

Modern firefighters are trained in the assessment and treatment of life-threatening conditions sustained by the public they serve. They are responsible for stabilizing the scene of an accident or emergency situation and performing basic first aid procedures, as well as assisting prehospital providers. Patient assessment and basic medical treatment is essential to the role of the firefighter. Upon the arrival of the ambulance, firefighters will transmit valuable information to emergency medical technicians (EMTs) and paramedics concerning the patient’s condition, chief complaints, and any medical assistance that was administered prior to their arrival. Today’s firefighter is truly a multifaceted, lifesaving professional.
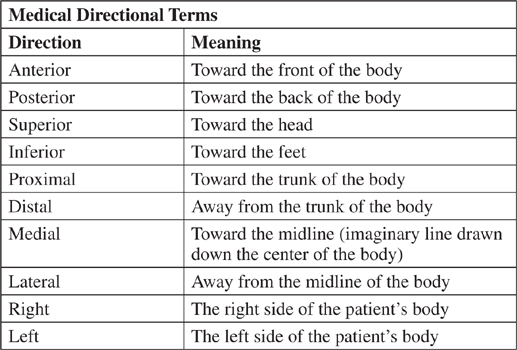
The human body is divided into areas with which firefighters should be very familiar. A working knowledge of these will aid the first responder to isolate the part of the body that is injured or that is giving the victim the most pain. It will facilitate providing treatment and communicating information to incoming medical personnel. The diagram shows the major areas of the human body.
The fire department is often the first agency to arrive at incidents where people are injured. Firefighters therefore should know the basic anatomy or structure of the body in order to communicate medical information to medical professionals (EMS) who will arrive subsequently.
When firefighters arrive at the scene of an accident or medical emergency, they must perform an initial assessment of the patient’s status. A general overview of the patient entails evaluating the scene to determine whether you are dealing with a trauma situation (injury sustained from a violent impact or sudden force) or a medical condition. If you are responding to the scene of an auto accident, you can assume that the patient(s) will be suffering from trauma injuries. Conversely, arriving at a patient’s home and noticing pills or drug paraphernalia on the kitchen table would most likely indicate you have a person with a medical or drug problem. Other general conditions to consider are the patient’s age and gender. Look for clues concerning the condition of the victim when you arrive on the scene. Is the person bleeding? Does the victim have contusions or abrasions that commonly result from trauma? Are there obvious deformities to the extremities, shoulders, or pelvis area that could indicate that the victim is suffering from a dislocation or bone fracture? Palpate or feel the patient’s body to search for irregularities (swelling, depressions, or tenderness). Also, utilize your sense of smell to ascertain if the victim has been drinking alcoholic beverages or has been poisoned. The first responder should also check the victim’s vital signs (respirations, pulse, temperature, pupils, and blood pressure) to obtain an accurate assessment of the patient’s condition.
The CUPS status assessment criteria may be used by first responders to determine the seriousness of the patient’s injury or illness. Victims considered in critical condition are receiving cardiopulmonary resuscitation (CPR), in respiratory arrest, or requiring and receiving life-sustaining ventilation/circulation support. Unstable victims are unresponsive to external stimuli or responsive but unable to obey commands. They also may exhibit difficulty breathing. Indications that a patient is going into shock (pale skin/rapid breathing), uncontrolled bleeding, and severe pain in any area of the body would warrant being classified as potentially unstable. People with minor injuries and illnesses would be determined to be in stable condition.
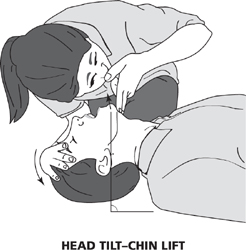
Assessing the vital signs of a victim is an essential way to monitor the functions of the body and discover abnormalities. Evaluating the information gleaned from a patient’s vital signs dictates the kind of treatment the firefighter will administer while awaiting the arrival of medical professionals.
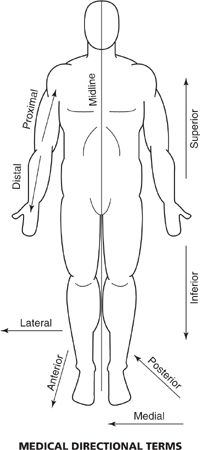
Measure the rate of breathing for 30 seconds. Count the number of breaths for this time frame and multiply by two to get the number of respirations per minute. The normal rate of breathing for adults is between 12 and 20 breaths per minute. Infants and children have a faster normal rate of breathing (20 to 30 breaths per minute). Observe the chest and abdomen for abnormal depth (deep or shallow) and pattern (irregular sequence) of breathing. Abnormalities can indicate brain trauma or difficulty breathing. Listen for any unusual sounds (wheezing, snoring) while the patient is breathing for indications of asthma, bronchitis, or airway obstruction.
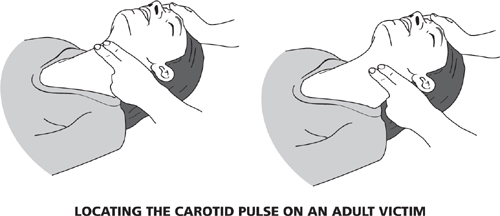
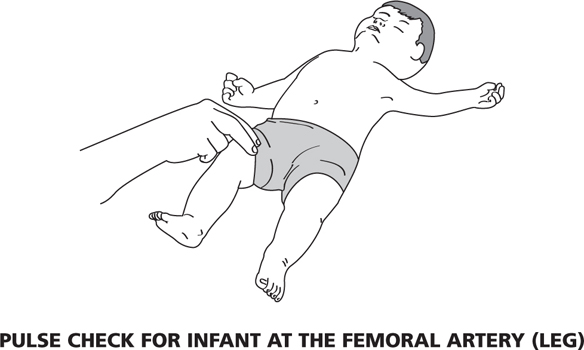
The pulse is the expansion and contraction of the body’s arteries as blood flows away from the heart. It is an indicator of the function of the patient’s circulatory system. It is measured by palpating (touching) an artery located close to the skin. Common arteries used by first responders to evaluate pulse rate, rhythm, and quality are the carotid (in an unresponsive adult or child), brachial (in a child or infant), radial (in an adult or child), and femoral (in an unresponsive child). Measure the pulse rate by counting the number of impulses or beats for 30 seconds. Multiply by two the number of beats for this time frame to ascertain the pulse rate per minute. The normal pulse range for adults and adolescents is approximately 60 to 100 beats per minute. Younger people tend to have higher normal pulse rates (80 to 130), while newborns have normal pulse rates from 120 to 160. The rhythm of a pulse is either regular or irregular, which directly reflects the functioning of the heart. A pulse’s quality can be normal, bounding (thumping), or vaguely detectable (thready). A bounding pulse could mean the victim has high blood pressure, while a thready pulse rate may indicate cardiac arrest or shock.
Use the posterior (back) surface of your hand on the patient’s forehead or side of the face to assess general body temperature. Also note the relative moisture on the skin. Findings can range from hot and dry, which can indicate heat stroke, to cold skin (hypothermia).
The pupil is the center, dark part of the eye. It normally changes diameter in relation to the amount of light to which it is exposed, constricting (shrinking) under bright light and dilating (expanding) in the absence of light. Constricted pupils in a dark area or dilated pupils in a well-lighted room can indicate that the victim is under the influence of drugs or has been poisoned. Pupils of unequal size are associated with head injuries, stroke, or damage to the eye, as are nonreactive pupils that do not react to a beam of light directed into the eye of the victim by a first responder’s penlight.
