Chapter 21
Ears
HOW TO . . . Communicate with a deaf person
HOW TO . . . Use a hearing aid
Deafness and the ageing ear
Deafness is a common, debilitating complaint that ↑ with age; 6% of adults, 33% of retired people, and 80% of octogenarians in the UK have impaired hearing. Deafness is often ignored (‘part of getting older’), yet it prevents communication, causes social isolation, anxiety, and depression, and can contribute to functional decline.
Around half of sufferers could be helped by a hearing aid, yet less than a quarter have one. Generally patients with unilateral, mild bilateral, or profound bilateral deafness do not benefit from conventional hearing aids.
► Be alert to hearing loss. A quick assessment directs appropriate referral to audiology or ENT when necessary.
Normal ageing
Presbyacusis
• Describes the decline in hearing that commonly occurs with age—‘degenerative deafness’
• Usually detectable from age 60–65
• Both the sensory peripheral (cochlea) and central (neural) components of the auditory system are affected, with peripheral degeneration being accountable for at least two-thirds of the clinical features of presbyacusis
• A variety of possible mechanisms exist—cellular degeneration gives rise to a reduction in the numbers of hair cells, particularly at the basal end of the cochlea (the part responsible for high-frequency sound appreciation). Circulatory changes such as atherosclerosis, microangiopathy, and atrophy of the stria vascularis contribute
• The relative contributions of ‘normal ageing’ and cumulative exposure to noxious stimuli (noise, toxins, oxidative stresses, otological disease, poor diet, vascular disease) are unclear, but not all older people have hearing problems
• The high frequencies are lost first—usually noticed when high-pitched ♀ voices become hard to hear. As consonants are high frequency, the patient can often hear noise, but not understand, feeling that everyone is ‘mumbling’ (loss of discrimination)
• ‘Recruitment’ is a common problem where the thresholds for hearing and discomfort are very close (‘Speak up . . . don’t shout’)
• Busy, noisy environments make hearing harder, so patients may avoid social situations
• There is no treatment to halt progression, but hearing aids may help
Other ear changes with age
These include:
• Thinner walls to the external auditory canal, with fewer glands, making it dry and itchy
• Drier wax due to ↓ sweat gland activity, making accumulation (a cause of reversible hearing impairment) more common. Ear syringing is no longer recommended—try olive oil or sodium bicarbonate drops. ENT can provide microsuction for resistant cases
• Degenerative changes of the inner ear and vestibular system contributing to ↑ in deafness, vertigo, and tinnitus
Classifying deafness
Conductive
A disturbance in the mechanical attenuation of sound waves in outer/middle ear, preventing sound from reaching the inner ear.
• It can be caused by outer ear obstruction (e.g. wax, foreign body, otitis externa), some types of tympanic membrane perforation, tympanosclerosis, or middle ear problems (effusion, otosclerosis, ossicular erosion 2° to infection or cholesteatoma)
• It may be surgically correctable and can be helped by a hearing aid
Sensorineural
A problem with the cochlea or auditory nerve, so impulses are not transmitted to the auditory cortex.
• Caused by genetic or perinatal factors in children
• In adults, may be traumatic, infective (viral, chronic otitis media, meningitis, syphilis), noise-induced, degenerative (presbyacusis), ototoxic (e.g. aminoglycosides, cytotoxics), neoplastic (acoustic neuroma), or others such as Ménière’s disease
• The appropriate hearing aid can be helpful
• Cochlear implants can be considered in severe sensorineural deafness but seem less effective than in younger patients, perhaps due to limitations in cerebral processing
Mixed
A combination of both conductive and sensorineural—probably the most common cause in older people.
HOW TO . . . Communicate with a deaf person
• Ensure hearing aids are inserted correctly, are turned on, and have working batteries
• Speak clearly and at a normal rate
• Use sentences, not one-word answers—this gives contextual cues to lip readers
• ↑ the volume, but do not shout
• Lower the pitch of the voice
• Maximize face-to-face visual contact—look straight at the person, and ensure there are not bright lights behind you that will dazzle
• Use visual cues when talking (e.g. hand gestures)
• Be patient—repeat things if asked, changing the sentence slightly if possible
HOW TO . . . Assess hearing
General
Conversation will give an informal idea of hearing ability.
