![]()
Straight out of the list of ‘Embarrassing things to see your GP about’, this is a presentation that patients love to hate. From a GP perspective, it’s one that is generally straightforward to deal with, and effective treatment can usually be offered immediately, much to the patient’s relief.
![]()
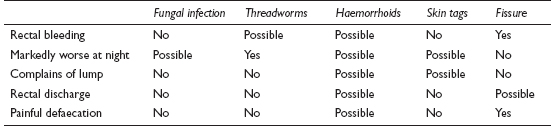
COMMON
 fungal infection – tinea, thrush
fungal infection – tinea, thrush
 threadworms
threadworms
 haemorrhoids
haemorrhoids
 perianal skin tags
perianal skin tags
 anal fissure
anal fissure
OCCASIONAL
 poor hygiene
poor hygiene
 recurrent or chronic diarrhoea
recurrent or chronic diarrhoea
 perianal warts
perianal warts
 streptococcal perianal infection in children
streptococcal perianal infection in children
 trauma from sexual practices – anal intercourse and foreign body insertion
trauma from sexual practices – anal intercourse and foreign body insertion
 faecal incontinence, including liquid faecal seepage round impacted scybala
faecal incontinence, including liquid faecal seepage round impacted scybala
 psoriasis
psoriasis
 secondary to underlying diabetes
secondary to underlying diabetes
 anorectal carcinoma
anorectal carcinoma
 chemical irritation: defaecation after a very spicy meal (commonly experienced, rarely presented in practice), bubble baths, soaps, sexual lubricants
chemical irritation: defaecation after a very spicy meal (commonly experienced, rarely presented in practice), bubble baths, soaps, sexual lubricants
RARE
 irritation from perineal decorative body piercing (the ‘Guiche’)
irritation from perineal decorative body piercing (the ‘Guiche’)
 lichen sclerosus et atrophicus (affects 1 in 100 women, 3 in 10 of these have anal symptoms)
lichen sclerosus et atrophicus (affects 1 in 100 women, 3 in 10 of these have anal symptoms)
 Crohn’s disease (anal/perianal fistula)
Crohn’s disease (anal/perianal fistula)
 rectovaginal fistula
rectovaginal fistula
 rectal prolapse
rectal prolapse
 any other cause of rectal discharge or anal swellings – see appropriate chapters
any other cause of rectal discharge or anal swellings – see appropriate chapters
 any serious cause of generalised pruritus – see chapter on anal itching. Rare here because pruritus ani is unlikely to be a presenting complaint
any serious cause of generalised pruritus – see chapter on anal itching. Rare here because pruritus ani is unlikely to be a presenting complaint
 STDs, e.g. syphilis, gonorrhoea, chlamydia
STDs, e.g. syphilis, gonorrhoea, chlamydia
![]()
![]()
LIKELY: none.
POSSIBLE: skin swab, FBC, ESR, fasting glucose or HbA1c, proctoscopy.
SMALL PRINT: none.
 In general, unless there are obvious pointers to other more serious disease, investigations would usually only follow after failure of empirical treatment.
In general, unless there are obvious pointers to other more serious disease, investigations would usually only follow after failure of empirical treatment.
 Skin swab for bacteriology may help identify local infection.
Skin swab for bacteriology may help identify local infection.
 FBC, ESR: may be helpful if Crohn’s disease is suspected, but only as an adjunct to referral as the appropriate management.
FBC, ESR: may be helpful if Crohn’s disease is suspected, but only as an adjunct to referral as the appropriate management.
 Fasting glucose or HbA1c is essential in recurrent or prolonged cases to exclude diabetes.
Fasting glucose or HbA1c is essential in recurrent or prolonged cases to exclude diabetes.
 Proctoscopy is quick to do in general practice and can yield valuable information if there is an underlying rectal cause.
Proctoscopy is quick to do in general practice and can yield valuable information if there is an underlying rectal cause.
 Most patients will have attempted self-treatment before presenting in the surgery. This may not always have been appropriate, and could have made the problem worse.
Most patients will have attempted self-treatment before presenting in the surgery. This may not always have been appropriate, and could have made the problem worse.
 Unless you are absolutely sure of an obvious cause, it is wise to perform a digital rectal examination to look for rectal causes.
Unless you are absolutely sure of an obvious cause, it is wise to perform a digital rectal examination to look for rectal causes.
 Perianal warts imply a sexually transmitted disease contact. Refer to GUM clinic for contact tracing and treatment.
Perianal warts imply a sexually transmitted disease contact. Refer to GUM clinic for contact tracing and treatment.
