CHAPTER 9
Animal Fats for the Mind
Smith-Lemli-Opitz Syndrome (SLOS) is a genetic disorder that prevents the body from manufacturing all the cholesterol it needs. Symptoms include intellectual disability, hyperactivity, irritability, poor attention span and tendency toward aggressive and self-injuring behavior. The most common treatment for SLOS is a cholesterol supplement, which leads to improvement in many of the symptoms found in SLOS patients—including hyperactivity, irritability, attention span, muscle tone, endocrine function, resistance to infection and gastrointestinal problems.
Twenty-five percent of the body’s cholesterol resides in the brain—an organ that provides only 2–3 percent of the body’s total weight. Cholesterol is so critical to the brain and all its functions, that it manufactures cholesterol on-site.1 Most of this manufacture occurs at night, during sleep, which is one of the reasons a good night’s sleep is so important to mental function.
Until recently, scientists held that cholesterol in the bloodstream could not get past the blood-brain barrier and that, as a consequence, the brain made all its own cholesterol. But the fact that cholesterol supplements uniformly help those suffering from SLOS indicates that at least some cholesterol from the bloodstream does pass into the brain. In 2010, scientists confirmed the fact that the brain is not a “closed circuit,” but that it can take cholesterol from the bloodstream as needed.2 In the elderly, eggs improve memory,3 again indicating that dietary cholesterol can be sequestered into the brain.
To better understand the role cholesterol plays, it’s important to look at the way the brain functions. Two types of cells populate the brain. First are the neurons, cells specialized to pass signals to other neurons or to other target cells. These signals—which can be electrical or chemical—pass across structures called synapses. All mental function—thoughts, memories, reasoning and learning—depends on the formation of synapses.
The other main type of cell in the brain and nervous system are the glial cells—from the Greek word for glue. These are nonneuronal cells that maintain homeostasis and provide support and protection for neurons in the central and peripheral nervous systems.
During sleep, the genes in the glial cells needed for the synthesis and maintenance of myelin become active. It is the glial cells that form myelin—a kind of electrical insulation material around the neurons, allowing them to send electrical impulses in a quick and orderly way. The myelin is especially rich in cholesterol. Multiple sclerosis is an illness in which the myelin sheaths are inadequate or disintegrating—yet typical advice for MS sufferers is to avoid saturated fat and full-fat dairy foods on the false premise that saturated fats cause inflammation. Butter, egg yolks, liver and saturated animal fats are some of our best sources of cholesterol, the essential building material of myelin, and the saturated fats they contain help resolve inflammation; they would seem to be the logical first treatment for this dreadful degenerative disease.
For over a century, investigators believed that the glial cells did not play any role in neurotransmission. However, we now know that the glial cells assist the neurons to form connections across the synapses.4 Early research discovered an unidentified compound made by glial cells that was responsible for the ability of neurons to form synapses. Without this “glial factor,” neurons formed few synapses, and the synapses they did form were inefficient and poorly functioning. In the presence of glial cells, which secrete the unknown factor, neurons formed many highly efficient synapses.
It was in 2001 that researchers identified the mysterious glial factor—it was cholesterol! The glial cells release the cholesterol in a carrier called apolipoprotein E (apoE). At first, the investigators thought that apoE was the glial factor itself, but neurons treated with apoE did not show any increased synapse formation. The apoE carries a number of compounds, including phosphatidylcholine, sphingomyelin and cholesterol. Yet only cholesterol increased synapse formation when applied to the neurons—in fact, a solution of cholesterol increased synapse formation twelvefold. The other compounds had little effect and actually inhibited synapse formation at high doses.5
The investigators then used the cholesterol-lowering drug mevastatin to reduce cholesterol secretion by the glial cells. The reduced-cholesterol glial secretion had a strongly diminished effect on synapse formation. When they added cholesterol back to the low-cholesterol secretion, synapse formation was fully restored.
The authors identified cholesterol as a limiting factor of synapse formation. In other words, low availability of cholesterol can directly limit the ability to form synapses.
CHOLESTEROL DOES MORE THAN HELP fire the synapses; it also helps the brain’s neurons grow and connect. Neurons have many tentacles or arms, which connect the neurons with other neurons, or with muscles across synapses. These arms are called neurites: those that send impulses away from the cell are called axons and those that receive impulses are called dendrites.
The synapses in our brains, where axons and dendrites meet, are constantly breaking and re-forming. The neurites grow toward other neurites in response to a stimulus given by a signaling protein in the membranes of neurons. These signaling proteins rely on cholesterol-rich lipid rafts (see Chapter 4), where long-chain saturated fatty acids secure some of the proteins. A 2004 study found that when investigators removed some of the cholesterol from the lipid rafts in the neuron membrane, the neurons could not find the signaling proteins.6
Because one of the characteristics of Alzheimer’s is a cholesterol by-product in the brain, the dietary gurus promote low-fat, low-cholesterol foods as brain-healthy and a way to prevent Alzheimer’s. But what the current research shows us is that the brain is completely dependent on cholesterol to function properly—for all thought processes and all memory—for reading, reasoning and relationships.
