ABNORMAL GAIT IN ADULTS
![]()
The GP overview
Very few patients present with abnormal gait. It is more often noticed by the GP, while the patient’s complaint is usually a manifestation of the gait (e.g. unsteadiness in Parkinson’s disease) or of its cause (e.g. pain in arthritis). Congenital causes are not considered here as patients are most unlikely to present such problems to the GP.
![]()
Differential diagnosis
COMMON
 trauma (back and leg)
trauma (back and leg)
 osteoarthritis (OA) or other painful joint problem
osteoarthritis (OA) or other painful joint problem
 vestibular ataxia (vestibular neuritis, Ménière’s disease, CVA)
vestibular ataxia (vestibular neuritis, Ménière’s disease, CVA)
 Parkinson’s disease
Parkinson’s disease
 intermittent claudication (IC)
intermittent claudication (IC)
OCCASIONAL
 foot drop (peroneal nerve atrophy)
foot drop (peroneal nerve atrophy)
 multiple sclerosis
multiple sclerosis
 spinal nerve root pain (especially L5 and S1)
spinal nerve root pain (especially L5 and S1)
 cauda equina lesions
cauda equina lesions
 myasthenia gravis
myasthenia gravis
RARE
 tabes dorsalis (syphilis)
tabes dorsalis (syphilis)
 dystrophia myotonica
dystrophia myotonica
 motor neurone disease
motor neurone disease
 cerebellar ataxia
cerebellar ataxia
 hysteria
hysteria
![]()
Ready reckoner

![]()
Possible investigations
Most cases requiring tests will need referral to a specialist. The role of the GP in investigating these patients is therefore very limited.
LIKELY: none.
POSSIBLE: X-ray, FBC, ESR/CRP, RA factor, uric acid.
SMALL PRINT: scans, lumbar puncture, angiography.
 FBC, ESR/CRP, RA factor, uric acid: some forms of arthritis will result in an anaemia of chronic disorder. ESR/CRP may also be raised. Depending on the pattern of joint pain, RA factor and uric acid may provide useful information in the diagnosis of rheumatoid arthritis and gout.
FBC, ESR/CRP, RA factor, uric acid: some forms of arthritis will result in an anaemia of chronic disorder. ESR/CRP may also be raised. Depending on the pattern of joint pain, RA factor and uric acid may provide useful information in the diagnosis of rheumatoid arthritis and gout.
 X-rays useful in bony trauma. Limited value in OA except to exclude other bony pathology.
X-rays useful in bony trauma. Limited value in OA except to exclude other bony pathology.
 Syphilis serology: if tabes dorsalis suspected.
Syphilis serology: if tabes dorsalis suspected.
 If neurological signs of incoordination, consider CT/MRI scan and lumbar puncture – usually arranged by the specialist.
If neurological signs of incoordination, consider CT/MRI scan and lumbar puncture – usually arranged by the specialist.
 Angiography: arranged by the vascular surgeon if surgery contemplated in claudication.
Angiography: arranged by the vascular surgeon if surgery contemplated in claudication.
TOP TIPS
 Look up from the notes or computer as the patient walks in – otherwise you may miss a useful clue in the patient’s gait.
Look up from the notes or computer as the patient walks in – otherwise you may miss a useful clue in the patient’s gait.
 If the patient actually complains of problems walking, take your time in assessing the symptom – in particular, give the patient the opportunity to demonstrate the problem by walking him or her up and down the corridor.
If the patient actually complains of problems walking, take your time in assessing the symptom – in particular, give the patient the opportunity to demonstrate the problem by walking him or her up and down the corridor.
 If the cause is not immediately apparent from the history, perform a careful neurological examination – this is a situation where there may be hard signs which contribute significantly to diagnosis.
If the cause is not immediately apparent from the history, perform a careful neurological examination – this is a situation where there may be hard signs which contribute significantly to diagnosis.
 Vestibular neuritis usually settles within a few days. If patient remains ataxic, especially with persistent nystagmus, consider a central lesion and refer urgently.
Vestibular neuritis usually settles within a few days. If patient remains ataxic, especially with persistent nystagmus, consider a central lesion and refer urgently.
 Numbness in both legs (saddle pattern) with back pain and incontinence suggests a cauda equina lesion. Admit urgently.
Numbness in both legs (saddle pattern) with back pain and incontinence suggests a cauda equina lesion. Admit urgently.
 If the patient is ataxic and has a past history of neurological symptoms, such as paraesthesia or optic neuritis, consider multiple sclerosis.
If the patient is ataxic and has a past history of neurological symptoms, such as paraesthesia or optic neuritis, consider multiple sclerosis.
 Beware of labelling the patient as hysterical – apparently bizarre gaits may signify obscure but significant neurological pathology.
Beware of labelling the patient as hysterical – apparently bizarre gaits may signify obscure but significant neurological pathology.
ABNORMAL MOVEMENTS
![]()
The GP overview
This is an infrequent cause for attendance – though the public is becoming increasingly aware of conditions such as restless legs syndrome (RLS) and Tourette’s, and their treatments. Obvious generalised seizures and tremor are not considered in this chapter but are covered elsewhere.
![]()
Differential diagnosis
COMMON
 RLS
RLS
 myokymia (affecting orbicularis oculi muscles)
myokymia (affecting orbicularis oculi muscles)
 drug induced – including choreoathetosis, dystonias, tardive dyskinesias and akathisia (drugs include l-dopa, tricyclic antidepressants, metoclopramide and antipsychotics)
drug induced – including choreoathetosis, dystonias, tardive dyskinesias and akathisia (drugs include l-dopa, tricyclic antidepressants, metoclopramide and antipsychotics)
 Tourette’s
Tourette’s
 simple partial seizures
simple partial seizures
OCCASIONAL
 anxiety/nervous tic (common, but rarely presented to the GP)
anxiety/nervous tic (common, but rarely presented to the GP)
 muscle fasciculation (e.g. benign fasciculation, motor neurone disease)
muscle fasciculation (e.g. benign fasciculation, motor neurone disease)
 simple childhood tics (common, but infrequently presented)
simple childhood tics (common, but infrequently presented)
 dystonias (e.g. writer’s cramp, blepharospasm, spasmodic torticollis)
dystonias (e.g. writer’s cramp, blepharospasm, spasmodic torticollis)
 period leg movements during sleep
period leg movements during sleep
RARE
 myoclonus
myoclonus
 chorea (Sydenham’s, Huntington’s)
chorea (Sydenham’s, Huntington’s)
 Wilson’s disease
Wilson’s disease
 hemiballismus (e.g. post stroke)
hemiballismus (e.g. post stroke)
 hysterical
hysterical
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: FBC, U&E, ferritin, B12, folate, TFT, fasting glucose or HbA1c, calcium.
POSSIBLE: CT/MRI of brain or spinal cord, EEG, EMG, nerve conduction studies.
SMALL PRINT: other specialised tests (e.g. for myoclonus and Huntington’s).
 FBC, ferritin: to assess for iron deficiency in RLS.
FBC, ferritin: to assess for iron deficiency in RLS.
 U&E: renal failure is a potential cause of RLS and can be implicated in partial seizures.
U&E: renal failure is a potential cause of RLS and can be implicated in partial seizures.
 B12, folate: deficiencies may cause or mimic RLS.
B12, folate: deficiencies may cause or mimic RLS.
 TFT: hypothyroidism may cause RLS.
TFT: hypothyroidism may cause RLS.
 Fasting glucose or HbA1c: diabetes may cause RLS or partial seizures.
Fasting glucose or HbA1c: diabetes may cause RLS or partial seizures.
 Calcium: hypocalcaemia may be implicated in seizures.
Calcium: hypocalcaemia may be implicated in seizures.
 CT/MRI of brain or spinal cord: may be required in investigation of fasciculation and seizures (usually arranged after specialist referral).
CT/MRI of brain or spinal cord: may be required in investigation of fasciculation and seizures (usually arranged after specialist referral).
 EEG: for investigation of seizures.
EEG: for investigation of seizures.
 Other specialised tests: usually arranged by neurologist to explore the more obscure diagnoses such as Huntington’s chorea and Wilson’s disease.
Other specialised tests: usually arranged by neurologist to explore the more obscure diagnoses such as Huntington’s chorea and Wilson’s disease.
TOP TIPS
 When faced with odd and otherwise inexplicable movements of recent onset in a patient, remember to take a drug history.
When faced with odd and otherwise inexplicable movements of recent onset in a patient, remember to take a drug history.
 Bear in mind that abnormal movements can be caused by a drug that the patient has been taking for some time (e.g. tardive dyskinesias).
Bear in mind that abnormal movements can be caused by a drug that the patient has been taking for some time (e.g. tardive dyskinesias).
 Patients with myokymia sometimes become disproportionately anxious about the symptom, imagining all sorts of possible neurological catastrophes – they may need a lot of reassurance.
Patients with myokymia sometimes become disproportionately anxious about the symptom, imagining all sorts of possible neurological catastrophes – they may need a lot of reassurance.
 Childhood tics tend to be single; the patient with the much more significant Tourette’s will probably have multiple tics.
Childhood tics tend to be single; the patient with the much more significant Tourette’s will probably have multiple tics.
 Drug-induced dystonias may cause odd posturing and require prompt treatment. The diagnosis is easily overlooked – antipsychotics are common culprits, so it is easy to erroneously attribute the dystonia to psychiatric pathology.
Drug-induced dystonias may cause odd posturing and require prompt treatment. The diagnosis is easily overlooked – antipsychotics are common culprits, so it is easy to erroneously attribute the dystonia to psychiatric pathology.
 Beware of the combination of personality changes and odd movements such as facial grimaces – this could be Huntington’s chorea. Also, don’t be misled by the lack of a positive family history – this background may have been concealed from the patient.
Beware of the combination of personality changes and odd movements such as facial grimaces – this could be Huntington’s chorea. Also, don’t be misled by the lack of a positive family history – this background may have been concealed from the patient.
BACK PAIN
![]()
The GP overview
Ongoing backache is a familiar presentation to all GPs, and acute back pain is one of the most common reasons for an emergency appointment in primary care. The average GP can expect about 120 consultations for this problem each year. Eighty per cent of the Western population suffer back pain at some stage in their lives: it is the largest single cause of lost working hours among both manual and sedentary workers; in the former it is an important cause of disability. Remember that many non-orthopaedic causes of back pain lie in wait, so be systematic.
![]()
Differential diagnosis
COMMON
 mechanical (muscular) back pain
mechanical (muscular) back pain
 prolapsed lumbar disc: nerve root pain
prolapsed lumbar disc: nerve root pain
 spondylosis (exacerbation)
spondylosis (exacerbation)
 pyelonephritis and renal stones
pyelonephritis and renal stones
 pelvic infection
pelvic infection
OCCASIONAL
 the spondoarthritides (e.g. ankylosing spondylitis, Reiter’s syndrome)
the spondoarthritides (e.g. ankylosing spondylitis, Reiter’s syndrome)
 neoplastic disease of the spine (usually secondaries), myeloma
neoplastic disease of the spine (usually secondaries), myeloma
 duodenal ulcer/acute pancreatitis
duodenal ulcer/acute pancreatitis
 depression and anxiety states
depression and anxiety states
 vertebral fracture (often compression fracture associated with osteoporosis)
vertebral fracture (often compression fracture associated with osteoporosis)
RARE
 spinal stenosis
spinal stenosis
 osteomalacia
osteomalacia
 aortic aneurysm
aortic aneurysm
 pancreatic cancer
pancreatic cancer
 spondylolisthesis
spondylolisthesis
 osteomyelitis
osteomyelitis
 malingering
malingering
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: none.
POSSIBLE: urinalysis, MSU, FBC, ESR/CRP, plasma electrophoresis, blood calcium, PSA.
SMALL PRINT: lumbar spine X-ray, IVU, HLA-B27, CT or MRI scan, bone scan, investigations for GI cause, ultrasound, DXA scan.
 Urinalysis useful if UTI suspected: look for blood, pus and nitrite as markers of infection; confirm with MSU; blood alone suggests possible stone.
Urinalysis useful if UTI suspected: look for blood, pus and nitrite as markers of infection; confirm with MSU; blood alone suggests possible stone.
 ESR/CRP elevated in malignant and inflammatory disorders.
ESR/CRP elevated in malignant and inflammatory disorders.
 FBC: Hb may be reduced in malignancy; a high WCC raises the possibility of osteomyelitis.
FBC: Hb may be reduced in malignancy; a high WCC raises the possibility of osteomyelitis.
 Plasma electrophoresis: paraprotein band in myeloma.
Plasma electrophoresis: paraprotein band in myeloma.
 Blood calcium: elevated in myeloma and bony secondaries; reduced in osteomalacia.
Blood calcium: elevated in myeloma and bony secondaries; reduced in osteomalacia.
 PSA: if disseminated prostate cancer suspected.
PSA: if disseminated prostate cancer suspected.
 Lumbar spine X-ray often not useful in mechanical pain. Consider if no resolution by 6 weeks to investigate possible underlying pathology. In younger patients, it may help diagnose sacroiliitis or spondylolisthesis; in older people, it is useful to check for vertebral collapse. Generally, if imaging is required, CT or MRI may be more helpful.
Lumbar spine X-ray often not useful in mechanical pain. Consider if no resolution by 6 weeks to investigate possible underlying pathology. In younger patients, it may help diagnose sacroiliitis or spondylolisthesis; in older people, it is useful to check for vertebral collapse. Generally, if imaging is required, CT or MRI may be more helpful.
 Bone scan: will detect bony secondaries and bone infection.
Bone scan: will detect bony secondaries and bone infection.
 CT or MRI scan usually a specialist’s request: good for spotting spinal stenosis, significant prolapsed disc and discrete bony lesions.
CT or MRI scan usually a specialist’s request: good for spotting spinal stenosis, significant prolapsed disc and discrete bony lesions.
 Investigations for GI cause might include endoscopy (for DU), serum amylase (for pancreatitis) and CT scan (for carcinoma of pancreas).
Investigations for GI cause might include endoscopy (for DU), serum amylase (for pancreatitis) and CT scan (for carcinoma of pancreas).
 Ultrasound: for aortic aneurysm.
Ultrasound: for aortic aneurysm.
 IVU: for recurrent pyelonephritis and possible renal or ureteric stones.
IVU: for recurrent pyelonephritis and possible renal or ureteric stones.
 DEXA scan: may be required to confirm suspicion of osteoporosis.
DEXA scan: may be required to confirm suspicion of osteoporosis.
TOP TIPS
 The vast majority are ‘mechanical’, and most of these improve regardless of treatment modality in 6–8 weeks; a positive and optimistic approach is important.
The vast majority are ‘mechanical’, and most of these improve regardless of treatment modality in 6–8 weeks; a positive and optimistic approach is important.
 Patients often expect an X-ray. Resist requests unless appropriate – and explain why. Even if the patient doesn’t make this request, consider volunteering why you’re not ordering an X-ray, as this can help maintain confidence in the doctor–patient relationship, especially if the symptoms take some time to settle.
Patients often expect an X-ray. Resist requests unless appropriate – and explain why. Even if the patient doesn’t make this request, consider volunteering why you’re not ordering an X-ray, as this can help maintain confidence in the doctor–patient relationship, especially if the symptoms take some time to settle.
 If the problem is recurrent, exclude significant pathology then explore the patient’s concerns. In simple recurrent mechanical back pain, it is worth discussing preventive measures and educating the patient for self-management of future episodes.
If the problem is recurrent, exclude significant pathology then explore the patient’s concerns. In simple recurrent mechanical back pain, it is worth discussing preventive measures and educating the patient for self-management of future episodes.
 True malingering is not common, but back pain is favoured among malingerers because of its subjectivity. Beware of patients who apparently cannot straight-leg raise, yet have no problem sitting up on the couch, and patients who decline to sit down during the consultation.
True malingering is not common, but back pain is favoured among malingerers because of its subjectivity. Beware of patients who apparently cannot straight-leg raise, yet have no problem sitting up on the couch, and patients who decline to sit down during the consultation.

