CHAPTER 4
The Many Roles of Saturated Fat
The human body contains almost forty trillion cells; each of these cells is surrounded by a membrane, which serves to separate the interior of the cell from the exterior environment.
As microscopes have become stronger and analytical techniques more advanced, scientists have discovered the cell membrane’s many marvels. The membrane’s construction allows for the passive diffusion of oxygen and carbon dioxide, while other compounds can only get inside the cell (or can be released from the cell) through channels created by proteins that span the thickness of the membrane, some of which are specific for just one single chemical. The cell “mem-brain” is indeed the brain of the cell; it senses the nutrients available on the outside and makes decisions about what should cross the barrier to enter the cell as well as what will be released from the cell to the exterior.
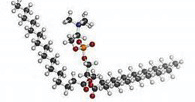
The cell membrane is both stable and fluid, thanks to its ingenious construction. Composed of a lipid bilayer, that is, a double layer of fatty acids, each membrane contains about one trillion fat molecules. At least half of these fat molecules must be saturated fatty acids for the cell to work properly. The basic structural unit of the membrane is a phospholipid, that is, two fatty acids joined to a structure containing phosphorus, forming a kind of head with two legs. The “legs” face inward, while the “head” faces outward to interact with the watery environment inside and outside the cell.

The cell membrane: Each phospholipid has two fatty acids attached to a phosphorus molecule. The fatty acids face inward while the phosphorus ends face outward to the watery environments inside and outside the cell. Specialized proteins allow the passage of compounds into and out of the cell.
The most common type of phospholipid contains one saturated fatty acid—a straight “leg”—and one unsaturated fatty acid—a bent “leg.” The saturated fatty acids give the cell stability, while the unsaturated fatty acid (usually a monounsaturated fatty acid) provides flexibility. The space created by the bent leg is often filled with a cholesterol molecule, which serves as a kind of structural support and ensures that the cell is waterproof.

Cholesterol is packed between the fatty acids in the cell membrane to provide solidity and waterproofing.
Dotted throughout the cell membrane are structures called lipid rafts, which are rich in cholesterol and molecules called sphingolipids. In these areas, more of the fatty acids are saturated, and they tend to be longer, making the rafts thicker than other parts of the bilayer. These slightly thicker and stiffer areas on the cell membrane can better accommodate certain membrane proteins necessary for numerous processes in the cell.
Trans fatty acids have many deleterious effects on the cell membrane, including blocking receptors and inhibiting enzyme function. Interestingly, saturated fats protect the cells from these effects. In experiments with swine, the undesirable effects of trans fats are mitigated when the proportion of saturated fats is high.1 This research indicates that if your diet contains liberal amounts of butter and other animal fats, you could actually eat French fries every now and then without causing much harm!
Inside the cells are mitochondria—called the powerhouses of the body, because they produce a fuel called adenosine triphosphate (ATP), the body’s main energy source.* A membrane also surrounds each of the mitochondria, very similar to that surrounding the cell. These membranes also require saturated fatty acids for stability and structure.
Thus, in the most basic sense, at the level of our cells and mitochondria, and in incalculable numbers, saturated fat molecules are essential for life. Without ample saturated fats, cell membranes lack stability—you might describe them as “floppy.” At the cellular level, a deficiency of necessary saturated fats leads to unpredictable, but certainly adverse, consequences.
In humans, a large fraction of the fatty acids in our cell membranes must be saturated because we are warm-blooded. We need larger amounts of saturated fats just like tropical plants, such as coconut and date palms, need larger amounts of saturated fatty acids in their leaves and fruit to provide needed stiffness in a hot climate. On the opposite end of the spectrum, cold-blooded animals from northern climates rely on unsaturated fatty acids, especially the longer and more unsaturated fatty acids, to serve as a kind of antifreeze—like DHA and EPA, two long and highly unsaturated fatty acids found in fish from Arctic waters.