Clarify by performing free field speech tests by asking the patient to repeat words spoken in a whispered voice, conversation voice, and shouted at 60cm from the ear. The non-test ear is masked by pressing the tragus backwards and rotating it with the index finger. Sit the patient next to you, so that lip reading is not possible.
History
• Rate of onset and progression (witnesses will often be more accurate than patients)
• History of trauma, noise exposure, or ear surgery
• Family history of hearing problems or hearing aid use
• History of ototoxic drugs, e.g. aminoglycoside antibiotics (gentamicin, streptomycin, etc.) and high-dose furosemide
• Associated symptoms (pain, discharge, tinnitus, vertigo)
Examination
• External ear and canal (looking for wax, inflammation, discharge, blood, abnormal growths, etc.)
• Drum (perforations, myringitis, retraction, bulging of drum, etc.)
• Tuning fork tests (with a 512kHz fork) may be helpful. Both are based on the principle of improved bone conduction perception with a conductive hearing loss
• Rinne’s—compares air and bone conduction. Hold the tuning fork in front of the ear, then place on the mastoid, to compare air and bone conduction. Air > bone is normal. Bone > air implies defective middle and outer ear function
• Weber’s—assesses bone conduction only. Hold the tuning fork at the vertex of the head, and ask which ear hears the sound most loudly. With conductive deafness, it is heard loudest in the deafer ear; with sensorineural deafness, it is heard most loudly in the normal ear
Who to refer?
Patients with sinister features should be referred to an ENT surgeon:
• Recent or abrupt hearing loss
• Unilateral hearing loss or tinnitus
► Sudden-onset sensorineural deafness is an ENT emergency and requires urgent referral (causes include infection, vascular event, tumour, leaking canals, etc.)
All other patients with suspected hearing loss should be referred routinely to an audiologist for further assessment and management.
Audiology
The majority of patients with hearing impairment are managed by audiologists and hearing therapists. They do the following.
Specialized hearing tests
• Audiometry—quantifies the degree and pattern of loss. May be ‘pure tone’ (using signals at varying frequencies and intensities) or ‘speech’ (discriminating spoken words at differing intensities). The hearing thresholds are charted on an audiogram and interpreted by the audiologist (indicates conduction or sensorineural deafness, which frequency, and which ear)
• Impedance tympanometry—indirectly measures the compliance of the middle ear, identifying infection and effusion in the middle ear and Eustachian tube dysfunction
• Evoked response audiometry—measures action potentials produced by sound. No conscious response is required by the patient and so tests are less open to bias. (Before MRI, this was the main diagnostic test for acoustic neuromas)
Recommend and fit hearing aids
Many types. Help patients to have realistic expectations about their hearing aids (rarely a ‘miracle cure’) and train them how to use them optimally (e.g. minimizing background noise). Programme digital hearing aids.
Offer practical advice
About assistive listening devices such as:
• Alternative signals—buzzers and flashing lights, instead of doorbell or telephone ring; vibrating devices that attach to the wrist and alert the wearer to environmental noises. Hearing dogs can also be used
• Television—subtitles, or devices that connect to the hearing aid allowing the television signal to be amplified
• Telephones—with high-/low-volume control and ‘T’ settings that amplify the telephone noise without the background noise
• Transmitter and receiver devices (infrared or FM radio wave) for use in theatres, etc. with transmission from the sound source. The listener can adjust the volume in their receiver
• Advise about better communication
Aural rehabilitation
Age-matched group sessions that help with adjustment to the sudden reintroduction of noise with a hearing aid (after what is usually a gradual hearing loss), teach skills (e.g. blocking out background noise, lip reading), and share practical tips (e.g. eating in a booth at a restaurant to limit background noise).
Other
• Counsel about psychosocial implications of hearing impairment
Hearing aids
The past decade has seen many advances in hearing aid technology and performance. Modern hearing aids offer improved fidelity, greater amplification, and frequency-specific amplification. Patients who have tried hearing aids in the past and not found them beneficial should be encouraged to try them again.
