CHAPTER 13
In Vitro Fertilization
In vitro fertilization, or IVF, is one of the more invasive forms of infertility treatment; though for many couples it offers the greatest chance for success. If IVF is in your game plan, understanding the basics can make the process a little bit easier. Read on for the essential information you need before starting IVF.
What Is IVF?
Literally translated, “in vitro” means “in the glass” and refers to a procedure done in the lab. When combined with fertilization, as in “in vitro fertilization,” it means that the fertilization of an egg with a sperm cell is done outside of the body and in the laboratory. And that is exactly what IVF is. Your ovaries are stimulated to produce many eggs, which are then surgically removed. They are then combined in the lab with your partners sperm so that fertilization will take place. The resulting embryos are allowed to develop for a few days and a select number are then transferred back into your uterus.

In vitro fertilization is used in fewer than 5 percent of all couples needing the aid of specialized fertility treatments and technologies, according to the American Society of Reproductive Medicine.
IVF was first used in England in the late 1970s. The first “test tube” baby, Louise Brown, was born in England in 1978. This launched a revolution in assisted reproductive technologies, making it possible for more families to conceive than before. Since 1981, in the United States, hundreds of thousands of babies have been born using IVF.
IVF Success Rates
IVF is used in cases that need extreme assistance in getting pregnant. This type of treatment is appropriate for you if:
You have not conceived using other infertility treatments.
You have tubal damage or scarring.
You have missing Fallopian tubes.
Your partner suffers from a low quality or quantity of sperm.
You have unexplained infertility.
The success rates for IVF will vary from fertility clinic to fertility clinic. Overall, the American Society for Reproductive Medicine says that success rates are at about 22.8 percent for using in vitro fertilization, which is about the same rate for a fertile couple in any given month. This number is an average of all of the fertility centers participating in the Society for Assisted Reproductive Technology (SART) reporting.
It is important to note that the range of success for IVF varies widely. Usual quotes on the success rates are about 25–35 percent, though they can be between 0–70 percent. The range depends on a lot of different factors. Some variations are physical — like the reason for your infertility, your hormonal response to medication, and your anatomy. Other reasons for the dramatic differences in success rates depend on the fertility clinic and physician, their knowledge base, and their skill set.
Deciding on IVF
Making the decision to proceed with IVF should not be taken lightly. You should make sure that your calendar is clear for the weeks while you are cycling and that you have the time necessary to dedicate to your care. Anticipate being available for frequent monitoring, and you may need to be out of work at the last minute for your egg retrieval and embryo transfer. It can help if you prepare for these absences in advance; that way you are not as stressed out as if you were in the middle of a big project with an impending deadline.
Make sure that you have all of your medication and have cleared up any insurance issues in advance. Again, knowing that you have everything in order will eliminate some of your stress. Being prepared for the commitment it requires will make the process significantly easier on you in the long run.
Medications
You will need to take a number of medications while going through an IVF cycle. Don't worry though; your doctor or nurse will thoroughly explain your protocol and how and when you take each of the prescribed medications. It is important to take each of them exactly as prescribed by your doctor; not taking certain medications exactly when instructed can potentially ruin your cycle. Don't hesitate to ask any questions you may have; the staff will gladly clear up any confusion you have to ensure that your cycle goes smoothly.
Controlled Ovarian Hyperstimulation (COH)
You will likely need to take a combination of medications to both stimulate your ovaries and suppress your natural hormones. These medications are very tightly controlled to maximize your response while ensuring that you do not get sick. This is why you'll need to be monitored so frequently and why your medication will be adjusted frequently as well.

Check out these helpful video guides to administering your medications: www.ferringfertility.com/medications/trainingguide.asp and www.fertilitylifelines.com/resources/medicationguide.jsp. The makers of Follistim and Antagon also have video guides on their website, www.follistim.com/consumer/index.asp, but you will need to navigate to the specific medication to find the instructional video.
Which suppressive medication you are prescribed depends on your age and diagnosis. Lupron (leuprolide), Cetrotide, and Antagon (Ganirelix) are common choices. You may also need to take a month or two of birth control prior to starting your IVF cycle. Your doctor will make the best decision possible using her clinical judgment.
