CHAPTER 55
Laser Safety
Introduction
Lasers have been used for surgery since the 1960s to cut, coagulate, and ablate tissue. Lasers provide several advantages compared to other surgical techniques, including the ability to target difficult-to-reach regions of the body as well as to deliver high amounts of energy to very small areas. The result is precise heating of surgical targets, often to the point of vaporization, with minimal swelling and trauma to surrounding tissues. This may minimize bleeding, reduce postoperative pain, and destroy small blood vessels at the target area.
Lasers are used by many surgical specialties (Table 55.1). For example, otolaryngologists often use lasers to target areas such as the larynx (voice box) and trachea (windpipe), while urologists use a different type of laser to destroy kidney stones. The use of lasers continues to expand throughout health care.
Table 55.1. Characteristics, Hazards, and Uses of Medical Lasers
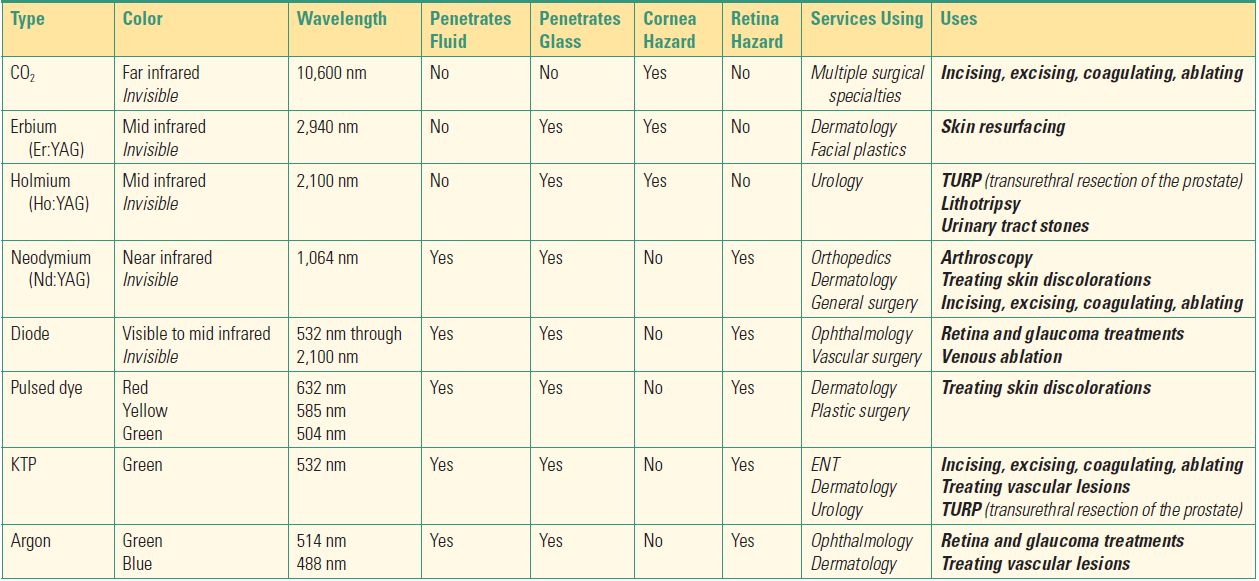
Many different laser types, with their typical uses and potential hazards, are listed here.
Laser use is not without risks. Anesthesia technicians will work throughout areas where lasers are in use and need familiarity with the various types of lasers, as well as the particular risks and protective measures that are unique to each.
Laser Technology
Laser is an acronym for “Light Amplification by Stimulated Emission of Radiation,” a process of producing and amplifying light energy. Laser light, like all forms of electromagnetic energy, travels in waves and may be either visible with a distinct color or lie outside the visible spectrum (Fig. 55.1). The length of each wave (wavelength) determines each laser’s unique properties, such as energy, color, and ability to affect certain tissues in the body.
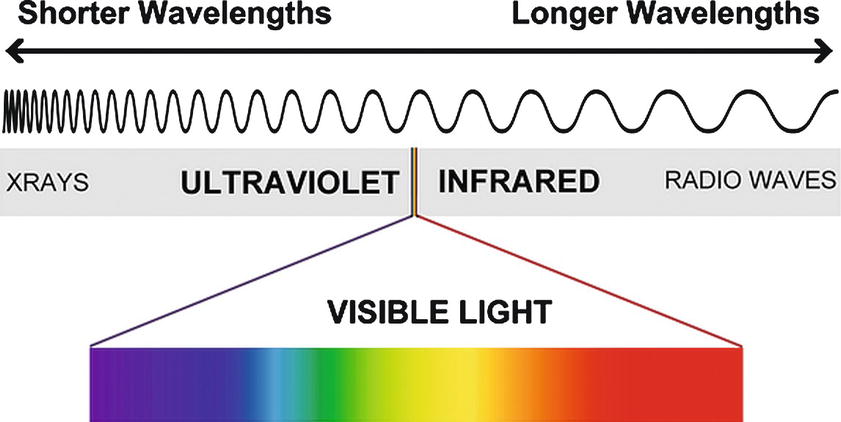
FIGURE 55.1. The wavelength of a laser beam determines whether it is invisible (infrared or ultraviolet) or visible, with a distinct color.
Three main components are required to produce laser light:
1. An energy or power source.
2. An active medium energized by the power source (solid, liquid, or gas).
3. Mirrors used to amplify and channel the energy from the active medium into the light that is emitted.
A laser beam is produced by energizing the active medium, thereby generating energy of a specific wavelength. The type of material used for the active medium determines the beam’s characteristics and therefore how it is used, as well as related hazards. Ordinary light consists of many wavelengths that are out of phase from each other and spread out over distance (Fig. 55.2). In contrast, the laser energy produced is monochromatic (a single wavelength), travels in the same direction with all waves in phase, and does not diverge or spread out over distance, permitting an intense amount of energy to focus on a small target from far away.
