Nutrient data for this listing was provided by USDA Sr-21. Each “~” indicates a missing or incomplete value.
If you’ve been diagnosed with celiac disease, you need to bid farewell to wheat, barley, rye, and triticale (a hybrid grain made from wheat and rye), because a gluten-free diet is the only treatment. But what if you don’t have health issues that stem from ingesting gluten? Why would you voluntarily give up your English muffin or bagel at breakfast, your stromboli or slice of pizza at lunch, your plate of pasta at dinner?
Consider this: Many people have gluten sensitivities that go undiagnosed. Once you eliminate gluten, you may notice that many bothersome or uncomfortable symptoms you’ve simply learned to live with over time have lessened or virtually vanished.
It’s difficult to dismiss the anecdotal evidence from those who never got a formal diagnosis of celiac disease, but—fed up with the cramps, bloating, moodiness, and mental fogginess—eliminated gluten from their diet in a bid to feel better. And many do feel better, physically and mentally. Many also report weight loss, along with more energy, brighter mood, and sharper mental focus. These individuals may in fact have non-celiac gluten sensitivity. If you suspect you have a gluten-related disorder, we strongly recommend you be tested by a doctor before starting a gluten-free diet to ensure you are taking every step to improve your overall health.
The gluten-free movement has exploded in recent years and the Flat Belly Diet Gluten-Free plan only increases its flavor, variety, and satisfaction. (All those yummy MUFAS!) This chapter explains how teaming the two eating styles can not only flatten your belly, but fight disease. But first, it’s essential to understand the main reasons for following a gluten-free diet: celiac disease and non-celiac gluten sensitivity.
Celiac disease affects just 1 percent of the population. But four times as many people have the condition today as compared to the 1950s, according to a 2012 study published in the American Journal of Gastroenterology. In another study published in 2010, researchers found that since the year 1974, the rate of celiac disease has doubled every 15 years. That research estimates that celiac disease may affect as many as 1 in every 133 Americans.
What gives? Why is this “rare” disease on the rise? One hypothesis among several: The grains we eat today are much richer in glutens than they were 70 or 80 years ago.
The bodies of people with celiac disease respond to gluten with a ferocious immune response that inflames the small intestine, damaging the millions of villi that carpet it. Normally, these slender, fingerlike projections that line the small intestine produce digestive enzymes and absorb nutrients. But if you looked at a piece of small intestine with celiac disease under a microscope, you would see flattened, stubby villi. This damage reduces their ability to make digestive enzymes and soak up nutrients.
People with celiac disease don’t always know they have it because they may not feel sick. If they do feel sick (common symptoms include nausea, vomiting and diarrhea, abdominal pain and bloating, unintended weight loss, malnutrition, and anemia), they don’t know celiac disease is the cause. Either way, their intestines are sustaining damage for as long as they continue to eat gluten-containing foods.
But that’s not all. Undiagnosed celiac disease can lead to gastrointestinal cancers and some research has linked it to serious autoimmune disorders such as insulin-dependent (type 1) diabetes. In addition, the nutritional deficiencies that are a hallmark of the disease can precipitate a host of seemingly unrelated problems, including osteoporosis and, in pregnant women, fetal distress. (Low folic acid stores in moms can predispose unborn babies to serious neurological problems such as spina bifida.)
Celiac disease can be masked by—or mistaken for—other conditions, including allergies, colitis, irritable bowel syndrome, diabetes, thyroid disease, and garden-variety stress. Throw in a gluten-related food sensitivity such as lactose intolerance (due to those damaged villi), and doctors often throw up their hands. No wonder it takes an average of 11 years to be diagnosed!
The good news is that dietary changes can soothe your symptoms and reverse the damage that can lead to more serious illness.
If you suspect celiac disease (either because you’re experiencing symptoms or you have a family history of the illness), schedule an appointment with a gastroenterologist pronto. These physicians, who specialize in problems of the stomach, intestines, gallbladder, and bile duct, typically have more experience with identifying and treating celiac and related diseases.
Once diagnosed, the only way to remain disease free is to swear off gluten. Because wheat is the primary source of gluten in the typical Western diet, any food made with wheat—from breakfast cereals to pizza, pasta, and bagels—must go. Fortunately, there are delicious swaps you can make for common gluten-containing ingredients, so you can still enjoy many of the foods you love. You will learn more about those in Chapter 3.
Most of the symptoms of celiac disease disappear within 6 months of totally eliminating gluten, although some people get relief within weeks. Even better news: Research suggests that in 5 years, the risk of intestinal cancers diminishes to match that of the general population.
