CHAPTER 7
Art Therapy, Health and Homelessness
In this chapter I consider how art therapy can provide the opportunity for a client to make sense of, and give meaning to, health difficulties within the context of homelessness. I introduce homelessness and art therapy with this client group. I then use a case study to illustrate how one client used art therapy to explore his sense of self and to think about his future following a double leg amputation.
Introduction to homelessness
I am an art therapist working in the NHS in Scotland with people who have experienced complex trauma and who are homeless, or at risk of homelessness.
To be homeless is to be without a home, but ‘homelessness’ is the ongoing state of not having a permanent home. The term ‘homelessness’ is often used to mean rough-sleeping, however, it also encompasses people living in temporary accommodation, or those at risk of losing their home due to being unable to cope practically or emotionally with their own tenancy.
Campbell (2006) suggests that homelessness physically externalises someone’s internal chaos or ‘outsiderness’. Many homeless clients say that they feel they have ‘never fitted in’, that they have always felt on the periphery of family, peers and society. In her article, Campbell discusses Henri Rey’s description of the ‘claustro-agoraphobic dilemma’. This dilemma, related to attachment, describes wanting closeness and settledness, but finding the emotions they generate intolerable. This may mean that clients with a history of interpersonal difficulties and homelessness may manage to settle in temporary accommodation, but struggle on a psychological level when they move into their own house. Campbell formulates this by saying:
The disruption caused by the move then repeats an original trauma, creating feelings of abandonment in an individual, then the cycle begins again, as the person seeks, and later feels compelled to leave, a home given to them by others (Campbell 2006, p.163)
Bentley (1997) also suggests that interpersonal relationships and self-esteem may be challenging for homeless clients. O’Connor (2003) has written about the centrality of the therapeutic alliance in treating relationship difficulties with this client group. He states, ‘The containment relationship is the first kind of home, before there is an awareness of what we later think of as home’ (O’Connor 2003, p.118).
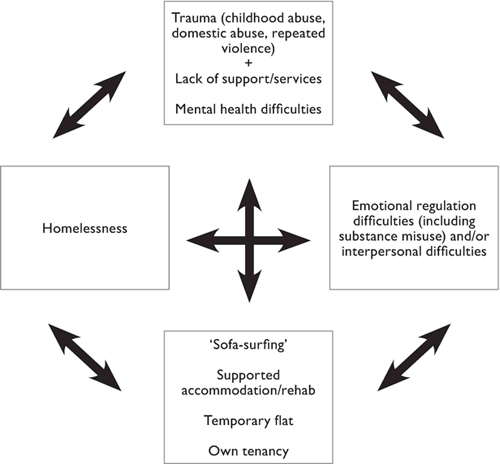
When people experience homelessness repeatedly, this is sometimes referred to as ‘the revolving door of homelessness’. I have tried to represent this in Figure 7.1 (page 150).
Some people only go around this cycle once before their own resilience, friends/family or services support them to move into their own home. However, others appear to be stuck in the cycle of homelessness, never quite finding a way out into a settled way of life.
Due to the complexity of some clients’ presentations, a holistic model needs to be adopted by services. Someone’s past experience of home, and their thoughts and feelings relating to this, affect their capacity to sustain their own home – so finding a solution to homelessness is more complex than just providing someone with a flat.
In Glasgow it was estimated that 89 per cent of people using homelessness services had experienced repeated traumas (Collins and Phillips 2003). Cloitre, Cohen and Koenen (2006) identify emotional regulation and interpersonal difficulties as being highly prevalent in clients who have experienced complex trauma. Clients often have not had the opportunity to learn helpful coping strategies, due to attachment difficulties or lack of positive modelling. Research (Classen, Palesh and Aggarwal 2005) shows that clients who have had trauma-related issues in childhood also have an increased risk of re-victimisation in adulthood if emotional regulation and relationship difficulties are not addressed.
