 Sip water often. A healthy mouth needs to be hydrated.
Sip water often. A healthy mouth needs to be hydrated.with Bethany O’Dell
Dental and oral health is not likely the first thing you think of when you think about men’s health. Nor has dental health been one of the National Institutes of Health’s priorities. If there was a report card for each dimension of men’s health (e.g., heart, diabetes, hearing), dental health would certainly receive a low “grade” for most men’s preventative efforts. Part of this too-close-to-failing grade reflects our individual efforts. Yet being able to afford to maintain the health of the mouth reveals the inequalities among men more than nearly any other type of health issue. We examine in this chapter the importance of oral health to a man’s physical and social function, the most common dental diseases and their treatment, and the stark generational and socioeconomic differences evident in men’s dental health.
“I think, therefore I am” is the statement of an intellectual who underrates toothaches.
—Milan Kundera
A lot of media attention was drawn to the fact that more than 50 million Americans were without health insurance before the Affordable Care Act became law in 2010. Despite the historic health care reform legislation, the alarming fact is that about 40 percent of adults under age 65 in the United States will remain without a dental plan and affordable access to dental care. Don’t think that older adults are better off. Once retired, 80 percent of older men are without dental insurance.1 You probably did not know that most dentists do not participate in Medicaid, and Medicare does not offer dental coverage.2 This leaves tens of millions of adult men unable to afford the essential dental health care they need because they may not be able to pay out of pocket and/or cannot find a provider who will treat them at reduced cost.3
As with general health, oral health tends to vary based on social factors, resulting in what amounts to “a silent epidemic” of dental and oral diseases for certain men.4 As an example, men from different generations vary significantly in their experiences with, attitudes toward, and expectations of dental health and dental care. Many men born in the 1930s and early 1940s already suffered from poor dental health by the time they reached voting age. Nearly 45 percent of these men have lost six or more teeth due to tooth decay or gum disease before age 65, and 20 percent have lost all of their teeth (and are called “edentulous,” meaning without any natural teeth).5 Part of the explanation for this is because preventative and restorative dental care wasn’t readily available until military service in World War II. The older generations did not visit dentists to improve their dental health; rather, extraction of a loose or decayed tooth was the usual “treatment.” They also feared the dentist;6 pain control had not yet been introduced when they were young. As one older man commented, “The injections they have today weren’t there when we were young.”7 Further, this World War II / Korean War generation had not benefitted from water fluoridation or fluoride toothpastes, and it was the economically deprived men within this generation who ended up with the greatest number of pulled and missing teeth.8
For the baby boomer generation, the common view held by their fathers that losing teeth is a normal part of aging is no longer acceptable. Boomers’ dental health education included television advertising when they were children which emphasized “brush, brush, brush” and encouraged regular dental checkups. Most boomers have some form of dental insurance. Owing to early self-care and preventive dental care, the boomer generation did not expect to lose teeth or endure painful dental infections. Many boomers retain their own teeth throughout their lives or have implants and/or caps to provide a full mouth of teeth. They have learned that the best thing they can do to avoid complicated and expensive dental work is to engage in regular dental visits, cleanings, and fixing small problems before they become big ones.
What does “dental health” mean to men? For the older generation, the concept meant having enough teeth to chew and speak.9 However, for boomers and younger men, they’ve learned that dental and oral health is important; they know that oral infections can lead to other health problems, and they’ve learned that periodontal (gum) disease contributes to stinky breath, lost teeth, and problems chewing, as well as doubling the risk of men suffering a fatal heart attack and tripling the risk of a stroke.10
Men also know that their teeth affect their well-being and social lives. The mouth is highly visible, and having missing teeth interferes with a person’s speech, perception of himself, and social standing. Having visibly missing teeth and/or bad breath might stigmatize, given the increasing importance the boomer generation has placed on appearance. White, evenly shaped and straight teeth and quality of breath are criteria people use to make judgments about a man and can affect his ability to find (or keep) a good job. A spokesperson for the Academy of General Dentistry recently reported, “Many (men) have noticed the positive effects of a colleague’s improved smile and … [how] a great smile has a lot of value in the business world.”11
This chapter is titled “Dental and Oral Health” and not “Dental Problems” for good reason. Dental diseases are more often lifestyle diseases, no different from how smoking-related lung cancer is a lifestyle disease. Toothbrushes and flossing have replaced “chew sticks” and herbs, and studies show that most men are taking up other self-care practices.
The key word is most men. Researchers continue to find that men follow oral hygiene recommendations less conscientiously and draw upon less dental care than do their sisters and wives. Studies by the American Dental Association (ADA) have noted that barely half of men brush their teeth twice a day, much fewer floss daily, and more than half develop periodontal (gum) disease and will lose at least five teeth by their early seventies. Even when men actively engage in dental self-care at home, too few see a dentist or dental hygienist annually, and many live with undiagnosed problems.12 Not every oral health problem is visible or results in the pain or discomfort that compels most men to seek dental care. Too many serious dental and oral problems are “silent.”
Brushing twice a day with a fluoride toothpaste, flossing daily, and regular dental checkups are the key factors in maintaining a healthy mouth and avoiding dental problems. The mouth includes more than the teeth and the gums (gingiva). There are the jaw bones and ligaments, the hard and soft palate, the soft tissue lining the mouth and throat, the tongue, the lips, the salivary glands, and the chewing muscles.
Men who smoke or chew tobacco are putting at risk not only their overall health but the health of their mouths as well. Cigars are not a safe alternative. Smokers are at increased risk for tooth abrasion from the grit in smoke, tooth discoloration (or staining of the teeth), hastened periodontal disease due to irritation of the gums, and the bad breath that comes from oral disease. Smokers routinely take longer to heal an oral wound, whether from an ordinary cut or following oral surgery.
Statistics show that chewing tobacco and snuff are less dangerous than cigarettes, but the smokeless products still raise the risk of oral cancer by 80 percent. The most frequent oral cancer sites are the tongue, floor of the mouth, soft palate, lips, and gums. It is very important for men who use tobacco to see a dentist frequently, not merely for cleanings but for an assessment of signs of an oral cancer. Most men do not recognize that when a dentist or hygienist begins your visit with a thorough look at your mouth, they are screening for oral cancer.