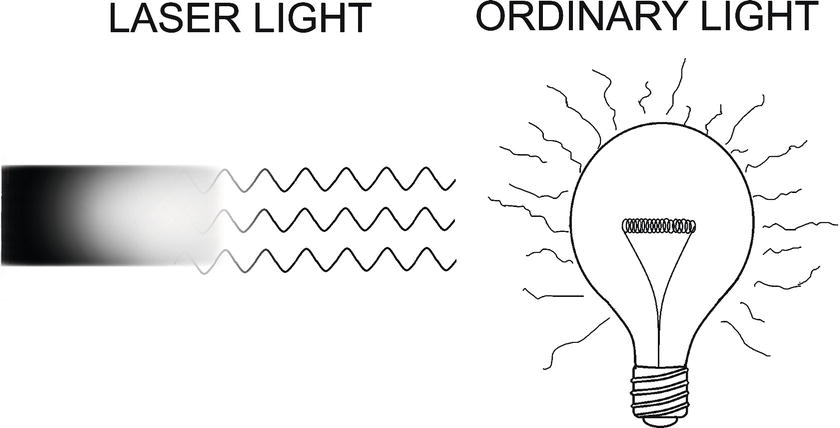
FIGURE 55.2. Laser beam energy travels in waves that are identical (monochromatic), line up perfectly (in phase), and travel together in the same direction (don’t diverge), in contrast to ordinary light.
Laser Interactions with Tissues
Laser energy has a variable interaction with a target tissue depending on its wavelength and the composition of the target substance. Laser energy may:
- Travel through a substance without affecting the substance
- Be absorbed by the substance at the point of impact, generating heat
- Reflect off the target substance, either unchanged or with scattering
The goal when using a laser is to produce the desired effect by heating the target tissue without affecting adjacent tissues. Laser energy absorbed as heat can produce a plume of smoke and steam. At lower temperatures, protein remodeling and coagulation occur.
A laser’s unique wavelength and characteristics are used to selectively treat a target tissue (Table 55.1). A particular laser is used because its wavelength is absorbed by certain colors (e.g., hemoglobin in vascular lesions such as port-wine stains or a particular pigment in the skin during removal of a colored tattoo). Laser beams with longer wavelengths, such as the carbon dioxide laser, are readily absorbed by water in the superficial tissue layers. This minimizes deeper penetration, making it ideal for targeting only the surface of a tissue. Other lasers, depending on their wavelength, interact with other substances and, as a result, can target deeper structures. The main factors determining the effect of a laser on a given tissue are listed below:
- Laser power (watts)
- Duration of exposure
- Surface area exposed (spot size)
- Wavelength
- Target tissue composition
Safety Concerns
Lasers have many hazards associated with their use, the most important being eye injury, fire, and air contamination. Other risks include damage to soft tissue, perforation of the trachea, venous gas embolism, and death. Laser usage must be limited to trained personnel in the operating room. Most lasers must be handled with care to avoid damage to the unit. Carbon dioxide lasers are the most susceptible to damage. The delivery system is composed of small mirrors necessary to carry the laser beam from the laser unit to a handpiece or scope. It is important to handle the machine carefully since the mirrors can easily be misaligned, resulting in a laser malfunction or a misdirected laser beam (Fig. 55.3).

FIGURE 55.3. A typical CO2 laser showing the articulated arm with mirrors located at each joint that are necessary to reflect the laser beam down the arm. These mirrors are easily knocked out of alignment, which can seriously affect laser function (Courtesy of Laser Engineering Inc., Nashville, TN.).
Some lasers use a fiber to deliver laser energy to the target tissue. These fibers are fragile, and stretching, bending, or kinking can cause damage to the fiber with the potential for laser energy to escape at the point of damage (Fig. 55.4A-C). The laser unit should always be in the standby mode when not actively being used (Fig. 55.5). Every laser has a red emergency stop button. When there is a malfunction, someone must press that button to shut down the laser (Fig. 55.6).

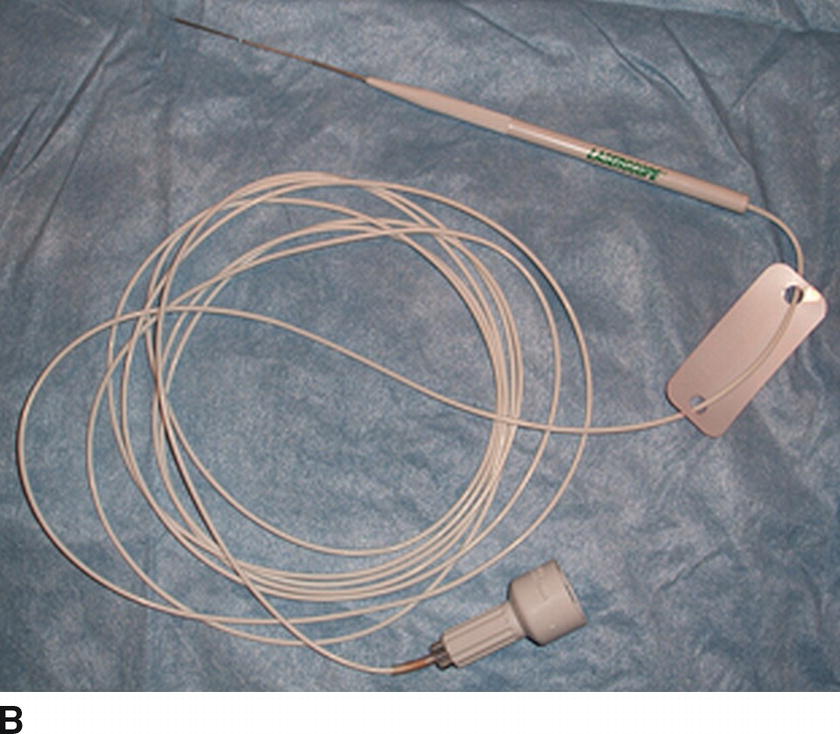
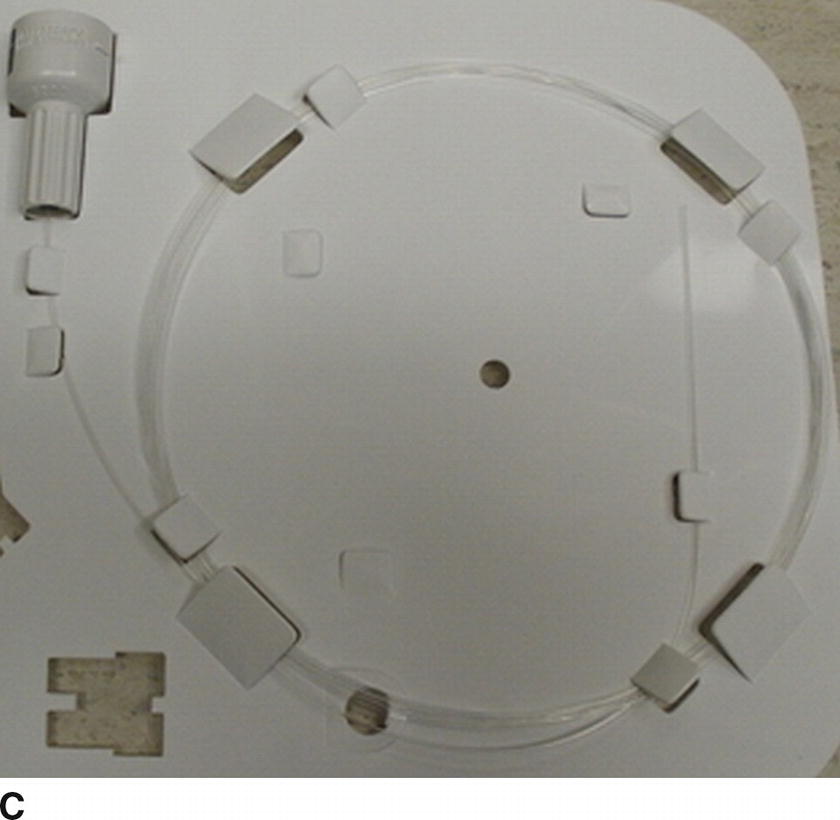
FIGURE 55.4. A KTP laser and its associated fibers. A: The Aura KTP laser (Boston Scientific Corp., Quincy, MA). B, C: Two types of fibers used with this laser. (Image provided courtesy of Boston Scientific. © 2018 Boston Scientific Corporation or its affiliates. All rights reserved.)