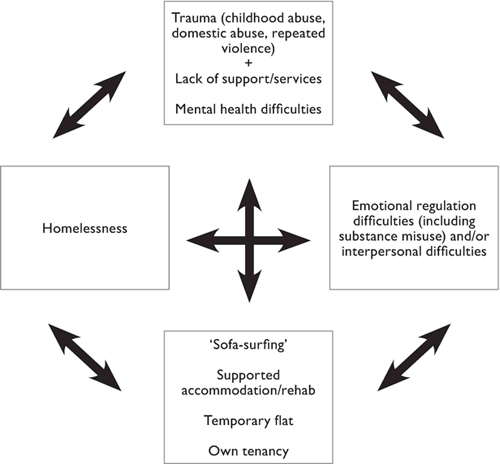
Figure 7.1 The revolving door of homelessness.
Art therapy and homelessness
Art therapy can provide a less threatening psychological intervention than talking therapy alone. Using art materials can dilute the intensity of the one-to-one relationship that some clients find quite intolerable and which prevents them from engaging with services on an ongoing basis. A ‘slow start’ to therapy with art activity and shared art-making can improve self-esteem, underpin identity work and consolidate the therapeutic alliance. Confidence in the treatment offered can be increased by psycho-education about the impact of both trauma and homelessness. Art therapy within a therapeutic relationship can facilitate communication of the client’s narrative when they lack the capacity to verbalise their experiences. It also enables fragmented parts of memory and ‘sense of self’ to be brought together and viewed as a whole. Images can create an objective distance between the client and their ‘material’; and this can reduce feelings of being ‘merged’ and overwhelmed, as well as creating the opportunity to examine and explore thoughts and feelings.
There is scant research about art therapy with people who have experienced, or are experiencing homelessness, and the majority is based on case studies from the USA (Arrington and Yorgin 2001; Cameron 1996). Davis (1997) describes her work with women in a homeless shelter in New York. She focuses on a 32-year-old woman with a history of childhood trauma, and how she used the materials in art therapy to make house-like structures. There seemed to be a process of the client’s internal sense of self shifting over time. The study shows her artworks as initially fragmented and fragile, then becoming stronger and more solid several months later. This change may have been due to the containment and reliability offered by both the art therapy sessions and the shelter.
Nelson Braun (1997) describes an art therapy open group with men in a homeless shelter. She notes that the use of clay appeared to provide a continuity that other media such as drawing or painting did not. The necessity for the men to return to glaze a piece made the previous week, or to collect a fired piece, appeared to aid a sense of commitment. In this way the art material, and the therapist’s need to ‘see to’ the artwork, offered a continuity that was scarce in other areas of the men’s lives. Nelson Braun suggests that the open studio provided the men with an opportunity to reconsider their self-image, since many of them enjoyed referring to themselves as ‘artists’. This enabled some of the men to see themselves and their strengths and resources in a different light, allowing an expression of potential. Although the literature does not focus on individual case studies, the therapeutic alliance in art therapy appears central.
Health-related difficulties and homelessness
Homelessness can impact upon both physical and mental health. Recent research (Homeless Link 2010) found that eight out of ten homeless clients had one or more physical health difficulties; seven out of ten clients had one or more mental health difficulties; in the previous six months, four in ten had been to Accident and Emergency at least once, and three in ten had been admitted to hospital.
Thomas’ (2011) research entitled ‘Homelessness: A silent killer’ states the average age of death as 48 for a homeless man and 43 for a homeless woman, compared to 74 and 80 for the general population; drug and alcohol abuse are common causes of death amongst this population, accounting for just over a third of all deaths; people who are homeless are over nine times more likely to commit suicide than the general population. Thomas concludes that the health of people experiencing homelessness is among the poorest in our society.
Case study: Jim
Jim was 45 and had slept rough and lived in homeless hostels since his early twenties. He was single, had been unemployed for 20 years and had been using alcohol for most of this period. His long history of rough-sleeping, often in extreme weather conditions, led to developing frostbite, and Jim had to undergo a double lower-limb amputation. He was in hospital for several months after his amputations, followed by a move into a flat; this broke down very quickly. He chose to sleep rough for a while in his wheelchair rather than move into supported accommodation. He then moved into another flat, but found it difficult to settle there. Jim had a huge number of services involved in his care: occupational therapy, physiotherapy, nursing, personal care team, psychiatry, community addiction team and social work. His occupational therapist referred him to art therapy, as she was aware that he had enjoyed attending an art class in the past, and she doubted that he would engage with other psychological interventions. The referral stated that Jim had difficulties in relationships and that his mood and self-esteem were low. As an independent man, he was struggling to come to terms with his freedom being curtailed by the major life change imposed on him by the amputations. In addition, he had begun drinking again after a lengthy period of abstinence and had been diagnosed with alcoholic hepatitis.
