CHAPTER 20
Patient Positioning
Introduction
In recent years, perioperative nerve injuries, soft tissue injuries, and other positioning-related problems have received increasing attention from the lay press, plaintiffs’ lawyers, the anesthesiology community, and clinical researchers. This chapter provides an update of current findings and discusses possible mechanisms of injury for these potentially devastating problems.
Patients under anesthesia are at risk for injuries because they cannot protect themselves. The goal of intraoperative positioning is to place and secure the patient on the operating room table to allow adequate surgical exposure and access, without compromising physiologic function (e.g., ventilation) or injuring the patient. Patient positioning is a routine function of operating room nursing personnel and the anesthesia team; however, all members of the operating room team may be involved in positioning a patient, including the anesthesia technician. For example, an anesthesia technician may place a wrist device for securing an arterial line that has the potential to overextend the wrist and places tension on the nerves. Anesthesia technicians (and providers) also perform increasingly complex robotics, advanced imaging, and out of OR cases, each of which presents positioning challenges. A full understanding of safe positioning enables the anesthesia technician safely to assist with this surprisingly complex aspect of patient care.
General Mechanisms of Injury
Patients can be injured in multiple ways due to positioning on the operating room table. Injuries attributable to patient positioning include vision loss, abrasions, skin breakdown, pressure ulcers, hair loss, nerve damage, and joint damage. The mechanisms by which patients sustain injuries include pressure, friction, and shear forces. Forces that compress the skin and underlying tissues can compromise blood flow to important structures, particularly nerves. Normal capillaries have a pressure between 23 and 33 mm Hg. Supine patients on a hard surface routinely have pressures greater than capillary pressure (thus stopping blood flow) at points that contact the table, including the back of the head, the heels, the arms, and the sacrum. Pressure injuries usually occur where tissue is compressed against a bony prominence or the tissue is at special risk (e.g., the eye).
Awake patients who do not have mobility problems change position frequently when they become uncomfortable, thus preventing pressure-related injuries. Unfortunately, patients with regional or general anesthesia do not become uncomfortable, nor can they move. The procedure team must take great care to assure that undue pressure is not placed on any portion of the body. Even things as simple as face masks or intravenous (IV) poles can be placed in such a way as to place pressure on the body and injure a patient. Patients with compromised blood flow to tissue are at an increased risk for pressure injuries, especially those with diabetes or peripheral vascular disease. Other patient factors that increase the risk of injury include thin patients (tissues have less padding from muscle mass or fat), the elderly, and the malnourished.
Friction or shear forces can also cause injury to patients. When skin rubs against a surface, it can sustain an abrasion or a burn-like injury that blisters. You might think that anesthetized patients are immobile, and most of the time, they are; however, the surgical team may move the patient. For example, during total knee replacement surgery, the operative knee is flexed and extended multiple times. Movement of one portion of the body can move other portions of the body or even the entire body. This movement can cause the skin to rub against some portion of the operating room table or attached equipment. Alternatively, the operating team may move equipment that may touch the patient.
A common mechanism of injury due to positioning involves the overextension of joints. Each individual joint in each individual patient has a range of motion through which the joint may comfortably move. Overextending a joint can damage the joint capsule and ligaments or tendons that surround the joint. Many common sports injuries like sprains involve the overextension of joints. When a joint is overextended, it is painful. In the operating room, an anesthetized patient will not be able to tell the operating room staff that a joint is overextended. As a patient is moved from one bed to another, positioned on the table, or moved during surgery to facilitate surgical exposure, the patient is at risk for a joint injury. During these movements, the operating room staff must take care to keep joints in a neutral position that is well within the joint’s normal range of motion. For example, an anesthetized patient is positioned in the lithotomy position with his or her arms extended on armboards for surgery. In this position, the hips may be externally rotated. The operating room staff must make sure that as the joints are moved and reach their final position, they are not overextended. The hips could be injured if they were rotated too far, and the shoulders could be injured if the arms were extended away from the body more than 90 degrees.
It is important to keep in mind that some patients, due to disease or previous injury, may have a reduced range of motion in a joint. These limitations should be identified preoperatively so that the operating room staff can avoid extending the joint beyond its reduced range of motion. For example, normal patients can tolerate an arm extended to the side up to 90 degrees. However, a patient with an old shoulder injury may not be able to tolerate having his or her arm moved more than 45 degrees away from his or her body.
Even if joints are properly positioned at the beginning of surgery, their position may change during surgery while covered by drapes. The patient should be secured to the operating room table to prevent limbs or even the entire patient from falling off the table. Keep in mind that the restraints must be applied in such a way as to prevent movement but also to not improperly compress a body part.
Nerves are at particular risk for positioning injury during surgery. Nerve function and injury is discussed in Chapter 12, the Peripheral Nervous System: nerve injury severe enough to cause malfunction or pain is referred to as neuropathy. Nerve injury in positioning is usually the result either of stretching the nerve or of prolonged compression, both of which compromise blood flow to the nerve. Both the amount of stretch or compression and the duration of the insult help determine the extent of injury. In addition, longer nerves seem to be more prone to injury. Other risk factors for nerve injury include nerves with an existing problem or medical conditions that can compromise blood flow. Nerve injuries range widely in severity: minor injuries tend to resolve over time (<6 months). However, some injuries are permanent and result in lifelong pain, altered sensation, or even paralysis.
Nerve stretch is usually the result of body parts, usually extremities, placed in extreme positions. Arms or legs can be easily overextended with the good intention of improving surgical exposure. A leg or arm can easily fall off the table or an armboard. An extreme position of the extremity may not be recognized because of drapes covering the patient. On some occasions, movement of one part of the body may stretch another part, particularly if that part is secured to the table. For example, the surgical team may be tugging on an arm to improve surgical exposure, which ends up moving the patient’s torso. If the patient’s head has been secured to the table, movement of the torso can put the neck in an abnormal position. Throughout a surgery, the operating room staff should periodically check to make sure that equipment, body parts, and restraints have not moved in such a way as to injure the patient.
