Health Supervision and Prevention of Illness and Injury in Children and Adolescents
DIPHTHERIA, TETANUS, AND ACELLULAR PERTUSSIS (DTAP)
HAEMOPHILUS INFLUENZAE TYPE B (HIB)
INACTIVATED POLIOVIRUS VACCINE (IPV)
PNEUMOCOCCUS (CONJUGATE VACCINE)
RESPIRATORY SYNCYTIAL VIRUS (RSV)
DIFFERENCES BETWEEN CHILDREN AND ADULTS
SUDDEN INFANT DEATH SYNDROME (SIDS)
Morbidity and Mortality
 The leading cause of death in children under 1 year of age is grouped under the term perinatal conditions, which include:
The leading cause of death in children under 1 year of age is grouped under the term perinatal conditions, which include:
 Congenital malformation, deformations, and chromosomal abnormalities (number one
cause).
Congenital malformation, deformations, and chromosomal abnormalities (number one
cause).
 Low birth weight.
Low birth weight.
 Sudden infant death syndrome (SIDS).
Sudden infant death syndrome (SIDS).
 Respiratory distress syndrome.
Respiratory distress syndrome.
 Complications of pregnancy.
Complications of pregnancy.
 Perinatal infections.
Perinatal infections.
 Intrauterine or birth hypoxia.
Intrauterine or birth hypoxia.
 From 1 year to 24 years of age, the leading cause of death is injury (unintentional injuries).
From 1 year to 24 years of age, the leading cause of death is injury (unintentional injuries).
Prevention
Prevention is of primary importance in caring for the pediatric patient and is promoted through:
 Parental guidance (anticipatory guidance and counseling).
Parental guidance (anticipatory guidance and counseling).
 Screening tests.
Screening tests.
 Immunization.
Immunization.
Parental Guidance
Age-appropriate anticipatory guidance is provided to parents at various well-child visits.
1 WEEK–1 MONTH
 A 1-month-old infant is brought to the ED with poor feeding, weak suck, drooling,
constipation, and ↓ spontaneous movements. He is exclusively breast-fed, and his mother
has been giving him a home remedy for “colic.” Physical exam is positive for hypotonia.
Think: Botulism and its relationship with some home remedies prepared with honey. Treatment is with
human botulism immune globulin (BIG-IV).
A 1-month-old infant is brought to the ED with poor feeding, weak suck, drooling,
constipation, and ↓ spontaneous movements. He is exclusively breast-fed, and his mother
has been giving him a home remedy for “colic.” Physical exam is positive for hypotonia.
Think: Botulism and its relationship with some home remedies prepared with honey. Treatment is with
human botulism immune globulin (BIG-IV).
 WARD TIP
WARD TIP
Be informed of social services and financial assistance available to parents and patients.
 Place infant to sleep on back to prevent sudden infant death syndrome (SIDS). Never
on the stomach or side.
Place infant to sleep on back to prevent sudden infant death syndrome (SIDS). Never
on the stomach or side.
 Keep soft objects and loose bedding such as comforters, pillows, bumper pass, and
stuffed animals in crib with infant.
Keep soft objects and loose bedding such as comforters, pillows, bumper pass, and
stuffed animals in crib with infant.
 Use a car seat. Rear facing in back seat.
Use a car seat. Rear facing in back seat.
 Know signs of an illness.
Know signs of an illness.
 Use a rectal thermometer.
Use a rectal thermometer.
 Maintain a smoke-free environment.
Maintain a smoke-free environment.
 Maintain water temperature at <120°F (48.8°C). Takes 10 minutes to get a burn at
this temperature if baby is exposed.
Maintain water temperature at <120°F (48.8°C). Takes 10 minutes to get a burn at
this temperature if baby is exposed.
 Do not give honey to a child under 1 year of age (risk for botulism).
Do not give honey to a child under 1 year of age (risk for botulism).
 EXAM TIP
EXAM TIP
Exposure to second-hand smoke:
 Increases incidence of SIDS
Increases incidence of SIDS
 Increases URI
Increases URI
 Increases lower respiratory tract infections (bronchiolitis, pneumonia)
Increases lower respiratory tract infections (bronchiolitis, pneumonia)
 Increases RAD, asthma
Increases RAD, asthma
 Increases ear infections
Increases ear infections
 Discuss normal crying behavior and give some suggestions for how to calm the infant.
Discuss normal crying behavior and give some suggestions for how to calm the infant.
 Techniques to calm infant: swaddling in a light blanket, rocking in a cradle, windup
swing, vibrating chair.
Techniques to calm infant: swaddling in a light blanket, rocking in a cradle, windup
swing, vibrating chair.
 Never shake your baby.
Never shake your baby.
 Assess parental well-being. Baby blues are normal but if they persist beyond 2
weeks provide resources for mother’s postpartum depression.
Assess parental well-being. Baby blues are normal but if they persist beyond 2
weeks provide resources for mother’s postpartum depression.
2 MONTHS–1 YEAR
 Childproof home to keep children safe from poisons, household cleaners, medications,
buckets and tubs filled with water, plastic bags, electrical outlet covers, hot liquids,
matches, small and sharp objects, guns, and knives.
Childproof home to keep children safe from poisons, household cleaners, medications,
buckets and tubs filled with water, plastic bags, electrical outlet covers, hot liquids,
matches, small and sharp objects, guns, and knives.
 EXAM TIP
EXAM TIP
Any child with a rectal temperature >100.4°F (38°C) in the first 2 months of life should be seen immediately, to rule out sepsis with GBS, Listeria, E. Coli.
 The American Academy of Pediatrics (AAP) does not recommend syrup of ipecac anymore.
Give telephone number to local poison control hotline.
The American Academy of Pediatrics (AAP) does not recommend syrup of ipecac anymore.
Give telephone number to local poison control hotline.
 No solid food until 4–6 months.
No solid food until 4–6 months.
 Introduce single ingredient foods one at a time to assess for allergies.
Introduce single ingredient foods one at a time to assess for allergies.
 Limit juice to less than 4 ounces a day.
Limit juice to less than 4 ounces a day.
 Avoid baby walkers.
Avoid baby walkers.
 Do not put baby to bed with bottle, as it can cause dental caries.
Do not put baby to bed with bottle, as it can cause dental caries.
 Breast-feed or give iron-fortified formula, but no whole milk until after 1 year
of age.