Assessment
I met Jim in a health centre close to where he lived. He stated very clearly that he ‘wasn’t sure about this art therapy thing’, and that he was not going to tell me anything about himself, as he did not think he needed any help at all. He made little eye contact and his self-care and personal hygiene were poor. He was reluctant to talk spontaneously, to answer my first few questions or to disclose anything personal. In previous notes, Jim had been described as being ‘difficult to assess’ and ‘uncooperative’, so I was aware that I had to build a therapeutic alliance slowly and carefully. I informed him about the team and its role, and about art therapy offering a different way of working that was not based solely on words, but on both of our experiences of the artworks he might make. I spoke of how we could work collaboratively to discover if art therapy could be helpful to him. I suggested that we met for three assessment sessions and then review whether we felt we could find a way of working collaboratively. Jim agreed to ‘give it a go’, albeit rather reluctantly. At this first meeting, I introduced him to the art materials, explaining that through them he could express anything he wanted to and that we would look at it together, and think about how it related to him and his current difficulties. I also set boundaries, pointing out that I would not be able to meet with Jim if he was heavily under the influence of alcohol or if he was aggressive in sessions. Jim, somewhat seriously, agreed to this.
Over the next three sessions, Jim used coloured pencils (black and grey) to write a single word. We quickly established a way of working together where I then read the word aloud, mirroring it back to him, and he took this as an invitation to expand on what the word meant to him (see Figure 7.2, page 154).
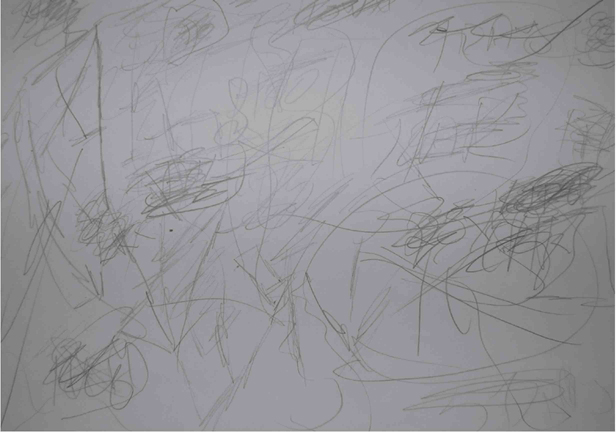
Figure 7.2 Jim’s tentative explorations.
Jim wrote ‘sister’.
Me: Sister?
Jim: I’ve been feeling fed up that I haven’t spoken to her for ages.
Me: Tell me a bit more about your relationship with your sister.
Jim went on to tell me a little about his sister, often drawing and doodling while speaking. He kept his focus on the paper rather than looking at me, and in this manner we were able to piece together a family history. Jim told me about his siblings. His parents had separated when he was young and his mother had remarried, and Jim had enjoyed a close relationship with his stepfather. From an early age alcohol seemed to feature frequently in the family’s socialising. Jim stated that his stepfather had introduced him to drinking shandy when he was seven years old. He described being ‘rewarded with alcohol’ in his early teens when going to buy drink for his stepfather and friends. It was clear that he had enjoyed the group aspect of this ‘drinking culture’, which seemed to be linked to family, friends and belonging. Unfortunately, Jim told me with great sadness, when he was 16 his family life changed significantly when his stepfather’s health deteriorated and he suffered a long, painful death through cancer, devastating the remaining family.
Jim said he had had two jobs after leaving school, losing both of them ‘because of the drink’. He moved out of the family home, isolated himself and began what became a 20-year period of rough-sleeping and living in hostels. Jim told me proudly, ‘I have lived in, and been thrown out of, every hostel in the city.’ He had not had any contact with his family for several years, as he felt he had let them down and did not want them to see him as he was now.