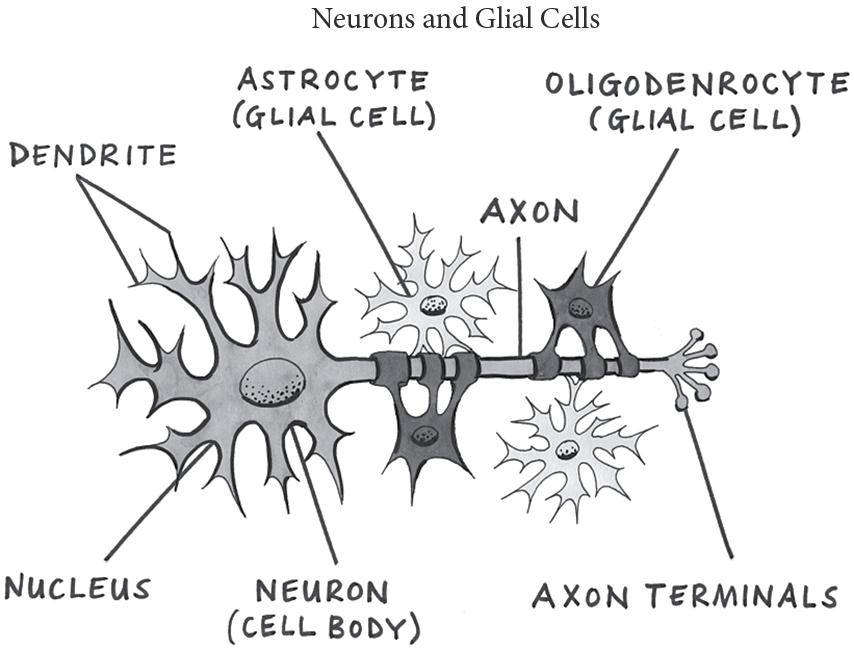
Glial cells attached to the neurons use cholesterol to support synapse formation.
The traditional view of human brain development is that babies are born with all the brain cells they will ever have, and that neurological development occurs through the connection of these cells in the early years. We now know that from birth through late adolescence, the brain adds billions of new cells, constructing its circuits out of freshly made neurons as children and teenagers interact with their environments. In adulthood, the process of adding new cells slows down but does not stop. Mature brain circuits appear to be maintained by new cell growth well into old age.7 In addition, the neurites are constantly seeking new connections, and the synapses fire millions of times per second.
These discoveries reveal why everyone benefits from high-cholesterol foods. For infants and growing children, who don’t make all the cholesterol they need, these foods are essential for optimal intellectual growth. For adults, these foods may be the critical input to protect against degenerative diseases like Alzheimer’s and even just annoying conditions like short-term memory loss.
High levels of cholesterol in the blood provide protection against mental decline. A 2005 Swedish study analyzed data from three hundred ninety-two men and women in Göteborg, Sweden, over an eighteen-year period. Researchers found that high total cholesterol at ages seventy, seventy-five and seventy-nine was associated with a reduced risk of dementia between ages seventy-nine and eighty-eight.8 American researchers found that in the elderly, the best memory function was observed in those with the highest levels of cholesterol. Low cholesterol was associated with an increased risk for depression and even death.9
These discoveries also show the increased risk of taking cholesterol-lowering statin drugs, which are so often associated with mental decline, amnesia and neurological disorders like Parkinson’s disease. But scientists wedded to the cholesterol theory of heart disease dare not make so bold a statement. Referring to the Swedish study, Michelle M. Mielke of the Center on Aging and Health at Johns Hopkins Bloomberg School of Public Health stated: “These findings raise more questions than they give answers. Therefore, we strongly urge that consumers not make changes in their diet or medication without consulting with their doctors first.” Rachel Whitmer, a research scientist specializing in cognitive aging at Kaiser Permanente Northern California Division of Research, also danced around the issue: “Lingering questions were not put to rest, but new exciting ones are raised… This study is another example of the importance of timing in terms of when one measures a risk factor, and the need to consider risk factors for dementia over the entire life course.”10
A 2005 follow-up to the famous Framingham Heart Study, published in Psychosomatic Medicine, found that lower naturally occurring total cholesterol levels were associated with poorer performance on cognitive measures such as abstract reasoning, attention, concentration, word fluency and executive functioning. Once again, double-talk was necessary: “Competing risks must always be taken into consideration,” said the researchers. “Lower cholesterol values may have modestly detrimental effects on cognitive function for the individual but, depending on the patient’s risk profile, may have beneficial effects with respect to cardiovascular morbidity and mortality.”11
It seems that cholesterol is important for neuromotor reactions as well. In 2009, the military funded a study to find out which foods are best for pilots. Since the military has a lot invested in pilots, they wanted to know which kind of diet supported them the best. University of North Dakota researchers found that forty-five pilots who ate the fattiest foods, such as butter or gravy, had the quickest response times in mental tests and made fewer mistakes when flying in tricky cloud conditions.*12
A growing body of research supports the idea that diets rich in animal fats improve and protect brain function in many ways. Animal fats supply much-needed cholesterol—cholesterol for the brain forming in utero, cholesterol for the brain that is growing and maturing in the infant and child, and cholesterol for the mature brain of the adult. In principle, an adult can make all the cholesterol he or she needs, but why not give the complex cholesterol-production mechanism relief by supplying as much cholesterol as possible from the diet, through sources like chicken liver, beef liver, chicken and turkey giblets, meat fats, egg yolks and butter? These foods nourish the brain in many other ways as well.
AT AGE TEN, BILLY (NOT his real name) could not speak. His parents suspected that he could read, but since he could not communicate with them, they were not sure. The diagnosis: autism. Standardized IQ tests indicated moderate intellectual disability.