It is important to control the growth of bacteria on the teeth, gums, and tongue. Removing the food particles from your mouth by brushing (or at least rinsing) as soon as possible prevents the development of bacteria, which cause bad breath, cavities, and other infections. First, drink plenty of water throughout the day. Water cleanses the mouth and removes food particles and bacteria that cause bad breath or other tooth and gum issues. Second, brushing your teeth and flossing are equal halves of the job of keeping a clean mouth, yet dentists report that most of their patients are not willing to floss. Fewer than 13 percent of the men in a recent study reported that they flossed daily.13 Even though it may seem like a bother until you make it a habit, if you take just a minute to floss your teeth on a daily basis, you will be helping to prevent plaque and tartar buildup, gingivitis, and periodontal disease. Although not a substitute for flossing, an oral irrigator or water pick can help clean between teeth.
Equally important is a visit to the dentist two times a year for a professional cleaning. The cleaning will more than whiten your teeth; the hygienist removes the plaque from those hard-to-reach places your toothbrush didn’t find. The dentist or hygienist will also be able to tell you how healthy your mouth is and what to do to improve your dental health.
These simple steps are the easiest way to keep control of your dental health. Much like the way flossing emerged as an added, valuable means of oral hygiene, dental professionals also recommend that we invest in an electric toothbrush and, if you need it, a tongue cleaner. The tongue tends to acquire a lot of bacteria, which is the main cause of bad breath, and cleaning your tongue will remove bacteria buildup that a brushing couldn’t get off. An electric toothbrush does a much better job brushing, is a good tongue massager, and makes it much easier to position the brush at the recommended 90-degree angle to clean the spaces where the gums and teeth meet. You are also more likely to brush your teeth longer and better clean the areas where gums and teeth meet.
Things Dentists Want Us to Know
• Use a soft-bristled toothbrush and reach every surface of each tooth.
• Brush your teeth and gums with fluoride toothpaste for 2–3 minutes each brushing. Choosing toothpaste with fluoride reduces tooth decay by as much as 40 percent.
• Brush your gums by positioning the toothbrush at a 45 degree angle where your gums and teeth meet.
• Change your toothbrush every 3 months. The bristles wear out.
• Rinse the toothbrush out with hot water after every use to help remove bacteria that collects in the bristles.
• Floss by using a back-and-forth motion, and curve the floss into a C shape against one tooth and then the other.
• Dental checkups and cleanings routinely screen for oral cancer.
• Men who smoke have a much greater risk of gum disease and oral cancer.
• Eating a nutritional diet with little sugar prevents periodontal disease and tooth decay.
• Bad breath is usually evidence of a dental problem, and mouthwash only hides the problem temporarily.
• Dental problems do not go away untreated.
• Fear of pain from dental work is something to be discussed with your dentist and hygienist. Dental work can be made painless.
• Should you need it, choose the root canal, not a pulled tooth.
Sources: Academy of General Dentistry and the American Dental Association.
The food we consume is directly associated with how healthy our mouths are. By having a meal plan of whole grains (breads, cereals), protein (fish, meat, beans), and dairy (milk, yogurt, cheese), we are giving our body the nutrients needed to maintain a healthy mouth. In contrast, practicing poor eating habits such as constant snacking, sipping on sodas, or even not eating at all will seriously harm your teeth and mouth. Constant snacking is detrimental simply because there are food particles being left on the surfaces of the teeth. The leftover food particles are fertilizer for bacteria. Drinking soda, even sugar-free soda, is equally harmful because the acid within the soda destroys the tooth’s enamel. A sugary diet, especially one that includes bakery products and carbonated drinks, increases dental problems.
The worst thing for your teeth, however, would be to not eat much at all. It is critical that our body get food and needed nutrients. You can lower your risk for cavities, gum infections, losing teeth, and periodontal disease by simply getting an adequate amount of vitamin D and calcium into your body. Researchers have found that people who have a deficit in vitamin D and calcium are more likely to develop osteoporosis and tooth loss.14 These two vitamins are essential for maintaining good bone to anchor the teeth and promoting overall oral health.
Vitamin D helps the body absorb the correct amounts of calcium and utilize it efficiently. Without enough vitamin D, the available calcium isn’t absorbed, and the body then starts to take calcium away from teeth and bones.15 Many adults, particularly men age 60 and older, have dietary intakes of calcium well below recommended levels.16 Adult men are recommended to have 1,000–1,500 IU of vitamin D daily (or 10–15 micrograms). Sunshine and certain foods and drinks, such as milk, orange juice, cheese, eggs with the yolk, and salmon, have good amounts of vitamin D. Because many men spend too little time in the sun (with sunscreen) and no longer consume enough of these sources, vitamin D supplements are encouraged. A year’s supply of a generic brand will cost little more than a case of beer. Men also need 1,000–1,500 mg of calcium daily in order to check the risk of bone loss and tooth loss. This level can be obtained by dietary intake or, if need be, from supplements. Dairy foods, bread, broccoli, and orange juice have large amounts of calcium. Low-fat and fat-free milk and dairy products (yogurt, cheeses) are especially good sources of both calcium and vitamin D.
Have you ever woken up feeling parched, as if you’ve traveled the desert without water for days? You probably spent the night breathing through your mouth, perhaps as a result of chapped lips or congestion from a head cold, or you drank way too much alcohol the night before and woke dehydrated. Without adequate salivary flow on a regular basis, we are much more at risk of early oral health problems.
Good mouth care means keeping the mouth moist, and it is saliva (not gulping bottled water) that is the key ingredient to keeping your mouth healthy. Saliva contains antibacterial proteins, mucins (mucous), and ions that prevent oral infections and dental cavities. It helps neutralize acids from our stomachs, which protects our esophagus, and is vital to our ability to chew, swallow, and talk comfortably throughout the day.
The mucous layer in saliva that covers our teeth acts as a shield, protecting the teeth from decay, and fights the bacteria that cause gum disease. For men who have dentures, saliva is equally vital to help keep the dentures comfortable and fitting in the mouth. The recommendation is to stimulate saliva production by chewing sugarless gum (especially xylitol gum), sucking on a sugarless gum ball, or eating foods that require chewing, such as apples, carrots, celery, and hard bread.
Many medications, such as heart or blood pressure medications or antide-pressants, reduce the natural production of saliva and cause dry mouth. Men who take saliva-inhibiting medications are at increased risk for cavities, periodontal disease, and other oral problems. Often the medications that are muscle relaxants, pain inhibitors, or sleeping aids (sedatives) or those that treat diabetes, allergies, colds (e.g., antihistamines), diarrhea, nausea, and hypertension (e.g., diuretics) will increase the risk of oral health problems.