Breast-feed or give iron-fortified formula, but no whole milk until after 1 year
of age.
 Avoid choking hazards such as coins, peanuts, popcorn, carrot sticks, hard candy,
whole grapes, and hot dogs.
Avoid choking hazards such as coins, peanuts, popcorn, carrot sticks, hard candy,
whole grapes, and hot dogs.
 May start using sippy cup at 6–9 months.
May start using sippy cup at 6–9 months.
 Do not leave baby alone in tub or high places.
Do not leave baby alone in tub or high places.
 Do not drink hot liquids while holding your baby.
Do not drink hot liquids while holding your baby.
 Importance of tummy time to meet milestones and decrease positional plagiocephaly.
Importance of tummy time to meet milestones and decrease positional plagiocephaly.
 Visit the dentist by 12 months or after first tooth erupts.
Visit the dentist by 12 months or after first tooth erupts.
 WARD TIP
WARD TIP
Assess head control before allowing baby to start solid foods to decrease the risk of choking.
 EXAM TIP
EXAM TIP
Falls and drowning are major risks of injury and death in toddlers.
1–5 YEARS
 Use toddler car seat (ages 1–4) and booster seat (ages 4–8) if proper weight and
height. See car seat section.
Use toddler car seat (ages 1–4) and booster seat (ages 4–8) if proper weight and
height. See car seat section.
 Brush teeth, see dentist. Brush teeth twice daily with plain water and a soft toothbrush
Brush teeth, see dentist. Brush teeth twice daily with plain water and a soft toothbrush
 EXAM TIP
EXAM TIP
Most infants drown in their own bathtub.
 Wean from bottle (start by 9 months of age with the introduction of cup).
Wean from bottle (start by 9 months of age with the introduction of cup).
 Make sure home is childproof again.
Make sure home is childproof again.
 Restrict child’s access to stairs.
Restrict child’s access to stairs.
 Allow child to eat with hands or utensils.
Allow child to eat with hands or utensils.
 Use sunscreen (can use as early as 6 months).
Use sunscreen (can use as early as 6 months).
 WARD TIP
WARD TIP
 Early childhood caries (cavities) is the number 1 chronic disease affecting young
children.
Early childhood caries (cavities) is the number 1 chronic disease affecting young
children.
 Early childhood caries is five times more common than asthma and seven times more
common than hay fever.
Early childhood caries is five times more common than asthma and seven times more
common than hay fever.
 Wear properly fitting bicycle helmet.
Wear properly fitting bicycle helmet.
 Provide close supervision, especially near dogs, driveways, streets, and lawnmowers.
Provide close supervision, especially near dogs, driveways, streets, and lawnmowers.
 Make appointment with dentist by 1 year of age.
Make appointment with dentist by 1 year of age.
 Ensure that child is supervised when near water; build fence around swimming pool
with latched gate.
Ensure that child is supervised when near water; build fence around swimming pool
with latched gate.
 Screen for amblyopia, strabismus, and visual acuity in all children younger than
5 years.
Screen for amblyopia, strabismus, and visual acuity in all children younger than
5 years.
 Strabismus: Cover test or Hirschberg light reflex test in children <3 years.
Strabismus: Cover test or Hirschberg light reflex test in children <3 years.
 Visual acuity: >3 years and screen every 1–2 years throughout childhood.
Visual acuity: >3 years and screen every 1–2 years throughout childhood.
 WARD TIP
WARD TIP
Temperature of the water heater should be kept below 120°F (49°C) to prevent accidental scalding injuries.
6–10 YEARS
 Reinforce personal hygiene.
Reinforce personal hygiene.
 Teach stranger safety.
Teach stranger safety.
 Provide healthy meals and snacks. Eat 5+ servings of fruits and vegetables a day;
eat breakfast.
Provide healthy meals and snacks. Eat 5+ servings of fruits and vegetables a day;
eat breakfast.
 Limit screen time to less than 2 hours a day.
Limit screen time to less than 2 hours a day.
 Be physically active 60 minutes a day.
Be physically active 60 minutes a day.
 Keep matches and guns out of children’s reach.
Keep matches and guns out of children’s reach.
 Use seat belt always, and booster seat until 4 feet 9 inches in height.
Use seat belt always, and booster seat until 4 feet 9 inches in height.
 Brush teeth twice daily with pea-sized amount of fluoride toothpaste.
Brush teeth twice daily with pea-sized amount of fluoride toothpaste.
 Limit screen time to less than 2 hours a day.
Limit screen time to less than 2 hours a day.
 Visit dentist 2×/year.
Visit dentist 2×/year.
 Teach pedestrian safety.
Teach pedestrian safety.
 Teach child to swim.
Teach child to swim.
 WARD TIP
WARD TIP
Adolescent HEEADDSSS assessment
Home
Education
Eating
Activities
Drugs and Alcohol
Depression
Safety
Sex
Suicide
11–21 YEARS
 Continue to support a healthy diet and exercise.
Continue to support a healthy diet and exercise.
 Wear appropriate protective sports gear.
Wear appropriate protective sports gear.
 Counsel on safe sex and avoiding alcohol and drugs.
Counsel on safe sex and avoiding alcohol and drugs.
 Promote a healthy social life, balanced diet, and at least 60 minutes of exercise
every day, with 30 minutes of vigorous exercise 3×/week.
Promote a healthy social life, balanced diet, and at least 60 minutes of exercise
every day, with 30 minutes of vigorous exercise 3×/week.
 Ask about mood or eating disorders (see below).
Ask about mood or eating disorders (see below).
 Address school performance, homework, and bullying.
Address school performance, homework, and bullying.
Screening
BLOOD PRESSURE
 High blood pressure (hypertension) in children is blood pressure that’s the same
as or higher than 95% of children who are the same sex, age, and height as your child.
High blood pressure (hypertension) in children is blood pressure that’s the same
as or higher than 95% of children who are the same sex, age, and height as your child.
 Routine monitoring of blood pressure should begin at age 3 years.
Routine monitoring of blood pressure should begin at age 3 years.
 Most common cause of high blood pressure reading in children is inappropriate cuff
size.
Most common cause of high blood pressure reading in children is inappropriate cuff
size.
 High blood pressure can be primary or secondary, the younger the child and the
higher the blood pressure, the greater the high blood pressure has an identifiable
cause.