Celiac disease is genetic—that is, your susceptibility is written in your chromosomes. But the disease isn’t always inherited, and if it is, it can be triggered at any stage of life, from infancy to adulthood, by severe emotional stress, physical trauma, viral infection, pregnancy, or surgery.
The tests for genetic markers don’t tell you if you have the disease; they’re used to rule it out. For a positive diagnosis, the gold standard remains a small-bowel biopsy, in which doctors remove a tiny piece of your intestinal wall to analyze its texture and note any changes related to celiac disease.
Before you sign on for this outpatient procedure, however, you may want to ask your doctor about two relatively new blood tests: the antiendomysial antibody test and the tissue transglutaminase test. Both are designed to reveal the presence of antibodies related to celiac disease in your blood. To use one of the new diagnostic blood tests, you must be consuming gluten at the time of the test, or your results may not be accurate. If you test positive, your doctor will want to follow up with a small-bowel biopsy to make sure.
Some people react to gluten in ways that experts don’t yet fully understand. They show neither the autoimmune reactions that characterize celiac disease nor the allergic responses that typify wheat allergy. They’re in the murky territory of non-celiac gluten sensitivity—one that’s been called a no-man’s-land of gluten-related problems.
Around 18 million Americans have gluten sensitivity, according to estimates from the University of Maryland’s Center for Celiac Research. There’s no official test for gluten sensitivity. Once your physician has determined that you do not have celiac disease or a wheat allergy, the next step is a gluten-elimination diet to see if symptoms resolve.
While some doctors have dismissed gluten sensitivity as an “all in your head” malady, there’s compelling evidence that it’s all too real. A recent University of Maryland study found that not only does gluten sensitivity exist, but it’s also quite different from celiac disease—at least, in terms of how it works in your body.
In this study, a team led by Alessio Fasano, MD, looked for differences in immune reactions between people with celiac disease and people with gluten sensitivity. They conducted a series of lab tests and intestinal biopsies on 100 subjects in both groups, which revealed key physical differences: For one thing, people with gluten sensitivity generally don’t have the damage to the small intestine that those with celiac disease have, nor do they have the specific markers in the blood used to diagnose celiac disease.
Researchers found that, compared to people with gluten sensitivity, those with celiac disease had a more severe immune response to gliadin, the toxic protein in gluten. This was indicated by higher levels of intestinal permeability, a condition in the GI tract that can lead to inflammation. In people with celiac disease, gliadin crosses the barrier between cells in the intestine, and the body attacks itself against what it sees as an invader: gluten.
While gluten sensitivity doesn’t damage the intestine as celiac disease does, it can have a profoundly negative impact on physical, emotional, and mental well-being. Common symptoms include abdominal pain similar to irritable bowel syndrome, headaches, tingling, fatigue, muscle pain, skin rashes, and joint pain.
Your belly is bloated, and you’ve got wicked stomach cramps. Or you’re so fatigued, irritated, or mentally foggy you can’t function. Your skin is breaking out, you’re wheezing at work (but only at work), or you’re unsteady on your feet.
Are you allergic to wheat? Do you have celiac disease or gluten sensitivity? Something rarer? More often than not, diagnosis and appropriate treatment can be a crapshoot. A recent proposal authored by heavyweights in the field of celiac disease aims to end that confusion. A group of 15 experts from seven countries is proposing a new classification system for the gluten-related disorders plaguing an increasing number of people worldwide, for reasons still unknown. The proposal (funded in part by a manufacturer of gluten-free products in Italy) defines a spectrum of illnesses based on the three kinds of immune defenses the human body mounts against gluten.
Allergic reactions. Symptoms occur minutes to hours after exposure to gluten, which could involve eating or breathing in wheat (the latter is known as baker’s asthma). Allergic reactions can affect the skin, gastrointestinal tract, or respiratory tract, and symptoms can include hives, nasal and chest congestion, nausea, vomiting, and anaphylaxis.
Autoimmune reactions. Symptoms occur weeks to years after exposure to gluten. This category includes celiac disease; dermatitis herpetiformis; and gluten ataxia, which affects brain tissue, resulting in an unsteady gait and lack of motor control. Gluten may be the cause of ataxia in one-fifth of all those with the ailment, the report notes.
Immune-mediated reactions. Symptoms occur hours to days after gluten exposure. This category would include gluten sensitivity, in which people report the same symptoms as celiac disease, plus foggy thinking and mood swings, but test negative for telltale antibodies.
The proposal also spells out diagnostic criteria to help doctors determine which disorder their patients may have, if any, as well as specific treatments. Hopefully, gluten-related health problems will be caught more quickly, so the healing can begin.