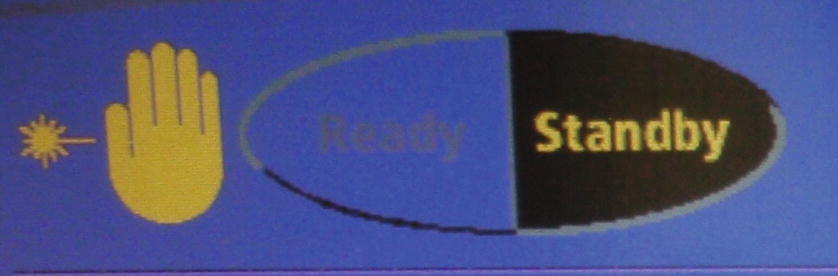
FIGURE 55.5. Here is an example of ready and standby buttons. The ready button switches the laser from the standby mode to the ready mode. By pressing the standby button, the laser changes from the ready mode to the standby mode.
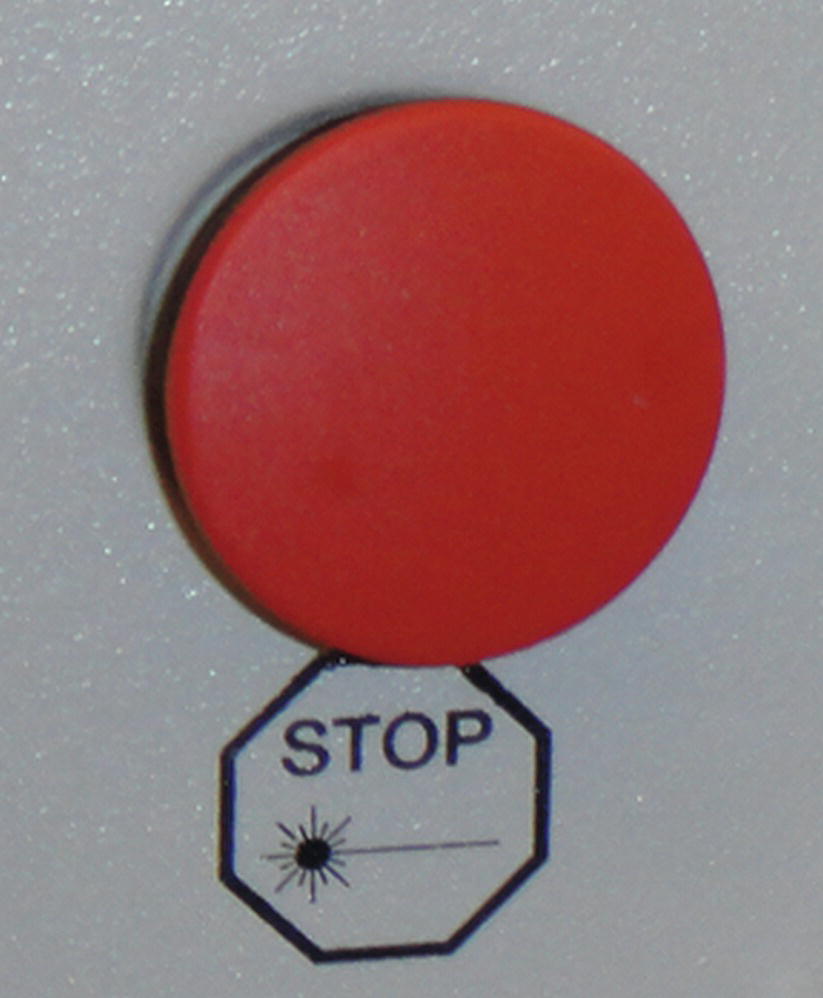
FIGURE 55.6. The emergency stop button is a large round red button that has the same function on all lasers.
Eye Injury and Protective Eyewear
Lasers used during surgery have the potential to damage both superficial (corneal) and deep (retinal) structures of the eye. Lasers with longer wavelengths, such as carbon dioxide and holmium, are incapable of penetrating fluid, so most of their effect is on the cornea. Other lasers, such as the Nd:YAG and diode lasers, are capable of penetrating fluids and act upon the deeper structures of the eye. Ophthalmologists often use diode lasers to treat the retina. If one of these laser beams able to penetrate fluid accidentally contacts the unprotected eye of a staff member or patient, the eye structures can focus that beam onto the retina and cause injury.
All laser units contain a high-powered treatment laser and a low-powered aiming beam laser, each with its own unique wavelength. The aiming laser beam is constantly emitted and visible while the laser unit is on. The treatment laser beam is only emitted when the laser is in ready mode and the pedal is depressed. It is important to wear protective eyewear specific to the type of treatment laser being used. The eyewear has been designed to absorb the specific wavelength originating from that particular laser. The physical space in which injury from a laser can occur, which may include the entire room where a laser is being used, is called the nominal hazard zone. Laser-specific protective measures, including laser eyewear, should be used in this area. The room where a laser is used must have a standardized sign, as mandated by the American National Standards Institute (ANSI), posted at each entrance. The wavelength of the treatment laser being used should be listed on these signs (Fig. 55.7A). Protective eyewear should be worn before entering this area. The manufacturer must specify the wavelength, in nanometers (nm), or a range of wavelengths, that the protective eyewear is designed to absorb (Fig. 55.7B and C). The wavelength in nanometers (nm) on the eyewear must match the wavelength (nm) listed on the sign for the treatment laser being used. It is important to note that the color of the protective eyewear itself is not a reliable indicator of which wavelengths are absorbed. Laser-protective eyewear may not completely protect against exposure to a direct beam of laser energy.