High blood pressure can be primary or secondary, the younger the child and the
higher the blood pressure, the greater the high blood pressure has an identifiable
cause.
 Other causes of high blood pressure in children: heart and kidney diseases; medications;
endocrine disorders.
Other causes of high blood pressure in children: heart and kidney diseases; medications;
endocrine disorders.
 Contributing factors: Family history, race, excess weight, or obesity.
Contributing factors: Family history, race, excess weight, or obesity.
METABOLIC SCREENING
At 24 hours of life, the neonate should receive screening for various metabolic disorders including hypothyroidism, phenylketonuria (PKU), sickle cell disease, and adrenal cortex abnormalities.
Newborn screens test for diseases that if caught early are manageable and will prevent long-term poor health outcomes
 WARD TIP
WARD TIP
Metabolic screening may vary from state to state in the United States.
LEAD SCREENING
 Exposure is ↑ by:
Exposure is ↑ by:
 Living in or visiting a house built before 1978 with peeling or chipped paint.
Living in or visiting a house built before 1978 with peeling or chipped paint.
 Plumbing with lead pipes or lead solder joints.
Plumbing with lead pipes or lead solder joints.
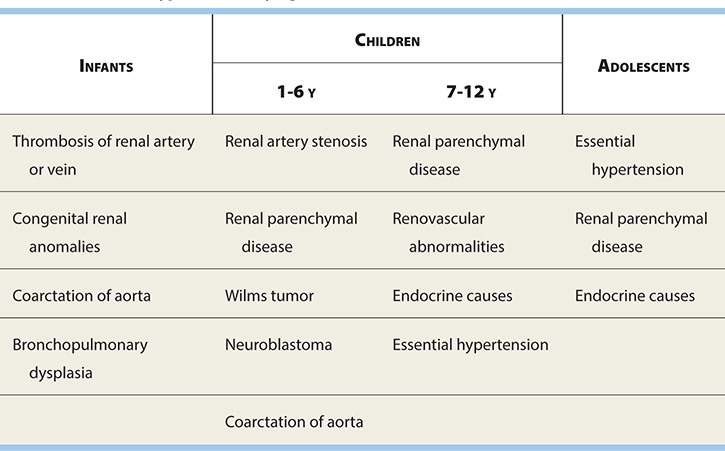
Common Causes of Hypertension by Age
 Living near a major highway where soil may be contaminated with lead.
Living near a major highway where soil may be contaminated with lead.
 Contact with someone who works with lead.
Contact with someone who works with lead.
 Living near an industrial site that may release lead into the environment.
Living near an industrial site that may release lead into the environment.
 Taking home remedies that may contain lead.
Taking home remedies that may contain lead.
 Toys from abroad.
Toys from abroad.
 WARD TIP
WARD TIP
Infants and young children are more likely to be exposed to lead than are older children. They may chew paint chips, and their hands may be contaminated with lead dust. Young children also absorb lead more easily and sustain more harm from it than do adults and older children.
 Traditional cosmetics: Kohl is a traditional cosmetic, often used as eyeliner.
Traditional cosmetics: Kohl is a traditional cosmetic, often used as eyeliner.
 Having friends/relatives who have had lead poisoning.
Having friends/relatives who have had lead poisoning.
 Screen for lead levels at age 12 months and 24 months.
Screen for lead levels at age 12 months and 24 months.
HEMATOCRIT
 EXAM TIP
EXAM TIP
Children’s blood lead levels increase most rapidly at 6–12 months and peaks at 18–24 months.
 Screen for anemia at 9–12 months of age where certification is needed for WIC (Women,
Infants, and Children) or if the appropriate risk factors are present.
Screen for anemia at 9–12 months of age where certification is needed for WIC (Women,
Infants, and Children) or if the appropriate risk factors are present.
 Second test 6 months later in high-risk communities for iron deficiency.
Second test 6 months later in high-risk communities for iron deficiency.
 Anemia: Hemoglobin levels <11 g/dL.
Anemia: Hemoglobin levels <11 g/dL.
 Risk factors for anemia include low socioeconomic status, birth weight under 1500
g, whole milk received before 6 months of age, low-iron formula given, low intake
of iron-rich foods.
Risk factors for anemia include low socioeconomic status, birth weight under 1500
g, whole milk received before 6 months of age, low-iron formula given, low intake
of iron-rich foods.
HYPERLIPIDEMIA
 Screen for hyperlipidemia in children older than 2 years with appropriate risk
factors:
Screen for hyperlipidemia in children older than 2 years with appropriate risk
factors:
 Family history of coronary or peripheral vascular disease before the age of 55
years in parents or grandparents.
Family history of coronary or peripheral vascular disease before the age of 55
years in parents or grandparents.
 Parent with a total serum cholesterol level >240 mg/dL.
Parent with a total serum cholesterol level >240 mg/dL.
 Obesity.
Obesity.
 Hypertension.
Hypertension.
 Diabetes mellitus.
Diabetes mellitus.
 Screening may also be considered in children with inactivity; also in adolescents
who smoke.
Screening may also be considered in children with inactivity; also in adolescents
who smoke.
 All children should be screened between 9 and 11 years and again between 17 and
21 years.
All children should be screened between 9 and 11 years and again between 17 and
21 years.
VISION AND HEARING
 WARD TIP
WARD TIP
Levels may be falsely low if screened during puberty because hormones require use of cholesterol to function.
 A hearing screen is recommended shortly after birth, ideally before discharge from
the newborn nursery.
A hearing screen is recommended shortly after birth, ideally before discharge from
the newborn nursery.
 Vision screening may begin at age 3 years, sooner if concerns.
Vision screening may begin at age 3 years, sooner if concerns.
 Suspect hearing loss earlier if child’s speech is not developing appropriately.
Suspect hearing loss earlier if child’s speech is not developing appropriately.
 A child’s cooperation is essential to obtaining an accurate result (~3 years).
A child’s cooperation is essential to obtaining an accurate result (~3 years).
AAP Car-Seat Recommendations
Infants and toddlers: Rear facing only or rear facing convertible (until 2 years and 20 lbs).
Toddlers and preschoolers: Convertible or forward facing with harness (until 4 years and 40 lbs).
School aged: Booster seats (until 4 feet 9 inches tall).
