THE ELECTRONIC HEALTH RECORD
As previously discussed, patient medical records are used by health care organizations for documenting patient care, as a communication tool for those involved in the patient’s care, and to support reimbursement and research. Historically most patient records have been kept in paper form. Numerous studies have revealed the problems with paper-based medical records (Burnum, 1989; Hershey, McAloon, & Bertram, 1989; Institute of Medicine, 1991). These records are often illegible, incomplete, or unavailable when and where they are needed. They lack any type of active decision-support capability and make data collection and analysis very cumbersome. This passive role for the medical record is no longer sufficient in today’s health care environment. Health care providers need access to active tools that afford them clinical decision-support capabilities and access to the latest relevant research findings, reminders, alerts, and other knowledge aids. Along with patients, they need access to systems that will support the integration of care across the continuum. The health record of the future will likely become as critical to the accurate diagnosis and treatment of patients as the physician’s stethoscope has been to detecting heart murmurs and respiratory problems.
EHR Definition and Functions
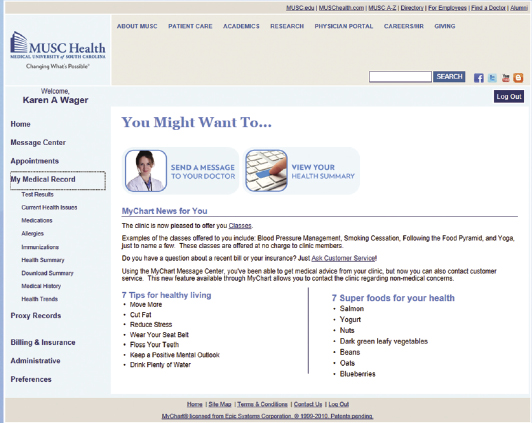
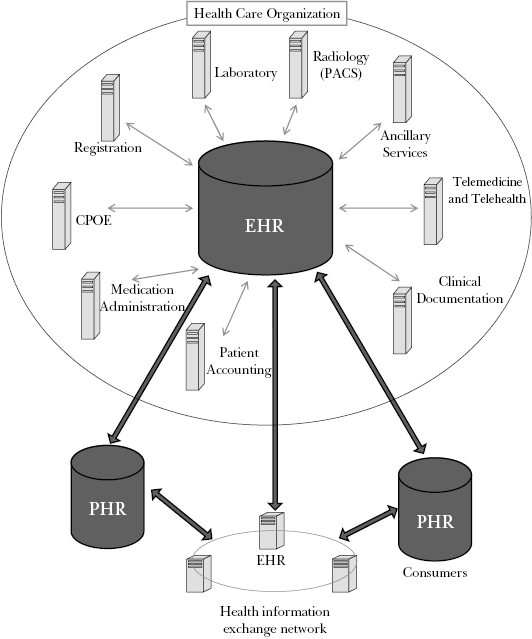
What are electronic health records, and how do they differ from merely automating the paper record? In Chapter Four we introduced the concept of the EHR when we described the Institute of Medicine’s definition of the computer-based patient record (CPR) in its 1991 report titled The Computer-Based Patient Record: An Essential Technology for Health Care. Since this Institute of Medicine (IOM) report was first published, a variety of terms have been used in the literature to describe EHR-related systems. By the late 1990s, the term CPR had been generally replaced with the terms electronic medical record (EMR) or electronic health record (EHR). In 2008, after having sought widespread input and consensus, the National Alliance for Health Information Technology proposed standard definitions for the electronic medical record, the electronic health record, and the personal health record. Table 5.1 displays these definitions. It is common to find the terms EMR and EHR used interchangeably. The IOM defines the EHR as a system that can perform eight electronic functions (Table 5.2); the first four functions are considered the core of an EHR, although all are important elements to achieving meaningful use.