 The traditional ‘red flags’ in back pain are thought to be of very limited use because of poor specificity and sensitivity. The only ones regarded as genuinely helpful are, for spinal fracture, older age, trauma, the presence of contusions or abrasions and steroid use, and, for spinal malignancy, a past history of cancer. Current consensus is that slavish adherence to red flags should be avoided and instead the overall clinical picture and progress assessed – although an ESR may be useful in ruling out significant disease.
The traditional ‘red flags’ in back pain are thought to be of very limited use because of poor specificity and sensitivity. The only ones regarded as genuinely helpful are, for spinal fracture, older age, trauma, the presence of contusions or abrasions and steroid use, and, for spinal malignancy, a past history of cancer. Current consensus is that slavish adherence to red flags should be avoided and instead the overall clinical picture and progress assessed – although an ESR may be useful in ruling out significant disease.
 Bilateral sciatica, saddle anaesthesia and bowel and/or bladder dysfunction suggests central disc protrusion: this is a neurosurgical emergency.
Bilateral sciatica, saddle anaesthesia and bowel and/or bladder dysfunction suggests central disc protrusion: this is a neurosurgical emergency.
 Consider prostatic cancer in men over 55 with atypical low back pain. Do a PR exam, together with PSA and bone assay.
Consider prostatic cancer in men over 55 with atypical low back pain. Do a PR exam, together with PSA and bone assay.
 Back pain without any restriction of spinal movement, or which is not exacerbated by back movement, suggests that the source of the problem lies elsewhere – consider renal, aortic or gastrointestinal disease, or pelvic pathology in women.
Back pain without any restriction of spinal movement, or which is not exacerbated by back movement, suggests that the source of the problem lies elsewhere – consider renal, aortic or gastrointestinal disease, or pelvic pathology in women.
 Tearing interscapular or lower pain in a known arteriopath suggests dissecting aortic aneurysm: admit straight away.
Tearing interscapular or lower pain in a known arteriopath suggests dissecting aortic aneurysm: admit straight away.
CRYING BABY
![]()
The GP overview
This is a very frequent reason for an out-of-hours call. A baby’s cry is almost impossible for parents to ignore. When crying continues unabated in spite of all that parents can do to settle an infant, parental distress sets in and they will turn to you for an answer and a solution.
![]()
Differential diagnosis
COMMON
 normal
normal
 colic
colic
 constipation
constipation
 teething
teething
 viral illness
viral illness
OCCASIONAL
 otitis media or externa
otitis media or externa
 severe nappy rash and/or inflamed foreskin
severe nappy rash and/or inflamed foreskin
 gastroenteritis
gastroenteritis
 UTI
UTI
 after immunisation
after immunisation
 respiratory distress – severe bronchiolitis, chest infection, croupy cough
respiratory distress – severe bronchiolitis, chest infection, croupy cough
RARE
 non-accidental injury
non-accidental injury
 mastoiditis
mastoiditis
 meningitis, encephalitis
meningitis, encephalitis
 septicaemia
septicaemia
 bowel obstruction including intussusception and strangulated hernia
bowel obstruction including intussusception and strangulated hernia
 appendicitis
appendicitis
 osteomyelitis
osteomyelitis
 testicular torsion
testicular torsion
 undiagnosed birth injury, e.g. fractured clavicle
undiagnosed birth injury, e.g. fractured clavicle
 congenital disorders, e.g. Hirschprung’s disease, pyloric stenosis
congenital disorders, e.g. Hirschprung’s disease, pyloric stenosis
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: none other than those performed after admission.
POSSIBLE: swab of any obvious discharge.
SMALL PRINT: see hospital investigations.
 Other than a swab for obvious discharge (e.g. in otitis externa), no investigations are appropriate in general practice – if no obvious cause is found and the baby continues to be distressed, admission for observation and investigation is mandatory.
Other than a swab for obvious discharge (e.g. in otitis externa), no investigations are appropriate in general practice – if no obvious cause is found and the baby continues to be distressed, admission for observation and investigation is mandatory.
 Secondary care investigations are likely to include urinalysis, MSU for bacteriology, bloods for FBC, ESR, glucose, U&E, and many others depending on the indication (e.g. CXR, AXR, lumbar puncture, blood gases).
Secondary care investigations are likely to include urinalysis, MSU for bacteriology, bloods for FBC, ESR, glucose, U&E, and many others depending on the indication (e.g. CXR, AXR, lumbar puncture, blood gases).
TOP TIPS
 Babies cry on average for 1½ to 2 hours per day. Some normal babies cry more than this or for long periods for no apparent reason.
Babies cry on average for 1½ to 2 hours per day. Some normal babies cry more than this or for long periods for no apparent reason.
 Remain calm and sensitive. Parents of a crying baby are often distraught, and whatever your perception of the seriousness or not of the situation, make a thorough assessment and make sure the parents understand you are taking them seriously.
Remain calm and sensitive. Parents of a crying baby are often distraught, and whatever your perception of the seriousness or not of the situation, make a thorough assessment and make sure the parents understand you are taking them seriously.
 Always explain your findings and advice clearly, and make sure the parents understand you. Write things down for them if necessary. Your patient depends completely on your communication skills.
Always explain your findings and advice clearly, and make sure the parents understand you. Write things down for them if necessary. Your patient depends completely on your communication skills.
 Remember the obvious – babies may cry because of tiredness, hunger, wind after feeds, boredom, and uncomfortably full nappies. Never assume that parenting skills are 100%, and do explore baby care issues that may seem to be too obvious to ask about.
Remember the obvious – babies may cry because of tiredness, hunger, wind after feeds, boredom, and uncomfortably full nappies. Never assume that parenting skills are 100%, and do explore baby care issues that may seem to be too obvious to ask about.
 Babies may be unsettled and cry more than normal for a day or two after immunisation. If a baby is crying excessively for longer than 48 hours after immunisation, it is unsafe to diagnose immunisation as the cause without clinical assessment.
Babies may be unsettled and cry more than normal for a day or two after immunisation. If a baby is crying excessively for longer than 48 hours after immunisation, it is unsafe to diagnose immunisation as the cause without clinical assessment.
 Telephone advice calls may be handled with careful triage and advice alone, providing there is always a fall back plan for the parents to call back or seek further advice if things do not settle rapidly. There is no substitute for a hands-on clinical assessment, and if in the slightest doubt, always see the baby as soon as possible.
Telephone advice calls may be handled with careful triage and advice alone, providing there is always a fall back plan for the parents to call back or seek further advice if things do not settle rapidly. There is no substitute for a hands-on clinical assessment, and if in the slightest doubt, always see the baby as soon as possible.
 Observe in the most general way how a baby handles during examination. Irritability on handling is a very important general sign. Regardless of other examination findings, this alone can be a reason to refer for paediatric assessment.
Observe in the most general way how a baby handles during examination. Irritability on handling is a very important general sign. Regardless of other examination findings, this alone can be a reason to refer for paediatric assessment.
 There is no clear physiological reason why babies should develop a fever during teething, but there is no doubt this happens in some babies, in spite of traditional medical teaching to the contrary. A fever is never high if due to teething alone. The fever of teething is usually very short-lived – less than 24 hours – while a fever caused by a viral infection can go on for several days.
There is no clear physiological reason why babies should develop a fever during teething, but there is no doubt this happens in some babies, in spite of traditional medical teaching to the contrary. A fever is never high if due to teething alone. The fever of teething is usually very short-lived – less than 24 hours – while a fever caused by a viral infection can go on for several days.
 Babies cannot tell us what’s wrong, but they can tell us something’s wrong. If in any doubt about the diagnosis, seek a second opinion or a paediatric assessment. Always follow your sixth-sense, intuition or personal alarm bells. Thoughtful and experienced paediatricians will respect your feeling on this, so do not worry if you can’t justify your referral on textbook clinical criteria.
Babies cannot tell us what’s wrong, but they can tell us something’s wrong. If in any doubt about the diagnosis, seek a second opinion or a paediatric assessment. Always follow your sixth-sense, intuition or personal alarm bells. Thoughtful and experienced paediatricians will respect your feeling on this, so do not worry if you can’t justify your referral on textbook clinical criteria.

 Be aware of the possibility of non-accidental injury as a cause for the baby crying. If you detect unusual anxiety, or unusual emotional detachment from the calling parent, make sure you see the baby and examine it thoroughly.
Be aware of the possibility of non-accidental injury as a cause for the baby crying. If you detect unusual anxiety, or unusual emotional detachment from the calling parent, make sure you see the baby and examine it thoroughly.
 A baby that has been crying a lot and goes on to become lethargic (as opposed to a normal calm state) is probably very ill. Even if you are unsure of the diagnosis, follow your intuition and arrange a paediatric opinion.
A baby that has been crying a lot and goes on to become lethargic (as opposed to a normal calm state) is probably very ill. Even if you are unsure of the diagnosis, follow your intuition and arrange a paediatric opinion.
 A constantly bulging fontanelle is always an indication for immediate paediatric referral.
A constantly bulging fontanelle is always an indication for immediate paediatric referral.
 Be sure to observe and note the general muscular tone of a crying baby. Constant stiffness or floppiness are ominous signs and immediate referral is indicated.
Be sure to observe and note the general muscular tone of a crying baby. Constant stiffness or floppiness are ominous signs and immediate referral is indicated.
DELAYED PUBERTY
![]()
The GP overview
Delayed puberty means delayed development of all the secondary sexual characteristics. It is a rare but serious symptom. In girls, it is usually presented as a delayed menarche (failure to menstruate by the age of 16), though it may present as failure to develop other secondary sexual characteristics from the age of 14. In boys, the defined age is 15. The following is a selection of the more important causes. (Remember that the subheadings Common, Occasional, Rare are relative – overall, this is a rare presenting symptom.)
![]()
Differential diagnosis
COMMON
 constitutional (50% of cases in boys, 16% of cases in girls)
constitutional (50% of cases in boys, 16% of cases in girls)
 hyperthyroidism
hyperthyroidism
 Turner’s syndrome
Turner’s syndrome
 anorexia nervosa (1% of all girls in Western countries)
anorexia nervosa (1% of all girls in Western countries)
 hypothalamic gonadotrophin-releasing hormone (GnRH) deficiency (e.g. Noonan’s and Kallmann’s syndrome)
hypothalamic gonadotrophin-releasing hormone (GnRH) deficiency (e.g. Noonan’s and Kallmann’s syndrome)
OCCASIONAL
 space-occupying hypothalamo-pituitary lesion (various types)
space-occupying hypothalamo-pituitary lesion (various types)
 chronic disease (e.g. diabetes, renal failure, cystic fibrosis, coeliac disease)
chronic disease (e.g. diabetes, renal failure, cystic fibrosis, coeliac disease)
 hyperprolactinaemia
hyperprolactinaemia
 adrenal disease: congenital adrenal hyperplasia and Cushing’s disease
adrenal disease: congenital adrenal hyperplasia and Cushing’s disease
 drugs (e.g. thyroxine, chemotherapy (both sexes); androgens, anabolic steroids (females only))
drugs (e.g. thyroxine, chemotherapy (both sexes); androgens, anabolic steroids (females only))
 radiotherapy
radiotherapy
 growth hormone deficiency
growth hormone deficiency
RARE
 other ovarian problems (e.g. pure dysgenesis, autoimmune disease)
other ovarian problems (e.g. pure dysgenesis, autoimmune disease)
 hypothyroidism if autoimmune (otherwise associated with early puberty)
hypothyroidism if autoimmune (otherwise associated with early puberty)
 pure gonadal dysgenesis
pure gonadal dysgenesis
 maldescent of the testes (rare nowadays: usually detected early)
maldescent of the testes (rare nowadays: usually detected early)
 trauma, infection and granulomas of hypothalamus/pituitary
trauma, infection and granulomas of hypothalamus/pituitary
![]()
Ready reckoner

![]()
Possible investigations
Cases requiring investigation are likely to need referral to a paediatrician or endocrinologist. The role of the GP is therefore limited. A few basic tests might be arranged in primary care in probable constitutional cases, mainly to exclude underlying disease and ‘reassure’ patient, parents and doctor (e.g. urinalysis, FBC, U&E, TFT). More complex investigations in secondary care might include CT scanning (tumours), ultrasound of pelvis (to examine ovaries and search for nonpalpable gonads), chromosomal analysis and various tests of endocrine function.
TOP TIPS
 Delayed puberty causes worry for parents and often misery for children, who may be teased or bullied by their adolescent peers. Take their concerns seriously from the outset.
Delayed puberty causes worry for parents and often misery for children, who may be teased or bullied by their adolescent peers. Take their concerns seriously from the outset.
 Remember to take a family history: constitutional delayed puberty often runs in families.
Remember to take a family history: constitutional delayed puberty often runs in families.
 The majority of children brought with ‘delayed puberty’ will be normal, with their parents either not recognising that secondary sexual characteristics are developing or not appreciating the age range which is normal for pubertal development.
The majority of children brought with ‘delayed puberty’ will be normal, with their parents either not recognising that secondary sexual characteristics are developing or not appreciating the age range which is normal for pubertal development.
 Distinguish between delayed puberty and primary amenorrhoea with otherwise normal pubertal development. The latter has different causes (e.g. vaginal atresia, cycle initiation defect and, very rarely, testicular feminisation).
Distinguish between delayed puberty and primary amenorrhoea with otherwise normal pubertal development. The latter has different causes (e.g. vaginal atresia, cycle initiation defect and, very rarely, testicular feminisation).

