Elizabeth A. Holey, John Dixon
Introduction
Connective tissue manipulation/massage (CTM) or bindegewebsmassage is a manual therapy applied with the therapist’s hands in contact with the patient’s skin. It is more correctly described as a manual reflex therapy as the effects are believed to occur through stimulation of cutaneovisceral reflexes which induce an autonomic reflex response. The ability to harness this response to achieve clinical outcomes directs the clinical decision-making when using the therapy to treat dysfunction. The modality is applied with the longest digit (third finger), or thumb of the therapist’s hand, through a lifting stroke, which carefully targets each interface within the skin to create a shear force. Superficial layers may have to be treated before the deep fascial layer, which is where the potent autonomic effects are thought to occur. A pattern of strokes must be learned to enable access to the fascia where it is relatively superficial, attaching to bone and between muscle fibers, for example. The reflex connective tissue (CT) zones utilized are based on those first identified by Henry Head more than 100 years ago (Head 1898). They are particularly interesting as reflex areas as they can be seen, palpated and anatomically understood (Schuh 1992, Holey 1995).
Skin rolling
A skin rolling technique is often used in CTM, at the superficial fascial layer. The same shear force is created at the fascial/skin interface, but, with the patient in a side-lying position, the skin layer is lifted up against gravity away from the spine. If the therapist feels tension at the end of the roll and continues to roll the skin, then the autonomic nervous system (ANS) will be stimulated. This is also commonly used as a technique in its own right, either as part of classical (Swedish) massage, within myofascial release techniques and in trigger point therapy. Some proponents grasp the skin within their palm to roll tissue against underlying tension.
Background
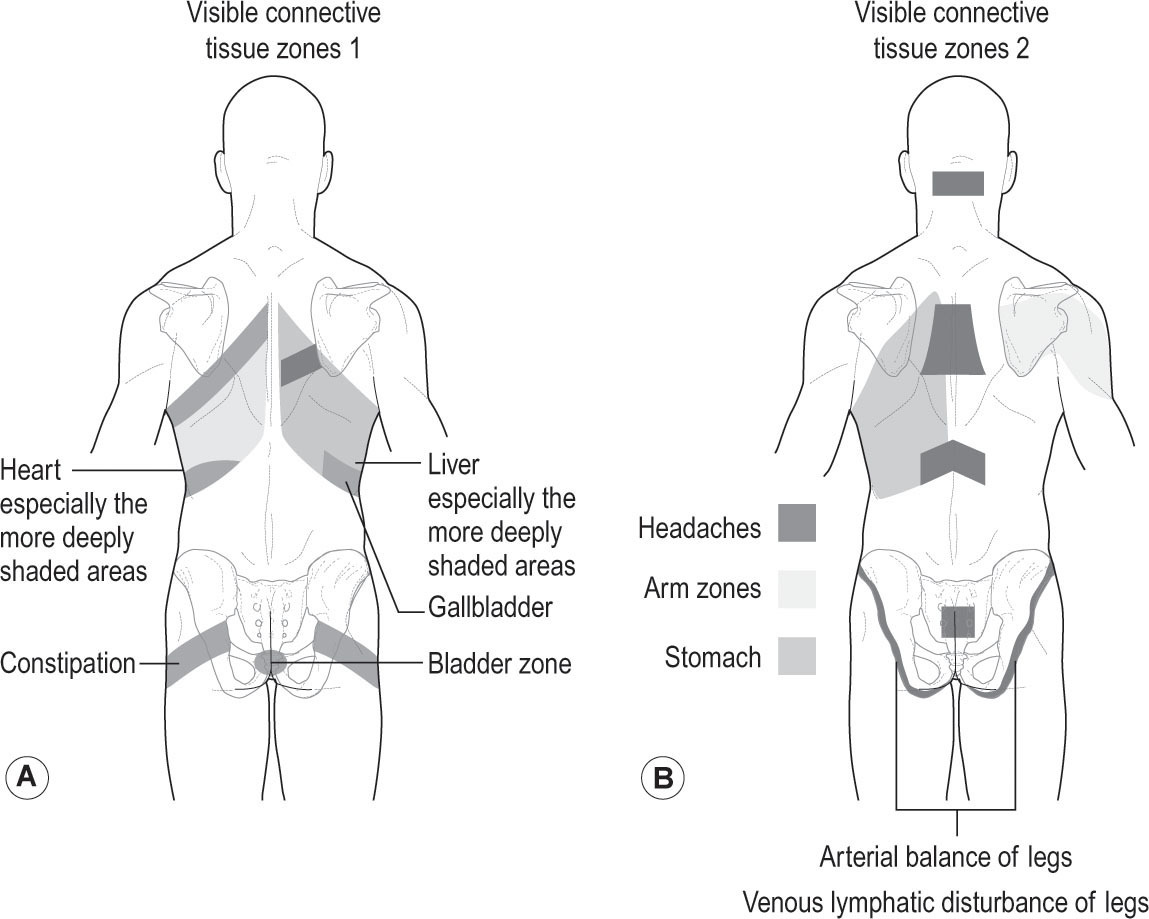
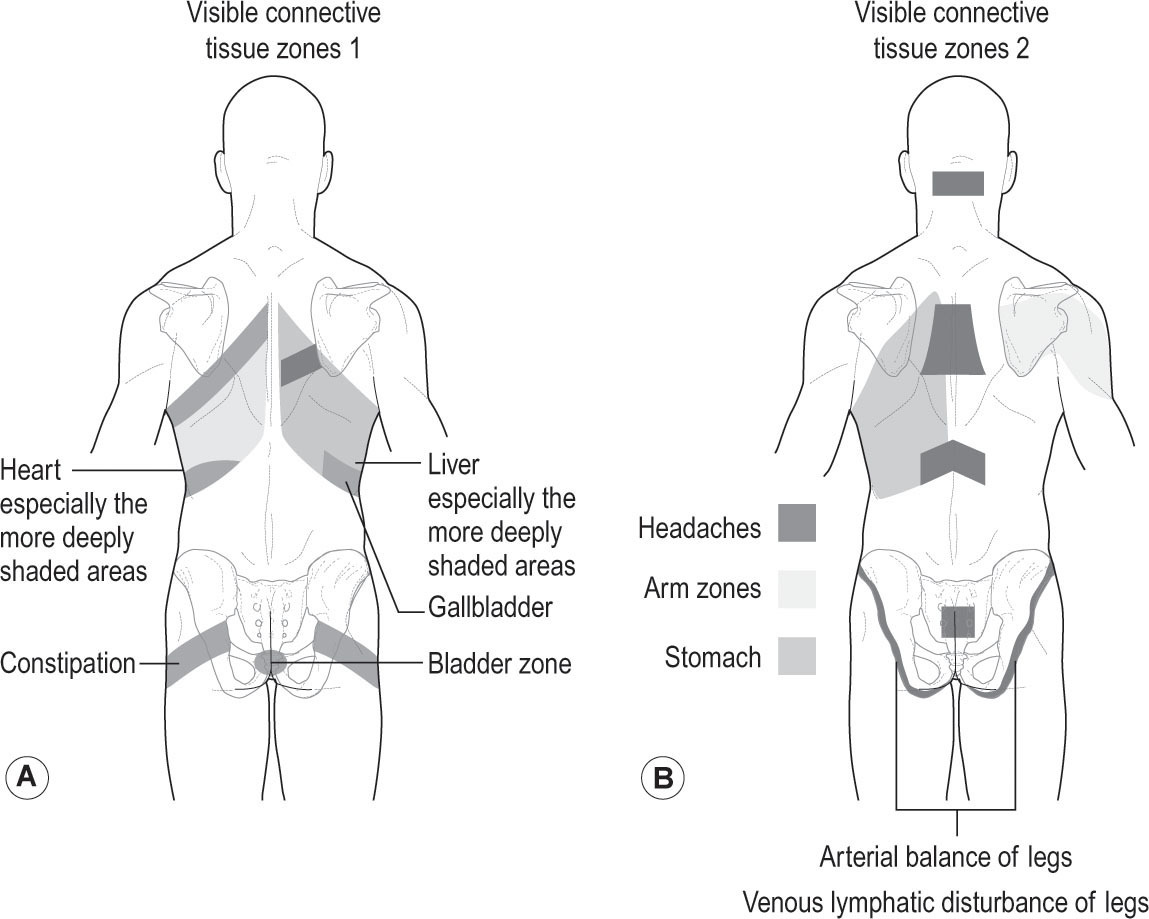
CTM originated in Germany in the 1930s. The story of its discovery by Elisabeth Dicke in the 1930s is helpful in understanding the range of problems CTM can help. A physiotherapist, Dicke relieved her lumbar pain by using a pulling and stretching technique on the soft tissues of her back. During this massage, she found that the tissues over her buttock area had become tight and thickened and as they released, the circulation improved to her leg. This had a dramatic consequence in that the amputation she had been waiting for, due to a severe arterial condition, was no longer required. The buttock area coincided with Head’s arterial (lower limb) zone. Dicke continued the treatment with the help of a colleague. As they continued the technique in other areas where the tissues were felt to be similarly affected, a stomach disorder improved. Head’s stomach zone is over the left side of the rib cage. Dicke recognized the reflex links and subsequently developed CTM as a modality (
Fig. 7.1
).
