Chapter 4
Rehabilitation
Aims and objectives of rehabilitation
Measurement tools in rehabilitation
Selecting patients for rehabilitation
Patients unlikely to benefit from rehabilitation
HOW TO . . . Plan a complex discharge
HOW TO . . . Conduct an MDT meeting
Occupational therapy assessments and interventions
Doctors in the rehabilitation team
Nurses in the rehabilitation team
Other members of the rehabilitation team
Introduction
Rehabilitation (rehab) is a process of care aimed at restoring or maximizing physical, mental, and social functioning. Can be used for:
• Acute reversible insults, e.g. sepsis
• Acute non-reversible or partially reversible insults, e.g. amputation, MI
• Chronic or progressive conditions, e.g. Parkinson’s disease
Involves both restoration of function and adaptation to reduced function, depending on how much reversibility there is in the pathology. Rehabilitation is an active process done by the patient, not to him/her. It is hard work for the patient (akin to training for a marathon)—it is not ‘convalescence’ (akin to a holiday in the sun).
Rehabilitation is the ‘secret weapon’ of the geriatrician, poorly understood and little respected by other clinicians. Many geriatricians feel it is what defines their specialty and it can certainly be one of the most rewarding parts of the job. The ‘black box’ of rehabilitation contains a selection of non-evidence-based, common-sense interventions comprising:
• Positive attitude. Good rehabilitationalists are optimists—this is partly because they believe all should be given a chance, and partly because they have seen very frail and disabled older people do well. A positive attitude from the team and other rehabilitating patients also improves the patient’s expectations. Rehabilitation wards should harbour an enabling culture where the whole team encourages independence: patients dressed in their own clothes, with no catheter bags on show, and eating meals at a table with other patients
• MDT coordinated working. By sharing goals, the team can ensure all team members are consistent in their approach
• Functionally based treatment, e.g. the Hb level only matters if it is making the patient breathless while walking to the toilet
• Individualized holistic outcome goals. These incorporate social aspects which must not be neglected. The team concentrates on activity and participation restrictions, rather than just impairments (see Box 4.1)
Settings
Specialized rehabilitation wards are not the only place for rehab. If the considerations outlined are in place, then successful rehabilitation can take place in:
• Specialist wards (e.g. stroke units, orthopaedic wards)
• Nursing and residential homes
These alternative sites often employ a roving rehabilitation team, which may be based in a hospital or the community.
Box 4.1 International Classification of Functioning, Disability and Health (ICF) World Health Organization (WHO) classification (2001)
This classification attempts to reconcile the medical model of disability (the disability of a person caused by a disease) with the social model (the disability caused when society attitudes and structures are not able to accommodate a person). A complex biopsychosocial model is required to adequately represent both contributions to disability.
Disability may be defined at three levels:
1. Impairments are ‘problems in body function or structure such as a significant deviation or loss’, e.g. hemiparesis after stroke
2. Activity limitations are ‘difficulties an individual may have in executing activities’, e.g. problems walking after stroke
3. Participation restrictions are ‘problems an individual may experience in involvement in life situations’, e.g. loses job following stroke
It can be seen that disability at different levels requires a different response. PT and time might improve gait after stroke, but modifications of the environment (e.g. use of a stick) may be better at restoring the activity limitation and social/political change may be required to restore participation.
Despite the attractive logic of such a classification, it is actually rarely used in clinical practice but can be used in research and particularly health economics.
The word ‘handicapped’ is now avoided due to negative connotations and stigma.
Further reading
World Health Organization. International Classification of Functioning, Disability and Health (ICF).  http://www.who.int/classifications/icf/en/.
http://www.who.int/classifications/icf/en/.
The process of rehabilitation
1. Selection of patients
see  ‘Selecting patients for inpatient rehabilitation’, p. 78.
‘Selecting patients for inpatient rehabilitation’, p. 78.
2. Initial assessment
This is not like a medical clerking; you need to get to know your patient on different levels (e.g. their mood, motivation, and expectations, complex social factors). Remember it is more meaningful to assess the full disability, not just the impairment (see Box 4.1).
3. Goal setting
see  ‘Aims and objectives of rehabilitation’, p. 73.
‘Aims and objectives of rehabilitation’, p. 73.
4. Therapy
• Medical—doctor-led (see  ‘Doctors in the rehabilitation team’, p. 92)
‘Doctors in the rehabilitation team’, p. 92)
• Physical—mainly PT (see  ‘Physiotherapy’, pp. 84–85) and nurse-led (see
‘Physiotherapy’, pp. 84–85) and nurse-led (see  ‘Nurses in the rehabilitation team’, p. 93). Mobility, balance, and stamina. Confidence is often a key issue
‘Nurses in the rehabilitation team’, p. 93). Mobility, balance, and stamina. Confidence is often a key issue
• Self-care—mainly OT (see  ‘Occupational therapy’, p. 89) and nurse-led
‘Occupational therapy’, p. 89) and nurse-led
• Environmental modification—aids and adaptations
• Carer/relative training—it is too late to leave this until just prior to discharge
5. Reassessment
Usually at weekly MDT meetings (see  ‘HOW TO . . . Conduct an MDT meeting’, pp. 82–83). Goals are adjusted and new goals are set. Points 3, 4, and 5 are repeated in a cycle until the patient is ready for discharge.
‘HOW TO . . . Conduct an MDT meeting’, pp. 82–83). Goals are adjusted and new goals are set. Points 3, 4, and 5 are repeated in a cycle until the patient is ready for discharge.