His pediatrician, Dr. Mary Megson of Richmond, Virginia, had noticed that night blindness and thyroid conditions—both signs of vitamin A deficiency—were common in family members of autistic children. Billy’s mother had a thyroid condition and also suffered from dry eyes (another sign of vitamin A deficiency) and gluten intolerance.13
Megson began giving Billy cod liver oil, supplying the boy with 2,500 IU vitamin A twice daily. After one week, his behavior began to change—he began to sit farther from the television and to notice paintings on the walls at home. He started running across the grass from the front door to the school bus—while before he had carefully followed the sidewalk and driveway to the bus. After three weeks, Megson gave Billy a small dose of a pharmaceutical version of choline, called Urocholine. Thirty minutes later, Billy swung his feet over the side of the chair, pointed to a glass candy jar on the shelf and spoke his first words in eight years: “May I have the red Jolly Rancher, please?” His parents now had proof that he could read.*
Megson and his mother took him outside. “The leaves, the leaves on the trees are green!” he said. “I see, I see!” When Megson asked to take his picture, he looked at the camera, smiled and waved. When he left the office, Megson said, “See you later,” to which he responded, “What time?”
As Dr. Megson explains, in genetically predisposed children, autism is linked to a G-alpha protein defect. G-alpha proteins form one of the most prevalent signaling systems in our cells, regulating processes as diverse as cell growth, hormonal regulation and sensory perception—like seeing. The defect may be triggered by a variety of factors, especially when the child is already deficient in vitamin A, and cause the separation of the G-alpha protein from retinoid receptors. Vitamin A helps reconnect the retinoid receptors.
Children like Billy do not see the way people with normal vision do. Dr. Megson explains: “These children live in a ‘magic-eye puzzle:’ you’ve probably seen these puzzles at the mall. You stare at a cluster of shapes and colors, and eventually an image will pop out. These children, because of the blocked pathway affecting their vision, can’t see like most people do. The blocked pathway has caused the rods in their eyes to not function correctly. They must compensate for the rod dysfunction the best way they can. They ‘see’ the world around them as though it’s in a 3-D box. They have such a limited visual field that everything that doesn’t fit in their box blurs and is perceived as color and shape alone. And, the most incredible thing is that they actually have to piece together each ‘box’ that they see in order to see a complete shape.”
According to Megson, the blocked visual pathways explain why children on the autism spectrum “melt down” when objects are moved or when you clean up their lines or piles of toys sorted by color. They work hard to piece together their world; it frightens and overwhelms them when the world as they are able to see it changes. It also might explain why children on the autism spectrum spend time organizing things so carefully. It’s the only way they can “see” what’s out there.
Megson claims that their main issue is a visual problem. They typically look at things sideways—including at parents telling them to “look at me.” They turn their eye so that the light reflected off the parent’s face lands on the edge of the fovea or the lateral retina, where they have some rod function remaining. The fovea is the area in the back of the eye where the cones are closest together. When you force the child to look directly at you, you are actually forcing them to look away from you because their only good field of vision is off to one side.*
With vitamin A from cod liver oil, Megson has witnessed improved rod function—vitamin A is not called retinol for nothing. She’s seen the sideways glance, so typical of an autistic child, disappear in front of her. Megson believes that Vitamin A—along with the jolt of pharmaceutical choline—made the connections that facilitated Billy’s speech as well. The retinoid receptors are critical not only for vision but for sensory perception, language processing and attention.†
What’s interesting is that Dr. Megson feels that the retinol form of vitamin A is absorbed best—retinol being the form found in butter and in the livers of animals and fish. Most vitamin supplements and infant formula contain vitamin A palmitate, which is not effective in connecting the G-alpha proteins to the retinoid receptors. Of all the food sources of retinol vitamin A, fish liver oil is the only source of a form of vitamin A called 14-hydroxy-retro-retinol (14-HRR). G-protein defects can block the conversion of vitamin A into this 14-HRR.
Urocholine is a prescription drug that stimulates the release of acetylcholine at nerve endings, and acts like an artificial acetylcholine. (Bethanechol is the generic name for Urecholine.) It stimulates gastric motility, increases gastric tone and often restores impaired rhythmic peristalsis of the intestines. It also increases bile and pancreatic secretions and indirectly stimulates the vitamin A receptors in the brain’s hippocampus.‡
In Billy’s case, he continued to improve as long as he faithfully took his cod liver oil and small doses of Urecholine. When he did not take it, he quickly regressed.
Megson’s work with Billy and other patients on the autism spectrum is supported in studies of mice. Researchers at the Salk Institute for Biological Studies found that removing vitamin A from the mouse diet diminishes chemical changes in the brain considered the hallmarks of learning and memory. Lack of vitamin A interferes with optimal function of the hippocampus. Earlier work indicated that mice born without receptors for vitamin A in the hippocampus performed under par in standardized learning tests. When vitamin A is added back to the diets of the mice, the impairment is reversed. Said the researchers, “These data suggest a major mental consequence for the hundreds of millions of adults and children who are vitamin A deficient.”14
Billy’s case, and others like it, indicate that vitamin A from animal fats like butter and cod liver oil can have profound effects on mental function and behavior. We need more of these old-fashioned foods to protect our young people from modern diseases.