Table 5.1. Health information technology definitions
Source: National Alliance for Health Information Technology, 2008.
| Electronic Medical Record | Electronic Health Record | Personal Health Record |
| An electronic record of health-related information on an individual that can be created, gathered, managed, and consulted by authorized clinicians and staff in one health care organization. | An electronic record of health-related information on an individual that conforms to nationally recognized interoperability standards and that can be created, managed, and consulted by authorized clinicians and staff across more than one health care organization. | An electronic record of health-related information on an individual that conforms to nationally recognized interoperability standards and that can be drawn from multiple sources while being managed, shared, and controlled by the individual. |
Table 5.2. Functions of an EHR system as defined by the IOM
Source: Adapted from IOM, 2003.
| Core Functions | Other Functions |
| Health information and data: includes medical and nursing diagnoses, a medication list, allergies, demographics, clinical narratives, and laboratory test results. Results management: manages all types of results (for example, laboratory test results and radiology procedure results) electronically. Order entry and support: incorporates use of computerized provider order entry, particularly in ordering medications. Decision support: employs computerized clinical decision-support capabilities such as reminders, alerts, and computer-assisted diagnosing. | Electronic communication and connectivity: enables those involved in patient care to communicate effectively with each other and with the patient; technologies to facilitate communication and connectivity may include e-mail, Web messaging, and telemedicine. Patient support: includes everything from patient education materials to home monitoring to telehealth. Reporting and population health management: establishes standardized terminology and data formats for public and private sector reporting requirements. |
An EHR can electronically collect and store patient data, supply that information to providers on request, permit clinicians to enter orders directly into a computerized provider order entry (CPOE) system, and advise health care practitioners by providing decision-support tools such as reminders, alerts, and access to the latest research findings or appropriate evidence-based guidelines. These decision-support capabilities make the EHR far more robust than a digital version of the paper medical record.
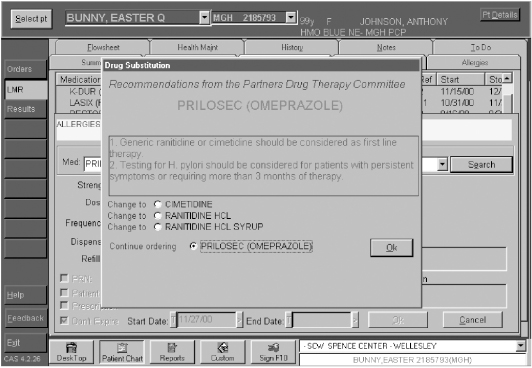
Figure 5.1 illustrates an EHR alert reminding the clinician that the patient is allergic to certain medication or that two medications should not be taken in combination with each other. Reminders might also show that the patient is due for a health maintenance test such as a mammography or a cholesterol test or for influenza vaccine (Figure 5.2).
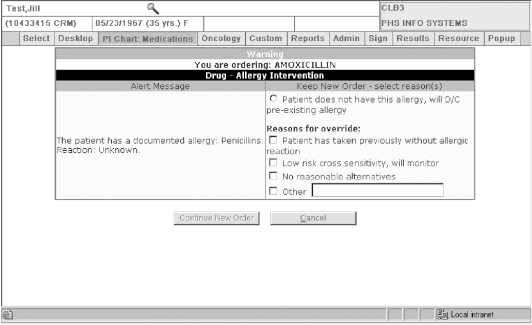
Figure 5.1. Sample drug alert screen
Source: Partners HealthCare.
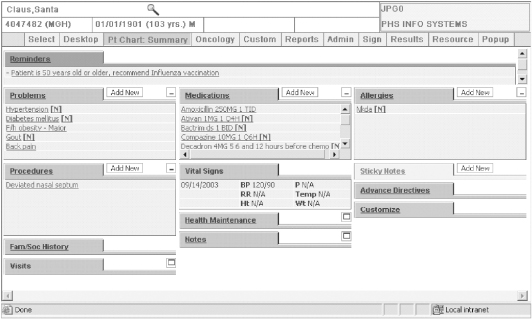
Figure 5.2. Sample EHR screen
Source: Partners HealthCare.
EHR Current Adoption and Use
How widely are EHR systems used in hospitals, physician practices, and other health care organizations? Up until most recently there have been few national studies to provide reliable estimates on the adoption rates of EHRs by U.S. physicians and hospitals, and estimates varied considerably. A number of professional organizations and researchers have attempted to estimate EHR adoption rates, yet accurately measuring adoption has been difficult for several reasons. First, no one definition for the EHR has been used consistently among researchers, and often convenience samples are used. Second, organizations may be in different stages of adoption. EHR adoption does not occur at a single moment in time, but rather evolves in stages over time. Further, the degree of usage and functionality can differ greatly from one organization to the next or even among divisions or departments in a single organization. It may not be clear whether health care providers use specific EHR functions such as decision support, even if they report having an EHR fully deployed.