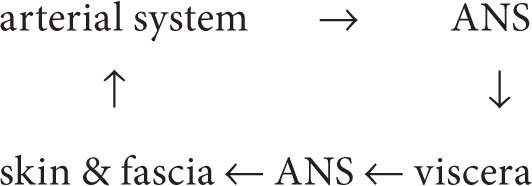
This history summarizes the clinical decision-making that is still relevant today. A seemingly musculoskeletal problem (such as Dicke’s back pain) would be assessed in the usual way. The presence of a CT zone and the potentially connected symptoms of circulatory and visceral problems would indicate that an autonomic CTM approach would be effective. The interconnectedness of these problems helps to explain the physiology of CTM. Dicke’s main problem was an arterial one. Arteries have a sympathetic nerve supply
(nervi vascularis)
. Dicke’s arterial dysfunction influenced the superficial tissues that shared the same spinal segment and they became painful. The nutritional state of the connective tissues was affected, resulting in altered fluid balance, thickenings and indurations that she could feel in her low back/buttock area, which she later identified as the arterial reflex zone. The stomach was similarly affected through its sympathetic nerve supply. Dicke demonstrated a self-perpetuating dysfunction loop connecting:
resulting in pain. All the dysfunctions in the loop improved with fascial manipulation. The cycle was broken by lowering the level of sympathetic activity, enabling balance restoration and improved function (Holey 2006).
There is some research evidence to support the proposed theoretical mechanisms underpinning CTM, but the evidence base is neither complete nor strong. CTM has been observed to have an effect on physiological measures of autonomic function. Controlled clinical studies are very limited but some evidence shows CTM can improve blood pressure, blood flow and pain (Goats & Kier 1991, Kaada & Torsteinbo 1989, Brattberg 1999).
Skin rolling can be used in a number of ways. The varying effects depend on the amount of force used and the way in which it is combined with other therapeutic tools. Where it works with the feeling of tissue tension (end-feel), its effect will progress from a relaxing technique to an autonomic reflex effect. Where it stretches beyond the end-feel, gradually increasing the tension felt by the therapist, it will have a mechanical stretching effect. The authors have called these three different applications of skin rolling grades 1, 2 and 3, respectively, for clarity within the text. There has been little scientific study on the effects of skin rolling as a separate technique to other bodywork approaches. For example, FitzGerald et al. (2009) conducted a feasibility study, which compared myofascial therapy (including a derivative of CTM) against ‘global therapeutic massage’ in male and female patients who were suffering from chronic pelvic pain (possibly involving symptoms including interstitial cystitis, painful
bladder syndrome), and reported results which warrant further study. In addition to the feasibility results, there were some positive clinical results in both groups, the myofascial group being slightly better, but inferences in relation to effectiveness of skin rolling or CTM are very limited.
Objectives
The problems likely to respond positively will fit into four categories:
1.
Visceral problems such as chronic postoperative pain. CTM can be used to reduce sympathetic overactivity and therefore pain (Holey 2000).
2.
Hormonal problems such as pre-menstrual syndrome or menopausal symptoms. CTM is used supra-segmentally to enhance autonomic imbalance and reduce symptoms (Holey 2000).
3.
Pain manifesting as musculoskeletal pain. This may be local and mechanical, such as chronic low back pain or intractable nerve root pain, but it may be secondary to a visceral ‘event’ such as surgery and is a result of sympathetic irritation through the spinal segment or zonal changes. Shin splints/anterior compartment syndrome, which shows tight fascia and altered circulation, responds well to CTM. Thickened, adherent (not keloid) or painful scars can respond very well to skin rolling (Fourie 2012). Pain caused by postural imbalance or movement dysfunction, thought to be due to tightening along the fascial train, can be helped by grade 3 skin rolling.
4.
Autonomic imbalance shown by fatigue (parasympathetic) or irritability, sleeplessness (sympathetic) that is not caused by other medical problems. Myofascial therapy practitioners will use grade 3 skin rolling in these cases (Andrade 2013).
CTM is most effective where there is autonomic imbalance contributing to symptoms and this is more certain when the symptoms fit into three or four of the categories above.
The aims of treatment are to:
•
Reduce pain – through post-synaptic inhibition of pain impulses
•
Increase circulation – by enhanced sympathetic stimulation to blood vessels
•
Normalize the tissues in zonal areas and in connected dermatomes by reducing tension and swelling, and stretching tissues at the interfaces
•
Balancing the sympathetic and parasympathetic components of the ANS.
The therapist must have the ability to distinguish these symptoms from the same ones that, in a different pattern, result from conditions requiring medical attention. This is possible through an in-depth understanding of pathophysiology, patient examination and clinical reasoning.
Skin rolling is a versatile technique that can be included within a variety of therapeutic approaches. Within massage, it is a soothing and relaxing grade 1 stroke. It can be used at grade 2 by myofascial therapists, bodyworkers and trigger point therapists as part of a range of strokes that are aimed at loosening and stretching tightened fascia and thereby potentially influencing the whole of the fascial network. When it pushes into grade 3, it stimulates the ANS.
Assessment
Assessment should follow the approach normally taken by the individual therapist. In patients presenting for physical therapy, osteopathy or chiropractic, for example, the pain and dysfunction presented will often appear to have a musculoskeletal component. CTM ‘cues’ should be listened for during the subjective
assessment, which should include questions eliciting the extent of autonomic imbalance. Pain that does not follow a dermatomal distribution or worsens during menstruation or bouts of constipation is an indicator, as is paresthesia –
burning, tingling or a sensation of crawling or water running under the skin, which is reproduced when palpating thickened tissues around the sacrum. Other signs of autonomic imbalance include an inability to sleep and relax. The balance between fluid input and output may be inadequate as when a patient drinks copious amounts of coffee but only empties the bladder twice in a whole day and has ‘puffy’ ankles. The symptoms may have started following a ‘visceral event’ such as a kidney infection or surgery.
During the objective assessment, in addition to the usual tests, the recognition of skin and subcutaneous tissue changes in CT zones (Holey & Watson 1995) signal autonomic dysfunction and are used to confirm the subjective impression that autonomic imbalance is contributing significantly to the patient’s symptoms. They are most easily observed on the back. The patient should sit with the back exposed down to the coccyx, with ankles, knees and hips flexed to 90° and fully supported. The lumbar spine should be slightly extended but not hyperextended, to place the connective tissues under comfortable tension. The tissue changes will become apparent when, after approximately 30 seconds, the tissues have adjusted against gravity. Chronic fascial tension is seen as an in-drawn area, surrounded by tissue fluid. More acute changes tend to show in superficial swellings.
The symptoms described by the patient should be linked with potential causative factors in the history and the relevant active zones to gain an understanding of how the pain, stiffness, autonomic disturbance and CT changes have created and perpetuate each other. This will inform a reasoned treatment plan.
Mechanisms
The theoretical model of physiological mechanisms underpinning CTM
CTM produces both mechanical and reflex effects, but is understood to work by mechanisms that are distinct from traditional massage techniques. Whilst CTM produces an immediate local response of swelling, it seems that the main mechanisms of action are neurophysiological via the ANS, which is stimulated at the fascial interfaces.
