Listen up: the combination of excessively high androgens is the most common hormone problem of women in their fertile years, and perhaps even before puberty. After menopause, high androgens are associated with serious health problems, such as heart disease, stroke, mood problems, and cancer. High androgens wreak havoc hormonally for women from the embryo to maturity.
Androgens are a group of sex hormones that strongly affect your liveliness, libido, mood, and self-confidence. When an embryo is about six weeks old, these hormones kick-start gender identity.
In males, androgens stimulate the embryo to increase the length and diameter of the penis and to develop the prostate and scrotum. The sex differentiation process that unfolds inside the uterus—and differentiates the boy from the girl fetus—is virilization, defined as the development of male physical characteristics such as the penis, and later, after puberty, muscle bulk, body hair on the chest and face, and a deep voice.
In females, lack of androgens causes the embryo’s ambiguous genitalia to commit to a female pattern, as a default setting. In a young girl, mildly high androgens might range from nuisance symptoms, such as acne, to more severe and serious symptoms requiring an endocrinologist’s evaluation, such as early signs of puberty (pubic hair growth before age eight), or equally worrisome, signs of female virilization. Virilization is normal in males, but requires swift medical attention in females. In adolescent and adult females, virilization—as evidenced in enlargement of the clitoris, increased muscle strength, deepening of the voice, and/or menstrual irregularity due to lack of ovulation—indicates a problem. Most worrisome is that it may be a result of tumors of the ovaries, adrenals, or pituitary glands.
Because they control the development of typically male characteristics, androgens are considered “masculinizing” hormones, but they also account for emotional well-being, assertiveness, and sense of agency—the capacity a person has to act powerfully in his social structure or an innate sense of belonging. Androgens are the biochemical underpinnings of dominance and desire, and even though males have more androgens than females do, having the right amount of androgens is just as essential to women’s health and well-being.
High androgens are everywhere you turn. A good friend of mine has this problem. Two of my cousins have it. Eighty-two percent of women with excess androgens have what is known as polycystic ovary syndrome (PCOS), a condition where the sex hormones become unbalanced for reasons we don’t quite understand. Women with PCOS—the top cause of infertility—start making more androgens, which causes the symptoms of high androgens such as acne and rogue hairs.
Here’s what confuses most people: not all women with excess androgens have PCOS, and not all women with PCOS have high androgens. While they do overlap, the difference is that PCOS is characterized by insulin resistance and ovarian cysts. Sadly, PCOS goes widely undetected; among women eventually diagnosed with it, 70 percent had not been previously diagnosed.1
Regardless of whether you suffer from excess androgens, PCOS, or there’s an overlap, it’s important to treat the root causes. (See “The Solution: The Gottfried Protocol for High Androgens” at the end of the chapter.) Excess androgens are thought by most doctors to affect women from teenage years to menopause, but new data shows women are affected far more seriously and much longer than previously believed, from in utero to menopause.
The best-known androgen is testosterone, the hormone that inspires motocross, wrestling, and bar fights. Although it is often thought of as the male hormone, women need to have some testosterone in their bodies as well. In fact, I believe women require testosterone to feel confident and sexy. The difference between men and women lies in the quantity of testosterone: women produce approximately 250 micrograms (0.25 milligrams) of testosterone a day, while men typically produce ten to forty times more than that. Of all the androgens circulating in your blood and tissues, testosterone is the superstar. It promotes muscles, bigger bones, and immune function, including the bone-marrow manufacture of red blood cells.
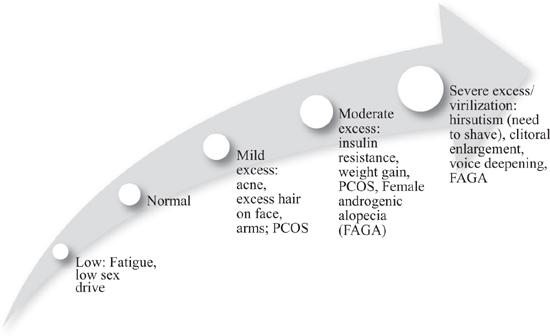
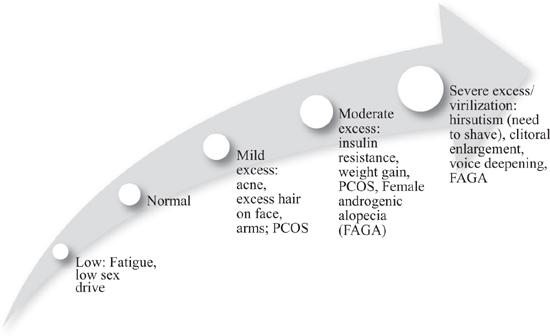
Figure 4. Spectrum of Androgen Levels in Women. Androgens normally decrease by 1 to 2 percent per year beginning in your twenties, so higher levels of androgens are less common after menopause. In reproductive-aged women, polycystic ovarian syndrome (PCOS) is common, affecting the majority of women with symptoms of androgen excess.
In men, testosterone is produced in the testes and adrenal glands; in women, it is produced in the ovaries and adrenal glands. Both sexes use testosterone to get the brain’s sexual engine fired up. In general, testosterone is released throughout the body, sending word to your erogenous zones that you are ready for sex. When testosterone is functioning properly, it revs up the hypothalamus, boosting erotic feelings and sensations. Growing research supports the role of testosterone in female desire, with evidence of low desire associated with low testosterone and increased desire with replacement.