SHAPED LIKE A SEAHORSE, THE hippocampus resides deep in the brain, halfway between the ears and the midpoint of the skull. Considered the seat of memory—humans in whom the hippocampus is damaged or removed cannot form memories of near-term experiences—the current view holds that the organ plays a key role in learning. The hippocampus also seems to play a role in spatial memory and navigation, impulse control and even olfaction—the sense of smell. In Billy’s case, vitamin A helped support hippocampus function as vitamin A is required to support neuroplasticity in the hippocampus; this is one reason that vitamin A deficiency will depress learning and memory.15 And if a lack of vitamin A results in impaired function of the hippocampus, so does a lack of vitamin D.
Aging rodents—one pictures rats in slippers and bathrobes—have helped researchers define the relationship between vitamin D and cognitive decline. Using middle-aged rats, scientists found that rats with high levels of vitamin D in their blood outperformed low and medium groups in an activity called maze reversal, a particularly challenging task for the aging rodent, one that detects subtle changes in memory. Their explanation was that vitamin D optimizes gene expression in the hippocampus—improving the “likelihood of successful brain aging,” an outcome desirable for both aging rats and aging humans.16
The discovery of vitamin D, its activating enzyme and vitamin D receptors in the brain has the research community aglow with enthusiasm about the role of vitamin D in neurological function. It seems that vitamin D is critical for brain development, brain protection (through programmed cell death), nerve growth throughout life, maintenance of glial cells and normal brain function. Vitamin D deficiency is associated with cognitive impairment, dementia, Parkinson’s disease, multiple sclerosis, epilepsy and schizophrenia.17
Vitamin D has also shown neuroprotective effects, including the clearance of amyloid plaques, a hallmark of Alzheimer’s disease.18 Associations of low vitamin D with Alzheimer’s disease and dementia emerged in an important European study, published in 2005.19 Researchers found that the risk of cognitive impairment was up to four times greater in severely deficient elders.20 Vitamin D seems to protect against stroke,21 and two large prospective studies indicate that low vitamin D concentrations may increase the risk of cognitive decline.22
However, study results on vitamin D and brain health are not uniform. Two studies, conducted in an older middle-aged healthy population who were participating in the Atherosclerosis Risk in Communities (ARIC) Brain MRI Study, failed to find significant associations between lower levels of vitamin D and lower cognitive test scores, dementia risk or the development of brain pathologies.23
But the link between low vitamin D and dementia was clear in a 2014 study, which found that participants who were severely vitamin D deficient were more than twice as likely to develop dementia and Alzheimer’s disease.24 Adults in the study who were moderately deficient in vitamin D had a 53 percent increased risk of developing dementia of any kind, and the risk increased to 125 percent in those who were severely deficient. Similar results were recorded for Alzheimer’s disease, with the moderately deficient group 69 percent more likely to develop this type of dementia, jumping to a 122 percent increased risk for those severely deficient.
A COMMON CHARGE LEVELED AGAINST vitamin A is the accusation that it causes depression. The main argument for this is the observed side effect of Accutane—a synthetic type of vitamin A used to treat acne—namely, depression and suicide.
But Accutane is not vitamin A; in fact, evidence indicates that it can cause vitamin A deficiency. When newborn mice receive treatment with dexamethasone, a drug that damages lung tissue, natural vitamin A helps treat the condition while the active ingredient of Accutane has no effect and may even make it worse.25 Accutane can cause night blindness, a traditional sign of vitamin A deficiency, whereas vitamin A supplementation is the treatment that cures night blindness.26 In rats, the active ingredient of Accutane accumulates in the eyes and interferes with vitamin A recycling; rats receiving it at high doses took fifty times longer to recover from exposure to intense light than controls.27
Natural vitamin A can actually resolve depression—this is the conclusion of a physician who had two patients who developed depression while taking Accutane28; when the physician took them off the drug and supplemented them with 10,000–12,000 IU of vitamin A for seven to ten days, the depression resolved.*
Researchers have not examined the relationship between vitamin A status and depression, but it appears that the physical ailments associated with such mental illnesses can be associated with vitamin A deficiency. For example, the incidence and severity of Crohn’s disease and ulcerative colitis, the two most common forms of inflammatory bowel disease, and the incidence and severity of asthma in children, are all associated with deficient blood levels of vitamin A.29 These findings imply that vitamin A might be involved in preventing depression or anxiety as these conditions often have depression as a side effect.
Looking at the evidence carefully, one can conclude that natural vitamin A might not cause depression, but actually chases away the blues.† While research has yet to confirm a direct link, the evidence is building. However, owing to vitamin A’s low status in the vitamin hierarchy, most scientists still stand behind the idea that vitamin A causes depression.30
THE ESKIMOS ARE A HAPPY people. This is the observation of many anthropologists who have lived with this resourceful population. The exception is a kind of hysteria called pibloktoq, a disorder where the victim becomes irritable and withdrawn, and then, in a sudden excitation, leaves the camp and engages in irrational and dangerous behavior. After that come convulsive seizures and a twelve-hour period of coma or stuporous sleep. Only after this train of events does the afflicted person’s behavior become normal again.
In the first paper to describe pibloktoq, published 1985, vitamin A got the blame.31 The researcher noted that the Eskimos consider polar bear liver, which is the richest source of vitamin A, to be toxic. Explorers who ate polar bear liver out of necessity experienced drowsiness, irritability, headaches and nausea within hours of consuming it. Case reports of vitamin A toxicity describe irritability, drowsiness, double vision and anorexia.