It is believed that when problems or imbalances in the CT zones occur, they change the discharge frequency of neurons. Other cells in the spinal cord are chemically alerted and the synapse becomes ‘irritated’ and its transmission threshold becomes lowered. The ANS responds with a heightened state of activity which spills over throughout the spinal segment. This corresponds to the osteopathic ‘facilitated segment’ concept. CTM is proposed to normalize any tonic imbalance in parasympathetic and sympathetic activity, usually to increase parasympathetic and decrease sympathetic output (for which there is some evidence, see below).
CTM is understood to elicit a shear force at the connective tissue interfaces between skin and fascia. The precise mechanisms of action have not been
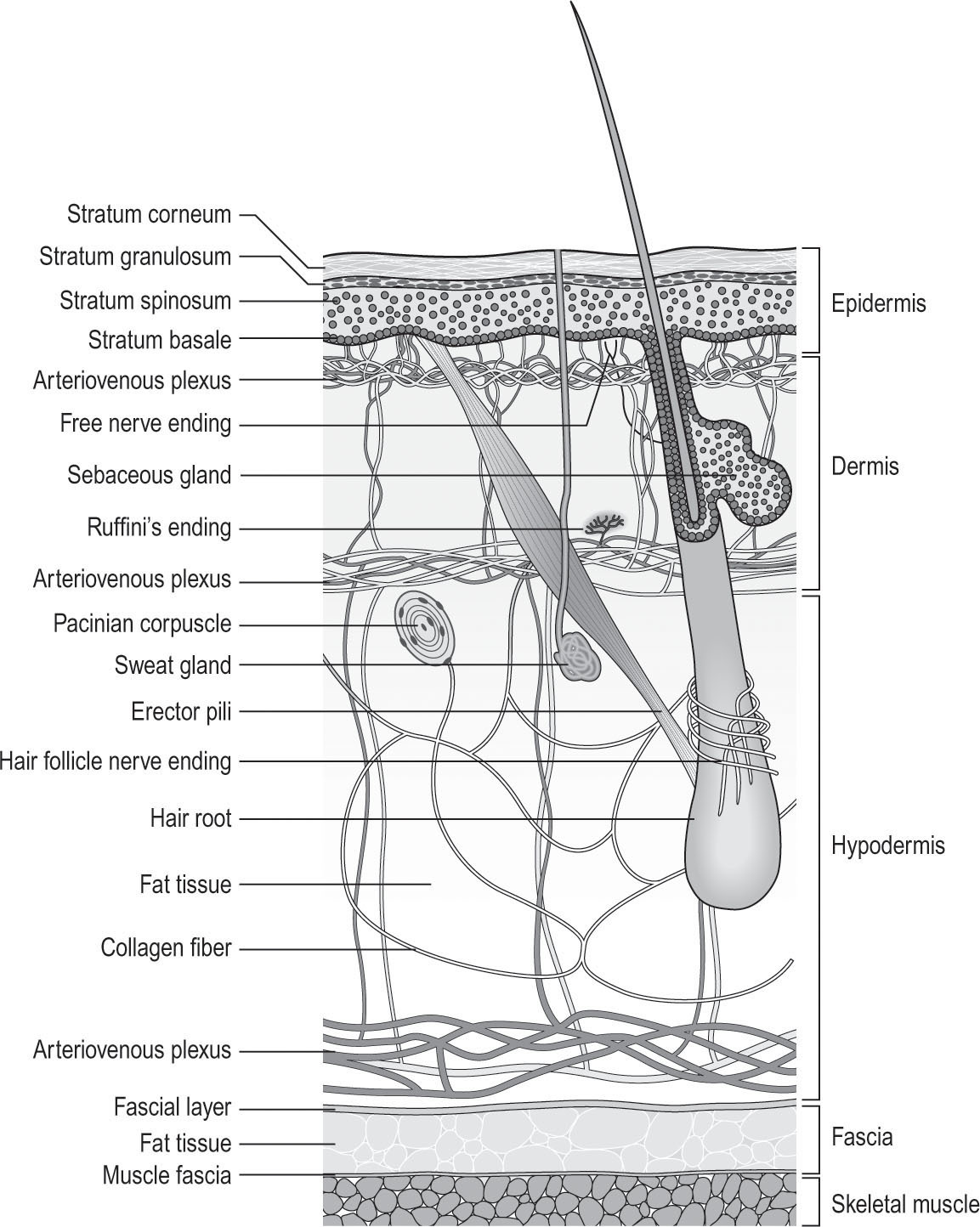
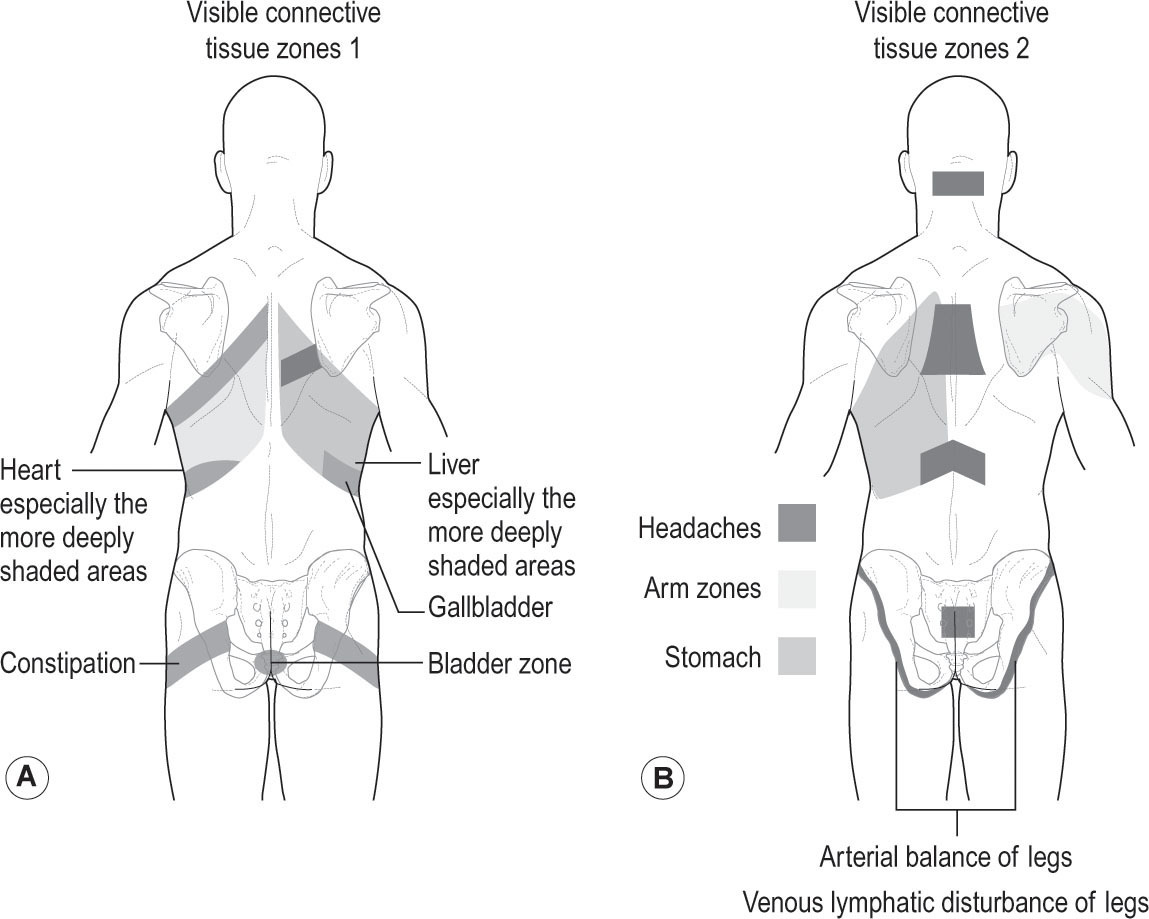
clarified; it should be noted that well-controlled studies in the area are few in number, and much of the detailed theory needs further evidence. It is important that skin/fascial interfaces are targeted accurately to achieve the precise effects of CTM as distinguished from other soft-tissue modalities. This is because these interfaces contain vascular plexi of blood vessels that are innervated by autonomic nerve endings (Holey 2000). Fascia itself is similarly well innervated (Simmonds et al. 2012). The precise detail of the site(s) of stimulation is lacking, and the theoretical model has changed slightly over the years but it is believed that the shear force of CTM stimulates cutaneovisceral reflexes via the nerve endings which surround the horizontal circulatory plexi, which in turn elicits a strong effect on the ANS (
Fig. 7.2
). It has been proposed that the primary mechanism is via the sympathetic nervous system at vascular plexi, as most blood vessels have only sympathetic innervation. However, with our increasing knowledge of fascia, and with the awareness that the ANS receives input from various somatosensory afferents, it may be a broader set of receptors that are stimulated, including, for example, fascial or cutaneous mechanoreceptors.