The latest national survey of U.S. hospitals found that approximately 12 percent had either a basic or comprehensive EHR system (Jha, DesRoches, Campbell et al., 2009). A “basic system” was defined as including clinical documentation (demographics, physician notes, nursing assessments, problem lists, medication lists, and discharge summaries); lab, radiology, and diagnostic test results; as well as electronic ordering of medications. The comprehensive system included all of the basic system components in addition to advance directives, diagnostic images, consultant reports, computerized provider order entry, and decision-support functions such as drug alerts and clinical reminders. Larger hospitals, teaching facilities, and those located in urban regions are more likely to have EHRs than their small, public, and rural hospital counterparts (Jha, DesRoches, Campbell et al., 2009; Jha, DesRoches, Kralovec, & Joshi, 2010).
The adoption rates in physician practices range from an estimated 17 percent (DesRoches, Campbell, Rao et al., 2008) to 56.9 percent (Hsiao, Hing, Socey, & Cai, 2011), depending on the source and definitions used. As with hospitals, the larger the physician practice, the more likely the practice is to use an EHR system (DesRoches et al., 2008). A 2008 national survey of physicians found 4 percent of physicians report having an extensive, fully functional EHR, and 13 percent reported having a basic system (DesRoches, Campbell, Rao et al., 2008). Table 5.3 lists the differences between a basic system and a fully functional system as defined by these researchers.
Table 5.3. Functions defining the use of EHRs
| Basic System | Fully Functional System | |
| Health Information Data | ||
| Patient demographics | X | X |
| Patient problem lists | X | X |
| Electronic lists of medications taken by patients | X | X |
| Clinical notes | X | X |
| Notes including medical history and follow-up | X | |
| Order Entry Management | ||
| Orders for prescriptions | X | X |
| Orders for laboratory tests | X | |
| Orders for radiology tests | X | |
| Prescriptions sent electronically | X | |
| Orders sent electronically | X | |
| Results Management | ||
| Viewing laboratory results | X | X |
| Viewing imaging results | X | X |
| Electronic images returned | X | |
| Clinical Decision Support | ||
| Warnings of drug interactions or contraindications provided | X | |
| Out-of-range test levels highlighted | X | |
| Reminders regarding guidelines-based interventions or screening | X |
Less than 7 percent of solo or two-physician practices reported having either a basic or fully functional EHR (Rao, DesRoches, Donelan et al., 2011). Even among those who have adopted EHR systems, physicians from small practices are less likely to use certain features such as viewing and ordering radiologic tests, electronic prescribing, and maintaining clinical notes electronically.
Less is known about EHR adoption rates in settings other than hospitals and physician practices. The first and only study found of home health and hospice agencies reported that approximately 32 percent of home health agencies and 18 percent of hospice agencies are estimated to use computerized systems for record keeping, although it is not clear if these systems offer the level of functionality defined by the IOM (Pearson & Bercovitz, 2006). Data used in estimating these adoption rates come from the 2000 National Home and Hospice Care Survey, conducted before the latest IOM definition existed. Some states, such as California, have attempted to assess health information technology use in nursing homes and long-term care facilities (Hudak & Sharkey, 2007), but again, EHR functions can differ in these settings, and national estimates are nearly nonexistent. Most are qualitative studies examining the barriers to adoption in long-term care facilities (Cherry, Carter, Owen, & Lockhart, 2008) and experiences of early adopters (Cherry, Ford, & Peterson, 2011).