What do hearing aids do?
Generally consist of a microphone that gathers sound, an amplifier that ↑ the volume and a receiver that transmits amplified sound. Most hearing aids also include circuitry that filters and processes sound prior to amplification.
Whom do they help?
• Help many to some degree, but not all
• Does not restore normal hearing—the wearer needs to learn to interpret the new auditory input efficiently
• Conductive hearing loss is helped more than sensorineural loss
What are the different types?
Different sizes
• Smaller units (e.g. completely-in-the-canal devices) are cosmetically more appealing and give good reception for mild to moderate hearing loss, but are fiddly and expensive
• Medium-sized units (e.g. in-the-ear devices) are more visible and have more feedback, but can be used for worse hearing loss
• Larger units (e.g. behind-the-ear) provide the most amplification and are easier to handle, but suffer from feedback if the ear mould deforms
Monaural versus binaural—binaural hearing aids yield a subjective improvement in sound clarity, but monaural may be considered for unilateral loss.
Analogue devices
• Cheapest, with least processing of sound
• Set to hearing loss at the time of fitting
• Audiologist adjusts amplification and tonality settings at time of fitting, but these are then fixed
• Patient can adjust the volume manually (turn the device volume up when the noise is quiet, and down when it is loud)
Digitally programmable devices
• More expensive, with moderate sound processing
• Analogue circuit that can be adjusted at the time of fitting by a computer programme to best fit the patient’s needs
Digital devices
• Most health authorities now fit digital hearing aids for all new referrals and exchange old analogue aids. All but the most expensive are funded by the NHS where clinically indicated
• Programmable with flexible digital circuits that manipulate each sound according to pitch and volume to give the clearest sound for that individual
• Higher clarity of sound, less circuit noise, faster processing, and automatic volume control
Disposable devices
• ‘One size fits all’—actually fit around 70% of patients
• Widely available, e.g. in pharmacies
• Not individually tailored, so less good
• No need for battery changes, low breakdown costs
• Last about 40 days, so expensive in the long term
Cochlear implants
• Unilateral cochlear implantation is recommended as an option for people with severe to profound deafness who do not receive adequate benefit from acoustic hearing aids
• Requires MDT assessment prior to insertion
• Simultaneous bilateral implants may be considered where there is coexistent blindness, making the patient more reliant on aural input
HOW TO . . . Use a hearing aid
To check a hearing aid
• Turn the volume up as far as it will go
• A working hearing aid will whistle
Putting it in
• The audiologist will take an impression of the ear to make an ear mould that fits snugly
• This should be inserted, so that it fits correctly and comfortably
Turning it on
• Most hearing aids have three settings: ‘O’ = off; ‘M’ = microphone (use this setting for normal conversation); ‘T’ = telecoil (use this setting with listening equipment such as loop devices. These transfer sound direct to the hearing aid and cut out background noise)
• In addition, there will often be a volume wheel, which can be adjusted as needed
What to do if there is no sound
• Check the hearing aid is not switched to ‘O’ or ‘T’
• Check the batteries are not dead, or put in upside down
• Check the mould is not clogged with wax
• Check the tubing is not wet (dry with a hairdryer) or twisted
What to do if there is a whistling or squealing noise (feedback)
• Occurs when the ear mould is not snug, allowing sound to escape into the microphone
• Check that the ear mould is a good fit (return to the audiologist if not) and is inserted correctly
• Ensure there is not excess earwax impeding fit
Maintaining the hearing aid
• Keep the hearing aid dry, away from strong heat or light
• Use a clean, dry tissue to clean, never a damp cloth
• Use wax remover on a regular basis
If the ear mould is separate (e.g. behind-the-ear), then periodically remove and wash with warm soapy water, ensuring it is totally dry before reconnecting it.
Tinnitus
The perception of a sound in one or both ears, without an external stimulus. Intermittent or continuous. Varying kinds of noises (ringing, humming, buzzing, occasionally other noises) and at varying pitches. Large spectrum of disease. More common in men than women, and incidence rises with age. Up to a quarter of older people may experience intermittent symptoms, but only 1 in 20 will be disabled by it. A quarter of patients will get worsening symptoms with time.