The digestive tracts of warm-blooded ruminant animals are designed to create saturated fatty acids from the unsaturated fatty acids naturally occurring in grasses and grains. Thus, the body of a warm-blooded vegetarian cow will be laced with highly saturated fat. With her high body temperature—101 degrees F—the cow needs even more saturated fatty acids than humans do to function properly. Efforts to increase the omega-3 content of beef are misguided—the cow does not need antifreeze; she needs stable saturated fats. That is why the omega-3 content in the fat of beef, lamb, and goat is very low—usually less than 1 percent, with levels largely resistant to dietary changes.
When saturated fats are not available, or when we mistakenly avoid them thinking they are not good for us, the body has a backup plan—it makes saturated fats out of carbohydrates, especially refined carbohydrates like sugar and white flour. This process is called de novo lipogenesis (DNL). A high-carbohydrate diet is thus a high-fat diet! In fact, avoiding saturated fat is a recipe for creating carb cravings—the body needs saturated fats so fundamentally, that it will get them one way or the other. Diets low in both saturated fat and carbohydrates—such as the South Beach Diet or low-fat versions of the paleo diet—pose a real danger and usually fail as the dieter gives in either to saturated fat or to carbohydrates in order to supply the basic building blocks for our cells.
While the body can make saturated fat by de novo lipogenesis, it is better to get it from the diet. To create saturated fat, DNL uses up the hydrogen ions and electrons carried by niacin (vitamin B3), making this essential nutrient much less effective.2 When niacin levels are depleted for DNL, it is no longer available to defend antioxidants and recycle folate and vitamin K—processes that protect us against heart disease.
SATURATED FATTY ACIDS ARE NO LESS IMPORTANT inside the cell, where they play many roles, especially in a process called protein acylation, which uses the fourteen-carbon saturated fat myristic acid and the sixteen-carbon saturated fat palmitic acid.
Myristoylation involves the attachment of myristic acid to the protein glycine. The resulting compound allows for many important reactions and signaling pathways inside the cell, the movement of proteins, and the interaction of proteins with the cell membrane.3 Myristoylation is an integral part of apoptosis, or programmed cell death.
Apoptosis is necessary for cell homeostasis and occurs when cells are under stress. Thus, myristic acid facilitates the regular functioning of the cell; and when apoptosis does not occur, we become vulnerable to cancer. Myristic acid also supports the conversion of the basic omega-3 fatty acid, linolenic acid, into the elongated forms DHA and EPA.4 Thus, a deficiency of myristic acid from the diet can have unfortunate consequences, including cancer, mental decline and immune system dysfunction.
Myristic acid is also involved in the amplification of important hormone signals, such as the hormone adrenaline. When the adrenal gland produces adrenaline, myristic acid acts to get the hormone to the parts of the body needed for action; the heart beats faster, the blood flow to the gut decreases while the blood flow to the muscles increases, and the production of glucose increases.5
The body makes myristic acid very slowly, and in times of great need, requires this fat from food. The most common source of myristic acid is butter, followed by cheese. It occurs in smaller amounts in meat fats and in tropical oils from the coconut and palm fruit.*
Sixteen-carbon palmitic acid is also important for cellular function. In the cell, palmitic acid binds with cysteine and other proteins, allowing them to attach to the cell membrane, where they can do their work. Palmitoylation helps proteins move around and interact with other proteins. Palmitoylation also plays an important role in regulating neurotransmitter release and memory formation.
Palmitic acid is the most prevalent fatty acid in animal fats (usually 30–40 percent of the total), and it is the fatty acid that the body makes first. It is frowned upon in cardiovascular circles, as research has shown that palmitic acid can raise LDL and total cholesterol slightly in feeding experiments. Myristic acid (fourteen carbons) and lauric acid (twelve carbons) do as well.6 These findings provide the vegetable oil industry with a platform to further demonize traditional fats, as dairy fat is a major source of myristic acid, coconut oil is a major source of lauric acid, and palm oil is especially rich in palmitic acid. Eighteen-carbon stearic acid, found predominantly in meat, poultry and fish, does not raise cholesterol in feeding experiments, and is thereby acceptable in “healthy” dietary guidelines, especially as stearic acid levels are greater in lean meat than fatty meat. Cocoa butter is rich in stearic acid, a fact that makes the chocolate makers happy.