 Although it accounts for 50% of male cases, do not diagnose constitutional delayed puberty in boys in the presence of a very small penis or anosmia – in these situations, an underlying disease is likely.
Although it accounts for 50% of male cases, do not diagnose constitutional delayed puberty in boys in the presence of a very small penis or anosmia – in these situations, an underlying disease is likely.
 More than 80% of cases in girls have a pathological cause, so investigation is the rule.
More than 80% of cases in girls have a pathological cause, so investigation is the rule.
 Short stature, malaise and symptoms or signs of hypothyroidism suggest an underlying disorder of the hypothalamus and/or pituitary.
Short stature, malaise and symptoms or signs of hypothyroidism suggest an underlying disorder of the hypothalamus and/or pituitary.
EPISODIC LOSS OF CONSCIOUSNESS
![]()
The GP overview
The terminology in this area can be very confusing with words like ‘syncope’ and ‘faints’ being used imprecisely. Episodic loss of consciousness can occur in any age group, though it tends to be commoner in the elderly. It is a frightening experience for the patient, and it demands thorough examination, investigation and a low threshold for referral. For the GP, the differential widens the older the patient – and cardiac causes should not be overlooked in the elderly.
![]()
Differential diagnosis
COMMON
 vasovagal attacks (faints)
vasovagal attacks (faints)
 paroxysmal arrhythmia, e.g. Stokes–Adams attacks, sinus bradycardia, SVT
paroxysmal arrhythmia, e.g. Stokes–Adams attacks, sinus bradycardia, SVT
 epilepsy (various forms)
epilepsy (various forms)
 hypoglycaemia
hypoglycaemia
 orthostatic hypotension
orthostatic hypotension
OCCASIONAL
 cardiac structural lesion, e.g. aortic stenosis, hypertrophic obstructive cardiomyopathy,
cardiac structural lesion, e.g. aortic stenosis, hypertrophic obstructive cardiomyopathy,
pulmonary stenosis
 micturition and cough syncope
micturition and cough syncope
 sleep apnoea
sleep apnoea
 Valsalva-induced syncope, e.g. weightlifting
Valsalva-induced syncope, e.g. weightlifting
 pseudoseizures
pseudoseizures
RARE
 narcolepsy
narcolepsy
 carotid sinus syncope
carotid sinus syncope
 hyperventilation
hyperventilation
 subclavian steal syndrome
subclavian steal syndrome
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: FBC; ECG (especially in elderly); if probable epilepsy, also EEG and CT scan.
POSSIBLE: glucometer, 24 h ECG.
SMALL PRINT: echocardiography, tilt-table testing.
 Glucometer ‘on the scene’ gives diagnosis of hypoglycaemia.
Glucometer ‘on the scene’ gives diagnosis of hypoglycaemia.
 FBC: anaemia will exacerbate any form of syncope and TIAs.
FBC: anaemia will exacerbate any form of syncope and TIAs.
 Standard ECG may reveal signs of ischaemia and heart block; 24 h ECG more useful for definitive diagnosis of arrhythmia.
Standard ECG may reveal signs of ischaemia and heart block; 24 h ECG more useful for definitive diagnosis of arrhythmia.
 CT scan and EEG essential if previously undiagnosed epilepsy suspected.
CT scan and EEG essential if previously undiagnosed epilepsy suspected.
 Echocardiography: if structural cardiac problem suspected.
Echocardiography: if structural cardiac problem suspected.
 Tilt-table testing: for unexplained syncope to assess susceptibility to vasovagal episodes.
Tilt-table testing: for unexplained syncope to assess susceptibility to vasovagal episodes.
TOP TIPS
 The key to diagnosis is an accurate history. This may not be available from the patient, so make a real effort to obtain an eyewitness account.
The key to diagnosis is an accurate history. This may not be available from the patient, so make a real effort to obtain an eyewitness account.
 In younger patients, the diagnosis is likely to lie between a vasovagal attack and a fit; in the middle-aged and elderly, the differential is much wider and will include, for example, arrhythmias and orthostatic hypotension.
In younger patients, the diagnosis is likely to lie between a vasovagal attack and a fit; in the middle-aged and elderly, the differential is much wider and will include, for example, arrhythmias and orthostatic hypotension.
 Episodic loss of consciousness is a symptom which merits diligent assessment. An accurate diagnosis has implications not only for the individual’s health, but also for employment and driving.
Episodic loss of consciousness is a symptom which merits diligent assessment. An accurate diagnosis has implications not only for the individual’s health, but also for employment and driving.
 Remember that, with a vasovagal episode, patients remaining upright (e.g. sitting or in a crowd) may develop tonic–clonic movements which mimic a fit.
Remember that, with a vasovagal episode, patients remaining upright (e.g. sitting or in a crowd) may develop tonic–clonic movements which mimic a fit.
 Unlike in syncope or seizures, the eyes are usually closed in pseudoseizures.
Unlike in syncope or seizures, the eyes are usually closed in pseudoseizures.
 An eyewitness account that the patient looked as though he or she had died, together with marked facial flushing on recovery, is characteristic of Stokes–Adams attacks. These can be fatal, so early diagnosis is important.
An eyewitness account that the patient looked as though he or she had died, together with marked facial flushing on recovery, is characteristic of Stokes–Adams attacks. These can be fatal, so early diagnosis is important.
 Discovery of an aortic stenotic murmur should prompt urgent referral. Severe aortic stenosis can cause sudden cardiac death.
Discovery of an aortic stenotic murmur should prompt urgent referral. Severe aortic stenosis can cause sudden cardiac death.
 Red flags suggesting a possible cardiac cause include a family history of sudden cardiac death, syncope during exercise and an abnormal ECG.
Red flags suggesting a possible cardiac cause include a family history of sudden cardiac death, syncope during exercise and an abnormal ECG.
 Syncope caused by neck pressure or head movement could be carotid sinus syncope – if recurrent, this will require a pacemaker.
Syncope caused by neck pressure or head movement could be carotid sinus syncope – if recurrent, this will require a pacemaker.
EXCESSIVE SWEATING
![]()
The GP overview
Under normal conditions, 800 mL of water is lost daily as insensible loss, mostly in sweat. Excessive sweating can at least double this figure. As a symptom, it is normally part of a package of other problems – it is unusual for the patient to present with excessive sweating in isolation.
![]()
Differential diagnosis
COMMON
 menopause
menopause
 anxiety
anxiety
 infections (common, acute)
infections (common, acute)
 hypoglycaemia: may be reactive, i.e. non-diabetic
hypoglycaemia: may be reactive, i.e. non-diabetic
 hyperthyroidism
hyperthyroidism
OCCASIONAL
 drugs: alcohol, tricyclic antidepressants, pilocarpine
drugs: alcohol, tricyclic antidepressants, pilocarpine
 alcohol and drug withdrawal
alcohol and drug withdrawal
 shock/syncope
shock/syncope
 intense pain
intense pain
 hyperhidrosis
hyperhidrosis
 other infections, e.g. TB, HIV, endocarditis, brucellosis
other infections, e.g. TB, HIV, endocarditis, brucellosis
RARE
 malignancy (e.g. lymphoma)
malignancy (e.g. lymphoma)
 organic nerve lesions: brain tumours, spinal cord injury (sweating is localised to dermatome involved)
organic nerve lesions: brain tumours, spinal cord injury (sweating is localised to dermatome involved)
 pachydermoperiostosis: localised to skin folds of forehead and extremities
pachydermoperiostosis: localised to skin folds of forehead and extremities
 hyperpituitarism/acromegaly
hyperpituitarism/acromegaly
 rare vasoactive tumours: phaeochromocytoma, carcinoid
rare vasoactive tumours: phaeochromocytoma, carcinoid
 connective tissue disorders
connective tissue disorders
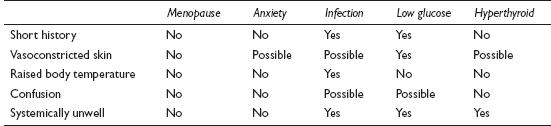
![]()
Ready reckoner
![]()
Possible investigations
LIKELY: FBC, ESR/CRP, TFT.
POSSIBLE: FSH/LH, LFT, glucose.
SMALL PRINT: autoimmune screen, CXR, tests for uncommon infections, 24-hour urinary catecholamines, CT/MRI scan.
 FBC/ESR/CRP: ESR/CRP and WCC raised in infection. Raised ESR/CRP and anaemia possible in lymphoma and other malignancies.
FBC/ESR/CRP: ESR/CRP and WCC raised in infection. Raised ESR/CRP and anaemia possible in lymphoma and other malignancies.
 TFTs: may reveal thyrotoxicosis as a cause of chronic sweating.
TFTs: may reveal thyrotoxicosis as a cause of chronic sweating.
 Glucose: in reactive hypoglycaemia only useful at the time of the sweating.
Glucose: in reactive hypoglycaemia only useful at the time of the sweating.
 FSH/LH: helps if diagnosis of menopause in doubt.
FSH/LH: helps if diagnosis of menopause in doubt.
 LFT: may reveal high alcohol intake.
LFT: may reveal high alcohol intake.
 CXR might reveal occult infection (especially TB) or malignancy.
CXR might reveal occult infection (especially TB) or malignancy.
 Tests for uncommon infections, e.g. blood test for HIV, echocardiography for endocarditis.
Tests for uncommon infections, e.g. blood test for HIV, echocardiography for endocarditis.
 Autoimmune screen: may help in confirming diagnosis of connective tissue disease.
Autoimmune screen: may help in confirming diagnosis of connective tissue disease.
 24 h urinary catecholamines traditionally used to look for phaeochromocytoma, but low specificity makes CT/MRI scan more useful.
24 h urinary catecholamines traditionally used to look for phaeochromocytoma, but low specificity makes CT/MRI scan more useful.
TOP TIPS
 Length of history is very helpful – short-term sweating is likely to have an apparent, acute cause; if long-term, the diagnosis is more likely to be constitutional or anxiety; in the medium-term, the differential diagnosis is much wider.
Length of history is very helpful – short-term sweating is likely to have an apparent, acute cause; if long-term, the diagnosis is more likely to be constitutional or anxiety; in the medium-term, the differential diagnosis is much wider.
 Anxiety rarely causes night sweats.
Anxiety rarely causes night sweats.
 Do not underestimate the potentially devastating effect of hyperhidrosis.
Do not underestimate the potentially devastating effect of hyperhidrosis.
 Lack of fever does not exclude infection. In some infections (e.g. TB, brucellosis) – and lymphoma – sweating can be out of phase with fever.
Lack of fever does not exclude infection. In some infections (e.g. TB, brucellosis) – and lymphoma – sweating can be out of phase with fever.
 If the problem is persistent, a full examination is advisable, paying attention to the lymph nodes, liver and spleen. If no cause is apparent, have a low threshold for investigations or referral, particularly if the patient is unwell or losing weight.
If the problem is persistent, a full examination is advisable, paying attention to the lymph nodes, liver and spleen. If no cause is apparent, have a low threshold for investigations or referral, particularly if the patient is unwell or losing weight.
 Consider unusual infections in the recently returned traveller (e.g. TB, typhoid).
Consider unusual infections in the recently returned traveller (e.g. TB, typhoid).
 Episodic skin flushing (especially provoked by alcohol) with diarrhoea and breathlessness is likely to be caused by anxiety – but don’t forget carcinoid syndrome as a rare possibility.
Episodic skin flushing (especially provoked by alcohol) with diarrhoea and breathlessness is likely to be caused by anxiety – but don’t forget carcinoid syndrome as a rare possibility.
FAILURE TO THRIVE
![]()
The GP overview
Failure to thrive is defined as the failure of a child to maintain the normal rate of growth for its age and gender. A logical and systematic approach is essential to navigate through the vast differential diagnosis list.
![]()
Differential diagnosis
There are very many causes of failure to thrive. To produce a workable list, we have given broad categories and emphasised within them the most common causes.
COMMON
 normal – the genetic components of height and weight kick in during the first 2 years, so babies of small parents may cross the centiles and appear to be ‘dropping off’
normal – the genetic components of height and weight kick in during the first 2 years, so babies of small parents may cross the centiles and appear to be ‘dropping off’
 neglect (emotional and physical)
neglect (emotional and physical)
 feeding problems (inadequate or inappropriate feeding, physical causes, e.g. cleft palate)
feeding problems (inadequate or inappropriate feeding, physical causes, e.g. cleft palate)
 vomiting from any cause (gastro-oesophageal reflux common, other causes such as pyloric stenosis rarer)
vomiting from any cause (gastro-oesophageal reflux common, other causes such as pyloric stenosis rarer)
 malabsorption – including cow’s milk intolerance (lactose or cow’s milk protein intolerance), coeliac disease
malabsorption – including cow’s milk intolerance (lactose or cow’s milk protein intolerance), coeliac disease
OCCASIONAL
 recurrent infections, e.g. UTI, frequent viral illnesses
recurrent infections, e.g. UTI, frequent viral illnesses
 metabolic/endocrine causes, e.g. diabetes, hypo- and hyperthyroidism
metabolic/endocrine causes, e.g. diabetes, hypo- and hyperthyroidism
 common chronic infection (UTI, gastroenteritis)
common chronic infection (UTI, gastroenteritis)
 syndromes, e.g. Turner’s, Down’s (though growth can follow centiles normally)
syndromes, e.g. Turner’s, Down’s (though growth can follow centiles normally)
 intrauterine growth retardation
intrauterine growth retardation
 premature delivery with complications
premature delivery with complications
 toxicity during pregnancy, e.g. maternal smoking, alcohol, cocaine and amphetamines
toxicity during pregnancy, e.g. maternal smoking, alcohol, cocaine and amphetamines
 maternal medication or infection during pregnancy
maternal medication or infection during pregnancy
RARE
 serious chronic disease, e.g. cerebral palsy, hepatic, cardiac or renal failure
serious chronic disease, e.g. cerebral palsy, hepatic, cardiac or renal failure
 severe chronic asthma
severe chronic asthma
 malignancy
malignancy
 rare (in UK) chronic infection: TB, congenital HIV, parasites
rare (in UK) chronic infection: TB, congenital HIV, parasites
 Munchausen’s syndrome by proxy
Munchausen’s syndrome by proxy
 cystic fibrosis
cystic fibrosis
 inborn errors of metabolism
inborn errors of metabolism
 rare causes of infant feeding difficulties, e.g. hypotonia, micrognathia, Prader–Willi syndrome
rare causes of infant feeding difficulties, e.g. hypotonia, micrognathia, Prader–Willi syndrome
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: urinalysis, MSU, FBC, U&E, LFTs, thyroid function tests, coeliac screen, stool studies.
POSSIBLE: immunoglobulins.
SMALL PRINT: PPD skin test, radiological studies, sweat chloride test, growth hormone levels, HIV testing.
 Urinalysis and MSU to seek evidence of UTI.
Urinalysis and MSU to seek evidence of UTI.
 FBC may reveal both the effects of malnutrition (anaemia) and possible causes of failure to thrive, e.g. a raised white cell count indicating chronic infection.
FBC may reveal both the effects of malnutrition (anaemia) and possible causes of failure to thrive, e.g. a raised white cell count indicating chronic infection.
 U&E and LFTs can both be markers of reduced metabolic function (reduced urea, creatinine and albumin, and reduced liver enzyme activity) or the signs of primary renal or hepatic disease.
U&E and LFTs can both be markers of reduced metabolic function (reduced urea, creatinine and albumin, and reduced liver enzyme activity) or the signs of primary renal or hepatic disease.
 Thyroid function tests: essential and simple to detect over- or underactive thyroid.
Thyroid function tests: essential and simple to detect over- or underactive thyroid.
 Coeliac screen and stool studies: for malabsorption (and look too for parasites, e.g. helminths or giardiasis).
Coeliac screen and stool studies: for malabsorption (and look too for parasites, e.g. helminths or giardiasis).
 Immunoglobulins: different patterns and levels of different immunoglobulin classes are associated with a vast range of infective, autoimmune and neoplastic conditions.
Immunoglobulins: different patterns and levels of different immunoglobulin classes are associated with a vast range of infective, autoimmune and neoplastic conditions.
 Purified protein derivative (PPD) skin test (for tuberculosis) is also known as the Mantoux test. A positive reaction to the injected tuberculin PPD may indicate current TB infection, or previous exposure.
Purified protein derivative (PPD) skin test (for tuberculosis) is also known as the Mantoux test. A positive reaction to the injected tuberculin PPD may indicate current TB infection, or previous exposure.
 Radiological studies: bone age may be helpful to distinguish genetic short stature from constitutional delay of growth.
Radiological studies: bone age may be helpful to distinguish genetic short stature from constitutional delay of growth.
 Sweat chloride test is a reliable diagnostic test for cystic fibrosis, which affects 1 in 2500 infants.
Sweat chloride test is a reliable diagnostic test for cystic fibrosis, which affects 1 in 2500 infants.
 Growth hormone levels. Growth hormone deficiency affects about 1 in 3500 children.
Growth hormone levels. Growth hormone deficiency affects about 1 in 3500 children.
 HIV testing if vertical transmission of HIV is suspected.
HIV testing if vertical transmission of HIV is suspected.
TOP TIPS
 Remember that 3% of normal infants fall below the third centile. Ask about height of other parent and grandparents in an otherwise healthy child. A constitutionally small child’s growth will still follow the centile curves albeit from a low starting point.
Remember that 3% of normal infants fall below the third centile. Ask about height of other parent and grandparents in an otherwise healthy child. A constitutionally small child’s growth will still follow the centile curves albeit from a low starting point.
 A third of children with psychosocial failure to thrive are developmentally delayed and have social and emotional problems.
A third of children with psychosocial failure to thrive are developmentally delayed and have social and emotional problems.
 If parents are small, and there is no other sign of an underlying problem, it is safe to wait and observe the baby with regular weight measurements. The baby should return to running parallel with the centiles after the second year.
If parents are small, and there is no other sign of an underlying problem, it is safe to wait and observe the baby with regular weight measurements. The baby should return to running parallel with the centiles after the second year.

 A diagnosis of a non-organic cause of failure to thrive may be the earliest indication of a serious parent–child interaction dysfunction.
A diagnosis of a non-organic cause of failure to thrive may be the earliest indication of a serious parent–child interaction dysfunction.
 Non-organically caused failure to thrive in the first year of life has an ominous prognosis. There is a high likelihood of ongoing child abuse in this group.
Non-organically caused failure to thrive in the first year of life has an ominous prognosis. There is a high likelihood of ongoing child abuse in this group.
 If child abuse is suspected, refer to paediatrics urgently – by admission to hospital.
If child abuse is suspected, refer to paediatrics urgently – by admission to hospital.
 The younger and more ill a child or baby is at presentation with failure to thrive, the more urgently assessment and action are required.
The younger and more ill a child or baby is at presentation with failure to thrive, the more urgently assessment and action are required.
 A study has shown that half of cases of organic failure to thrive were also associated with a contributory psychosocial factor. Be alert to the fact that this can be a multifactorial condition.
A study has shown that half of cases of organic failure to thrive were also associated with a contributory psychosocial factor. Be alert to the fact that this can be a multifactorial condition.
FALLS WITH NO LOSS OF CONSCIOUSNESS
![]()
The GP overview
This is a common problem in the elderly and may represent an acute or chronic problem. A home visit is often necessary and can be very valuable, assisting diagnosis and management decisions.
NOTE: The term ‘drop attacks’ is inconsistently defined in the literature as ‘falls with no loss of consciousness’, ‘falls with loss of consciousness’ or may be regarded as a distinct diagnostic entity rather than a symptom. It is a term best left unused.
![]()
Differential diagnosis
COMMON
 orthostatic hypotension
orthostatic hypotension
 brainstem ischaemia (vertebrobasilar insufficiency)
brainstem ischaemia (vertebrobasilar insufficiency)
 iatrogenic (e.g. phenothiazines, hypoglycaemics, tricyclics and hypotensives)
iatrogenic (e.g. phenothiazines, hypoglycaemics, tricyclics and hypotensives)
 postural instability (osteoarthritis, quadriceps weakness)
postural instability (osteoarthritis, quadriceps weakness)
 any acute illness (e.g. sepsis, CVA)
any acute illness (e.g. sepsis, CVA)
OCCASIONAL
 lack of concentration (tripping over mats etc.)
lack of concentration (tripping over mats etc.)
 visual disturbance
visual disturbance
 acute alcohol intoxication and chronic alcohol misuse
acute alcohol intoxication and chronic alcohol misuse
 Parkinson’s disease
Parkinson’s disease
 cardiac arrhythmias
cardiac arrhythmias
 any cause of vertigo (e.g. labyrinthitis, Ménière’s disease) or non-specific dizziness (e.g. anaemia)
any cause of vertigo (e.g. labyrinthitis, Ménière’s disease) or non-specific dizziness (e.g. anaemia)
RARE
 hypothyroidism
hypothyroidism
 hydrocephalus
hydrocephalus
 third ventricular tumour
third ventricular tumour
 diabetic autonomic neuropathy
diabetic autonomic neuropathy
 aortic stenosis
aortic stenosis
 painless (‘silent’) myocardial infarction
painless (‘silent’) myocardial infarction
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: urinalysis, FBC.
POSSIBLE: TFT, LFT, ECG (or 24 h ECG).
SMALL PRINT: CT scan, echocardiography.
 Urinalysis for glucose may reveal underlying diabetes – a major cause of autonomic neuropathy – or evidence of UTI.
Urinalysis for glucose may reveal underlying diabetes – a major cause of autonomic neuropathy – or evidence of UTI.
 FBC: anaemia will exacerbate any cause of postural hypotension, or may itself cause dizziness. Sepsis is suggested by a raised WCC. A high MCV may be a useful pointer to alcohol misuse or hypothyroidism.
FBC: anaemia will exacerbate any cause of postural hypotension, or may itself cause dizziness. Sepsis is suggested by a raised WCC. A high MCV may be a useful pointer to alcohol misuse or hypothyroidism.
 TFT: hypothyroidism is common in the elderly and develops insidiously.
TFT: hypothyroidism is common in the elderly and develops insidiously.
 LFT: for evidence (γGT) of alcohol misuse.
LFT: for evidence (γGT) of alcohol misuse.
 ECG or 24 h ECG is useful to identify an arrhythmia, conduction defect or MI.
ECG or 24 h ECG is useful to identify an arrhythmia, conduction defect or MI.
 CT scanning (e.g. for tumours or hydrocephalus) or echocardiography (for aortic stenosis) may be arranged by the specialist after referral.
CT scanning (e.g. for tumours or hydrocephalus) or echocardiography (for aortic stenosis) may be arranged by the specialist after referral.
TOP TIPS
 Failure to observe the patient’s gait may mean that significant diagnoses, such as Parkinson’s disease, are missed.
Failure to observe the patient’s gait may mean that significant diagnoses, such as Parkinson’s disease, are missed.
 Recurrent falls in the elderly are often caused by a combination of factors, such as failing vision, poor lighting and trip hazards at home. A home assessment may give valuable clues.
Recurrent falls in the elderly are often caused by a combination of factors, such as failing vision, poor lighting and trip hazards at home. A home assessment may give valuable clues.
 In the acute situation, management may depend more upon the ability of the patient to remain safely at home (e.g. social support) rather than the precise diagnosis.
In the acute situation, management may depend more upon the ability of the patient to remain safely at home (e.g. social support) rather than the precise diagnosis.
 Don’t underestimate the importance of what you prescribe in causing morbidity. Attempt to reduce polypharmacy and review therapy regularly.
Don’t underestimate the importance of what you prescribe in causing morbidity. Attempt to reduce polypharmacy and review therapy regularly.
 In dealing with this problem, don’t forget to look for cause and effect: the aetiology of the falls and any significant injuries sustained.
In dealing with this problem, don’t forget to look for cause and effect: the aetiology of the falls and any significant injuries sustained.
 Sudden onset of falls in the previously well elderly patient is likely to represent acute pathology – have a low threshold for investigation or admission.
Sudden onset of falls in the previously well elderly patient is likely to represent acute pathology – have a low threshold for investigation or admission.
 Gradual onset of recurrent falls is often multifactorial in the elderly; in younger patients, specific underlying disease is more likely, so refer for investigation.
Gradual onset of recurrent falls is often multifactorial in the elderly; in younger patients, specific underlying disease is more likely, so refer for investigation.
 Evidence of injury (e.g. bruises or fractures) and multiple attendance slips from A&E department indicate either a very frail, vulnerable elderly person or significant underlying illness.
Evidence of injury (e.g. bruises or fractures) and multiple attendance slips from A&E department indicate either a very frail, vulnerable elderly person or significant underlying illness.
THE FEBRILE CHILD
![]()
The GP overview
This symptom probably generates more GP advice calls and parental anxiety than any other. It is nearly always caused by an infection of some kind. The list of culprits is so vast that we have concentrated on the common and occasional ones more likely to be seen in general practice in the UK.
![]()
Differential diagnosis
COMMON
 non-specific viral URTI, e.g. colds, flu-type illness, pharyngitis, tracheitis
non-specific viral URTI, e.g. colds, flu-type illness, pharyngitis, tracheitis
 gastroenteritis
gastroenteritis
 otitis media
otitis media
 tonsillitis
tonsillitis
 chest infection
chest infection
OCCASIONAL
 urinary tract infection
urinary tract infection
 bronchiolitis
bronchiolitis
 croup
croup
 common viral exanthems, e.g. chickenpox, roseola, hand, foot and mouth, fifth disease
common viral exanthems, e.g. chickenpox, roseola, hand, foot and mouth, fifth disease
 appendicitis
appendicitis
 cellulitis (especially orbital) and other significant skin infections, e.g. abscess, scalded skin
cellulitis (especially orbital) and other significant skin infections, e.g. abscess, scalded skin
 glandular fever
glandular fever
 post-immunisation
post-immunisation
 giardiasis
giardiasis
RARE
 meningitis/meningococcal septicaemia
meningitis/meningococcal septicaemia
 encephalitis
encephalitis
 hepatitis
hepatitis
 AIDS
AIDS
 rare exanthems, e.g. measles, rubella
rare exanthems, e.g. measles, rubella
 mumps
mumps
 acute epiglottitis
acute epiglottitis
 atypical infections, e.g. brucellosis, listeriosis, Lyme disease, cat scratch fever
atypical infections, e.g. brucellosis, listeriosis, Lyme disease, cat scratch fever
 tuberculosis
tuberculosis
 protozoal diseases, e.g. cryptosporidium, leishmaniasis, toxoplasmosis, malaria
protozoal diseases, e.g. cryptosporidium, leishmaniasis, toxoplasmosis, malaria
 septic arthritis, osteomyelitis
septic arthritis, osteomyelitis
 Kawasaki’s disease
Kawasaki’s disease
![]()
Ready reckoner