Blood pressure is a measure of the force the blood exerts on the walls of the arteries. It provides a functional status indicator of the heart and blood vessels. A victim’s blood pressure is commonly recorded using the auscultation method (a stethoscope and blood pressure cuff, referred to as a sphygmomanometer). Blood pressure is denoted by two numbers in fractional form (the systolic blood pressure number over the diastolic blood pressure number). The systolic number is the pressure when the heart is contracting (pumping) blood through the blood vessels. The diastolic number is the pressure in the blood vessels when the heart is relaxed and not pumping blood. A first responder can use the auscultation method by placing the blood pressure cuff around the patient’s brachial artery just above the elbow. The brachial artery is palpated and then the stethoscope is positioned over the brachial pulse point. Next, air is pumped into the cuff using its squeeze bulb until the gauge on the cuff stops rising and falling, usually between 150 and 200 mmHg (millimeters of mercury). Listen for brachial pulse sounds through the stethoscope. At 150 to 200 mmHg, brachial pulse sounds tend to disappear. This is the time to slowly release air from the cuff and begin listening for audible brachial pulse sounds. Read the gauge when the pulses are first heard, this is the systolic blood pressure number. Read the gauge again when the pulse sounds stop, this is the diastolic blood pressure number. Normal blood pressure for adults varies with age. It is generally in the range of from 100–150 over 60–90. The normal blood pressure range for children is from 100–130 over 60–80. High blood pressure can indicate hypertension and is associated with cardiovascular disease, kidney malfunction, stroke, and drug use. Low blood pressure can indicate hypotension and may be the result of shock.
Another important procedure is to evaluate how alert the patient is to exterior stimulus. Is the patient conscious, semiconscious, or unconscious? If the patient is conscious, is he or she in an oriented or disoriented state? Does the patient know her name, where she is, and what happened? Can the patient communicate to you his or her chief complaint? If the victim is semiconscious, what type of stimulus (verbal or touch) gets a response? An unresponsive person is considered unconscious. Tapping the victim’s shoulders or chest, rubbing the breast bone (sternum), or pinching the muscles of the neck are common physical ways to assess responsiveness. Your ability to gather valuable medical information from the patient will depend on the response status of the individual you encounter.
Emergency medical care must first focus on establishing the patient’s airway, breathing, and circulation.
The patient’s airway can initially be assessed by responsiveness. In general, a person who can readily communicate to you his or her chief complaint can be considered to have a clear airway. A patient having trouble talking and/or breathing can be assessed as having a partially obstructed airway. Encourage the patient to cough in an attempt to dislodge the object. If the object is not expelled, the person should be transported via EMS to the nearest medical facility.
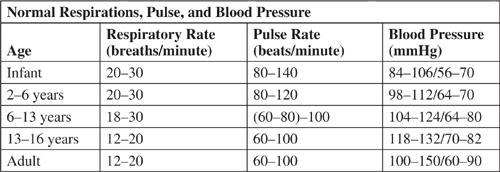
In unresponsive adults and children where there is no sign of trauma, firefighters should have them placed on their back (supine) and open the airway performing the head tilt–chin lift technique. It is applied from the side of the victim by placing one hand on the patient’s forehead to tilt the head back while lifting the jaw forward with your fingers.
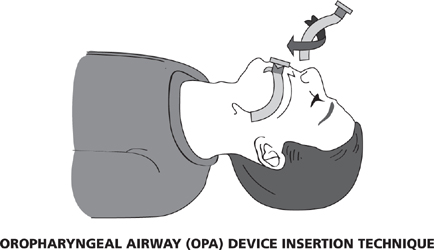
An airway obstructed by fluid should be cleared using a suction unit with attached catheter that is placed inside the victim’s mouth. Mucus, vomit, and fluid are cleared from the mouth using a negative pressure through the catheter. An oropharyngeal airway (OPA) device is used by first responders to maintain an open airway on an unresponsive patient once it has been established. The OPA is a hard plastic, C-shaped device positioned into the mouth of the patient using a twisting (rotational) action to move the tongue forward. Sizes vary to fit infants through adults.
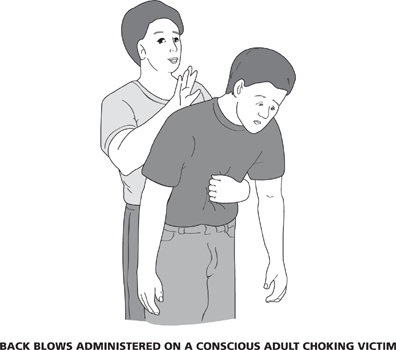
For conscious adults and children with a completely obstructed (solid foreign object) airway, showing signs of choking (inability to speak, breathe, or cough), position yourself behind the victim, support the victim with one arm around the waist or shoulders and deliver five back blows with the heel of your hand. Your hand should land right between the shoulder blades.
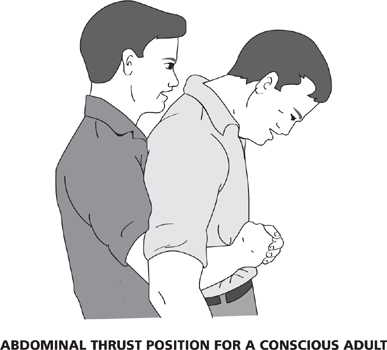
If the back blows do not dislodge the foreign object, remain in your position behind the victim and place your fist with the thumb-side just above the navel and the second hand atop the first. Apply five quick inward and upward abdominal thrusts. Continue sets of five back blows and five abdominal thrusts until the object is dislodged, the victim can cough or breathe, or the person becomes unconscious.
In an unconscious adult or child with an airway completely obstructed by a visible foreign object, the firefighter should open the airway using the head tilt–chin lift and finger sweep the mouth on a supine victim in an attempt to remove it. Check for normal breathing. If unsuccessful, start cardiopulmonary resuscitation (CPR).

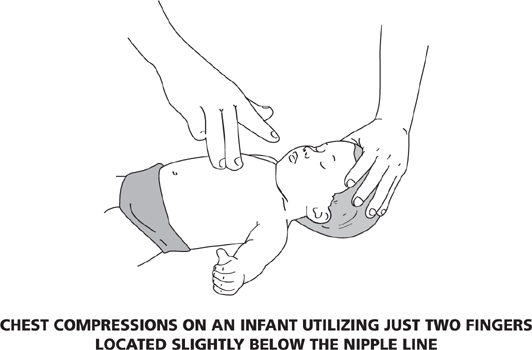
Opening the airway of an infant is handled differently. Infants have larger heads in comparison to the rest of their body which can cause the airway to be closed off should the head be tilted back. A hand beneath the shoulders while the victim is in the supine position will help keep the airway open. If the airway is obstructed, try to remove a visible foreign object from a conscious infant using a finger sweep. If the foreign object is not visible, place the infant face down (prone) on your arm while cradling the face with your hand. Five back blows are then firmly given with the heel of one hand to the middle of the back between the shoulder blades. The infant is then shifted to a supine position on the forearm and five rapid, downward chest thrusts are given, just below the nipple line, using just two fingers. Check for breathing. Repeat these techniques until the object is removed or the infant becomes unconscious. If the infant becomes unconscious, stop giving back blows and chest thrusts and start CPR.

To remove a visible foreign object from the airway of an unconscious infant, place the baby on your forearm face up with your hand supporting the back of the head. Use the head tilt–chin lift to open the airway and look for an obstruction. If visible, remove using finger sweep. Check for breathing. If the victim is not breathing, start CPR.
The use of the look, listen, and feel method is a simple way to determine the patient’s breathing status. Look to see if the person is struggling to breathe. Is the patient breathing very quickly or slowly? When encountering an unconscious person, check to see if the chest of the victim is rising and falling. Check the color of the skin. Blue-gray color around the mouth and the end of the fingers is usually attributed to a lack of oxygen to the body and respiratory distress. Listen to the victim. Put your ear next to the victim’s nose and mouth and listen for the sounds of breathing, if the person is unconscious. If the person is conscious, is he or she able to communicate difficulty in breathing? Is the patient experiencing loud, labored breathing? In an unconscious victim, feel for breathing by placing your hand on the chest to check for movement. Place the side of your head next to the victim’s mouth and feel for any air movement against your cheek. A victim who is not breathing requires the administration of positive pressure ventilation (PPV) methods or rescue breathing.