A recent discovery indicates that eighteen-carbon stearic acid also plays important roles inside the cell—along with its fourteen-carbon and sixteen-carbon brothers. Researchers developed a genetic line of flies whose cells were not able to produce stearic acid naturally. Flies with the defect did not develop beyond the pupal stage. It turns out that stearic acid is involved in signaling functions, and without it, the cells’ mitochondria cannot function.7
Mitochondrial dysfunction is a recent disorder, occurring with increasing frequency in humans. Symptoms include just about everything that can ail us—poor growth, loss of muscle coordination, muscle weakness, visual problems, hearing problems, learning disabilities, heart disease, liver disease, kidney disease, gastrointestinal disorders, respiratory disorders, neurological problems, autonomic dysfunction and dementia. Conventional medicine blames the disorder on faulty genes, but new discoveries about the role of saturated stearic acid in the mitochondria point the finger at diets low in animal fats.
THE KIDNEY IS ONE OF the body’s most important organs and systems. Properly functioning kidneys are essential for maintaining normal blood volume and composition; for filtering and excreting or saving various chemical metabolites; and for helping to maintain proper blood pressure. Hypertension (high blood pressure) can result from improperly functioning kidneys. Research carried out during the last few years indicates that both saturated fat and cholesterol play important roles in maintaining kidney function, as do the omega-3 fatty acids.
The kidneys need stable fats both for their cushioning and as their energy source. The fat around the kidneys is very hard, because it has a higher concentration of saturated fatty acids than are found in any of the body’s other fat deposits. These saturated fatty acids are myristic acid (the fourteen-carbon saturate), palmitic acid (the sixteen-carbon saturate), and stearic acid (the eighteen-carbon saturate). When we consume various polyunsaturated fatty acids in large amounts, they are incorporated into kidney tissues, usually at the expense of oleic acid, because the body resists changing the normal high level of saturated fatty acids in the kidney fat.8 Myristoylation is a particularly active process in kidney function, so saturated fat supports the internal workings of the kidney as well.
“WHATEVER IS THE CAUSE OF heart disease,” wrote the eminent biochemist Michael Gurr, “it is not primarily the consumption of saturated fats.”9 In fact, a careful look at the scientific literature indicates that saturated fats play a beneficial role in cardiovascular health. For example, a strong marker for proneness to heart disease is something called lipoprotein-a or Lp(a), which tends to be higher in those with coronary heart disease (CHD), cerebrovascular disease (CVD), atherosclerosis, thrombosis and stroke.10 High Lp(a) predicts risk of early atherosclerosis independently of other cardiac risk factors, including LDL. One study from Tanzania found that vegetarians have higher levels of Lp(a) than fish eaters, leading to speculation that the types of fats in fish oil could be helpful to lower Lp(a).11
But the real surprise is the finding that saturated fats actually lower Lp(a).12 Other research indicates that saturated eighteen-carbon stearic acid and sixteen-carbon palmitic acid are the preferred foods for the heart, which is why the fat around the heart muscle is highly saturated, just like the fat around the kidney.13 The heart draws on this reserve of fat in times of stress. These findings—that saturated fat lowers Lp(a) and serves as the preferred food for the heart—are buried in their respective scientific reports, and not mentioned in the abstracts.
We’ve all heard the accusation “Saturated fats clog the arteries,” as though our arteries were some kind of pipe and saturated fats build up in the arteries the way that grease does when poured down the drain. Actually, the artery “clogs” occur inside the intima, that is, inside the lining of the artery, as biological tissue and not as pure fat stuck to the smooth warm arteries. The fat in artery “clogs” is actually only about 26 percent saturated. The rest is unsaturated, of which more than half is polyunsaturated—a very unnatural situation in human biochemistry.14 In most human tissues, polyunsaturated fatty acids comprise less than 10 percent of the total.