Factors Influencing EHR Adoption
Despite the relatively low rates of EHR use historically, a number of factors are driving demand. The extraordinary focus in recent years on health information technology at the federal level is a major factor. One of the primary goals of the HITECH part of the American Recovery and Reinvestment Act (ARRA) of 2009 is to improve the quality and value of health care through meaningful use of EHR systems. The law specifies that meaningful use includes electronic prescribing, health information exchange, and the reporting of quality measures. Providers participating in Medicare and Medicaid programs have the opportunity to receive incentive dollars for achieving meaningful use of EHR, or risk Medicare payment reductions if they fail to achieve meaningful use of EHR within a specified period of time. Health care payment reform initiatives require that health care providers and organizations are able to provide high-quality, coordinated, cost-effective care and report on quality indicators and outcomes. Trying to achieve these goals in a paper-driven environment, often laden with inefficient processes and duplicate tests, is nearly impossible.
In addition, over the years a number of empirical studies suggest that there is growing evidence that EHR-type systems help improve the quality and efficiency of care. Examples of this include the Veterans Health Administration (VA), which uses an EHR systemwide, so that any veteran treated at any VA hospital throughout the nation will have electronic access to his or her medical record. The VA has also been able to transform its health care system to one of the best in the world based upon quality measures (Jha, Perlin, Kizer, & Dudley, 2003). The Kaiser Permanente Health Plan is another example of an EHR adopter that has made significant improvements in the management and treatment of patients with chronic conditions through their systemwide EHR (Chen, Garrido, Chock, Okawa, & Liang, 2009). Since the early 1990s, Institute of Medicine has called repeatedly for the increased use of EHR systems in health care (1991, 2000, 2001), provided systems are safe and implemented appropriately (2011).
Health care leaders are becoming increasingly aware of the value of EHR systems to the patient, the provider, the organization, and the health care community at large in improving quality, managing population health, addressing patient safety concerns, and decreasing administrative costs. It is no longer a matter of if a health care organization will adopt and implement an EHR system; it is now a matter of when and how.
Value of EHR Systems
A number of studies over the past thirty years have demonstrated the value of using EHR systems and other types of clinical information systems within organizations. The potential benefits fall into three major categories: (1) quality, outcomes, and safety; (2) efficiency, productivity, and cost reduction; and (3) service and satisfaction. Following is a discussion of each of these major categories, along with several examples illustrating the value of EHR systems to the health care process. It is important to note, however, that not all studies have demonstrated positive outcomes. Some have shown no effect and others have shown possible safety issues associated with the introduction and use of features such as CPOE (Han et al., 2005; Koppel, Metlay, Cohen, Kimmel, & Storm, 2005) and other types of health information technology (Koppel & Kreda, 2009; Sittig & Singh, 2011; Sittig, Teich, Osheroff, & Singh, 2009). With the increased interest in and adoption of health IT, the Office of the National Coordinator for Health Information Technology (ONC) asked the IOM to establish a committee to investigate how private and public participants can make health IT–assisted care safer. In 2011, the IOM published its report Health IT and Patient Safety and outlined a number of key recommendations that are discussed more fully in Chapter Seven.
Quality, Outcomes, and Safety
Clinical information systems, including EHRs, can have a significant impact on patient quality, outcomes, and safety. Three major effects on quality are increased adherence to guideline-based care, enhanced surveillance and monitoring, and decreased medication errors. For example, several early studies have shown that physicians who had access to clinical practice guidelines and features such as computerized reminders and alerts were far more likely to provide preventive care than were physicians who did not (Balas et al., 2000; Bates et al., 1999; Kuperman, Teich, Gandhi, & Bates, 2001; Ornstein, Garr, Jenkins, Rust, & Arnon, 1991; Teich et al., 2000). Other studies have found that computerized reminders used in an outpatient setting can have a significant effect on cancer prevention activities such as the performance of stool occult-blood tests, rectal examinations, breast examinations, smoking cessation counseling, and dietary counseling (Landis, Hulkower, & Pierson, 1992; McPhee, Bird, Fordham, Rodnick, & Osborn, 1991; McPhee, Bird, Jenkins, & Fordham, 1989; Yarnall et al., 1998). EHR-related systems have also been shown to improve drug prescribing and administration by providing clinicians with information on the appropriate use of antibiotics at the point of care (Berman, Zaran, & Rybak, 1992), to reduce adverse drug reactions (Bates & Gawande, 2003; Burke & Pestotnik, 1999), to improve the accuracy of drug dosing (Duxbury, 1982), and to reduce errors of omission such as failing to act on results or to carry out indicated tests (Bates & Gawande, 2003; Overhage, Tierney, Zhou, & McDonald, 1997). Bates and Gawande (2003) suggest that information technology can reduce the rate of medical errors by (1) preventing errors and adverse effects, (2) facilitating a more rapid response after an adverse event has occurred, and (3) tracking and providing feedback about adverse effects. Likewise, EHR systems can improve communication, make knowledge more readily available, require key pieces of information (such as the dose of the drug), assist with calculations, perform checks in real time, assist with monitoring, and provide decision support. If effectively incorporated into the care process, all of these features have the potential to improve quality, outcomes, and patient safety.