The most common source of nerve compression is inadequate padding of body parts that come into contact with the operating room table. Most operating room tables are covered with padded material to reduce the risk of pressure injuries. Even so, the majority of operating rooms apply additional padding to the arms, legs, heels, and head. Special care needs to be taken to ensure that any additional operating room equipment does not press on any part of the patient. It is easy for an improperly positioned Mayo stand, IV pole, or retractor support, or even the surgeon leaning against a body part, to cause nerve compression. As with nerve stretch, inadvertent changes in patient position can lead to nerve compression that may go unrecognized for prolonged periods due to surgical draping. For example, a leg that has fallen partially off the table may be resting directly upon metal or some other unpadded portion of the table or operating room equipment. Nerve compression can also arise from excessive tissue pressure unrelated to positioning, as occurs when a crush injury or an infiltrated IV line leads to swelling of an extremity that compromises blood flow.
Neuropathies
Ulnar Neuropathy
Nerve injuries are some of the most common and serious positioning injuries. Anesthesia providers focus routinely on their prevention, and anesthesia technicians should understand how they occur. Among perioperative nerve injuries, ulnar neuropathy is the most common. There are a number of factors that may be associated with ulnar neuropathy, including direct compression from the outside on the nerve (which runs next to the bony point of the elbow, along its “medial” side, i.e., the side closest to the body), nerve compression from the inside (which happens during prolonged elbow flexion), and inflammation. Key points of interest:
- Timing of postoperative symptoms: Most symptoms develop during the postoperative, not the intraoperative, period. There are good data that most surgical patients who develop ulnar neuropathy experience their first symptoms at least 24 hours postoperatively, suggesting that the mechanism of acute injury occurs primarily outside of the operating room setting (i.e., resting against a stretcher side rail for a prolonged period of time in the postanesthesia care unit). Medical patients (as well as surgical patients) also develop ulnar neuropathies during hospitalization.
- Impact of elbow flexion: The ulnar nerve is the only major peripheral nerve in the body that always passes on the outside of a joint, in this case the elbow. All other major peripheral nerves primarily pass on the inner side of joints (e.g., median and femoral nerves). This difference in anatomy may play a role in some perioperative ulnar neuropathies. In general, peripheral nerves begin to lose function and develop ischemia (poor blood supply) when they are stretched more than 5% of their resting lengths. Elbow flexion, particularly more than 90 degrees (0 degrees is when the arm is completely extended), stretches the ulnar nerve. Prolonged elbow flexion and stretch of the ulnar nerve can result in ischemic areas, causing symptoms in awake and sedated patients as well as potential long-lasting damage in all patients.
- Anatomy and elbow flexion: Flexion of the elbow stretches the tendons around the bony elbow joint and generates high pressures within the nerve as it passes through (Fig. 20.1). This may be as important a factor as prolonged pressure on the outside of the elbow joint.
- Forearm supination and ulnar neuropathy: Supination of the forearm and hand (turning the hand to face up on the armboard) does not by itself reduce the risk of ulnar neuropathy. The action of forearm supination occurs in the forearm, beyond the elbow. Supination is typically used when positioning arms on armboards or at patients’ sides because of the impact it has on rotation of the upper arm. That is, supination is uncomfortable for most patients, and they will externally rotate their upper arm to increase comfort. It is this external rotation of the upper arm that lifts the inner aspect of the elbow, including the ulnar nerve, from directly resting on the table or armboard surface. This rotation helps reduce any compression on the ulnar nerve.
- Inflammation: In many instances, it is not possible to determine the cause of ulnar neuropathy. There are a growing number of studies that document a generalized inflammation of peripheral nerves after surgery, which may present with symptoms of ulnar neuropathy. Therefore, in a subset of patients, it may be appropriate to initiate treatment with high-dose steroids.
- Outcomes of ulnar neuropathy: Forty percent of sensory-only ulnar neuropathies resolve within 5 days; 80% resolve within 6 months. But if the ulnar neuropathy is both sensory and motor, it is unlikely to resolve within 5 days; only 20% resolve within 6 months, and most result in permanent motor dysfunction and pain. The motor fibers in the ulnar nerve are primarily located in the center of the nerve. Injury to those fibers likely is associated with a more significant ischemia or pressure insult to all of the ulnar nerve fibers, and recovery may be prolonged or not possible.
- Prevention of ulnar neuropathy: Special attention should be given to padding the elbow and making sure it is not hyperextended or flexed greater than 90 degrees.