First responders frequently utilize a combination fixed-flow inhalator (for patients who are able to breathe with difficulty) and mouth-to-mask rescue breathing resuscitator oxygen unit (for patients who are not breathing) to provide supplemental oxygen to victims having difficulty breathing or forced ventilation to those who are not breathing. Cylinders typically provide 20 to 60 minutes of oxygen to the patient depending on how the unit is being used.
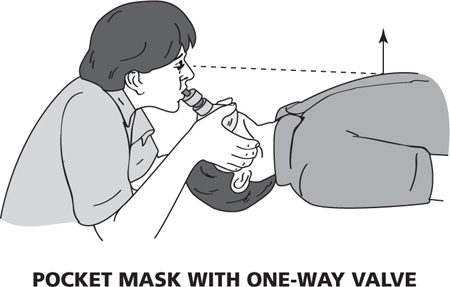
A common and relatively safe rescue breathing method performed today by firefighters is known as mouth-to-mask ventilation. The transparent plastic pocket mask used has a one-way valve that provides a barrier that can prevent the transmission of communicable diseases between the victim and the first responder. The valve diverts the patient’s exhalations. It also allows the firefighter to create a tight seal around the patient’s nose and mouth in order to perform effective rescue breathing.
The first responder takes a position at the top of the victim’s head as shown in the diagram, maintains an open airway, and places the pocket mask over the victim’s nose and mouth. The firefighter then places his or her mouth over the mouthpiece of the pocket mask. The firefighter breathes slowly into the mouthpiece, causing the victim’s chest to rise visibly. The firefighter then allows the victim to exhale by removing his or her mouth from the mouthpiece.
Another rescue breathing method utilizes a bag-valve-mask device. The bag-valve-mask is made of soft, collapsible plastic and can be used to provide air forcibly to the victim with or without supplementary oxygen attached. All of these rescue breathing devices and equipment are used in conjunction with an OPA.

Rescue breathing is also known as artificial respiration. First responders should administer rescue breathing when a victim stops breathing and becomes unconscious. Administering rescue breathing greatly increases the probability of recovery without permanent brain damage from the lack of oxygen. Position the victim on his or her back and tilt the head back slightly (if there is no obvious head or neck injury) to open the airway. Check for possible obstructions in the airway and that the victim is, in fact, not breathing before performing rescue breathing. Pinch the victim’s nose shut gently to negate ventilation leakage and lift the chin prior to giving rescue breaths. Take a normal breath before giving mouth-to-mask ventilation while checking to see if the victim’s chest rises.
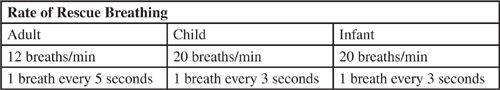
Blowing slowly but firmly, give one breath every five seconds for an adult. Wait five seconds, then repeat the breath and check the victim’s pulse. If there is no pulse, you will have to perform cardiopulmonary resuscitation (CPR). Otherwise, keep breathing into the victim every five seconds until he or she is able to breathe unassisted. For children and infants, give two slow breaths into the victim’s mouth or mouth and nose (infant). Deliver rescue breaths every three seconds for a minute. After one minute, stop and check for pulse and breathing for approximately five to ten seconds. If there is no pulse, you will have to perform CPR.
Assess the patient’s circulation by checking for bleeding, pulse rate, and skin color. Analyze the scene to see if the patient is bleeding heavily (hemorrhaging). Uncontrollable bleeding is potentially life threatening. Is there a pool of blood on the ground? Are there bloodstains on the victim’s body, hair, or clothing? Check the back of the victim for the possibility of hidden blood. The loss of large amounts of blood can also cause the victim to go into shock. A shock victim may exhibit pale skin color. The patient’s skin color also reflects the status of the circulatory system. Bluish (cyanotic) skin indicates a restriction of oxygen to the living tissues and organs of the body.
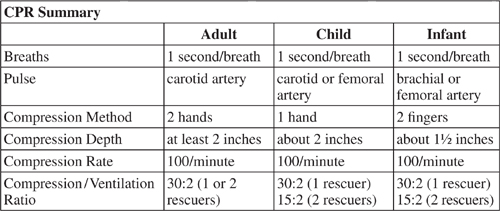
The pulse rate is commonly taken at one of the four arteries listed in the table “CPR Summary” and shown in figures later in this section, dependent on whether the victim is responsive or unresponsive and his or her age. Determine if the pulse rate is regular or irregular, fast or slow, weak or strong. A patient without a pulse requires the first responder to start CPR.
CPR should be administered by first responders on victims of cardiac arrest (lacking a pulse and not breathing). It is used to promote blood flow (compressions) and provide oxygen (ventilation) to the body’s heart and brain. When blood stops circulating, oxygen cannot be transported to the body’s vital organs and tissues. Without oxygen for four to six minutes, brain cells begin to die.
Ensure that unresponsive adults and children with no sign of trauma are positioned supine on the ground. Use the head tilt–chin lift technique to open airway. Rescuers place themselves on their knees at opposite sides of the victim to administer CPR.
The American Heart Association (AHA) now recommends that chest compressions be the first step for rescuers to revive victims of sudden cardiac arrest. Therefore, the acronym C-A-B for compressions-airway-breathing is used when performing CPR. During the first few minutes of cardiac arrest, victims will have oxygen still remaining in their lungs and bloodstream. All victims in cardiac arrest, however, will require chest compressions to pump oxygenated blood to the brain and heart. AHA research has shown that rescuers who started CPR with opening the airway took much longer (30 seconds) to begin chest compressions than rescuers who began CPR with chest compressions.
C-A-B entails starting compressions within 10 seconds of recognition of a cardiac arrest. Compressions are at a rate of at least 100 per minute with a depth of at least two inches for adults, approximately two inches for children, and about one and a half inches for infants. Administering compressions requires complete chest recoil, allowing the heart to refill with blood between compressions. Effective ventilation is indicated when the victim’s chest rises.
Adult CPR techniques are performed on victims from eight years old and up. Generally two first responders administer CPR to an adult. Occasionally, CPR is performed by a lone rescuer. If the victim is not breathing, administer 30 chest compressions at a rate of 100 compressions per minute, followed by ventilation. Give the victim a breath big enough to make the chest rise. Repeat ventilation once more when the chest falls. Repeat chest compressions and ventilation for approximately two minutes (five cycles of 30 compressions and two ventilations). After two minutes, check the victim for breathing. If the victim is still not breathing, continue CPR. The pulse check for adults and children is the carotid artery (neck). In two-rescuer CPR, rotate the rescuer performing compressions at regular intervals.
Note: Chest compressions are given with the heel of one hand positioned in the middle of the chest between the nipples. Place the heel of the other hand on top and interlace your fingers. Elbows are locked as compressions are given directly over the sternum. Once the chest is compressed, it should be allowed to come back up to its original position.
Child CPR techniques are administered on victims one to eight years of age. Similar to adults, it is generally performed by two rescuers. A lone rescuer would follow the same 30:2 compression to ventilation ratio and rate as stated for an adult. For two rescuers performing CPR, one rescuer gives 15 chest compressions followed by two breaths by the second rescuer. The compression and ventilation rates are the same as for adults. The compressions are performed with the heel of one hand on the breastbone directly between the child’s nipples. The victim’s pulse can be checked at the carotid or femoral artery.
Infant CPR techniques are performed on babies younger than one year old. It is a one- or two-rescuer operation. A lone rescuer follows the 30:2 compressions to ventilation ratio as performed on adults and children. The chest compressions, utilizing just two fingers, are positioned slightly below the nipple line. Two-rescuer CPR follows the 15:2 compression to ventilation ratio as performed on children. The compression and ventilation rates are the same as for adults and children. The pulse can be checked at the brachial or femoral artery.