Tinnitus can be due to actual sounds that are generated by local structures:
• Vascular structures (aneurysmal vessels, vascular tumours, etc.—generate a pulsatile or humming noise that may worsen with exercise)
• Muscle spasms (palatal or middle ear muscles—generate a clicking noise. Usually indicates underlying neurological disease)
• Eustachian tube may be patulous (can occur after dramatic weight loss), resulting in a roaring sound
• Joints (e.g. temporomandibular joint, cervical spine joints)
More commonly, the noise is generated from somewhere within the auditory pathway (cochlear organ, nerve, brainstem, or auditory cortex) after some sort of damage or injury. The following are associated with tinnitus:
• Hearing loss—a very common cause in older people. Mechanism unclear—may be akin to phantom limb pain. Note tinnitus may precede deafness. May be associated with conductive (e.g. wax accumulation) or more commonly sensorineural deafness (including presbyacusis). Treatment of deafness (with hearing aid or occasionally cochlear implant) often results in improvement of tinnitus
• Drugs—many commonly prescribed drugs in older people can either cause or exacerbate tinnitus (see Box 21.1)
• Vascular disease—microvascular damage to the auditory system, or a stroke affecting the auditory cortex. Modify vascular risk factors to limit progression
• Infection, e.g. chronic otitis media. Treat the cause, but may have residual problems
• Other—Ménière’s disease, diabetes, thyroid disease, Paget’s disease, brain tumour (intracanalicular and cerebello-pontine), trauma, and autoimmune disease. Treat underlying cause
History
• Obtain a description of tinnitus. This may indicate the cause, e.g. pulsatile noise is often vascular; clicking noise is often due to palatal muscle spasms; high-pitched continuous noise is usually due to sensorineural hearing loss; low-pitched continuous noise is more commonly seen (but not exclusive to Ménière’s disease)
• Screen for possible causes (drug history, ear disease, noise exposure, injury, etc.)
Examination
Should include full head and neck examination, cranial nerve examination, auscultation for bruits, and inspection of the auditory canal.
Investigation
Check FBC, glucose, and thyroid function. Refer to specialist for full audiometric assessment and possible imaging, especially if unilateral (MRI ± angiography).
Treatment
• Difficult and frustrating—often best done in specialist clinics with MDT support
• Stop all ototoxic medication and avoid in future
• Assess whether caffeine, aspartame sweetener, alcohol, nicotine, and marijuana worsen tinnitus and avoid if so
• Treat the cause wherever possible
• Strong association with insomnia and depression, both of which worsen the suffering and should be treated. Some evidence to suggest that antidepressants (SSRIs) may help, even when there is no overt depression
• Many other treatments have been tried (e.g. lidocaine, magnetic and ultrasonic stimulation, melatonin, Ginkgo biloba, niacin, and zinc), but limited evidence they work and adverse effects common
• Hearing aids are useful if hearing loss—the ↑ awareness of the background sound tends to make the noise less apparent
• Masking techniques involve wearing a ‘white noise’ generator, rather like a hearing aid that aims to distract the patient from the tinnitus by reducing the contrast between the tinnitus signal and background noise, improving the plasticity of the central auditory cortex and thereby facilitating a reduction in perception of the sound
• Mainstay of treatment is aimed at adjusting patients’ perception of the tinnitus, trying to habituate them to the noise and limiting the negative emotions it generates. Includes tinnitus retraining therapy, biofeedback, stress reduction techniques, and cognitive and behavioural therapy
• Tinnitus support groups can be helpful ( http://www.tinnitus.org.uk)
http://www.tinnitus.org.uk)
Box 21.1 Drugs causing or exacerbating tinnitus
Vertigo
Definition
Vertigo is the hallucination of movement. A sensation of rotatory motion either of the patient with respect to the environment (‘it’s like being on a roundabout’) or the environment with respect to the patient (‘the room is spinning’). The key element is a feeling of motion, without which a clinical diagnosis of vertigo should not be made.