Once your period starts and your cycle is ready to begin, you'll begin taking your ovarian stimulation, a combination of FSH and LH in the form of injectable synthetic hormones. Brands of these hormones include:
Bravelle
Follistim
Gonal-F
Menopur
Repronex
Pergonal
The purpose of these medications is to help the ovaries produce lots of eggs instead of the usual one. Keep in mind that your doctor will have her own protocols and will tell you exactly how to take the medication. You will take the stimulation medication for approximately ten to twelve days and will likely be in for blood and ultrasound monitoring every morning. Once your follicles are ready, after about ten to fourteen days on average on the medication, you will take a final injection of hCG that will trigger the final maturation of the eggs and prepare them for retrieval.
Hormonal Supplements
Once your eggs are retrieved, usually around thirty-six hours after your final hCG injection, you will need to start a new regimen of progesterone and estrogen supplements to strengthen your uterine lining and prepare your body for the embryo transfer. There are many different forms of progesterone. The most commonly prescribed are vaginal inserts or suppositories, and the dreaded progesterone in oil intramuscular injection. Sometimes, you may be asked to take a combination of both forms of progesterone, again depending on your clinic's policies.

Make sure to ask how your progesterone should be stored, as it varies depending on the form. For example, the injectable progesterone in oil should be stored in a warm dry place, due to the potential of the oil congealing in the cold. On the other hand, the progesterone vaginal suppositories could melt if left out of the fridge.
You may also be asked to take an estrogen supplement to boost your estrogen level. This can take the form of either a pill or a transdermal patch, where the estrogen is absorbed through the skin. Remember, progesterone and estrogen are both the major hormones of pregnancy, which is why your doctor will want to make sure that you have as much hormonal support as possible.
Finally, depending on your clinic's policy, you will most likely need to take your antibiotic and Medrol, usually started around the time of your retrieval. These medications will help boost your chances of implantation.
Egg Retrieval
The egg retrieval, a surgical procedure to remove your eggs from the ovaries, is one of the most anxiety-provoking parts of undergoing IVF. This is particularly true if you've never had surgery before, but rest assured, the procedure is brief and relatively safe. Most clinics will have an anesthesiologist on site that will give you medication to help you relax or even fall asleep. The retrieval itself is only about twenty to thirty minutes long and recovery is usually pretty easy.
Preparing for Surgery
Once the doctor has instructed you to take your final injection of hCG, she will likely give you your preoperative instructions as well. If you will be sleeping during the procedure, you will be asked to refrain from eating or drinking for about eight to ten hours before the procedure. You should wear comfortable clothing and leave all jewelry at home. You might want to consider wearing your glasses that day, if you ordinarily wear contact lenses. Finally, they will give you a time to arrive at the clinic for you procedure. Try to be on time; likely there will be a lot to do to prepare before the surgery.
Make sure to ask about arrangements for your partner to produce his sperm — will he produce at home or at the clinic? Will you need to be with him when he produces? Is there anything you need to do for him to produce at home, i.e., pick up a sterile container? Discussing all of this beforehand ensures that everything will go smoothly on retrieval day.
What to Expect
When you arrive at the clinic, a staff member will escort you to the area where you will be prepped for surgery. You will be given a gown to put on and asked to remove all other clothing, including your underwear. If you are bringing sperm from home or need to be with your partner to produce his sperm, make sure to let the staff know ahead of time. Likely, you will not feel up to participating in his sperm production after the retrieval.
You will meet with both a nurse and the anesthesiologist prior to your procedure. They will both ask you questions about your medical history, allergies, medications you are taking, and other pertinent medical information. Quite likely, they will be asking you similar, if not the same questions. This is not to annoy you, or because they aren't communicating with each other. Rather it is to make sure that they each have the most accurate information possible. The anesthesiologist will also need to start an IV so he can give you medications throughout the procedure.

If you are nervous about becoming nauseous from the anesthesia, tell the anesthesiologist beforehand. They can pretreat you with antinausea medicine before you wake up. The anesthesiologist will also monitor you very closely to make sure that you are not nauseous after the procedure.
You will be escorted to the procedure room and placed into position. Your legs may be placed into the stirrups before you actually go to sleep. Don't worry though, the staff will make every effort to respect your privacy. The embryologist will also meet with you, either in the procedure room or before you go in, in order to identify you and make sure that the eggs are labeled appropriately once they are retrieved.