 Anal itching is often associated with soreness. If it precludes a rectal examination but there is no obvious primary anal cause for itching, treat symptomatically and bring the patient back to complete the assessment when more comfortable to do so. The patient is unlikely to want to return for this without understanding a clear explanation of why it is necessary.
Anal itching is often associated with soreness. If it precludes a rectal examination but there is no obvious primary anal cause for itching, treat symptomatically and bring the patient back to complete the assessment when more comfortable to do so. The patient is unlikely to want to return for this without understanding a clear explanation of why it is necessary.
 Four per cent of women with lichen sclerosus et atrophicus go on to develop vulval cancer. Refer if the vulva is affected, or if treatment fails.
Four per cent of women with lichen sclerosus et atrophicus go on to develop vulval cancer. Refer if the vulva is affected, or if treatment fails.
 Refer any suspicious anal lesion for biopsy.
Refer any suspicious anal lesion for biopsy.
 Be confident to ask about recent sexual encounters and sexual practices if possibly relevant. Sexual history may be important.
Be confident to ask about recent sexual encounters and sexual practices if possibly relevant. Sexual history may be important.
![]()
Because of embarrassment on the part of the patient, this may well present as a ‘while I’m here’ symptom. The temptation to make a diagnosis without examination should be resisted – some of the causes (such as perianal abscesses) require urgent attention and others may, rarely, provide something of a surprise (e.g. fistulae, carcinoma).
![]()
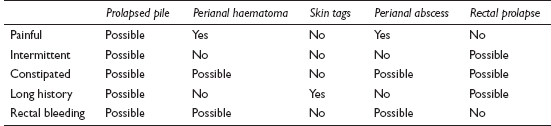
COMMON
 prolapsed pile
prolapsed pile
 perianal haematoma
perianal haematoma
 skin tags
skin tags
 perianal abscess
perianal abscess
 rectal prolapse
rectal prolapse
OCCASIONAL
 warts
warts
 sebaceous cyst
sebaceous cyst
 sentinel pile
sentinel pile
 infected pilonidal sinus
infected pilonidal sinus
RARE
 hidradenitis
hidradenitis
 anal fistula
anal fistula
 carcinoma
carcinoma
![]()
![]()
In most cases, investigation will be unnecessary. The only exceptions are warts (in which case referral to the local GUM clinic may be required to screen for sexually transmitted disease) and possible carcinoma (in which case biopsy will be performed in secondary care). Also, any suspicion of Crohn’s disease causing perianal disease would be investigated in hospital in the usual way.
 This is one of those situations in which a brief history can be taken while the patient is undressing, or during the examination. Atypically for primary care, it’s the examination, rather than the history, which usually provides the definitive diagnosis.
This is one of those situations in which a brief history can be taken while the patient is undressing, or during the examination. Atypically for primary care, it’s the examination, rather than the history, which usually provides the definitive diagnosis.
 If a discharge, as well as a lump, is mentioned by the patient, then abscesses, warts, prolapses and fistulae top the list of differentials.
If a discharge, as well as a lump, is mentioned by the patient, then abscesses, warts, prolapses and fistulae top the list of differentials.
 The patient with an anal swelling who has obvious difficulty walking into the consulting room has either an abscess, a large perianal haematoma or strangulated prolapsed piles.
The patient with an anal swelling who has obvious difficulty walking into the consulting room has either an abscess, a large perianal haematoma or strangulated prolapsed piles.

 Recurrent or multiple fistulae suggest Crohn’s disease.
Recurrent or multiple fistulae suggest Crohn’s disease.
 If a prolapsed pile is very swollen and painful, it is probably strangulated, and so requires urgent surgical attention.
If a prolapsed pile is very swollen and painful, it is probably strangulated, and so requires urgent surgical attention.
 A persistent, ulcerating anal swelling, especially in the middle-aged or elderly, requires urgent biopsy to exclude carcinoma.
A persistent, ulcerating anal swelling, especially in the middle-aged or elderly, requires urgent biopsy to exclude carcinoma.
![]()
This is usually severe and distressing. Because of reflex sphincteric spasm, constipation very often follows and increases the pain and suffering further. Adequate examination is also difficult for the same reason; fortunately if a PR exam is too difficult, a visual inspection can often yield the diagnosis.