We explored Jim’s emotional regulation skills and he readily acknowledged that alcohol was his main coping strategy: ‘I’ve never known anything else.’ His mood was low but this was difficult to assess due to his drinking. He spoke of preferring to be alone, as he found it very difficult to trust others, but the more he drank, the lower his mood became and the more he kept himself to himself. He was finding it particularly difficult to rely on services for help with personal care. He spoke with great fondness of when he ‘used to be free, when I could do whatever I wanted, whenever I wanted’. At times, he appeared to try and live as he had done previously, spending the weekend drinking in the city centre, sleeping in parks, being picked up by the police (to whom he was well known), and ‘just doing what I did before’. It felt to me as though Jim had lost a lot more than his mobility when he had his surgery: he had lost his way of life.
Formulation
I found Jim a likeable, outgoing character who liked a joke and loved to tell stories about some of his past adventures. He had an infectious laugh. He had an independent spirit, but his experience of long-term hostel dwelling with many years of bullying and violence had made him cautious of trusting people, meaning that he isolated himself and had no friends or social supports. This lack of trust impacted upon his relationships with support services. Jim had good insight into how alcohol was detrimental to both his health and relationships. He acknowledged that after drinking he was far more likely to become irritable or angry with support staff, who visited him several times a day. There appeared to be themes of loss for Jim. He was struggling to come to terms with his amputations and how these had curtailed his chosen lifestyle. The adjustment to his current situation appeared overwhelming and Jim made it clear that he longed for his former life. There was also unresolved grief relating to his stepfather’s death and the subsequent disintegration of the family unit.
After the three assessment sessions, Jim said he would like to continue art therapy sessions, saying, ‘It’s my time in the week when I can think about things.’ We agreed to focus on the following:
•emotional regulation and self-esteem
•interpersonal difficulties
•loss of former lifestyle
•loss of stepfather and family.
The impact of amputation
Having an amputation is likely to have a marked physical and psychological impact on an individual. Saberi (2004) likens the process of losing a limb to the grieving process of a loved one. She quotes the five stages of grief defined by Kübler-Ross (1969) and contextualises them with limb loss:
1.Denial and isolation: ‘It’s not really happening!’
2.Anger: ‘Why is this happening to me?’
3.Bargaining: ‘If I promise to do such and such, maybe I’ll get my old life back.’
4.Depression: ‘I feel hopeless. Why bother trying? I give up.’
5.Acceptance: ‘I don’t like it, but the amputation is a reality. I’ll find ways to make the best of it and go on.’
Coming to terms with the psychological impact of an amputation is therefore often as important as coping with the physical demands. We know that the process of grief is not defined in easily identifiable stages, but is a fluid process that is dependent on varying factors.
The NHS Choices web site (2012) states that the outlook for people who have had an amputation to adapt and move forward in their lives depends on their age and how much of the limb was removed. How well they cope with the emotional and psychological impact of amputation is directly related to how a person coped with life’s challenges before their amputation.
Applying these considerations to Jim’s case, he was middle-aged when he had his surgery, and the two above-the-knee amputations greatly impacted upon many areas of his life. Reflecting upon Jim’s coping skills before the operation, to suggest how well he might cope afterwards, I concluded that he had a limited repertoire of coping strategies for life’s difficulties. He found problem-solving challenging and had usually removed himself physically, or emotionally via alcohol use, when he felt overwhelmed. Thus it was always going to be hard for Jim to maintain the resilience he needed to overcome his extensive difficulties.
Reflection
When Jim was referred to the team, he was probably at what Saberi (2004) defined as ‘Stage 4: Depression’ in the grief model. He was feeling hopeless and helpless. He was no longer able to sustain the lifestyle he had become accustomed to, despite continuing to try. However, with the opportunity to reflect on his sense of self in a safe, reliable, consistent space, framed by a robust community support team, Jim appeared to make progress in coming to terms with his life events. He built up a coherent narrative and could think about the future. His self-care and personal hygiene improved. He appeared to move into ‘Stage 5: Acceptance’ and expressed more insight into his situation. Jim began to talk about a time during his rehabilitation when he had watched other people who had had lower limb amputations learning to walk using artificial limbs. He spoke of how this had inspired him to learn to walk using one prosthetic leg, and how he had managed to continue doing this for some time. He explored the potential of the future, including how he wanted to renew relationships with family members. He appeared to be optimistic and was motivated to address day-to-day problems.