Women reach their peak testosterone levels in their midtwenties, after which comes a slow but steady decline, about 1 to 2 percent per year, of available testosterone. Fifty percent of the testosterone in a woman’s body comes from conversion of two other types of androgens—DHEA and androstenedione—in the skin and fat tissues; 25 percent from the adrenal glands; and 25 percent from the ovaries. By menopause, testosterone levels are at half the peak level, mostly due to decline in adrenal production. (Even after your ovaries stop producing estradiol—the most common estrogen during a woman’s reproductive years—the ovaries continue to make testosterone.)
We’re learning more each day about the role of testosterone in women, particularly from studying females who have had their ovaries removed. Since ovaries produce testosterone, women whose ovaries have been excised are suddenly operating with 75 percent less testosterone. Most of these women feel the drop almost immediately, often with hot flashes and a substantial decline in libido, confidence, and verve.
If all this talk about mood and libido sounds familiar, it should: testosterone has an overlapping role with our old friend estrogen. You see, testosterone can be converted to estrogen; fat cells contain an enzyme, called aromatase, that converts testosterone to estradiol. The more fat you have, the more likely it is that you’ll create an excess of both androgens and estrogens. We know that excess estrogen may make it extremely difficult to lose weight, which then reinforces the cycle of more fat, estrogen, and weight. We also know that too much testosterone is associated with mood problems such as depression and anxiety, weight gain, and what we call sexual issues (as in, “Back off, Cowboy!”).
Women with too much testosterone have deeper voices, more pubic and facial hair, and more muscular builds than women with normal amounts of this hormone (Figure 4, page 207). Occasionally, high testosterone is so significant that it causes balding, a full beard, or growth of the clitoris. We also know that criminal violence and aggressive dominance in women are linked to higher testosterone.2 As if that weren’t enough, recent data shows that women with higher testosterone levels have more depressive symptoms during the menopausal transition.3
Women with higher testosterone levels have been shown to have a greater appetite for risk.4 A group of MBA students enrolled in a lab game in which they could choose to gamble or to take a certain amount of a guaranteed win, which increased each time. Measuring testosterone levels in the saliva on two occasions two years apart, the researchers found that the women with the highest testosterone levels were the most likely to gamble. Testosterone levels also predicted ultimate career choice: women with higher testosterone were more likely to have chosen riskier careers, such as investment banking and finance. These jobs tend to have fatter salaries, but also less security and a higher probability of turnover.
FROM THE FILES OF SARA GOTTFRIED, MD
Patient: Cheryl
Age: Fifty-five
Plea for help: “My clit is growing!”
Cheryl is a midlevel executive at a public relations firm who recently married for the second time. Her libido had been abysmal for the past ten years, yet she loves her new husband and wanted to feel more passionate toward him. Her woes led her to a doctor, who prescribed 2 percent testosterone cream, which she applied to her vagina. Within a few weeks, Cheryl had large, painful pimples on her cheeks and jawline and had to wash her hair more often.
When I performed an exam, her clitoris indeed looked like a tiny penis. The clitoris has a wide normal range and engorges with blood during sexual arousal; the nonaroused clitoris is normally 3 to 4 mm wide by 4 to 5 mm long. Cheryl’s was 8 mm wide by 7 mm long. The testosterone in her blood was, not surprisingly, elevated: the normal range of free testosterone—I’ll explain what that is in a minute—is 0.1 to 6.4 picograms/milliliter (pg/mL); Cheryl’s was 10.6 pg/mL.
Sometimes high doses of testosterone can cause liver damage and lower the level of HDL (good cholesterol) in the blood. After checking Cheryl’s liver enzymes and doing a cholesterol test, I was relieved to find normal levels.
Treatment protocol: Upon my recommendation, Cheryl stopped using the testosterone vaginal cream. After six weeks, both her clitoris and testosterone level were back in the normal range. I recommended instead a trial of maca, an herb proven to raise sex drive in menopausal women, to help her libido.
Results: Four weeks later, Cheryl reported that her hair and skin were less greasy, and lovemaking with her new husband was much steamier.
Besides testosterone, your body makes several other androgens, including the following:
Dehydroepiandrosterone (DHEA). Considered the prehormone to testosterone, DHEA can convert into testosterone when needed. High DHEA has been associated with depression in menopause and acne in women with PCOS.5 DHEA has been used topically in the vagina to reverse atrophy and dryness.6
Androstenedione. A steroid sex hormone that is an intermediate in the production of testosterone and estrogen from cholesterol, androstenedione has both androgen and estrogen activity. In other words, it’s promiscuous and likes more than one hormone receptor. Too much androstenedione can cause “minor” symptoms, such as acne and hair loss.
Dihydrotestosterone (DHT). Testosterone also can be converted to dihydrotestosterone (DHT). Three times more potent than testosterone, DHT is the main cause of male-pattern hair loss, which occurs in both men and women. High DHT can cause female androgenic alopecia, or FAGA.7 Most women with FAGA have hair loss from the temples (the places where men commonly have bald spots).