![]()
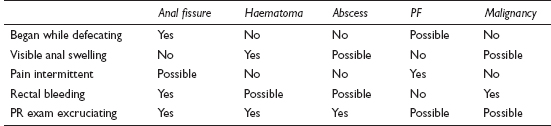
COMMON
 anal fissure
anal fissure
 thrombosed haemorrhoids/perianal haematoma
thrombosed haemorrhoids/perianal haematoma
 perianal abscess
perianal abscess
 proctalgia fugax (PF)
proctalgia fugax (PF)
 anorectal malignancy
anorectal malignancy
OCCASIONAL
 levator ani syndrome
levator ani syndrome
 Crohn’s disease
Crohn’s disease
 coccydynia
coccydynia
 descending perineum syndrome
descending perineum syndrome
 prostatitis
prostatitis
 ovarian cyst or tumour
ovarian cyst or tumour
 solitary rectal ulcer syndrome
solitary rectal ulcer syndrome
RARE
 anal tuberculosis
anal tuberculosis
 cauda equina lesion
cauda equina lesion
 endometriosis
endometriosis
 trauma
trauma
 presacral tumours
presacral tumours
![]()
![]()
LIKELY: none.
POSSIBLE: FBC, ESR/CRP, proctoscopy, faecal calprotectin.
SMALL PRINT: urinalysis, ultrasound, barium enema, other imaging.
 FBC/ESR/CRP: WCC may be raised in abscess and Crohn’s disease. ESR/CRP raised in these and carcinoma.
FBC/ESR/CRP: WCC may be raised in abscess and Crohn’s disease. ESR/CRP raised in these and carcinoma.
 Proctoscopy valuable if pain allows (specialist might also take biopsy).
Proctoscopy valuable if pain allows (specialist might also take biopsy).
 Faecal calprotectin: may help in diagnosing Crohn’s disease.
Faecal calprotectin: may help in diagnosing Crohn’s disease.
 Urinalysis: pus cells and blood may be present in prostatitis or invasive bladder tumour.
Urinalysis: pus cells and blood may be present in prostatitis or invasive bladder tumour.
 Ultrasound of pelvis if pelvic examination reveals a mass. Barium enema may be necessary to assess possible bowel involvement. In obscure cases, specialists may request other forms of imaging.
Ultrasound of pelvis if pelvic examination reveals a mass. Barium enema may be necessary to assess possible bowel involvement. In obscure cases, specialists may request other forms of imaging.
 If the patient uses dramatic language (e.g. red-hot poker) to describe fleeting pain, is otherwise well and there are no obvious abnormalities on examination, the diagnosis is likely to be proctalgia fugax.
If the patient uses dramatic language (e.g. red-hot poker) to describe fleeting pain, is otherwise well and there are no obvious abnormalities on examination, the diagnosis is likely to be proctalgia fugax.
 Examine the patient – the cause is usually a thrombosed pile, anal fissure or an abscess, and these can usually be diagnosed by simple inspection.
Examine the patient – the cause is usually a thrombosed pile, anal fissure or an abscess, and these can usually be diagnosed by simple inspection.
 Provide symptomatic relief but remember to deal with any underlying causes – especially constipation.
Provide symptomatic relief but remember to deal with any underlying causes – especially constipation.
 Don’t forget to ask about thirst and urinary frequency: recurrent abscesses may be the first presentation of diabetes.
Don’t forget to ask about thirst and urinary frequency: recurrent abscesses may be the first presentation of diabetes.
 Preceding weight loss and/or change in bowel habit should prompt a full urgent assessment with carcinoma and inflammatory bowel disease in mind.
Preceding weight loss and/or change in bowel habit should prompt a full urgent assessment with carcinoma and inflammatory bowel disease in mind.
 Some perianal abscesses do not result in external swelling. If PR exam is prohibitively painful, consider this possibility – especially if the patient is febrile.
Some perianal abscesses do not result in external swelling. If PR exam is prohibitively painful, consider this possibility – especially if the patient is febrile.
 In florid or recurrent perianal problems, think of Crohn’s disease as a possible cause.
In florid or recurrent perianal problems, think of Crohn’s disease as a possible cause.
 Remember rarer causes in intractable, constant pain in a patient with no obvious signs on PR.
Remember rarer causes in intractable, constant pain in a patient with no obvious signs on PR.
![]()
This is a very common presenting complaint and creates a lot of anxiety in the patient. By far the likeliest causes are haemorrhoids or a fissure, but more sinister pathologies should be considered according to the clinical picture. In children, constipation causing a fissure is the most frequent cause.