Pibloktoq proved perplexing for researchers, however. The Eskimos consumed a diet rich in vitamin A throughout the year, while the specific symptoms of pibloktoq occurred in Arctic latitudes only in late winter and early spring. Furthermore, they consider polar bear liver safe as long as the membrane is removed. And they eat seal liver, which is also high in vitamin A, in unlimited quantities. How is vitamin A toxicity to blame?
A better theory ties pibloktoq to tetany, which is characterized by involuntary muscle contractions and caused by severe deficiencies of calcium and vitamin D. The muscle contractions occur because the peripheral nerves cannot regulate their impulses without calcium. Other symptoms of tetany include “emotional and cognitive disorganization” and convulsive seizures, probably resulting from the absence of calcium in the central nervous system. As with pibloktoq, episodes are acute and sporadic.
The primary source of vitamin D and calcium in the Eskimo diet is fish, and in the late winter and early spring, when stores of dried fish may become depleted, vitamin D and calcium deficiencies may occur.* These two nutrients are critical for the production of endocannabinoids—and one of the roles of these calming chemicals is the prevention of seizures.
VITAMIN K2—THE THIRD IN OUR triumvirate of fat-soluble vitamins—supports cognitive processes in a variety of ways. The brain contains one of the highest concentrations of vitamin K2 in the body; only the pancreas, the salivary glands and the cartilaginous tissue of the sternum contain more.† Vitamin K2 supports the formation of compounds called sphingolipids in both the neurons and the glial cells, and in this way vitamin K2 is critical to optimal myelination of the nerve cells. Also, there is growing evidence that the most prevalent vitamin K2 isomer has anti-inflammatory activity and offers protection against oxidative stress.
In addition to supporting sphingolipid function, vitamin K2 supports the enzymes within the brain that produce an important class of fats called sulfatides, two fatty acids—again, saturated fatty acids—attached to, among other things, a sulfur molecule. The levels of vitamin K2, vitamin K–dependent proteins and sulfatides in the brain decline with age; and low levels are associated with neurological degeneration in the elderly.32 Alzheimer’s patients have up to 93 percent lower sulfatide levels in the brain.33 Animals that completely lack the enzymes to make sulfatides progressively suffer from growth retardation, loss of locomotor activity, weak legs and seizures.34
ANIMAL FATS PROVIDE NOT ONLY vitamins A, D and K2 for our brains but other nutrients as well. One of these is choline. Choline is involved in the process of brain cells making connections with each other. In humans, higher dietary choline is related to better cognitive performance and sharper memory—in other words, those who ignore conventional dietary advice and eat plenty of egg yolks and liver, our best sources of choline, have a better chance of keeping all their marbles into old age.
Want smart children? Then Mom needs to consume an abundance of food containing choline while pregnant, and give lots of choline-rich foods—egg yolks and pureed liver—to baby, especially during the critical first two years when a large portion of the nerve connections are made. Brain function in baby rats was enhanced by feeding extra choline during the equivalent of the third trimester of pregnancy, according to a 1998 study at Duke University Medical Center. The offspring performed significantly better on memory tests than those of mothers with the normal intake of choline. Researchers found that choline enhanced a brain function responsible for paving the path between nerve cells, allowing electrical messages to travel more easily. The improved brain wiring persisted in the rats through early adulthood.35
And then we have our fatty acid brothers, DHA and AA, found primarily in certain nutrient-dense animal foods—DHA in seafoods like oily fish, cod liver oil, shellfish and fish eggs, and AA in butter, animal fats and organ meats. Together, these two fatty acids make up 20 percent of the fats in the brain.
DHA is essential for the growth and functional development of the brain in infants and for maintenance of normal brain function in adults. The inclusion of plentiful DHA in the diet improves learning ability, whereas deficiencies of DHA are associated with deficits in learning.36 DHA is taken up by the brain in preference to other fatty acids. The turnover of DHA in the brain is rapid, although saturated fats ensure that DHA stays in the tissues as long as possible.
DHA deficiencies are associated with fetal alcohol syndrome, attention deficit hyperactivity disorder, cystic fibrosis, phenylketonuria, unipolar depression, aggressive hostility and a degenerative disease called adrenoleukodystrophy.37 Higher DHA levels in middle-aged adults are related to better performance on tests of nonverbal reasoning and mental flexibility, working memory and vocabulary.38 DHA deficiency is associated with cognitive decline,39 and DHA levels are reduced in the brain tissue of severely depressed patients.40
AA seems to play roles similar to those of its DHA brother. For example, low AA contributes to neurological disorders such as Alzheimer’s disease and bipolar disorder.41
However, study results for both DHA and AA are mixed, probably because many researchers use the algae-derived, synthetic forms of these nutrients, rather than natural forms in whole foods like cod liver oil, liver and butter. These natural foods also supply vitamins A and D, which help regulate the actions of these important fatty acids. For example, calcium supports the conversion of AA to other compounds in the cells, and we need vitamin D to properly maintain the proper levels of calcium in the blood and tissues. Vitamin A works with vitamin D in many ways and also helps us synthesize AA from omega-6 fatty acids in plant foods.42 In nature, the fatty acid twins occur in the same foods that provide us with vitamins A and D; scientists giving supplements of algae-derived DHA and AA to patients lacking vitamins A and D should not expect beneficial results.