Of all the circulating androgens, only testosterone and DHT can bind to androgen receptors. Translation: the other members of the family can’t trigger the androgen sequence of events, whether good (building muscle and bone, boosting confidence and libido) or not good (hair loss, rogue hair growth). What the ancillary androgens offer is the intermediate prehormones needed for production of testosterone and estrogen.
In my practice, I’ve seen many women who got the brushoff from their primary-care doctors when they expressed concern over thinning locks or raging acne. Yet the problems go far beyond losing or gaining hair or having a complexion like your teenage daughter’s.
Most women with high androgens suffer from insulin resistance, and androgens and insulin have their own tango. Insulin resistance is when you need higher and higher levels of insulin for the same result—that is, to drive glucose into cells as fuel. It’s the law of diminishing returns: over time, insulin becomes less effective at lowering blood glucose because the cell becomes numb. Eventually, you have high insulin and high glucose. This is bad because high insulin causes the ovaries to make excessive amounts of androgens, and insulin also gets the liver to make less sex-hormone-binding globulin (SHBG), the key protein that binds testosterone and keeps it from causing trouble. This combination results in more free testosterone charging around the bloodstream like a bull in a china shop. High glucose inches you toward prediabetes and diabetes.
Here’s the lowdown: insulin is made in the pancreas, and under normal circumstances, its release is finely calibrated to produce just the right amount so that glucose is extracted from food in your gut, sent into your bloodstream, and then driven into cells, particularly the fat, muscle, and liver cells. In other words, the main job of insulin is to regulate your blood sugar. Think of insulin as the knock on the door of your muscle, liver, and fat cells. The cell hears the knock and opens the door to let in the glucose. Once insulin gets glucose inside the cell, the cell can get busy with crucial tasks such as growth, movement, and repair. With insulin resistance, insulin is banging on the door of the cell like an irate neighbor, yet the cell can’t be bothered with opening the door anymore, so the pancreas gets the message to make more insulin. Then a vicious cycle is off and running, and the knock of the insulin just gets louder and louder—insulin levels rise and the cell is numb. Insulin is also a fat-storage hormone, so you deposit more fat, notably at your waist.
When you need higher and higher amounts of insulin to deliver glucose as fuel to your cells, you burn out the ability of the pancreas cells (islet cells, to be precise) to keep up with demand. You lose pancreatic reserve. When this happens, you cannot stabilize your blood sugar within the normal range anymore—defined as a fasting blood sugar of less than 87 mg/dL. Your blood sugar rises, initially to prediabetes levels, and possibly to the diabetes range.
Insulin resistance heralds several serious problems, including excess weight, obesity, prediabetes, diabetes, dementia, Alzheimer’s, stroke, and some cancers. Insulin is not something to mess with. Here’s an analogy: insulin resistance fosters a bad neighborhood around the cells of your body, but instead of drive-by shootings, muggings, and other high crime influencing your vulnerable cells, you have too much sugar, inflammation, clogged arteries, and weight gain. These problems lead to accelerated aging, wayward hormones, and poor organ reserve.
It’s the classic chicken or egg scenario: it’s not clear whether high androgens cause insulin resistance or insulin resistance causes high androgens. Either way, we know that high insulin levels drive the ovaries to make more testosterone. Insulin resistance is also a major factor in the troubling condition called metabolic syndrome, a cluster of ominous signs that are linked to a greater risk of diabetes and heart disease; it affects one in four women in the United States.
Do you have a problem with insulin? Think back to Part F of the questionnaire in chapter 1. If you answered yes to the question about ovarian cysts, consider having an ultrasound to find out if you have multiple small cysts in a characteristic string-of-pearls pattern, the “Pearl Sign.” If you do, your risk of type 2 or adult-onset diabetes is increased by a whopping 80 percent. Indeed, simply having menstrual irregularities or symptoms of high androgens increases your risk of diabetes by 50 percent. Or perform the mirror test, as described by Dr. Mark Hyman: Stand in front of a mirror without a shirt. Jump up and down. If your belly jiggles, you have a problem with insulin.
Of all of the problems I see in my practice, balancing insulin and glucose is the biggest challenge. This is because of the serious health consequences and the great difficulty most of us have eating less sugar and fewer carbohydrates. It’s a common thread in my practice to see patients who struggle to limit pizza, pasta, and pie.
Experts estimate that between 25 and 50 percent of the U.S. population is insulin resistant, which can lead to a number of problems in women that relate to polycystic ovary syndrome (PCOS) and reinforces symptoms of excess testosterone.
Insulin resistance:
• raises the activity of aromatase, the enzyme chiefly responsible for estrogen production, which sets the stage for estrogen dominance and lack of ovulation.
• enhances the activity of 12/21 lyase, an enzyme that increases androgen levels.
• lowers sex-hormone-binding globulin (SHBG), allowing more free testosterone to roam the bloodstream and trigger rogue hairs and pimples.
• raises blood markers of inflammation (biomarkers) such as interleukins, cytokines, and adopokines, which initiate a perpetual cycle of inflammation.