Anatomy of a Tooth
A tooth is composed of several layers. The outermost layer, above the gum line, is called the enamel, and this is the hardest substance in the body. Beneath the gum line, a substance called cementum covers the tooth roots. Under the enamel and cementum is the dentin. The dentin is about as hard as bone, and it is the dentin that contains nerve endings. Beneath the dentin is the vascular tissue called the dental pulp.
Healthy teeth are clean and have few cavities, healthy gums are pink and firm, and a healthy mouth is a window offering clues about your body’s overall health. The enemy is bacteria. Plaque is a soft, colorless film of bacteria constantly forming on your teeth. It combines with sugar and other carbohydrates to form acids. Without brushing and flossing, the acids eat right through tooth enamel to cause cavities, and the plaque hardens into a porous, coarse tartar. The acids produced by the bacteria will cause your gums to become chronically infected (or inflamed), and the gum tissue next to the teeth breaks down and separates from the teeth. Plaque begins to accumulate on your teeth 20 minutes after eating, and if it isn’t removed, you are at greater risk of tooth decay or gum inflammation. Together, plaque and tartar lead to a number of problems: gingivitis, periodontitis, bad breath (halitosis), tooth loss, and cavities. Before each of these dental problems is briefly reviewed, we discuss two other common problems: dry mouth and taste problems.
Adult men often suffer from dry mouth (known as xerostomia), especially as we get older. It is perhaps one of the most underappreciated, underdiagnosed, and undermanaged oral health conditions.17 Dry mouth happens when the salivary glands are not working properly, resulting in decreased saliva production. Because saliva is the moisture that helps you talk, swallow, and digest your food, the sensation of dry mouth needs to be taken seriously. The amount of salivary tissue in the mouth decreases with aging, but it isn’t physiological aging that causes dry mouth.18 Rather, it is the prescription medications we are taking and/or the underlying medical conditions we have.
The uncomfortable, dry feeling can be a temporary problem or a chronic one. Your dry mouth may have started shortly after starting a new prescription or over-the-counter medication; dry mouth is a side effect of many medications, but especially the diuretics used to manage hypertension and the over-the-counter medications used for allergies and antidepressants. Two decades ago there were over 400 medications known to negatively affect salivary function.19 Given that 50 percent of the adult male population in the United States is on at least one medication, most men will experience some change in how their salivary glands work.20 The advice “Know your medications” is essential. Other times, it is the disease itself that decreases saliva functioning—diabetes, Parkinson’s and Alzheimer’s diseases, or more likely sleep apnea. Recent studies show that sleep-disordered breathing and snoring contribute to chronic dry mouth. Finally, radiation therapy and chemotherapy can cause damage to the salivary glands or make saliva thicker than normal.
There are plenty of ways to relieve the uncomfortable sensation of dry mouth. The absolute worst method is by sucking on sugared candies or lozenges. The key advice is to not ignore the problem and bring it to the attention of both your physician and dentist. If you are using medication and experiencing the discomfort of dry mouth, take control and ask your physician if there is an alternative medication. Below are a few tips to prevent dry mouth (at night) or help make your mouth a little more comfortable:
 Sip water often. A healthy mouth needs to be hydrated.
Sip water often. A healthy mouth needs to be hydrated.
 Sip water at meals as well. This will help with the process of chewing and swallowing and circumvent the problem of dry mouth caused by illness or medical treatment.
Sip water at meals as well. This will help with the process of chewing and swallowing and circumvent the problem of dry mouth caused by illness or medical treatment.
 Just like sugar, caffeine can dry out the mouth. Put down that soda, and watch how much coffee or tea you drink.
Just like sugar, caffeine can dry out the mouth. Put down that soda, and watch how much coffee or tea you drink.
 Keep sugarless gum or sugarless hard candy in your pocket. Chewing and sucking help to stimulate saliva flow in your mouth. Lemon and tart flavored are best to stimulate saliva.
Keep sugarless gum or sugarless hard candy in your pocket. Chewing and sucking help to stimulate saliva flow in your mouth. Lemon and tart flavored are best to stimulate saliva.
 At night use a nasal strip to reduce snoring and sleeping with your mouth open. Snoring is a leading cause of experiencing dry mouth at night.
At night use a nasal strip to reduce snoring and sleeping with your mouth open. Snoring is a leading cause of experiencing dry mouth at night.
 If you mostly sleep with your mouth open and breathe through your mouth at night, it is a good idea to run a humidifier in the room to keep moisture in the air.
If you mostly sleep with your mouth open and breathe through your mouth at night, it is a good idea to run a humidifier in the room to keep moisture in the air.
 Ask a dentist about oral moisturizers and gels that are designed to provide relief from dry mouth.
Ask a dentist about oral moisturizers and gels that are designed to provide relief from dry mouth.
Humans’ taste palate falls into five basic groups: sweet, bitter, sour, salty, and umami (a Japanese word for “good” flavor, or savoriness). An anatomy professor would tell you that your sweet/salty taste buds are located near the front of your tongue, whereas the sour and bitter taste buds line the sides and very back of your tongue (see figure 17.1). As we age, our sense of taste changes, and this is going to be certainly noticed by the baby boomer generation, which has grown up with sugars and salt. The order of “lost taste” begins with sweet and salty eroding first and sour last. Because 75 percent of what we “taste” actually comes from our sense of smell, and because the olfactory bulb in the brain responsible for processing smell becomes smaller as we age, both smell and taste become more blunted.
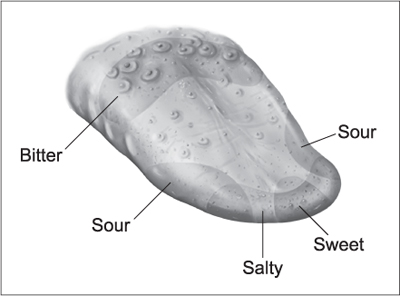
Figure 17.1. Tongue and taste regions. Illustration by Carlyn Iverson.
Aroma is what enhances our ability to taste our food, so when our sense of smell is decreased, many of us find that our food is bland. If your diet has long had a lot of salt (or sodium), as you get older you probably think whatever you are eating “needs a little more salt.” It doesn’t; you just think it does. Changes in tastes not only reduce the pleasure and comfort from food; they represent risks for nutritional deficiencies and challenge our willingness to adhere to a healthy diet. Don’t pick up the salt shaker.