CANNABINOIDS, OPIATES (SUCH AS heroin and morphine), and cocaine come from plants. One of the great discoveries of modern science is the finding that our bodies can manufacture the same feel-good compounds. Moreover, we have receptors for these compounds, especially in the brain and the nervous system, and also in surprising places like the pancreas and the liver. Endorphins (from “endogenous morphine”) like serotonin and dopamine are produced by the central nervous system and the pituitary gland, while endocannabinoids are formed during neurotransmission.*
The earliest clear description of the use of opium as a recreational drug comes from China, where opium was promoted as increasing masculinity and vigor. Opium became popular during the eighteenth century as a remedy for nervous disorders. Recognizing its sedative and tranquilizing properties, physicians gave it to those with psychosis or insomnia, and to help treat people considered insane. But the dark side of “God’s Own Medicine,” as it was called, soon emerged. Doctors noted that in cases of psychosis, opium could cause anger, and that the drug’s euphoric effects often gave way to depression.
In the nineteenth century, the most common use of opium was for the treatment of “female problems,” usually to relieve menstrual pain. Unfortunately, the treatment was addictive. Up to two hundred thousand opiate addicts lived in the United States in the late nineteenth century, and between two-thirds and three-quarters of these addicts were women.43
Cocaine acts by inhibiting the reuptake of the endorphins serotonin and dopamine. This results in greater concentrations of these neurotransmitters in the brain, with a stimulating and feel-good effect. Cocaine increases alertness, feelings of well-being and euphoria, energy and motor activity, and feelings of competence and sexuality. Unfortunately, after the high comes the body’s reaction—which is lower-than-normal levels of serotonin and dopamine in the brain, leading to anxiety, restlessness and depression.
Along with endogenous cannabinoids and opiates, scientists have discovered a neuropeptide and neurotransmitter called CART, which elicits behavior in animals similar to that of cocaine and amphetamine. CART is found at the same locations where cocaine and methamphetamine act in the brain, leading to speculation that CART serves as an “endogenous cocaine.”44
A KEY FACTOR IN LEADING a successful life is the ability to deal with stress. Everybody encounters stress. Those who use this stress as a springboard for action can accomplish many good things; those who are paralyzed by stress can disappear down the rabbit hole of depression and anxiety.
One of the potential reactions to stress is the fight-or-flight response. The adrenal glands produce the hormone cortisol, which raises blood sugar, increases muscle tension and strength, and prepares us for the kind of extreme reactions needed in situations of danger or urgency. However, the body is not designed to be in a fight-or-flight mode all the time. If we react to the minor stresses in our daily lives with the fight-or-flight response, we develop chronic disease or burn out.
The endocannabinoids are key regulators of cortisol production. Do we chill out or freak out with minor stresses? Our internal marijuana production may determine the outcome.†
Researchers can create a stress reaction in rats by physically restraining them for thirty minutes. The rats become terrified and their blood levels of fight-or-fight hormones increase sevenfold. When they are given a drug that raises the level of natural endocannabinoids in the brain, however, these hormones only rise two-to threefold.45
Scientists can study the reaction of rats to stress in another way, using the “elevated zero maze.” Rats are placed in a maze held high off the ground and are given the opportunity to stay in closed spaces or explore open spaces—the freaked-out, fearful rat will stay in an enclosed space; the chilled-out rat will be curious and explore. Rats on an ordinary lab chow diet spend only 20 percent of the time in open spaces, but rats given a drug that raises the level of natural endocannabinoids spend about half the time in the open spaces.46 This finding suggests that the levels of endocannabinoids in the brain determine whether our behavior is cool and productive, or fearful and stressed.
Endocannabinoids made within the body activate the same receptors as THC, the active component of marijuana, but without the undesirable effects. While the study of endocannabinoids is in its infancy, we already know that this system of multipurpose chemicals plays many roles, including balancing short-term and long-term memory; developing nerve cells in the hippocampus; regulating appetite, hunger, taste perception and the pleasure value of food; modulating the stress response—or as scientists would put it, regulating “the organism’s overall sense of arousal during novel situations”; reducing pain; determining the receptivity of the uterus to embryonic implantation; regulating intestinal motility for normal digestion and elimination; and protecting against diabetes, cardiovascular disease and multiple sclerosis. In other words, wherever researchers have looked, they have found the family of endocannabinoids playing critical roles in helping us feel well and helping the body to work normally.
Do animal fats play a role in helping us produce these feel-good chemicals? Yes, they do! Arachidonic acid—that magical omega-6 fatty acid we get from animal fats—is the direct precursor to the endocannabinoids; and a brain cell will convert arachidonic acid into endocannabinoids only in response to a rapid influx of calcium into the cell—which means that vitamin D is intimately involved in this process.*47 If calcium is not present, due to deficiency of either calcium or vitamin D, there will be no influx of calcium into the cell to initiate the conversion of arachidonic acid to endocannabinoids.
If our internal cannabinoids are not working, or if we can’t make them due to a lack of AA and vitamin D—and also vitamins A and K2 and saturated fats, because all these compounds work together—we feel terrible. A diet without sufficient animal fat, and sufficiently nutrient-dense animal fat, leaves your cannabinoids lacking. We feel chronically depressed, anxious and tense. Enter marijuana to give a temporary high—a temporary sense of feeling normal—followed by its unfortunate aftereffects, which make you feel worse than before.