6. Discharge planning
see  ‘HOW TO . . . Plan a complex discharge’, p. 81—should be started as soon as the patient is admitted, but the efforts escalate towards the end of the inpatient period. A home visit and family meeting are often held to clarify issues.
‘HOW TO . . . Plan a complex discharge’, p. 81—should be started as soon as the patient is admitted, but the efforts escalate towards the end of the inpatient period. A home visit and family meeting are often held to clarify issues.
7. Follow-up and maintenance
Post-discharge DVs, outpatients, or DH attendance. Ideally done by the same team, but in reality this function often taken over by community, in which case good communication is vital.
Aims and objectives of rehabilitation
It is essential that the MDT, ideally in conjunction with the patient, states what it plans to do and to achieve, in clear terms that are shared within the team and can be worked towards. A large part of this is achieved through the agreement and statement of targets at two hierarchical levels: aims and objectives.
Aims
Best set by the team, in discussion with the patient. One or two patient-centred targets that encompass the broad thrust of the team’s work—a team ‘mission statement’ for that individual, e.g.:
• To achieve discharge home, with the support of spouse, at 6 weeks
• To transfer easily with the assistance of one, thus allowing return to existing residential home place at 4 weeks
Objectives
Best set by individual team members, in discussion with the patient. More focused targets, usually several, that reflect specific disabilities and help focus the team’s specific interventions, e.g.:
• To walk 10m independently, with a single stick, at 3 weeks
• To achieve night-time urinary continence at 4 weeks
Both aims and objectives should have five characteristics, summarized by the acronym ‘SMART’:
• Specific, i.e. focused, unambiguous
• Measurable, hard to assess nebulous targets
• Realistic, acknowledging time and/or resource limitations. It is futile and demoralizing to set targets that cannot be achieved. Conversely, the team (and patient) should be ‘stretched’, i.e. the target should not be inevitably achievable
• Time-bounded. Specify when the target should be achieved. Many patients are motivated and cheered by the setting of a specific date (especially for discharge). Setting dates for specific functional achievements prompts further actions, e.g. ordering of equipment for the home
Predicted date of discharge
Specifying a predicted date of discharge (PDD) from the point of admission is useful for patients, carers, and MDT members.
• Emphasizes to the patient that inpatient care is not indefinite and that a more pleasant home or care home environment is the aim
• Can be intrinsically motivating for patient and team
• Prompts the carers and MDT to think ahead to pre- and post-discharge phases of care
Measurement tools in rehabilitation
Principles
The most widely used standardized measurement instruments are structured questionnaires that deliver a quantitative (numerical) output. They vary in precision, simplicity, and applicability (to patient groups or clinical settings). For each domain of assessment, several tools of differing size are usually available, reflecting tensions between brief assessments (speed, easy-to-use, well-tolerated) and a more prolonged evaluation (precision improved, give added layers of information).
Measurement tools are helpful at single points (especially entry and exit to a therapy programme), and also in assessing progress and guiding discussion around a likely discharge destination.
Advantages
• Widely understood and transferable across boundaries
• Facilitate communication between professionals and settings of care
• May permit a less biased, more objective view of the patient
• Facilitate a structured approach to assessment and clinical audit
Disadvantages
• Scores may conceal considerable complexity—patients scoring the same may be very different
• Intra-individual, intra-rater and inter-rater variabilities mean that a score may change while a patient remains static, e.g. 3- or 4-point change in the (20-point) Barthel is needed before a team can be absolutely confident that the patient has changed
• There are many scales available, and some are not in general use, leading to confusion when staff or patients move between units
Measurement instruments
Activities of daily living
Personal ADLs (pADLs) or basic ADLs (bADLs). Include key personal tasks, typically transfers, mobility, continence, feeding, washing, and dressing. A single scale is valid for all.
• The most common is the Barthel (see  Appendix, ‘Barthel Index’, pp. 702–703). Score range from 0 (dependent) to 20 (independent). It is quick and apparently simple to use but is not very sensitive to change, as steps within each domain (e.g. transfers) are large. A marked ceiling effect is seen, especially for a range of impaired patients living independently at home, many of whom score 20
Appendix, ‘Barthel Index’, pp. 702–703). Score range from 0 (dependent) to 20 (independent). It is quick and apparently simple to use but is not very sensitive to change, as steps within each domain (e.g. transfers) are large. A marked ceiling effect is seen, especially for a range of impaired patients living independently at home, many of whom score 20
• The Function Independence Measure (FIM) takes longer to complete but is more sensitive to change during rehabilitation and can be useful in predicting length of stay and discharge destination
Extended activities of daily living (eADLs)
Also known as instrumental ADLs (iADLs). Include key daily household tasks, e.g. housework, shopping. Useful for the more independent person. Scales are selected according to an individual patient’s needs, e.g. Frenchay Activities Index, Nottingham ADL Score.
Mobility
For example, Elderly Mobility Scale (EMS), Tinetti Mobility Score (TMS), timed get up and go test.