![]()
Possible investigations
Usually none are necessary in practice. If a febrile child is ill enough to require investigation, the problem will usually be sufficiently urgent to need management by acute admission. Urinalysis, as a pointer to UTI (assuming obtaining a urine sample is feasible), is sometimes helpful in avoiding or facilitating admission. If possible, extend this to an MSU for bacteriological analysis.
TOP TIPS
 Many clinical markers (see Ready reckoner) are non-specific and are present in many different infections. It is often a matter of degree as to how likely they are a pointer to a specific pathology. For example, many infections cause mesenteric adenitis with abdominal pain, but the tenderness of appendicitis, for example, is usually far greater on examination. Respiratory rate is raised in all fevers, but a chest problem will increase it further along with the presence of chest signs. A good policy is to be as thorough as possible in an examination so as to be able to cross-reference the maximum clinical information.
Many clinical markers (see Ready reckoner) are non-specific and are present in many different infections. It is often a matter of degree as to how likely they are a pointer to a specific pathology. For example, many infections cause mesenteric adenitis with abdominal pain, but the tenderness of appendicitis, for example, is usually far greater on examination. Respiratory rate is raised in all fevers, but a chest problem will increase it further along with the presence of chest signs. A good policy is to be as thorough as possible in an examination so as to be able to cross-reference the maximum clinical information.
 Remember that parents will be worried about their child, and no matter how simple the management of this common problem appears to you, to the parent it may be the harbinger of a serious illness. Practise a calm and polite demeanour, empathy and sensitivity.
Remember that parents will be worried about their child, and no matter how simple the management of this common problem appears to you, to the parent it may be the harbinger of a serious illness. Practise a calm and polite demeanour, empathy and sensitivity.
 In telephone advice calls, always do three things: first, check that the parent is satisfied with your advice; second, put a robust safety net/plan B in place with easily identifiable guidelines for the parent, e.g. ‘if by X hours Y has not happened, then call back’; third, record your clinical assessment and the last two points in detail.
In telephone advice calls, always do three things: first, check that the parent is satisfied with your advice; second, put a robust safety net/plan B in place with easily identifiable guidelines for the parent, e.g. ‘if by X hours Y has not happened, then call back’; third, record your clinical assessment and the last two points in detail.
 If in doubt, always see a child in person. Be sensitive to your intuition. If something nags you after an advice call, ring back and arrange a consultation. You will never look stupid for doing this – only careful.
If in doubt, always see a child in person. Be sensitive to your intuition. If something nags you after an advice call, ring back and arrange a consultation. You will never look stupid for doing this – only careful.
 Remember to follow up children in whom you’ve diagnosed UTI according to NICE guidelines, which recommend further investigation, varying according to the age of the child.
Remember to follow up children in whom you’ve diagnosed UTI according to NICE guidelines, which recommend further investigation, varying according to the age of the child.
 It is very easy to print computerised clinical notes immediately after writing them. Handing a consultation note to a parent can be invaluable to the parent (and the clinician) if the child is seen later on out of hours, when clinical records are often unavailable. The baseline findings from earlier in the day can be priceless information in the dark hours later on.
It is very easy to print computerised clinical notes immediately after writing them. Handing a consultation note to a parent can be invaluable to the parent (and the clinician) if the child is seen later on out of hours, when clinical records are often unavailable. The baseline findings from earlier in the day can be priceless information in the dark hours later on.
 Spend time explaining the nature of fever and that the key issue is the cause of the fever rather than the fever itself – many parents are ‘fever phobic’.
Spend time explaining the nature of fever and that the key issue is the cause of the fever rather than the fever itself – many parents are ‘fever phobic’.
 It’s often more important to be able to distinguish between ‘well’ and ‘ill’ babies and children than it is to make a clever, precise diagnosis – the NICE ‘traffic light’ guidance may help.
It’s often more important to be able to distinguish between ‘well’ and ‘ill’ babies and children than it is to make a clever, precise diagnosis – the NICE ‘traffic light’ guidance may help.
 It’s easy to be tempted into complacency in the telephone or consultation management of this problem – fever is just so common. Never forget that uncommon very serious illnesses may all begin with a fever. Always be diligent and systematic in assessment, no matter how busy your winter on-call day is turning out to be.
It’s easy to be tempted into complacency in the telephone or consultation management of this problem – fever is just so common. Never forget that uncommon very serious illnesses may all begin with a fever. Always be diligent and systematic in assessment, no matter how busy your winter on-call day is turning out to be.

 Dehydration can kill a baby quickly. Ensure you have satisfied yourself about the state of hydration of a child. The colour and quantity of urine passed, or frequency of nappy changes are useful practical guides, together with the general ‘look’ of the child and the capillary refill time.
Dehydration can kill a baby quickly. Ensure you have satisfied yourself about the state of hydration of a child. The colour and quantity of urine passed, or frequency of nappy changes are useful practical guides, together with the general ‘look’ of the child and the capillary refill time.
 A febrile baby or child who is floppy or drowsy should be admitted immediately.
A febrile baby or child who is floppy or drowsy should be admitted immediately.
 Be suspicious of the irritable and inconsolable infant. Even without other hard evidence, suspect a serious problem and arrange urgent paediatric assessment.
Be suspicious of the irritable and inconsolable infant. Even without other hard evidence, suspect a serious problem and arrange urgent paediatric assessment.
 The petechial rash of meningococcal septicaemia is a late phenomenon. Do not be reassured by its absence. Its presence should prompt a 999 call and administration of immediate parenteral antibiotics according to local protocols.
The petechial rash of meningococcal septicaemia is a late phenomenon. Do not be reassured by its absence. Its presence should prompt a 999 call and administration of immediate parenteral antibiotics according to local protocols.
 In most cases, the height of a fever is no guide to the severity of the illness – the exception being babies, where a temperature of 38°C or more in those under 3 months is seen as a ‘red’ and one of 39°C or more in those between 3 and 6 months is viewed as ‘amber’ according to NICE.
In most cases, the height of a fever is no guide to the severity of the illness – the exception being babies, where a temperature of 38°C or more in those under 3 months is seen as a ‘red’ and one of 39°C or more in those between 3 and 6 months is viewed as ‘amber’ according to NICE.
FEELING TENSE AND ANXIOUS
![]()
The GP overview
The patient complaining of feeling tense and anxious may induce similar feelings in the GP – because there are many possible underlying and contributory causes, the consultation may be lengthy, and the patient may well present in a crisis. A calm, methodical approach, possibly stretching over more than one consultation, will pay dividends.
![]()
Differential diagnosis
COMMON
 life events (may be underlying ‘anxious personality’)
life events (may be underlying ‘anxious personality’)
 pre-menstrual tension
pre-menstrual tension
 generalised anxiety disorder
generalised anxiety disorder
 panic disorder
panic disorder
 depression
depression
OCCASIONAL
 obsessive–compulsive disorder
obsessive–compulsive disorder
 phobias
phobias
 drug side effect (for example, in the early stages of SSRI treatment)
drug side effect (for example, in the early stages of SSRI treatment)
 hyperthyroidism
hyperthyroidism
 drug/alcohol use or withdrawal
drug/alcohol use or withdrawal
 somatisation disorder
somatisation disorder
 post-traumatic stress disorder
post-traumatic stress disorder
RARE
 psychotic illness
psychotic illness
 any cause of palpitations (may be ‘misinterpreted’ by the patient or others as anxiety)
any cause of palpitations (may be ‘misinterpreted’ by the patient or others as anxiety)
 organic brain disease, e.g. tumour
organic brain disease, e.g. tumour
![]()
Ready reckoner

![]()
Possible investigations
It would be very unusual for the GP to require any investigations when dealing with this symptom. Thyroid function tests would be indicated in suspected hyperthyroidism, and a blood screen, to include LFT, if alcohol was thought to be playing a significant part. Investigations in the rare event of suspected organic brain disease would usually be left to the specialist.
TOP TIPS
 It is tempting to lump many of these scenarios under a catch-all label of ‘tension’ or ‘anxiety’. But attempts at making a more precise diagnosis are worthwhile, as this may significantly alter the management.
It is tempting to lump many of these scenarios under a catch-all label of ‘tension’ or ‘anxiety’. But attempts at making a more precise diagnosis are worthwhile, as this may significantly alter the management.
 Do not overlook an alcohol or drug history: abuse or withdrawal may be the cause of the symptoms, or a significant contributor.
Do not overlook an alcohol or drug history: abuse or withdrawal may be the cause of the symptoms, or a significant contributor.
 It may be worthwhile carefully reviewing the patient’s old records to establish patterns of symptoms or attendance, and to check previous response to treatment.
It may be worthwhile carefully reviewing the patient’s old records to establish patterns of symptoms or attendance, and to check previous response to treatment.
 Whenever possible, life events should not be ‘medicalised’ – otherwise this may, in the future, encourage re-attendance and foster dependence on treatment.
Whenever possible, life events should not be ‘medicalised’ – otherwise this may, in the future, encourage re-attendance and foster dependence on treatment.
 Apparent pre-menstrual tension may be a sign of some other underlying disorder – the patient may be suffering generalised anxiety disorder, for example, but may tend to focus on the pre-menstrual phase, when the symptoms are at their worst.
Apparent pre-menstrual tension may be a sign of some other underlying disorder – the patient may be suffering generalised anxiety disorder, for example, but may tend to focus on the pre-menstrual phase, when the symptoms are at their worst.
 Do not accept a self-diagnosis of ‘panic attacks’ at face value – the patient may actually mean any one of a number of possible symptoms.
Do not accept a self-diagnosis of ‘panic attacks’ at face value – the patient may actually mean any one of a number of possible symptoms.
 If the underlying diagnosis turns out to be depression, assess for any suicidal ideas or intent.
If the underlying diagnosis turns out to be depression, assess for any suicidal ideas or intent.
 Check for any psychotic features – anxiety can occasionally be a presenting feature of serious psychotic illness.
Check for any psychotic features – anxiety can occasionally be a presenting feature of serious psychotic illness.
 New onset of tension or anxiety without any obvious explanation – especially in the context of personality change, neurological features or new headaches – could, rarely, reflect organic brain disease.
New onset of tension or anxiety without any obvious explanation – especially in the context of personality change, neurological features or new headaches – could, rarely, reflect organic brain disease.
 It’s important to make diagnoses such as somatisation disorder when appropriate – otherwise the patient may suffer years of unnecessary tests and treatment.
It’s important to make diagnoses such as somatisation disorder when appropriate – otherwise the patient may suffer years of unnecessary tests and treatment.
FLUSHING
![]()
The GP overview
This symptom presents more often in women than in men, not only because of its cosmetic importance, but also because the menopause accounts for the vast majority of presentations. It is different from emotional blushing in its context, severity, duration and extent.
![]()
Differential diagnosis
COMMON
 menopause
menopause
 chronic alcohol misuse
chronic alcohol misuse
 rosacea
rosacea
 iatrogenic (e.g. calcium antagonists)
iatrogenic (e.g. calcium antagonists)
 anxiety
anxiety
OCCASIONAL
 polycythaemia rubra vera
polycythaemia rubra vera
 hyperthyroidism
hyperthyroidism
 drug/alcohol interaction: metronidazole, disulfiram
drug/alcohol interaction: metronidazole, disulfiram
 mitral valve disease (malar flush)
mitral valve disease (malar flush)
 hyperglycaemia and hypoglycaemia
hyperglycaemia and hypoglycaemia
 epilepsy (aura)
epilepsy (aura)
RARE
 carcinoid tumour
carcinoid tumour
 phaeochromocytoma
phaeochromocytoma
 Zollinger–Ellison syndrome
Zollinger–Ellison syndrome
 systemic mastocytosis
systemic mastocytosis
 ACTH-secreting bronchogenic carcinoma and Cushing’s syndrome
ACTH-secreting bronchogenic carcinoma and Cushing’s syndrome
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: none.
POSSIBLE: FBC, LFT, TFT, blood sugar.
SMALL PRINT: echocardiogram, EEG, urinary 5HIAA and VMA, gastrin level, further specialised endocrine tests.
 FBC: raised haemoglobin and PCV in polycythaemia (may also be elevated platelets and WCC), raised MCV in chronic alcohol misuse.
FBC: raised haemoglobin and PCV in polycythaemia (may also be elevated platelets and WCC), raised MCV in chronic alcohol misuse.
 Biochemistry: LFT and γGT abnormal in alcohol misuse. TFT will reveal hyperthyroidism.
Biochemistry: LFT and γGT abnormal in alcohol misuse. TFT will reveal hyperthyroidism.
 Blood sugar: to reveal hypo- or hyperglycaemia.
Blood sugar: to reveal hypo- or hyperglycaemia.
 FSH/LH of limited use as does not correlate well with symptoms (useful only if premature menopause suspected).
FSH/LH of limited use as does not correlate well with symptoms (useful only if premature menopause suspected).
 Echocardiography: if mitral stenosis suspected.
Echocardiography: if mitral stenosis suspected.
 EEG: for possible epilepsy.
EEG: for possible epilepsy.
 Specialist tests might include urinary 5HIAA (carcinoid) and VMA (phaeochromocytoma), gastrin level (Zollinger–Ellison syndrome) and further endocrine tests (e.g. for Cushing’s syndrome).
Specialist tests might include urinary 5HIAA (carcinoid) and VMA (phaeochromocytoma), gastrin level (Zollinger–Ellison syndrome) and further endocrine tests (e.g. for Cushing’s syndrome).
TOP TIPS
 Most women complaining of flushing will suspect the cause is the menopause. Address this possibility in the consultation, especially in young women fearing ‘an early change’.
Most women complaining of flushing will suspect the cause is the menopause. Address this possibility in the consultation, especially in young women fearing ‘an early change’.
 A constantly flushed face in older men is likely to be due to alcohol, polycythaemia or rosacea.
A constantly flushed face in older men is likely to be due to alcohol, polycythaemia or rosacea.
 Anxiety is likely if the circumstances fit – but bear in mind that hyperthyroidism can produce a very similar clinical picture.
Anxiety is likely if the circumstances fit – but bear in mind that hyperthyroidism can produce a very similar clinical picture.
 It can be difficult to distinguish anxiety from menopausal symptoms in a woman of menopausal age. Flushes with sweats waking the woman at night are more likely to be caused by the menopause – but a trial of treatment is the acid test (though beware of an initial placebo response).
It can be difficult to distinguish anxiety from menopausal symptoms in a woman of menopausal age. Flushes with sweats waking the woman at night are more likely to be caused by the menopause – but a trial of treatment is the acid test (though beware of an initial placebo response).
 Diarrhoea and dyspnoea with flushing after alcohol, food and exercise suggest possible carcinoid syndrome.
Diarrhoea and dyspnoea with flushing after alcohol, food and exercise suggest possible carcinoid syndrome.
 Flushing followed by an episode of altered consciousness points to a significant cause, such as recurrent hypoglycaemia or epilepsy.
Flushing followed by an episode of altered consciousness points to a significant cause, such as recurrent hypoglycaemia or epilepsy.
 Do not be tempted to write this symptom off as the hot flushes of emotional blushing. While common, this problem is unlikely to present in daily practice.
Do not be tempted to write this symptom off as the hot flushes of emotional blushing. While common, this problem is unlikely to present in daily practice.
 Recent onset of severe flushing which is not obviously menopausal or anxiety may have a significant cause, especially if the patient has other symptoms. Have a low threshold for investigations or referral in such cases.
Recent onset of severe flushing which is not obviously menopausal or anxiety may have a significant cause, especially if the patient has other symptoms. Have a low threshold for investigations or referral in such cases.
INFERTILITY
![]()
The GP overview
About 80% of couples conceive within the first year of trying, and a further 5–10% in the second. Infertility is defined as a failure to conceive after 2 years of regular intercourse. However, depending on the circumstances, it may be appropriate for the GP to intervene before this arbitrary 2-year cut-off. Management is likely to be dictated by prevailing national and local guidelines and protocols.
![]()
Differential diagnosis
COMMON
 unexplained (27%)
unexplained (27%)
 defective sperm (24% – may be various underlying causes)
defective sperm (24% – may be various underlying causes)
 anovulatory cycles/defective ovulation (21%)
anovulatory cycles/defective ovulation (21%)
 fallopian tube blockage (14%)
fallopian tube blockage (14%)
 endometriosis (6%)
endometriosis (6%)
OCCASIONAL
 hostile cervical mucus
hostile cervical mucus
 PCOS
PCOS
 other causes of amenorrhoea or hypomenorrhoea (see Absent periods, p. 374)
other causes of amenorrhoea or hypomenorrhoea (see Absent periods, p. 374)
 uterine fibroids, polyp
uterine fibroids, polyp
 cervical problems: inflammation, polyps, stenosis
cervical problems: inflammation, polyps, stenosis
 systemic illness, e.g. anaemia, thyroid disorders
systemic illness, e.g. anaemia, thyroid disorders
RARE
 congenital uterine, vaginal, fallopian or ovarian malformation or absence
congenital uterine, vaginal, fallopian or ovarian malformation or absence
 sexual dysfunction
sexual dysfunction
 adrenocortical tumours
adrenocortical tumours
 chromosomal abnormalities: Turner’s syndrome (XO), super-female (XXX)
chromosomal abnormalities: Turner’s syndrome (XO), super-female (XXX)
 endometrial tuberculosis
endometrial tuberculosis
![]()
Ready reckoner