When food seems to have lost that taste that we enjoyed so much and sometimes crave, this can lead to a loss of appetite and a slow decrease in an older man’s food intake, which eventually will make him more vulnerable to illnesses because of his lack of vitamins and nutrients. Alternatively, he might begin salting or sugaring up his food in order to get that flavor back, which puts him at further risk of obesity and hypertension.
We can be thankful that taste is one of the best senses we have and is not affected as drastically by aging as our other senses. Actual taste disorders are very rare, but over time we usually experience a gradual decrease in our ability to taste salty, sweet, sour/bitter, and pleasurable things such as the texture of chocolate, the hops in beer, or the zing in pepper-flavored Chinese food. Similar to dry mouth, our “loss of taste” is often caused by outside (exogenous) sources, not just aging. It might actually be caused by medicines you’re taking, since both prescription and over-the-counter medications (including herbs) are chemicals that change your sense of taste. Many antibiotics and blood pressure pills can cause an unpleasant taste in our mouths. Viral infections—especially sinus infections and head colds—dull the sense of smell and then taste, and the problem can be chronic. Smoking damages the soft tissue inside the mouth and dulls the palate, as well as our sense of smell.
What can you do? First, check with your physician and/or dentist to see whether you are on any medications that alter smell and taste and, if so, whether the medication can be changed. Also, practice good oral hygiene to prevent gum disease and to retain your teeth. If you have a loss of appetite because food doesn’t taste like you want it to, try to make your food appealing to the eye by using different colors and textures, or add herbs and spices instead of salt and sugar to provide a newer range of flavors.
Having bad breath is a dreadful, often embarrassing situation, if you know you have it. It is virtually impossible for people to find out if their own bad breath is an affront, simply because we become used to our odors and do not perceive whether our breath offends. Blowing into your hands and smelling your breath doesn’t give you reliable feedback. That breath is from the lungs, whereas bad breath comes from the back of the mouth and is exhaled when we talk or sigh.
Bad breath is a common symptom of periodontal disease (discussed below) and can occur as a result of xerostomia. The primary cause is a dental problem, so don’t rely on mouthwash or a breath freshener to “fix” your bad breath. They only mask the odor for a few minutes. A mouthwash kills some of the bacteria, but within a short time the remaining bacteria begin to multiply in an unrelenting, hard-hitting manner. Bad breath happens whenever the millions of bacteria in our mouths digest protein particles, which then produces sulfur gases.
Having a dry mouth sharply increases the chance of bad breath because the saliva that cleanses the mouth isn’t in sufficient quantity. If you slept with your mouth open, your mouth has dried out. That dry environment is a perfect breeding ground for the anaerobic sulfur-producing bacteria that cause the morning’s dragon breath. Whenever bad breath is caused by dry mouth, it stems from the back of the tongue, where there is too little saliva to cleanse that area. Typically, men age 65 or older will have to work a little harder to conquer their midday or continuous bad breath, since we have a higher probably of developing xerostomia as we age. Recall that it isn’t aging itself that triggers the dry mouth and bad breath; it is most likely one of the medications you use. Your physician would know if there is an alternative medication that doesn’t cause dry mouth as a side effect.
When that morning breath doesn’t go away after brushing or when bad breath becomes an all-day fellow traveler, it is most likely a sign of gingivitis or periodontal disease. As troubling as the foul breath is, it is also a clear message to see a dentist and begin trying to manage the gum disease.
There are a number of easy things you can do to decrease the presence of bad breath while you and your dentist work to improve your overall dental health:
 Quick fixes: eat an orange, chew a handful of mini carrots, or eat an apple. Both the saliva flow caused by chewing and the coating these foods provide help cleanse the mouth.
Quick fixes: eat an orange, chew a handful of mini carrots, or eat an apple. Both the saliva flow caused by chewing and the coating these foods provide help cleanse the mouth.
 Eat yogurt (at least 6 ounces a day). Unsweetened yogurt contains two common bacteria called streptococcus thermophilus and lactobacillus bulgaricus. These bacteria battle the stink-causing bacteria; like a shield, the yogurt coats the mouth with the good bacteria to help prevent new stink-causing bacteria from forming.
Eat yogurt (at least 6 ounces a day). Unsweetened yogurt contains two common bacteria called streptococcus thermophilus and lactobacillus bulgaricus. These bacteria battle the stink-causing bacteria; like a shield, the yogurt coats the mouth with the good bacteria to help prevent new stink-causing bacteria from forming.
 Chew sugarless, xylitol, or an antimicrobial gum. Chewing gum stimulates saliva flow, and it is the saliva that acts as a natural mouthwash, cleansing the teeth of bacteria. An antibacterial chewing gum can kill harmful mouth bacteria, such as the streptococcus mutants. There are different antimicrobial “agents” (additives to the gum), and several are digestible, benefiting the whole body.
Chew sugarless, xylitol, or an antimicrobial gum. Chewing gum stimulates saliva flow, and it is the saliva that acts as a natural mouthwash, cleansing the teeth of bacteria. An antibacterial chewing gum can kill harmful mouth bacteria, such as the streptococcus mutants. There are different antimicrobial “agents” (additives to the gum), and several are digestible, benefiting the whole body.
 Use peppermint oil. Because of its antiseptic properties, it can remove bad breath temporarily. Put a few drops in a glass of water and rinse before you have a social event or face-to-face meeting. It’s no wonder that peppermint is added to many toothpastes and chewing gum.
Use peppermint oil. Because of its antiseptic properties, it can remove bad breath temporarily. Put a few drops in a glass of water and rinse before you have a social event or face-to-face meeting. It’s no wonder that peppermint is added to many toothpastes and chewing gum.
 Don’t skip breakfast. Chewing food in the morning not only is nutritious but gets the saliva flowing. Do brush afterward to remove the microscopic particles of food that could become fertilizer for bacteria growth.
Don’t skip breakfast. Chewing food in the morning not only is nutritious but gets the saliva flowing. Do brush afterward to remove the microscopic particles of food that could become fertilizer for bacteria growth.
 Brush the tongue. This is one of the easiest ways to fight halitosis, since it is the tongue surface that hosts millions of bacteria. Alternatively, have a tongue scraper handy and use once or twice a day to remove the layer of mucus on the top of the tongue, particularly toward the back. Don’t let your tongue become a dirty carpet.
Brush the tongue. This is one of the easiest ways to fight halitosis, since it is the tongue surface that hosts millions of bacteria. Alternatively, have a tongue scraper handy and use once or twice a day to remove the layer of mucus on the top of the tongue, particularly toward the back. Don’t let your tongue become a dirty carpet.