Wherever the precise stimulus occurs, CTM seems to produce effects both general and segmental. The general (or supra-segmental) effect produces a more
evenly balanced autonomic system, with feelings of relaxation, improved energy and sleep patterns. This may have some similarities with traditional massage, but the more potent effect of CTM also may be due to the release of endorphins. The segmental effect is believed to be a key factor in clinical treatment. It gives an improved functioning of tissues linked by the same spinal segment of the reflex zone under treatment. This can be seen as enhanced hydration and texture of the skin, increased circulation, better muscle tone and visceral function. Alongside this, pain improves and there is lowered tissue stiffness, which, as Pohl (2010) speculates based on viewing ultrasound scans after manipulating the skin, could be partially due to a wider distribution of tissue fluid in the dermis with relaxation of skin fibroblasts.
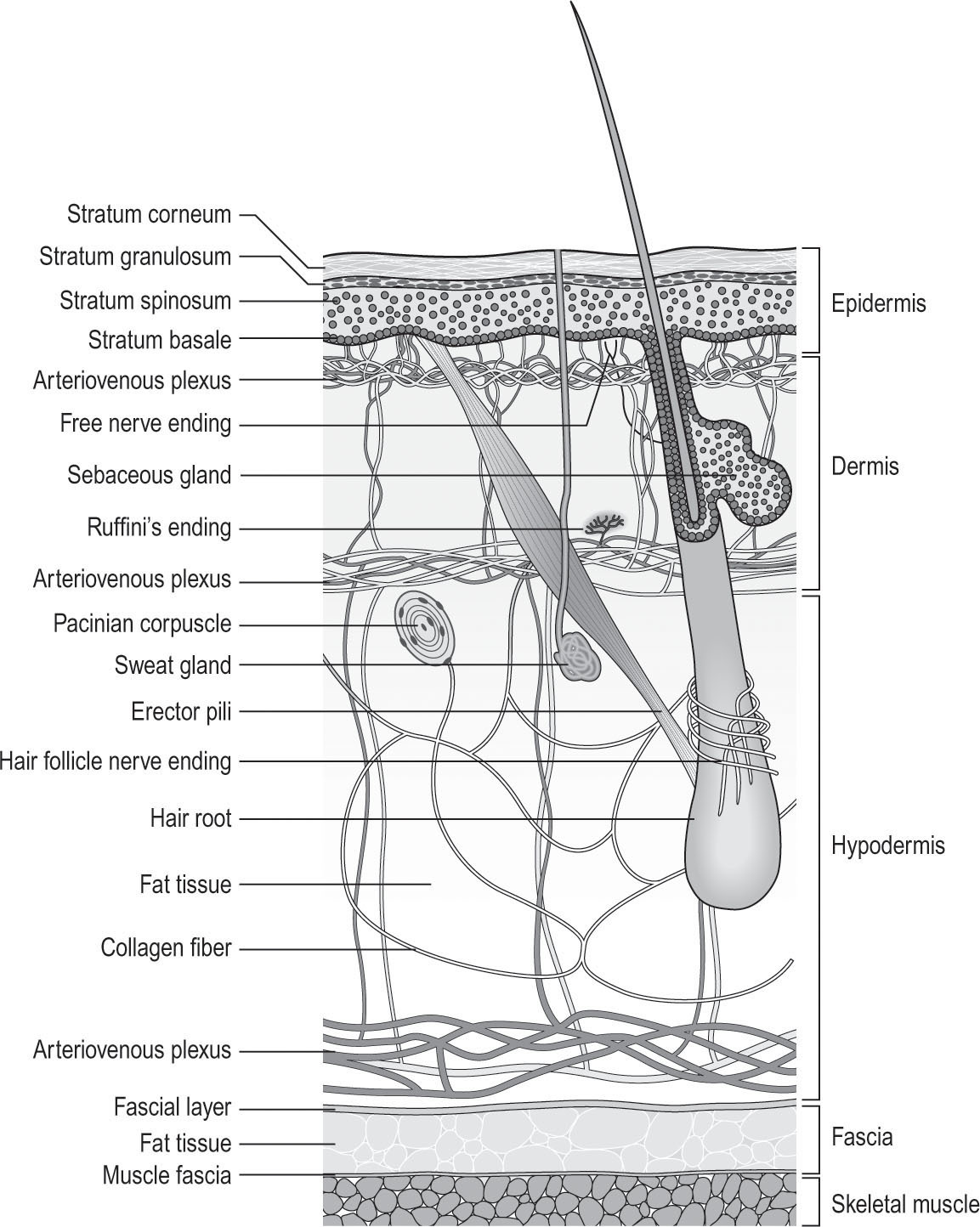
Figure 7.2
Layers of the skin and circulatory plexi. Adapted from Holey & Cook 1995, originally published in Schuh 1992.
Evidence for the proposed mechanisms and effects of CTM
There is not a large volume of high quality scientific evidence for the proposed mechanisms
of CTM. Some studies have shown measurable physiological responses in autonomic function from CTM.
•
Holey et al. (2011) observed an immediate moderate increase in diastolic (but not systolic) blood pressure in healthy women after a single CTM session. No change in heart rate or foot temperature was seen.
•
Kisner and Taslitz (1968) also showed that CTM increased sympathetic activity, with the effect seemingly on diastolic blood pressure.
•
In contrast, Reed and Held (1988) found no effects in healthy people.
•
Horstkotte et al. (1967) investigated the effect of CTM in men with occlusive arterial disease. The group (n=18) receiving CTM showed an immediate reduction in peripheral blood flow followed by an increase after 2 weeks.
•
Thirty minutes of CTM in people with various types of pain caused moderate increases in levels of plasma beta-endorphins, but not in the vasodilator vasoactive intestinal polypeptide (Kaada & Torsteinbo 1989).
Regarding the different types of CTM strokes, there is evidence of a physiological difference in the effects of the fascial and the preparatory flashige techniques (see Protocol
below). Holey et al. (2011) report that the fascial technique produces an observable reddening of the skin and an increase in skin temperature, from 15 minutes after treatment, lasting at least an hour (the end of data collection). This was not observed with the flashige technique (see below).
As some of the studies of CTM on the ANS have been carried out on healthy participants, it must be remembered that if CTM is proposed to rebalance the ANS, then little effect may be expected in healthy people and greater responses may occur in clinical groups. Much more research is needed to determine the detailed mechanisms of CTM.
Regarding the
clinical effects
of CTM in patient groups, good scientific evidence is rare. This is because the majority of published CTM clinical studies are limited in either applying CTM alongside another treatment or in being uncontrolled or case studies. Combined studies add little to the evidence base for CTM; inferences cannot be made about the actual CTM effect. Uncontrolled studies have various potential problems such as placebo effects. Apart from two promising pilot studies (Bakar et al. 2014, Joseph et al. 2016), the authors currently know of only three controlled studies of CTM from which inferences can be made about clinically relevant outcome measures in patient groups.
•
A high quality study, in which 98 people with type 2 diabetes and peripheral arterial disease were randomized to receive CTM or a placebo control for 15 weeks, was carried out by Castro-Sanchez et al. (2011). They found the CTM group displayed significant improvements in various
outcomes such as differential segmental blood pressure, blood flow, temperature and oxygen saturation at the foot, and walking distance scores. The improvements in most measures were still observed after a year.
•
A trial of 34 lower limb amputees with Buerger’s disease by Ülger et al. (2002) randomized participants to three groups: CTM; interferential therapy; or control (all groups received the control intervention of exercise and prosthetic training). Although no between-group statistical comparisons were carried out, the reduction in pain was significant in all three groups, but of a lower magnitude in the control group.