One recent study blames saturated fat for blood vessel inflammation. Published in the American Heart Association journal Circulation Research and entitled, “Pro-inflammatory Phenotype of Perivascular Adipocytes: Influence of High-Fat Feeding,” the authors found more markers of vascular inflammation in mice placed on a “high-fat Western diet.”15 But nowhere in the article or the accompanying press release do the authors disclose the type of fat they fed to the mice.
After an e-mail query, Neil Weintraub, the principal study author, revealed the feeding formula they used—the fat used was indeed an animal fat, what the industry calls anhydrous milk fat; that is, butterfat with most of the moisture removed. The other main components of the formula were casein (20 percent by weight), sucrose (34 percent by weight) and cornstarch (15 percent by weight)—all problematic ingredients that could have contributed to the resulting inflammation. As there was no control group fed the same formula but with polyunsaturated oil instead of anhydrous milk fat, the researchers could not compare the effects of mostly saturated versus mostly polyunsaturated fatty acids.
And anhydrous milk fat may not even have the same fatty acid profile as butter. The industry has figured out how to add polyunsaturated fatty acids to milk fat through a process called enzymatic interesterification. But Weintraub believes that his results prove that “high-fat diets” can predispose individuals to heart disease even if they do not have high cholesterol levels. “Many patients who consume high fat diets do not exhibit abnormal lipid profiles, but still develop atherosclerosis nonetheless. These new findings suggest a direct link between poor dietary habits and inflammation of blood vessels.” The study was again funded by the National Institutes of Health, which preaches that “poor dietary habits” mean consumption of foods like meat, butter and cheese, all high in saturated fat.
As saturated fats are stable, they do not become rancid easily, do not call upon the body’s reserves of antioxidants, do not initiate cancer and do not irritate the artery walls. Contrary to everything you hear in the media, saturated fats are safe and healthy. Trans fats from partially hydrogenated vegetables oils and free radicals in processed liquid oils are the likeliest culprits in the current epidemic of chronic disease—a subject we will explore in more detail in Chapter 7.
Even monounsaturated fatty acids—the kind found in olive oil—can be problematic when not supported by adequate saturated fat. According to a 1998 report, mice fed a diet containing monounsaturated fats were more likely to develop atherosclerosis than mice fed a diet containing saturated fat. In fact, the mice fed monounsaturated fatty acids were more prone to heart disease than those fed polyunsaturated fatty acids.16
How much total saturated fat do we need? During the 1970s, researchers from Canada found that animals fed rapeseed oil and canola oil developed heart lesions. This problem was corrected when they added saturated fat to the animals’ diets. On the basis of this and other research, they ultimately determined that the diet should contain at least 25 percent of fat as saturated fat. Among the food fats that they tested, the one found to have the best proportion of saturated fat was lard, the very fat we are told to avoid under all circumstances!17
SATURATED FATS PLAY NUMEROUS OTHER roles within the body. For one, they contribute to the health of our bones. To effectively incorporate calcium into the skeletal structure, at least 50 percent of the dietary fats should be saturated.18
Also, several studies have shown that saturated fat can protect the liver from the effects of alcohol and other toxins, such as Tylenol.*19 For example, a study published in the Journal of Nutrition found that saturated fat from beef tallow reduced alcoholic liver toxicity in rats whereas corn oil increased markers of liver toxicity.20 Moral: if you drink, eat plenty of butter and fatty meats—your liver will thank you.