While scientists lack consensus on the best way to measure your sensitivity or resistance to insulin, here’s my advice: ask your doctor to measure your levels of glucose and insulin after you’ve fasted for eight to twelve hours (check with your local lab). I believe the optimal range for blood glucose after fasting is 70 to 86 mg/dL; insulin should be less than 7 mcU/mL. Most gynecologists use a glucose-to-insulin ratio to determine if a patient is insulin resistant. Overall, a G:I ratio of less than 4.5 is abnormal.8
However, the Androgen Excess and PCOS Society (I kid you not) recommends that all women with PCOS get a two-hour oral glucose tolerance test to look for blood sugar problems every one to two years.9 If you get this test, it’s essential to add an insulin level to the fasting glucose prior to the test, and then check glucose and insulin one and two hours after drinking the “glucola,” which is a standardized sugar drink laboratories provide.
While they vary according to the specific type of androgen, the main causes for high androgens are genetics, chronic stress, and excess body fat.
Genetics. It’s often easy to blame our parents for everything, but sometimes that blame is appropriate. From looking at how symptoms cluster in families, we know that genetics plays an important role in androgen levels. Forty percent of women with PCOS have a sister with the same condition, and 35 percent have a mother with it. You can inherit the risk from either your mother or your father.
Chronic stress. Ah, our old friend stress. Seems connected to everything, doesn’t it? Some women have high androgens simply because they are habitually stressed and their bodies are rebelling. Continual stress can throw your adrenal glands into overdrive, increasing the release of stress hormones, such as cortisol, and also increasing the level of androgens. When you produce too much DHEA, you get symptoms such as pimples and rogue hairs. Even mild anxiety raises your DHEA.10
Excess body fat. Extra body fat impacts androgen levels. In adults, body fat is necessary for normal gonadotropin levels. Gonadotropins are the control system for hormones: they determine how much estrogen, progesterone, and testosterone you make, depending on how much luteinizing hormone (LH) and follicle-stimulating hormone (FSH) your brain releases. Think of LH and FSH like mafioso who normally share the territory. They’re the bosses of hormone underlings, estrogen and testosterone, who vary in brains and brawn. When you have excess body fat, the extra testosterone and estrogen you produce blocks the FSH. FSH gets demoted. This leads to LH dominating FSH, and from there, it’s a short step to irregular menstrual cycles.11 LH becomes the new mafia boss, and you no longer ovulate every month. Women with polycystic ovary syndrome (PCOS) almost always have an aberration in secretion of gonadotropins versus women with normal menstrual cycles.
Rare causes. Uncommonly, androgens rise because of an androgen-secreting tumor in the ovary. That’s usually how the bearded lady got that way, although sometimes those women suffer instead from untreated PCOS. Another unusual cause is called congenital adrenal hyperplasia (CAH), a group of inherited disorders of the adrenal glands that affects both males and females. All people with CAH have in common a deficiency of an enzyme that is involved in the synthesis of cortisol, or aldosterone, another hormone made in the adrenals, or both. I recommend considering CAH before a diagnosis of PCOS is made, since the treatments are different.
Most women with excess androgens have PCOS. It sounds like a scary syndrome, and it is. The most common hormone condition in women of reproductive age, PCOS affects 20 percent of women and can interfere with fertility by blocking regular monthly ovulation. If you are trying to conceive, I recommend asking—no, demanding—that your doctor do a blood test to check your fasting insulin, glucose, progesterone on Day 21, and leptin. This will clarify whether or not you have insulin resistance. Before you go the übermedical route, you may be able to improve your fertility with a few small lifestyle and food changes specifically targeted to women who want to get pregnant.
Women with PCOS typically develop many small cysts on their ovaries—often between ten and one hundred small cysts. We believe the cysts are a result of disturbed hormones and ovulation, so that eggs don’t go through the normal maturation sequence of (1) a cyst forming around a ripening egg (the corpus luteum); (2) the release of luteinizing hormone (LH) from the brain to trigger the ripe egg to pop out of the cyst and head toward the fallopian tube for possible fertilization; and (3) the now-empty cyst getting reabsorbed into the ovary. Short version: the maturation sequence of the eggs is disturbed so that there is a breakdown and ovulation doesn’t happen. And if you’re not ovulating, you won’t be getting pregnant.
The cysts in PCOS are not dangerous. It’s more that the multiple cysts, along the periphery of the ovaries like a string of pearls, are along for the ride—they are a sign that ovulation is not happening. Over time, the cysts do not grow. They are not the type of cysts that require surgical removal and, unlike some other cysts, are not associated with an increased risk of ovarian cancer. Women are often treated for PCOS with a birth control pill, which suppresses LH and thereby lowers production of ovarian androgens. Not the sort of treatment you want if you’re trying to get pregnant.
The exact cause of PCOS is obscure. However, we know that there are two main hormonal underpinnings: high androgens in 50 to 82 percent of women with PCOS, and high insulin in 50 to 80 percent.12 Additionally, PCOS is often associated with obesity. Among women with obesity, 28 percent have PCOS, whereas only 5 percent of lean women have PCOS.
Perhaps PCOS is often left out of many hormone books because the topic is so complex and hard to diagnose. Symptoms are varied and manifest differently over time, which makes it very difficult to determine a precise, uniform definition of the syndrome. Some women with all the other symptoms of PCOS do not have polycystic ovaries. Some, but not all, women with PCOS have hirsutism, or increased hair growth where it doesn’t belong. Some women with PCOS are obese or overweight, but others are lean. Regardless, it’s important to treat the root cause.