Older children: When large enough, use standard lap and shoulder belts. Younger than 13 should sit in backseat.
Other Car-Seat Note: Never place a car seat in front of an air bag (front passenger-side and side-impact air bags). The safest place for the infant is the middle portion of the rear seat.
 WARD TIP
WARD TIP
Newborns should not leave the hospital without a car seat.
Vaccines
 See latest CDC vaccine schedule (Figure 6-1).
See latest CDC vaccine schedule (Figure 6-1).
FIGURE 6-1. Recommended Immunization Schedule for Children and Adolescents Aged 18 Years or Younger—United States, 2017. (Source: Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html.)
 Site of injection:
Site of injection:
 Infants: Anterolateral thigh.
Infants: Anterolateral thigh.
 Children: Deltoid.
Children: Deltoid.
HEPATITIS B
 A 25-year-old female who is hepatitis B surface antigen positive is about to deliver
a baby and she asks what is the best way to prevent the baby from having hepatitis
B. Think: Prevention.
A 25-year-old female who is hepatitis B surface antigen positive is about to deliver
a baby and she asks what is the best way to prevent the baby from having hepatitis
B. Think: Prevention.
Babies born to women who are hepatitis B surface antigen positive receive hepatitis B immunoglobulin and hepatitis B vaccine shortly after birth, and 1–2 months after completing three doses of hepatitis B vaccine, they should be tested for hepatitis B surface antigen as well as the antibody.
 First dose given intramuscularly (IM) at birth or within first 2 months of life.
First dose given intramuscularly (IM) at birth or within first 2 months of life.
 Second dose given 1 month after first dose.
Second dose given 1 month after first dose.
 WARD TIP
WARD TIP
Fever is not a contraindication to receiving immunization. Moderate/severe illness is a precaution, not a contraindication. This holds true for all vaccines.
 Third dose given 4 months after first dose and 2 months after second dose, but
not before 6 months of age.
Third dose given 4 months after first dose and 2 months after second dose, but
not before 6 months of age.
 Must give at birth along with hepatitis B immune globulin (HBIG) if baby is exposed
transplacentally or if maternal status is unknown.
Must give at birth along with hepatitis B immune globulin (HBIG) if baby is exposed
transplacentally or if maternal status is unknown.
 Infants born to HBsAg-positive mothers should be tested for HBsAg and antibody
to HBsAg 1–2 months after completion of at least three doses of the HepB vaccine,
at age 9–18 months.
Infants born to HBsAg-positive mothers should be tested for HBsAg and antibody
to HBsAg 1–2 months after completion of at least three doses of the HepB vaccine,
at age 9–18 months.
CONTENT
Adsorbed recombinant hepatitis B surface antigen proteins.
SIDE EFFECTS
 Pain at injection site.
Pain at injection site.
 Fever >99.9°F (37.7°C) in 1–6%.
Fever >99.9°F (37.7°C) in 1–6%.
CONTRAINDICATIONS
 Anaphylactic reaction to vaccine, yeast, or another vaccine constituent.
Anaphylactic reaction to vaccine, yeast, or another vaccine constituent.
 Infants <2 kg.
Infants <2 kg.
DIPHTHERIA, TETANUS, AND ACELLULAR PERTUSSIS (DTaP)
 EXAM TIP
EXAM TIP
DTaP is preferred for children under 7 years of age. Td or Tdap is given after 7 years of age.
 Minimum age: 6 weeks.
Minimum age: 6 weeks.
 Given IM at 2, 4, and 6 months, and a fourth dose between 15 and 18 months of age.
Given IM at 2, 4, and 6 months, and a fourth dose between 15 and 18 months of age.
 The fourth dose may be administered as early as age 12 months; provided 6 months between third and fourth doses.
The fourth dose may be administered as early as age 12 months; provided 6 months between third and fourth doses.
 Administer the final dose at age 4–6 years.
Administer the final dose at age 4–6 years.
 DT without pertussis vaccine can be used in children <7 years of age if pertussis
vaccine is contraindicated.
DT without pertussis vaccine can be used in children <7 years of age if pertussis
vaccine is contraindicated.
 TDaP is administered at age 10–12.
TDaP is administered at age 10–12.
CONTENT
 EXAM TIP
EXAM TIP
DTP has greater risks of side effects than DTaP.
 DTaP is diphtheria and tetanus toxoids with acellular pertussis.
DTaP is diphtheria and tetanus toxoids with acellular pertussis.
 DTP contains a whole-cell pertussis.
DTP contains a whole-cell pertussis.
SIDE EFFECTS
 EXAM TIP
EXAM TIP
DTaP is not a substitute for DTP if a contraindication to pertussis exists.
 Erythema, pain, and swelling at injection site.
Erythema, pain, and swelling at injection site.
 Fever >100.4°F (38°C).
Fever >100.4°F (38°C).
 Crying ≥ 1 hour.
Crying ≥ 1 hour.
 Severe side effects (more common with DTP, rare with DTaP): crying >3 years; hypotonic-hyporesponsive
episode; seizures; fever >40.5°C.
Severe side effects (more common with DTP, rare with DTaP): crying >3 years; hypotonic-hyporesponsive
episode; seizures; fever >40.5°C.
CONTRAINDICATIONS
 WARD TIP
WARD TIP
A common misconception is that DTaP is contraindicated in patients with a family history of seizure or SIDS. This is NOT true.
 Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine
component
Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine
component
 Encephalopathy not attributable to another cause within 7 days of a prior dose
of pertussis vaccine.
Encephalopathy not attributable to another cause within 7 days of a prior dose
of pertussis vaccine.
PRECAUTIONS
 Seizure disorder or seizures within 3 days of receiving a previous dose of DTaP.
Seizure disorder or seizures within 3 days of receiving a previous dose of DTaP.
 Poorly controlled or new-onset seizures: Defer pertussis immunization until seizure
disorder is well controlled and progressive neurologic disorder is excluded.
Poorly controlled or new-onset seizures: Defer pertussis immunization until seizure
disorder is well controlled and progressive neurologic disorder is excluded.
 Personal or family history of febrile seizures. Give DTaP and antipyretics around
the clock for 24 hours after immunization.
Personal or family history of febrile seizures. Give DTaP and antipyretics around
the clock for 24 hours after immunization.
 Temperature of 40.5°C (104.8°F) within 48 hours after immunization with previous
dose of DTaP.