Hands-Only CPR is conducted without ventilation. The practitioner begins hands-only CPR by providing chest compressions by pushing hard and fast in the center of the victim’s chest with minimal interruptions. Hands-only CPR is recommended for use by untrained civilians who are confronted with an adult who suddenly collapses outside a hospital setting. The AHA, however, recommends conventional (chest compressions and ventilation) CPR for all adult victims who are discovered already unconscious and not breathing normally as well as children and infants.
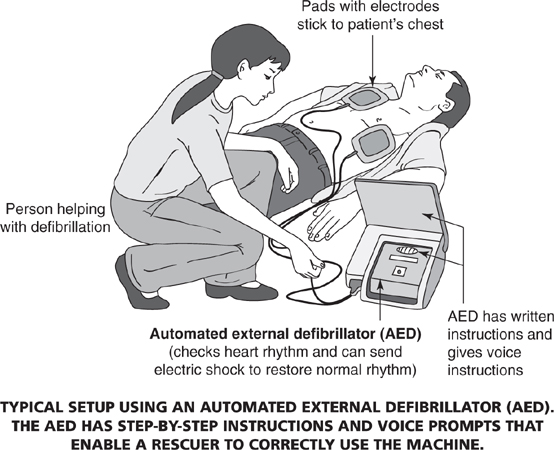
CPR cannot sustain life indefinitely. Cardiac arrest victims usually suffer from an abnormal heart rhythm that causes the heart to stop beating. An automated external defibrillator (AED) is required to supply an electrical current to the heart (defibrillation) in order for it to start to beat and regain a stable rhythm.
AEDs are lightweight medical machines carried by first responders to provide an electrical shock to victims of cardiac arrest. The AED is easy to use because it analyzes the heart rhythm of the victim and instructs (voice prompts) the first responder whether or not to administer an electrical current by pressing the SHOCK button on the machine. If electrical current is warranted, the AED will generally indicate the administration of three stacked SHOCKS. Heart analysis and electrical impulses are provided via pads that are connected to the AED and attached to the victim’s bare chest. If the chest is wet, dry it. Metal (necklaces and underwire bras) should be removed from the victim since these items may conduct electricity and cause burns.
Safety also dictates that before analysis and the administration of a shock all rescuers stay clear of the victim. Additionally, before using an AED, check for accumulations of water in and around the area you will be working in. If necessary, move the victim to a dry location. Checking for breathing and pulse, providing CPR, and reusing the AED are based on the victim’s recovery status subsequent to the initial use of the machine.
Pediatric AEDs, designed to apply a reduced electrical charge through small pads, are employed by rescuers for attempted defibrillation of children one to eight years of age. If, however, a pediatric AED is not available, rescuers should use a standard AED. For infants less than one year of age, a manual defibrillator (generally found in hospitals) is preferred.
To prevent the spread of disease, it is imperative that firefighters carry and utilize adequate medical personal protection equipment (PPE) when administering first aid and CPR. The level of protection worn should correlate with the potential threat of infection and disease. The following is a short list of essential PPE that all firefighters generally wear when providing patient care.
Gloves—In general, gloves (made from latex) are worn by firefighters as standard practice during emergency medical incidents. However, if the firefighter or patient has allergies to this material, vinyl or other type synthetic material gloves are substituted. The patient should be asked if he or she has a latex allergy prior to care. A new pair of gloves must be worn for each patient treated.
Eye protection is worn to inhibit bodily fluids from entering the rescuer’s eyes as well as to provide a certain measure of impact resistance. Safety glasses or goggles are commonly used for this purpose. First responders who wear prescription glasses may require some modification to their protective eyewear.
Gowns—Disposable outer garments to protect exposed skin and uniforms from bodily fluid contamination and blood-borne pathogens should be available to firefighters during certain emergency medical care situations. Gowns are of special value when treating trauma patients.
Masks—To protect the firefighter from airborne pathogens and bodily fluids, surgical-type masks are used. If a patient is suspected of having a communicable respiratory disease, however, greater protection will be needed. Respirators, which require fit testing to ensure a proper seal on the wearer’s face, are worn in these instances.
Firefighters often encounter situations where victims of fires and emergencies need to be removed from danger. Listed below are a number of drag and carry techniques commonly utilized by first responders. These procedures can be used inside burning structures, at the scene of an automobile accident where gasoline has been spilled or ignited, and during radiological, chemical, and biological incidents. They are simple and require a minimum amount of training. These techniques can also be implemented very quickly and effectively to remove the maximum number of victims in life-or-death situations. In general, a victim should not be moved if he or she has or is suspected to have sustained an injury to the neck or spinal column due to trauma, for fear of causing further injury and paralysis. If time allows, spinal immobilization techniques using a cervical collar (head and neck) and short board, immobilization vest, or long backboard (spine) should be employed prior to movement.
A victim is usually moved from a prone to a supine position for reasons ranging from medical evaluation to transport. Rolls are generally performed by more than two rescuers.
To perform a log roll to place a backboard under a supine victim when a neck or spine injury is suspected, the lead rescuer is repositioned from the side of the victim to the top of the victim’s head. Three other rescuers line up on their knees along the same side of the victim (see figure). These three rescuers reach across the prone victim to the far side of the body. The lead rescuer provides manual head stabilization by placing his or her hands on either side of the victim’s head. The next rescuer holds the victim’s arms and shoulders. The third rescuer holds the trunk and thigh area of the victim. The end rescuer holds the victim’s feet and pelvis. The victim is rolled on the order of the lead rescuer in a single movement toward the rescuers to a side position, and the backboard is placed beside the victim on the side opposite the rescuers. The victim is then rolled in a single movement back to a supine position on the backboard upon the order of the lead rescuer. The victim is strapped to the backboard before being moved.

Drags are normally performed by a lone rescuer. A second rescuer, however, can be employed to roll the victim to a supine position and to take the weight off the lower trunk as the victim is being removed.
A firefighter’s drag is performed during structural firefighting operations to remove a victim from a smoky or high heat environment. The rescuer instructs the supine victim to drape his or her arms onto the back of the rescuer’s neck while the rescuer is straddling the victim on hands and knees. The rescuer crawls forward on hands and knees with the victim. This drag method allows the rescuer to move the victim low to the floor, thereby protecting him or her from high heat conditions and the products of combustion.
In a shoulder drag, the rescuer goes behind the victim and raises up the victim’s head and shoulders, using the arms to under-hook the upper trunk. The victim’s arms are at the side. The rescuer’s arms are positioned beneath the armpits of the victim with palms up as the rescuer walks backward dragging the victim. To drag a person down a flight of stairs, the rescuer modifies the arm position of the victim and crosses them at waist level. The rescuer’s arms are then placed beneath the armpits of the victim with palms down grabbing the wrists. The rescuer walks backward down the stairs, supporting the victim’s head and back during the descent. This modification is known as the incline drag.
To perform a clothes drag, the rescuer goes behind the victim to grab his or her clothes at the neck collar/shoulder area. The head of the victim is supported by the arms of the rescuer while moving backward.
Carries are commonly performed on the fireground to remove unconscious and nonambulatory victims out of burning buildings. They are also used in emergency situations to remove victims from dangerous areas.
In a firefighter carry the victim is raised up to a standing position facing the rescuer. The firefighter then grabs the victim’s wrist with one hand while using the arm closest to the victim to grab behind the victim’s leg. The victim is raised onto the shoulders of the firefighter and carried off.
The victim is raised to a standing position and his or her arms are positioned around the firefighter’s neck as the rescuer rotates 180 degrees to carry the victim off. The firefighter leans slightly forward while walking to support the person’s weight and raise the victim off the ground.
The victim is in a supine or sitting position on the ground. If supine, place one arm behind the victim’s back (just below the shoulders) and raise him or her to a sitting position. The firefighter’s other arm is placed under the victim’s knees. While keeping your back straight, raise the victim to approximately waist height and remove to safety.