Nearly all women with PCOS share these symptoms:
• Difficulty losing weight. Up to 75 percent of women with PCOS are overweight. While losing weight is hard enough for most people, women with PCOS have an even harder time, probably because of their high insulin levels, which alert the body to store fat at all costs. High insulin also increases hunger and carbohydrate cravings. When women with PCOS have high insulin levels, it exacerbates all the features of PCOS.
• Rogue hairs. When you have too much androgen circulating in your bloodstream, it can stimulate your hair follicles to thicken and grow. The result can be increased hair growth on the upper lip, chin, breasts, between the breasts, back, belly, arms, and thighs. Hirsutism, or excess hair growth, in a male pattern, is present in 80 percent of women with excess androgens and is a diagnostic condition of PCOS.13
• Inflammation. Women with PCOS have chronic, low-grade inflammation, which may provide the molecular basis for PCOS.14 I encourage you to reduce inflammation if you have PCOS by following the lifestyle reset, described in “The Solution: The Gottfried Protocol for High Androgens” (page 222).
How PCOS is manifested depends on age, genes, and environment, including lifestyle and body weight. Figure 5 provides the age-related ways that PCOS may appear, from tween years to middle age.
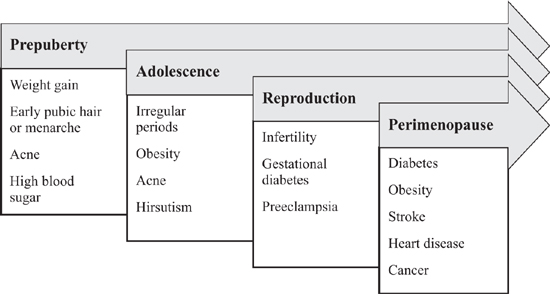
Figure 5. Signs of PCOS Across the Female Life Span. How a woman shows signs of PCOS varies according to her age and life stage, as well as her genetic and environmental influences.
PCOS is also linked to other significant health concerns:
Heart disease. PCOS puts you on the fast track to major diseases, like heart disease and stroke.15 PCOS is associated with an undesirable cardiometabolic profile, as measured by belly fat, high blood pressure, inflammation, insulin resistance, and abnormal glucose metabolism—and a sevenfold increase in diabetes.
The risks can last a lifetime: insulin resistance, high ovarian output of androgens, and inflammation all persist after menopause.16
Cancer. PCOS may be associated with an increased risk of hormone-dependent cancer, such as breast cancer and perhaps endometrial cancer.17 The underlying mechanism is that when women rarely ovulate, the ovaries continue to make estrogen but it’s not balanced by progesterone, which is released by ovulation. Over time, this can lead to buildup of the uterine lining and precancerous changes.
Mood problems. Even among lean women with PCOS, there is an increased rate of body dissatisfaction and depression symptoms, as well as more anxiety, depression, withheld anger, diminished sexual satisfaction, and lower health-related quality of life.18 Anxiety correlates with androgen levels and insulin resistance, but not with body mass index or age.19
Abnormal liver enzymes. Blood tests show that 30 percent of women with PCOS have high levels of liver enzymes, which indicates inflammation in the liver and probably scarring.20 In other words, one in three women with PCOS has a liver that doesn’t work normally. If you’ve been diagnosed with PCOS, you’ll want to get your liver checked, and I recommend caution with alcohol and medications that overtax the liver and can harm it.
PCOS generally starts early in life, probably in utero, but it’s very hard to diagnose until puberty, when a girl starts to have a menstrual cycle. Classic signs then appear, such as irregular periods, acne, increased hair growth (on the chin and chest), and sometimes acanthosis nigricans, a dark-colored, velvety discoloration on the underarms and back of the neck. I recommend diagnosing PCOS as early as possible, so that lifestyle changes can be instituted and, ideally, the unfortunate consequences of subfertility, obesity, diabetes, and heart disease can be prevented. If you think you may have PCOS, I recommend seeing your physician for hormone tests and a possible ultrasound.
Here’s a recap of why awareness and diagnosis of PCOS are so important:
• PCOS is the top hormone imbalance in women up to age fifty.
• Overall, one in five U.S. women have PCOS, yet 70 percent don’t know it.
• Of women with high androgens, most have PCOS, and the high androgens are associated with high insulin, obesity, and inflammation. It’s a vicious cycle that is extremely difficult to break.
• High androgens (and by extension, PCOS) affect women across all stages of life, even though most people think about its role only in reproductive-aged women.
• Most of the treatments that doctors offer for PCOS (birth control pills or metformin) do not address the root cause of the problem, which is why I believe a systems-based approach such as The Gottfried Protocol is preferable to synthetic medication.
You’ve seen the infomercials. You’ve clipped the ads for your beloved. Rogaine (minoxidil) and Propecia (finasteride) are two treatments for hair loss. Before I tell you why I don’t think you should be in a rush to slime your hair follicles every day or remove every molecule of testosterone in your body, let’s first consider why we’re doing so poorly with hair loss. Thirty percent of women report serious hair loss by age thirty. By age fifty, that statistic climbs to 50 percent. This is a major problem, of both vanity and sanity.