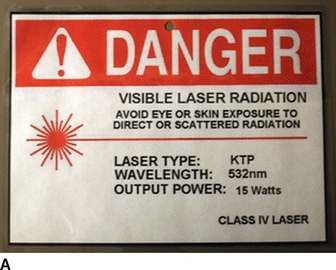
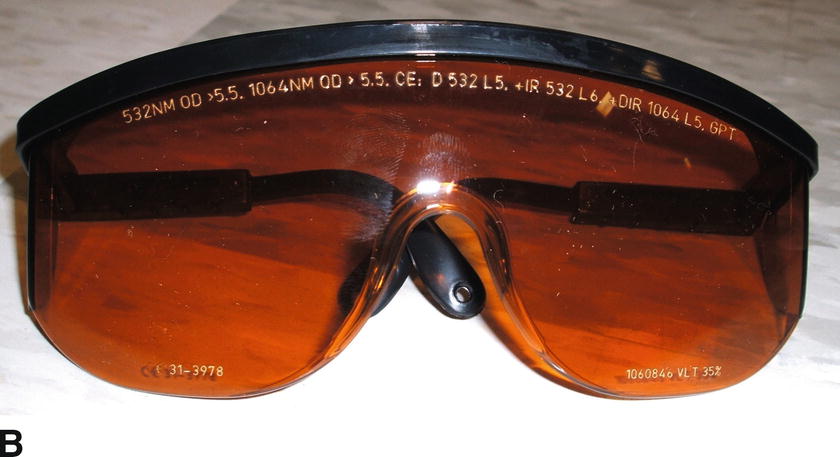
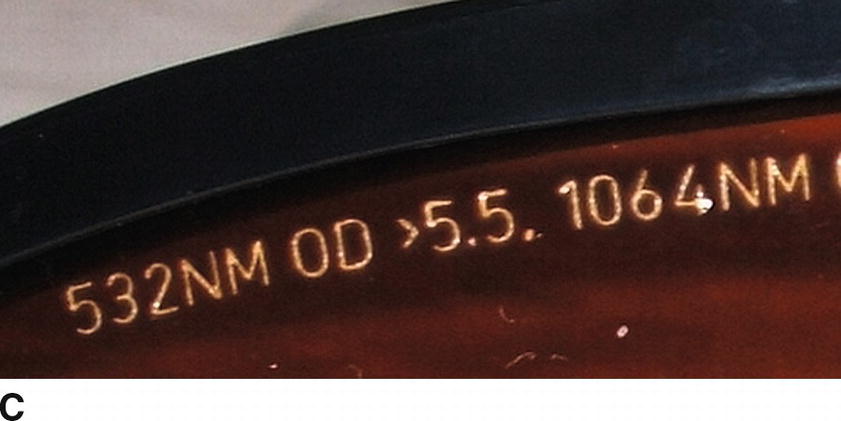
FIGURE 55.7. Laser signs must list the laser type, wavelength, maximum power the unit is capable of emitting, and laser classification. This information suggests hazards and necessary protective measures. Laser eyewear is designed to protect the wearer from laser light of a specific wavelength and therefore a specific laser type. A: This sign is for a KTP type laser, wavelength 532 nm. B: This eyewear is used for a KTP laser with a wavelength of 532 nm. It can also be used with a laser wavelength of 1,064 nm. C: Enlarged view showing the wavelengths of 532 nm and 1,064 nm indicating the two different lasers this eyewear can be used for.
Lasers can also reflect unchanged off shiny mirrorlike surfaces and cause unintended harm. For this reason, most operating room instruments and equipment used during laser surgery are nonreflective with a matte finish to minimize the risk of laser beam reflection. Many of the lasers used in the operating room can penetrate glass, so an opaque covering should be used to completely cover all windows.
Laser eyewear is expensive (costing as much as $1,000 each) and easily damaged. They must be handled carefully to avoid scratches, cracks, and abrasions, which can degrade the quality of protection. Use only optical quality lens wipes to clean the lenses. Appropriate protective eye measures should also be used on all patients undergoing laser surgery. The type of laser as well as how the beam is delivered and the target tissue’s location will determine appropriate protective patient measures. These may include taping the eyes closed, using corneal shields, and/or covering the eyes with wet materials such as gauze or towels.
Air Contamination
Laser surgery can produce a plume of smoke and steam containing small particles and substances that can be a health hazard. Laser plume particulates can be an irritant to the lungs, eyes, and skin and have the potential to transmit infectious agents. The most effective method of protection against inhaling these small particles is to avoid contamination of the operating room atmosphere by evacuating the smoke plume with a vacuum device. Smoke evacuators are designed for this purpose and contain filters that capture particulate as well as gaseous contaminants. Surgical masks cannot filter out all particulate and gaseous contaminants in laser plumes and don’t seal to the face. An N95 respirator mask is recommended if additional protection is desired.
Fire Hazard
Fire in the operating room is life threatening. Fires require an ignition source, a fuel, and an oxidizer (oxygen or nitrous oxide) (the fire triangle, see Chapter 61, Fire). Reducing the risk of fire requires eliminating at least one of the three elements of the fire triangle. Lasers can ignite operating room fires. Since the operating room is filled with flammable objects such as surgical drapes, sponges, foam positioning devices, tapes, ointments, plastic tubing, prep solutions, and polyvinyl chloride (PVC) endotracheal tubes (ETTs), by removing flammable objects (fuels), keeping them wet, or covering them with wet towels or drapes, the risk of ignition by a laser can be reduced. Prep solutions containing alcohol must be thoroughly dry and their fumes dissipated before laser use. Fire risk can also be reduced by decreasing the oxygen concentration, either flowing in ETTs or when using face masks or nasal cannulas (open oxygen sources). Oxygen must not be allowed to collect under the surgical drapes; this is a particular concern during facial surgery under sedation or MAC anesthesia.