![]()
Possible investigations
NOTE: amenorrhoea will need investigation in its own right – see Absent periods, p. 374. The degree of investigation undertaken for infertility will depend very much on the particular situation and local guidelines.
LIKELY: semen analysis, serum progesterone 7 days before anticipated onset of period.
POSSIBLE: if menstrual irregularity/amenorrhoea/unwell – FBC, FSH, LH, prolactin, TFT, U&E, testosterone. In secondary care: ovarian/uterine ultrasound.
SMALL PRINT: laparoscopy and dye, hysterosalpingogram, post-coital test. In the male: further investigation of sperm problems, e.g. FSH, LH, testosterone, testicular ultrasound.
 Semen analysis: may need repeating if first test sub-optimal.
Semen analysis: may need repeating if first test sub-optimal.
 Serum progesterone 7 days before anticipated onset of period: to check for ovulation.
Serum progesterone 7 days before anticipated onset of period: to check for ovulation.
 FBC, FSH, LH, prolactin, TFT, U&E, testosterone: to check for underlying pathology if female is unwell or has menstrual problems.
FBC, FSH, LH, prolactin, TFT, U&E, testosterone: to check for underlying pathology if female is unwell or has menstrual problems.
 Ovarian and uterine ultrasound: to exclude structural abnormalities. Can be extended to visualise ovarian follicle development and ovulation.
Ovarian and uterine ultrasound: to exclude structural abnormalities. Can be extended to visualise ovarian follicle development and ovulation.
 Laparoscopy and dye, hysterosalpingogram: to check for tubal patency.
Laparoscopy and dye, hysterosalpingogram: to check for tubal patency.
 Post-coital test: cervical mucus sampled 12 hours post-coitally is examined under high-power microscope. More than 10 motile sperm per high-power field implies satisfactory coitus, adequate sperm and antibody-free cervical mucus.
Post-coital test: cervical mucus sampled 12 hours post-coitally is examined under high-power microscope. More than 10 motile sperm per high-power field implies satisfactory coitus, adequate sperm and antibody-free cervical mucus.
 Male FSH, LH and testosterone: to check for endocrine causes of sperm production failure.
Male FSH, LH and testosterone: to check for endocrine causes of sperm production failure.
 Testicular ultrasound: if anatomical abnormalities found on examination, e.g. varicocoele.
Testicular ultrasound: if anatomical abnormalities found on examination, e.g. varicocoele.
TOP TIPS
 Adopt an optimistic approach whenever possible. A surprising number of couples conceive successfully as soon as preliminary investigations are initiated!
Adopt an optimistic approach whenever possible. A surprising number of couples conceive successfully as soon as preliminary investigations are initiated!
 Don’t overlook health promotion opportunities – especially female rubella status and advice about taking folic acid.
Don’t overlook health promotion opportunities – especially female rubella status and advice about taking folic acid.
 In primary care, hormone tests (other than progesterone) are not necessary if the periods are normal.
In primary care, hormone tests (other than progesterone) are not necessary if the periods are normal.

 Infertility will only very rarely be the presenting symptom of serious pathology. However, there are circumstances where it is important to act promptly in terms of investigation or referral, such as:
Infertility will only very rarely be the presenting symptom of serious pathology. However, there are circumstances where it is important to act promptly in terms of investigation or referral, such as:
 if the female
if the female
– is over the age of 35
– has amenorrhoea
– has a history of previous pelvic surgery or PID
– has any abnormality on pelvic examination
 or if the male
or if the male
– has a history of urogenital problems or STD
– has a varicocoele.
ITCHING
![]()
The GP overview
Itching is the commonest presenting dermatological symptom. It is frequently distressing, and may interfere with the patient’s quality of life – for example, by preventing normal sleep. Therefore, it should be taken seriously. A good history alone will reveal the diagnosis in the majority of cases. The remainder will yield to thorough examination and investigation. Dermatological referral need only be a last resort to achieve diagnosis.
![]()
Differential diagnosis
COMMON
 contact allergy (contact dermatitis)
contact allergy (contact dermatitis)
 scabies (and other pediculoses)
scabies (and other pediculoses)
 atopic eczema
atopic eczema
 pityriasis rosea
pityriasis rosea
 psoriasis
psoriasis
OCCASIONAL
 urticaria (e.g. food or drug allergy)
urticaria (e.g. food or drug allergy)
 jaundice of any cause
jaundice of any cause
 iron deficiency anaemia
iron deficiency anaemia
 endocrine: diabetes mellitus, hypo- and hyperthyroidism
endocrine: diabetes mellitus, hypo- and hyperthyroidism
 renal failure (uraemia)
renal failure (uraemia)
 lichen planus
lichen planus
 prickly heat
prickly heat
RARE
 herpes gestationis
herpes gestationis
 dermatitis herpetiformis
dermatitis herpetiformis
 psychogenic (includes dermatitis artefacta)
psychogenic (includes dermatitis artefacta)
 leukaemia and myeloproliferative disorders
leukaemia and myeloproliferative disorders
 simple pruritus: no other cause found
simple pruritus: no other cause found
 drug side effect (with or without rash)
drug side effect (with or without rash)
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: none.
POSSIBLE: urinalysis, blood glucose or HbA1c, FBC, ESR, U&E, LFT, TFT.
SMALL PRINT: none.
 Urine: dipstick for glycosuria (blood glucose or HbA1c if positive).
Urine: dipstick for glycosuria (blood glucose or HbA1c if positive).
 FBC: will reveal iron-deficiency anaemia and polycythaemia; eosinophil count may be raised in allergic conditions; WCC may be very high in leukaemia; ESR may be elevated in lymphoma.
FBC: will reveal iron-deficiency anaemia and polycythaemia; eosinophil count may be raised in allergic conditions; WCC may be very high in leukaemia; ESR may be elevated in lymphoma.
 U&E: will reveal uraemia.
U&E: will reveal uraemia.
 LFT: deranged liver enzymes and raised bilirubin in liver disease.
LFT: deranged liver enzymes and raised bilirubin in liver disease.
 TFT: both hypo- and hyperthyroidism can lead to skin changes which cause itching.
TFT: both hypo- and hyperthyroidism can lead to skin changes which cause itching.
TOP TIPS
 An itchy, unidentifiable rash which is worse at night is likely to be scabies, particularly if any contacts are affected.
An itchy, unidentifiable rash which is worse at night is likely to be scabies, particularly if any contacts are affected.
 Warn the patient that scabies treatment may take a week or two fully to relieve symptoms – otherwise, the patient may apply the treatment repeatedly, causing a chemical irritation and diagnostic confusion.
Warn the patient that scabies treatment may take a week or two fully to relieve symptoms – otherwise, the patient may apply the treatment repeatedly, causing a chemical irritation and diagnostic confusion.
 The books usually state that psoriasis doesn’t itch – but it certainly can, so don’t let this symptom put you off the diagnosis.
The books usually state that psoriasis doesn’t itch – but it certainly can, so don’t let this symptom put you off the diagnosis.
 It is usually very difficult to identify the allergen in a single episode of urticaria. Tell the patient to keep a note of foods or medicines just ingested so that, in the event of recurrence, the culprit can be identified.
It is usually very difficult to identify the allergen in a single episode of urticaria. Tell the patient to keep a note of foods or medicines just ingested so that, in the event of recurrence, the culprit can be identified.
 If no obvious cause, always examine the abdomen and lymph nodes: do not miss lymphadenopathy, or enlarged liver, spleen or kidneys.
If no obvious cause, always examine the abdomen and lymph nodes: do not miss lymphadenopathy, or enlarged liver, spleen or kidneys.
 Don’t be tempted not to examine the itchy, malodorous self-neglected patient: poor personal hygiene may deceptively mask some other identifiable underlying cause.
Don’t be tempted not to examine the itchy, malodorous self-neglected patient: poor personal hygiene may deceptively mask some other identifiable underlying cause.
 Beware of apparently florid eczema appearing for the first time in an elderly patient – this may be a manifestation of serious underlying pathology.
Beware of apparently florid eczema appearing for the first time in an elderly patient – this may be a manifestation of serious underlying pathology.
 Don’t forget iatrogenic causes – enquire about any drugs recently prescribed.
Don’t forget iatrogenic causes – enquire about any drugs recently prescribed.
JAUNDICE IN ADULTS
![]()
The GP overview
Patients rarely present with the complaint of ‘turning yellow’; more often – though still infrequently – the GP notices jaundice during an examination of the patient. A systematic clinical assessment together with relevant laboratory investigations will help pinpoint the cause.
![]()
Differential diagnosis
COMMON
 gallstones in common bile duct
gallstones in common bile duct
 viral hepatitis (e.g. glandular fever, hepatitis A, B, C)
viral hepatitis (e.g. glandular fever, hepatitis A, B, C)
 carcinoma of head of pancreas
carcinoma of head of pancreas
 hepatic carcinoma (usually metastases)
hepatic carcinoma (usually metastases)
 alcoholic cirrhosis
alcoholic cirrhosis
OCCASIONAL
 alcoholic hepatitis
alcoholic hepatitis
 primary biliary cirrhosis
primary biliary cirrhosis
 drugs: chlorpromazine, isoniazid, anabolic steroids, methyldopa, paracetamol overdose
drugs: chlorpromazine, isoniazid, anabolic steroids, methyldopa, paracetamol overdose
 haemolytic anaemia (many causes, such as autoimmune, malaria, drugs)
haemolytic anaemia (many causes, such as autoimmune, malaria, drugs)
 venous congestion: cardiac failure, constrictive pericarditis
venous congestion: cardiac failure, constrictive pericarditis
 cholangitis (and stricture in common bile duct afterwards)
cholangitis (and stricture in common bile duct afterwards)
 pancreatitis
pancreatitis
RARE
 carcinoma of bile duct
carcinoma of bile duct
 leptospirosis
leptospirosis
 Rotor, Dubin–Johnson and Mirizzi syndromes
Rotor, Dubin–Johnson and Mirizzi syndromes
 cholestasis or fatty liver of pregnancy
cholestasis or fatty liver of pregnancy
 genetic: Gilbert’s syndrome, Wilson’s disease, α1-antitrypsin deficiency, galactosaemia, glycogen storage diseases, haemochromatosis
genetic: Gilbert’s syndrome, Wilson’s disease, α1-antitrypsin deficiency, galactosaemia, glycogen storage diseases, haemochromatosis
 amyloidosis
amyloidosis
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: urinalysis, FBC, LFT, hepatitis serology.
POSSIBLE: ultrasound, antimitochondrial antibody.
SMALL PRINT: serum amylase, secondary care tests (e.g. ERCP, liver biopsy).
 Urinalysis: if bilirubin is present in the urine, the jaundice is cholestatic. If present with urobilinogen, it is hepatocellular. If not, it is obstructive.
Urinalysis: if bilirubin is present in the urine, the jaundice is cholestatic. If present with urobilinogen, it is hepatocellular. If not, it is obstructive.
 LFT: bilirubin very high in biliary obstruction. AST and ALT raised in hepatic causes. Alkaline phosphatase rises moderately in hepatic causes and markedly in biliary obstruction and primary biliary cirrhosis.
LFT: bilirubin very high in biliary obstruction. AST and ALT raised in hepatic causes. Alkaline phosphatase rises moderately in hepatic causes and markedly in biliary obstruction and primary biliary cirrhosis.
 FBC: anaemia in chronic illness. Raised WCC in hepatitis. May be macrocytosis, reticulocytosis and other red cell abnormalities in haemolytic anaemia. MCV raised by alcohol.
FBC: anaemia in chronic illness. Raised WCC in hepatitis. May be macrocytosis, reticulocytosis and other red cell abnormalities in haemolytic anaemia. MCV raised by alcohol.
 Hepatitis serology: may reveal cause of viral hepatitis.
Hepatitis serology: may reveal cause of viral hepatitis.
 Serum amylase: raised in pancreatitis.
Serum amylase: raised in pancreatitis.
 Antimitochondrial antibody test: positive in over 95% of patients with primary biliary cirrhosis.
Antimitochondrial antibody test: positive in over 95% of patients with primary biliary cirrhosis.
 Ultrasound useful to assess liver, pancreas and gall bladder: may reveal stones, primary tumours and metastases.
Ultrasound useful to assess liver, pancreas and gall bladder: may reveal stones, primary tumours and metastases.
 Referral may result in various other specialised tests including ERCP and liver biopsy, to establish the underlying cause.
Referral may result in various other specialised tests including ERCP and liver biopsy, to establish the underlying cause.
TOP TIPS
 Remember to look at the patient: if significant jaundice is present it will probably strike you at first glance.
Remember to look at the patient: if significant jaundice is present it will probably strike you at first glance.
 In younger patients, the diagnosis is likely to be viral hepatitis. In older age groups, the differential is much wider.
In younger patients, the diagnosis is likely to be viral hepatitis. In older age groups, the differential is much wider.
 Don’t forget iatrogenic causes. Remember too that the presence of jaundice implies liver dysfunction, so take great care if prescribing any medication.
Don’t forget iatrogenic causes. Remember too that the presence of jaundice implies liver dysfunction, so take great care if prescribing any medication.
 If the patient is well, with no pain and fever, it is reasonable to arrange initial investigations – especially LFT – and arrange for review in a day or two. Most other cases will require admission.
If the patient is well, with no pain and fever, it is reasonable to arrange initial investigations – especially LFT – and arrange for review in a day or two. Most other cases will require admission.
 Remember to ask about foreign travel, contact with travellers, drug misuse and sexual history if necessary in the suddenly jaundiced febrile patient.
Remember to ask about foreign travel, contact with travellers, drug misuse and sexual history if necessary in the suddenly jaundiced febrile patient.