Sometimes hair loss is associated with high androgens, but more commonly, I find in women that the root cause is low iron, thyroid hormone imbalance, or insulin resistance. Before my patients start looking for a solution to their hair loss in a box from the drugstore or a pill bottle from a dermatologist, I encourage them to look inside their bodies. Remember that most symptoms women try to solve with a pill bottle are a message from the body that something is awry. To find a patient’s particular reason for hair loss, I order the blood panel listed below.
Minoxidil, which you can buy without a prescription, is actually a drug for lowering blood pressure, but when applied topically, it slows hair loss and promotes regrowth. It dilates blood vessels, allowing more oxygen, blood, and nutrients to reach the hair follicles, resulting in new, thicker, and better hairs. If you are wigging out because of hair loss and need to do something while investigating root causes, I recommend parting your hair down the middle, snapping a few photos (your smartphone works nicely) to document the width of your part and your hairline, and applying the lower dose to your scalp (2 percent minoxidil, not the higher dose for men, which is 5 percent). Then wait patiently for four months and watch your hair grow. Unfortunately, there’s no cure—when you stop using minoxidil, you will return to the rate of hair loss you had unless you’ve corrected the cause.
Taken orally, finasteride acts systemically to reduce androgens by inhibiting the enzyme that converts testosterone to DHT. While most people take these treatments to hang on to their hair, they are actually treating the downstream symptoms of high testosterone and DHT.
Both these treatments for hair loss have been studied primarily in men. Are they safe for women? Minoxidil has been used for more than thirty years, so it’s got a longer track record.
There are a few other details you should know before taking these medications. Neither treatment addresses the root cause of hair loss. My advice is to try therapies aimed at the root cause of your hair loss first, and to ask your doctor for my top blood tests, including these:
• complete blood count (a measure of whether you are anemic and your immune system is functioning)
• ferritin (the most sensitive test for iron stores in your body)
• thyroid-stimulating hormone (TSH), free T3, and possibly, reverse T3
• cortisol
• fasting insulin and glucose
• testosterone (I prefer total and free testosterone in women with hair loss)
• antinuclear antibody (tells you whether the hair loss is related to an autoimmune condition)
Remember, when it comes to your hair loss and prescription therapies, we want to reproportion your hormones, not search and destroy.
Lifestyle reset, consisting of targeted nutrition and exercise, for a period of twelve to twenty-four weeks helps women with excess androgens. The most effective strategy for reducing the levels of androgens in the blood is losing weight by eating a low-glycemic-index and high-fiber food plan, decreasing stress, and practicing yoga.
Lose weight and exercise. We know that weight loss reduces insulin resistance and excess androgens; an exercise program designed to help need not be dramatic: one program of a brisk walk twenty minutes per day resulted in a 7 percent weight loss.21 Even in adolescent girls with PCOS, weight loss corrects irregular periods, normalizes androgens, and improves cardiovascular risk factors.22
Eat for lower androgens. The glycemic index (GI) is a measure of how much the carbohydrates in a food raise your blood sugar. A low GI is less than 55 (out of 100). To put this in perspective, a baguette has a glycemic index of 95; grapefruit, a glycemic index of 25. Eating a low-GI food plan reduces androgens by up to 20 percent.23 In one study, volunteers fed a low-glycemic diet—25 percent protein, 30 percent fat, 45 percent carbohydrate—had lower levels of insulin-like growth hormone (IGF-1) after seven days. That was good news, because IGF-1 is known to affect three important aspects of acne: growth of skin cells, skin-cell production of androgens, and rate of oil production.
Fiber! Scientists agree that for women with PCOS, a low-GI, high-fiber diet is best.24 That’s because unless you have sufficient fiber to remove it, most testosterone is secreted into the bile and then reabsorbed in the gut and used again. Fiber increases excretion of testosterone in the stool. Foods that contain fiber include fresh fruits and vegetables, certain whole grains, and beans. Just a tiny sampling of fiber content to give you an idea: 1 cup of raspberries contains 8 grams, 1 cup of adzuki beans contains 17 grams, 1 ounce of oat bran contains 12 grams, and 2 cups of cooked chard has 8 grams. Once you get familiar with the amounts of fiber in foods, you can keep loose track to make sure you are getting enough each day. I recommend 35 to 45 grams of fiber per day.
Eat foods containing zinc. Zinc plays an important role in sexual development, menstruation, and ovulation. Zinc deficiency is associated with higher androgens and acne. If you have acne, eat foods with zinc, such as green beans and sesame and pumpkin seeds. It’s better to get zinc from food sources, since cases of zinc toxicity have been found among people who supplement to excess.
Avoid dairy. Milk, cheese, and eggs have been shown to increase matrix metalloproteinase (MMK), which then drums up inflammation, which leads to higher androgens and acne. You can take antibiotics to block MMK, but I suggest removing dairy for six weeks to see if it helps your symptoms.