•
In a randomized trial of the effect of 10 weeks of CTM in 48 people with fibromyalgia (Brattberg 1999), it was reported that current pain was significantly better in the CTM group (but average pain did not differ between groups) as was quality of life as measured by the Fibrositis Impact Questionnaire. Hospital Anxiety and Depression Scale scores also showed a trend for a difference between the groups.
Overall, the evidence base for the proposed mechanisms and effects of CTM is small and further research would be welcomed.
Protocol
The contraindications to CTM are: acute inflammation; active infection; malignancy; unstable blood pressure/heart conditions; haemorrhage; early or late stage pregnancy (some prefer not to treat pregnant women at all); where a resultant heavy menstrual flow would be unacceptable to the patient; and use of anxiolytic drugs.
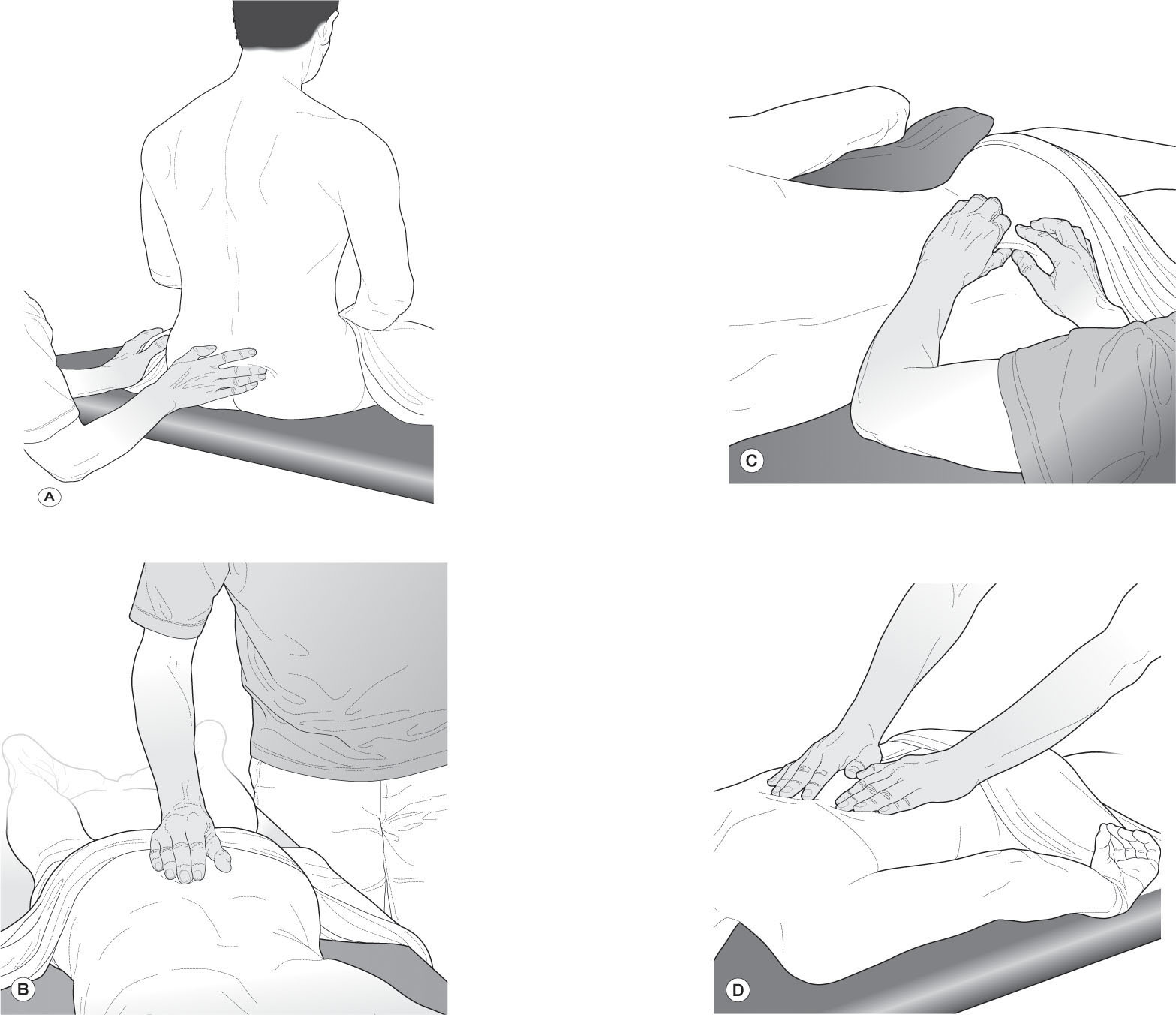
The fascial stroke is easiest if the patient is sitting, as described above. The preparatory strokes can be applied with the patient side-lying. The therapist sits behind.
The therapist should choose from three preparatory strokes:
•
Skin (haut) technique (
Fig. 7.3B
)
– a rapid, light brushing with the fingertips to reduce skin tenderness.
•
Flat/shallow (flashige) technique (
Fig. 7.3C
)
– like the fascial stroke at the fascial interface, to but not beyond the end-feel. It is recommended that this is carried out prior to fascial strokes, but not usually in the same treatment.
•
Subcutaneous (unterhaut) technique (
Fig. 7.3D
)
– a light pushing of the skin layers on the fascia, not quite to the end-feel. This reduces tension in the skin and ensures that subsequent attempts to access the fascial layer are achievable and comfortable to the patient.
The preparatory strokes may be performed for the first two or more sessions, if necessary.
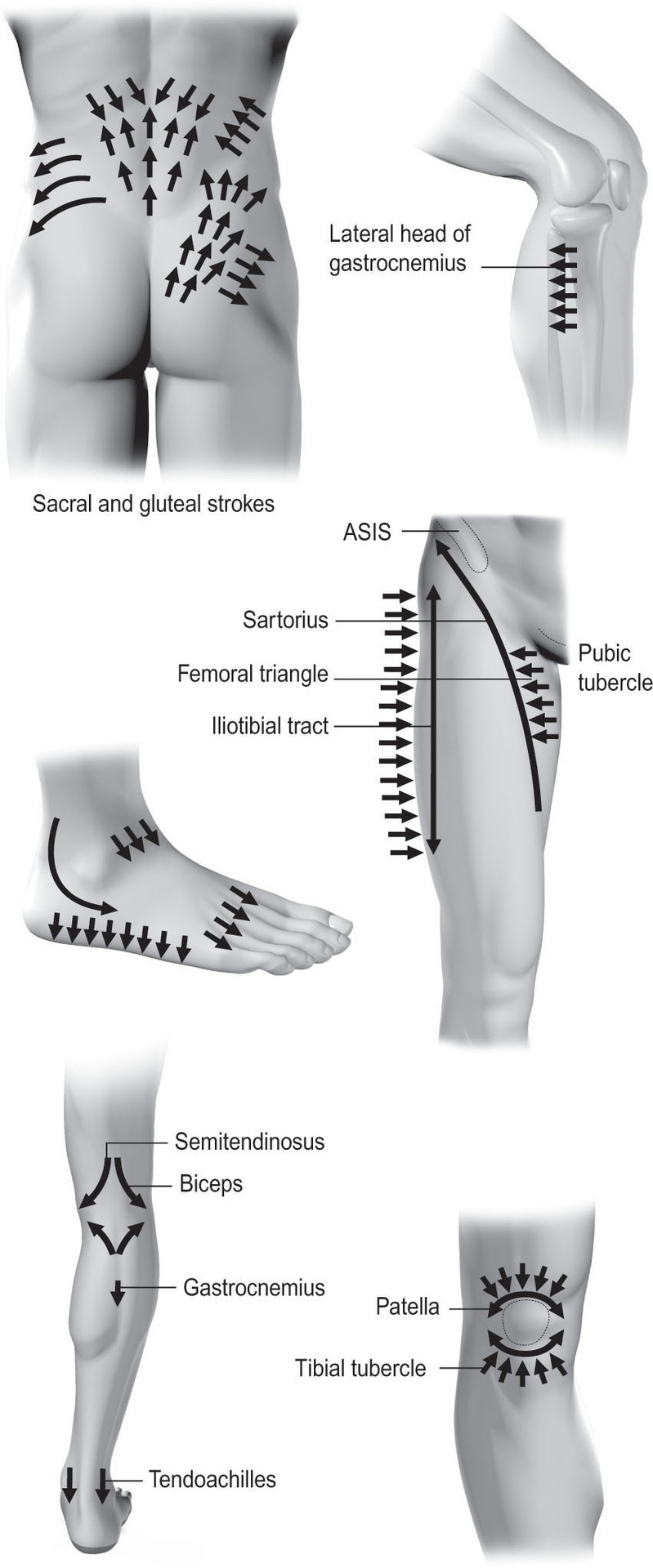
The pad of the middle finger (or the thumb if the patient is side-lying) makes contact with the skin and the distal interphalangeal joint is flexed until the fingertip, but not the nail, is on the skin and the tension in the skin layers is gathered up. Tension is felt at the skin–fascial interface. The therapist then slowly and gently lifts the tissues against gravity into the end-feel but not sufficiently to cause pain. After a pause, the tissue is released. Each stroke is repeated up to six times. The strokes follow the prescribed pattern known to access the fascia in superficial places (
Fig. 7.4
). The ‘basic section’ is always treated first, to avoid overstimulating the sympathetic nervous system. This is the section from the coccyx tip to the lower costal margin. With many patients, the symptoms resolve without leaving this area, otherwise progression is in following the affected zones or, in the case of limb symptoms (such as chronic nerve root pain), the dermatomes.