Laser surgery performed in or near the airway, or on the face, head, and neck, can be particularly hazardous. The presence of a potentially flammable ETT in the airway combined with an oxygen-enriched atmosphere can be fatal if the ETT is ignited. Therefore, it is critical for the anesthesia provider to keep the oxygen concentration as low as the patient will tolerate, ideally below 30%, while also avoiding the use of nitrous oxide. By increasing the flow of room air to reduce the fractional inspired concentration of oxygen (FiO2), combustion is much less likely to occur. Heliox, a mixture of helium and oxygen that is provided from a tank on the back of the anesthesia machine, can also reduce the risk of combustion. It is provided as a mixture of 70%-80% helium and 20%-30% oxygen and can be combined by the anesthesia provider with a low flow of oxygen to keep the FiO2 below 30% (Fig. 55.8A and B).


FIGURE 55.8. Oxygen and heliox tanks may look very similar. A: An oxygen cylinder with a silver-colored body and a green top. B: This heliox tank is mostly brown but with a green top.
Airway Management during Laser Surgery
Several methods have been devised to allow laser surgery of the face, head, neck, and airway while decreasing the risk of fire. It is important that the anesthesia provider and surgeon collaborate to select the most optimal method of airway management. Techniques for airway management that avoid the use of an ETT altogether are spontaneous ventilation, intermittent apneic oxygenation (IAV), and jet ventilation. Alternatively, specialized laser-resistant ETTs can be used if a secured airway is desired for laser airway surgery.
Spontaneous ventilation is normal, unassisted breathing. IAV involves providing 100% oxygen for short intervals in patients who are not breathing (apneic), usually via an ETT that is removed from the airway during laser use, and put back each time it is necessary to oxygenate the patient; this is convenient during prolonged rigid laryngoscopy when the larynx is continuously in view. Oxygen can also be provided by intermittent mask ventilation. By eliminating the fuel from the airway, both spontaneous ventilation and IAV effectively minimize the risk of an airway fire. These techniques may require general anesthesia to be maintained with intravenous (IV) anesthetic agents since an ETT is not always present to deliver inhaled anesthetics. The patient’s oxygenation must be monitored with pulse oximetry. Issues related to the use of these techniques include difficulty providing adequate oxygenation, hypoventilation with decreased exhalation of CO2 and possible acidosis, and the risk of aspirating gastric contents due to the absence of an ETT to seal the trachea. Depending on the concentration of any supplemental oxygen used, there is still a risk of fire if anything flammable (for instance, facial hair) is near the laser target area.
Jet ventilation, which also requires total intravenous anesthesia, is useful when the surgeon requires a completely unobstructed view of the airway. A high-pressure source of oxygen, often a wall source at 50 psi, is connected via a regulator to a jet ventilation catheter or operating bronchoscope, through which oxygen is delivered at safe pressures of 20-30 psi (Fig. 55.9A). The anesthesia provider intermittently oxygenates by squeezing a handle that enables delivery of high-pressure oxygen. Ventilation is confirmed by visualization of chest wall rise and fall (Fig. 55.9B). Curiously, it is not the jet of oxygen alone that ventilates the patient. The jet creates a rushing stream of gas within the tube of the trachea and bronchoscope, and this rushing stream pulls the room air along beside it at high speed (the Venturi effect). If the jet catheter is too shallow, or too deep, in the airway, it will not pull in enough air. Thus, the jet of oxygen creates ventilation with a mixture of oxygen and room air. A benefit of jet ventilation over spontaneous ventilation or apneic oxygenation is the ability to ventilate continually, with less interruption of the surgical procedure. The risk of an airway fire is essentially eliminated because there is no ETT or oxygen tubing near the airway. Proper positioning of the ventilation port during jet ventilation is crucial in order to avoid complications including pneumothorax, aspiration (due to stomach distention with air), vocal cord or tracheal trauma, and hypercarbia (also called hypercapnia, increased systemic carbon dioxide).
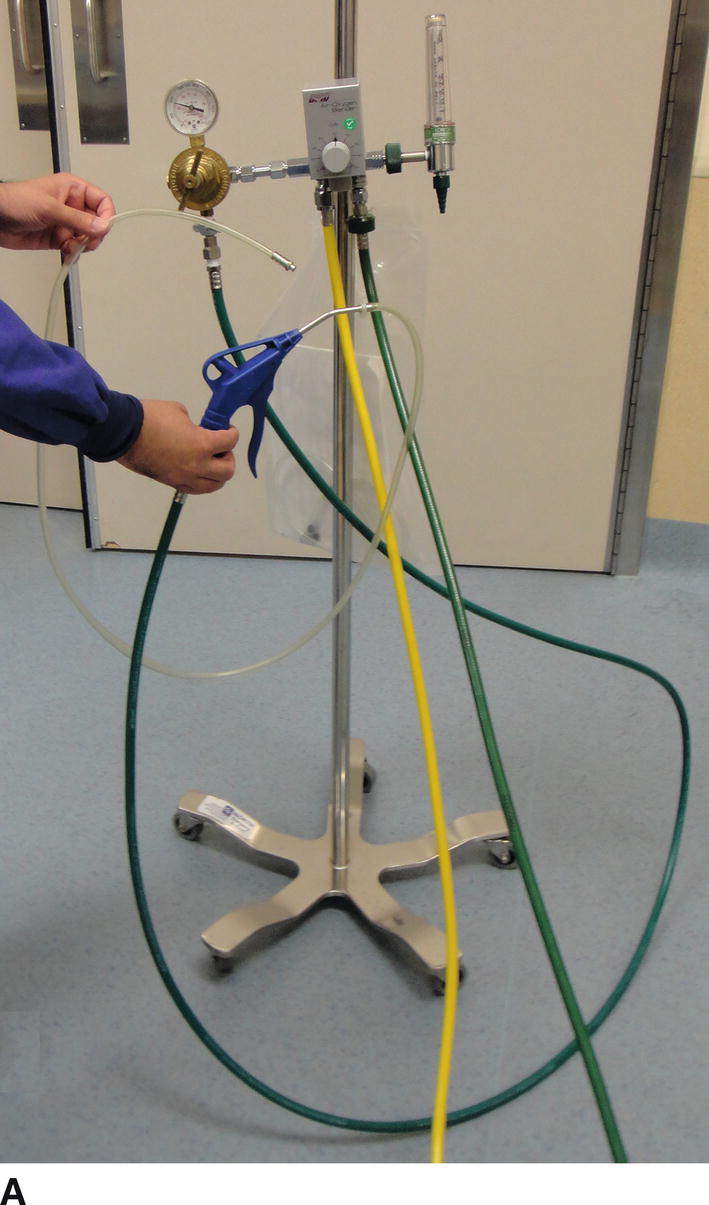
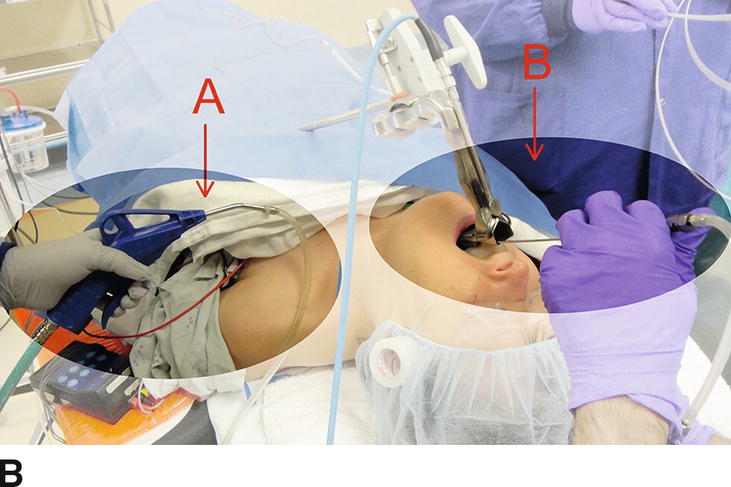
FIGURE 55.9. A: The setup for a jet ventilator. B: A jet ventilator in use. A points to the handle being squeezed to deliver oxygen, and B points to the long nozzle, which directs oxygen into the patient’s airway.