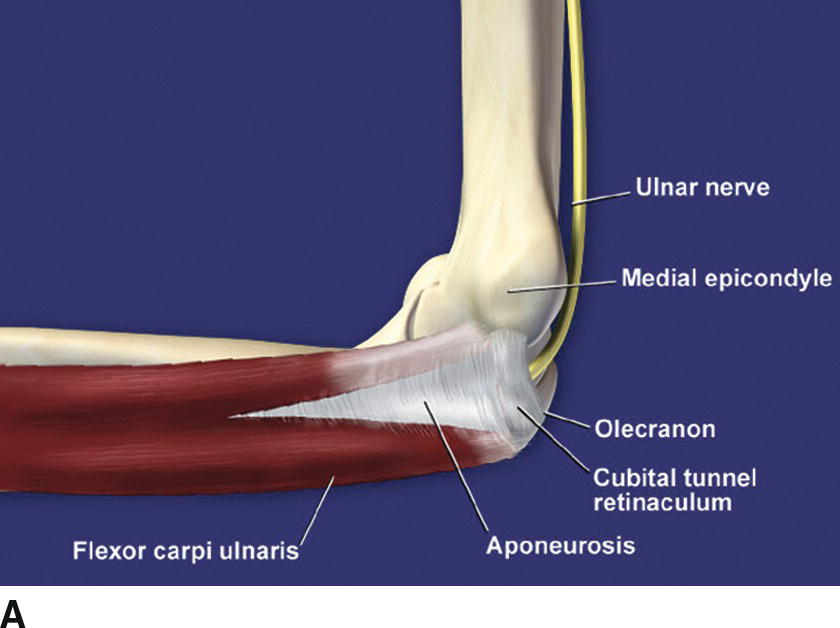
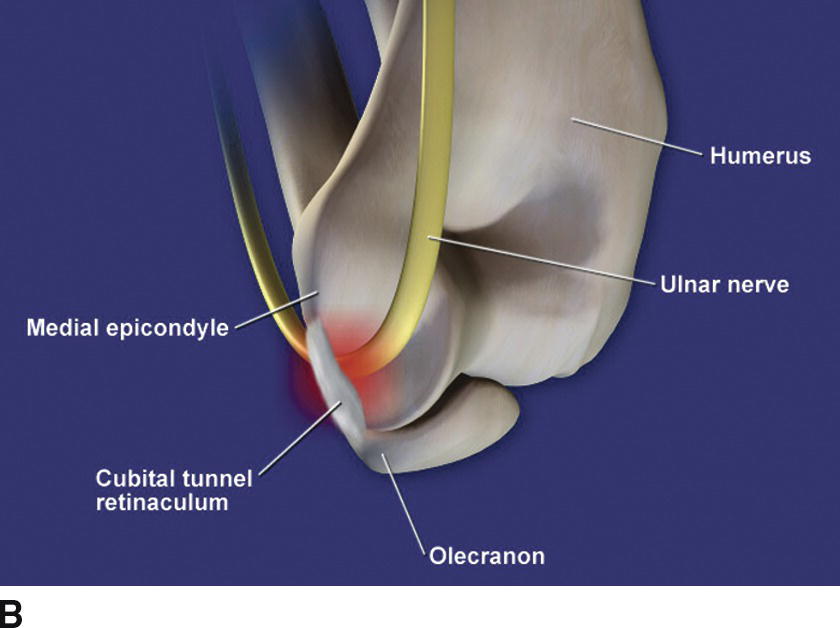
FIGURE 20.1. Ulnar nerve anatomy. A: The ulnar nerve of the right arm passes distally behind the medial epicondyle and underneath the aponeurosis that holds the two heads of the flexor carpi ulnaris together. The proximal edge of the aponeurosis is sufficiently thick in 80% of men and 20% of women to be distinct anatomically from the remainder of the tissue. It is commonly called the cubital tunnel retinaculum. B: Viewed from behind, the ulnar nerve is intrinsically compressed by the cubital tunnel retinaculum when the elbow is progressively flexed beyond 90 degrees and the distance between the olecranon and the medial epicondyle increases.
Brachial Plexopathies
The brachial plexus is the bundle of somatic nerves that originate in the neck and travel to the upper extremity. Brachial plexopathies (dysfunction of the brachial plexus) occur most often in patients undergoing sternotomies, usually for cardiac surgery. This finding is presumed to be associated with excessive retraction on the chest wall and potential compression of the nerves between the clavicle and the rib cage, or stretch of the nerves. Otherwise, patients in prone and lateral positions have a higher risk of developing this problem than those in supine positions. Finally, patients with their head secured to the operating room table and/or in the sitting position are at increased risk for brachial plexus injury. If the head is moved in the opposite direction of an arm, it can cause stretch of the brachial plexus. This can happen when the head is rotated too far to one side, the head falls off to one side, or an arm is pulled away from the body but the head is secured to the table. Key points of interest:
- Brachial plexus entrapment: There are many problems that can occur in prone and laterally positioned patients. For example, the brachial plexus can become entrapped between compressed clavicles and the rib cage.
- Anatomy of shoulder abduction: Abduction of the shoulder (lifting the arm away from the side) more than 90 degrees potentially stretches the plexus (Fig. 20.2). Therefore, it is best to keep the arm at less than 90 degrees at the shoulder, especially for extended periods.
- Prone positioning: In the prone position, it may be prudent to tuck the arms to prevent brachial plexus stretch; nerve conduction testing can detect changes in some patients if the arms are at more than 90 degrees to the body with the hands beside the head (the so-called “surrender” or “Superman” position).


FIGURE 20.2. Stretching the brachial plexus. A: The neurovascular bundle to the upper extremity passes on the flexion side of the shoulder joint when the arm is at the side or abducted less than 90 degrees. B: Abduction of the arm beyond 90 degrees transitions the neurovascular bundle to where it now lies on the extension side of the shoulder joint. Progressive abduction greater than 90 degrees increases stretch on the nerves at the shoulder joint.
Median Neuropathies
Median neuropathies primarily occur in men aged 20-40 years. These men often have large biceps and reduced flexibility (think of weight lifters). The large biceps and reduced flexibility tend to prevent complete extension at the elbow. This chronic limitation in range of motion results in shortening of the median nerve over time. Median neuropathies typically involve motor dysfunction and do not resolve readily; up to 80% of median neuropathies are still present 2 years later. Key points of interest:
- Stretch of a nerve: As mentioned in the section on ulnar neuropathy, nerves lose adequate blood flow when stretched more than 5% of their resting length.
- Arm support: When we subsequently anesthetize these men, we may fully extend their arms at the elbow and place them on armboards or at the patients’ sides. This full extension of the elbow stretches chronically contracted median nerves and promotes ischemia, often at the level of the elbow. Thus, it is important to support the forearm and hand to prevent full extension in men who have large, bulky biceps and who cannot fully extend their elbows because of a lack of flexibility.