![]()
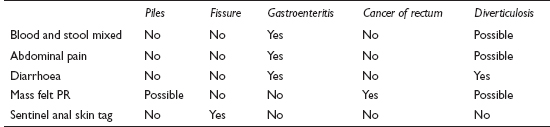
COMMON
 haemorrhoids
haemorrhoids
 anal fissure
anal fissure
 gastroenteritis
gastroenteritis
 rectal carcinoma
rectal carcinoma
 diverticular disease
diverticular disease
OCCASIONAL
 villous adenoma
villous adenoma
 trauma (especially non-accidental injury (NAI) if in children)
trauma (especially non-accidental injury (NAI) if in children)
 anticoagulant therapy
anticoagulant therapy
 inflammatory bowel disease
inflammatory bowel disease
 colonic carcinoma
colonic carcinoma
RARE
 blood clotting disorders (including anticoagulants)
blood clotting disorders (including anticoagulants)
 bowel ischaemia
bowel ischaemia
 angiodysplasia
angiodysplasia
 intussusception
intussusception
 Meckel’s diverticulum (in children)
Meckel’s diverticulum (in children)
![]()
![]()
LIKELY: proctoscopy.
POSSIBLE: FBC, ESR/CRP, LFTs, bone biochemistry, U&E, stool for microbiology and faecal calprotectin, sigmoidoscopy, colonoscopy, barium enema.
SMALL PRINT: clotting screen.
 FBC: check for anaemia from acute or chronic bleeding; low platelets may cause or aggravate bleeding.
FBC: check for anaemia from acute or chronic bleeding; low platelets may cause or aggravate bleeding.
 ESR/CRP raised in active inflammatory bowel disease and malignancy.
ESR/CRP raised in active inflammatory bowel disease and malignancy.
 If malignancy is suspected, LFT, U&E and bone biochemistry are useful early on as a baseline.
If malignancy is suspected, LFT, U&E and bone biochemistry are useful early on as a baseline.
 Clotting screen: if clotting disorder a possibility; INR if on warfarin.
Clotting screen: if clotting disorder a possibility; INR if on warfarin.
 Stool specimen: helpful in the presence of diarrhoea. May show evidence of infective cause (especially Campylobacter) or white cells in inflammatory bowel disease. Faecal calprotectin may be useful in diagnosing IBD.
Stool specimen: helpful in the presence of diarrhoea. May show evidence of infective cause (especially Campylobacter) or white cells in inflammatory bowel disease. Faecal calprotectin may be useful in diagnosing IBD.
 Proctoscopy: helpful in primary care in visualising haemorrhoids and proctitis to confirm a clinical diagnosis.
Proctoscopy: helpful in primary care in visualising haemorrhoids and proctitis to confirm a clinical diagnosis.
 Sigmoidoscopy or colonoscopy are the most helpful investigations if significant pathology is suspected, and allow biopsy of suspicious lesions.
Sigmoidoscopy or colonoscopy are the most helpful investigations if significant pathology is suspected, and allow biopsy of suspicious lesions.
 Barium enema good for revealing strictures related to the underlying pathology, but if diverticulosis present, may not rule out coexistent neoplasia.
Barium enema good for revealing strictures related to the underlying pathology, but if diverticulosis present, may not rule out coexistent neoplasia.
 Eighty per cent of rectal tumours are within fingertip range. Always do a PR examination unless, in a child or young adult, the diagnosis is manifestly obvious from the history.
Eighty per cent of rectal tumours are within fingertip range. Always do a PR examination unless, in a child or young adult, the diagnosis is manifestly obvious from the history.
 If blood is on the toilet paper and surface of the motions, the cause is likely to be palpable PR or visible on proctoscopy; if mixed in with the motions, referral for further investigation will be required to make a definite diagnosis.
If blood is on the toilet paper and surface of the motions, the cause is likely to be palpable PR or visible on proctoscopy; if mixed in with the motions, referral for further investigation will be required to make a definite diagnosis.
 In young adults, the diagnosis is usually clear from the history and is likely to be haemorrhoids or a fissure. In such cases, if and when you refer, to allay anxiety, emphasise that this is for treatment rather than investigation.
In young adults, the diagnosis is usually clear from the history and is likely to be haemorrhoids or a fissure. In such cases, if and when you refer, to allay anxiety, emphasise that this is for treatment rather than investigation.
 The presence of diarrhoea with rectal bleeding in young or middle-aged adults suggests gastroenteritis (especially Campylobacter) or colitis.
The presence of diarrhoea with rectal bleeding in young or middle-aged adults suggests gastroenteritis (especially Campylobacter) or colitis.

 Change of bowel habit and weight loss with rectal bleeding are ominous symptoms which should prompt urgent referral.