Cognition
• Several screening and assessment tools are in common use
• The 10-point AMTS (see  Appendix, ‘The abbreviated mental test score’, p. 704) is brief and useful for screening in both outpatient and inpatient settings
Appendix, ‘The abbreviated mental test score’, p. 704) is brief and useful for screening in both outpatient and inpatient settings
• Clock drawing tests (see  Appendix, ‘Clock-drawing and the Mini-Cog™’, p. 707) are alternative screening tests
Appendix, ‘Clock-drawing and the Mini-Cog™’, p. 707) are alternative screening tests
• The 30-point Mini-Mental State Examination (MMSE) provides sufficient precision to be used for serial assessment, e.g. tracking recovery from delirium, or therapeutic response to cholinesterase inhibitors in dementia—but takes <10min to administer
• The Middlesex Elderly Assessment of Mental State assesses systematically the major cognitive domains, using a range of targeted subtests. Time-consuming (15min) but gives more detailed information. Often used by therapists
Depression
For example, the GDS. Several versions of this are available, but the most commonly used is the 15-point score (see  Appendix, ‘Geriatric Depression Scale’, p. 701), administered in 5–10min. Superficially distressing questions, but well tolerated by most patients. Sensitive (80%), but only moderately specific (60%).
Appendix, ‘Geriatric Depression Scale’, p. 701), administered in 5–10min. Superficially distressing questions, but well tolerated by most patients. Sensitive (80%), but only moderately specific (60%).
Nutrition
The Malnutrition Universal Screening Tool (MUST) (see  Appendix, ‘Malnutrition Universal Screening Tool (MUST)’, p. 709) is widely used to screen inpatients and is superior at predicting malnutrition than weight alone.
Appendix, ‘Malnutrition Universal Screening Tool (MUST)’, p. 709) is widely used to screen inpatients and is superior at predicting malnutrition than weight alone.
Pressure area risk
Prompt systematic evaluation of patients at risk, and brisk response in those at risk, is essential. Several scores are available, but the most widely used is the Waterlow Pressure Sore Prevention Score, a summary score derived from easily available clinical data. High score indicates high risk. Note that the score does not take into account the ability of the patient to lessen risk by changing position, the acuity of the medical condition, etc.
Disease-specific scales
All of the common diseases have dedicated scales, usually developed for use in research and then introduced variably into clinical practice. They are often more complex than used in general clinical practice, with corresponding disadvantages—time-consuming, less easily transferable. For example, the Unified Parkinson’s Disease Rating Scale (UPDRS) quantifies all the motor and behavioural aspects of the disease as a single number.
Selecting patients for rehabilitation
Most hospitals do not have enough rehabilitation services to cater for all patients who could benefit, so places are a valuable resource. This is often not understood by the patients, relatives, or referrers. Be aware that some referrers are motivated to get the patient ‘out of their beds’. Patient selection is a time-consuming, important, and complex task.
Settings
Rehab can be provided in acute hospitals, CHs, care homes, or even at home (e.g. virtual wards), depending on availability and motivation of carers, as well as how services are set up locally.
Who should select patients?
Review of referrals is often done by geriatricians but can equally well be done by another experienced rehabilitation professional. In some settings, a team assessment is done and discussed in conference.
Who to choose?
Two factors need to be considered:
• Which patients will benefit most from what is a limited resource?
• What does the MDT need to keep it positive and functioning well?
At first glance, the ‘best’ rehabilitation patient has had an acute event with good prognosis (e.g. a fracture), who is motivated and cognitively intact—able to participate enthusiastically in therapy and who has clear, easily attainable goals. Rapid results provide turnover, variety, and interest for the team. However, consider whether this patient might actually get better in almost any supported setting with a bit of supported convalescence time.
Contrast this with a frail elderly woman with multiple medical problems, moderate cognitive impairment, barely managing at home alone before a prolonged hospital inpatient stay with repeated complications, who has gone downhill physically and mentally. If asked, she wishes to go home, but this may not appear altogether realistic. Her daughter thinks she should go into a care home for ‘her own safety’. It is all too easy to write this patient off, deny them rehabilitation, and arrange placement. This is the kind of complex ‘heartsink’ patient who has the most to gain personally (and who provides cost-effective utilization) of the expertise of the rehabilitation team. In any other specialty, the most complex cases are dealt with by the specialist; the same applies to rehabilitation. These types of patient sometimes do remarkably well and should be considered for a trial of rehabilitation. Even patients with virtually no recovery potential can benefit, e.g. learning adaptation, teaching skills to carers, or arranging complex discharge packages.
In practice, it is often a balance between the two types of patient where a broad case mix is maintained—some slower-stream complex cases with some more rapidly treated, simpler cases.
►► In general, the harder a problem seems to be, the less likely it is that it will be sorted out in a non-specialist setting and the more likely it is that the patient will benefit from the rehabilitation team.
Information required for patient selection
Should be gleaned from all available sources (including nurses, hospital notes—medical, nursing, and therapy, family, carers, 1° care team, specialists, etc.) and may involve telephone calls and/or several visits. Regardless of who does the assessment, the following information should be acquired.
Premorbid features
• Physical problems—list of medical conditions, how active they were, and how disabilities impact on life; list of medications
• Functional limitations—assess by conversation (Did you use a stick? Did you ever go out alone? Could you get up and down stairs?, etc.) Quantify with a rating scale
• Social set-up—who do they live with (and how fit and willing to help are they?); where do they live (rural or in town)?; what is the property like (e.g. flat or house, any stairs to access and once inside the property, whether the bedroom and bathroom are up or downstairs)?; does anyone help out (formally, e.g. home carers, or informally, e.g. neighbours, family, friends)?; what did they do on a regular basis (e.g. walk to the pub for lunch, attend day centres or lunch clubs, cycle into town for groceries, etc.)?