Radial Neuropathies
Radial neuropathies occur more often than median neuropathies. The radial nerve appears to be injured by direct compression (in contrast to the median nerve being injured primarily by stretch). The important factor appears to be compression of the nerve in the middle of the upper arm where it wraps around behind the bone (Fig. 20.3). Radial neuropathies tend to have a better chance of recovery than ulnar or median neuropathies. Approximately half get better within 6 months, and 70% appear to resolve completely within 2 years. Key points of interest:
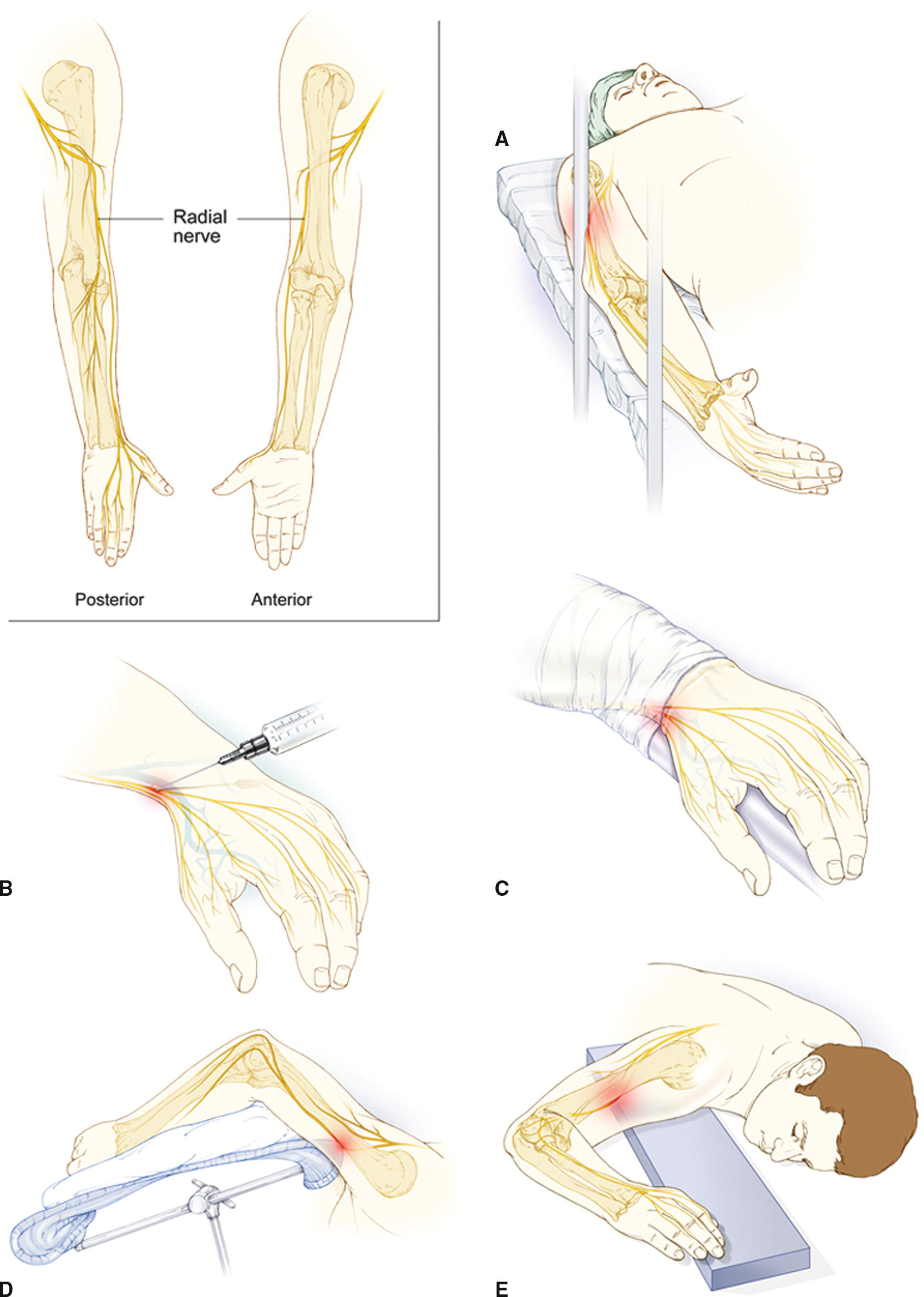
FIGURE 20.3. Potential radial nerve injuries: The anatomy of the radial nerve is shown in the upper left corner, illustrating how it wraps around the midhumerus. Reported mechanisms of perioperative injury include (A) compression by surgical retractor support bar, (B) direct needle trauma at the wrist, (C) compressive tourniquet effect by a drawsheet at the wrist, (D) impingement by an overhead armboard, and (E) compression in the midhumerus level as the arm supports much of the weight of the upper extremity.
- Surgical retractors: A case series reported several radial neuropathies associated with compression of the radial nerve by the vertical bars of upper abdominal retractor holders. The arms reportedly were impinged by these vertical support bars (Fig. 20.3A-C).
- Lateral positions: The radial nerve may be impinged by the upper armboard or sling when they protrude into the soft tissue of the mid-upper arm (Fig. 20.3D).
- An unsupported arm: Anecdotal reports discuss compression on the nerve when the elbow of a fixated arm (at side or on an armboard) slips and loses support and the weight of the upper extremity is supported at the mid-upper arm (Fig. 20.3E).