Temperature of 40.5°C (104.8°F) within 48 hours after immunization with previous
dose of DTaP.
 Collapse or shock like state (hypotonic-hyporesponsive episode within 48 hours
of receiving a previous dose of DTaP).
Collapse or shock like state (hypotonic-hyporesponsive episode within 48 hours
of receiving a previous dose of DTaP).
 Persistent inconsolable crying lasting >3 hours within 48 hours of receiving a
previous dose of DTaP.
Persistent inconsolable crying lasting >3 hours within 48 hours of receiving a
previous dose of DTaP.
 Guillain-Barre syndrome within 6 weeks after a prior dose.
Guillain-Barre syndrome within 6 weeks after a prior dose.
HAEMOPHILUS INFLUENZAE TYPE B (HIB)
 Minimum age: 6 weeks.
Minimum age: 6 weeks.
 Given IM at 2, 4, and 6 months of age, then again between 12 and 15 months of age.
Given IM at 2, 4, and 6 months of age, then again between 12 and 15 months of age.
CONTENT
Consists of a capsular polysaccharide antigen conjugated to a carrier.
SIDE EFFECTS
Erythema, pain, and swelling at injection site in 25%.
CONTRAINDICATIONS
Anaphylactic reaction to vaccine or vaccine constituent.
MEASLES, MUMPS, AND RUBELLA
 A 12-month-old boy is due for his vaccines in the middle of October. His mother mentions
that he developed a skin rash as well as some respiratory problems 1 month prior after
she fed him eggs for the first time. He is due for MMR, varicella, and influenza vaccines.
Think: Egg allergy and the vaccines that are contraindicated: influenza vaccine, yellow fever vaccine.
MMR can be given safely to children with egg allergy.
A 12-month-old boy is due for his vaccines in the middle of October. His mother mentions
that he developed a skin rash as well as some respiratory problems 1 month prior after
she fed him eggs for the first time. He is due for MMR, varicella, and influenza vaccines.
Think: Egg allergy and the vaccines that are contraindicated: influenza vaccine, yellow fever vaccine.
MMR can be given safely to children with egg allergy.
 Minimum age: 12 months.
Minimum age: 12 months.
 First dose given subcutaneously (SC) at 12–15 months of age, and second dose at
4–6 years of age.
First dose given subcutaneously (SC) at 12–15 months of age, and second dose at
4–6 years of age.
 Second dose may be given at any time after 4 weeks from first dose if necessary.
Second dose may be given at any time after 4 weeks from first dose if necessary.
 Must be at least 12 months old to ensure a sufficient response.
Must be at least 12 months old to ensure a sufficient response.
 EXAM TIP
EXAM TIP
MMR is a live virus vaccine.
CONTENT
Composed of live attenuated viruses.
SIDE EFFECTS
 Fever >102.9°F (39.4°C) 6–12 days after immunization can last up to 5 days in 10%.
Fever >102.9°F (39.4°C) 6–12 days after immunization can last up to 5 days in 10%.
 Transient rash in 5%. May occur 1–6 weeks after vaccination.
Transient rash in 5%. May occur 1–6 weeks after vaccination.
 Febrile seizures and encephalopathy with MMR vaccine are rare. Transient thrombocytopenia
may occur 2–3 weeks after vaccine in 1/40,000.
Febrile seizures and encephalopathy with MMR vaccine are rare. Transient thrombocytopenia
may occur 2–3 weeks after vaccine in 1/40,000.
 Swollen lymph nodes.
Swollen lymph nodes.
 Pain or stiffness in joints.
Pain or stiffness in joints.
CONTRAINDICATIONS
 Anaphylactic reaction to prior vaccine.
Anaphylactic reaction to prior vaccine.
 Anaphylactic reaction to neomycin or gelatin.
Anaphylactic reaction to neomycin or gelatin.
 Immunocompromised states.
Immunocompromised states.
 Pregnant women.
Pregnant women.
PRECAUTIONS
 Recent intravenous immunoglobulin (IVIg) administration requires delaying vaccinations
by 11 months.
Recent intravenous immunoglobulin (IVIg) administration requires delaying vaccinations
by 11 months.
 Throbocytopenia or history of thrombocytopenic purpura, however, benefits outweigh
risks.
Throbocytopenia or history of thrombocytopenic purpura, however, benefits outweigh
risks.
INACTIVATED POLIOVIRUS VACCINE (IPV)
 Minimum age: 6 weeks.
Minimum age: 6 weeks.
 Given IM or SQ at 2 and 4 months, then again between 6 and 18 months, then a fourth
between 4 and 6 years of age.
Given IM or SQ at 2 and 4 months, then again between 6 and 18 months, then a fourth
between 4 and 6 years of age.
 The final dose should be administered on or after the fourth birthday and at least
6 months following the previous dose.
The final dose should be administered on or after the fourth birthday and at least
6 months following the previous dose.
 If four doses are administered prior to age 4 years, a fifth dose should be administered
at age 4–6 years.
If four doses are administered prior to age 4 years, a fifth dose should be administered
at age 4–6 years.
 OPV is given orally. No longer used in the United States.
OPV is given orally. No longer used in the United States.
CONTENT
 IPV contains inactivated poliovirus types 1, 2, and 3.
IPV contains inactivated poliovirus types 1, 2, and 3.
 Live oral poliovirus vaccine (OPV) contains live attenuated poliovirus types 1,
2, and 3.
Live oral poliovirus vaccine (OPV) contains live attenuated poliovirus types 1,
2, and 3.
SIDE EFFECTS
 EXAM TIP
EXAM TIP
An all-IPV schedule is recommended in the United States to prevent VAPP (vaccine-associated paralytic polio). Under certain circumstances, OPV may be used.
 Vaccine-associated paralytic polio (VAPP) with OPV in 1/760,000.
Vaccine-associated paralytic polio (VAPP) with OPV in 1/760,000.
 Local reactions, fever.
Local reactions, fever.
CONTRAINDICATIONS
 EXAM TIP
EXAM TIP
OPV is contraindicated in immunodeficiency disorders or when household contacts are immunocompromised.
 Anaphylaxis to vaccine or vaccine constituent.
Anaphylaxis to vaccine or vaccine constituent.
 Anaphylaxis to streptomycin, polymixin B, or neomycin.