• Cognitive state—range from mild memory problems (may predispose to delirium) to significant dementia. Ask about any objective assessments (e.g. MiniCog™) and the difficulties the problem causes in everyday life
Acute features
• Nature of acute insult—is it reversible (compare amputation to acute confusional state)
• What is the expected recovery curve?—Varies with the disease: a patient with a large stroke may show very slow progress at outset and then steady, but slow, progress after several weeks; a patient with a fractured neck of femur, by contrast, is likely to improve rapidly after the operation and continue to make quick progress; a septic patient is unlikely to improve at all until the acute illness has resolved and is then likely to improve steadily. If the assessor has limited knowledge of the disease, obtain information from the specialist currently caring for the patient
Patient wishes
• Do they understand about the problems they face?
• Do they know what they wish to do when they leave hospital (e.g. go home as soon as possible, return to their residential home, not go home unless they are able to function as before, etc.)?
Patients unlikely to benefit from rehabilitation
• Patients in a steady state who are awaiting placement
• Patients for whom the process of waiting for a rehabilitation bed will delay discharge (e.g. where expected recovery to discharge fitness is under a week)
• Patients with a single requirement for discharge (e.g. provision of commode)
• Patients who are still medically unstable, requiring frequent medical review, investigation, or treatment
• Patients with pure nursing needs (e.g. unconscious patient)
• Probably inappropriate for terminal care patients (palliative care teams likely to be able to support discharge planning when needed)
Dementia and rehabilitation
This can be frustrating and difficult (but also very rewarding). Therapists will often prefer patients with ‘carry over’—who are able to recall the last session and build on it. Nurses may find patients with behavioural problems disruptive to the ward. Safety issues are more difficult, as awareness of danger and the ability to make an informed decision about risk-taking are less. Relatives’ anxiety is likely to be high. However, there is still a lot that can be done.
Repeated exercise can build stamina and some learning may occur. Rehabilitation settings allow more time for spontaneous recovery to occur. The more complex the discharge, the less likely it is that this can be managed in a non-specialist setting and the greater the need for the MDT expertise. Patients with dementia are most at need of an advocate for their rights and wishes, and the expert team assessment of feasibility and risk is the best way to ensure they are respected.
► In general, dementia alone is not a reason for refusing rehabilitation.
HOW TO . . . Plan a complex discharge
• There is no such thing as a safe discharge—only a safer one. There is widespread misapprehension that hospitals and nursing homes are ‘safe’, while home is dangerous, but this is the wrong way round, e.g. rate of falls in institutions is higher (there is just someone there to pick you up) and the ↑ exposure to infection (e.g. meticillin-resistant Staphylococcus aureus (MRSA), ‘flu) can be life-threatening
• The timing of discharge is sometimes obvious (e.g. when the patient returns to premorbid functioning) but can be controversial. Some patients want to go before the MDT feels they are ready and others (or their families) wish to stay longer (usually due to unrealistic aspirations or dislike of the chosen discharge destination)—communication is the key to avoiding this. Patients should understand that discharge is not necessarily the end of recovery following an illness
• Start to plan discharge from day 1, e.g. by obtaining background social history and patient aspirations. Set a target that patient and team are aware of—it is better to revise a PDD or destination than to have none at all, because it helps to focus goal-planning
• Involve relatives early—family meetings will ensure effective two-way communication. It will also reduce the chance of ‘the daughter from America syndrome’ where a relative comes out of the woodwork just before a carefully planned discharge to challenge or block existing plans
The MDT members should anticipate and pre-empt, but the following are common pitfalls which can cause a discharge to fail:
• Care availability (especially night-times)—check well in advance with the care manager that the care package you plan is available
• Modifications and equipment—ideally any environmental modifications should be in place before your patient is ready for discharge; otherwise there can be lengthy delays. It is amazing how long it can take for simple measures such as a bed to be moved downstairs. For more complex interventions (e.g. stairlifts, walk-in showers, deep cleaning), get a realistic estimate of time—sometimes the patient may need alternative accommodation while these works are completed
• Appropriate transport available (relative, ambulance)—remember not just for the patient, but also for their equipment
• Keys—who has got them? Who needs keys/door entry codes?
• Night-times—discharge plans often fail because the patient who looks good by day has unanticipated needs at night. Check with the nurses that they are not incontinent, immobile, or confused at night
HOW TO . . . Conduct an MDT meeting
This is a ward- or team-based meeting with the 1° functions of communication, goal-setting, reviewing progress, and discharge planning.
There are also wider aims of:
• Team building. There is usually a chance for discussion over tea and biscuits. This is not time-wasting, it is vital for team bonding
• Education. Sharing knowledge and insight into each other’s jobs
Usually weekly for inpatient settings but can be less frequent in community or outpatients. Most commonly, the team meets in a room away from patients/relatives—sometimes involving the patient by bringing them into the room.