His art-making continued in the same vein as during the assessment process, but with Jim’s initial prompt becoming more specific. He wrote an abbreviation or the initials of what was on his mind, and when he was satisfied that I understood what he meant, he frantically scribbled the words while we discussed the topic, as if our conversation had to be kept confidential and hidden, being exclusive to him and me. I then tried to connect our discussion to other areas or themes he had mentioned, attempting to bring together these separate parts of his life. As I did this, Jim drew lines connecting the disparate fragments into a more cohesive form. Jim worked on his images for several sessions until either the paper was full or he was satisfied with the outcome. The drawings became more intense (see Figure 7.3, page 158).
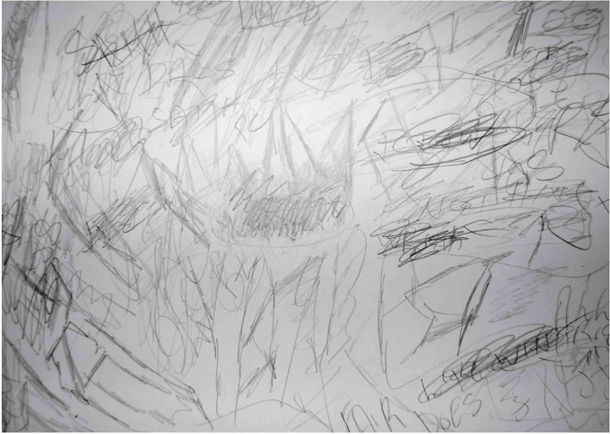
Figure 7.3 Jim’s visual expression of our verbal communication.
During discussion, while we both tried to make sense of what Jim brought to the session, if he agreed with my interpretation, he said or wrote ‘Fair do’s’. If he did not agree, he added a further discussion topic until he was satisfied we were on the same wavelength. Occasionally he got quite frustrated with me when I did not pick up his intention. I worked with this by reflecting back to him how important it was for him that I understood what was on his mind. I felt like an ‘intuitive mother’, trying to tune in to my baby’s needs. We seemed to be working at an early stage of emotional development, one where the mirroring-back of the parent provides containment and reflects a sense of self for the infant.
Jim attended almost every session and phoned to say he could not attend on the two sessions he missed. He never attended under the heavy influence of alcohol. His self-esteem appeared to improve. His personal care improved and he took more pride in his appearance. He made regular eye contact and appeared more confident in the consistency and continuity of the art therapy sessions. He informed me that he was coping more positively with the challenges of using his wheelchair. When I first started working with him, he told me he ‘threw’ himself off the kerb to cross the road, and just expected cars to stop for him. He began to adopt safer behaviour, crossing at the correct places and asking for help when appropriate.
Jim used the same technique to address relationship difficulties. He wrote names or situations on the paper, allowing us to discuss current conflicts and frustrations, while he worked through how to address them. Once he had resolved a problem, he scribbled the word out. About three-quarters of the way through therapy, Jim told me he had significantly reduced his alcohol use, although he was still drinking daily. We explored coping strategies to maintain this, such as listening to music, spreading out his appointments during the week, and planning his days to have his first drink as late as possible. He was able to consider how his alcohol use had impacted upon his relationships with his family and people in his life who had been important to him, whom he had loved and lost. He became more thoughtful and reflective. He began talking about how life was when he used his artificial limb. He told me how triumphant he had felt when he had been able to walk up a flight of stairs in the hospital. He said he had been thinking a lot about how he could get this level of mobility back. He wanted to engage with physiotherapy services again and ask for another prosthesis, as he had lost it while sleeping rough. He spoke about completing a rehabilitation project some years previously, after which he had maintained five years’ sobriety. He hoped that this could be achieved again.
Deterioration
After ten months of art therapy, Jim became increasingly physically unwell due to his deteriorating liver function. His appetite was poor and his energy was low. He had to attend hospital appointments for further tests. He spoke of his fear of hospitals due to people dying in the ward he had been in. Jim knew he needed medical help, but absconded at the last minute from the waiting room on several occasions, unable to tolerate the anxiety of waiting. At first Jim’s mental health was considerably better than his physical health. He was upbeat and still making jokes. He was able to think rationally about his fears and anxieties, and about how non-action might impact upon his long-term health. He was able to identify positive and helpful coping strategies. He still spoke of the future with relish for what it might hold.