 Use a natural oil toothpaste that contains fluoride. Even though you probably grew up using a minty toothpaste that left you feeling like you had a fresh mouth, mint has actually the least strength to mask bad breath. Many natural oils and herbs found across the world are concentrated within natural toothpastes and protect teeth, heal gums, and provide extended mouthwash-type freshness. However, ensure that your toothpaste has the ADA seal of approval and still contains fluoride.
Use a natural oil toothpaste that contains fluoride. Even though you probably grew up using a minty toothpaste that left you feeling like you had a fresh mouth, mint has actually the least strength to mask bad breath. Many natural oils and herbs found across the world are concentrated within natural toothpastes and protect teeth, heal gums, and provide extended mouthwash-type freshness. However, ensure that your toothpaste has the ADA seal of approval and still contains fluoride.
 It’s not “girly” to use a straw. A straw can send sugary or sticky liquids past the teeth and tongue so they don’t stay in the mouth and become home for bacteria.
It’s not “girly” to use a straw. A straw can send sugary or sticky liquids past the teeth and tongue so they don’t stay in the mouth and become home for bacteria.
 Consuming plenty of water keeps your mouth moist and reduces the acidity of your mouth, creating a less friendly environment for bacteria.
Consuming plenty of water keeps your mouth moist and reduces the acidity of your mouth, creating a less friendly environment for bacteria.
When the protective gum tissue around your teeth pulls away from the crown and moves downward toward the root, this is called gingival recession. Many times, we have no control over whether or not our gum tissue will recede; people who take care of their mouths on a daily basis may still experience this as they get older. One culprit is genetics. Because some people are born with teeth that crowd one another or with thin layers of gingival tissue, their gum tissue will most likely recede with time.
But there are causes of receding gum tissue that we are in control of. This includes harsh brushing of the gums, which can lead to their deterioration. It is important to be gentle with your gums, change your toothbrush regularly, and floss on a daily basis in order to combat the potential receding of gingival tissue. Another common cause is inadequate oral hygiene, which eventually results in periodontal disease. If you are noticing that your gums are not where they used to be, notify your dentist to plan treatment options.
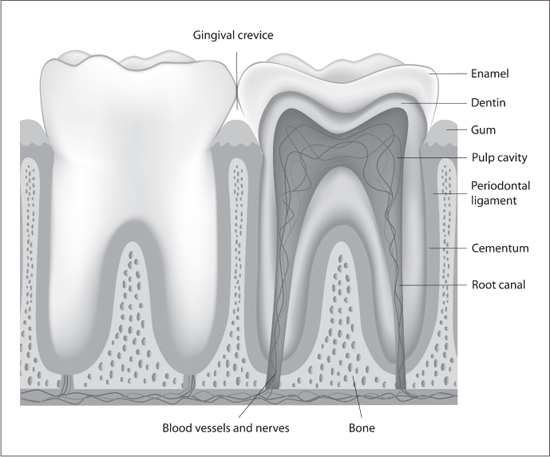
Figure 17.2. Anatomy of the tooth. Courtesy of Alila Sao Mai / Shutterstock.com.
Gingivitis is the earliest and reversible form of gum disease; periodontitis is the next and is subdivided into moderate and severe (or advanced) gum disease. Both gingivitis and periodontitis have decreased in prevalence since the early 1970s,21 principally as a result of improved dental care, secondary to employer-based dental health insurance, which helps offset the cost of professional care. Both forms of gum disease remain more common among men, especially those with limited economic resources.22
Most men age 50 and older have given their gums quite the opportunity to become diseased, simply because we weren’t encouraged to practice the rigorous oral habits that children are taught nowadays. More than half of all adult men, and nearly two-thirds of Hispanic men, have the gingivitis warning signs that include persistent bad breath, bleeding gums when brushing, and swollen, inflamed red gums.23 Unfortunately, the more severe gum disease becomes, the more men report quality-of-life problems with eating, relaxing, feeling self-conscious, and avoiding going out.24
Gum disease is caused by plaque—the layer of bacteria that forms on our teeth when not properly cleansed. The gum tissue next to the teeth normally has a small “pocket” no more than 3 millimeters in depth. When the gum is chronically infected, the gingival tissue around the teeth decomposes and draws away from the teeth to cause deeper “pockets” between teeth and gum tissue. Bleeding of gum tissue when you brush or when the dentist probes the tissue is an indication that you already have gingivitis. Without conscious, active self-care and regular dental cleaning, the ride into periodontal disease becomes a free fall.
With periodontal disease, the pocket depth will increase to 5 millimeters or greater, becoming a virtual “pit” and breeding space for yet more aggressive bacteria to be produced, weakening tooth attachment to the bone. Eventually, if too much bone is lost, the teeth become loose and/or require removal. Most times gum disease causes us no pain, but there are other ways to self-diagnose. You will notice the persistent bad breath, even minutes after you’ve brushed and/or used a mouthwash. You find your gums tender (not necessarily painful or sore), and when you examine them in the mirror, most of the tissue looks redder rather than the expected salmon pink. You are witnessing periodontal disease. Should you find that your gums bleed while brushing or as you spit the toothpaste, the red flag is up. Changes in the way your teeth fit together and getting more food stuck in between your teeth are also warning signs.
Periodontal disease is treatable; however, the success rate depends on the progression of the disease before treatment and your commitment to self-care after therapy. As mentioned, severity is defined by the depth of the pockets—the spaces between the teeth and gums. If the disease isn’t yet severe, the primary treatment includes root planing and scaling, along with medications to control the infections. When a dental hygienist does a “scaling” (or deep cleaning), the objective is to remove the plaque and tartar within the pockets under the gum line. Root planing entails the smoothing of the tooth’s root surfaces, which makes it more difficult for plaque to build up and easier for the damaged gum tissue to heal. Traditionally, both procedures were done with a hand instrument (a scalar), which still may be the method of choice. The dental hygienist may want to use an ultrasonic cleaner or a diode laser to better remove the plaque-causing bacteria. The scaling and planing can be uncomfortable, and they are usually completed with a local anesthetic rubbed on or injected into the gums. The dentist also may prescribe some medication (usually a heavy-duty dose of ibuprofen) to help ease the posttreatment pain and induce a faster healing process. The scaling and root planing may be sufficient to stabilize the progression of the gum disease, and with ongoing dental visits for deep cleaning you can sustain your mouth’s health.