Any member of the team can ‘run’/chair the meeting, but in practice, where a doctor attends, they usually take this role. The chair is responsible for:
• Timing—the last few patients discussed should not be rushed. Some patients take a lot longer than others, but this should be a function of need, not just where they happen to appear on the list. Do not use the same order each week
• Involving all team members—ensure each member has an unimpeded opportunity to comment on each patient—some may need prompting. Do not allow assumptions that everyone knows certain information or that it is unimportant. A well-established team may automatically take turns—others may need you to force an order. Ask members to clarify jargon or code that may not be universally understood
• Ensuring decisions are made/goals are set. Without good leadership, a long discussion can occur without a positive action plan. Prompt with ‘So what are we going to do about this?’, ‘Who is going to take that on?’, ‘When will that actually happen?’. If discussion is going in circles or there is dispute, it can be helpful to summarize what has been said so far to allow things to move on. Where there is agreement on goals, make sure they are SMART (see  ‘Objectives’, p. 73)
‘Objectives’, p. 73)
• Maintaining morale—remember case conferences can be stressful. Keep discussions professional and good-humoured. Careful use of humour and frequent reminders that individuals, and the team, have done well are very important
• Encourage feedback—it is interesting and educational to hear follow-up on discharged patients. Ensure thank-you letters, etc. are shared, as well as news on deaths, readmissions, etc.
The conventional order of presentation is:
1. Doctor—diagnosis, current management and changes planned, prognosis—particularly if symptoms are limiting therapy
2. Nurse—nursing requirements, mood and behaviour, continence, sleeping, relatives/visitors comments
3. PT—mobility, equipment, progress, and potential
4. OT—functional assessments (e.g. dressing, kitchen), cognition, and DVs
5. Social worker/care manager—background, discharge discussions, external liaison (e.g. with council, funding panels, etc.)
This order allows discussions to flow naturally from medical background to current function (therapists) to goal planning and discharge plans (social worker). There is no reason why the order should not be different, but beware one person dominating and avoid discussing endpoints (e.g. discharge) before going through the logical steps, or you will become inefficient or miss something.
Notes of the meeting are vital—ideally they should be written only once, somewhere that all team members have access to. As a minimum, record the date, current status, notes about the content of discussion (even if solutions not found), goals, and plans. You have failed if you summarize a 20min important discussion as ‘continue’ or ‘aim home next week’.
Physiotherapy
Training
BSc (Hons) Physiotherapy is a 3–4 years’ full-time course. MSc Physiotherapy can be done as a 2-year accelerated postgraduate course. After 1° training, PTs usually sub-specialize in one area such as care of the elderly. See the UK Chartered Society of Physiotherapy website  http://www.csp.org.uk.
http://www.csp.org.uk.
The role of the physiotherapist
• Aimed at improving physical functioning by exercise, reducing pain, and providing appropriate aids
• May be for recovery, adaptation, or prevention, e.g. falls
• Patient needs sufficient motivation, muscle strength, and energy to participate—it is not a passive process
• Duration of therapy may be short initially but ↑ as the patient tolerates more
• Cognitive impairment may limit learning and ‘carry-over’ of skills from session to session, but stamina may be improved with repeated sessions; dementia is not a reason to withhold PT
• PTs are the experts who plan and supervise physical therapy, but rehearsal of skills is often delivered by other members of the MDT or patients are given exercises to do alone (often with written instructions). PT assistants, nursing staff, and relatives can all assist in this rehearsal process
• Involved in training others to move dependent patients safely (e.g. carers)
Range of interventions
Increasing range of movement
• Use after stroke or prolonged bed rest to ↑ joint mobility and prevent pain and contractures
Increasing strength of muscles
• Usually general strengthening to improve stamina
• Can be targeted at specific areas of weakness and enhanced by the use of resistance and weights
• Important part of falls prevention
Improve coordination
• Repeated movements rehearse skills and improve coordination
Transfers (i.e. the ability to get from one place (bed) to another (chair))
• Strategy depends on patient ability
• Totally dependent patients are hoisted
• Once there is sitting balance, then transfers with assistance of two people and a sliding board can be attempted
• Once there is standing ability, then standing transfers with one person, then a frame can be worked on
Ambulation
• Exercises aimed at improving independence in mobilizing
• Realistic goals should be set—ideally premorbid state should be achieved, but 10m may be adequate for discharge home if this is the distance from chair to kitchen
• Balance aided by bars, then walking aids
Heat treatment
Using packs, hydrotherapy pools, ultrasound, etc. to treat pain and improve joint mobility.
Other treatments
For example, cold treatments, electrical stimulation for pain relief (e.g. transcutaneous nerve stimulation (TENS) machine).
Provision of aids
Usually ambulatory aids.
Walking aids
These ↑ stability, leading to improved confidence and function, and ↓ falls. In general, identifying the need for an aid should prompt consideration of: the cause of functional decline (is it reversible?); provision of a PT assessment for prescription (correct aid, correct size); education (use of the aid, how to get up after falls); and treatment (strength/balance training).
All walking aids without wheels should be fitted with rubber ferrules to optimize grip and then checked for wear regularly (see Fig. 4.1).
