation
NARM is a scientifically informed approach to the experience of self, embodied self, and self-in-relationship. Through the use of somatic mindfulness, NARM calls upon the body’s natural regulatory mechanisms to support the brain’s relationship to and interpretation of sensory experience. Somatic mindfulness is a bottom-up, nonverbal skill for self-reflection that helps us examine the internal relationships between body, brain, and self. It supports being present to, but not identified with, shame- and pride-based identifications. By exploring the links between our in-the-moment conscious experience and our unconsciously held in-the-gut encoded memories, NARM supports the capacity for regulation. By helping clients build tolerance for stress and increased levels of arousal, NARM seeks to expand the neural networks of descending and ascending communication that organize experience. In this way we can better know what we are feeling about our thoughts and what we think about our feelings.
NARM principles, tools, and techniques, described in Chapter 10, contribute unique approaches to stabilizing nervous system activation by encouraging new neurological connections, facilitating neural interconnectivity, and nurturing neurological deficits. For example, by making resourcing central to NARM therapy while supporting greater compassion for ourselves and others, treatment is delivered in a context of support, accessing the brain-building capacity of positive experiences. Many of the disorders that have been seen as purely psychological are now being reframed to include neurobiological correlates and mechanisms. Taking into consideration that trauma can damage the brain itself, NARM supports the development of skill-building techniques that bring organization and regulation to impaired functioning.