Efficiency, Productivity, and Cost Reduction
In addition to improving the quality of care the patient receives, some studies have shown that the EHR can improve efficiency, increase productivity, and lead to cost reductions (S. Barlow, Johnson, & Steck, 2004; Grieger, Cohen, & Krusch, 2007; Tierney, Miller, Overhage, & McDonald, 1993). It is not uncommon for clinicians who do not have EHR access to order a second set of tests because the results from the first set are unavailable, so one way EMR systems improve efficiency is by making test results readily available to clinicians (Bates, Kuperman et al., 1999; Tierney, McDonald, Hui, & Martin, 1988; Tierney, Miller, & McDonald, 1990). In addition, EHR features such as computerized reminders and alerts can reduce pharmaceutical costs by prompting physicians to use generic and formulary drugs (Bates & Gawande, 2003; Donald, 1989; Garrett, Hammond, & Stead, 1986; Karson et al., 1999; Levit et al., 2000). EHRs can also provide the infrastructure necessary to measure care processes and aid in continuous quality improvement efforts (Edwards, Huang, Metcalfe, & Sainfort, 2008).
The cost of EHR implementations can range from $15,000 to $50,000 per provider. A network of twenty-six primary care practices in north Texas recently conducted a study evaluating the hardware and software costs, as well as the time and effort invested in EHR implementation. The average cost per physician of implementing an EHR through the first sixty days of launch was $32,409 with an estimated 134.2 hours of staff time expended per physician (Fleming, Culler, McCorkle, Becker, & Ballard, 2011). Several studies have shown that the use of EHR systems can reduce costs related to the retrieval and storage of medical records. For instance, the Memorial Sloan-Kettering Cancer Center estimated that it realized space savings of two thousand square feet after implementing an EMR, equating to a savings of approximately $100,000 a year (Evans & Hayashi, 1994). Twenty-eight ambulatory care providers affiliated with the University of Rochester Medical Center found initial EHR costs were recaptured within sixteen months of implementation, with ongoing annual savings of $9,983 per provider (Grieger et al., 2007). Much of their savings was due to reductions in storage and retrieval costs. Savings have also been realized through the decreased use or elimination of transcription services (Zlabek, Wickus, & Mathiason, 2011). Others have reported that an EHR system has led to higher-quality documentation, resulting in improved coding practices and subsequently higher reimbursement (Barlow et al., 2004; Bleich, Safran, & Slack, 1989; Wager, Lee, White, Ward, & Ornstein, 2000) and also in savings from lower drug expenditures, reduced laboratory and radiology tests (Zlabek, Wickus, & Mathiason, 2011), and decreased billing errors (Wang et al., 2003). As to the impact of EHRs on clinician time, results are mixed. Nurses are more likely to realize time savings in using computer systems to document patient information than their physician counterparts are (Poissant, Pereira, Tamblyn, & Kawasumi, 2005). This may be due in part to the fact that nurses often document using standardized forms or care plans, whereas physicians rarely use standardized templates to document their notes. One recent time-motion study found it took twenty-five seconds longer to enter a prescription order using CPOE than to handwrite the order (Devine, Hollingworth, Hansen et al., 2010). However, the study did not examine time spent in interpreting the legibility of the handwritten orders or time spent in processing the orders. Investments in patient safety and quality of care may well be worth the investment in time.