 Painless progressive jaundice suggests carcinoma of pancreas. Refer urgently.
Painless progressive jaundice suggests carcinoma of pancreas. Refer urgently.
 An enlarged, knobbly, hard liver is nearly always caused by metastases.
An enlarged, knobbly, hard liver is nearly always caused by metastases.
 Beware of restlessness, poor concentration and drowsiness. These suggest fulminant hepatic failure.
Beware of restlessness, poor concentration and drowsiness. These suggest fulminant hepatic failure.
LIMP IN A CHILD
![]()
The GP overview
This is an infrequent but alarming presentation, as it may herald significant pathology and may be difficult to manage properly in an uncooperative toddler. Assessment should be methodical and patient, and follow-up arranged unless the diagnosis is obvious at the outset.
![]()
Differential diagnosis
COMMON
 trauma, including foreign body in foot (especially toddlers)
trauma, including foreign body in foot (especially toddlers)
 irritable hip (transient synovitis)
irritable hip (transient synovitis)
 acute viral infection with arthralgia
acute viral infection with arthralgia
 pauciarticular juvenile chronic arthritis (JCA: 1 in 1000)
pauciarticular juvenile chronic arthritis (JCA: 1 in 1000)
 slipped femoral epiphysis (usually over 10 years old)
slipped femoral epiphysis (usually over 10 years old)
OCCASIONAL
 Perthes’s disease (1 in 2000 between 4 and 10 years old)
Perthes’s disease (1 in 2000 between 4 and 10 years old)
 septic arthritis
septic arthritis
 idiopathic scoliosis
idiopathic scoliosis
 congenital dislocation of the hip (5–10 per 1000)
congenital dislocation of the hip (5–10 per 1000)
 acute lower abdominal pain – especially appendicitis
acute lower abdominal pain – especially appendicitis
 unequal leg length
unequal leg length
 neurological, e.g. cerebral palsy
neurological, e.g. cerebral palsy
RARE
 acute osteomyelitis
acute osteomyelitis
 rheumatic fever
rheumatic fever
 autoimmune disorders (e.g. SLE, dermatomyositis)
autoimmune disorders (e.g. SLE, dermatomyositis)
 rickets
rickets
 genuine juvenile rheumatoid arthritis
genuine juvenile rheumatoid arthritis
 malignancy affecting bone
malignancy affecting bone
 Duchenne’s muscular dystrophy
Duchenne’s muscular dystrophy
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: FBC, ESR/CRP, X-ray.
POSSIBLE: autoimmune screen.
SMALL PRINT: calcium, phosphate, alkaline phosphatase, creatine kinase, ASO titre, blood culture.
 FBC and ESR/CRP: WCC and ESR/CRP elevated in an underlying inflammatory or infective cause.
FBC and ESR/CRP: WCC and ESR/CRP elevated in an underlying inflammatory or infective cause.
 Hip X-ray: may reveal fracture, slipped femoral epiphysis, congenital dislocation, Perthes’s and other significant disorders – but may be normal in the presence of serious pathology.
Hip X-ray: may reveal fracture, slipped femoral epiphysis, congenital dislocation, Perthes’s and other significant disorders – but may be normal in the presence of serious pathology.
 Rheumatoid factor and autoimmune screen may be helpful if a connective tissue disorder is suspected.
Rheumatoid factor and autoimmune screen may be helpful if a connective tissue disorder is suspected.
 Serum calcium, phosphate and alkaline phosphatase: calcium and phosphate low, alkaline phosphatase high in rickets.
Serum calcium, phosphate and alkaline phosphatase: calcium and phosphate low, alkaline phosphatase high in rickets.
 Creatine kinase: markedly elevated in muscular dystrophy.
Creatine kinase: markedly elevated in muscular dystrophy.
 ASO titre is raised in 80% of cases of rheumatic fever.
ASO titre is raised in 80% of cases of rheumatic fever.
 In hospital, blood culture may identify the infecting organism in osteomyelitis and septic arthritis.
In hospital, blood culture may identify the infecting organism in osteomyelitis and septic arthritis.
TOP TIPS
 Never forget to examine the soles of the feet and between the toes for obvious and potentially simple to treat, non-serious causes of limp.
Never forget to examine the soles of the feet and between the toes for obvious and potentially simple to treat, non-serious causes of limp.
 It’s worth investing some time gaining the child’s confidence – this will enable you to make a proper assessment and feel positive about your management.
It’s worth investing some time gaining the child’s confidence – this will enable you to make a proper assessment and feel positive about your management.
 Parents may try to rationalise the symptom by recalling a recent minor episode of trauma which is likely to be purely coincidental.
Parents may try to rationalise the symptom by recalling a recent minor episode of trauma which is likely to be purely coincidental.
 Don’t forget referred pain. Hip pathology can cause pain in the knee.
Don’t forget referred pain. Hip pathology can cause pain in the knee.
 Marked restriction of movement and/or dramatic bony tenderness suggests a significant problem – especially fracture, septic arthritis and osteomyelitis.
Marked restriction of movement and/or dramatic bony tenderness suggests a significant problem – especially fracture, septic arthritis and osteomyelitis.
 Fever with a limp requires an urgent specialist opinion. Admit to exclude osteomyelitis or septic arthritis.
Fever with a limp requires an urgent specialist opinion. Admit to exclude osteomyelitis or septic arthritis.
 Beware the fat pubertal boy with groin pain and a limp: slipped femoral epiphysis is likely.
Beware the fat pubertal boy with groin pain and a limp: slipped femoral epiphysis is likely.
 Do not confine your assessment to the hip: for example, abdominal pain, especially appendicitis, can make a child limp.
Do not confine your assessment to the hip: for example, abdominal pain, especially appendicitis, can make a child limp.
NUMBNESS AND PARAESTHESIAE
![]()
The GP overview
Paraesthesiae and numbness are taken here to mean sensations of tingling, pins-and-needles, subjective numbness, and feelings of cold and heat. They may appear spontaneously or be a result of touching the area of skin concerned. Patients are often alarmed and may make an immediate association with serious disease. The differential is huge but most cases in primary care involve anxiety, nerve entrapment or cerebrovascular disease.
![]()
Differential diagnosis
COMMON
 anxiety with hyperventilation
anxiety with hyperventilation
 carpal tunnel (CT) syndrome
carpal tunnel (CT) syndrome
 sciatica
sciatica
 diabetic neuropathy
diabetic neuropathy
 cervical spondylosis
cervical spondylosis
OCCASIONAL
 multiple sclerosis and dorsal myelitis
multiple sclerosis and dorsal myelitis
 peripheral polyneuropathy (especially alcohol; also vitamin B12 and folate deficiency, iatrogenic, metabolic, connective tissue disorder, malignancy and rare causes such as Guillain–Barré, leprosy)
peripheral polyneuropathy (especially alcohol; also vitamin B12 and folate deficiency, iatrogenic, metabolic, connective tissue disorder, malignancy and rare causes such as Guillain–Barré, leprosy)
 stroke and TIA
stroke and TIA
 trauma/compression involving a peripheral nerve or spinal cord
trauma/compression involving a peripheral nerve or spinal cord
 migraine with focal neurological signs
migraine with focal neurological signs
RARE
 intramedullary spinal cord tumour
intramedullary spinal cord tumour
 syringomyelia
syringomyelia
 trauma, brain tumour and epilepsy affecting sensory cortex
trauma, brain tumour and epilepsy affecting sensory cortex
 hysteria
hysteria
 vascular: ischaemic heart disease, peripheral vascular disease
vascular: ischaemic heart disease, peripheral vascular disease
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: urinalysis, blood sugar or HbA1c.
POSSIBLE: FBC, LFT, γGT, U&E, serum calcium, B12 and folate, TFT, nerve conduction studies.
SMALL PRINT: autoimmune screen, cervical spine X-ray, secondary care investigations (MRI/CT scan, lumbar puncture, carotid imaging, angiography, myelography).
 Urinalysis: to pick up glycosuria in undiagnosed diabetes.
Urinalysis: to pick up glycosuria in undiagnosed diabetes.
 Blood sugar or HbA1c: to confirm diabetes.
Blood sugar or HbA1c: to confirm diabetes.
 FBC: to look for macrocytosis (sign of alcohol excess or B12/folate deficiency). May be anaemia of chronic illness or malignancy.
FBC: to look for macrocytosis (sign of alcohol excess or B12/folate deficiency). May be anaemia of chronic illness or malignancy.
 LFT and γGT if alcoholic neuropathy suspected.
LFT and γGT if alcoholic neuropathy suspected.
 Metabolic screen (including U&E, calcium, LFT, B12 and folate).
Metabolic screen (including U&E, calcium, LFT, B12 and folate).
 TFT: hypothyroidism can cause a polyneuropathy or precipitate carpal tunnel syndrome.
TFT: hypothyroidism can cause a polyneuropathy or precipitate carpal tunnel syndrome.
 Autoimmune screen: to help diagnose a connective tissue disorder.
Autoimmune screen: to help diagnose a connective tissue disorder.
 Nerve conduction studies: to confirm a diagnosis of nerve compression prior to surgical treatment.
Nerve conduction studies: to confirm a diagnosis of nerve compression prior to surgical treatment.
 X-ray cervical spine: confirms clinical diagnosis of cervical spondylosis, but not really helpful as positive findings common and don’t correlate well with symptoms, and the investigation is unlikely to alter the management.
X-ray cervical spine: confirms clinical diagnosis of cervical spondylosis, but not really helpful as positive findings common and don’t correlate well with symptoms, and the investigation is unlikely to alter the management.
 Secondary care investigations might include: lumbar puncture (MS, Guillain–Barré syndrome), carotid imaging (TIA), CT or MRI scan (spinal pathology or compression, MS, cerebral tumour, syringomyelia), angiography (vascular causes), myelography (cord compression).
Secondary care investigations might include: lumbar puncture (MS, Guillain–Barré syndrome), carotid imaging (TIA), CT or MRI scan (spinal pathology or compression, MS, cerebral tumour, syringomyelia), angiography (vascular causes), myelography (cord compression).
TOP TIPS
 Intermittent perioral paraesthesiae are pathognomic of hyperventilation.
Intermittent perioral paraesthesiae are pathognomic of hyperventilation.
 Use a logical approach: a careful history will often reveal the likely underlying problem. For example: well-demarcated area in anatomically explicable distribution – peripheral nerve entrapment; larger area, one limb – root compression; whole side of body – cerebral lesion; hands and feet – peripheral neuropathy; legs alone – cord lesion.
Use a logical approach: a careful history will often reveal the likely underlying problem. For example: well-demarcated area in anatomically explicable distribution – peripheral nerve entrapment; larger area, one limb – root compression; whole side of body – cerebral lesion; hands and feet – peripheral neuropathy; legs alone – cord lesion.
 Wasting of the thenar eminence suggests significant CT syndrome which will require decompression.
Wasting of the thenar eminence suggests significant CT syndrome which will require decompression.
 Remember to tell women taking the combined oral contraceptive who develop migraine with focal symptoms to use an alternative method of contraception.
Remember to tell women taking the combined oral contraceptive who develop migraine with focal symptoms to use an alternative method of contraception.

 Sudden and progressive bilateral leg symptoms with sphincter disturbance suggest cord compression: admit immediately.
Sudden and progressive bilateral leg symptoms with sphincter disturbance suggest cord compression: admit immediately.
 Intermittent paraesthesiae in varying distributions – especially with other features, such as vertigo or optic neuritis – suggest MS.
Intermittent paraesthesiae in varying distributions – especially with other features, such as vertigo or optic neuritis – suggest MS.
 Patients with TIAs with an ‘ABCD2’ score of 4 or more should be seen by a specialist within 24 hours; those with lower scores should be seen within 1 week.
Patients with TIAs with an ‘ABCD2’ score of 4 or more should be seen by a specialist within 24 hours; those with lower scores should be seen within 1 week.
 The borders of sensory loss in hysteria are often sharply demarcated and do not correspond to an anatomical pattern.
The borders of sensory loss in hysteria are often sharply demarcated and do not correspond to an anatomical pattern.
 Constant, progressive paraesthesiae, especially with other neurological symptoms or signs, suggest significant pathology. Refer urgently.
Constant, progressive paraesthesiae, especially with other neurological symptoms or signs, suggest significant pathology. Refer urgently.
PROLONGED FEVER
![]()
The GP overview
GPs deal with fevers on a daily basis – the vast majority are caused by viruses and are self-limiting. This section deals with a different and much less common scenario: a temperature above normal for 3 weeks or more. It may be continuous or swinging. Many more causes exist than can be named here, but those likeliest in general practice are listed.
![]()
Differential diagnosis
COMMON
 glandular fever (GF)
glandular fever (GF)
 abscess (anywhere)
abscess (anywhere)
 chronic pyelonephritis (recurrent UTI)
chronic pyelonephritis (recurrent UTI)
 carcinoma (especially bronchial)
carcinoma (especially bronchial)
 rheumatoid arthritis (RA)
rheumatoid arthritis (RA)
OCCASIONAL
 lymphoma and leukaemia
lymphoma and leukaemia
 systemic lupus erythematosus, polyarteritis nodosa, polymyositis
systemic lupus erythematosus, polyarteritis nodosa, polymyositis
 Crohn’s disease and ulcerative colitis
Crohn’s disease and ulcerative colitis
 drug idiosyncrasies
drug idiosyncrasies
RARE
 malaria and other tropical diseases
malaria and other tropical diseases
 Lyme disease
Lyme disease
 tuberculosis, syphilis
tuberculosis, syphilis
 actinomycosis
actinomycosis
 HIV infection: AIDS
HIV infection: AIDS
 infective endocarditis
infective endocarditis
 factitious
factitious
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: FBC, ESR/CRP, LFT, U&E, urinalysis, MSU.
POSSIBLE: Paul–Bunnell test, CXR, autoimmune screen.
SMALL PRINT: faecal calprotectin, blood cultures, malaria films, syphilis serology, HIV test and a variety of other secondary care-based tests.
 FBC, ESR/CRP, U&E, LFT: anaemia will be revealed in a variety of disorders (e.g. malignancy, connective tissue disorders); WCC raised in many inflammatory or infective processes and also some blood dyscrasias. Elevated ESR/CRP a non-specific finding in many of the illnesses listed. Abnormal U&E or LFT may point to an underlying renal or hepatic problem.
FBC, ESR/CRP, U&E, LFT: anaemia will be revealed in a variety of disorders (e.g. malignancy, connective tissue disorders); WCC raised in many inflammatory or infective processes and also some blood dyscrasias. Elevated ESR/CRP a non-specific finding in many of the illnesses listed. Abnormal U&E or LFT may point to an underlying renal or hepatic problem.
 Urinalysis, MSU: may be proteinuria, haematuria and evidence of infection in chronic pyelonephritis.
Urinalysis, MSU: may be proteinuria, haematuria and evidence of infection in chronic pyelonephritis.
 Paul–Bunnell test: may be positive in glandular fever.
Paul–Bunnell test: may be positive in glandular fever.
 CXR: will show signs of malignancy (e.g. lung, lymphoma), occult infection and TB.
CXR: will show signs of malignancy (e.g. lung, lymphoma), occult infection and TB.
 Autoimmune screen: may suggest a connective tissue disorder.
Autoimmune screen: may suggest a connective tissue disorder.
 Faecal calprotectin: if symptoms suggest possible IBD.
Faecal calprotectin: if symptoms suggest possible IBD.
 Secondary care-based tests: a number of tests may be performed after referral to the specialist in cases which remain obscure after initial assessment and investigation. These include further microbiological tests (e.g. stool, blood cultures), blood tests (e.g. for malaria, syphilis and HIV), isotope scans, ultrasound and CT scans (for occult infection or malignancy), tuberculin testing (for possible TB) and esoteric tests for tropical diseases.
Secondary care-based tests: a number of tests may be performed after referral to the specialist in cases which remain obscure after initial assessment and investigation. These include further microbiological tests (e.g. stool, blood cultures), blood tests (e.g. for malaria, syphilis and HIV), isotope scans, ultrasound and CT scans (for occult infection or malignancy), tuberculin testing (for possible TB) and esoteric tests for tropical diseases.
TOP TIPS
 Prolonged fever is usually an uncommon presentation of a common disorder (unless there has been recent travel), so review the situation regularly and encourage the patient to report new symptoms, which may help reveal the diagnosis.
Prolonged fever is usually an uncommon presentation of a common disorder (unless there has been recent travel), so review the situation regularly and encourage the patient to report new symptoms, which may help reveal the diagnosis.
 Refer early if the patient is unwell or has lost weight; if not, arrange initial investigations yourself.
Refer early if the patient is unwell or has lost weight; if not, arrange initial investigations yourself.
 Don’t always accept self-reporting of this symptom at face value. Flushing or sweating may be misreported as ‘fever’. If in doubt, get the patient to record the temperature over a period of time.
Don’t always accept self-reporting of this symptom at face value. Flushing or sweating may be misreported as ‘fever’. If in doubt, get the patient to record the temperature over a period of time.
 Always take a travel history, and specifically enquire about insect bites and compliance with antimalarial therapy. Remember, too, occupation and recent contact with infectious illness.
Always take a travel history, and specifically enquire about insect bites and compliance with antimalarial therapy. Remember, too, occupation and recent contact with infectious illness.