Laser-Resistant ETTs
Conventional PVC ETTs and red rubber ETTs are both ignitable and therefore should not be used during laser surgery involving the airway or nearby structures. Specialized laser-resistant ETTs have been developed for use if a secured airway is required. Each tube is intended for use with a specific laser. It is important to note that laser-resistant ETTs are not laser-proof. When a laser is used near the ETT, especially in the airway, wet packing should be placed by the surgeon to protect the ETT and should be kept moist, and the oxygen concentration should be kept as low as possible.
1. Mallinckrodt Laser-Flex ETT (Mallinckrodt Inc., St. Louis, MO) (Fig. 55.10): The Laser-Flex ETT is a PVC ETT wrapped with a flexible stainless steel coil and has two PVC cuffs. Both cuffs should be filled with water and can be filled with methylene blue to help detect cuff rupture more easily (not included from the manufacturer). The Laser-Flex ETT was designed so that the distal cuff can be inflated if the proximal cuff (closest to the mouth) is ruptured by the laser beam. The Mallinckrodt ETT can only be used with carbon dioxide and KTP lasers. The smallest size cuffed tube is 4.5 mm inner diameter (ID), though the Laser-Flex is also available in 3-, 3.5-, and 4-mm ID uncuffed tubes.
2. Sheridan Laser-Trach ETT (Teleflex, Morrisville, NC) (Fig. 55.11): The Laser-Trach ETT is made with red rubber wrapped in copper foil and is compatible with carbon dioxide and KTP lasers. It is a single-cuff design, and its smallest size available is 4.0-mm ID.
3. Rusch Lasertubus ETT (Teleflex, Morrisville, NC) (Fig. 55.12): The Lasertubus ETT is made from white rubber that is covered with silver foil overlaid for a portion of its length with a Merocel sponge, which should be kept moist. The tube is a dual cuff-within-a-cuff system and its smallest size available is 4.0-mm ID. An advantage of the Lasertubus ETT is that it can be used with many medical lasers including Nd:YAG.
4. Adhesive-wrapped ETTs (Fig. 55.13): The management of pediatric patients may occasionally call for a laser-resistant ETT (either cuffed or without a cuff) with an ID smaller than 4.0 mm. These small sizes are not commercially available. Anesthesia providers can wrap a conventional PVC ETT with metallic adhesive tape; however, this method is not approved by the Food and Drug Administration. During spiral wrapping of the ETT, the tape must be wrapped smoothly and continuously to prevent rough edges, which may abrade tissues, with the adhesive edge facing away from where the laser would be pointing. The edges should overlap sufficiently so that bending of the tube will not expose the PVC. Wrapping a cuffed PVC ETT still leaves the cuff unprotected. Commercially available adhesive tapes include those clad with aluminum foil, copper foil, or with another thin metal coating. Protection can vary depending on the type of metal and the type of laser used. There is also a danger from the metal reflecting the laser beam to nontargeted tissues.
5. Hunsaker Mon-Jet (Fig. 55.14): The Hunsaker Mon-Jet is designed for use in elective jet ventilation procedures. It consists of a distal cage for centering the tube in the airway, a laser-resistant fluoroplastic shaft, and a CO2 sampling line. The jet ventilator is attached to it via a Luer-lock connector. The Mon-Jet can be used with both carbon dioxide and Nd:YAG lasers.

FIGURE 55.10. A Mallinckrodt Laser-Flex ETT (Mallinckrodt Inc., St. Louis, MO). The arrows point to the two fluid-filled cuffs.

FIGURE 55.11. A Sheridan Laser-Trach ETT (Image courtesy of Teleflex Incorporated. Copyright © 2018 Teleflex Incorporated. All rights reserved.).
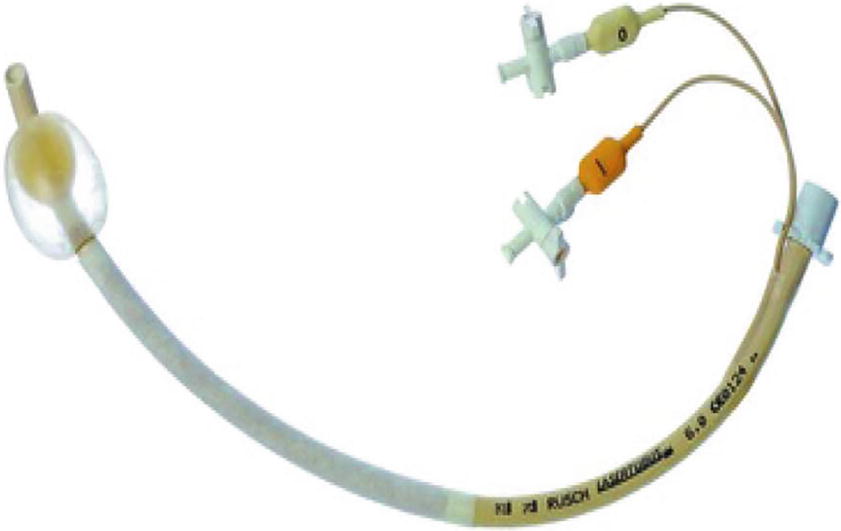
FIGURE 55.12. A Rusch Lasertubus ETT (Image courtesy of Teleflex Incorporated. Copyright © 2018 Teleflex Incorporated. All rights reserved.).