Portable stretcher—A simple transport device commonly consisting of two wooden poles and a canvas attachment.
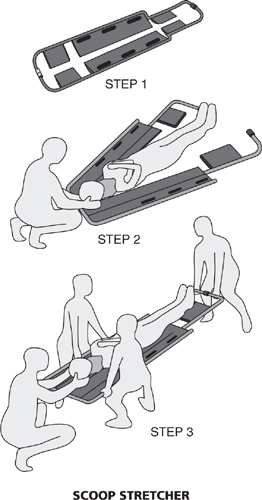
Scoop stretcher—Composed of two pieces of light metal that can be separated and placed on either side of the victim to be transported and then reattached when properly positioned.
Basket stretcher—Made from plastic, fiberglass, or lightweight metal, this type of device is used to remove victims vertically from confined spaces.
Wheeled stretcher—Provides easy transfer of a victim to, into, and out of an ambulance.
Stair chair—Used to transport victims down stairs.
Long backboard—Used for victims who are lying down or standing up and to immobilize victims with neck and spine injuries prior to transporting.
Below is a brief listing of some of the more common first-aid, trauma, and medical emergency incidents encountered by firefighters during a typical tour of duty. Signs and symptoms of the injury are noted where applicable. Basic stabilization and treatment procedures are provided to give the reader a fundamental knowledge of emergency medical care techniques.
Asthma—Difficulty breathing as a result of muscle spasms, which are triggered by an allergic reaction to pollen, dust, smoke, animal fur, medications, certain foods, mold, and cold air. Symptoms include wheezing, coughing, anxiousness, or distress. Sit the patient up and leaning forward to facilitate breathing. Calm the person and have him take his own medication (aerosol spray or puffer) to ease the condition.
Bleeding (external)—Apply direct pressure onto the wound using a protected hand or sterile dressing to control the flow of blood. Elevate, if the wound involves an extremity. Bandage the wound (to hold the dressing in place).
Burns (thermal)—Classification of burns is based on depth. First-degree (superficial) burns involve only the epidermis (top) layer of the skin. The top layer of the skin contains sweat ducts and blood capillaries. Sunburn is the standard example given for first-degree burns. The skin appears reddened and is dry and warm to the touch. Other symptoms include swelling, elevated body temperature, and pain. Application of cool water will help to reduce the patient’s pain and discomfort. Second-degree (partial-thickness) burns involve both the top layer and middle (dermis) layer of the skin. The middle layer of the skin contains nerve endings and hair follicles. Symptoms of second-degree burn include intense pain, pink or reddish skin, and blistering. Leave blisters intact and cover the burn area with a dry, sterile dressing. Third-degree (full-thickness) burns involve the epidermis, dermis, and subcutaneous tissue (fat cells and blood vessels). The skin can appear charred, yellow-brown, dark red, or white. The patient feels no pain because the nerve cells of the skin are destroyed. Flush the damaged area with water and remove smoldering clothing. Cover the burn area with a dry, sterile dressing. For burns to the hands or feet, separate the fingers or toes with dressings. Burns that involve muscle and bone are sometimes referred to as fourth-degree burns. To determine the percentage of body surface that the burn covers, use the rule of nines. The rule of nines accounts for approximately 100 percent of the total body surface.
The head (9%), chest (9%), abdomen area (9%), upper back (9%), lower back (9%), each arm-anterior and posterior (9% × 2 = 18%), each leg-anterior (9% × 2 = 18%), and each leg-posterior (9% × 2 = 18%) account for 99 percent of an adult’s body surface. The groin area (calculated as 1%) raises the total to 100%.
For children the rule of nines is slightly modified. The head counts for 18%. The calculations for the chest (9%), abdomen area (9%), upper back (9%), lower back (9%), and arms-anterior and posterior (9% × 2 = 18%) remain the same as for adults. The legs, anterior and posterior, however, account for (13.5% × 2 = 27%). The estimate for the groin area (1%) of a child is similar to adults.
Chest injury—Indicators include difficulty breathing and chest pain. Treat the patient by assisting with breathing and provide supplemental oxygen as needed.
Contusion (bruise)—Apply cold or an ice pack to inhibit swelling and elevate the injured part.
Eye wound—To protect against eye movement and further injury, bandage both eyes of the patient, even if only one eye is injured, because the eyes move in unison.
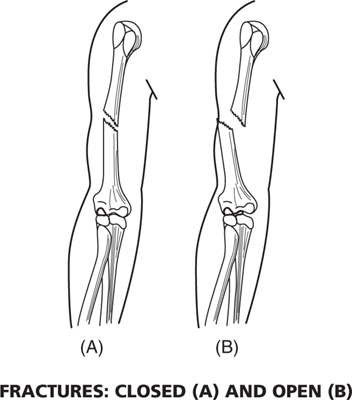
Fracture (broken bone)—Classified as either an open (skin is broken) or closed (skin is not broken) fracture. Indicators include open wound, deformity, pain with movement, tenderness, and swelling. Initially the first responder should cut away clothing to expose the injury using trauma shears. Also check for dislocation (separation of the bone from its joint). Treatment involves stabilizing the area above and below the site of injury. Apply a dressing to open wounds, administer cold or an ice pack to inhibit swelling, and splint the injury as required. A splint is a device used to immobilize the area around the broken bone(s) and joint. In general, bones should be splinted in the position found. Splints can be either rigid (wood, padded cardboard) or soft and flexible (foam, air).
Frostbite—Is the freezing of a body part caused by unprotected or inadequately protected skin exposed to cold weather or cold water. It usually occurs in the extremities. Indicators include whitish skin color and loss of feeling in the affected area. Treatment entails removing the patient from the cold environment, taking off wet clothing, and maintaining body heat using dry towels and blankets. Warm the frostbitten body part by placing it next to a warm body part, and do not rub.
Head or neck injury—Can result in permanent paralysis if not treated correctly. Indicators include open wound, bleeding, deformity or swelling, confusion and disorientation, inability to talk, and irregular breathing. Treatment includes controlling bleeding, manual head stabilization, maintaining an open airway, providing supplemental oxygen, and monitoring the vital signs of the patient. Proper care also includes application of a cervical collar and full immobilization to a long backboard prior to transport.
Heat exhaustion—Caused by the excessive loss of fluids from the body due to overwork or overexercising. Signs and symptoms include sweating profusely, cold and moist skin, rapid/shallow breathing, and dizziness. The first responder should remove the patient to a cool environment and check vital signs. Remove tight-fitting clothing and allow the victim to drink fluids (water). Reduce body temperature by wetting the skin with cool water and apply ice packs to the patient’s neck, back, armpits, and groin to reduce body temperature. If left untreated, heat exhaustion can progress to heat stroke, which is a more serious condition.
Heat stroke—A condition where the body cannot cool itself. If not treated quickly and properly, it can cause brain damage and be life threatening. Indicators of heat stroke are inconsistent breathing (deep/shallow) and pulse (rapid strong/rapid weak) patterns; dry, hot skin; dilated pupils; and seizures. If possible, move the victim to a cool/shady area or into an air-conditioned environment and remove any unnecessary clothing. Cool the victim off by wetting the skin. Apply ice packs to the patient’s neck, back, armpits, and groin to reduce body temperature.
Hypoglycemia—Abnormally low blood sugar. A diabetic health problem (the patient has taken insulin and not eaten or the patient has not taken insulin as required) whose major symptom is an altered mental state (combativeness, hostility, agitation) due to the brain’s need for glucose. Other signs include rapid heart rate; fruity odor on the breath; cold, pale, and moist skin; and dilated pupils. Treat for shock. Additionally, maintain and monitor an open airway and administer supplemental oxygen, when required. Check vital signs and provide sugar or glucose solution orally to conscious patients.