Lower Extremity Neuropathies
Although common peroneal and sciatic neuropathies have the most impact on walking, the most common perioperative neuropathies in the lower extremities involve the obturator and lateral femoral cutaneous nerves (see Fig. 20.4, which shows the arrangement of these nerves in the pelvis). Key points of interest:
- Impact of hip abduction on the obturator nerve: Hip abduction (moving the hip out to the side) greater than 30 degrees results in significant strain on the obturator nerve. This nerve passes out a small bony hole in the pelvis and, with hip abduction, pulls sharply around this rim of bone and compresses at a steep angle as it stretches along its full length. Thus, excessive hip abduction should be avoided whenever possible. With obturator neuropathy, motor dysfunction is common. Thankfully, it is usually not painful, but it can be crippling. Approximately 50% of patients who have motor dysfunction in the perioperative period will continue to have it 2 years later.
- Impact of hip flexion on the lateral femoral cutaneous nerve: Prolonged hip flexion (bending the hip up toward the torso) of greater than 90 degrees increases ischemia on fibers of the lateral femoral cutaneous nerve. One-third of this nerve’s fibers pass through the inguinal ligament in the groin as they pass into the thigh (Fig. 20.4). Hip flexion of greater than 90 degrees results in stretch of the inguinal ligament, which compresses the penetrating nerve fibers; with time, they may lose blood flow and become dysfunctional. The lateral femoral cutaneous nerve carries only sensory fibers, so there is no motor disability when it is injured. However, patients with this perioperative neuropathy can have long-term (>1 year) disabling pain in the lateral thigh. Approximately 40% of these patients have pain and sensory abnormalities that last for more than 1 year.
- Peroneal neuropathies and leg holders: It appears that most peroneal neuropathies are associated with direct pressure on the lateral leg, just below the knee, where the peroneal nerve wraps around the protruding bony head of the lower leg. Leg holders for lithotomy positioning, ranging from “candy cane” leg holders to various leg holders or “crutches” that hold the leg and foot, can impinge on the nerve as it wraps around the head of the fibula. The result can be devastating, with prolonged foot drop and difficulty walking.
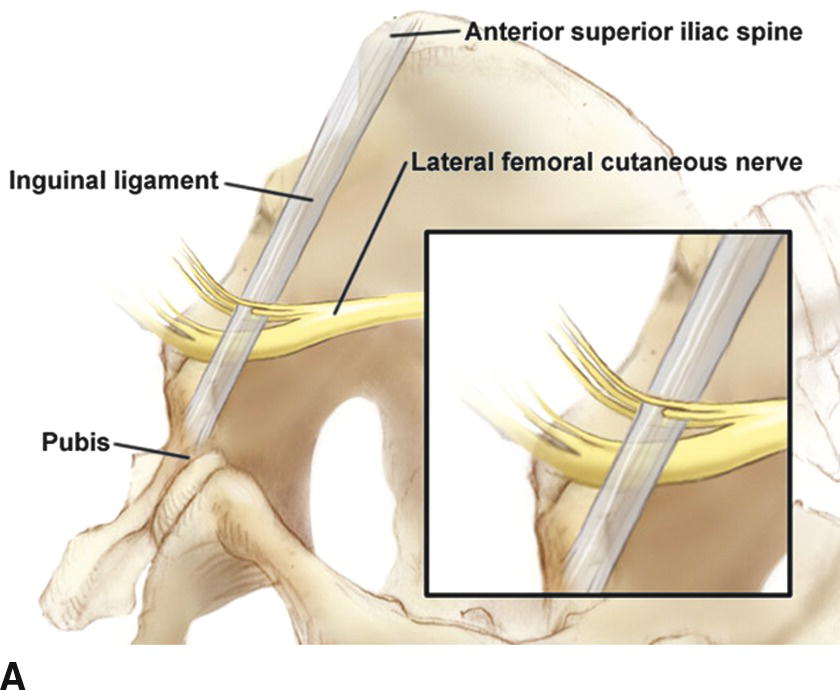
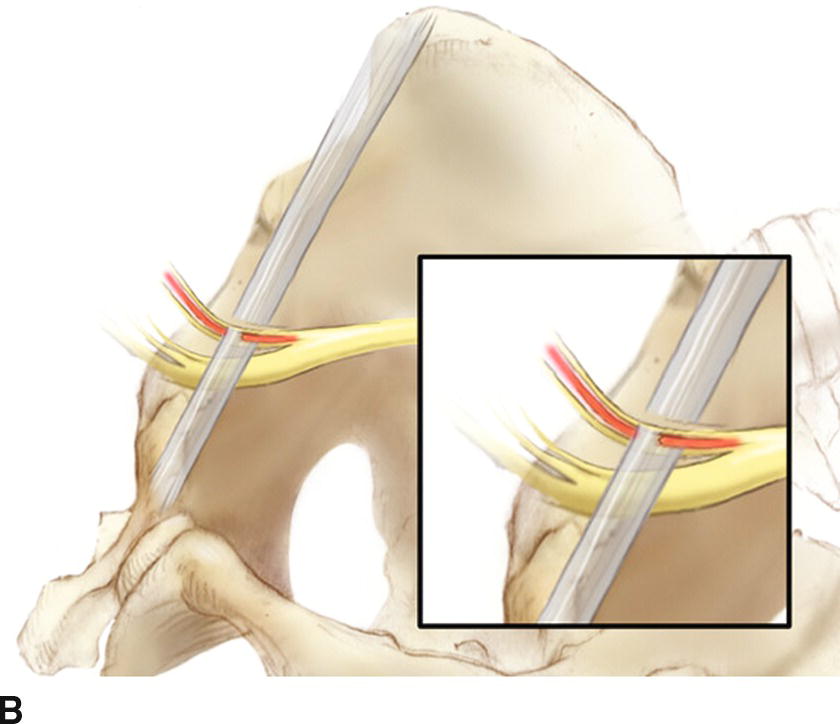
FIGURE 20.4. Anatomy of the lateral femoral cutaneous nerve. A: Approximately one-third of the lateral femoral cutaneous nerve fibers penetrate the inguinal ligament as the nerve passes out of the pelvis and distally into the lateral thigh. B: Hip flexion, especially when greater than 90 degrees, leads to stretch of the inguinal ligament as the ilium is displaced laterally. This stretch causes the intraligament pressure to increase and compresses the nerve fibers as they pass through the ligament.