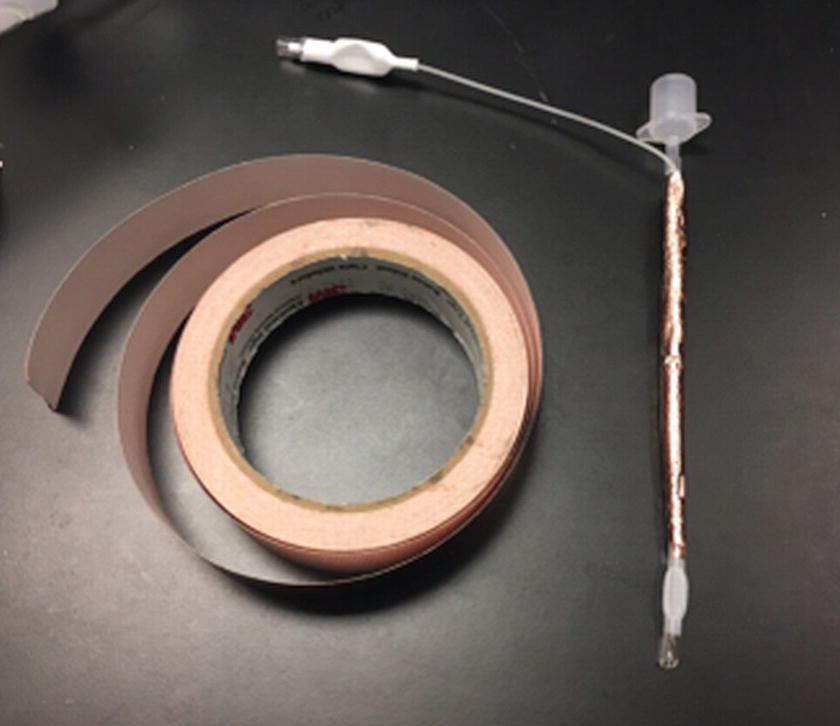
FIGURE 55.13. This is an example of a copper foil–wrapped ETT. Overlapping edges of the copper foil should be smooth. If there is adhesive backing, the tube should be wrapped such that the tape edge faces away from where the laser would be pointing (photograph courtesy of Dr. Kirk Lalwani and Amie Lorisch).
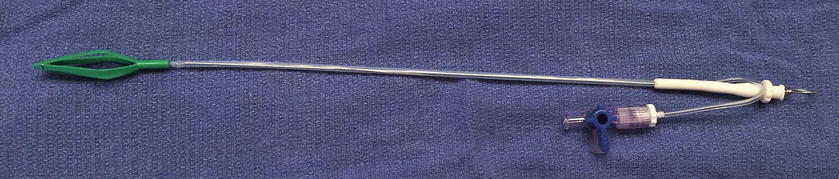
FIGURE 55.14. A Hunsaker Mon-Jet (Medtronic Xomed Inc., Jacksonville, FL) showing the cage and port for CO2 monitoring. (Reproduced with permission of Medtronic, Inc.)
Summary: The Role of the Anesthesia Technologist
Lasers represent an important surgical tool used to treat patients for a variety of disease processes. However, they pose a risk to patients and all members of the surgical team. Anesthesia technologists should understand how lasers work and the risks associated with their use. This enables them to participate effectively in protecting patients, themselves, and other staff from harm, as well as reducing the risk of damage to the equipment being used. When lasers are used, they will be better equipped to support the anesthesia provider, identify risks, and reduce the likelihood that an adverse event occurs.
Communication and preplanning are essential before and during procedures involving lasers. Knowing the type of procedure and the laser to be used can help to prepare for its use and assist in determining what safety precautions will help to prevent possible injury (Table 55.2). It is important to be familiar with department protocols and policies regarding laser use and airway management in the OR. Particularly in laser airway surgery, anesthesia technician planning, assistance, and safety awareness are critical. The AT can assist by supplying appropriate airway management supplies such as laser-resistant ETTs, setting up necessary equipment such as the jet ventilator, and ensuring the heliox tank is adequately filled. They may need to provide proper eyewear for themselves and the anesthesia provider and help make sure appropriate laser protection is provided for the patient. The technician can assist the anesthesia provider with measures to reduce oxygen concentrations when there is risk of oxygen buildup under surgical drapes, such as using suction tubing to remove excess oxygen or deliver air to dilute. Importantly, the technician, just like any member of the operating room staff, should be willing to question any practices that seem unsafe. This aspect of team safety will be extensively covered in the next chapter, Simulation and Crisis Resource Management.