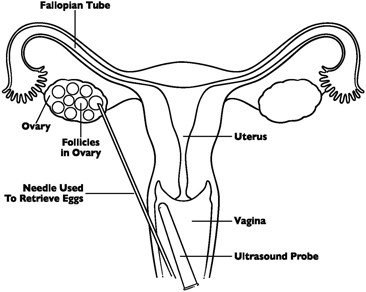
Egg retrieval
Once the procedure room and embryology staff is ready, you will be given medication through your IV to help you sleep or relax. Your doctor will then clean your vagina and cervix and insert the transvaginal ultrasound probe into your vagina. The probe has a needle attached to it. As the doctor is looking at the follicles on the ultrasound screen, he will use the needle to puncture the ovary through the vaginal wall and aspirate all of the fluid from the follicle. That fluid will go to the lab for analysis. Once all of the follicles have been drained, you will be woken up and sent to the recovery room. Most women experience a little cramping after the procedure, which is easily treated by Tylenol as necessary. Once you have fully come out of the anesthesia, you will be given your discharge instructions and discharged home to recover the rest of the day.
Recovery
Recovery after egg retrieval is generally pretty easy. You may have some light bleeding or cramping following the procedure, both of which are entirely normal. You'll want to take it easy the day of your retrieval, but pending your doctor's approval, should be able to go back to work the next day.
Your discharge instructions should include your new medication regimen and any restrictions that you need to follow until your pregnancy test. This may or may not include bathing (don't worry, showering is fine; you just want to avoid sitting in the water), intercourse, and any other activities your doctor wants you to avoid.
Though rare, it is possible to have complications after your procedure. Keep an eye out for any of these symptoms and make sure to let your doctor know if you have any of them:
Severe pain or cramping that worsens over time
Extreme lower abdominal bloating
Fever
Difficulty urinating
A lot of sudden weight gain
Feeling faint or dizzy
If you are not able to get in touch with your physician and are concerned about worsening symptoms after your retrieval, don't hesitate to go to the emergency room. You are always better off getting checked out, just in case.
In the Lab
Once your eggs have been retrieved, they will be given to a trained embryologist who will analyze and count them. By this point, they should also have your partner's sperm, which will then be placed in a Petri dish with your eggs. The dishes will be placed in the incubator overnight and allowed to fertilize. The following day, the embryologist will check the dish to see how many of your eggs actually fertilize to become embryos.
The Role of the Lab
The embryology team is wholly responsible for your embryos at this time. The embryos will be periodically checked to determine how well they are developing and will be assigned a grade to reflect that. This information of course will be given your doctor.

It's not abnormal for less than 100 percent of the eggs to fertilize and become good embryos. This can happen because of several reasons, including the maturity of the eggs, and the quality of the sperm may inhibit fertilization. Sometimes the resulting embryos have a genetic defect that prevents them from further development.
Finally, as the embryos are growing, they will need to be placed in special cultures to ensure that their environment is as similar to that of your Fallopian tubes and uterus as possible.
Are My Embryos Safe?
Rest assured. While every now and again, the story of a mistake makes the news, this is an extremely rare occurrence. The laboratory has a detailed and rigid plan in place for labeling and handling your embryos. In addition, the FDA and Department of Health have set specific guidelines when it comes to how your embryos are managed. Your lab must be periodically inspected by these organizations to ensure that they are complying with the state and federal guidelines. If the lab is found to be deficient, they risk losing their license.
Embryo Transfer
On either the third or fifth day after your retrieval, you will be instructed to come back into the office for your embryo transfer. Which day your transfer is depends on a number of factors that your doctor and embryologist will look at along with your medical history to determine which day is better for you.
On day five after your retrieval, your embryos should have progressed to the blastocyst stage. If your embryos are able to reach that point for transfer, it's generally better because that is the stage that embryos are in when they reach the uterus after fertilizing “the natural” way in the body. This is not always possible, however, depending on how the embryos have developed and your center's policies. Some clinics perform a majority of their transfers on day three; others will be more aggressive in extending embryos toward day five. Whichever day your transfer is, the procedure will be the same.