Service and Satisfaction
The third category of potential benefits to be realized as a result of using EHR systems is improved service and satisfaction, from both the patient’s and the user’s perspectives. Patients whose physicians use EHR systems like the fact that their health information (health history, allergies, medications, and test results) is readily available when and where it is needed. Several early qualitative studies have shown that patients’ response to physicians using an EMR in the examination room is quite positive (Ornstein & Bearden, 1994; Ridsdale & Hudd, 1994). Patients in practices that use an EHR system view their physicians as being innovative and progressive. And even though some physicians initially expressed concern that using the EHR in the examination room might distance them from patients or impede the physician-patient relationship, the majority by far of the studies in this area have shown that EMR use has had no negative impact on the physician-patient relationship (Gadd & Penrod, 2000; Legler & Oates, 1993; Shield, Goldman, Anthony, Wang, Doyle, & Borkan, 2010; Solomon & Dechter, 1995; Wager, Ward et al., 2005) and can enhance it by involving patients more fully in their own care (Marshall & Chin, 1998). Both physicians and patients at Kaiser Permanente found the EHR can expand and strengthen the physician-patient relationship (Cochran, 2010).
In fact, a recent national study of U.S. hospitals found that those with EHRs had significantly higher patient satisfaction scores on items such as “staff always giving patients information about what to do for recovery at home,” “patients rating the hospital as a 9 or a 10 overall,” and “patients would definitely recommend the hospital to others” than hospitals that did not (Kazley, Diana, Ford, & Menachemi, 2011, p. 26). Yet the same study found that EHR use was not significantly associated with other patient satisfaction measures (such as having clean rooms) that one would not expect to be affected by EHR use. The patient’s perception of his experience and care is important, and EHRs may play an increasing role in facilitating communication.
EHR systems can also positively affect provider and support staff satisfaction. In a 2008 national survey of physicians, 90 percent of providers using EHRs reported that they were satisfied or very satisfied with them, and large majorities could point to specific quality benefits (DesRoches, Campbell, Rao et al., 2008). Those who have had systems in place for two or more years are more likely to be satisfied (Menachemi, Powers, Au, & Brooks, 2010). Physicians who have successfully implemented an EHR system in their practice have also reported that it has improved the quality of documentation, efficiency, and had a positive impact on their job satisfaction and stress levels (Wager et al., 2000, 2005, 2008). They are proud of the quality of their records and believe that their documentation is now more complete, accurate, and available and more useful in substantiating the diagnostic and procedural codes assigned for billing purposes. EHR users such as nurses and support staff have reported that the EHR has enhanced their ability to respond to patient questions promptly. Support staff who have historically been responsible for filing paper reports, pulling paper records, and processing bills tout the many benefits of having easy access to patient information through the use of an EHR system (Wager et al., 2000).
Limitations and Need for Future Research
Despite the promising work that has been done to date in evaluating EHRs, much more work is needed, particularly in studying the impact of such systems on organizations or communities that share patient data across organizational boundaries through a health information exchange. Until most recently, the majority of research on EHRs has been limited to four academic institutions that implemented internally developed systems over many years (Chaudhry et al., 2006). In addition, studies that have examined the impact of EHR systems on efficiency have tended to focus on the user level instead of the organizational level or, ultimately, the health system level (Poissant et al., 2005). Thus, an EHR might not save an individual physician time in documenting patient information, yet that information may be more complete and therefore may reduce unnecessary tests or improve the coordination of care, and so the process may save time or money in the long run. The “system-” level benefits such as impact on quality and cost reductions over time will be increasingly important to measure with health care reform. Some experts argue that to improve quality of care, merely implementing an EHR is not sufficient (Zhou et al., 2009). Long-term users are more likely to have relatively mature EHRs with well-designed clinical decision support and order entry management, and they may be more willing to use these features. Use of decision-support features has historically been quite low among EHR users, despite its availability (DesRoches, Campbell, Vogeli et al., 2010; Zhou et al., 2009).
Noteworthy EHR Implementations
There are many examples of health care organizations that have successfully implemented EHR systems and have realized the value that comes from using them. The following examples profile the 2011 Nicholas E. Davies Award recipients in the ambulatory care category and the community health organization category. The Nicholas E. Davies Award was established in 1994 by the Computer-Based Patient Record Institute (CPRI) to recognize organizations that have carried out exemplary implementations of EMR systems. (The Healthcare Information and Management Systems Society [HIMSS] has administered the Davies Award since 2002, the year that CPRI merged with HIMSS.)