For some men, scaling and planing are not sufficient; periodontal surgery becomes necessary when the gum tissue around your teeth is unhealthy and cannot be repaired with nonsurgical strategies. Rarely is this surgical procedure done by your general dentist. You are referred to a periodontal specialist, who will perform one or more types of periodontal surgery. One is pocket reduction surgery, which involves “folding back the gum tissue” and removing the disease-causing bacteria before securing the tissue back into place. More precisely, this surgery involves removal of the unhealthy gum tissue; it effectively reduces the pocket depth, and afterward there is less remaining gum surrounding the teeth. Another is a “regenerative procedure” to assist the bone supporting your teeth. When your bone loss is severe enough, the periodontist may prefer the latter method. Bone grafts or tissue-stimulating proteins can be used to encourage your body’s natural ability to regenerate bone and tissue. A third type of surgery involves a soft tissue graft to cover exposed tooth roots and hopefully develop new gum tissue. All forms of periodontal surgery can be accomplished in one or more office visits. They require a few days of liquid or soft-food diets to give the gums time to heal. Each of the procedures is expensive, though often partially covered if you have dental insurance.
As we age, we may become more susceptible to tooth decay caused by periodontal disease, which exposes our teeth’s roots to bacteria.25 Cavities (also called caries) are decayed areas of your teeth that develop into tiny openings or holes. Untreated, the size of the cavity expands, and the decay usually causes a toothache if it reaches the pulp. In its early stages a cavity will not usually cause pain and can be treated by a simple filling; this is why regular dental checkups and early detection are so important. Otherwise, untreated cavities are the main cause for having to undergo a root canal and, sometimes, the need for a tooth implant or being fitted for dentures.
To avoid losing the ability to chew, swallow, and talk, it is worthwhile to understand how we get cavities. They develop when we eat food that contains carbohydrates (the starches and sugars from bread, grains, pasta, soda, beer, candy) but neglect to clean the teeth’s surface afterward. The particles left behind feed the bacteria, and the acid produced by the bacteria is what destroys the tooth’s enamel. The acid literally eats through the outside surface of the tooth, the enamel, and then exposes the root’s protective coat, the cementum, which is more vulnerable than the enamel. When the bacteria and acid next invade the dentin, with its many nerve endings, we feel the pain.
Before resorting to pulling a tooth and hopefully replacing it with a permanent implant, saving the tooth is always the first line of defense. This might mean having a crown added—literally, capping the top of the tooth—or it might involve a root canal procedure. The benefit of both is a better quality of life compared with managing life with lost teeth.
A tooth needs to be treated when it is badly decayed or cracked, or when the tooth has already undergone several previous dental procedures. If your dentist tells you that you need a root canal, it is important to be informed on what the reasons are and what is going to happen. If you need a root canal, get it done. It is no longer the horror story that legends suggest. Your dentist will always first try to fill a decayed tooth and will only recommend a root canal procedure when the decay has infected the dental pulp.
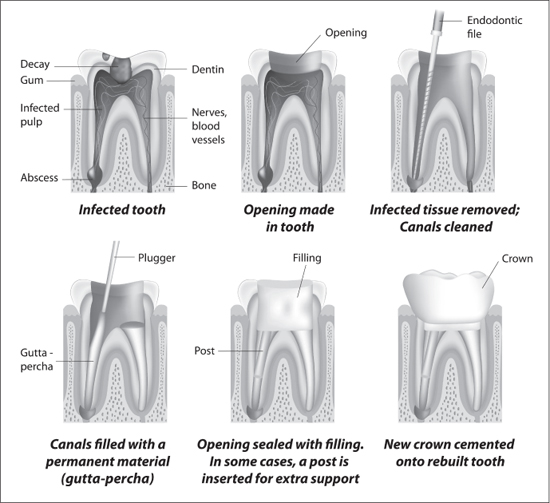
Figure 17.3. Root canal treatment. Courtesy of Alila Sao Mai / Shutterstock.com.
You may wonder why it is called a “root canal” if the infected dental pulp is the part of the tooth that is being removed. Inside the root canals is the dental pulp, which contains blood vessels and nerves, and when the dental pulp becomes infected, the nerves in the canals are (electrically) charged and we experience nagging discomfort, often pain. This “sensation” demonstrates that the pulp is inflamed or infected and needs to be removed and then the area cleaned and sealed. Otherwise, bacteria will begin to fully colonize the dental pulp, and then there is risk for an abscess to be formed. An abscess is a pocket of pus that will fill at the ends of the tooth’s roots, and if not taken care of promptly and correctly, it can cause worse damage, including significant bone loss and pain.
A root canal is called an endodontic treatment, which means that it treats the inside of the tooth. You can go to either your dentist or an endodontist, depending on the amount of damage to the tooth and level of difficulty. Much of the procedure parallels the experience of having a cavity filled. X-rays are used to examine the tooth and surrounding bone structures, the area of the jaw is numbed, and a hole is drilled into the tooth to access the internal canal, so that the entire inside of the tooth can be cleaned. If there is an infection active within the tooth, the endodontist usually puts medication inside the tooth, secures a temporary filling, and resumes the treatment a week later. More times than not, however, the root canal procedure is finished in the same appointment. The area of the dental pulp and the root’s canal are filled with a rubber-based material, and the hole drilled into the tooth is sealed with a filling. After a procedure like this, the integrity of the tooth’s structure is often weakened, and to avoid fracture the tooth will need to be restored with a cap or crown.
Each crown is original, built to fit the tooth. To make and apply a crown, the dentist first files down the sides and top of the natural tooth, intentionally reshaping it. An impression is made of the tooth using a Silly Putty type of molding compound, and this impression is then sent to a laboratory to construct a permanent crown that the dentist will insert in a follow-up appointment. Before concluding the initial visit, the dentist applies a temporary crown to protect the tooth.
There are a few different kinds of crowns, which look different, cost different amounts, and have different durability and lasting ability. It is important for you to choose the crown that will best fit your needs of appearance, functionality, and pocketbook. Metal crowns are made of different types of alloy (e.g., gold), and even though they are not truly appealing to the eye, they are known for being the most durable and lasting crown. They are also least likely to chip and do damage to other teeth that are nearby. The biggest downfall is that they make you look like you are in a rap music video, so keep the metal crowns for the back, out-of-sight teeth. Porcelain-fused-to-metal crowns have been the standard for many years. All-ceramic or all-porcelain crowns provide the best natural color, are preferred for the frontal teeth, and are the best choice when aesthetics are important, because they are the most able to replicate your normal teeth. Not only are they durable and long-lasting when properly maintained, but the development of new ceramic materials (referred to by such names as E-max, Laur, Bruxzir) has enabled dentists to dramatically improve the cosmetic appearance of the crowns. The new ceramics also permit the dentist to just cover that part of the tooth that is visible; this is known as a veneer and discussed later in the chapter. There are essentially no differences in the prices of ceramic and porcelain crowns; all-gold crowns are a little more expensive. Finally, all-resin crowns are made to match your teeth color and are the least expensive crown, but they are not used as a long-term solution, as they are prone to chipping.