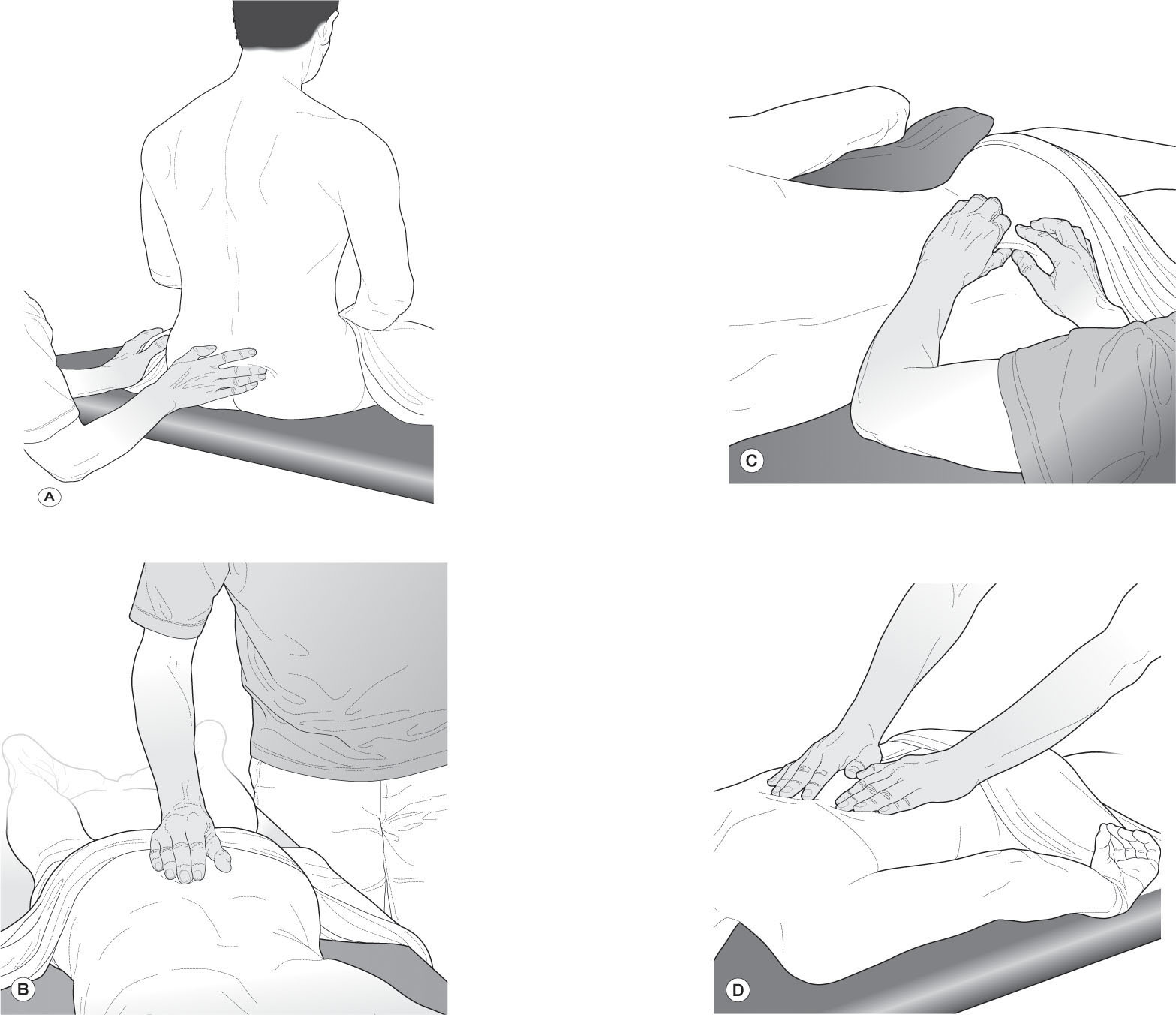
Figure 7.3
The four strokes of CTM.
The principles of treatment are:
1.
The skin must be displaced in relation to the underlying layer.
This creates a shear force at the tissue interface which stimulates mechanoreceptors. It also activates mast cell secretion, including histamine, nitric oxide, vasoactive intestinal polypeptide (a vasodilator) and heparin. The CTM fascial stroke should produce a triple response reaction of reddening and swelling in a line (wheal) as these cells are present in large numbers around blood vessels (Theoharides et al. 2010). Inaccurate or excessive strokes will produce skin irritation and discomfort.
2.
Work caudad to cephalad.
Treatment should start at the apex of the sacrum, to reduce potential unwanted reactions, which, if the principles are not followed, can include dizziness and sweating, fainting, extreme tiredness or irritability and restlessness. These effects are often delayed and uncontrolled, so must be avoided. They are most likely to happen if the skin is over dense, sympathetically supplied areas (such as between the scapulae). To desensitize the skin area, which is reflexively linked to the parasympathetic nervous system, the ‘bladder zone’ (as the bladder has a parasympathetic nerve supply) should be treated first. This reduces sympathetic activity.
Figure 7.4
The pattern of CTM strokes, based on work by E. Dicke and H. Tierich-Leube.
3.
Work superficial to deep.
A shear force is applied to the interface between the deep fascia, the target tissue, and the skin, to create a potent autonomic effect. The treatment will be painful where edema is in superficial fascia and skin, or there is excess skin tension. Pain increases sympathetic activity so will undermine achievement of the intended outcomes. Adverse reactions are avoided by use of preparatory strokes which remove tissue fluid and tension.
4.
Target appropriate tissue interfaces to stimulate the fascia.
As well as using recommended stroke patterns, which correlate to places where the deep fascia lies superficially under the skin, the correct tissue interface should be targeted, to reduce the possibility of unwanted reactions and making the treatment as effective as possible. Stimulation of the deep fascia is recognized when a non-painful sharp or ‘cutting’ sensation is felt by the patient.
As the effects are delayed, progress is not normally seen immediately after treatment, so thorough evaluation at the next session is vital. For this reason, treatments are best spaced over 3 consecutive days until the sensitivity of response is understood by the therapist. Thereafter, twice weekly is acceptable although beneficial results have been seen by the author on once-weekly treatments over 6 weeks. Positive effects should be apparent by the third treatment otherwise the treatment should be stopped. Sessions should stop when improvement reaches a plateau and this will vary between individuals.