Table 55.2. Anesthesia Laser Safety Considerations
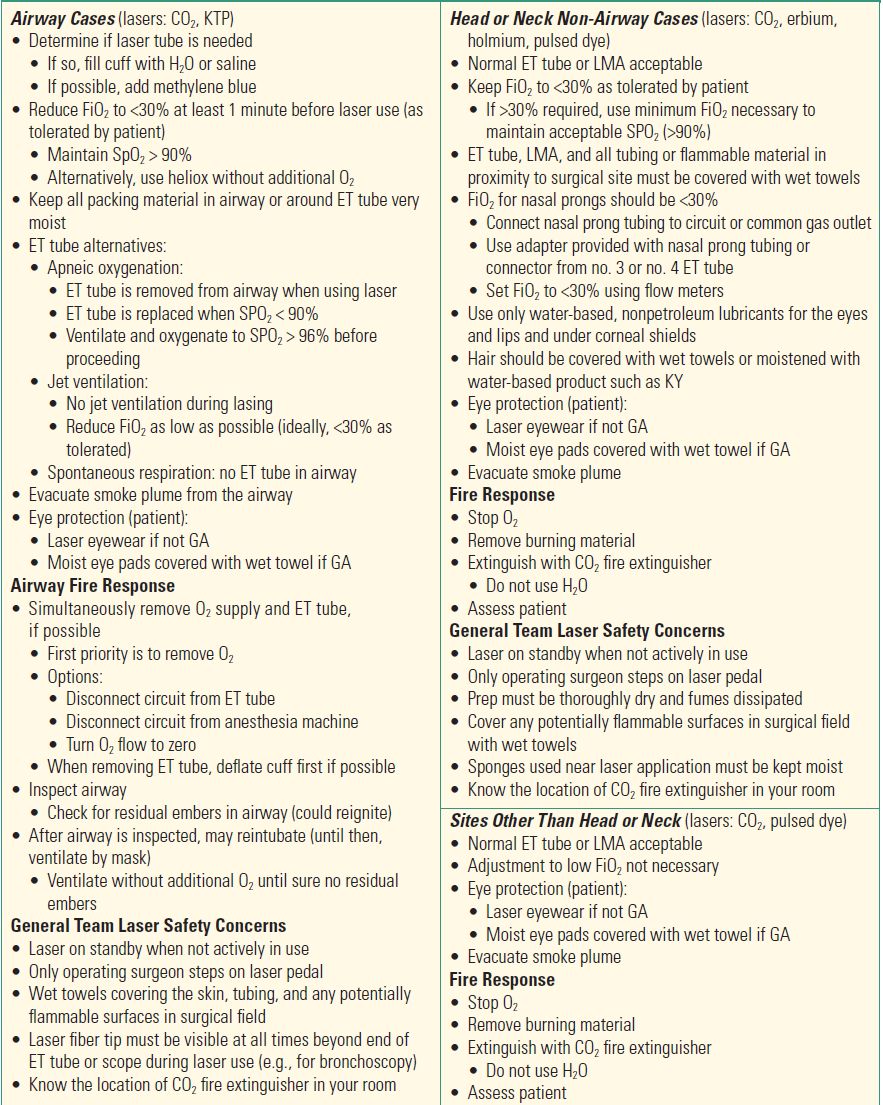
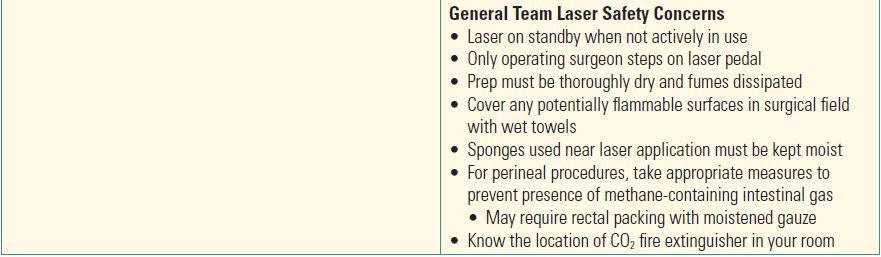
Suggested safety considerations for intraoperative use of some common lasers.
Should an adverse event occur, be prepared to provide support, for example, by knowing the response to an operating room or airway fire (see Chapter 61, Fire).
Review Questions
1. Nonintubating techniques available for laser surgery of the airway that remove the fire potential of an ETT include all EXCEPT
A) Apneic oxygenation
B) Spontaneous ventilation
C) Venturi jet ventilation
D) Laryngeal mask airway (LMA™)
E) None of the above
Answer: D
Apneic oxygenation, spontaneous ventilation, and Venturi jet ventilation represent available nonintubating techniques for laser surgery of the airway. They minimize the risk of fire during laser surgery of the airway while allowing direct visualization of the airway. Although a laryngeal mask airway can be used as an alternative to endotracheal intubation, it does not allow direct visualization of the airway due to its position in the oropharynx.
2. A fire in the operating room requires three components:
A) Match, plastic, and oxidizer
B) Ignition source, plastic, and nitrous oxide
C) Fuel, nitrous oxide, and explosives
D) Fuel, oxidizer, and ignition source
E) Oxidizer, ignition source, and helium
Answer: D
A fire requires three essential components: fuel, an oxidizer, and an ignition source. Lasers may act as an ignition source during laser surgery, and safety measures must be taken to minimize the risk of an operating room fire by eliminating fuel sources or oxidizers. These safety measures include the use of nonflammable objects near the treatment site and the attempt to minimize the use of supplemental oxygen during laser surgery of the neck, head, and face.
3. Risks associated with jet ventilation include
A) Eye injury
B) Burns
C) Aspiration of gastric contents
D) Infection
E) Pain
Answer: C
Jet ventilation is a nonintubating technique used for laser airway surgery when the surgeon wants a completely unobstructed view of the airway. Due to the high-pressure oxygen used to ventilate the patient, a risk of the procedure includes aspiration of gastric contents since the stomach may be inadvertently distended with air.
4. A laser beam of energy can be all of the following EXCEPT
A) Invisible
B) Multicolored
C) A single color
D) Derived from an active medium (solid, liquid, or gas)
E) Travel through a substance without affecting the substance at all
Answer: B
Each laser type emits a specific wavelength producing one color (only if the wavelength falls in the visible spectrum). A laser can also be in the invisible portion of the light spectrum. Lasers can be produced from a variety of active mediums (solids, liquids, or gases) and can travel through some substances without affecting them. If the substance absorbs the light energy, heat can be produced, which can affect the substance.
5. Benefits of laser over other surgical techniques include all EXCEPT
A) Decreased pain
B) Expense
C) Decreased swelling
D) Decreased bleeding
E) Ability to target difficult-to-reach regions of the body
Answer: B
Lasers used in surgical procedures offer several unique advantages over traditional surgical methods. A laser is capable of targeting a specific layer of tissue and can often target difficult-to-reach regions of the body. Since a laser beam does not diverge as it travels over a distance, it can treat a precise target while often sparing the surrounding tissue of edema and pain. Lasers are also associated with decreased amounts of bleeding due to their ability to clot off small blood vessels. Unfortunately, lasers can be quite costly to use.
6. What three components are required to create a laser?
A) Power source, mirrors, and a fiber
B) Active medium, mirrors, and a fiber
C) Power source, concentrator, and mirrors
D) Power source, active medium, and mirrors
Answer: D
A laser is produced by energizing an active medium with a power source. Mirrors then channel and amplify the energy produced into the emitted light.
SUGGESTED READINGS
Ehrenwerth J, Seifert HA. Electrical and fire safety. In: Ehrenwerth J, Eisenkraft JB, Berry JM, eds. Anesthesia Equipment: Principles and Applications. 2nd ed. Philadelphia, PA: Elsevier Saunders; 2013:621-652.
Hermens JM, Bennett MJ, Hirschmann CA. Anesthesia for laser surgery. Anesth Analg. 1983;62:218-229.
Rampil IJ. Anesthetic considerations for laser surgery. Anesth Analg. 1992;74:424-435.
Sheinbein DS, Loeb RG. Laser surgery and fire hazards in ear, nose, and throat surgeries. Anesthesiol Clin. 2010;28:485-496.
Sosis M. Anesthesia for laser surgery. J Voice. 1989;3: 163-174.