Yet saturated fat often gets the blame for liver dysfunction. One example is a 2006 study entitled, “Saturated Fatty Acids Promote Endoplasmic Reticulum Stress and Liver Injury in Rats with Hepatic Steatosis,” published in Endocrinology.21 In this study, markers for liver function worsened in rats on a diet high in sucrose (68 percent sucrose, 12 percent corn oil and 20 percent casein) or high in lard (45 percent lard oil, 35 percent cornstarch and 20 percent casein) compared to a high-starch diet (68 percent cornstarch, 12 percent corn oil and 20 percent casein) or a high polyunsaturated diet (35 percent cornstarch, 45 percent corn oil and 20 percent casein). The lard oil diet was described as high in saturated fat, hence the title of the study, which fingers saturated fatty acids. The title contains no mention of the similar adverse effects from the high-sucrose diet; but even worse is the characterization of lard oil as high in saturated fat. The definition of lard oil is “oil consisting chiefly of olein that is expressed [extracted] from lard.” Olein is a monoglyceride of monounsaturated oleic acid; that is, oleic acid joined to a glycerol molecule. Thus the diet described as high in saturated fatty acids was actually high in monounsaturated fatty acids! (And none of the diets could be called normal diets, representative of how and what we actually eat.)
Saturated fats enhance the immune system.22 Transplant patients get specific instructions to avoid saturated fats because they increase the chances of organ rejection—polyunsaturated vegetable oils depress the immune system, resulting in lower rates of organ rejection. Those of us who have not had organ transplants should stick with saturated fats, not polyunsaturated oils, so that our immune systems will function properly and reject whatever is foreign or harmful to the body.
A key component of our immune systems is white blood cells, also called T-cells. When researchers looked at the fatty acid composition of the phospholipids in the T-cells, from both young and old donors, they found that a loss of saturated fatty acids in the lymphocytes was responsible for age-related declines in white blood cell function; they also found that they could correct cellular deficiencies in palmitic acid and myristic acid by adding these saturated fatty acids to the diet.
DHA and EPA are vital for many processes in the body. Saturated fats, especially myristic acid, support the production of these elongated omega-3 fatty acids and are needed for the proper utilization of essential fatty acids.23 Elongated omega-3 fatty acids are better retained in the tissues when the diet is rich in saturated fats.24 Short-and medium-chain saturated fatty acids, such as those found in butter, have important antimicrobial properties. They protect us against harmful microorganisms in the digestive tract.25
Saturated fats support hormone production.26 One study showed that in men, decreasing dietary saturated fat and increasing polyunsaturated fatty acids reduced the amount of androstenedione, testosterone and free testosterone in the bloodstream. Similar results hold for women—consumption of more saturated fat results in higher production of various types of estrogen.27
Finally, let us consider the lungs. Proper lung function depends on a compound called lung surfactant, a soap-like substance that allows the passage of air into and out of the lungs—oxygen-rich air coming in and carbon dioxide–rich air coming out. Surfactant is composed primarily of phospholipids, that is, two fatty acids joined to a phosphate group (a structure similar to the phospholipids that make up the cell membrane). The most common phospholipid in the surfactant contains two sixteen-carbon palmitic fatty acids. This is the ideal structure for air to pass through the surfactant membrane. The passage of air is impeded when the phospholipids incorporate trans fatty acids rather than saturated fatty acids; the membrane tends to break if polyunsaturated fatty acids predominate in the phospholipids.28 Thus saturated fats are essential for lung function—a fact that helps explain the results of several studies showing that children on whole milk and butter diets have less asthma than children eating reduced-fat milk and margarine.29
A molecule of lung surfactant is typically composed of two sixteen-carbon saturated fatty acids.
Current thinking blames lung cancer on smoking or exposure to secondhand smoke, but lots of people get lung cancer who have never smoked and who live in smoke-free houses. Many people who live a “healthy lifestyle” have been shocked to receive a diagnosis of lung cancer. Although the percentage of Americans who smoke has declined by half, we have seen only a slight drop in the rate of lung cancer. Currently, more than one hundred fifty thousand American men and women die of lung cancer every year; it is the leading cause of cancer death and the second most common type of cancer. Lung cancer patients usually receive admonitions to avoid sources of saturated fat, like red meat, but given the basic facts of lung biochemistry, avoiding industrial fats and oils and consuming natural animal fats seems a more rational dietary strategy.