Stick (or cane (USA))
• May be single-ended (‘straight’), double-ended (‘hemi-’ or ‘bipod’), three-ended (‘tripod’), or four-ended (delta-, quadrupod). The latter offers modest additional stability, compared to the straight stick
• Held in the hand opposite the most impaired leg, thus unweighting the impaired limb
• The level of hand placement should be at the greater trochanter, permitting 20–30° of elbow flexion—the most efficient elbow muscular function
• The choice of handle is important, e.g.:
• Contoured: improves grip, reduces pressure, in permanent users or those with deformities
• Swan neck: weight is centred over the base of the stick, providing a little more stability
• Right-angled: more comfortable, but not easily secured when not in use
• Crook handle: hooked over the arm when not in use
Frame
• A structure of lightweight alloy metal that is self-stabilizing (usually based around four points in contact with the floor), providing unweighting of the lower limbs and greater stability than a stick
• Various heights, depths, and widths are available
• Bulky and difficult to transport. Some folding versions (often only three legs) are available
• The handgrips should be at wrist level, with the elbows slightly (15°) flexed. Shorter frames are used in patients who fall backwards
• To use a non-wheeled frame, lift it and move it 10–30cm in front of the body; then lean forwards a little, taking some weight through the arms before taking two equal steps towards the centre of the frame
• A weighted frame has weights low on the frame structure to provide additional counter-balance against falls
• A wheeled frame has wheels at the front, permitting faster walking and an improved gait pattern, but it provides a slightly less stable base. Small-wheeled frames are suitable only for smooth surfaces
• A gutter frame has forearm rests, enabling weight-bearing through the forearms, rather than the hands alone, providing additional support in the early stages of mobilization or when hands/wrists are impaired
Crutches
A full assessment by a therapist is needed before selecting crutches. Crutches may be of the axilla- or elbow-type. Both are available with various features that should be individually prescribed, e.g. closed elbow cuffs provide added security and enable the user to let go of the handgrip to open a door without the crutch falling to the floor.
Walkers or rollators
• A frame that has three or four wheels and often hand-operated brakes (for added stability while static)
• Three-wheeled versions usually fold, permitting stowage in a car
• Rollators with additional features, such as bigger wheels (for uneven ground), a seat, or an attached basket for shopping or other house/garden tasks, are larger than most standard frames and are usually used outdoors
• A trolley walker combines walking support with a means of transporting items from room to room. One or two shelves. The lower shelf is recessed at the back, so that it does not interfere with walking
Early walking aids (EWAs)
For example, post-amputation mobility aid (PAM-aid). Used early (usually from ~day 7) following amputation, in patients in whom a permanent prosthesis is planned or being considered.
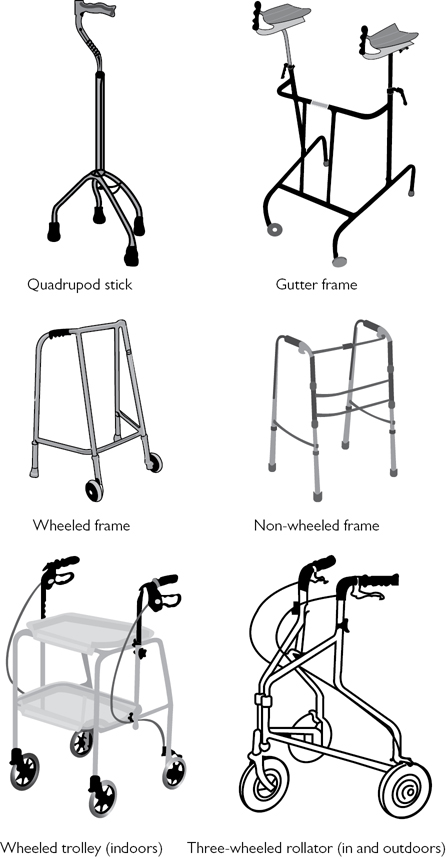
Fig. 4.1 Different types of walking aid.
Occupational therapy
Training
BSc Occupational Therapy is a 3–4 years’ full-time course or can be done as a 2-year accelerated postgraduate course. The courses are 2/3 academic and 1/3 field work. After 1° training, OTs usually sub-specialize in one area such as care of the elderly. See (for the UK) the British Association of Occupational Therapists and Royal College of Occupational Therapists website  http://www.cot.org.uk.
http://www.cot.org.uk.
Role of the occupational therapist
The College of Occupational Therapy definition:
‘OT enables people to achieve health, well-being and life satisfaction through participation in occupation (i.e. daily activities that reflect cultural values, provide structure to living and meaning to individuals; these activities meet human needs for self-care, enjoyment and participation in society)’.
OTs achieve this by assessing both functional status and the environment, then advising how to adapt.
Skills versus habits
• A skill is having the ability to start, carry out, and complete a task effectively (e.g. making a cup of tea)
• A habit is those tasks that are actually carried out (e.g. a person may be able to make a meal but does not do so when alone as they do not feel hungry)
Components of personal ability
Assessed by direct observation during tasks, formal testing, and information taken from carers, relatives, and other professionals.
• Cognition—to understand the task and why it needs doing. May be limited by dementia, poor concentration span, poor problem-solving skills, etc. Assessed with cognitive tests such as Middlesex Elderly Assessment of Mental State (MEAMS)
• Psychology—wanting to do and complete the task. Limited by depression, apathy, impaired coping skills, etc.