ENDORPHINS—NATURAL HEROIN COMPOUNDS LIKE SEROTONIN and dopamine, along with their binding proteins and receptors—also occur throughout the body. Like the endocannabinoids, they are involved in multiple processes, not just helping us feel good, but making sure the body functions properly. Derived from the amino acid tryptophan, serotonin is produced primarily in the intestinal tract, where it regulates intestinal movement; the rest is produced in the central nervous system, where its functions include regulation of mood, appetite and sleep; support of memory and learning, and direct brain development in the womb.
The blood platelets store serotonin, and when these platelets bind to form a clot, they release serotonin, which helps vasoconstriction and works to prevent both excessive clotting and bleeding. Serotonin also plays a role in wound healing. When humans smell food, the release of dopamine increases appetite; serotonin works to decrease appetite. Low levels of serotonin receptors are associated with increased weight gain. If irritants are present in food, the gut releases more serotonin to make digestion move faster, resulting in diarrhea to empty the gut of the offending substance. If serotonin is released into the blood faster than the platelets can absorb it, serotonin receptors are activated to induce vomiting.
In humans, serotonin controls the release of insulin (which regulates blood sugar levels) and also of insulin-like growth factor (IGF) (which regulates growth). Does that mean that happy children achieve optimal growth and happy adults enjoy stable blood sugar? Something to consider.
Serotonin also regulates executive function and social behavior—low levels are associated with attention deficit/hyperactivity disorder, bipolar disorder, schizophrenia and impulsive behavior.48
A key role of this happy-making chemical is to reduce aggression. Those lacking one type of serotonin receptor are at double the risk of suicide.49 Serotonin in the brain is recycled, and anxiety-related personality disorders are common in those whose recycling mechanisms are faulty.50 Genetically altered mice lacking one type of serotonin receptor show increased aggressiveness and lack of maternal care for their young.51 Alcohol consumption leads to a reduction of tryptophan and a resulting decrease in serotonin. The impulsive behavior associated with drunkenness can be partially explained by this decrease in serotonin.52
“The life of the body is a heart at peace, but envy rots the bones” (Proverbs 14:30). Research on serotonin tells us why. Adequate levels of serotonin in the blood are a sign of good bone health—low levels are associated with low bone density. The bones have three different receptors for serotonin, and can even manufacture it.53
Depletion of serotonin can lead to obsessive-compulsive disorder, depression and anxiety.54 Surprisingly, depletion of serotonin can occur in people who have recently fallen in love—an explanation for the lack of appetite or obsessive behavior in the early stages of a relationship.55 Cupid’s arrow has its sting! As do insects. Wasps, hornets and scorpions have serotonin in their venom, and it is one of the chemicals responsible for the feeling of pain after a bite.
Antidepressants called serotonin selective reuptake inhibitors (SSRIs) keep serotonin longer in the nerve synapses, thus increasing levels in the brain. However, the benefits may decline over time as overall serotonin levels tend to fall in reaction to the drug. Side effects include repressed libido, erectile dysfunction, difficulty achieving orgasm, fatigue, weight loss or weight gain, apathy, insomnia, headaches and birth defects.56 SSRIs can also cause suicidal thoughts and actions, especially in teenagers. None of this is good. Another way to treat depression and anxiety might exist without the difficult side effects—supporting the body’s serotonin system with good nutrition, including plenty of animal fats.
How do animal fats affect our production and use of serotonin? One important factor is cholesterol—the serotonin receptors need adequate cholesterol to work properly, and many studies have linked low cholesterol with violent and aggressive behavior, in dogs and monkeys as well as in humans. People with low cholesterol levels are more likely to be violent when drunk; prisoners with low cholesterol levels are more likely to be aggressive; and dogs with low cholesterol are more likely to be vicious.57
A growing body of evidence suggests that vitamin D regulates the enzyme that converts the amino acid tryptophan into serotonin, and vitamin D activates genes that release serotonin. This may explain why sunbathing—or fatty foods—gives our moods a boost. Vitamin K2 may also play a role in supporting an active and curious outlook on life. In rats, vitamin K2 deficiency causes lack of exploratory behavior and reduced physical activity.58
ENDOCANNABINOIDS AND ENDORPHINS WORK TOGETHER to make us feel good. For example, endocannabinoids regulate dopamine production in the brain—dopamine is an endorphin, like serotonin, that helps with mood.
Far from causing depression, vitamin A supports the production of arachidonic acid, leading to the production of feel-good dopamine. Vitamin A also helps stimulate the production of dopamine receptors, and certain proteins support the cellular response to dopamine.59 Dopamine concentrations ordinarily increase in response to novel or pleasurable experiences, such as food and sex, but this increase can be completely abolished by feeding rats a drug that blocks the cannabinoid receptor.60
Dopamine plays many roles in the human biochemistry—often balancing the actions of serotonin. In the bloodstream, dopamine acts as a vasodilator; in the kidneys it increases sodium excretion and urine output (it makes you pee more); in the pancreas it reduces insulin production; in the digestive system it reduces motility (slows down digestion) and protects the intestinal mucosa; in the immune system, it reduces the activities of lymphocytes. If serotonin revs things up, dopamine dampens them down. In the brain, dopamine plays important roles in motor control (dopamine depletion is associated with Parkinson’s disease), motivation, arousal, cognitive control, reinforcement and reward—as well as lactation and sexual gratification.
We even have dopamine-secreting neurons in the eye. Dopamine enhances activity of the cone cells and suppresses activity of the rod cells, allowing increased sensitivity to color and contrast when the light is bright, at the expense of reduced sensitivity when the light is dim.