Hyperglycemia (high blood sugar)—Occurs when there is enough glucose in the body but not enough insulin being produced in the pancreas. This condition is encountered less commonly than hypoglycemia. Symptoms include rapid breathing, weak/rapid pulse, and intense thirst. Administer fluids if the person is conscious. Treat for shock and continually monitor the victim’s vital signs.
Hypothermia—Is low body temperature, generally below 95°F (normal adult body temperature is 98.6°F). Hypothermia is commonly caused when victims are exposed to cold weather, snow, or cold water for long periods of time. Indications include cold skin temperature, decreased mental and motor functioning, and muscle stiffness. Treatment should include removal from the cold environment, taking off wet clothing, and maintaining body heat.
Impaled wound—Impaled objects include knives, sticks, metal bars, arrows, and fencing. Expose the object to perform a medical examination. Do not remove the object from the wound unless it is impairing the victim’s breathing. Control bleeding and secure the object with bulky dressings so it does not move.
Nosebleed—Have the patient sit down and lean forward to keep blood from flowing back into the throat. Pinch the nostrils together.
Open wounds—Treatment for abrasions (scrapes), lacerations (cuts), puncture (stab) wounds, and avulsions (skin tears) involve controlling the bleeding and applying a sterile dressing and bandage.
Poisoning—Common causes include medicines, carbon monoxide, household cleaning fluids, paints, insecticides, illegal drugs, chemicals, and food. Some symptoms are headache, weakness, dizziness, confusion, profuse sweating, chemical-smelling breath, burns around the mouth, unusual odors, nausea, diarrhea, eye irritation, muscle twitching/convulsions, difficulty in breathing, rapid pulse, pinpoint pupils, and unconsciousness. Treatment may entail removing the victim to a clean air environment; flushing with water; inducing vomiting; monitoring airway, breathing, and circulation; checking vital signs; administering rescue breathing or CPR; and contacting the local Poison Control Center for advice.
Seizures—May involve twitching, jerking, and violent contracting of the muscles (convulsions). Seizures can have a variety of causes, including a medical condition, fever, infection, poisoning, and head injury. Protect the patient from objects in the immediate area that can cause injury. Vomiting may occur and the first responder must therefore monitor and ensure an open airway. Provide oxygen to the patient as necessary. Seizures may be for a short (several minutes) or long duration. Do not restrain the victim or put anything in the person’s mouth, which could cause further injury. Prolonged seizures can be life threatening.
Shock—A condition that is a result of inadequate blood circulation in the body and thereby a reduction of oxygen to living cells. It is indicated by anxiety and restlessness in the patient. The patient’s skin may be pale, cool, and moist. The patient will also exhibit an increased pulse and respiratory rate. Place the individual in a supine position with legs slightly elevated to facilitate blood flow from the lower extremities back to the heart. Loosen restrictive clothing. Keep the victim immobile and cover with a blanket to keep warm. Do not administer fluids. Check and maintain the ABCs of patient care.
Smoke inhalation—The most common cause of death in fires. Symptoms include burning of the eyes, nose, and throat and difficulty breathing. Treatment entails removing the victim to a clean and uncontaminated environment. Follow the ABCs for patient care and treat for shock. Begin CPR, if needed.
Spinal column injury—Can result in permanent paralysis if not treated correctly. This injury is usually associated with trauma. Signs and symptoms include confused mental status, loss of feeling and movement in the extremities, “pins and needles” sensation in extremities, neck/back pain, and loss of bladder or bowel control. The victim should be fully immobilized utilizing a cervical collar and long backboard prior to transport. Attention should be given to maintaining an open airway.
Sprains (damaged ligament) and strains (damaged muscle)—Apply cold or an ice pack to the injured area to control swelling and pain. Splint the injury if necessary.
Stroke—Caused by the disruption of blood to the brain. Symptoms include partial face drooping or paralysis, slurred speech, dilated pupils, nausea/vomiting, and blurred vision. Treatment entails monitoring and maintaining an open airway, rescue breathing, and CPR if required.
Circle the letter of your choice.
1. An injured auto accident victim who is displaying signs and symptoms of shock would be assessed according to CUPS criteria by first responders as
(A) stable
(B) unstable
(C) potentially unstable
(D) critical
2. The normal anatomical position for a person is most accurately described in which of the following statements?
(A) Sitting up facing you with arms at the side and palms facing you
(B) Prone with arms at the side and palms facing away from you
(C) Supine with arms crossed and palms facing you
(D) Standing upright facing you with arms at the side and palms facing you
Directions: Match the body directional term in column A with its correct corresponding meaning in column B. Write the letter of your choice in the space provided.
Column A |
Column B |
____ 3. Lateral |
(A) Toward the midline of the body |
____ 4. Anterior |
(B) To the left side of the patient’s body |
____ 5. Medial |
(C) Away from the trunk of the body |
____ 6. Proximal |
(D) Toward the feet |
____ 7. Superior |
(E) Toward the front of the body |
____ 8. Left |
(F) Away from the midline of the body |
____ 9. Inferior |
(G) Toward the head |
____10. Right |
(H) Toward the back of the body |
____11. Distal |
(I) To the right side of the patient’s body |
____12. Posterior |
(J) Toward the trunk of the body |
13. An injury sustained from a violent impact or sudden force is called
(A) a medical condition
(B) trauma
(C) depression
(D) initial patient assessment
14. A first responder should check a patient’s vital signs to help monitor the individual’s health condition and discover abnormalities. All but which of the following is included in the evaluation of a victim’s vital signs?
(A) Pulse rate
(B) Respiration rate
(C) Blood pressure
(D) CPR
15. The normal rate of breathing for adults is
(A) between 12 and 20 breaths per minute
(B) between 20 and 30 breaths per minute
(C) between 30 and 40 breaths per minute
(D) none of the above
16. An infant’s normal rate of breathing is
(A) between 8 and 12 breaths per minute
(B) between 12 and 20 breaths per minute
(C) between 20 and 30 breaths per minute
(D) between 30 and 40 breaths per minute
17. The pulse is an indicator of the functioning of the victim’s
(A) central nervous system
(B) respiratory system
(C) body temperature
(D) circulatory system
18. The normal pulse range for adults and adolescents is approximately
(A) 120 to 160 beats per minute
(B) 100 to 130 beats per minute
(C) 60 to 100 beats per minute
(D) 30 to 60 beats per minute
19. The artery commonly used by first responders to check the pulse rate of a responsive infant is the
(A) radial artery
(B) brachial artery
(C) femoral artery
(D) carotid artery
20. The carotid artery is normally used to check the pulse rate of a (an)
(A) unresponsive adult or child
(B) responsive infant
(C) responsive adult or child
(D) unresponsive infant
21. The pulse rate of a victim is commonly determined by first responders in which manner listed below?
(A) Counting the number of beats for three minutes and dividing by two
(B) Counting the number of beats for one minute and multiplying by four
(C) Counting the number of beats for half a minute and multiplying by two
(D) Counting the number of beats for two minutes and dividing by four
22. A bounding (thumping) pulse would most likely indicate the patient is suffering from
(A) high blood pressure
(B) cardiac arrest
(C) shock
(D) none of the above
23. What procedure is usually performed by the first responder to assess a patient’s general body temperature?
(A) Inserting a finger into the victim’s mouth under the tongue
(B) Grabbing the wrist of the victim
(C) Examining the pupils of the patient
(D) Placing the back of the hand on the patient’s forehead
24. Cold and clammy skin with profuse sweating can be indicative of what condition listed below?
(A) Heat cramps
(B) Heat exhaustion
(C) Heat stroke
(D) None of the above
25. Nonreactive pupils that do not react to a beam of light from the penlight of the first responder directed into the eye of the victim are indicative of all of the following with the exception of
(A) damage to the eye
(B) stroke
(C) head injury
(D) the victim is wearing contact lenses
26. Blood pressure is the measure of the force the blood exerts on the walls of the arteries. It provides a functional status of
(A) the lungs
(B) the circulatory system
(C) the central nervous system
(D) the musculoskeletal system
27. A victim’s blood pressure is commonly recorded using a
(A) bag-valve mask device
(B) watch
(C) stethoscope
(D) none of the above
28. The proper position for a blood pressure cuff when taking a reading on a patient is
(A) around the brachial artery
(B) around the radial artery
(C) around the carotid artery
(D) around the ankle
29. Blood pressure is denoted by two numbers in fractional form. Select the correct answer that accurately denotes what these two numbers are called and what they represent.