However, as time went on, Jim began to consume more alcohol in a frantic effort to cope with his difficulties. In sessions we revisited his strategies for coping with anxiety. Although he said he did not want to return to his previous chaotic lifestyle, his drinking, and associated negative behaviours, rapidly increased, despite input from other services. Therefore our work focused on the stark reality of him stabilising his alcohol use or knowing the consequences of continuing to drink, which was acceleration towards an early death. There were several sessions when he appeared to alternate between the two directions, and although I hoped he would ‘choose life’, I knew the decision was only his to make. Decision and choice seem clumsy words, considering the complexities of this situation.
It soon became apparent how things were going to progress. Jim was increasingly reluctant to follow medical advice and spend time in hospital, saying he felt his freedom was being restricted. His use of alcohol had a negative impact on his ability to look after himself, as well as exacerbating his deteriorating liver condition. Community services were struggling to find ways of supporting him and Jim’s quality of life was declining as a result of his chronic alcohol use and poor self-care. His memory waned and he was losing weight rapidly. As he no longer had the energy to propel himself in his wheelchair, he became dependent on services for going out.
Jim was still keeping to the boundaries we set up regarding attending art therapy sessions. He did not attend when ‘heavily under the influence’, and continued to use the therapeutic space to think about week-to-week problem-solving. He felt huge pressure from medical staff to go into hospital ‘so they can just take over my life’. He referred to himself as ‘stubborn’ and wanting ‘to do it my way’. He continued to use the art materials to communicate how he was feeling, and when we discussed the certainty that he would die of liver disease if he did not receive treatment, he was able to acknowledge this in a matter-of-fact manner. He was clear that, for him, this was preferable to being ‘confined’ to hospital.
Over a period of weeks it became apparent that our work had changed direction. Our focus on Jim coming to terms with his amputations and ‘getting better’ had shifted to coming to terms with the fact that he was dying. Our initial therapeutic goals seemed redundant. Jim began to use the art materials in a more structured, calmer and almost organic way (see Figure 7.4).
He started using colour and his mark-making seemed sensitive and thoughtful, with none of the urgency and secrecy of his early drawings. He no longer seemed to need me to interpret for him in the same way. I wondered if this was because he felt understood and contained – or simply more self-confident. It seemed that Jim had begun to accept the inevitability of his death. By this time, consultants had visited him at home and he knew what lay ahead. He was resolute in his determination to remain living in his flat. There was also a serenity that appeared to come from knowing he was in control, that he had chosen this ending for his life. I felt that Jim’s marked changes in his artworks signified a sense of peace and acceptance.
Figure 7.4 The introduction of colour and structure (see colour plate).
I had to push Jim’s wheelchair into his last session (as it turned out to be), as his energy was so low. His face was jaundiced. He said very little but the silence was comfortable between us. Jim used felt tips for the first time and made slow but confident marks (see Figure 7.5). At the end of the session he said, ‘See you next week then, usual time,’ and wrote ‘11 o’clock next week’ on his drawing. I replied that I hoped to see him then. However, Jim did not attend the following week and died two weeks later.
Conclusion
In health services, the aims of treatment are to improve physical health by decreasing pain and extending life, and/or to increase psychological wellbeing. With homelessness services, one of the goals may be to support someone to move into their own home and be able to sustain it in the long term.
This combination was not enough for Jim. He was a man who had experienced significant loss: of family, of a home, and of where he fitted into society. These losses were compounded by 20 years of homelessness and its cost to his health. Jim did not want to be restricted by other people’s expectations but wanted to live life as he chose. Physical and psychological freedom were important to him.