What to Expect
The procedure is very simple and is similar to having an insemination or pap smear. It's not painful and won't take very long at all. Many clinics will prescribe Valium for you to take approximately thirty minutes before your scheduled embryo transfer. Yes, it will help your anxiety, but this isn't the reason why you're taking it. The Valium is also a smooth muscle relaxant, which means it will help the muscles in your uterus avoid contracting when the catheter is placed through the cervix.
Once you have changed into a gown and have been prepped by a nurse, your doctor will come in and discuss the quality and number of your embryos with you. Quite likely, he'll make recommendations about how many and which embryos to transfer. He will notify the laboratory staff, who will also double check your identity and the number of embryos that are being transferred.
Once the embryos are ready to be transferred, you will be asked to lie back on the exam table and put your legs in the stirrups. A speculum will be inserted into your vagina and the doctor will clean your cervix. While all of this is happening, a sonographer will be looking at your uterus using an abdominal ultrasound. A special catheter will be placed through the cervix and into the uterus. It will then be advanced to the measurement that was taken when you had the special water sonogram before starting your IVF cycle.
The doctor will check the ultrasound to make sure that the catheter is in the correct place, then slowly load the embryos through the catheter and into your uterus. After it is removed, the catheter will be examined under the microscope to ensure that none of your embryos are left in it. Once the all clear is given, the speculum will be removed. You will likely be asked to remain in this position (though covered up) for a short period of time, usually around thirty minutes, and then allowed to head home.
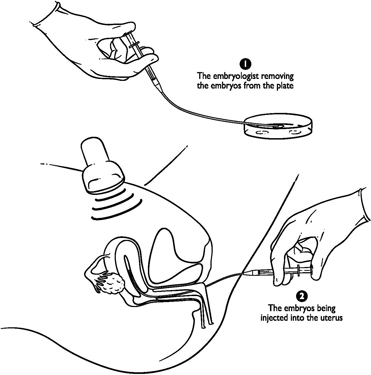
An embryo transfer
After Your Embryo Transfer
Most doctors will ask that you remain on bed rest for one to three days after your transfer to keep your uterus as relaxed and calm as possible. This is thought to facilitate implantation of the embryos into the uterine wall. After your period of bed rest is over, you may be asked to modify your activity and rest as much as possible until your pregnancy test. You should be given detailed instructions about what to avoid and what medications to take after your transfer. You will continue taking the progesterone and estrogen supplements until you know the results of your pregnancy test, but the doctor may need to alter your regimen depending on your hormone levels.

You may feel fluid dripping out after the transfer, but this is just the fluid that was used to clean your cervix. Your embryos will not fall out once you stand up or go to the bathroom. They are safe and sound in your uterus and no amount of activity, even straining to go to the bathroom, can push them out.
Finally, you will be given a date to come back for your pregnancy test. You may be tempted to cheat and take a home pregnancy test earlier then your scheduled date, but don't forget that the hCG you took to prepare you for your egg retrieval is the same hCG that is detected by urine pregnancy tests. You will get a false positive if you test too early!
Assisted Reproductive Technologies (ART)
The beauty of fertility treatments is that the technology is evolving every day. New techniques are being developed to help patients overcome challenges to their fertility that doctors fifty years ago didn't even know existed. Many of these techniques take place in the lab and certainly aren't appropriate for every couple. Your reproductive endocrinologist should let you know which, if any, are in your plan. Many of them do cost extra and may not be covered by insurance. You'll want to investigate this early in the process so you don't get a surprise bill at the end of your cycle.
Intracytoplasmic Sperm Injection, or ICSI
For a long time there was little help available if your partner suffered from oligospermia or other conditions that result in very small numbers of sperm or damaged sperm. Without this sperm, the only treatment readily available was the use of donor sperm. This meant that there was no way for you to have a biological child that was also your partner's biological child. Fortunately, the ICSI procedure now makes it possible to overcome the problems of low sperm count.

The pregnancy rate using intracytoplasmic sperm injection (ICSI) is about 30 percent. This is a consistent rate for a typical IVF cycle. The difference is that these pregnancies are occurring where they previously never would have been possible without the ICSI technology.