Anaphylaxis to streptomycin, polymixin B, or neomycin.
VARICELLA
 EXAM TIP
EXAM TIP
Varicella vaccine contains live virus.
 Minimum age: 12 months.
Minimum age: 12 months.
 Given SC between 12 and 18 months of age; second dose between 4 and 6 years (may
be administered before age 4, provided at least 3 months have elapsed since the first
dose).
Given SC between 12 and 18 months of age; second dose between 4 and 6 years (may
be administered before age 4, provided at least 3 months have elapsed since the first
dose).
 Susceptible persons >13 years of age must receive two doses at least 4 weeks apart.
Susceptible persons >13 years of age must receive two doses at least 4 weeks apart.
CONTENT
Cell-free live attenuated varicella virus.
SIDE EFFECTS
 Erythema and swelling in 20–35%.
Erythema and swelling in 20–35%.
 Fever in 10%.
Fever in 10%.
 Varicelliform rash in 1–4%.
Varicelliform rash in 1–4%.
CONTRAINDICATIONS
 Anaphylactic reaction to vaccine, neomycin, or gelatin.
Anaphylactic reaction to vaccine, neomycin, or gelatin.
 Patients with altered immunity, including corticosteroid use for > 14 days.
Patients with altered immunity, including corticosteroid use for > 14 days.
 Patients on salicylate therapy. Avoid salicylates for 6 weeks after vaccine administration.
Patients on salicylate therapy. Avoid salicylates for 6 weeks after vaccine administration.
 Pregnant women.
Pregnant women.
 Recent blood product or IG administration (defer at least 11 months).
Recent blood product or IG administration (defer at least 11 months).
INFLUENZA VACCINE (SEASONAL)
 WARD TIP
WARD TIP
LAIV is no longer available because of inefficacy.
 Minimum age: 6 months (quadrivalent inactivated influenza vaccine [TIV]); 2 years
(live attenuated influenza vaccine) [LAIV]).
Minimum age: 6 months (quadrivalent inactivated influenza vaccine [TIV]); 2 years
(live attenuated influenza vaccine) [LAIV]).
 Given IM to children >6 months of age yearly beginning in autumn, usually between
October and mid-November (two doses 1 month apart for the first time).
Given IM to children >6 months of age yearly beginning in autumn, usually between
October and mid-November (two doses 1 month apart for the first time).
 All children should receive this vaccine, especially high-risk children.
All children should receive this vaccine, especially high-risk children.
 Caution! LAIV should not be given to children aged 2–4 years who have had wheezing
in the past 12 months.
Caution! LAIV should not be given to children aged 2–4 years who have had wheezing
in the past 12 months.
CONTENT
 Contains four virus strains, usually both type A and type B based on the expected
prevalent influenza strains for the coming winter.
Contains four virus strains, usually both type A and type B based on the expected
prevalent influenza strains for the coming winter.
 Children <9 years of age should receive the “split” vaccine only.
Children <9 years of age should receive the “split” vaccine only.
 Children receiving vaccine for the first time should receive 2 doses 1 month apart
in order to obtain a good response.
Children receiving vaccine for the first time should receive 2 doses 1 month apart
in order to obtain a good response.
SIDE EFFECTS
 WARD TIP
WARD TIP
It is especially important to vaccinate for influenza those with asthma, chronic lung disease, cardiac defects, immunosuppressive disorders, sickle cell anemia, chronic renal disease, and chronic metabolic disease.
 Pain, swelling, and erythema at injection site.
Pain, swelling, and erythema at injection site.
 Fever may occur, especially in children <24 months of age.
Fever may occur, especially in children <24 months of age.
 In children >13 years of age, fever may occur in up to 10%.
In children >13 years of age, fever may occur in up to 10%.
 Guillain-Barré syndrome, if given at the same time as PCV13 and/or DTaP.
Guillain-Barré syndrome, if given at the same time as PCV13 and/or DTaP.
CONTRAINDICATIONS
Severe allergic reaction (e.g., anaphylaxis) after a previous dose of any IIV or LAIV or to a vaccine component, including egg protein.
PRECAUTIONS
 WARD TIP
WARD TIP
Influenza vaccine does not cause the disease. The vaccine has been associated with an ↑ risk of Guillain-Barré syndrome (GBS) in older adults, but no such cases have been reported in children.
 Moderate or severe acute illness with or without fever.
Moderate or severe acute illness with or without fever.
 History of GBS within 6 weeks of previous influenza vaccination.
History of GBS within 6 weeks of previous influenza vaccination.
 Persons whose egg allergy reaction is limited to hives only may receive RIV (if
age 18–49) or, with additional safety precautions, IIV.9
Persons whose egg allergy reaction is limited to hives only may receive RIV (if
age 18–49) or, with additional safety precautions, IIV.9
PNEUMOCOCCUS (CONJUGATE VACCINE)
 WARD TIP
WARD TIP
Chemoprophylaxis against influenza is recommended as an alternative means of protection in those who cannot be vaccinated.
 Minimum age: 6 weeks for pneumococcal conjugate vaccine (PCV), 2 years for pneumococcal
polysaccharide vaccine (PPSV).
Minimum age: 6 weeks for pneumococcal conjugate vaccine (PCV), 2 years for pneumococcal
polysaccharide vaccine (PPSV).
 Babies receive three doses (shots) 2 months apart starting at 2 months, and a fourth
dose when they are 12–15 months old.
Babies receive three doses (shots) 2 months apart starting at 2 months, and a fourth
dose when they are 12–15 months old.
 Also given to high-risk children ≥ 2 years of age.
Also given to high-risk children ≥ 2 years of age.
 PCV is recommended for all children aged younger than 5 years. Administer one dose
of PCV to all healthy children aged 24–59 months who are not completely immunized
for their age.
PCV is recommended for all children aged younger than 5 years. Administer one dose
of PCV to all healthy children aged 24–59 months who are not completely immunized
for their age.
 Administer PPSV ≥2 months after last dose of PCV to children aged 2 years or older
with certain underlying medical conditions, including a cochlear implant.
Administer PPSV ≥2 months after last dose of PCV to children aged 2 years or older
with certain underlying medical conditions, including a cochlear implant.
CONTENT
 WARD TIP
WARD TIP
The pneumococcal vaccine helps to protect against meningitis, bacteremia, pneumonia, and otitis media caused by serotypes of Streptococcus pneumoniae.