Compared to earlier generations, fewer men are experiencing tooth loss. Adult men have 28 to 32 teeth to start. When a man has six or more teeth removed due to decay/disease, it is medically called partial edentulism. Complete edentulism is when no natural teeth remain. Tooth loss can be caused by tooth decay or periodontal disease. Whenever there is tooth loss, it affects the mouth’s functionality (e.g., chewing), speaking, and the way a man perceives himself. The treatment for tooth loss depends on the number of teeth lost—ranging from permanent dental implants, to dental bridges, to the replacement of teeth with dentures, partial or full.
The replacement of missing teeth is very important. When teeth are lost, the remaining teeth tend to shift and fill some of the empty space created. The shifting leaves the remaining natural teeth leaning in odd directions, resulting in a crooked appearance. The basic types of tooth replacement are dental implants, fixed dental bridges, removable partial dentures, and removable complete dentures. All types of tooth replacement make a huge, positive impact on your life. They will increase your confidence with your appearance and enhance your ability to enjoy eating (biting and chewing), talking, laughing, and going out with family and friends.26
The cost-benefit analysis when considering one to several replacement teeth leans more favorably toward having dental implants. Implants can be used to replace one or several missing teeth. The result feels like a natural tooth. They do not rely on neighboring teeth for support, and each implant is designed to permanently fill the existing empty space. Within a short time you will not remember that you have a “false tooth” in your mouth. Implants involve titanium-threaded screws that are surgically placed into the jaw bone where the teeth are missing; the screws become the “roots” to hold a replacement tooth. If several adjacent teeth are missing, you do not have to place an implant for every tooth. An implant can hold one replacement (or prosthetic) tooth, and several implants can anchor a row of replacement teeth or an entire arch of teeth. The work is typically completed in stages. Most often you will be referred to a periodontist or oral surgeon for surgical implant(s), and then after you heal your dentist will attach a temporary cap. After you’ve healed for 1–2 months, your dentist will complete the procedure by adding the permanent crown or a row of crowns. Implants are quickly becoming the ideal way to replace teeth, since they will preserve the jaw bone and do not affect your adjacent teeth.
An alternative is a fixed bridge, which used to be a dentist’s first choice in treating missing teeth, before implants came along. A bridge is a permanent restoration and will look stunningly similar to the natural teeth. For a fixed bridge, crowns are placed over the teeth residing next to the vacant spot and a “false tooth” is connected to these crowns. The adjacent teeth are what anchor the replacement tooth or teeth. Fixed bridges are sometimes preferred when the adjacent teeth are loose, because the bridge joins all these teeth together and provides greater strength. The cost of a fixed bridge is about the same as implants.
When dental implants or a fixed bridge are not affordable, partial dentures are a smart option. They are designed to keep the remaining teeth in their natural positions and fill empty tooth spaces to ensure proper biting and chewing, as well as a gap-free smile. A denture is a prosthesis that affixes false teeth to the existing natural teeth. The replacement teeth are traditionally attached to a pink or gum-colored plastic dental base that is held together by a metal structure. When inserted, there are small wire clasps that grip the surrounding natural teeth to secure the denture. All in all, a removable partial denture is the preferred option only if a fixed alternative is not affordable.
Complete dentures are used when there are no healthy teeth left in the mouth. If there are a few remaining teeth that are not salvageable, the dentist will pull them in order to make room for the complete denture. The conventional dentures are placed immediately after all the teeth are removed and then adjusted after 8–12 weeks. This is the time needed for the gums to shrink and for the fit to improve. Two common problems that many men have with their dentures is the adjustment needed to finally obtain the right fit and the need to have the dentures relined after a period of time. A small amount of denture adhesive may be applied to properly fit the denture.
Most men with a new denture are initially hesitant to bite and chew some foods, but after a while they get used to the feel and also learn to cut food into smaller pieces. Having dentures doesn’t often interfere with maintaining a balanced nutritional diet, and dentists will often recommend that men with dentures take supplemental vitamins to assure their health.
It is clear that in today’s society, image counts, and as a flood of advertising suggests, what better way is there to impress the person next to you than flashing a smile with perfectly white, straight teeth? Improving our image and in turn our self-esteem is becoming a key reason for middle-aged and older men to take care of their teeth. Even though brushing, flossing, and visiting the dentist are all part of the routine to keeping our mouths healthy, let’s not kid ourselves—most men are as concerned with how our teeth and mouth appear. We can become embarrassed by the color of our teeth and go through great lengths not to show them. If you can afford it, is it time to stop hiding and start flashing those pearly whites? There are many ways to reverse all the coffee and food stains on the outside of our teeth, from getting our teeth professionally cleaned and examined for dental problems, to using whitening toothpastes or gels, to new professional cosmetic dentistry techniques.
The means to obtain a white(r) smile differ in significant ways. They involve variations in cost, in the length of their effect, and in the amount of time needed for the procedure.
The first method includes over-the-counter whitening toothpaste, whitening strips, and/or whitening mouth guards. Each includes a very low level of whitening (or bleaching) agent, 3–6 percent hydrogen peroxide, and they are the most cost-efficient way of initially achieving a white(r) smile. The best part about whitening toothpaste is that you will not feel like you are going out of your way to whiten your teeth. It is necessary to be persistent in order to achieve the results you want, so you should brush with it at least twice a day. Over-the-counter whitening strips require a little more effort, but they can be worn as you go along with your everyday activities. Teeth-whitening strips are thin, clear, flexible pieces of plastic coated on one side with a thin film of hydrogen peroxide bleaching agent. The strips are positioned over the teeth and then gently pressed into place to stabilize them and maximize the contact between the whitening agent and the teeth. The process requires two sessions of roughly 30 minutes per day for 2 weeks before results are noticeable. If you are unable to find time or remember the white strips during the day, a great alternative is a night whitening mouth guard. Simply put the mouth guard on before bed, and within 2 weeks your teeth may look much brighter.