Change of bowel habit and weight loss with rectal bleeding are ominous symptoms which should prompt urgent referral.
 If a child is presented with rectal bleeding without any clear cause, consider NAI.
If a child is presented with rectal bleeding without any clear cause, consider NAI.
 The presence of haemorrhoids does not necessarily clinch the diagnosis – another lesion may be present, especially in the elderly.
The presence of haemorrhoids does not necessarily clinch the diagnosis – another lesion may be present, especially in the elderly.
 A brisk, painless haemorrhage in an elderly patient is likely to be caused by diverticular disease. Significant amounts of blood can be lost, so assess urgently with a view to admission.
A brisk, painless haemorrhage in an elderly patient is likely to be caused by diverticular disease. Significant amounts of blood can be lost, so assess urgently with a view to admission.
![]()
This unpleasant symptom causes considerable embarrassment and inconvenience. The presenting complaint may well be itching rather than a history of discharge or dampness. The most common causes are benign, but serious pathology is sufficiently likely to warrant thorough examination.
![]()
COMMON
 haemorrhoids
haemorrhoids
 anal fissure
anal fissure
 rectal prolapse
rectal prolapse
 proctitis
proctitis
 perianal warts
perianal warts
OCCASIONAL
 rectal carcinoma
rectal carcinoma
 IBS
IBS
 anal/perianal fistula (may be associated with Crohn’s disease)
anal/perianal fistula (may be associated with Crohn’s disease)
 villous adenoma
villous adenoma
 poor anal hygiene
poor anal hygiene
 solitary rectal ulcer syndrome
solitary rectal ulcer syndrome
RARE
 anal tuberculosis
anal tuberculosis
 anal carcinoma
anal carcinoma
 STD, e.g. syphilis, gonorrhoea, chlamydia
STD, e.g. syphilis, gonorrhoea, chlamydia
 AIDS
AIDS
![]()

![]()
LIKELY: swab if purulent.
POSSIBLE: FBC, ESR/CRP, U&E and direct visualisation techniques (see below).
SMALL PRINT: STD screen.
 Anorectal swab for bacteriology if pus and local inflammation is present.
Anorectal swab for bacteriology if pus and local inflammation is present.
 FBC/ESR/CRP: WCC and ESR/CRP raised in inflammatory bowel disease.
FBC/ESR/CRP: WCC and ESR/CRP raised in inflammatory bowel disease.
 U&E: profuse mucus discharge from a villous adenoma can cause hypokalaemia.
U&E: profuse mucus discharge from a villous adenoma can cause hypokalaemia.
 Proctoscopy easily done in practice and guides management and referral.
Proctoscopy easily done in practice and guides management and referral.
 Sigmoidoscopy allows definitive examination and biopsy of suspicious lesions or inflammation.
Sigmoidoscopy allows definitive examination and biopsy of suspicious lesions or inflammation.
 STD screen – if STD suspected.
STD screen – if STD suspected.
 This symptom is likely to be associated with embarrassment. A clinical examination is important – so help the patient overcome any reticence with a sympathetic approach.
This symptom is likely to be associated with embarrassment. A clinical examination is important – so help the patient overcome any reticence with a sympathetic approach.
 Normal secretions from the anus should not be discounted – from perianal sweat glands and the anal glands themselves. This can sometimes cause a significant problem, particularly in the obese and those with poor anal hygiene.
Normal secretions from the anus should not be discounted – from perianal sweat glands and the anal glands themselves. This can sometimes cause a significant problem, particularly in the obese and those with poor anal hygiene.
 In women, the source of the discharge may be unclear. Speculum examination and protoscopy may be required to resolve any doubt.
In women, the source of the discharge may be unclear. Speculum examination and protoscopy may be required to resolve any doubt.
 Sexual history may be important. Don’t be coy in asking about recent sexual encounters and sexual practices if relevant.
Sexual history may be important. Don’t be coy in asking about recent sexual encounters and sexual practices if relevant.
 Rectal discharge in the elderly suggests carcinoma unless proved otherwise.
Rectal discharge in the elderly suggests carcinoma unless proved otherwise.
 A history of diarrhoea and abdominal pain suggests bowel pathology. Ulcerative colitis or Crohn’s disease is most likely in this context.
A history of diarrhoea and abdominal pain suggests bowel pathology. Ulcerative colitis or Crohn’s disease is most likely in this context.
 Any ulcerating lesion in the perianal area other than an obvious haemorrhoid should prompt referral for biopsy.
Any ulcerating lesion in the perianal area other than an obvious haemorrhoid should prompt referral for biopsy.