Understanding vertigo
The vestibular system comprises the temporal bone labyrinths (composed of the semicircular canals, the saccule, and the utricle), the vestibular nerve, and the central vestibular structures in the brainstem. Normally, there is a constant input from both ears updating the central structures on head position. In the brainstem, they are integrated with inputs from the visual cortex and from proprioceptive receptors (most important are the neck and ankles). Any interruption of this input leads to an excess of information from the good side, and so an acute feeling of dizziness and nausea (vertigo), along with disruption of the vestibulo-ocular reflex (which will cause nystagmus). This situation continues until either input is restored or the vestibular system adapts to the altered balance of signals.
Adaptation means that:
• Vertigo is not a chronic condition. Multiple recurrences may occur, but a complaint of long-standing continuous dizziness is not vertigo
• Vertigo rarely occurs with slowly progressive conditions (e.g. acoustic neuroma), as adaptation occurs along the way
• All vertigo is made worse by head movement—if not, then seek an alternative diagnosis
• The use of vestibular sedatives, e.g. prochlorperazine, should be limited to the acute phase for symptom relief only—prolonged use will delay adaptation
► There is no indication for long-term use of vestibular sedatives.
Causes
(See Table 21.1.)
• Many patients complaining of dizziness will have vertigo (see  ‘Dizziness’, p. 112)
‘Dizziness’, p. 112)
• Over all ages, 80% of vertigo arises from peripheral structures (the ears) and 20% from central structures (the brain)
• Peripheral vertigo is due to benign positional paroxysmal vertigo in up to 50%
• Central vertigo is usually due to stroke
• The proportion of central vertigo ↑ with age, because of the ↑ incidence of stroke
Table 21.1 Common causes of vertigo
| Condition | Features | Cause | Treatment |
| Benign paroxysmalpositional vertigo (BPPV) | Mild episodes lasting less than a minute, recurring frequently over weeks to months |
Resolves spontaneously but may recur Epley’s manoeuvre may help (see |
|
| Acute vestibular failure(labyrinthitis) |
Acute onset of severe vertigo, lasting hours to days |
Ischaemia of vestibular apparatus, often preceded by a viral respiratory tract infection |
High-dose steroids acutely may speed recovery Treat with vestibular sedatives only while vomiting, then allow adaptation to occur |
| Ménière’s disease | Recurrent episodes of violent vertigo, vomiting, tinnitus, ear fullness (lasting up to 12h), and fluctuating hearing loss | Dilation of endolymphatic space in the canals—primary cause still unknown |
Symptomatic treatment of acute attacks Betahistine is a labyrinthine vasodilator Diuretics may reduce attack frequency Surgical options include grommet insertion, transtympanic gentamicin, endolymphatic decompression, and vestibular nerve sectioning |
| Vertebrobasilar stroke |
TIAs cause stuttering symptoms (see Box 5.1). Stroke will cause abrupt onset, prolonged symptoms Vertigo is most common symptom, usually associated with other neurology (e.g. ataxia, diplopia, visual loss, slurred speech, motor or sensory impairment) Cerebellar stroke can cause vertigo alone |
After stroke, slow improvement is normal, but often residual defects Modify vascular risk factors (see |
Vertigo: assessment
History
• This is the most important diagnostic tool in vertigo. Use open questions with clarification
• Describe the dizziness—is it a sensation of movement of self or the room (likely vertigo)? Or a light-headed feeling (less likely vertigo)? A non-specific description does not exclude vertigo
• Establish if likely peripheral (abrupt onset and cessation with nausea, vomiting, and tinnitus) or central (more prolonged, less severe, less positional episodes; usually with other neurological symptoms and signs)
• Ask about onset, severity, duration, progression, and recurrence to narrow down the cause (see Table 21.1)
• Ask about provoking factors—may be spontaneous or brought on by changes in middle ear pressure (sneezing, coughing) or head/neck position (question carefully to distinguish this from orthostatic symptoms)
• Ask about associated symptoms, e.g. tinnitus and hearing loss (is it worse during an attack?)