Eliminating wheat and gluten can result in a “snack gap”—suddenly, there are no cookies, pretzels, crackers, or snack bars. But, if you’re eyeing stomach-friendly versions of these items in the gluten-free section of your supermarket, think twice before you buy. “Gluten free” doesn’t always mean “healthy.”
Gluten gives our favorite foods that special touch: It makes pizza dough stretchy, gives bread its spongy texture, and is used to thicken sauces and soups. Without it, food companies are forced to add extra fat and sugar to make up for the lack of texture and flavor. Previous studies that have analyzed the nutrient composition of packaged gluten-free products have found that these products tend to have high levels of fats (including unhealthy trans fats), sugars, and salt. What these packaged foods don’t typically offer is fiber, which is essential to helping you maintain a healthy weight.
Other research has shown that people with celiac disease tend to compensate for the restrictions of a gluten-free diet by eating foods high in fat, sugar, and calories. Not surprisingly, they also consume excessive amounts of total and saturated fats overall. Not great for their health—or their waistlines, either.
Gluten-free foods tend to be pricier, too. (Six bucks for a box of cookies or crackers? Seriously?) Our suggestion: Enjoy gluten-free snacks as an occasional treat. But more often than not, opt for foods that are naturally gluten free, like those on the Flat Belly Diet Gluten-Free plan.
Gluten-free eating and the Mediterranean-inspired Flat Belly Diet are two great plans that taste great together. Both center on whole foods, deliver ample amounts of vital nutrients, and allow generous amounts of carbs from gluten-free grains, potatoes, and other natural foods. (And yes, you get dessert!) Combine the two eating styles, and you’ve got a plan that will peel off pounds—and belly fat—as it reduces your risk of diabetes, heart disease, and other maladies. If you have celiac disease or are sensitive to gluten, you’ll likely find relief from your symptoms as you drop weight.
Although the core of the Flat Belly Diet Gluten-Free plan is those delicious, flavorful, and oh-so-satisfying MUFA foods, you’ll be eating more (a lot more!). Here’s a summary of the plan’s building-block foods, which help you lose weight and protect your health.
Nutrition experts have long recommended that we swap refined carbs made with white flour for whole grains, and for good reasons. Whole grains are naturally low in fat, cholesterol free, and good sources of protein, fiber, minerals, vitamins, and other nutrients. And it has been well established by the scientific community that diets rich in whole grains are linked to a reduced risk of cardiovascular disease, diabetes, and some cancers.
Normally, when you think of whole grains, you think of wheat. But guess what? Gluten-free grains, also known as ancient or alternative grains, are also whole grains. (Technically, some are actually grasses, but you prepare and eat them like grains.) Historically, rice, corn, and potato were substitutes for grains that contain gluten. Today, other grains such as amaranth, buckwheat, flax, millet, teff, and quinoa offer more variety, nutrition, and flavor.
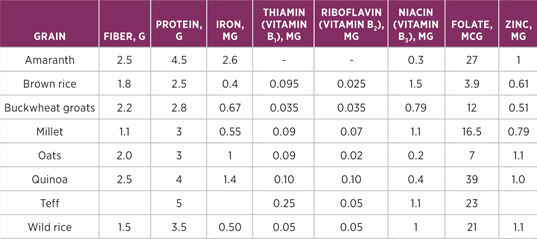
Ancient grains like amaranth, millet, and quinoa are often a richer source of nutrients than modern grains. For example, quinoa has been called a super-grain, because researchers have found that it can contain up to 50 percent more protein than common grains and higher levels of calcium, phosphorus, iron, and B vitamins. (See the “Nutrient Content of Common Gluten-Free Grains” chart.) Gluten-free whole grains are also good fiber sources. That’s excellent news, because research has found that gluten-free diets often run low in fiber.
You’ll find alternative grains in the organic section of your supermarket or in natural foods stores. They’re typically cooked and used like white rice and/or ground into flour. Their names may be unfamiliar to you, but humans around the world have been eating them for, well, forever. Amaranth and quinoa were the staple foods of the mighty Aztecs and Incas, respectively. Once the food of warriors, these grains now help us fight the diseases of modern civilization, obesity included. When you buy these grains at the store, you must ensure the packaging is labeled “gluten free” to avoid cross-contamination. For this reason, avoid buying from bulk bins.