• Sensorimotor ability—especially in the upper limb
Occupational therapy assessments and interventions
Assessments
• Washing and dressing—aim to be done in the morning, when the patient would normally be carrying out these tasks
• Kitchen—looking at competence and safety for required tasks (depending on circumstances, e.g. may need to make a meal on a gas stove, or just pour a drink from a prepared Thermos™)
• Access visits—are done without the patient, to study the layout and potential problems of a patient’s own home
Home assessment visits
• A visit done with the patient, to see them in their own environment
• Can be done by the OT alone, or with another member of the MDT (e.g. PT, care manager)
• May be useful to include intended carers (family or professional), as concerns can be addressed during the visit
• Can be done in the community while the patient is still at home, from a hospital ward prior to discharge to ensure that it is feasible and that all possible problems and dangers have been minimized, or after discharge as a follow-up
• Sometimes surprising—patients may either perform considerably better than expected (as they are in a familiar environment to which they have been adapting for years) or considerably worse (especially when a new physical limitation has occurred, such as stroke, as being at home emphasizes how different life will now be)
• Standard format for assessing all aspects of the property
• Followed by a report containing observations on client performance and a list of recommendations regarding reorganization of furniture (e.g. bring bed downstairs), equipment provision, and care required
• Often typed and circulated to all MDT members
Interventions
Teaching new skills (e.g. putting on a jumper with an arthritic shoulder) and habits (e.g. heating up microwave meals every lunchtime). Looking at how much can be done by the patient themselves and how much help is needed (family or professional carers). Assessing need for equipment and advising about suitability, as well as training carers in its use. Commonly used equipment includes aids to:
• Access—ramps, rails, banisters, stairlifts, perching stools (high stools to enable seated access to a kitchen work surface), etc.
• Transfers—‘banana boards’ (curved boards that the patient slides across from one horizontal surface to another), swivel mats (two circles that twist to allow easier turning of an immobile patient, usually in a car seat)
• Mobility—wheelchairs, scooters, etc.
• Bathing and dressing—bath boards, accessible baths and showers, long shoehorns, grab handles (to allow picking things up without bending), etc.
• Toileting and continence—seat raises, commodes, non-return urine bottles (for use when lying flat), etc.
• Eating and drinking—cutlery and cups with easy-grip handles, aids to improve safety with hot water (kettle holders, full-cup alarms), tap turners, etc.
• Splints—for wrists (prevent pain) and ankles (foot drop)
• Sensory aids—enhanced signals, e.g. large dials on a clock or altered signals, such as flashing light, instead of a bell for the deaf
Doctors in the rehabilitation team
Doctors are commonly part of hospital rehabilitation teams but may be missing from community rehabilitation teams where a nominated doctor (e.g. GP or community geriatrician) can be consulted about specific issues.
When present, doctors often chair MDT meetings—this may be partly historical and partly because they are ‘professional risk-takers’ who are more confident at coaxing a shared decision from a team, sometimes in very uncertain circumstances.
Medical ward rounds are often less frequent than on acute wards (a weekly round would be usual), and since the patient is usually medically stable, communication with patient and family may predominate over medical management.
In a rehabilitation setting, the doctor’s main duties to the patient are:
• Selecting patients and maintaining a waiting list
• Optimizing and stabilizing medical treatments (e.g. ensure adequate analgesia)
• Rationalizing drug therapy (e.g. stop night sedation)
• Anticipating and treating complications (e.g. pressure sores, Clostridium difficile-associated diarrhoea (CDAD), DVT)
• Diagnosing and treating depression
• Identifying and managing co-morbid conditions (e.g. incontinence, skin tumours)
• Initiating 2° prevention (e.g. aspirin for stroke, bisphosphonates following osteoporotic fractures, influenza vaccination)
• Organizing 2° referral to other specialists (e.g. dermatology, orthopaedics)
Additional duties to the team include:
• Context-setting—doctors often cross health sector boundaries, whereas therapists and nurses can be fixed in teams or wards. They should share information about the patients on the waiting list and about those who do not reach the rehabilitation unit and why. This overview can help the team understand pressure on beds, etc.
Nurses in the rehabilitation team
The role of rehabilitation nurses in the recovery of a patient is often underestimated. They spend the longest time, and often have the most intimate relationship, with patients and their relatives.
Their wide role encompasses:
• Rehabilitation helper—particularly rehearsal of new tasks learned with therapists (e.g. transfers, dressing). It takes longer and more skill to encourage a patient to wash/dress themselves than simply to provide personal care—this is the fundamental difference between rehabilitation and normal ward nursing
• Overall performance assessors versus snapshot—they can detect any differential performance between what a patient ‘can do’ with the therapist and what he/she ‘does do’ when on their own, when tired, or when relatives are visiting
• Communication and liaison—first port of call between members of the team and patient and relatives. Emotive information sometimes more readily revealed in such non-threatening discussions
• Nocturnal assessment—they are the only professionals able to monitor sleep, nocturnal confusion/wandering, and nocturnal continence/toileting
• Pressure and wound care management
• Medication administering and monitoring self-medication
Some senior specialist nurses have roles that overlap with the doctor’s, e.g. in selecting patients for rehabilitation, chairing MDT and family meetings, nurse prescribing, etc. This is especially true in some CHs which can be exclusively run by nurse consultants.
Other members of the rehabilitation team
Speech and language therapy
Trained to degree level (3–4 years) or postgraduate diploma. See the Royal College of Speech and Language Therapists (RCSLT) website  http://www.rcslt.org.
http://www.rcslt.org.
Assessment and treatment of swallowing disorders forms the bulk of inpatient work. Careful bedside evaluation of the patient is central to this, complemented, if necessary, by videofluoroscopy, the assessment ‘gold standard’.
Useful interventions include patient positioning, changes in the texture or consistency of food/fluid, and carer supervision or prompting with food boluses. A period of ‘nil by mouth’ may be necessary until possible recovery of a safer swallow, during which artificial feeding should be considered.
Assessment and treatment of speech disorders forms the remainder of their work, commonly following stroke or head/neck surgery. Therapists are experts in communication disorders, and their assessments are useful in distinguishing between severe dysarthria and dysphasia, for example. They provide: advice to patient, carers, and staff; and alternatives to speech, including communication boards, non-verbal strategies, and electronic communicators.