• Ask about predisposing factors, e.g. vascular risk factors, recent infections, headache, ototoxic drugs, ear discharge, deafness, tinnitus, etc.
• Ask about psychiatric symptoms (e.g. low mood)—these are rarely offered spontaneously
Examination
• General examination (including cardiovascular examination)
• Examine eye movements for pursuit and saccades. Abnormalities in a patient with balance complaints suggests a cerebellar origin
• Head and neck examination, including otoscopy (to assess auditory canals and tympanic membranes)
• Hearing test (see  ‘HOW TO . . . Assess hearing’, p. 552)
‘HOW TO . . . Assess hearing’, p. 552)
• Vestibular assessment (see  ‘HOW TO . . . Examine the vestibular system’, p. 563)
‘HOW TO . . . Examine the vestibular system’, p. 563)
HOW TO . . . Examine the vestibular system
This is hard to do directly—it largely relies on testing the integrity of the vestibulo-ocular reflex.
• Test eye movements with the head still, looking for nystagmus (the eyes drift slowly towards the bad side, and the rapid correction phase is towards the good side). Visual fixation may suppress a peripheral nystagmus, but not a central. Peripheral lesions cause horizontal nystagmus in both eyes; central lesions cause nystagmus in any direction that is more prolonged and severe
• Try to provoke vertigo and nystagmus by asking the patient to gently flex, extend, rotate, and laterally bend the cervical spine
• Check visual acuity with a Snellen chart, both with the head still and with the patient slowly shaking their head. If acuity is >4 lines worse with head shaking, this suggests impairment
• Head thrust test—ask the patient to fix the gaze on the examiner’s nose, while the examiner turns the head rapidly to one side or the other. The patient should be able to keep the gaze fixed. If there is a peripheral vestibular problem, the gaze may drift during rotation to that side, which is manifest by a catch-up saccade back to the point of fixation. When done properly, this test has a better than 80% sensitivity and specificity for vestibular hypofunction
• Ask the patient to shake their head, and then check for nystagmus—if it is present, this implies unilateral impairment
• Nystagmus after 30s of hyperventilation can be an indicator of a vestibular schwannoma
Hallpike manoeuvre
• Tests for BPPV (50–80% sensitive)
• Sit the patient up, and stand behind them
• Hold their head turned 45° to one side
• Keep holding the head at this angle, and rapidly lie the patient down so the head is 30° below the level of the couch, looking down to the floor (steps 1 and 2 of the Epley’s manoeuvre; see  ‘HOW TO . . . Perform Epley’s manoeuvre’, p. 564)
‘HOW TO . . . Perform Epley’s manoeuvre’, p. 564)
• Ask about symptoms, while watching for nystagmus (towards the floor)
• BPPV can be diagnosed confidently when the nystagmus is latent (occurs after a few seconds), transient (stops after <30s), and fatigable (lessens with repeat testing)
• If any of these features are absent, the vertigo is likely to be due to another cause
Vertigo: management
Some specific treatments depending on the cause (see Table 21.1).
Symptomatic relief in the short term can be achieved with vestibular sedatives:
• Anticholinergics (e.g. hyoscine patch)
• Antihistamines (e.g. cyclizine, cinnarizine)
• Phenothiazines—usually sedating (e.g. prochlorperazine)
• Benzodiazepines (e.g. diazepam) if unable to take anticholinergics
May also benefit from antiemetics (e.g. metoclopramide).
These drugs are not for long-term use, and rarely beneficial in BPPV as attacks are so short-lived. Most vertigo will resolve with vestibular adaptation, leaving only brief feelings of imbalance on rapid head turns.
Some, however, will develop chronic dysfunction, in which case management is directed towards facilitating adaptation and development of coping strategies—vestibular rehabilitation. This is done by PTs or ENT specialist nurses and adopts a holistic approach. It involves a series of habituating exercises performed regularly to enable adaptation via compensation to occur. In addition to vestibular rehabilitation, consider spectacles to improve visual acuity, exercise to improve muscle strength, and a walking stick to aid peripheral balance.
Specific manoeuvres (see  ‘HOW TO . . . Perform Epley’s manoeuvre’, p. 564) and exercises are used for BPPV.