 The older PPV-23 vaccine (not indicated under age 2) contains the purified capsular
polysaccharide antigens of 23 pneumococcal serotypes. The PPV-23 is usually reserved
for high-risk children.
The older PPV-23 vaccine (not indicated under age 2) contains the purified capsular
polysaccharide antigens of 23 pneumococcal serotypes. The PPV-23 is usually reserved
for high-risk children.
 The newer PCV-13 is the conjugate vaccine described above.
The newer PCV-13 is the conjugate vaccine described above.
SIDE EFFECTS
 Erythema and pain at injection site.
Erythema and pain at injection site.
 Anaphylaxis reported rarely.
Anaphylaxis reported rarely.
 Fever and myalgia are uncommon.
Fever and myalgia are uncommon.
CONTRAINDICATIONS
 For PCV13, severe allergic reaction (e.g., anaphylaxis) after a previous dose of
PCV7 or PCV13 or to a vaccine component, as well as to any vaccine containing diphtheria
toxoid.
For PCV13, severe allergic reaction (e.g., anaphylaxis) after a previous dose of
PCV7 or PCV13 or to a vaccine component, as well as to any vaccine containing diphtheria
toxoid.
 For PPSV23, severe allergic reaction (e.g., anaphylaxis) after a previous dose
or to a vaccine component.
For PPSV23, severe allergic reaction (e.g., anaphylaxis) after a previous dose
or to a vaccine component.
HEPATITIS A VACCINE
 Minimum age: 12 months.
Minimum age: 12 months.
 Administer to all children aged 1 year (12–23 months).
Administer to all children aged 1 year (12–23 months).
 Administer two doses at least 6 months apart.
Administer two doses at least 6 months apart.
 Recommended for older children who live in areas where vaccination programs target
older children, who are at ↑ risk for infection, or for whom immunity against hepatitis
A is desired.
Recommended for older children who live in areas where vaccination programs target
older children, who are at ↑ risk for infection, or for whom immunity against hepatitis
A is desired.
 are <24 months of age
are <24 months of age
HUMAN PAPILLOMAVIRUS (HPV)
 May be given between age 9 and 26 years to both girls and boys.
May be given between age 9 and 26 years to both girls and boys.
 Three dose series, with second dose 2 months after the first dose and the third
dose 6 months after the first dose.
Three dose series, with second dose 2 months after the first dose and the third
dose 6 months after the first dose.
 Contains nine strains of HPV.
Contains nine strains of HPV.
SIDE EFFECTS
Pain, swelling, dizziness, syncope.
MENINGOCOCCAL VACCINE
 WARD TIP
WARD TIP
Recommend observation for syncope for 15 minutes after administration of HPV vaccine.
 Available against groups A, C, Y, W-135.
Available against groups A, C, Y, W-135.
 New vaccine available against group B.
New vaccine available against group B.
 All children receive tetravalent conjugate vaccine (MCV-4) at age 11, booster at
age 16.
All children receive tetravalent conjugate vaccine (MCV-4) at age 11, booster at
age 16.
 Minimum age: 2 years for meningococcal conjugate vaccine (MCV4) and meningococcal
polysaccharide vaccine (MPSV4).
Minimum age: 2 years for meningococcal conjugate vaccine (MCV4) and meningococcal
polysaccharide vaccine (MPSV4).
 Administer MCV4 to children aged 2–10 years with:
Administer MCV4 to children aged 2–10 years with:
 Persistent complement component deficiency.
Persistent complement component deficiency.
 Anatomic or functional asplenia.
Anatomic or functional asplenia.
SIDE EFFECTS
 EXAM TIP
EXAM TIP
Live attenuated vaccines include:
 MMR
MMR
 VZV
VZV
 Nasal influenza vaccine
Nasal influenza vaccine
 OPV
OPV
 Smallpox
Smallpox
 Typhoid
Typhoid
 Yellow fever
Yellow fever
These should be avoided in the immunocompromised.
 Localized erythema and pain.
Localized erythema and pain.
 Fever.
Fever.
 Headache.
Headache.
 Fatigue.
Fatigue.
CONTRAINDICATION
Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component.
PRECAUTION
History of Guillain-Barré syndrome.
ROTAVIRUS VACCINE
 Minimum age: 6 weeks.
Minimum age: 6 weeks.
 Administer the first dose at age 6–14 weeks (maximum age: 14 weeks 6 days). Vaccination
should not be initiated for infants aged 15 weeks 0 days or older.
Administer the first dose at age 6–14 weeks (maximum age: 14 weeks 6 days). Vaccination
should not be initiated for infants aged 15 weeks 0 days or older.
 The maximum age for the final dose in the series is 8 months 0 days.
The maximum age for the final dose in the series is 8 months 0 days.
 If Rotarix rotavirus vaccine is administered at ages 2 and 4 months, a dose at
6 months is not indicated.
If Rotarix rotavirus vaccine is administered at ages 2 and 4 months, a dose at
6 months is not indicated.
CONTRAINDICATION
SCID.
PRECAUTIONS
Preexisting chronic gastrointestinal disease, history of intussusception, spina bifida, or bladder exstrophy.
SIDE EFFECTS
Diarrhea, intussusception.
RESPIRATORY SYNCYTIAL VIRUS (RSV)
 Palivizumab (synagis) is a monoclonal antibody used for prophylaxis against infections
with RSV.
Palivizumab (synagis) is a monoclonal antibody used for prophylaxis against infections
with RSV.
 Given IM once a month at the beginning of RSV season, usually beginning in October
and ending in March.
Given IM once a month at the beginning of RSV season, usually beginning in October
and ending in March.
 Who should receive the vaccine:
Who should receive the vaccine:
 Children <2 years of age with chronic lung disease who have required medical therapy
6 months before the anticipated RSV season.
Children <2 years of age with chronic lung disease who have required medical therapy
6 months before the anticipated RSV season.
 Children born at 32 weeks’ gestation or earlier with other risk factors for lung
disease.
Children born at 32 weeks’ gestation or earlier with other risk factors for lung
disease.
 Infants born <29 weeks, if less than 12 months old at the start of the RSV season.
Infants born <29 weeks, if less than 12 months old at the start of the RSV season.
 Infants born 29 to <32 weeks, if <6 months at the start of the RSV season.