Eat more protein. To lower your androgens, eat organic chicken and turkey, low-mercury fish, and grass-fed beef. Most of us don’t get enough of the lean stuff. I recommend eating 0.75 to 1 gram of lean protein per pound of lean body mass. A 125-pound woman with 20 percent body fat (or 25 pounds of fat) has a lean body mass of 100 pounds. She needs to eat 75 grams of protein per day if she is relatively sedentary. She needs 100 grams of protein per day if she exercises intensively. Recreational exercisers should eat 80 to 90 grams of protein per day. I count myself as a recreational athlete and eat about 85 to 90 grams per day. Here’s a typical protein lineup: breakfast, 4 ounces of tempeh (6 grams of protein/ounce, for a total of 24 grams); lunch, 4 ounces of chicken or turkey breast meat (9.5 grams/ounce, total 38 grams); dinner, 4 ounces wild Alaskan salmon (7 grams of protein/ounce, for a total of 28 grams)—grand slam total of 90 grams of protein.
Omit sugar. Sugar, that irresistible substance reviled by nutritionists but loved by the rest of us, is a big factor in excess androgens. Significant levels of sugar increase serum insulin and IGF-1, both of which raise androgens and cause excess-androgen symptoms. Advice? Sorry for all of you sweeth-toothers. Avoid it altogether.
Get your oil changed. You’ve probably heard that omega-3, long-chain polyunsaturated fatty acids (such as fish oil) are the most proven supplement on the market for improving health. We evolved as human beings with a good balance between omega-3 and omega-6.25 But our modern diet has led us to eat too many omega-6s, which are found in processed food, corn and safflower oils, and farm-raised fish. Not all omega-6s are bad, but they tend to cause more inflammation in the body, whereas omega-3s are anti-inflammatory. Here’s more data on PCOS: women with too much omega-6 compared with omega-3 have higher circulating androgens.26 Women with more omega-3s in their blood have lower androgens in the blood plus a better cholesterol profile, and as a result, less risk of cardiovascular disease, one of the risks of excess androgens. You get good sources of omega-3s from eating wild Alaskan salmon and taking a daily fish oil supplement that’s been shown to be low in mercury.
Take up yoga. Yoga was shown recently to be more effective than other forms of exercise at improving insulin resistance in PCOS.27
FROM THE FILES OF SARA GOTTFRIED, MD
Patient: Casey
Age: Twenty-nine
Plea for help: Pimples, irregular periods, trouble losing weight, an increase in hair on her arms and face.
Casey wants to try getting pregnant soon. She exercises five days a week and eats what she believes is a healthful diet, but the scale wouldn’t budge, and she really wanted to lose 15 pounds. She had a body mass index of 27 (normal BMI is 18 to 25).
Recently, she moved to San Francisco from Boston, where she had an ultrasound that showed the Pearl Sign (several cysts in a row) on her ovaries. Her doctor suggested taking a birth control pill to regulate her periods and help with weight loss. When I met her, she was still getting her period every thirty-eight to forty-five days. When Casey showed me her lab test, it revealed a total testosterone level of 156, which is high.
Remember the criteria of the Androgen Excess and PCOS Society? It doesn’t take a detective to note that Casey has all the criteria: high testosterone and hirsutism, multiple cysts on her ovaries and oligomenorrhea (fewer than nine menstrual cycles a year), and no other reason for her high testosterone. When I checked Casey’s glucose:insulin ratio, we found she had insulin resistance.
Treatment protocol: I put Casey on a low-GI food plan, with 45 percent carbohydrates, 30 percent fat, 25 percent protein. For breakfast, she ate eggs with chopped spinach or kale. For lunch, she ate lean protein such as chicken or beans with a large serving (6 ounces) of steamed vegetables and a small serving (2 ounces) of whole grains, such as brown or black rice. Her dinner was similar, with the addition of a large salad (8 ounces) with 2 tablespoons of dressing. Casey gave up dairy products and grew to love eggplant, bell peppers, carrots, and avocado. She started a yoga practice.
Results: Within six weeks, she had lost 8 pounds and her skin was almost completely clear. She began menstruating regularly (every twenty-nine days). When I retested her GI, I found she no longer had insulin resistance.
Even a 5 percent reduction in weight can normalize your hormone levels—a small lifestyle and nutritional change with a huge impact. I’m looking forward to seeing her future baby pictures.
Chromium. Chromium is a mineral that acts as an insulin sensitizer, which means it helps to reverse insulin resistance and lowers both your serum insulin and glucose levels when they are high.28 Folks with type 2 diabetes, the type that results from insulin resistance, have lower blood chromium levels compared with nondiabetic people. Chromium levels also decline with age.29 Chromium is a safe supplement worth trying if you are insulin resistant. I recommend a dose of 200 to 1,000 mcg per day of chromium picolinate.
Inositol. When they want to conceive, many women are given big-gun prescription drugs such as metformin and clomiphene. However, metformin, an antidiabetic drug that lowers blood sugar, can cause serious side effects such as lactic acidosis, which is an excessive accumulation of lactic acid in the body. In addition to diet, nutraceuticals that influence insulin can make a big difference, and may be a better alternative in younger women and girls. Inositol is a naturally occurring B-complex vitamin known to improve insulin sensitivity.30 Two inositol supplements you can get at the drugstore or health food store show promise in correcting PCOS: D-chiro-inositol (DCI) and myo-inositol (MI).