Practical Considerations for Perioperative Peripheral Neuropathies
A variety of different types of padding (e.g., foam) have been used to distribute compressive forces. Although there are few studies that demonstrate that padding impacts the frequency or severity of perioperative neuropathies, it makes sense to distribute point pressure. The use of padding has been found by juries to be important in medicolegal actions. It is also prudent to position joints to avoid excessive stretching, recognizing that stretch of any nerve greater than 5% of its resting length over a prolonged period results in varying degrees of poor blood flow and dysfunction.
For patients who develop a peripheral neuropathy, it is important to first determine if the injury has primarily affected sensory or motor function. If the loss is sensory only, it is reasonable to monitor the patient daily for up to 5 days. Many sensory deficits in the immediate postoperative period will resolve during this time. If the deficit persists for more than 5 days, it is likely that the neuropathy will have an extended impact. If the loss is motor only or combined sensory and motor, it is more likely that these patients have a significant neuropathy and will need prolonged postoperative care.
Unique Positioning Problems with Catastrophic Results
Spinal cord ischemia (inadequate blood flow to the spinal cord) is a rare event that may occur when patients undergoing pelvic procedures (e.g., prostatectomy) are placed with the back arched in an extreme position, with greater than 15 degrees of hyperflexion at the L2-L3 interspace. This results in spinal cord ischemia and infarction. It is best detected with magnetic resonance imaging (MRI). Operating room tables made in the United States are designed to limit this degree of backward bending in supine patients, even when the table is maximally retroflexed with the kidney rest elevated. In almost all reported cases, the table has been maximally retroflexed, the kidney rest has been elevated, AND towels or blankets have been placed under the lower back to promote further anterior or forward tilt of the pelvis (to improve vision of deep pelvic structures). In general, anesthesia providers should not allow placement of materials under the lower back for this purpose.
Placing the patient in a steep head-down position (e.g., during robotic surgery in the pelvis) can result in sliding of anesthetized patients head-down on operating room tables. Patients often are fixated to these tables with drawsheets and other retaining devices (e.g., shoulder braces). This shifting can lead to neck (including the cervical spinal cord) injury from stretch and subclavian vessel obstruction from compression. Although the intracranial pressure also increases, it rarely results in a negative outcome. However, facial and airway edema after prolonged cases in the steep head-down position requires careful evaluation of the airway prior to extubation.
Corneal abrasions are among the most common perioperative injuries. A standardized approach to eye protection during general anesthesia has yet to emerge. Techniques to prevent abrasion injuries like taping of the eyes either are not entirely effective or, worse, may contribute to injury. Anesthesia technicians should be aware of risk factors associated with corneal injury: these include patients positioned in the prone position, patients positioned in the steep head-down lithotomy positions utilized in robotic-assisted and laparoscopic surgery, and very long surgical duration. The entire operating team should be aware that current robotic-assisted procedures carry added (not reduced) positioning risks to patients compared to previous open approaches and take measures to reduce the time patients remain in steep head-down positions.
In the steep head-up position (i.e., beach chair position used for shoulder surgery), the patient is at risk for injury related to a significant decrease in blood pressure, since blood pools in the veins of the legs and intestine. In addition, a number of severe brachial and cervical plexopathies have been reported. It appears that at least some of these plexopathies have been associated with nerve stretch or compression when patients who have their heads fixated slide laterally or distally during procedures.
Prone positioning is common during surgery and deserves special discussion. When the patient is placed facedown, the neck, face, and eyes are at particular risk for injury. Special headrests should be utilized to properly pad the face but not put pressure on the eyes. Some operating room personnel add goggle-type eye protection to further reduce the risk of injury to the eye. Special attention should be given to neutral positioning for the neck. The shoulder and arms are also at risk for injury in the prone position as discussed above and should be tucked or positioned at less than 90 degrees of abduction at the shoulder. Additional body parts that can be easily compressed in the prone position include the knees, feet, and prominent aspects of the bony pelvis. Special care should be given to properly pad these areas and to ensure that male genitals are free of pressure.
Finally, poor positioning may result in excess pressure on skin and other soft tissues and cause severe tissue breakdown. For example, tissues in direct contact with rolls that extend from the shoulder girdle across the chest and to the pelvis may become ischemic with prolonged pressure (Fig. 20.5). There are multiple cases of women with large breasts who developed severe injury of one or both breasts when they were pushed in between chest rolls. The lateral pressure was sufficient to cause crushing, tissue death, and, in most, require mastectomy. Furthermore, in extreme situations, large amounts of tissue necrosis may occur due to pressure on skin and muscle (i.e., obese patients in the prone position during spine surgery) during prolonged surgery and result in release of muscle enzymes into the blood in high enough concentrations to cause permanent kidney damage.