(A) The systolic number is the denominator and represents the pressure in the blood vessels when the heart is relaxed.
(B) The diastolic number is the numerator and represents the pressure when the heart is contracting and pumping blood through the blood vessels.
(C) The systolic number is the numerator and represents the pressure when the heart is contracting and pumping blood through the blood vessels.
(D) None of the above.
30. Normal blood pressure for adults is generally within what range listed below?
(A) 150–170/120
(B) 150/200
(C) 80–130/40–60
(D) 100–150/60–90
31. High blood pressure is associated with all but which of the following?
(A) Hypotension
(B) Cardiovascular disease
(C) Kidney malfunction
(D) Drug use
32. Select the choice that is not considered to be a common physical way to assess patient responsiveness.
(A) Pinching the muscles of the neck
(B) Rubbing the breast bone
(C) Pulling the hair
(D) Tapping the chest/shoulders
33. The ABCs of patient care represent all of the choices listed below with the exception of
(A) airway
(B) anatomy
(C) breathing
(D) circulation
34. To open the airway on a victim with a solid object lodged inside his or her mouth the first responder should utilize what correct procedure on the patient?
(A) Insert a suction unit catheter into the mouth of the victim
(B) Use the head tilt–chin lift technique
(C) Insert an OPA device into the victim’s mouth
(D) None of the above
35. The medical technique used by first responders to dislodge a foreign object from the throat of a conscious victim is known as a
(A) finger sweep
(B) side straddle
(C) head tilt–chin lift
(D) abdominal thrust
36. Firefighters should follow what foreign object removal procedure stated below for an unconscious adult with an airway completely obstructed?
(A) Place the adult face up and apply chest compressions using two fingers.
(B) Position the victim face down and perform abdominal thrusts.
(C) Place the victim face up and perform a finger sweep.
(D) Position the victim face down and give five strong back blows.
37. Abdominal thrusts are best delivered in what manner noted below?
(A) Inward and upward with hands just below the victim’s navel
(B) Inward and upward with two fingers on top of the navel
(C) Inward and upward with hands just above the victim’s navel
(D) None of the above
38. Select the procedure that is NOT correct to remove a foreign object from the airway of a conscious infant.
(A) Place the infant face down on your arm.
(B) Deliver five back blows with the heel of one hand.
(C) Shift the infant to a supine position on your arm.
(D) Apply chest compressions with the heel of one hand.
39. Which of the following is NOT one of the simple ways of determining a patient’s breathing status?
(A) Administer positive pressure ventilation
(B) Listen for sounds of breathing
(C) Look to see if the victim is struggling to breathe
(D) Feel for breathing by placing your hand on an unconscious victim’s chest
40. A common and relatively safe rescue breathing method used today by firefighters is known as
(A) mouth-to-mouth resuscitation
(B) mouth-to-mask ventilation
(C) mouth-to-stoma ventilation
(D) none of the above
41. The rescue breathing ratio for an adult victim is
(A) three breaths every five seconds
(B) one breath every three seconds
(C) one breath every five seconds
(D) none of the above
42. A firefighter performing rescue breathing on a child or infant should administer one breath every
(A) two seconds
(B) one second
(C) three seconds
(D) five seconds
43. Assessing a patient’s circulation includes all but which of the following checks?
(A) Airway
(B) Pulse rate
(C) Bleeding
(D) Skin color
44. A patient exhibiting a cyanotic skin color will look
(A) pink
(B) yellow
(C) blue
(D) orange
45. A patient without a pulse requires the first responder to start
(A) abdominal thrusts
(B) CPR
(C) finger sweeps
(D) none of the above
46. CPR should be administered by first responders on victims of
(A) eye injury
(B) hemorrhaging
(C) cardiac arrest
(D) high blood pressure
47. CPR, if performed correctly, will provide the victim with
(A) controlled bleeding and a reduction of pain
(B) oxygen and enhanced blood flow
(C) needed fluids and electrolytes
(D) none of the above
48. Without oxygen, brain cells begin to die in
(A) one to two minutes
(B) two to four minutes
(C) four to six minutes
(D) eight to twelve minutes
49. While performing CPR on an adult, first responders will normally check the pulse at the
(A) brachial artery
(B) radial artery
(C) femoral artery
(D) carotid artery
50. During two-rescuer CPR on an adult victim, the ratio of chest compressions to ventilation is
(A) 30 compressions to 2 ventilations
(B) 2 compressions to 15 ventilations
(C) 15 compressions to 2 ventilations
(D) 1 compression to 5 ventilations
51. Adult CPR techniques are performed on patients aged
(A) one year old and up
(B) five years old and up
(C) eight years old and up
(D) 15 years old and up
52. Chest compressions administered during CPR, regardless of the age of the victim, are given at the rate of
(A) 100 per minute
(B) 80 per minute
(C) 60 per minute
(D) 40 per minute
53. Select the INCORRECT point of information concerning two-rescuer CPR on a child victim.
(A) Child CPR techniques are performed on victims aged one to eight years.
(B) One rescuer gives 15 chest compressions followed by two ventilations given by the second rescuer.
(C) Compressions are performed directly over the sternum using two fingers.
(D) Effective ventilation is indicated when the victim’s chest rises.
54. An INCORRECT statement concerning infant CPR technique performed by a lone rescuer is
(A) it is performed on babies younger than one year old
(B) CPR can also be performed on infants by two rescuers
(C) the ratio of chest compressions to ventilation is 15 to 2
(D) chest compressions are given utilizing just two fingers
55. The benefit of an automated external defibrillator (AED) is best described in
(A) it maintains an open airway
(B) it supplies an electric current to the heart
(C) it provides positive pressure ventilation
(D) none of the above
56. Pediatric AEDs are employed by rescuers for attempted defibrillation of children within what age bracket listed below?
(A) Children from ages one to eight
(B) Children from ages eight to 12
(C) Children older than 12 years of age
(D) All of the above
57. The pads connected to the AED get attached to
(A) the head of the victim
(B) the hands of the rescuers
(C) the feet of the victim
(D) the bare chest of the victim
58. When using the AED, safety dictates that before analysis and the administration of a shock all rescuers
(A) touch the victim
(B) interlock arms
(C) stay clear of the victim
(D) remove metal objects from their pockets
59. In general, a victim should not be moved if he or she has or is suspected to have sustained an injury to the neck or spinal column due to trauma for fear of
(A) loss of blood
(B) disorientation
(C) seizures
(D) paralysis
60. The device commonly used to immobilize the head and neck of a trauma injury victim is called a (an)
(A) cervical collar
(B) short backboard
(C) immobilization vest
(D) stair chair
61. Rolls are used on victims by first responders for all but which of the following reasons?
(A) To move the victim from a prone to a supine position
(B) For medical evaluation
(C) For transport
(D) They can be performed easily by a lone rescuer.
62. The end rescuer at the lower legs performing a log roll on a victim grabs what parts of the victim’s anatomy?
(A) The arms and shoulders
(B) The feet and pelvis
(C) The trunk and thigh
(D) None of the above
63. The lead rescuer during a log roll of a victim with a suspected neck injury should perform what technique during the procedure?