(per ½ cup serving, cooked)
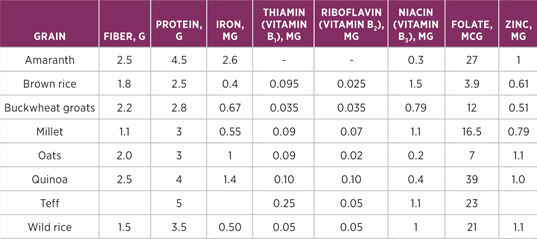
Nutrient data for this listing was provided by USDA Sr-21. Each “~” indicates a missing or incomplete value.
Wondering what they taste like and how to cook them? You’ll find the answers in Chapter 3—check out our cheat sheet to help you get familiar with the many exotic (and delicious!) varieties, including preparation methods and serving suggestions.
MUFA-rich foods such as walnuts, flaxseed, and olive and canola oils deliver a double dose of healthy fats: They’re good sources of omega-3 and omega-6 fatty acids (fatty fish, too—see below). Among the benefits of these good fats:
They fight inflammation. Omega-3s cool chronic inflammation in the body, a major contributor to numerous chronic conditions, including insulin resistance and diabetes. Omega-6s suppress production of inflammation-related compounds, according to the American Heart Association. (The AHA recently recommended adding some omega-6s to our diets. While omega-6s have been demonized as a cause of inflammation, if you eat omega-3s and omega-6s in balance, both are beneficial.)
They reduce heart disease risk. A study at the Harvard School of Public Health found that women with diabetes who ate fish just once a week had a 40 percent lower risk of dying from heart disease than did women with diabetes who rarely ate fish.
You’ve no doubt heard about the heart-protecting powers of the omega-3 fats found in fatty, cold-water fish like salmon and mackerel (as well as in fish oil capsules). Worried about toxins in fish? It’s true that fatty fish like salmon can accumulate chemical pollutants such as PCBs in their fat and skin, while leaner fish such as tuna can accumulate mercury in their flesh. But don’t shy away from fin food—you need the good fats! To minimize your risk, eat two fish meals a week, eat a variety of fish, and favor types with lower levels of toxins, such as wild salmon (available in cans at the grocery store as well as in pricier fillets at the fish counter), mackerel, and herring.
Getting some of your omega-3s from walnuts, ground flaxseed, and flaxseed oil may help, too. These contain alpha-linoleic acid, which your body converts into the more potent omega-3 DHA, the type found in fish and fish oil capsules.
If you enjoy dining out or are an on-the-run eater, Flat Belly Diet Gluten-Free has the flexibility and variety you need to stay on plan, whether you’re at the local diner or the best bistro in town. While people with celiac disease, wheat allergy, or gluten sensitivity will need to be on their game when it comes to what they order and how it’s prepared, a few basic guidelines can simplify the process.
Do some restaurant research. Before you go out, go online to look at restaurant menus and find meals that follow the guidelines we’ve set out in this book. Better yet, use the Internet to find local restaurants that accommodate their gluten-free patrons. (It might be easier than you think—there are entire Web sites devoted to cataloging gluten-free hot spots! We have listed a few in our Resources.)
Plan ahead for special events. If you are attending a party at someone’s home and are unsure of the menu, prepare and bring a dish to share that you know you can eat. If the party is at a restaurant or hotel, call the chef or food service manager for information about the menu. Ask if there is a gluten-free menu or whether you can request a special meal. You’ll have more success if you call several days to a week in advance. Once you arrive at the party, confirm that your special meal is being prepared and let the kitchen staff know where you are seated.
Get assertive and proactive. Even small traces of gluten will cause cross-contamination—such as bread crumbs that accidentally come in contact with gluten-free food prepared on the same surface or with the same utensils. Be sure to tell the server or chef that it’s important to use extra care in preparing and serving your food.
If you get a salad with croutons, send it back and ask for a fresh-made salad to avoid getting the same salad with the croutons picked off. If you don’t trust the chef, restaurant, or party host or hostess to deliver a safe, gluten-free meal, eat something at home beforehand and order a beverage, fruit plate, or another safe alternative.
Rely on a safe bet. You can always order a salad of leafy greens and raw veggies, topped with pan-grilled chicken or salmon, and drizzled with olive oil and balsamic vinegar. Add a fist-size serving of one of the following: baked or roasted red, white, or sweet potato; brown or wild rice or a starchy veggie such as beans, peas, or corn. This meal should keep you within your calorie budget and contains a MUFA. Or follow the guidelines for building your own Flat Belly Diet Gluten-Free meal (see Chapter 1).