Dieticians
Trained to degree level (3/4 years) or postgraduate diploma. See the British Dietetic Association website  http://www.bda.uk.com.
http://www.bda.uk.com.
• Malnutrition in older people is common, underdiagnosed, and undertreated. Prevalence and severity are especially high with (acute or chronic) comorbidity and in inpatients
• Community-dwelling older people may have an unvaried diet, depleted in fruit and vegetables (‘tea and toast’)
• Dieticians are experts in the assessment and treatment of nutritional problems, but other members of the MDT must be alert to the possibility of malnutrition and initiate interventions and dietician referral. Screening tools are useful (see  Appendix, ‘Malnutrition Universal Screening Tool (MUST)’, p. 709)
Appendix, ‘Malnutrition Universal Screening Tool (MUST)’, p. 709)
• Effective interventions include offering attractive food tailored to the individual, asking the family to bring in food, offering food frequently, and providing a dedicated assistant by the bedside to assist with feeding (this could be a staff member, family, or an informal carer). Modern packaging (prepacked margarine, snack boxes) can be obstructive
• Where ‘normal’ feeding is impossible, e.g. after acute stroke, the dietician can provide assessment, monitoring, and advice to the patient (and family) regarding artificial feeding (see  ‘Nutrition’, pp. 354–355)
‘Nutrition’, pp. 354–355)
Pharmacists
Pharmacists train for at least 4 years, leading to the MPharm degree. See the Royal Pharmaceutical Society website  http://www.rpharms.com.
http://www.rpharms.com.
• Pharmacists are involved in preparation, prescribing, packaging, and dispensing of medicines. They are key to the system delivering quality drug use to outpatients and inpatients, to older people
• Gatekeepers of many health community formularies (limited drug lists optimizing costs and effectiveness). They advise on all aspects of prescribing, especially interactions and dosing
Issues where pharmacists may help:
• High frequency of adverse drug reactions (up to 17% of hospital admissions)
• Underuse of medications, e.g. preventatives in asthma
• Poor concordance/compliance/adherence
• Poor administration technique, e.g. inhalers
• Frequent and complex changes in medication
• Poor communication with 1° care on discharge
• Absence of full medication history on admission
The National Service Framework (NSF) for older people states that all patients >75 should have their medicines reviewed at least annually, and those taking four or more medicines 6-monthly. Every area must have schemes for older people to access help from pharmacists in using their medicines.
Social work and care management
Social workers are trained to degree level (3/4 years) or postgraduate diploma. See the British Association of Social Workers website  http://www.basw.co.uk. Care managers may have less formal training.
http://www.basw.co.uk. Care managers may have less formal training.
• Care managers are based in both community and hospital settings and may work with patients of all ages
• The quality of support that they provide to a geriatric medicine service is a key determinant of patient throughput and quality of care
• Any inpatient clinical area managing the needs of older people should have significant input from a social worker with experience in working with older people
• Many EDs in UK hospitals now have a dedicated social worker, aiming to avoid admissions by optimizing access to social care
• To function effectively, social workers must have a detailed understanding of local services and facilities, how those services are accessed, as well as about supporting information such as transport, costs, and waiting lists
Elements of their role include:
• Assessment of client needs, often informed by the MDT in hospital settings
• Translation of care needs into a package of care
• Monitoring delivery of care and modifying its content or providers, if necessary
• Providing patients and families with details of care homes that can meet the patient’s needs, in the desired geographical area
• Providing advice about finances and financial support, care homes, and home care
• Performing financial assessments to determine who will fund their own care and who will receive assistance
• Counselling and support to patients and families
• Crisis management. For example, if a carer becomes ill or dies, a care package may be ↑ urgently or emergency admission to a care home arranged. ‘Social admission’ to hospital should be a last resort, unless the condition of the patient has also changed, in which case urgent medical assessment, perhaps in a hospital, is essential
• Arranging short breaks (for the carer) or respite care (for the patient)
Community nurses and health visitors
Both are trained nurses with further postgraduate training and experience that enable them to work more independently in community settings. Their precise role and professional relationships vary greatly between districts.
Community nurses
Usually work for one or more GP practices, providing domiciliary nursing services in excess of those provided by non-nurse carers. A district nurse is a community nurse who has undergone further training.
Specialist skills include:
• Wound care—assessment and treatment
• Insulin injections and diabetes monitoring
• Education of patients and carers (e.g. PEG feed, catheter care)
Although caring for adults of all ages, much of their work involves older people, especially the frail elderly. They are often an excellent source of information about older people admitted to hospital, often having frequent contacts with frail elderly people who are unable to leave the home and are therefore seen only rarely by GPs.
Community matrons are experienced senior nurses who are responsible for identifying and care-coordinating high-intensity users of healthcare. They coordinate agencies for complex, frail, and often elderly patients to promote well-being and try to obtain maximum efficiency from 1° care and 2° care providers. Often this involves trying to reduce emergency admissions to hospital and/or calls to out-of-hours GPs.
Health visitors
Again, health visitors (HVs) usually work with one or more GP practice, but the dominant focus is on health promotion. Most work with mothers and babies/children, but they can work with any age group. Some HVs specialize in working with older people and carers. They may help older people maintain independence by:
• Providing information about local activities
• Advising on help available from social services to support them in their homes