CHOLESTEROL GETS TARRED WITH THE same brush as saturated fat, although the molecules are very different. Both saturated fat and cholesterol are insoluble in water, but they play very different roles in the body’s chemistry.
The richest dietary source of cholesterol is animal fats, but your body can also make cholesterol—about 2,000 milligrams per day. In general, the average American absorbs about 100 milligrams of cholesterol per day from food. So in theory, even reducing animal foods to zero will result in a mere 5 percent decrease in the total amount of cholesterol available to the blood and tissues.
It is worth repeating that cholesterol is vital to the integrity of the cell membrane—but that is only one of its many important roles. Cholesterol acts as a precursor to vital corticosteroids, hormones that help us deal with stress and protect the body against heart disease and cancer; and to the sex hormones like androgen, testosterone, estrogen and progesterone. When cholesterol levels are low, the body cannot make these hormones, especially in times of stress. Infertility, impotency and difficulty dealing with stress are the logical consequences.
Cholesterol is a precursor to vitamin D, a vital fat-soluble vitamin needed for healthy bones and nervous system, proper growth, mineral metabolism, muscle tone, insulin production, reproduction and immune system function; and it is the precursor to bile salts, which are vital for digestion and assimilation of fats in the diet.
The subject of antioxidants is everywhere in the news these days, as people look to increase their fruit and vegetable intake to protect themselves against cancer. But we never hear about the role of cholesterol as an antioxidant. Research shows that cholesterol acts as a vital antioxidant in the cell membrane.*30 As an antioxidant, cholesterol protects us against free radical damage that leads to heart disease and cancer.
Cholesterol is the body’s repair substance, manufactured in large amounts when the arteries are irritated or weak. Scar tissue is rich in cholesterol. Blaming heart disease on high serum cholesterol levels is like blaming firemen who have come to put out a fire for starting the blaze.
Cholesterol nourishes the digestive tract and supports digestive function. Dietary cholesterol plays an important role in maintaining the health of the intestinal wall,31 which is why low-cholesterol vegetarian diets can lead to leaky gut syndrome and other intestinal disorders. And cholesterol helps protect against infection and endotoxins from pathogenic bacteria—especially the vilified LDL-cholesterol, the so-called “bad” cholesterol.32
Cholesterol is needed for proper function of serotonin receptors in the brain.33 Serotonin is the body’s natural “feel-good” chemical. This explains why low cholesterol levels have been linked to aggressive and violent behavior, depression and suicidal tendencies. (More on this in Chapter 9.)
Mother’s milk is especially rich in cholesterol and contains lipase enzymes to ensure that the baby absorbs 100 percent of this nutrient.34 Babies and children lack the enzymes to make cholesterol and require cholesterol-rich foods throughout their growing years to ensure proper development of the brain and nervous system.
Low cholesterol levels are a definite marker for cancer,35 a fact that scientists recognized before the anticholesterol agenda was applied to every man, woman and child in the country. We can do no better than quote verbatim from a 1974 paper on leukemia: “Leukemia in mice and humans is accompanied by a marked deficiency of unesterified cholesterol in the surface membrane of leukemic cells as compared to normal leukocytes. This deficiency induces a significant reduction in their membrane microviscosity. Since cholesterol in the cell surface membrane is exchangeable with the cholesterol in the serum lipoproteins, concomitant to the cellular deficiency of cholesterol, the average levels of cholesterol in the blood serum of leukemic patients is substantially below the average normal level.” And from the conclusion: “A controlled reduction of cholesterol level in normal leukocytes may thus sensitize immune response processes or phagocytic activity above threshold level beyond which malignant transformation and the development of leukemia may occur. On the other hand, a controlled enrichment of cellular cholesterol in leukemic cells may prevent the development of latent leukemia and may hopefully remit leukemia in its active form.”36 In other words, low cholesterol predisposes to leukemia, and higher cholesterol prevents this terrible disease.