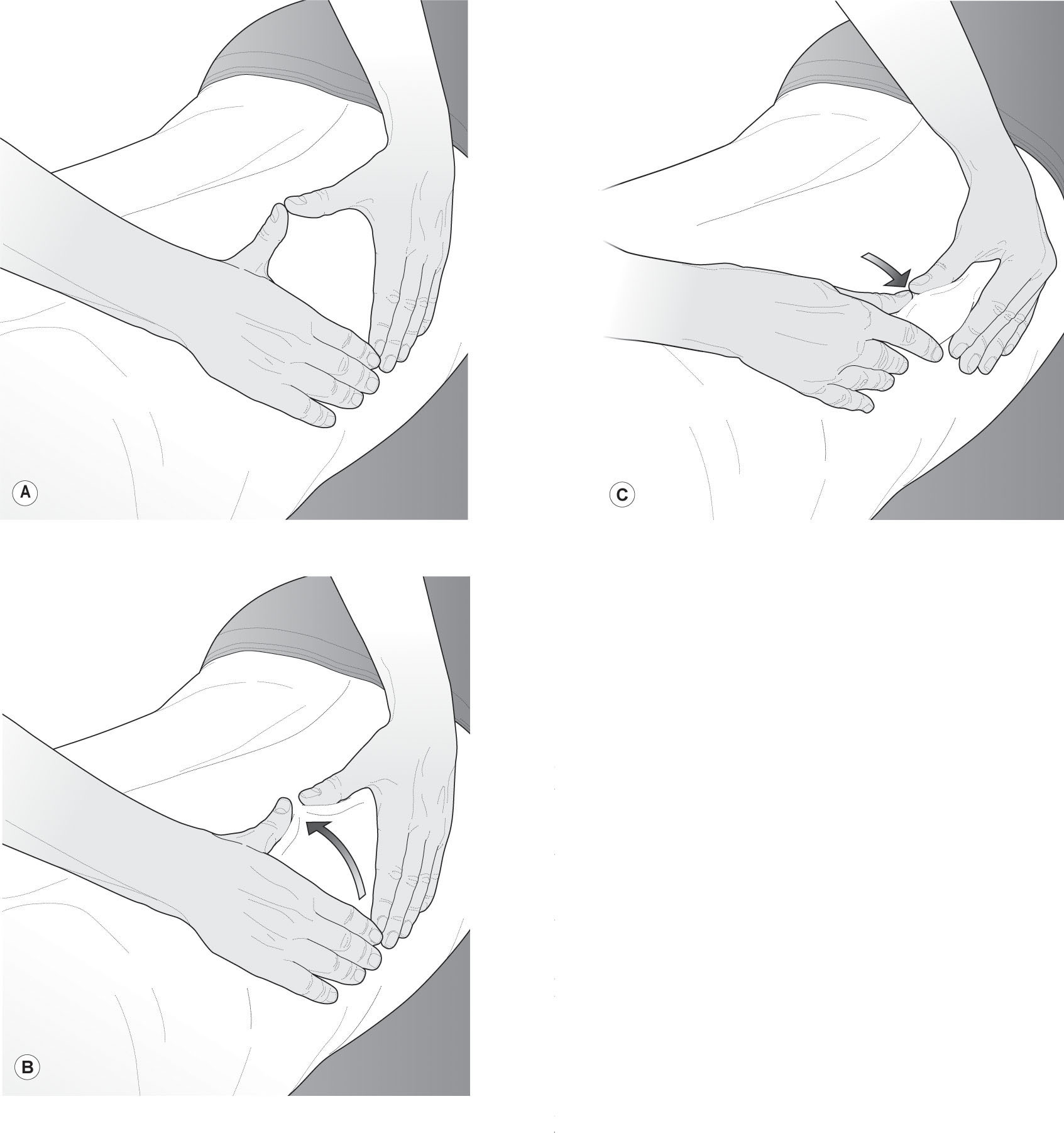
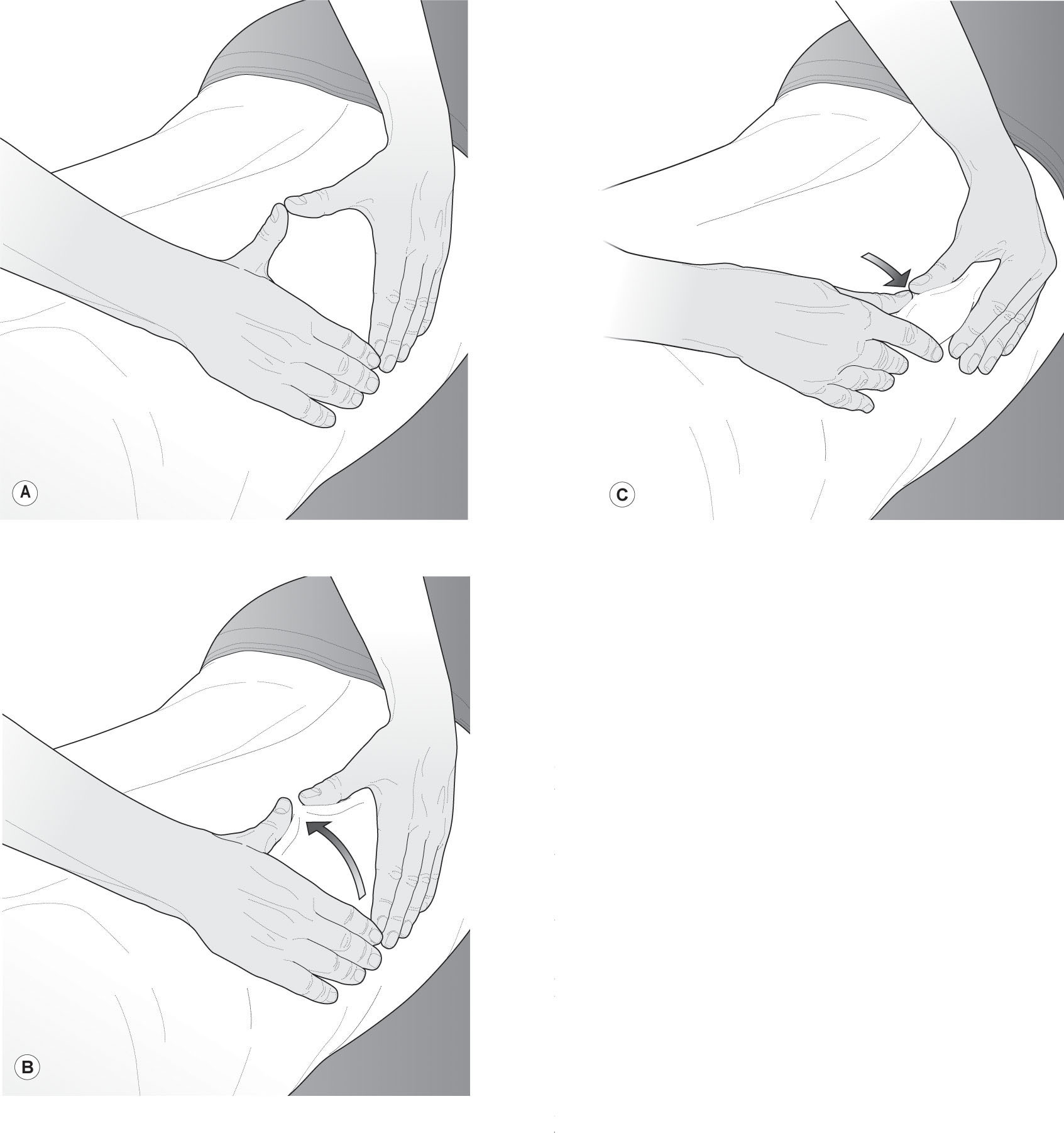
The therapist places her hands on the skin with the thumbs abducted and the fingers adducted, forming a kite-shaped space between the index fingers and thumbs. Contact is made with the skin and the fingers pulled towards the thumbs, bringing a roll of tissue with them. This tissue can contain skin or muscle. The fingers relax their pressure, allowing the thumbs to gently push the tissue roll forward, avoiding pinching the tissues. By the time the thumb tips have met the index fingers, the roll has virtually disappeared (Holey & Cook 2011). Keeping the thumbs in contact with the skin, the fingers lift and are replaced along the aspect being treated, so the hands ‘roll and walk, roll and walk’.