 Tuberculosis is rare but on the increase in the UK. Consider this diagnosis, particularly in
Tuberculosis is rare but on the increase in the UK. Consider this diagnosis, particularly in
Asian immigrants and vagrants.
 Itching with prolonged pyrexia suggests leukaemia or lymphoma.
Itching with prolonged pyrexia suggests leukaemia or lymphoma.
 Refer to a tropical medicine centre a patient with PUO who has recently been abroad somewhere exotic – in such a case, the differential is much wider and the possibility of an obscure pathology therefore much greater.
Refer to a tropical medicine centre a patient with PUO who has recently been abroad somewhere exotic – in such a case, the differential is much wider and the possibility of an obscure pathology therefore much greater.
 Factitious prolonged fever is rare, but possibly more common among health staff; beware the health worker with apparent fever but who never feels hot and who never appears unwell, especially if basic investigations are all normal.
Factitious prolonged fever is rare, but possibly more common among health staff; beware the health worker with apparent fever but who never feels hot and who never appears unwell, especially if basic investigations are all normal.
 Don’t forget the possibility of infective endocarditis in a patient with a cardiac murmur.
Don’t forget the possibility of infective endocarditis in a patient with a cardiac murmur.
SWOLLEN GLANDS
![]()
The GP overview
There are very many causes of swollen glands (lymphadenopathy), but in general it is possible to narrow the list of possible causes down to a manageable few by careful history and examination. Age, geography (or travel history) and distribution of enlarged glands have a considerable influence on the differential diagnosis.
![]()
Differential diagnosis
COMMON
 local infection (e.g. URTI, tonsillitis)
local infection (e.g. URTI, tonsillitis)
 generalised viral infection (e.g. glandular fever, rubella)
generalised viral infection (e.g. glandular fever, rubella)
 malignancy: secondary metastasis
malignancy: secondary metastasis
 white cell malignancy: lymphoma, leukaemia, myeloma
white cell malignancy: lymphoma, leukaemia, myeloma
 septicaemia
septicaemia
OCCASIONAL
 sarcoid
sarcoid
 cat scratch fever (especially in children)
cat scratch fever (especially in children)
 rubella/measles
rubella/measles
 SLE
SLE
 rheumatoid arthritis
rheumatoid arthritis
 tropical/subtropical sexually transmitted infection: lymphogranuloma venereum (LGV), granuloma inguinale (GI)
tropical/subtropical sexually transmitted infection: lymphogranuloma venereum (LGV), granuloma inguinale (GI)
RARE
 syphilis (primary or secondary)
syphilis (primary or secondary)
 HIV: AIDS and AIDS-related complex (ARC)
HIV: AIDS and AIDS-related complex (ARC)
 tuberculosis
tuberculosis
 tropical infections: leprosy, filariasis, trypanosomiasis, tularaemia
tropical infections: leprosy, filariasis, trypanosomiasis, tularaemia
 drug reactions (e.g. phenytoin, penicillins, sulphonamides)
drug reactions (e.g. phenytoin, penicillins, sulphonamides)
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: none if localised; FBC and ESR/CRP if generalised.
POSSIBLE: Paul–Bunnell test, CXR, acute and convalescent sera, HIV testing, lymph node biopsy.
SMALL PRINT: autoimmune blood tests, syphilis serology, cultures and scrapings for LGV and GI, Kveim test, CT scan, indirect fluorescent antibody blood test for Bartonella henselae.
 FBC: atypical lymphocytes reflect acute viral infection; many of the causes listed will result in a raised WCC and ESR/CRP. Hb may be low in malignancy and connective tissue disease; WCC and film may show evidence of lymphoma or leukaemia.
FBC: atypical lymphocytes reflect acute viral infection; many of the causes listed will result in a raised WCC and ESR/CRP. Hb may be low in malignancy and connective tissue disease; WCC and film may show evidence of lymphoma or leukaemia.
 Paul–Bunnell test: to confirm glandular fever.
Paul–Bunnell test: to confirm glandular fever.
 CXR: may reveal carcinoma, TB, lymphoma, sarcoid and the source of septicaemia.
CXR: may reveal carcinoma, TB, lymphoma, sarcoid and the source of septicaemia.
 Serology: acute and convalescent sera may confirm specific viral infection.
Serology: acute and convalescent sera may confirm specific viral infection.
 Kveim test for sarcoid.
Kveim test for sarcoid.
 Abdominal and chest CT scan is a sensitive test to detect pelvic, para-aortic, mesenteric, hilar or paratracheal node enlargement (e.g. in lymphoma).
Abdominal and chest CT scan is a sensitive test to detect pelvic, para-aortic, mesenteric, hilar or paratracheal node enlargement (e.g. in lymphoma).
 Autoimmune blood tests: may help in diagnosis of connective tissue disorder.
Autoimmune blood tests: may help in diagnosis of connective tissue disorder.
 Culture/scrapings (GUM clinic): for LGV and GI.
Culture/scrapings (GUM clinic): for LGV and GI.
 Syphilis serology, HIV testing: for syphilis and AIDS.
Syphilis serology, HIV testing: for syphilis and AIDS.
 Indirect fluorescent antibody test for B. henselae: this is the causative organism in cat scratch disease.
Indirect fluorescent antibody test for B. henselae: this is the causative organism in cat scratch disease.
 Lymph node biopsy may be necessary to reach a definitive diagnosis.
Lymph node biopsy may be necessary to reach a definitive diagnosis.
TOP TIPS
 Normal cervical lymph nodes are often palpable in children; they swell with URTIs and may be presented by anxious parents fearing significant disease.
Normal cervical lymph nodes are often palpable in children; they swell with URTIs and may be presented by anxious parents fearing significant disease.
 Remember geography: a young adult from the UK with persistent cervical nodes is likely to have Epstein–Barr virus (EBV) infection while, in Africa, the likeliest diagnosis would be tuberculosis. Swollen groin glands in the latter group might be caused by LGV or GI.
Remember geography: a young adult from the UK with persistent cervical nodes is likely to have Epstein–Barr virus (EBV) infection while, in Africa, the likeliest diagnosis would be tuberculosis. Swollen groin glands in the latter group might be caused by LGV or GI.
 Patients often attach great significance to swollen glands. It is worth explaining that lymphadenopathy usually represents a normal part of the immune system’s defence against infection and does not in itself require attention from the doctor unless there are unusual features.
Patients often attach great significance to swollen glands. It is worth explaining that lymphadenopathy usually represents a normal part of the immune system’s defence against infection and does not in itself require attention from the doctor unless there are unusual features.
 Unexplained and persistent cervical lymphadenopathy in the middle-aged and elderly should prompt urgent ENT assessment to exclude nasopharyngeal carcinoma.
Unexplained and persistent cervical lymphadenopathy in the middle-aged and elderly should prompt urgent ENT assessment to exclude nasopharyngeal carcinoma.
 An enlarged left supraclavicular node (Troisier’s) in a patient with weight loss suggests gastrointestinal carcinoma.
An enlarged left supraclavicular node (Troisier’s) in a patient with weight loss suggests gastrointestinal carcinoma.
 Generalised, persistent lymph nodes with weight loss and sweats in a young adult suggest glandular fever, lymphoma or AIDS.
Generalised, persistent lymph nodes with weight loss and sweats in a young adult suggest glandular fever, lymphoma or AIDS.
 A slowly enlarging, non-tender cervical node in an unusual site is likely to be malignant.
A slowly enlarging, non-tender cervical node in an unusual site is likely to be malignant.
THIRST OR DRY MOUTH
![]()
The GP overview
The complaint of thirst rings alarm bells in doctor and patient alike. Diabetes clearly needs to be excluded but the differential may need to be extended beyond this in the light of negative initial tests. Dry mouth tends to create less concern but can sometimes herald significant pathology and may be a serious nuisance to the patient.
![]()
Differential diagnosis
COMMON
 diabetes mellitus
diabetes mellitus
 dehydration
dehydration
 medication (e.g. tricyclic antidepressants, antihistamines)
medication (e.g. tricyclic antidepressants, antihistamines)
 mouth breathing (usually through nasal blockage)
mouth breathing (usually through nasal blockage)
 anxiety
anxiety
OCCASIONAL
 normality (children sometimes presented because ‘they are always thirsty’)
normality (children sometimes presented because ‘they are always thirsty’)
 smoking
smoking
 excess alcohol
excess alcohol
 Sjögren’s syndrome
Sjögren’s syndrome
 hypercalcaemia
hypercalcaemia
 chronic kidney disease (CKD)
chronic kidney disease (CKD)
RARE
 pregnancy (common condition but rarely causes significant thirst)
pregnancy (common condition but rarely causes significant thirst)
 compulsive water drinking
compulsive water drinking
 sickle-cell disease
sickle-cell disease
 previous head/neck irradiation
previous head/neck irradiation
![]()
Ready reckoner
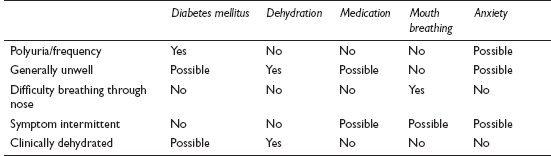
![]()
Possible investigations
LIKELY: urinalysis, fasting blood glucose or HbA1c.
POSSIBLE: FBC, ESR/CRP, U&E, calcium, rheumatoid factor and other autoantibody screen.
SMALL PRINT: serum and urine osmolality, sickle-cell screen.
 Urinalysis: glycosuria in diabetes, specific gravity raised in dehydration and reduced in diabetes insipidus and compulsive water drinking, may be proteinuria and/or microscopic haematuria in CKD.
Urinalysis: glycosuria in diabetes, specific gravity raised in dehydration and reduced in diabetes insipidus and compulsive water drinking, may be proteinuria and/or microscopic haematuria in CKD.
 Fasting blood glucose or HbA1c: to definitively diagnose diabetes.
Fasting blood glucose or HbA1c: to definitively diagnose diabetes.
 FBC/ESR: Hb may be reduced and ESR elevated in Sjögren’s linked to connective tissue disorder; Hb may also be reduced in CKD.
FBC/ESR: Hb may be reduced and ESR elevated in Sjögren’s linked to connective tissue disorder; Hb may also be reduced in CKD.
 U&E: may suggest dehydration or CKD.
U&E: may suggest dehydration or CKD.
 Calcium: elevated in hypercalcaemia.
Calcium: elevated in hypercalcaemia.
 Rheumatoid factor and other autoantibodies: Sjögren’s may be linked to rheumatoid arthritis, SLE or other connective tissue disease.
Rheumatoid factor and other autoantibodies: Sjögren’s may be linked to rheumatoid arthritis, SLE or other connective tissue disease.
 Serum and urine osmolality: serum osmolality raised and urine osmolality low in diabetes insipidus; in compulsive water drinking, serum osmolality low.
Serum and urine osmolality: serum osmolality raised and urine osmolality low in diabetes insipidus; in compulsive water drinking, serum osmolality low.
 Sickle-cell screen: to detect sickle-cell anaemia.
Sickle-cell screen: to detect sickle-cell anaemia.
TOP TIPS
 The assessment of thirst does not stop at the exclusion of diabetes mellitus – consider other causes.
The assessment of thirst does not stop at the exclusion of diabetes mellitus – consider other causes.
 Intermittent dry mouth in an anxious individual also reporting episodic perioral paraesthesiae is likely to be caused by anxiety – perhaps aggravated by certain medications the patient might be taking for the problem.
Intermittent dry mouth in an anxious individual also reporting episodic perioral paraesthesiae is likely to be caused by anxiety – perhaps aggravated by certain medications the patient might be taking for the problem.
 Do not underestimate the complaint of dry mouth, especially in the elderly – it can cause significant distress.
Do not underestimate the complaint of dry mouth, especially in the elderly – it can cause significant distress.
 Remember hypercalcaemia, particularly in palliative care patients – this is a potentially remediable cause of troublesome thirst.
Remember hypercalcaemia, particularly in palliative care patients – this is a potentially remediable cause of troublesome thirst.
 Children who are ‘always thirsty’, have been like that for as long as the parents can remember and are otherwise well will not have diabetes – though the parents may feel short-changed if this isn’t tested for.
Children who are ‘always thirsty’, have been like that for as long as the parents can remember and are otherwise well will not have diabetes – though the parents may feel short-changed if this isn’t tested for.

 In the acute presentation of thirst, it is essential to exclude diabetes immediately – a very high glucose level with ketonuria will require admission.
In the acute presentation of thirst, it is essential to exclude diabetes immediately – a very high glucose level with ketonuria will require admission.
 Beware the thirsty elderly patient with an acute illness, particularly if the patient is on ACE inhibitors – he or she may be significantly dehydrated and developing renal failure.
Beware the thirsty elderly patient with an acute illness, particularly if the patient is on ACE inhibitors – he or she may be significantly dehydrated and developing renal failure.
 Dry eyes and joint swellings in association with a dry mouth may indicate Sjögren’s.
Dry eyes and joint swellings in association with a dry mouth may indicate Sjögren’s.
 Beware that the elderly with diabetes may complain of dry mouth rather than thirst.
Beware that the elderly with diabetes may complain of dry mouth rather than thirst.
TIREDNESS
![]()
The GP overview
Feeling tired all the time is such a common presenting symptom that ‘TATT’ has become the universal GP acronym. In around 85% of first consultations the cause is apparent by the end. Although the vast majority turn out to have a non-organic cause, it is clearly important not to get lulled into ignoring important physical illness. A structured approach can turn this heartsink calling card into a rewarding and successful consultation.
![]()
Differential diagnosis
COMMON
 true depressive illness
true depressive illness
 stress (overwork, young children, boredom, etc.)
stress (overwork, young children, boredom, etc.)
 anaemia
anaemia
 acute post-viral fatigue
acute post-viral fatigue
 hypothyroidism
hypothyroidism
OCCASIONAL
 diabetes mellitus
diabetes mellitus
 iron deficiency (in the absence of anaemia)
iron deficiency (in the absence of anaemia)
 coeliac disease
coeliac disease
 any cause of insomnia (see p. 80)
any cause of insomnia (see p. 80)
 chronic post-viral fatigue syndrome (‘ME’)
chronic post-viral fatigue syndrome (‘ME’)
 major organ failure (heart, liver, kidney)
major organ failure (heart, liver, kidney)
 hyperthyroidism
hyperthyroidism
 substance misuse
substance misuse
 drug therapy (β-blockers, diuretics)
drug therapy (β-blockers, diuretics)
RARE
 malignant disease
malignant disease
 chronic infection (e.g. TB, hepatitis, HIV)
chronic infection (e.g. TB, hepatitis, HIV)
 chronic neurological disorders (Parkinson’s disease, myasthenia gravis, MS, motor neurone disease)
chronic neurological disorders (Parkinson’s disease, myasthenia gravis, MS, motor neurone disease)
 other endocrine disorders and deficiency states (e.g. Addison’s disease, hypo- or hypercalcaemia, hyponatraemia, hypokalaemia)
other endocrine disorders and deficiency states (e.g. Addison’s disease, hypo- or hypercalcaemia, hyponatraemia, hypokalaemia)
 connective tissue diseases (RA, polymyalgia rheumatica (PMR), SLE)
connective tissue diseases (RA, polymyalgia rheumatica (PMR), SLE)
 carbon monoxide poisoning
carbon monoxide poisoning
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: urinalysis, FBC, blood glucose or HbA1c, TFT.
POSSIBLE: ESR/CRP, U&E, LFT, ferritin, calcium, anti-endomysial and anti-gliadin antibodies.
SMALL PRINT: CXR, autoantibody screen, further blood tests as indicated such as HIV, glandular fever test, hepatitis serology.
 Urinalysis: simple screen for diabetes and renal disease.
Urinalysis: simple screen for diabetes and renal disease.
 Blood glucose or HbA1c: for diabetes.
Blood glucose or HbA1c: for diabetes.
 TFT for hypo- or hyperthyroidism.
TFT for hypo- or hyperthyroidism.
 FBC: the anaemias, infection and alcohol abuse.
FBC: the anaemias, infection and alcohol abuse.
 ESR/CRP: raised in a host of causes; not diagnostic but suggests a possible underlying physical cause.
ESR/CRP: raised in a host of causes; not diagnostic but suggests a possible underlying physical cause.
 U&E: deranged in renal failure, hyponatraemia, hypokalaemia and Addison’s disease.
U&E: deranged in renal failure, hyponatraemia, hypokalaemia and Addison’s disease.
 LFT: for liver disease (malignancy, alcohol abuse and hepatitis).
LFT: for liver disease (malignancy, alcohol abuse and hepatitis).
 Ferritin: iron deficiency may cause tiredness in the absence of anaemia.
Ferritin: iron deficiency may cause tiredness in the absence of anaemia.
 Calcium: hyper- or hypocalcaemia may cause tiredness.
Calcium: hyper- or hypocalcaemia may cause tiredness.
 Anti-endomysial and anti-gliadin antibodies: will suggest a diagnosis of coeliac disease.
Anti-endomysial and anti-gliadin antibodies: will suggest a diagnosis of coeliac disease.
 Autoantibody screen: for connective tissue disease.
Autoantibody screen: for connective tissue disease.
 Further blood tests: these will be dictated by the clinical picture and might include HIV, glandular fever or hepatitis testing.
Further blood tests: these will be dictated by the clinical picture and might include HIV, glandular fever or hepatitis testing.
 CXR: may reveal malignancy, cardiac failure or TB.
CXR: may reveal malignancy, cardiac failure or TB.
TOP TIPS
 Tiredness as a presenting symptom, in the absence of other significant volunteered symptoms – particularly weight loss or gain – is unlikely to have a physical cause.
Tiredness as a presenting symptom, in the absence of other significant volunteered symptoms – particularly weight loss or gain – is unlikely to have a physical cause.
 The longer tiredness has been a problem, the less likely you will find any remediable cause.
The longer tiredness has been a problem, the less likely you will find any remediable cause.
 Make eye contact with the patient and shake hands – your first impressions as to whether or not the patient is actually ‘ill’ are likely to prove correct, and may give early clues to easily overlooked causes such as Parkinson’s disease.
Make eye contact with the patient and shake hands – your first impressions as to whether or not the patient is actually ‘ill’ are likely to prove correct, and may give early clues to easily overlooked causes such as Parkinson’s disease.
 If you suspect depression, enquire directly about relevant symptoms – you do not have to ‘exclude’ physical illness before making a presumptive diagnosis of this sort.
If you suspect depression, enquire directly about relevant symptoms – you do not have to ‘exclude’ physical illness before making a presumptive diagnosis of this sort.
 Investigations ordered are often more therapeutic than diagnostic.
Investigations ordered are often more therapeutic than diagnostic.
 Ask about other household members’ health and well-being. Carbon monoxide poisoning would be likely to affect them too.
Ask about other household members’ health and well-being. Carbon monoxide poisoning would be likely to affect them too.
 Do not be too trigger-happy with the usual ‘blood screen’. Many patients ‘promised’ blood tests if their symptoms persist another month do not return.
Do not be too trigger-happy with the usual ‘blood screen’. Many patients ‘promised’ blood tests if their symptoms persist another month do not return.