‘HOW TO . . . Perform Epley’s manoeuvre’, p. 564) and exercises are used for BPPV.
HOW TO . . . Perform Epley’s manoeuvre
(See also Figs. 21.1–21.6.)
• Aims to clear debris from the posterior semicircular canal
• Requires the patient to be fairly flexible (modified version is available for more immobile patients)
• Stand behind the patient, firmly holding the head between your hands
• Make movements quickly and smoothly, holding each position for at least 30s
• The procedure takes approximately 3–5min:
1. With the patient upright, turn the head 45° to the affected side
2. Lie the patient down, with the head still turned, until they are reclined beyond the horizontal (as in the Hallpike manoeuvre)
3. With the patient still reclined beyond horizontal, rotate the head through 90°, with the face upwards
4. Keeping the head still, ask the patient to roll on to their side
5. Rotate the head so the patient is facing downwards
6. Keep the head at this angle, and raise the patient to the sitting position
7. Finally, rotate the head so it faces the midline with the neck flexed (looking forward and downwards)
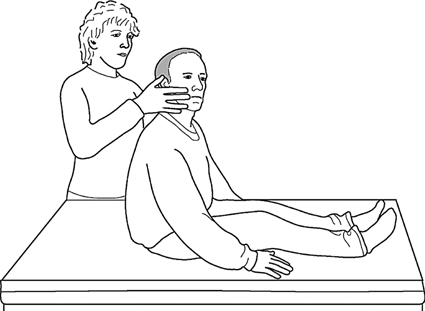
Fig. 21.1 With the patient upright, turn the head 45° to the affected side.
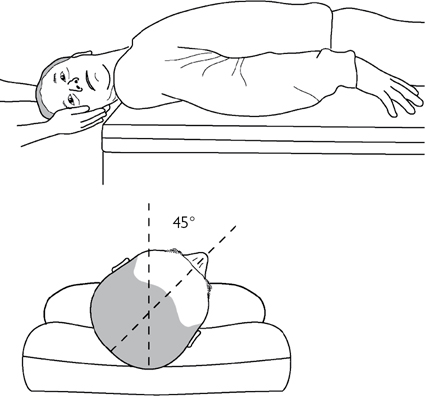
Fig. 21.2 Lie the patient down, with the head still turned, until they are reclined beyond the horizontal (as in the Hallpike manoeuvre).
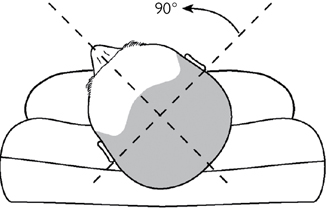
Fig. 21.3 With the patient still reclined beyond horizontal, rotate the head through 90°, with the face upwards.
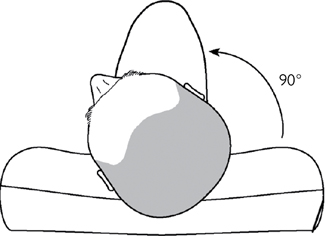
Fig. 21.4 Keeping the head still, ask the patient to roll on to their side.
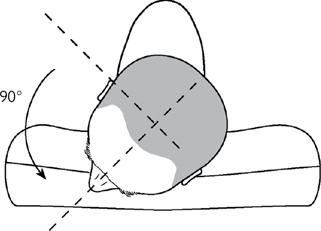
Fig. 21.5 Rotate the head so the patient is facing downwards.
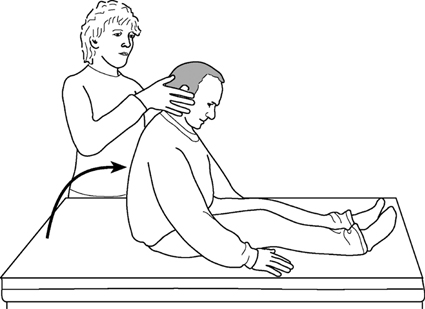
Fig. 21.6 Keep the head at this angle, and raise the patient to the sitting position. Finally, rotate the head so it faces the midline, with the neck flexed (looking forwards and downwards).