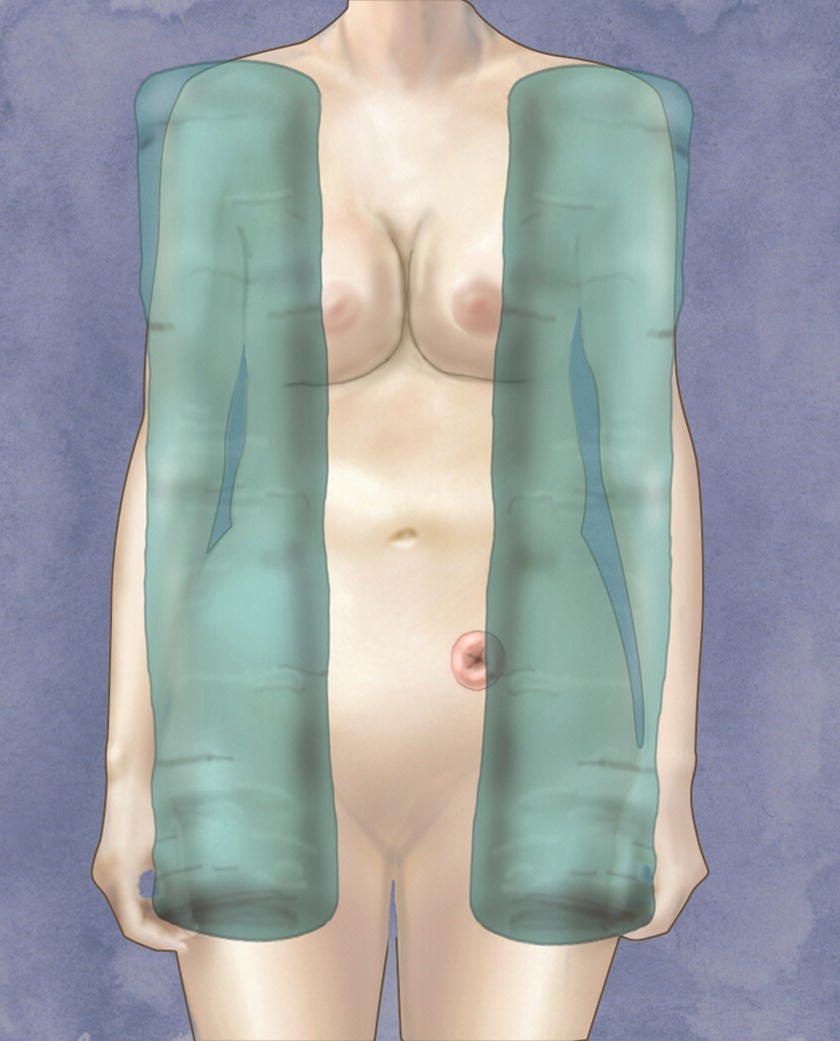
FIGURE 20.5. Chest rolls for prone positioning: soft tissues can be compressed and even become ischemic if there is too much pressure on them for long periods of time. This figure illustrates how chest rolls may compress the lateral aspects of large breasts or a stoma in prone-positioned patients.
Skin is vulnerable to injury whenever skin is fragile and wherever a noncompressible object encounters the skin. Elderly patients, burn patients and patients with other severe skin diseases, patients with chronic edema, and neonates have particularly fragile skin, and the slightest injury can remove skin, exposing the patient to infection and creating permanent scarring. In these patients, adhesives must be used with caution and removed with even greater caution; an EKG lead carelessly pulled off can remove all the underlying skin. Any item remaining under any patient, or within a tight tucking position, can cause compression even on normal skin and lead to scarring. This is of particular concern in prone positioning and arm tucking, and the anesthesia technician should be particularly alert to removal of items that have been used for placement of IVs and monitoring, location of EKG cables (none of which should be compressed directly against the patient’s skin), and padding of any items that may need to be wrapped within compressive tucking of arms such as IV or arterial lines. A small plastic cap inadvertently left under the arm for several hours can cause skin breakdown or scarring. When tucking arms, monitoring cables and IV lines should run outside tucking blankets, both to protect skin and for accessibility.
Anesthesia Technicians and Patient Positioning
The anesthesia technician is not directly responsible for positioning safety but will frequently assist the anesthesia provider. The above discussion should illustrate the multiple details involved in positioning and the specific concerns and potential hazards. Every member of the operating room team assists with positioning, and every member of the team should speak up if they see a positioning hazard. Examples where the anesthesia technician might be directly involved with patient positioning include applying a blood pressure cuff and then positioning the arm on the armboard, extending the wrist and applying a wrist guard with tape for insertion of an arterial line, turning an anesthetized patient’s head to the side in preparation for central venous access, taping of the patient’s eyes prior to intubation, or transporting a patient. In addition, while assisting with the care of a patient, the anesthesia technician may recognize that the patient is positioned in such a way as to make an injury more likely. For example, while drawing a blood gas, the anesthesia technician may notice that the arm has fallen off the armboard, an IV line is infiltrated, or the shoulder is hyperextended because the armboard has been moved. An alert anesthesia technician would notify the anesthesia provider of the potential problem. In the out-of-operating room setting, additional positioning aids may need to be brought from the operating room (and returned at the end of the case). The anesthesia technician may have the most experience with the anesthetized patient in the out of OR setting and may need to provide more assistance. Every member of the team present, including the anesthesia technician, should observe the patient and equipment during motion of tables or large imaging devices and always speak up if a hazard approaches.
Summary
Anesthetized patients are at risk for injury from positioning during surgery due to their lack of awareness or lack of sensation. Because these patients cannot protect themselves, the operating room team must take special precautions to avoid positioning injuries. Patients can sustain multiple types of injuries that can include hair loss, vision loss, or even paralysis. The most common mechanisms of injuring a patient due to positioning are stretching a joint or nerve, excessive pressure on a body part, friction, or shear forces. Eyes, nerves, and skin are at particular risk for injury due to positioning. Anesthesia technicians are important members of the operating room team and should be aware of how to properly position and pad patients to reduce the risk of positioning injuries.
Review Questions
1. The most common perioperative neuropathy involves which peripheral nerve?
A) Median
B) Sciatic
C) Ulnar
D) Obturator
Answer: C
Studies have shown that a new perioperative ulnar neuropathy typically develops more than 24 hours after surgery. This finding, along with the discovery that 90% of patients with a symptomatic ulnar neuropathy in one arm have nerve conduction problems in the opposite, nonsymptomatic arm, suggests that patients may have abnormal but asymptomatic nerves before surgery, and a variety of factors during the perioperative period cause one or both ulnar nerves to become symptomatic.