More recently, scientists have discovered a novel role for cholesterol, one that explains why low cholesterol is linked to cancer and many other diseases. Cholesterol in cell membranes appears to anchor a signaling pathway linked to cell division and cancer. “Cell signals have to be tightly controlled,” says Dr. Richard G.W. Anderson, chairman of cell biology at UT Southwestern Medical Center. “If the signaling machines do not work, which can happen when the cell doesn’t have enough cholesterol, the cell gets the wrong information, and disease results.”37 The cholesterol-containing regions of the cell membrane are more rigid than the other areas and play a critical role in organizing signaling machinery at the cell surface. The correct arrangement of signaling modules in these domains is vital for communication inside the cell and is dependent on proper levels of cholesterol.
The fact is, higher cholesterol levels are associated with a longer life, especially in the elderly and in women of all ages—a finding confirmed in numerous studies.38 So why is high cholesterol associated with increased risk of heart disease in young and middle-aged men? The likely explanation is the fact that at this age, men are in the midst of their careers and subject to high levels of stress. Since cholesterol provides the building blocks of stress hormones, cholesterol levels rise to provide protection—obviously not always successfully. Sometimes the effects of a stressful lifestyle are so great that they overwhelm the protective system that cholesterol provides.
THE HUMAN TONGUE HAS REMARKABLY sensitive receptors for fat. Test subjects showed a response in the blood when they tasted potatoes mashed with butter, but no response when they tasted mashed potatoes without fat, or mashed potatoes made with fat substitutes.
The biochemical response to tasting mashed potatoes with butter was elevated triglycerides, which investigators say is a bad thing. But if the human tongue has a taste for fat, that must mean humans need fat. Perhaps the fat taste buds steer people toward foods that contain essential fatty acids, say puzzled investigators. But most natural nonfatty foods contain some essential fatty acids—even potatoes. The logical conclusion is that the human body knows better than thousands of politically correct nutritionists that humans need high-fat foods, so much so that it possesses a delicate instrument for determining which foods contain lots of fat. So precise is the human taste for fat that it can distinguish real fat from imitation fat substitutes like Olestra.39
How long can medical orthodoxy oppose the consumption of saturated fat and cholesterol in the face of contradictory evidence? Animal foods containing saturated fat and cholesterol provide vital nutrients necessary for growth, energy and protection from degenerative disease. Like sex, animal fats are necessary for reproduction. Humans are drawn to both by powerful instincts. Suppression of natural instincts leads to weird nocturnal habits, fantasies, fetishes, bingeing, purging and splurging.
Young people these days, especially young women, grow up in a culture of fat phobia. Our natural appetite for fats gets suppressed in the fearmongering and finger wagging that permeates the media and the classroom—from nutrition lessons to fashion magazines. The result is eating disorders and a culture of thinness. Those who can resist the lure of satisfying fats keep themselves too thin, and those who can’t resist give in instead to carb bingeing and let themselves get fat.
Fat cells, called adipocytes, are often blamed for conditions like diabetes, cancer and heart disease, but they may actually protect us against these illnesses. Researchers at Purdue University have discovered that pig fat cells (very similar to human fat cells) help regulate energy metabolism, anti-inflammatory pathways and certain aspects of the body’s immune response that protect us against bacterial toxins. In addition, normal adipocytes produce factors that promote insulin regulation of glucose levels. These regulatory mechanisms are absent in people who are too thin, and are thwarted in the case of obesity, when the adipocytes enlarge due to lipid accumulation.40
This research gives new meaning to the phrase “pleasingly plump.” A nice layer of fat—not too much but also not too little—goes a long way to ensuring good health. Animal fats are nutritious, they are satisfying, and they taste good. And yet the high priests of the lipid hypothesis continue to lay their curse on the fairest of culinary pleasures—butter and béarnaise, whipped cream, soufflés and omelets, full-bodied cheeses, juicy steaks and pork sausage. Our bodies know better; they know that the very foods that we love to eat also support everything from breathing to energy production to feeling good. Those who deny themselves these pleasures tend to live with chronic sadness or smoldering rage.