(A) Lifting of the arms and shoulders of the victim
(B) Manual head stabilization
(C) Head tilt–chin lift technique
(D) Rescue breathing
64. A drag technique requiring crawling on hands and knees, performed during structural firefighting operations to remove a victim safely from a smoke-filled environment, is called
(A) a shoulder drag
(B) a clothes drag
(C) a firefighter’s drag
(D) a duck walk drag
65. What area of the body is grabbed during the clothes drag technique of victim removal?
(A) The collar/shoulder area
(B) The pant leg area
(C) The belt/pelvis area
(D) The ankle area
66. A drag technique requiring the rescuer to under-hook the upper trunk of the victim while walking backward is known as the
(A) clothes drag
(B) firefighter’s drag
(C) shoulder drag
(D) blanket drag
67. The carry technique that requires the rescuer to grab the victim’s wrist and leg and lift the victim onto the shoulders is known as the
(A) pack strap carry
(B) firefighter carry
(C) piggyback carry
(D) none of the above
68. A carry that requires the rescuer to position the victim’s arms around his or her neck as the rescuer leans forward while walking to support the victim’s weight is called
(A) a firefighter carry
(B) a cradle carry
(C) a pack strap carry
(D) none of the above
69. A stretcher used to remove a victim vertically from a confined space is referred to as a
(A) basket stretcher
(B) scoop stretcher
(C) wheeled stretcher
(D) portable stretcher
70. A stretcher composed of two pieces of light metal that can be separated and placed on either side of the victim to be moved and then reattached is called a
(A) basket stretcher
(B) portable stretcher
(C) stair chair
(D) scoop stretcher
71. A device used to immobilize a victim who is lying down or standing up with a suspected spinal chord injury prior to transport is known as a
(A) stair chair
(B) scoop stretcher
(C) portable stretcher
(D) long backboard
72. Choose the item that is NOT an example of personal protective equipment (PPE) for a medical emergency.
(A) Utility knife
(B) HEPA mask
(C) Latex gloves
(D) Gown
73. It is essential for first responders to wear PPE during medical emergencies to protect against
(A) head trauma injury
(B) heat exhaustion
(C) infection and disease
(D) burns from direct flame contact
74. Which of the following is NOT a proper way to control the flow of blood from a laceration of the leg?
(A) Splint the wound.
(B) Apply direct pressure with a gloved hand.
(C) Place a dressing over the wound.
(D) Bandage the dressing.
Directions: Match the burn classification in column A with the correct description found in column B. Write the letter of your choice in the space provided.
Column A |
Column B |
____ 75. First-degree burn |
(A) Involves muscle and bone |
____ 76. Second-degree burn |
(B) Involves only the top layer of the skin |
____ 77. Third-degree burn |
(C) Symptoms include intense pain, pink skin, and blisters |
____ 78. Fourth-degree burn |
(D) Known as a full-thickness burn |
79. Proper treatment for a second-degree burn is to
(A) scrape off blisters with a knife and apply a dry, sterile dressing
(B) apply petroleum jelly ointment to blisters and don’t cover
(C) leave blisters intact and cover with dry, sterile dressing
(D) none of the above
80. A standard example used to depict a first-degree burn is
(A) blistering skin from contact with boiling water
(B) sunburn
(C) charring of skin from direct flame contact
(D) all of the above
81. The middle layer of the skin is known as the
(A) dermis layer
(B) epidermis layer
(C) subcutaneous layer
(D) muscle and bone layer
82. A third-degree burn can demonstrate which of the following skin characteristics?
(A) A charred appearance
(B) A yellow-brown color
(C) A dark red or white color
(D) All of the above
83. For burns to the hand or feet, separate the fingers or toes with
(A) splints
(B) bandages
(C) dry, sterile dressing
(D) ice packs
84. To determine the percentage of body surface that a burn covers on a victim, first responders use
(A) a stethoscope
(B) a thermometer
(C) the rule of nines
(D) none of the above
85. The head of an adult accounts for what percentage of the body when determining the extent of a burn using the rule of nines?
(A) 18%
(B) 9%
(C) 13.5%
(D) 1%
86. An adult victim with burns covering the entire chest and abdominal area would be estimated using the rule of nines to have what percentage of the body burned?
(A) 18%
(B) 9%
(C) 27%
(D) 36%
87. A child having burned both legs (anterior and posterior) would be estimated by first responders as having what percentage of the body burned using the rule of nines?
(A) 36%
(B) 18%
(C) 9%
(D) 27%
88. A child or adult having burns on both arms (anterior and posterior) would be determined by the rule of nines to have what percentage of the body affected?
(A) 9%
(B) 18%
(C) 27%
(D) 36%
89. A cerebral vascular accident (stroke) is commonly caused by
(A) thermal burn
(B) nosebleed
(C) disruption of blood to the brain
(D) inability of the pancreas to produce insulin
90. All of the following are indicators of a closed fracture with the exception of
(A) an open wound
(B) a deformity
(C) pain with movement
(D) tenderness
91. An example of a soft splint is a
(A) wood splint
(B) padded cardboard splint
(C) air splint
(D) all of the above
92. Which of the following is NOT a correct treatment procedure for a frostbite victim?
(A) Removing the patient from the cold environment
(B) Taking off wet clothing
(C) Maintaining the body heat of the victim using dry towels and blankets
(D) Rubbing the affected area to stimulate blood circulation
93. What immobilization device is essential to apply on a victim suffering from a traumatic head and neck injury?
(A) A short board
(B) A cervical collar
(C) A rigid splint
(D) A vest-type device
94. Which of the following is not indicative of heat stroke?
(A) Inconsistent breathing and pulse patterns
(B) Cold and clammy skin
(C) Dilated pupils
(D) Seizures
95. A diabetic health problem caused by abnormally low blood sugar resulting in an altered mental state on the part of the victim is called
(A) hypoglycemia
(B) hyperglycemia
(C) hypothermia
(D) none of the above
96. Normal adult body temperature is
(A) below 95 degrees Fahrenheit
(B) 96.5 degrees Fahrenheit
(C) 97.8 degrees Fahrenheit
(D) 98.6 degrees Fahrenheit
97. Hypothermia is commonly caused when victims
(A) have too much insulin
(B) ingest too much sugar
(C) are exposed to cold weather
(D) are suffering from a head or neck injury
98. An INCORRECT treatment measure to take when encountering a patient suffering a seizure with convulsions is to
(A) protect the patient from objects in the immediate area that can injure him or her
(B) monitor and ensure an open airway
(C) place a tongue depressor in the patient’s mouth
(D) provide supplemental oxygen as necessary
99. An INCORRECT measure in the administration of medical care to a patient in shock is
(A) place the victim in a prone position with legs slightly elevated
(B) keep the person warm with blankets
(C) check and maintain the ABCs of patient care
(D) provide supplemental oxygen if required
100. A spinal column injury patient discovered inside a playground was IMPROPERLY treated by first responders if
(A) a cervical collar was applied to immobilize the head and neck
(B) the patient was transported to the hospital prior to immobilization
(C) attention was given to maintaining an open airway
(D) a long backboard was utilized to immobilize the spine
1. C
2. D
3. F
4. E
5. A
6. J
7. G
8. B
9. D
10. I
11. C
12. H
13. B
14. D
15. A
16. C
17. D
18. C
19. B
20. A
21. C
22. A
23. D
24. B
25. D
26. B
27. C
28. A
29. C
30. D
31. A
32. C
33. B
34. B
35. D
36. C
37. C
38. D
39. A
40. B
41. C
42. C
43. A
44. C
45. B
46. C
47. B
48. C
49. D
50. A
51. C
52. A
53. C
54. C
55. B
56. A
57. D
58. C
59. D
60. A
61. D
62. B
63. B
64. C
65. A
66. C
67. B
68. C
69. A
70. D
71. D
72. A
73. C
74. A
75. B
76. C
77. D
78. A
79. C
80. B
81. A
82. D
83. C
84. C
85. B
86. A
87. D
88. B
89. C
90. A
91. C
92. D
93. B
94. B
95. A
96. D
97. C
98. C
99. A
100. B