Intracytoplasmic sperm injection (ICSI, pronounced “ick-see”) is a procedure in which a single sperm is used to fertilize a single egg. The procedure is done for each egg available after an egg retrieval. The retrieval of the sperm can typically be done under local anesthesia if the specimen can't be obtained by normal collection methods.
To begin the ICSI procedure, you will first enter an IVF cycle. You will be placed on medications that will cause you to begin to produce several eggs at once. As these eggs mature, you will go in for a retrieval of the eggs. During or just before the retrieval, your partner will have his sperm removed via fine needle aspiration through the testicle, by testicular biopsy, or by regular semen collection. The method used to retrieve his sperm will depend upon his diagnosis.
One single sperm is then placed inside a very small glass needle. Using magnification, the egg is visualized and the wall of that egg is penetrated using the glass needle. The sperm is then released into the egg's cytoplasm. This is repeated until either all of the eggs are used or all of the available sperm are used.
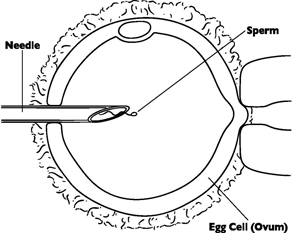
An intracytoplasmic sperm injection (ICSI)
Once the egg is fertilized, it is allowed to continue growing for between two and five days. At this point the egg is transferred back into your uterus using the thin catheter. This is exactly like the regular IVF cycle at this point.

Should we have ICSI even without sperm count issues?
Probably not. Using ICSI for cases other than those for male factor infertility issues and egg penetration issues hasn't been shown to improve pregnancy rates. Since it will add to the cost of your bill, it may be something better left out if it's not something you absolutely need.
The good news about ICSI is that fertilization is now possible with even a “weaker,” less capable sperm. This is one of the best aspects of ICSI for the couples that need this type of technology.
Assisted Hatching
Another technology that may be able to help you conceive is called “assisted hatching.” This can be used if your egg quality is low or there are problems with cellular division of the egg. Not all fertility clinics offer this technology.
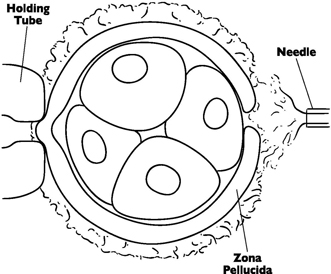
Assisted hatching
With assisted hatching, the egg is fertilized and allowed to develop as it normally would be in IVF. Once you are ready to have the embryos transferred, a hollow tube is used to deliver an acid solution to create a small hole in the shell or zona pellucida; the egg is then transferred shortly thereafter. The hole allows the embryo to hatch out of the zona pellucida, a process that must happen in order for the embryo to implant in the uterus. Some clinics use a weak laser beam to weaken the zona instead of the acid solution. Which technique is used will depend on your clinic and the qualifications of the embryologist.
Cryopreservation
The use of frozen embryos is another area where the technology is growing by leaps and bounds. Typically, in an IVF cycle, the fertilized eggs are used immediately. But there are also reasons that you might choose to freeze the embryos produced for later use.
The freezing of embryos is done for a variety of reasons. It may be done because your doctors have returned as many embryos to your uterus as possible (a number which is determined by many factors) and you have “extra” embryos remaining. You will pay about $500 to $2,000 a year to have the embryos frozen and stored to be available at a later date to be used by you for another pregnancy. In that case, the next time around you could skip the phase of ovarian stimulation in an IVF cycle and simply prepare the uterus for the transfer or return.
You might choose to use the frozen embryo program if you are about to undergo medical treatment for something like cancer that could potentially damage your reproductive system or ovaries. This allows you the option to have your own biological children at a later date when your treatment is completed and you are ready.
While the rates of pregnancy using frozen embryos are slightly less than those of using “fresh” embryos, the benefits are great. You will find that it is a lot less expensive and medically draining to do a frozen cycle. The need for preparation is much less and there is no need for the stimulation or egg retrieval phases of the cycle. This is a huge benefit for many families.
While the whole in vitro fertilization process is long and involved, the changing technology can offer hope to many families who previously could not have children even when you have had previously untreatable problems like severe male factor infertility. Though this technology offers new hope, it is not without pain and side effects and can lead to pregnancy or failure. The emotional aspects should also be considered when considering such an invasive and expensive procedure.