2. Which of the following is not an important step in prevention of perioperative neuropathy?
A) Avoiding hyperextension of the knee
B) Ensuring that operating room equipment is positioned securely
C) Ensuring that the shoulder is not abducted greater than 90 degrees
D) Supination of the elbow
E) Ensuring that the head is in a midline, neutral position
Answer: A
Hyperextension of the knee can cause joint injury but is not associated with neuropathy. Improperly positioned operating room equipment can easily press against an extremity and cause nerve compression. Shoulder abduction can stretch the brachial plexus. Any time the head is not maintained in a neutral position, it can stretch cervical nerves. Elbow supination is the process of turning the hand and forearm upward; this positioning will rotate the upper arm and ulnar nerve off the table, which lessens the risk of compression-related injury.
3. After surgery, a patient complains of numbness in the lateral hand and fourth and fifth finger, as well as being unable to firmly close their little finger against their thumb. Why does the motor dysfunction suggest a more significant ulnar nerve injury and a slower recovery time than a neuropathy with only sensory loss?
A) The motor fibers are damaged more easily than sensory fibers.
B) Sensory fibers heal more quickly than motor fibers.
C) A more significant ischemic injury has occurred if the motor fibers deep in the ulnar nerve are affected.
D) The motor fibers are more superficial on the ulnar nerve.
Answer: C
The motor fibers of the ulnar nerve are typically buried in the core of the nerve and surrounded by the sensory fibers. Thus, an injury that impacts the motor nerve function usually involves the sensory fibers and also suggests that a significant ischemic event has occurred to the nerve.
4. Which maneuver increases the risk of brachial plexopathy in a prone-positioned patient?
A) Abduction of the shoulder for greater than 90 degrees
B) Flexion of the elbow for greater than 90 degrees
C) Neutral position of the head
D) Placement of the arms at the sides
Answer: A
Abduction of the shoulder greater than 90 degrees places the distal nerves of the plexus on the extensor side of the shoulder joint and potentially stretches the plexus. While flexion of the elbow for greater than 90 degrees may increase the risk of ulnar neuropathy, it does not appear to increase stretch on the brachial plexus.
5. Which joint maneuver increases the risk of an obturator neuropathy in a patient who is placed in a lithotomy position?
A) Hip flexion greater than 90 degrees
B) Trendelenburg position
C) Lumbar hyperextension
D) Hip abduction for greater than 30 degrees
Answer: D
Hip abduction results in significant strain on the obturator nerve as it crosses the pelvic rim and passes through the obturator foramen. With hip abduction, the superior and lateral rim of the foramen serves as a fulcrum, compressing the nerve. Abduction beyond a patient’s normal range of motion (e.g., typically >30 degrees) may also stretch the nerve. Hip flexion greater than 90 degrees increases the risk of a neuropathy not in the obturator but in the lateral femoral cutaneous (and, less commonly, femoral) nerves, which can be compressed as they pass through the inguinal canal. Trendelenburg position places patients at risk for slipping on the operating room table, for upper extremity neuropathies if cervical stretch occurs or arms slip, and for airway edema if this is for a prolonged period, but not specifically for obturator neuropathy. Lumbar hyperextension stresses the lumbar spine and can cause spinal cord ischemia.
6. Which would be the most common cause of perioperative peroneal neuropathy in a patient in a lithotomy position?
A) Compression of the nerve by a leg holder as the nerve wraps around just below the knee
B) Hyperextension of the knee and ankle simultaneously
C) Prolonged dorsiflexion of the foot in a leg holder
D) Excessive hip flexion when the lower extremity is placed in a leg holder
Answer: A
Leg holders should be padded to avoid direct pressure on the upper lateral leg when the peroneal nerve wraps around the fibular head, which is the bony prominence located on the outside of the lower leg just below the knee. Peroneal neuropathies typically result in significant motor dysfunction, resulting in foot drop and difficulty with walking or running.
7. Which is the primary reason to pad peripheral nerves when positioning patients?
A) The pad improves blood flow.
B) The pad limits stretch of the nerve.
C) The pad decreases stretch on the nerve.
D) The pad distributes point pressure.
Answer: D
Padding typically is used to distribute and disperse point pressure from hard surfaces. This dispersion of pressure reduces the risk of compressive injury to peripheral nerves. There are no studies that indicate any specific type of padding (e.g., gel, form, or other padding materials) to be any better than the others. The key is to distribute point pressure broadly or avoid pressure on a peripheral nerve entirely.
SUGGESTED READINGS
American Society of Anesthesiologists Task Force on the Prevention of Perioperative Neuropathies. Practice guidelines for the prevention of perioperative neuropathies. Anesthesiology. 2000;92:1168-1182.
American Society of Anesthesiologists Task Force on Perioperative Visual Loss. Practice advisory for perioperative visual loss associated with spine surgery: an updated report. Anesthesiology. 2012;116(2):274-285.
Johnson RL, Warner ME, Staff NP, et al. Neuropathies after surgery: anatomical considerations of pathologic mechanisms. Clin Anat. 2015;28:678-685.
Laughlin RS, Dyck PJ, Watson JC, et al. Ipsilateral inflammatory neuropathy after hip surgery. Mayo Clin Proc. 2014;89:454-461.
Mills JT, Burris MB, Warburton DJ, et al. Positioning injuries associated with robotic assisted urological surgery. J Urol. 2013;190:580-584.
Staff NP, Engelstad J, Klein CJ, et al. Post-surgical inflammatory neuropathy. Brain. 2010;133:2866-2880.
Warner MA. Patient positioning and related injuries. In: Barash PG, et al., eds. Clinical Anesthesia. 7th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2013:803-823.
Warner MA, Warner DO, Matsumoto JY, et al. Ulnar neuropathy in surgical patients. Anesthesiology. 1999;90:54-59.