Dopamine is like family—we need it, but not too much. When we have an overproduction or overexpression of dopamine, we are revved up, unfocused. Too little has the opposite effect—we are lethargic and unable to function. Too much dopamine can result in schizophrenia61; too little is associated with depression.62 The treatment for attention deficit hyperactivity disorder (ADHD) is drugs that stimulate dopamine, while antipsychotic drugs act by suppressing the effects of dopamine.
Dopamine plays a role in dampening pain*—decreased levels of dopamine often manifest as painful conditions like burning mouth syndrome, fibromyalgia and restless legs syndrome.
The conventional view of dopamine is that it serves as a “reward” stimulus, as most types of reward increase the level of dopamine in the brain. But a more accurate description is that dopamine increases the effects of motivators, of what is called “seeking” behavior. In test animals, dopamine-stimulating drugs like cocaine and methamphetamine increase seeking behaviors, but do not increase expressions of pleasure, while opiate drugs like heroin and morphine produce increases in expressions of pleasure, but do not increase seeking behaviors.
One way scientists study the behavior of rats is by making them do work—like pushing levers—to obtain a food they like. If the rats are depleted of dopamine, either through surgery or drugs, they will stop doing the work. At first the researchers concluded that without dopamine, food is no longer pleasurable. But after many more lever pushes, another conclusion emerged. It seems that rats with low dopamine levels are less oriented to the future and only willing to do work that will provide an immediate reward.63 When no lever pressing is required, rats still chose a pleasurable food, whether or not their dopamine levels were low. When dopamine-depleted rats have to push a lever for a short time—even a lever that has weights on it—they will do so to get the food they prefer. But the low-dopamine rats can’t seem to go the distance. If they have to push a lever many times to get a food they enjoy, they just give up. But rats with normal dopamine levels will keep pushing that lever—even hundreds of times—to get their reward. What all these lever-pushing rats teach us is that the endorphin dopamine helps us look to the future, helps us sustain effort over time toward a goal.
It is the endocannabinoids that regulate dopamine production in the brain. Normally, new or pleasurable experiences cause dopamine to increase. But when rats receive a drug that blocks cannabinoid receptors, no dopamine increase occurs.64
Chris Masterjohn, PhD, explains it so well: “Endocannabinoids regulate the adrenal response to stress, mediated primarily by the hormone cortisol, which is responsible for the “fight-or-flight” response; they also regulate the production of dopamine in the brain, which is responsible for the motivation to sustain goal-oriented effort over time. By curbing the excess production of cortisol and supporting adequate production of dopamine, endocannabinoids help prevent excess tension, anxiety, burnout and feelings of self-defeat, and help support the confrontation of challenges with the attitudes necessary for success… Endocannabinoids thus not only prevent the anxiety and feeling of self-defeat that leads us to run from challenges rather than confronting them, but also help support the future-oriented maintenance of sustained effort that is necessary for personal financial and career success and a prosperous society.”65
To summarize: arachidonic acid (from animal fats) is the precursor of the endocannabinoids; vitamin D (from animal fats) regulates calcium needed for this conversion; vitamin A (from animal fats) is needed for the production of arachidonic acid and supports the dopamine system more directly by stimulating the production of dopamine receptors; vitamin K2 (from animal fats) supports neurological function in many ways; cholesterol (from animal fats) supports all receptors in the brain and saturated fat (also from animal fats) supports all hormonal conversions. For thinking, remembering, adjusting, planning, enjoying, learning and loving, animal fats are our best friends.
BEING HIGH IS THE NATURAL state of a well-nourished brain. Taken as a whole, modern research points to the conclusion that animal fats, rich in cholesterol, fat-soluble vitamins, arachidonic acid and many other components, not only help us avoid mental illnesses such as depression and anxiety, but also give us the curiosity, courage and stick-to-it-iveness to act positively and accomplish goals in a challenging world—activities that create the foundation of real happiness. Multiple studies have shown the link between achieving long-term goals and changes in subjective well-being; most research shows that achieving goals that hold personal meaning to an individual increases feelings of contentment.66
No wonder so many people are struggling with depression, chronic pain and even addiction in our fat-phobic world! Almost 50 percent of Americans suffer psychiatric disorders for at least one period of time during their lives. Those born after the Second World War—when processed foods based on vegetable oils entered the American diet—experience depression, anxiety, lack of impulse control and substance abuse at twice the rate as those born before. The proportion of Americans diagnosed with three or more disorders has more than tripled during the last sixty-five years.67
The addict is not degenerate or perverse, but someone who takes drugs to feel normal, to feel the way human beings should feel every day, even during times of difficulty and challenge.
The foods that protect us against depression and help us engage in future-oriented activities are the same foods that traditional cultures valued for good health. They provide fat-soluble vitamins. They contain cholesterol and arachidonic acid in abundance—along with other factors that support the lipid components, such as calcium, magnesium and B vitamins. By and large—with the exception of cod liver oil—these foods are satisfying and delicious: creamy pâté, aged cheeses, caviar with sour cream, full-cream milk, homemade ice cream made with real cream and egg yolks, eggs and bacon, omelets and quiche, cream-based soups, potatoes cooked in goose fat, oysters on the half shell, crab cakes and shrimp, lobster with (real) drawn butter, and in fact anything at all with butter, lots of butter—including potatoes, bread, fish, meat and vegetables.