Since one of the goals of Flat Belly Diet Gluten-Free is to reduce the amount of saturated fat you eat, we recommend lean protein, such as skinless poultry, beans, and lean and well-trimmed cuts of beef and pork. (And eat your fish, too!) Here’s what lean protein has to offer:
A weight loss advantage. The more muscle you have, the more calories your body burns around the clock. Losing muscle, in contrast, slows your metabolism. Protein contains the amino acid leucine, which helps preserve more muscle while you diet. In a recent study of 48 overweight women dieters, those who ate more protein lost 20 percent more weight than those on an equal-calorie, highercarb plan, and most of their loss was body fat, not muscle.
Fiber—in meatless protein. You’ll enjoy beans several times a week on our plan; they’re a good source of soluble fiber, the type that helps control blood sugar. And some varieties, like navy beans and lentils, are also packed with a type of fiber called resistant starch. Because it breaks down extremely slowly in your digestive system, it slows the absorption of sugar into your bloodstream, keeping you fuller longer and protecting you from the physical and emotional ups and downs of a blood sugar spike.
Healthier blood sugar levels. Researchers at the University of Minnesota tested two diets, one high in protein and one with only half as much. The fat content was the same in both diets. In the group that followed the high-protein diet (which was also lower in carbs) for 5 weeks, A1c levels—a test of long-term blood-sugar control—fell by nearly 1 full point, a significant improvement.
This plan’s five to eight servings of fruits and vegetables a day are critical for flattening your belly, losing weight, and controlling your blood sugar. Here’s why:
They chill systemwide inflammation. Low-level inflammation interferes with the absorption of blood sugar by scrambling signals meant to tell cells to carry sugar molecules inside. But produce cools off inflammation. In a Harvard School of Public Health study of 486 women, those who ate the most produce had the lowest levels of C-reactive protein, a marker of chronic inflammation. Those who ate the most fruit were 34 percent less likely to have metabolic syndrome; those who ate the most veggies cut risk by 30 percent.
They’re fiber-full. Fiber fills you up, slows digestion, and slows the release of glucose into your bloodstream. For the most part, fruits and veggies have a low glycemic load, a term that refers to how fast and how high carbs boost blood sugar. Including produce at every meal helps slow the rise in your blood sugar afterward. (So do the fats you eat and protein.)
They safeguard your heart. A diet full of fruits and vegetables cuts the risk of heart disease by 28 percent and stroke by 20 percent. One reason: Many fruits and veggies are rich in pectin, a type of water-soluble fiber that helps lower levels of “bad” LDL cholesterol.
We hope you’re convinced that you’ll enjoy plenty of heart-satisfying food on the Flat Belly Diet! Gluten-Free plan. (And we really hope you dig into the grains listed on this page. Their flavor can’t be beat and they are far more nutritious than plain old white rice.) Moreover, feel free to make those reservations—you’ll find plenty to keep you satisfied and on-plan at virtually any eatery (we’ve listed some sites to find gluten-free dining options in our Resources section).
Our point: All diets that rein in calories can lead to weight loss, but not all diets can do so deliciously and in ways that actually benefit your health. Flat Belly Diet Gluten-Free goes beyond weight loss. It actually targets belly fat, which is strongly implicated in inflammatory processes associated with just about every chronic disease.
If you’re a gluten-free veteran, you’re bound to find Flat Belly Diet Gluten-Free one of the most delicious, satisfying, and effective weight loss plans you’ve ever tried. If you’re a gluten-free newbie, add “easy” to that list of adjectives. We’ve tried to make gluten-free eating as simple as it is tasty and healthful. Stick to the plan, and you’re on your way to a slimmer waistline, healthier blood sugar and cholesterol numbers, boundless energy, and a brighter mood. What you gain is even more important than what you lose. As you shed belly fat, you bolster your health and vitality. Within a few weeks, you’ll look slimmer and feel better—all with three mouthwatering meals and two yummy snacks a day!
Of course, maybe you just want to flatten your belly so you’re happy with what you see in the mirror. Fine with us! But you’ll be healthier, too—and that makes us happy. In the next chapter, you’ll take the science behind gluten-free and Flat Belly Diet eating and apply it in the place where all of the plan’s benefits begin: your kitchen.
If you have been diagnosed with celiac disease or another gluten-related health condition, it’s essential that you completely eliminate the foods below. As you can see, the lion’s share is wheat and its many varieties of flour.
Keep in mind that wheat is the primary source of gluten in our diets, and that includes many processed foods. For a comprehensive list of foods you need to look at twice, see “Sneaky Sources of Gluten.”
Wheat
Spelt
Einkorn
Emmer
Kamut
Durham
Triticale
Bulgur
Semolina
Couscous
Faro
Wheat bran
Wheat starch
Wheat germ (only trace amounts are safe)
Barley
Barley malt/Barley extract
Brewer’s yeast
Rye
Oats (unless labeled “gluten free”)