 Take tiredness associated with weight loss seriously – this combination suggests malignant disease or hyperthyroidism.
Take tiredness associated with weight loss seriously – this combination suggests malignant disease or hyperthyroidism.
 Don’t miss depressive illness by being coy in enquiry or colluding with patient denial.
Don’t miss depressive illness by being coy in enquiry or colluding with patient denial.
 Don’t miss easy-to-find signs when physical illness seems a real possibility – check pulse rate, mucous membranes for pallor, lymph nodes, chest and abdomen.
Don’t miss easy-to-find signs when physical illness seems a real possibility – check pulse rate, mucous membranes for pallor, lymph nodes, chest and abdomen.
 Consider a rare cause if the symptoms progress and the patient starts to look unwell.
Consider a rare cause if the symptoms progress and the patient starts to look unwell.
TREMOR
![]()
The GP overview
This is rhythmic movement of parts of the body. There are three clinical types: rest tremor (worst at rest), postural tremor (worst in a fixed posture, e.g. outstretched arms) and intention tremor (worst during voluntary movement). Tremor may be noticed by the GP during an assessment for some other problem, or it may be the presenting symptom. In the latter case, the patient may be embarrassed by the lack of ‘self-control’, so a sympathetic approach is important.
![]()
Differential diagnosis
COMMON
 anxiety
anxiety
 thyrotoxicosis
thyrotoxicosis
 drug withdrawal (e.g. opiates, benzodiazepines, alcohol)
drug withdrawal (e.g. opiates, benzodiazepines, alcohol)
 benign essential tremor (familial)
benign essential tremor (familial)
 Parkinson’s disease
Parkinson’s disease
OCCASIONAL
 adverse drug reaction (e.g. phenothiazines, β-agonists)
adverse drug reaction (e.g. phenothiazines, β-agonists)
 carbon dioxide retention (e.g. COPD)
carbon dioxide retention (e.g. COPD)
 multiple sclerosis (MS)
multiple sclerosis (MS)
 cerebellar ataxia: many causes, including tumour, acoustic neuroma, Friedreich’s ataxia, CVA, abscess
cerebellar ataxia: many causes, including tumour, acoustic neuroma, Friedreich’s ataxia, CVA, abscess
RARE
 fulminant hepatic failure
fulminant hepatic failure
 Wilson’s disease
Wilson’s disease
 tertiary syphilis
tertiary syphilis
 hysterical: usually restricted to one limb and is very gross
hysterical: usually restricted to one limb and is very gross
 meningoencephalitis
meningoencephalitis
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: TFT.
POSSIBLE: FBC, LFT.
SMALL PRINT: syphilis serology and, in secondary care, MRI scan, lumbar puncture, visual evoked response, serum caeruloplasmin/blood copper, blood gases.
 FBC: macrocytosis in chronic alcohol excess.
FBC: macrocytosis in chronic alcohol excess.
 LFT: for evidence of alcohol abuse or liver failure.
LFT: for evidence of alcohol abuse or liver failure.
 TFT: if hyperthyroidism suspected.
TFT: if hyperthyroidism suspected.
 MRI most sensitive test for picking up CNS demyelination and tumours (e.g. cerebellar).
MRI most sensitive test for picking up CNS demyelination and tumours (e.g. cerebellar).
 Lumbar puncture: CSF electrophoresis may show oligoclonal bands in MS, or evidence of meningoencephalitis.
Lumbar puncture: CSF electrophoresis may show oligoclonal bands in MS, or evidence of meningoencephalitis.
 Visual evoked response: prolonged in MS.
Visual evoked response: prolonged in MS.
 Syphilis serology: in suspected syphilis.
Syphilis serology: in suspected syphilis.
 Blood gases: will reveal carbon dioxide retention.
Blood gases: will reveal carbon dioxide retention.
 Serum caeruloplasmin/blood copper: to diagnose Wilson’s disease.
Serum caeruloplasmin/blood copper: to diagnose Wilson’s disease.
TOP TIPS
 Patients who present with their tremor are invariably worried about significant disease, especially Parkinson’s disease. Ensure that these anxieties are resolved during the consultation.
Patients who present with their tremor are invariably worried about significant disease, especially Parkinson’s disease. Ensure that these anxieties are resolved during the consultation.
 Essential tremor is characteristically suppressed by a small dose of alcohol. This can be a useful pointer from the history.
Essential tremor is characteristically suppressed by a small dose of alcohol. This can be a useful pointer from the history.
 A tremor can have more than one cause and may not necessarily follow the neat patterns described, especially in the elderly.
A tremor can have more than one cause and may not necessarily follow the neat patterns described, especially in the elderly.
 The tremor of early Parkinson’s disease usually causes the patient few problems. It may therefore be noticed by the doctor when the patient presents with other symptoms, or be presented by concerned relatives or friends.
The tremor of early Parkinson’s disease usually causes the patient few problems. It may therefore be noticed by the doctor when the patient presents with other symptoms, or be presented by concerned relatives or friends.
 Have a low threshold for arranging TFT: anxiety can closely mimic thyrotoxicosis and vice versa.
Have a low threshold for arranging TFT: anxiety can closely mimic thyrotoxicosis and vice versa.
 Parkinson’s disease may well present with a consultation for frequent falls. Look for other signs such as mask face, small handwriting, slow movement, festinant gait and difficulty rising from chair.
Parkinson’s disease may well present with a consultation for frequent falls. Look for other signs such as mask face, small handwriting, slow movement, festinant gait and difficulty rising from chair.
 Think of alcohol problems in isolated middle-aged and elderly men developing postural tremor.
Think of alcohol problems in isolated middle-aged and elderly men developing postural tremor.
 Intention tremor with nystagmus or dysarthria suggests significant cerebellar pathology.
Intention tremor with nystagmus or dysarthria suggests significant cerebellar pathology.
WEIGHT GAIN
![]()
The GP overview
By far the commonest cause of this problem is simple obesity. This is 50% commoner in women, who also present more often than men. It may be the primary problem presented or it may be a ‘while I’m here’ symptom – either way, it tends to be viewed as a ‘heartsink’ symptom, as such patients may have unrealistic expectations of what the doctor can achieve.
![]()
Differential diagnosis
COMMON
 simple obesity (usually hereditary component with poor diet and lack of exercise)
simple obesity (usually hereditary component with poor diet and lack of exercise)
 hypothyroidism
hypothyroidism
 pregnancy
pregnancy
 oedema of any cause (e.g. cardiac failure, renal failure, hepatic failure)
oedema of any cause (e.g. cardiac failure, renal failure, hepatic failure)
 alcohol excess
alcohol excess
OCCASIONAL
 menopause
menopause
 iatrogenic (e.g. steroids, insulin, sulphonylureas, oestrogen, pizotifen)
iatrogenic (e.g. steroids, insulin, sulphonylureas, oestrogen, pizotifen)
 polycystic ovary syndrome
polycystic ovary syndrome
 large single ovarian cyst
large single ovarian cyst
 physical or mental disability restricting activity (e.g. CVA, Down’s syndrome)
physical or mental disability restricting activity (e.g. CVA, Down’s syndrome)
RARE
 anabolic steroid abuse
anabolic steroid abuse
 Cushing’s syndrome
Cushing’s syndrome
 hypothalamic lesion or hypopituitarism
hypothalamic lesion or hypopituitarism
 insulinoma
insulinoma
 rare genetic syndromes such as Prader–Willi syndrome
rare genetic syndromes such as Prader–Willi syndrome
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: TFT.
POSSIBLE: urinalysis, FBC, LFT, U&E, pregnancy test, cardiac investigations if the cause is possible cardiac failure, pelvic ultrasound.
SMALL PRINT: secondary care investigations for endocrine dysfunction.
 Urinalysis: proteinuria may be present in oedema caused by underlying renal disease.
Urinalysis: proteinuria may be present in oedema caused by underlying renal disease.
 FBC: anaemia may precipitate cardiac failure; MCV raised in hypothyroidism and alcohol excess.
FBC: anaemia may precipitate cardiac failure; MCV raised in hypothyroidism and alcohol excess.
 TFT: will reveal hypothyroidism.
TFT: will reveal hypothyroidism.
 U&E: deranged in renal failure and Cushing’s syndrome.
U&E: deranged in renal failure and Cushing’s syndrome.
 LFT: to check for liver failure, evidence of alcohol abuse and hypoproteinaemic states.
LFT: to check for liver failure, evidence of alcohol abuse and hypoproteinaemic states.
 Pregnancy test: to exclude pregnancy if this is a possibility.
Pregnancy test: to exclude pregnancy if this is a possibility.
 Pelvic ultrasound: will confirm ascites, ovarian cysts and pregnancy.
Pelvic ultrasound: will confirm ascites, ovarian cysts and pregnancy.
 Cardiac investigations: CXR, ECG, BNP and echocardiography if the underlying cause is possible cardiac failure.
Cardiac investigations: CXR, ECG, BNP and echocardiography if the underlying cause is possible cardiac failure.
 Secondary care investigations for endocrine dysfunction: for insulinoma, hypopituitarism, Cushing’s syndrome.
Secondary care investigations for endocrine dysfunction: for insulinoma, hypopituitarism, Cushing’s syndrome.
TOP TIPS
 Patients presenting with weight gain, especially if it is a long-term or fluctuating problem, usually have a clear agenda of their own – such as wanting a blood test or drug treatment. Much time can be wasted giving unwanted advice about diet and exercise which the patient will have heard before. Establish the patient’s agenda early in the consultation.
Patients presenting with weight gain, especially if it is a long-term or fluctuating problem, usually have a clear agenda of their own – such as wanting a blood test or drug treatment. Much time can be wasted giving unwanted advice about diet and exercise which the patient will have heard before. Establish the patient’s agenda early in the consultation.
 Parents anxious about weight gain in their children often want to be reassured that the child’s ‘glands’ are normal. If the child’s height is in proportion to its weight, or the parents have a similar physiognomy, and the child is otherwise well, it is highly unlikely that there is an underlying cause.
Parents anxious about weight gain in their children often want to be reassured that the child’s ‘glands’ are normal. If the child’s height is in proportion to its weight, or the parents have a similar physiognomy, and the child is otherwise well, it is highly unlikely that there is an underlying cause.
 Patients with Down’s syndrome have a relatively high prevalence of hypothyroidism – consider this possibility if a patient with Down’s syndrome experiences inexplicable weight gain.
Patients with Down’s syndrome have a relatively high prevalence of hypothyroidism – consider this possibility if a patient with Down’s syndrome experiences inexplicable weight gain.
 Investigation is usually clinically unnecessary, but may be useful to clear the way to dealing with the real cause.
Investigation is usually clinically unnecessary, but may be useful to clear the way to dealing with the real cause.

 Correction of hypothyroidism may not solve a weight gain problem, merely unmask an underlying simple obesity. Don’t falsely raise expectations.
Correction of hypothyroidism may not solve a weight gain problem, merely unmask an underlying simple obesity. Don’t falsely raise expectations.
 Establish whether the weight gain is diffuse or whether there is predominantly abdominal swelling. The latter may indicate pregnancy, ascites or a large ovarian cyst.
Establish whether the weight gain is diffuse or whether there is predominantly abdominal swelling. The latter may indicate pregnancy, ascites or a large ovarian cyst.
 Recent onset of weight gain in an elderly patient suggests probable congestive cardiac failure or possible hypothyroidism.
Recent onset of weight gain in an elderly patient suggests probable congestive cardiac failure or possible hypothyroidism.
 Young women may not consider, or accept, a diagnosis of pregnancy as a cause of their weight gain. Arrange a pregnancy test if in any doubt.
Young women may not consider, or accept, a diagnosis of pregnancy as a cause of their weight gain. Arrange a pregnancy test if in any doubt.
 The yield from routine blood tests is low – but consider investigation if the patient is unwell or the history atypical.
The yield from routine blood tests is low – but consider investigation if the patient is unwell or the history atypical.
WEIGHT LOSS
![]()
The GP overview
The significance of weight loss should not be underestimated: in about one-third of patients, there is no specific cause, but in the rest, a serious underlying pathology is found. The minority of these are psychiatric; 90% have organic illness. Thorough assessment from the start is the rule.
![]()
Differential diagnosis
COMMON
 ‘normal’ stressful life events without psychiatric illness (e.g. changing job, divorce, redundancy, bereavement, exam pressure)
‘normal’ stressful life events without psychiatric illness (e.g. changing job, divorce, redundancy, bereavement, exam pressure)
 clinical depressive illness
clinical depressive illness
 eating disorders: anorexia nervosa and bulimia nervosa
eating disorders: anorexia nervosa and bulimia nervosa
 hyperthyroidism: thyrotoxicosis and iatrogenic (excess thyroid replacement)
hyperthyroidism: thyrotoxicosis and iatrogenic (excess thyroid replacement)
 malignancy anywhere
malignancy anywhere
OCCASIONAL
 anxiety (of whatever cause)
anxiety (of whatever cause)
 any terminal illness (e.g. malignancy, motor neurone disease)
any terminal illness (e.g. malignancy, motor neurone disease)
 substance misuse: alcohol, opiates, amphetamines, laxatives
substance misuse: alcohol, opiates, amphetamines, laxatives
 organ failure: cardiac, renal and hepatic
organ failure: cardiac, renal and hepatic
 undiagnosed diabetes mellitus
undiagnosed diabetes mellitus
 chronic inflammatory conditions (e.g. RA, SLE)
chronic inflammatory conditions (e.g. RA, SLE)
 gastrointestinal disease (e.g. peptic ulcer, inflammatory bowel disease, coeliac disease, parasites)
gastrointestinal disease (e.g. peptic ulcer, inflammatory bowel disease, coeliac disease, parasites)
RARE
 any chronic infection (especially tuberculosis)
any chronic infection (especially tuberculosis)
 endocrine: Addison’s disease, phaeochromocytoma
endocrine: Addison’s disease, phaeochromocytoma
 AIDS
AIDS
 malnutrition (rare in developed countries, common worldwide)
malnutrition (rare in developed countries, common worldwide)
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: urinalysis, FBC, ESR/CRP, TFT, U&E, LFT, CXR, blood glucose or HbA1c.
POSSIBLE: autoimmune screen, HIV test, bowel investigations such as faecal calprotectin or anti-endomysial and anti-gliadin antibodies, other hospital-based investigations.
SMALL PRINT: none.
 Urinalysis: for possible undiagnosed diabetes; proteinuria in renal failure.
Urinalysis: for possible undiagnosed diabetes; proteinuria in renal failure.
 FBC and ESR/CRP: Hb may be reduced and ESR/CRP elevated in malignancy and any chronic disorder.
FBC and ESR/CRP: Hb may be reduced and ESR/CRP elevated in malignancy and any chronic disorder.
 U&E: abnormal in renal failure and sometimes in eating disorders; sodium reduced, potassium and urea elevated in Addison’s disease.
U&E: abnormal in renal failure and sometimes in eating disorders; sodium reduced, potassium and urea elevated in Addison’s disease.
 TFT: will confirm hyperthyroidism.
TFT: will confirm hyperthyroidism.
 LFT: deranged in alcoholism and liver disease.
LFT: deranged in alcoholism and liver disease.
 Blood glucose or HbA1c: to confirm diabetes.
Blood glucose or HbA1c: to confirm diabetes.
 Autoimmune screen: may be helpful in suspected connective tissue disorder.
Autoimmune screen: may be helpful in suspected connective tissue disorder.
 HIV test: if AIDS suspected.
HIV test: if AIDS suspected.
 Bowel investigations such as faecal calprotectin or anti-endomysial and anti-gliadin antibodies: if IBD or coeliac disease suspected.
Bowel investigations such as faecal calprotectin or anti-endomysial and anti-gliadin antibodies: if IBD or coeliac disease suspected.
 CXR: may reveal carcinoma, TB, lymphadenopathy or cardiac failure.
CXR: may reveal carcinoma, TB, lymphadenopathy or cardiac failure.
 Other investigations (usually hospital-based) may be required according to the symptoms accompanying the weight loss and the results of preliminary investigations.
Other investigations (usually hospital-based) may be required according to the symptoms accompanying the weight loss and the results of preliminary investigations.
TOP TIPS
 Weight loss needs to be taken seriously but can be complex and time-consuming to assess. If presented as a ‘by the way’ at the end of a consultation for some other matter, it is reasonable to reverse the normal approach by arranging basic blood tests and urinalysis first, and booking a follow-up appointment, with the results, for a more complete assessment.
Weight loss needs to be taken seriously but can be complex and time-consuming to assess. If presented as a ‘by the way’ at the end of a consultation for some other matter, it is reasonable to reverse the normal approach by arranging basic blood tests and urinalysis first, and booking a follow-up appointment, with the results, for a more complete assessment.
 Establish whether episodes of weight loss have happened before. Patients, or their records, may indicate, for example, that they always lose weight when stressed.
Establish whether episodes of weight loss have happened before. Patients, or their records, may indicate, for example, that they always lose weight when stressed.
 Check that the patient really has lost weight. The history may not be clear, and there is often a record available (e.g. new patient check or health promotion data) of previous weight.
Check that the patient really has lost weight. The history may not be clear, and there is often a record available (e.g. new patient check or health promotion data) of previous weight.
 Look at the patient. The obviously cachectic will have significant disease and require urgent and thorough investigation.
Look at the patient. The obviously cachectic will have significant disease and require urgent and thorough investigation.

 Rapid weight loss with malaise and respiratory or gastrointestinal symptoms strongly suggest a physical cause.
Rapid weight loss with malaise and respiratory or gastrointestinal symptoms strongly suggest a physical cause.
 Think of eating disorders in young females: look for acid dental erosion on palatal surfaces of upper teeth as a giveaway sign of recurrent vomiting.
Think of eating disorders in young females: look for acid dental erosion on palatal surfaces of upper teeth as a giveaway sign of recurrent vomiting.
 Weight loss in a child is caused either by significant organic pathology or emotional abuse. Look out for signs of non-accidental injury (NAI) during physical examination.
Weight loss in a child is caused either by significant organic pathology or emotional abuse. Look out for signs of non-accidental injury (NAI) during physical examination.
 Depression with weight loss is a difficult problem; it may be the primary cause or the change in mood may be secondary to some physical illness. Either way, don’t overlook significant depression while you arrange investigations; there is nothing to be lost in starting antidepressants while you continue to exclude a physical cause, so long as you explain your strategy to the patient.
Depression with weight loss is a difficult problem; it may be the primary cause or the change in mood may be secondary to some physical illness. Either way, don’t overlook significant depression while you arrange investigations; there is nothing to be lost in starting antidepressants while you continue to exclude a physical cause, so long as you explain your strategy to the patient.