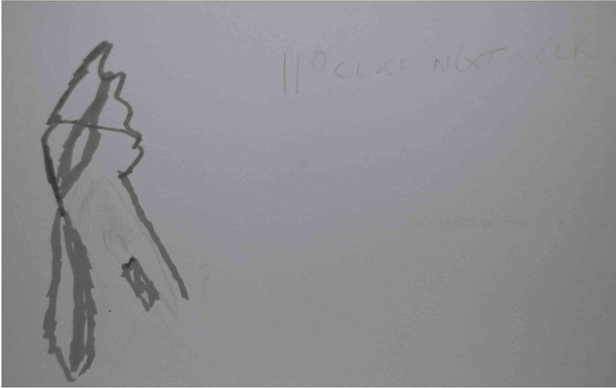
Figure 7.5 Jim’s last image in art therapy (see colour plate).
I believe art therapy provided Jim with the opportunity to examine and explore some of his difficulties and conflicts in a facilitating, supportive environment. It enabled him to find his own way of expressing his thoughts and feelings and to give meaning to them. Although Jim was not able to engage with medical intervention, which might have prolonged his life, he was able to accept the psychological containment that art therapy provided.
Acknowledgements
I would like to thank my colleagues Dr Lisa Reynolds, Consultant Clinical Psychologist and Team Lead, Dr Laura Barrie, Principal Clinical Psychologist, Dr Lynn Steele, Clinical Psychologist, and Sue Wallace, Adult Psychotherapist and Group Analyst, for their help and advice with structuring and editing. Thanks also to Dr Anne Douglas, Consultant Clinical Psychologist, for supervising the piece of work. But my biggest thanks go to Jim for giving me permission to write about his work. It was a privilege to work with him.
References
Arrington, D. and Yorgin, P.D. (2001) ‘Art therapy as a cross-cultural means to assess psychosocial health in homeless and orphaned children in Kiev.’ Journal of the American Art Therapy Association 18, 80–88.
Bentley, A. (1997) ‘The psychological effects of homelessness and their impact on the development of a counselling relationship.’ Counselling Psychology Quarterly 10, 195–210.
Cameron, D.F. (1996) ‘Conflict resolution through art with homeless people.’ In M. Liebmann (ed.) Arts Approach to Conflict. London: Jessica Kingsley Publishers.
Campbell, J. (2006) ‘Homelessness and containment: A psychotherapy project with homeless people and workers in the homelessness field.’ Psychoanalytic Psychotherapy 20, 157–174.
Classen, C.C., Palesh, O.G., and Aggarwal, R. (2005) ‘Sexual revictimization: A review of the empirical literature.’ Trauma, Violence and Abuse 6, 2, 103–129.
Cloitre, M., Cohen, L. and Koenen, K. (2006) Treating Survivors of Childhood Abuse: Psychotherapy for the Interrupted Life. New York: Guilford Press.
Collins, M. and Phillips, J. (2003) Disempowerment and disconnection: Trauma and Homelessness. Glasgow: Glasgow Homelessness Network.
Davis, J. (1997) ‘Building from the scraps: Art therapy within a homelessness community.’ Journal of the American Art Therapy Association 14, 210–213.
Homeless Link (2010) ‘The health and wellbeing of people who are homeless: evidence from a national audit.’ Available at homeless.org.uk/sites/default/files/Health%20Audit%20Findings_National%20evidence_0.pdf. Accessed on 23 August 2012.
Kübler-Ross, E. (1969) On Death and Dying. New York: The Macmillan Company. London: Tavistock (1970).
Nelson Braun, L. (1997) ‘In from the cold: Art therapy with homeless men.’ Journal of the American Art Therapy Association 14, 18–122.
NHS Choices (2012) ‘Complications of amputation.’ Available at www.nhs.uk/Conditions/Amputation/Pages/Complications.aspx. Accessed on 8 June 2012.
O’Connor, J. (2003) ‘Homelessness and the problem of containment.’ European Journal of Psychotherapy, Counselling and Health 6, 111–128.
Saberi, O. (2004) ‘Dealing with grief and depression.’ Available at http://limblossinformationcentre.com/rehabilitation/counselling/dealing-with-grief-and-depression. Accessed on 24 July 2012.
Thomas, B. (2011) Homelessness: A Silent Killer. Sheffield: University of Sheffield and London: Crisis. Available at www.crisis.org.uk/data/files/publications/Homelessness%20-%20a%20silent%20killer.pdf. Accessed on 25 June 2012