The next strategies involve making trips to the dentist and greater expense. As much as we like to avoid having a dentist scrape the plaque off our teeth, it is a fact that a regular professional cleaning whitens teeth. If you visit the dentist at least once a year for a cleaning, then you are already doing your appearance and teeth a favor. Your dentist is also able to provide you a whitening mouth guard sculpted specifically for your teeth. If you feel that your teeth need a dramatic change in color, another option is in-office bleaching. This method requires a high level of whitening agent being applied to the teeth, 25–35 percent hydrogen peroxide, and then use of heat or light to further increase the whitening effect. Results can be seen after only one appointment; however, maintaining the whiteness will require additional future appointments. This can also cause some tooth sensitivity, so you should discuss options with your dentist.
The lower the percentage of peroxide whitening agent, the more time is needed to whiten the teeth, but the less the expense. By comparison, if your teeth are already stained and have a darker baseline to start with, whitening methods will take longer to achieve the results you see advertised, and it is unlikely that you will ever mimic the “doctored” photos. Be careful: you can construct such a dazzlingly white set of teeth that the appearance effect is “unreal.”
Veneers are thin, custom-made porcelain moldings that are put over our teeth to hide cracks, gaps, and misshapen teeth. If you have been whitening and bleaching and not seeing results, veneers give a white smile that will not fade or discolor over the years. The process is much simpler than required to fit a cap or crown. First, the tooth (or teeth) is shaved down a bit by removing some of the existing enamel. This is done in order to keep the added thickness of the veneer from looking odd. Then, a mold is taken of the tooth (or teeth) for a lab to make the veneers custom fit your mouth. The last step is applying the veneers with an adhesive that binds to natural teeth.
The decision to invest in veneers pivots on the aesthetics versus costs. With veneers there is no need to be self-conscious about misshapen or cracked teeth anymore. Plus, they are stain-proof and retain the same whiteness from the day they are applied. This means that there is no need to use whitening or bleaching methods anymore, but it also means that you must studiously maintain the upkeep on your other teeth. Because there is no noticeable way to tell the difference between a natural tooth and a veneer, you would take care of veneers the same way that you would take care of natural teeth—by brushing and flossing regularly. Recognize, however, that the decision to get veneers is irreversible because of the enamel taken from natural teeth to fit the veneers.
Along with whitening and veneering, cosmetic dentistry also includes straightening teeth. If you believe that braces are too embarrassing for a middle-aged or older man, or simply not appropriate for a man your age, then there is a clear alternative: Invisalign. These clear “braces” are usually worn for 12 or 18 months, and during this time they can dramatically improve the straightness of your teeth and your bite without having an adolescent’s “metal mouth.” Much like a very thin mouth guard, the “braces” can be removed when eating, drinking, and for special occasions.
Another interesting advantage is that you can choose the way you want your smile to look. This is accomplished by the orthodontist showing you through computer technology how they can control the way your teeth shift to get that (perfect) smile. The Invisalign molds are changed every 2 weeks in order to keep your teeth and bite modification on track. However, Invisalign is expensive, equivalent to conventional metal braces, and depending on your dental insurance, the orthodontist visits could be costly. They cannot correct all problems, and a consultation with an orthodontist is necessary to determine if you are a candidate.
Oral cancer is a scary topic to examine in the context of dental and oral health; however, it is important for men to understand that oral cancer is a growing risk. Public health agencies anticipate that the risk for oral or pharyngeal cancers is growing, affecting tens of thousands of men annually. Of men newly diagnosed, only half will be alive in 5 years. The high death rate is not because it is hard to diagnose, but because the cancer is routinely discovered very late in its development. Oral cancer commonly originates on tissue on the lips or tongue, but it can occur on cheek lining, gums, or either the roof or floor of the mouth. The tumors may resemble small ulcers or lumps, and men may initially disregard them as “cankerous sores.” Symptoms include white (or mixed red and white) patches inside your mouth, a growing lump that is crusted and rough, and bleeding.
Oral and pharyngeal cancers have become the sixth most common type of cancer in men, mostly because men engage in high-risk behaviors and underrate the importance of routine dental cleanings and checkups. Early detection is crucial to increasing the survival rate for these cancers, but early signs of oral cancer are difficult for us to detect at home. Regular dental visits are your way to assure an early diagnosis.

Figure 17.4. Routine oral cancer exam. Illustration by Jacqueline Schaffer.
The prominent cause is tobacco use. The decision to smoke—particularly cigarettes, but men who use cigars or a pipe are not immune—is a gamble against your health. Playing craps might have better Las Vegas odds than other types of gambling, yet the house nearly always wins. Smokers inevitably lose. “Smokeless” tobacco—whether called spit or spitting tobacco, dip, chew, or snuff—also leads to oral cancer. Men using snuff place a “pinch” between the cheek and gums or behind the upper or lower lip. Men who “chew” usually hold or “store” the tobacco toward the back of the mouth in the cheek, typically the lower cheek. By holding the tobacco against the cheek and gums, the nicotine and cancerous chemicals in tobacco are absorbed through the tissues lining the mouth, which can cause cancerous changes in the adjacent tissue.
The other prominent cause is the human papillomavirus (HPV), a sexually transmitted disease that men invisibly carry, rarely exhibiting symptoms.27 Men are more likely to have an oral HPV infection than women, and a rise in oral sex may be driving up HPV infection rates in men. For men who smoke and reenter (or remain in) the dating marketplace, there is a near doubling of the risk of oral cancers. Sadly, the methods used to treat oral cancers (surgery, radiation, and chemotherapy) are disfiguring and costly.
Men’s motivation to participate in self-care and seek dental care has begun to shift from “doing nothing” to embracing oral health for life. The way we care for our teeth, gums, and mouth reflects and affects the way we view ourselves. Most of all, it affects our entire attitude toward how to live the second half of our lives. We now have the ability to make ourselves look and feel good about our mouth’s appearance and ensure that our teeth and mouth retain their functionality. Struggling to chew, swallow, or talk diminishes your quality of life. Why should poor dental health be an accepted consequence of getting older, much as it marred our grandfathers’ and fathers’ well-being? We have the power to not be that guy grossing out others with his dragon breath. By taking up good dental health habits and, equally importantly, going to the dentist, we won’t have to deal with the hassles of serious oral health problems. Any less distress is always a good thing. If you want to have strong and functional teeth, then take care of them. They are the only teeth you have.