The direction of roll varies with the underlying anatomy, against the tension lines, to maximize the mobility of the skin. Muscle and tendons can also be rolled in this manner. A grade 1 skin roll will roll the layers of skin on each other in a gentle technique. Grade 2 will go deeper into the tissues, and roll the skin loosely on the fascial layer. Grade 3 will roll into the end-feel at the interface between the skin and fascia and care must be taken not to push into pain. The therapist must be aware of potential autonomic effects. To roll muscle, the muscle belly is grasped, beyond the
depth of the fascia. This is a deep technique and less mobility will normally be expected.
Progression of treatment is dictated by the symptoms, but the stroke can be applied across adherent scars, moved around an area of tightness or recovering injury or over the whole of the skin in a relaxing massage.
Effects on the fascia
These techniques rely on accurately targeting the interface between the tissue layers and the fascial stroke of CTM and grade 3 skin rolling will primarily influence the ANS. The patient describes a feeling of looseness – for example, being able to bend more easily the next day, which could be a result of increasing circulation at the interface. The effects on the fascia itself by these techniques are not proven, but the theories include:
•
A stretch in one part of the fascial network may influence other parts of the fascial network, along fascial ‘trains’, which describe pathways of force transmission (Myers 2009).
•
The biotensegrity model whereby altering the tension in one part of the fascial network improves force transmission and improves movement (Levin & Martin 2012).
•
The mechanostimulatory effects on the fascial myofibroblasts may impact positively on tissue stiffness. The enhanced circulation caused by stimulation at the horizontal circulatory plexus at the fascial-skin interface may have an anti-inflammatory effect on the myofibroblasts, reducing fascial tone (Schleip et al. 2012).
•
Shear forces on the blood vessel wall are known to release nitric oxide (NO) and it has been suggested that NO also may relax myofibroblasts (Schleip et al. 2012).
•
The cytokine TGF-β1, a myofibroblast stimulator, is increased by sympathetic stimulation. CTM balances the ANS in a parasympathetic direction, so it is possible that as it reduces sympathetic activity, this reduces levels of TGF-β1 (see
Ch. 1
), which in turn reduces fascial contractility and creates a feeling of looseness in the fascia (Bhowmick et al. 2009).
Exercise: CT zone recognition
Ask your model/patient to sit as for a CT assessment (see
Fig. 7.3A
) in a very good light.
Support feet so the hips and knees are at 90°.
Observe:
look at the contours of the body surface, thinking about the underlying muscles. Take those into account when you observe any in-drawn areas of tissue, subtle swellings (puffiness), skin folds.
Palpate:
place the flat of your fingertips on the skin and move the skin on the underlying fascial layer, pushing upwards against gravity until you feel the fascial tension. Note any discrepancies between the right and left sides. Look at the fold of skin above your fingers – is it the same on both sides? Look at the tension gathered up below your fingers – does it stop where you expect the restrictions of bone to be or is it within the skin itself?
Now gather a roll of skin between your fingertips and thumb and gently roll upwards on either side of the spine. Do areas where the roll starts to be lost due to underlying tension match your previous findings? Can you see any parts of the skin having an ‘orange peel’ appearance?
Now very gently tap any apparent puffy areas. Can you observe tiny ripples of fluid in the skin?
Compare your findings with the Head CT zones map (see
Fig. 7.1
) and see if you can identify any zones.
References
Andrade C-K 2013 Outcome-based massage. Lippincott Williams and Wilkins, Philadelphia
Bakar Y, Sertel M, Öztürk A et al 2014 Connective tissue massage on pressure pain threshold and muscle relaxation response in women with chronic neck pain: a preliminary study. J Manipulative Physiol Ther 37(6):415–421
Brattberg G 1999 Connective tissue massage in the treatment of fibromyalgia. Eur J Pain 3:235–244
Bhowmick S, Singh A, Flavell RA et al 2009 The sympathetic nervous system modulates CD4(+)FoxP3(+) regulatory T cells via a TGF-beta-dependant mechanism. J Leukocyte Biol 86:1275–1283
Castro-Sanchez AM et al 2011 Connective tissue reflex massage for type 2 diabetic patients with peripheral arterial disease: randomized controlled trial. Evid Based Complement Alternat Med (eCAM) 8:1–12
FitzGerald MP, Anderson RU, Potts J et al 2009 Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J Urol 182:570–580
Fourie W 2012 Surgery and scarring. In: Schleip et al (eds) Fascia: the tensional network of the human body. Churchill Livingstone Elsevier, Edinburgh
Goats GC, Kier KA 1991 Connective tissue massage. Br J Sports Med 25:131–133
Head H 1898 ‘Die Sensibilitaetsstoerungen der Haut bei Viszeral Erkrankungen.’ Berlin. Cited in: Bischoff I, Elminger G 1963 ‘Connective tissue massage’ in Licht S (ed) Massage, manipulation and traction. Waverley Press, Baltimore, pp 57–83
Holey LA 1995 Connective tissue manipulation: towards a scientific rationale. Physiotherapy 81:730–739
Holey EA 2000 Connective tissue massage: a bridge between complementary and orthodox approaches. J Bodyw Mov Ther 4:72–80
Holey EA 2006 Connective-tissue manipulations. In: Carriere B, Feldt CM (eds) The pelvic floor. Georg Thieme Verlag, Stuttgart
Holey LA, Watson M 1995 Inter-rater reliability of connective tissue zone recognition. Physiotherapy 81:369–372
Holey E, Cook E 2011 Evidence-based therapeutic massage. A practical guide for therapists, 3rd edn. Churchill Livingstone Elsevier, Edinburgh
Holey LA, Dixon J, Selfe J 2011 An exploratory thermographic investigation of the effects of connective tissue massage on autonomic function. J Manipulative Physiol Ther 34:457–462
Horstkotte W, Klempien EJ, Scheppokat KD 1967 Skin temperature and blood flow changes in occlusive arterial disease under physiological and pharmacological therapy. Angiology 18:1–5
Joseph LH, Paungmali A, Dixon J et al 2016 Therapeutic effects of connective tissue manipulation on wound healing and bacterial colonization count among patients with diabetic foot ulcer. J Bodyw Mov Ther 20(3):650–658
Kaada B, Torsteinbo O 1989 Increase of plasma beta-endorphins in connective tissue massage. General Pharmacology 20:487–489
Kisner CD, Taslitz N 1968 Connective tissue massage: influence of the introductory treatment on autonomic functions. Phys Ther 48:107–119
Levin SM, Martin D-C 2012 Biotensegrity – the mechanics of fascia. In: Schleip et al (eds) Fascia: the tensional network of the human body. Churchill Livingstone Elsevier, Edinburgh
Myers T 2009 Anatomy Trains, 2nd edn. Churchill Livingstone Elsevier, Edinburgh
Pohl H 2010 Changes in the structure of collagen distribution in the skin caused by a manual technique. J Bodyw Mov Ther 14: 27–34
Reed BV, Held JM 1988 Effects of sequential connective tissue massage on autonomic nervous system of middle-aged and elderly adults. Phys Ther 68:1231–1234
Schuh I 1992 Bindegewebsmassage. Fischer-Verlag, Stuttgart
Schleip R, Jager H, Klinger W 2012 Fascia is alive. In: Schleip et al (eds) Fascia: the tensional network of the human body. Churchill Livingstone Elsevier, Edinburgh
Simmonds N, Miller P, Gemmell H 2012 A theoretical framework for the role of fascia in manual therapy. J Bodyw Mov Ther 16(1):83–93
Theoharides TC et al 2010 Mast cells and inflammation. Biochim Biophys Acta 1822(1):21–33
Ülger OG, Yigiter K, Sener G 2002 The effect of physiotherapy approaches on the pain patterns of amputees for Buerger’s disease. Pain Clinic 14:217–221

Pain and parasthesia in a non-dermatomal pattern
Pain and parasthesia in a non-dermatomal pattern

Autonomic skin changes apparent in the region of pain
Autonomic skin changes apparent in the region of pain

Symptoms worsen when constipated or menstruating
Symptoms worsen when constipated or menstruating

Symptoms started shortly after surgery or infection
Symptoms started shortly after surgery or infection

General autonomic imbalance – fluid balance, energy levels, outlook on life
General autonomic imbalance – fluid balance, energy levels, outlook on life

CT zones apparent: bladder, pelvic, central zones
CT zones apparent: bladder, pelvic, central zones

Symptoms resistant to usual methods of treatment
Symptoms resistant to usual methods of treatment