Women with PCOS appear to be deficient in DCI. New evidence supports that overweight women with PCOS be given the combination of DCI and MI first, prior to any prescription therapy. A while back, the New England Journal of Medicine reported the bold news that in women with PCOS, DCI cut free testosterone by more than half and lowered blood pressure and triglycerides in eight weeks or less.31 DCI also works in lean women with PCOS.32 Recommended dose: DCI 600 mg twice per day (but you can also find DCI in carob, buckwheat, and grapefruit) and myo-inositol at a dose of 2 grams once or twice per day.
Vitamin D. Vitamin D is a fat-soluble vitamin that is present in eggs and fish. It is added to other foods, such as milk, and is also available as a dietary supplement. I recommend about 2,000 IU per day. Vitamin D deficiency is emerging as a factor in the metabolic disturbance of PCOS.33 In fact, 44 percent of women with PCOS are vitamin D–deficient, compared with 11 percent of controls.
Women with metabolic syndrome and insulin resistance have a higher tone to their sympathetic nervous system. In other words, the coveted balance between the sympathetic nervous system, activated by stress into fight or flight, dominates over the parasympathetic nervous system, also known as rest and digest. This may show up as an increased diastolic blood pressure (the lower number of the blood pressure fraction).
Yoga. Yoga has been shown to rebalance the wayward hormones of PCOS, as described earlier.
Acupuncture. Acupuncture induced regular ovulation in one-third of women with PCOS, suggesting that acupuncture is a good alternative for many women before they turn to prescription medications, such as metformin or clomiphene, to induce ovulation.34
BPA. Women with PCOS have higher levels of BPA, and the amount correlates with both androgen level and insulin resistance.35 It’s a good idea to minimize your exposure: BPA is a plastic found in thermal print receipt paper, the plastic lining most canned food, and flame retardants. See chapter 6, “Excess Estrogen,” for a discussion of BPA.
Cinnamon. That innocent-looking cinnamon stick in your hot milk or sprinkle of cinnamon in Moroccan stew adds more than just flavor. One Cochrane Review of four trials assessing Chinese herbal supplements in subfertile women with PCOS found increased pregnancy rates when herbs such as cinnamon were added to clomiphene, a medication that may induce ovulation in infertile women.36 Cinnamon is a natural insulin-sensitizer—so it acts like metformin, but in a natural way—stimulating glucose uptake by fat cells, which lowers both glucose and insulin levels. In a study of people with diabetes, cinnamon reduced fasting glucose and cholesterol.37 As a bonus, cinnamon lowers blood pressure (often elevated in women with PCOS and metabolic syndrome) and helps correct abnormal cholesterol levels. Cinnamon also increases lean body mass.38 You don’t even need much—the most effective dose is 1/2 teaspoon per day.
Saw palmetto. While it has not been proven in randomized trials to help women improve hyperandrogenism, saw palmetto is known to reduce the conversion of testosterone to the more potent DHT and to block the androgen receptors. In other words, it acts as an antiandrogen. If you have high androgens, particularly FAGA, you may want to try a small dose of saw palmetto in a capsule at the low dose of 160 mg/day.
Tian Gui. In Traditional Chinese Medicine (TCM), PCOS doesn’t fit neatly into a single category. Tian Gui capsule is a composite of various herbs proven more effective than metformin (though less effective than a birth control pill) at lowering androgens.39
I commonly see women on hefty doses of testosterone who are not having their blood levels monitored carefully. Sometimes the result of excessive dosing is cystic acne, head-hair loss, or excessive sweating and body odor. When I measure testosterone levels in women with these symptoms, they are often closer to the normal levels for a man. Once the dosage drops, their symptoms resolve.
If, after meticulous informed consent, you choose to take testosterone, I recommend checking several things in your blood: your free, total, and bioavailable testosterone levels; cholesterol levels (because testosterone can lower HDL, your good cholesterol); and liver enzymes (because testosterone can damage your liver). Part of your informed consent should include that we do not know the long-term effects of augmenting your testosterone levels. The longest duration of the randomized trials of testosterone in women is six months.
Sometimes women read online or in a magazine that DHEA is a good idea for dealing with low energy. They go to their local health food store, buy a bottle of pills, and start taking a dose of 25 mg/day, the level usually recommended for women. But side effects inevitably ensue: greasy skin and hair, acne breakouts. When I lower the dose to 2 to 5 mg/day, the side effects often resolve. If they don’t resolve, I strongly suggest stopping the DHEA.
Other than reducing excessive doses of testosterone or DHEA, however, I can’t make any recommendations for bioidentical hormones—none are proven to lower your androgens.
Women who take cortisol or adrenal extract—ground-up adrenal gland from animals—can lower their DHEA, the prehormone to testosterone. However, I advise extreme caution with glandular extracts because they are over the counter, with no regulatory oversight. If you take glandular extracts, you do so at your own risk; please consult your local physician.
When you have balanced levels of androgens, you feel calm and confident and look your best.
• You exhibit optimal mood and assertiveness.
• Your skin is not excessively greasy or dry, but clear, with minimal to no acne.
• You’re neither pumped up like a bodybuilder nor flabby and undertoned, but have the right bone density, muscle size, and strength for your size and weight.
• Your hair is where it should be: on your head, not your chin or nipples or chest, and you have a normal distribution of pubic hair.
• You conceive when you’re ready, not held hostage by ovaries that make too much testosterone and prevent ovulation.