Infants born 29 to <32 weeks, if <6 months at the start of the RSV season.
 Infants born at 32–35 weeks who are <3 months at the start of the RSV season and
who are likely to have increased RSV exposure (child care exposure or siblings <5
years old).
Infants born at 32–35 weeks who are <3 months at the start of the RSV season and
who are likely to have increased RSV exposure (child care exposure or siblings <5
years old).
 Infants with congenital abnormalities of the airway or neuromuscular disease.
Infants with congenital abnormalities of the airway or neuromuscular disease.
 Infants with hemodynamically significant cyanotic or acyanotic congenital heart
disease.
Infants with hemodynamically significant cyanotic or acyanotic congenital heart
disease.
TUBERCULOSIS (TB)
 WARD TIP
WARD TIP
Ask the following questions to determine the need for a PPD:
 Has a family member or contact had tuberculosis disease?
Has a family member or contact had tuberculosis disease?
 Has a family member had a positive tuberculin skin test?
Has a family member had a positive tuberculin skin test?
 Was your child born in a high-risk country (countries other than the United States,
Canada, Australia, New Zealand, or Western European countries)?
Was your child born in a high-risk country (countries other than the United States,
Canada, Australia, New Zealand, or Western European countries)?
 Has your child traveled (had contact with resident populations) to a high-risk
country for more than one week?
Has your child traveled (had contact with resident populations) to a high-risk
country for more than one week?
 Children at risk include:
Children at risk include:
 Children living in a household with an adult who has active tuberculosis or has
a high risk of contracting TB.
Children living in a household with an adult who has active tuberculosis or has
a high risk of contracting TB.
 Children infected with HIV or another condition that weakens the immune system.
Children infected with HIV or another condition that weakens the immune system.
 Children born in a country that has a high prevalence of TB.
Children born in a country that has a high prevalence of TB.
 Children visiting a country where TB is endemic and who have extended contact with
people who live there.
Children visiting a country where TB is endemic and who have extended contact with
people who live there.
 Children from communities that generally receive inadequate medical care.
Children from communities that generally receive inadequate medical care.
 Children living in a shelter or living with someone who has been in jail.
Children living in a shelter or living with someone who has been in jail.
 The Mantoux test contains five tuberculin units of purified protein derivative
(PPD).
The Mantoux test contains five tuberculin units of purified protein derivative
(PPD).
SCREENING
 Asymptomatic children at high risk for tuberculosis should be screened with a PPD
test annually.
Asymptomatic children at high risk for tuberculosis should be screened with a PPD
test annually.
 Interpretation: See Table 6-1.
Interpretation: See Table 6-1.
TABLE 6-1. Guidelines for Determining a Positive Tuberculin Skin Test Reaction

 The QuantiFERON®-TB Gold test (QFT-G) is a newer alternative for detection of TB, approved by the
U.S. Food and Drug Administration (FDA) in 2005.
The QuantiFERON®-TB Gold test (QFT-G) is a newer alternative for detection of TB, approved by the
U.S. Food and Drug Administration (FDA) in 2005.
 Advantages:
Advantages:
 Requires a single patient visit to draw a blood sample.
Requires a single patient visit to draw a blood sample.
 Results can be available within 24 hours.
Results can be available within 24 hours.
 Does not boost responses measured by subsequent test, which can happen with tuberculin
skin tests (TSTs).
Does not boost responses measured by subsequent test, which can happen with tuberculin
skin tests (TSTs).
 Is not subject to reader bias that can occur with TSTs.
Is not subject to reader bias that can occur with TSTs.
 Is not affected by prior BCG (bacille Calmette-Guérin) vaccination.
Is not affected by prior BCG (bacille Calmette-Guérin) vaccination.
 Disadvantages:
Disadvantages:
 Blood samples must be processed within 12 hours after collection while white blood
cells are still viable.
Blood samples must be processed within 12 hours after collection while white blood
cells are still viable.
 Limited data in children <17 years of age, among persons recently exposed to Mycobacterium tuberculosis, and in immunocompromised persons.
Limited data in children <17 years of age, among persons recently exposed to Mycobacterium tuberculosis, and in immunocompromised persons.
 Errors in collecting or transporting blood specimens or in running and interpreting
the assay can ↓ the accuracy of QFT-G.
Errors in collecting or transporting blood specimens or in running and interpreting
the assay can ↓ the accuracy of QFT-G.
 Limited data on the use of QFT-G to determine who is at risk for developing TB
disease.
Limited data on the use of QFT-G to determine who is at risk for developing TB
disease.
Medications
Only 25% of Food and Drug Administration (FDA)-approved drugs have been approved for pediatric use.
DIFFERENCES BETWEEN CHILDREN AND ADULTS
ABSORPTION
 Infants have thinner skin; therefore, topical substances can more likely cause
systemic toxicity.
Infants have thinner skin; therefore, topical substances can more likely cause
systemic toxicity.
 Children do not have the stomach acidity of adults until age 2, and gastric emptying
time is slower and less predictable, → ↑ absorption of some medications.
Children do not have the stomach acidity of adults until age 2, and gastric emptying
time is slower and less predictable, → ↑ absorption of some medications.
DISTRIBUTION
 WARD TIP
WARD TIP
Controls with Candida, measles, or diphtheria can be placed along with the PPD to test for anergy, although opinion may vary in practice.
 Less predictable in children.
Less predictable in children.
 Total body water ↓ from 90% in infants to 60% in adults.
Total body water ↓ from 90% in infants to 60% in adults.
 Fat stores are similar to adults in term infants, but much less in preterm infants.
Fat stores are similar to adults in term infants, but much less in preterm infants.
 Newborns have smaller protein concentration, therefore less binding of substances
in the blood.
Newborns have smaller protein concentration, therefore less binding of substances
in the blood.
 Infants have an immature blood–brain barrier.
Infants have an immature blood–brain barrier.
METABOLISM
Infants metabolize some drugs more slowly or rapidly than adults and may create a different proportion of active metabolites.
ELIMINATION
Kidney function ↑ with age, so younger children may clear drugs less efficiently.
DOSAGE
Pediatric medications are generally dosed by milligrams per kilogram (mg/kg).
Poisoning
EPIDEMIOLOGY
More often accidental in younger children and suicide gestures or attempts in older children/adolescents.
SIGNS AND SYMPTOMS
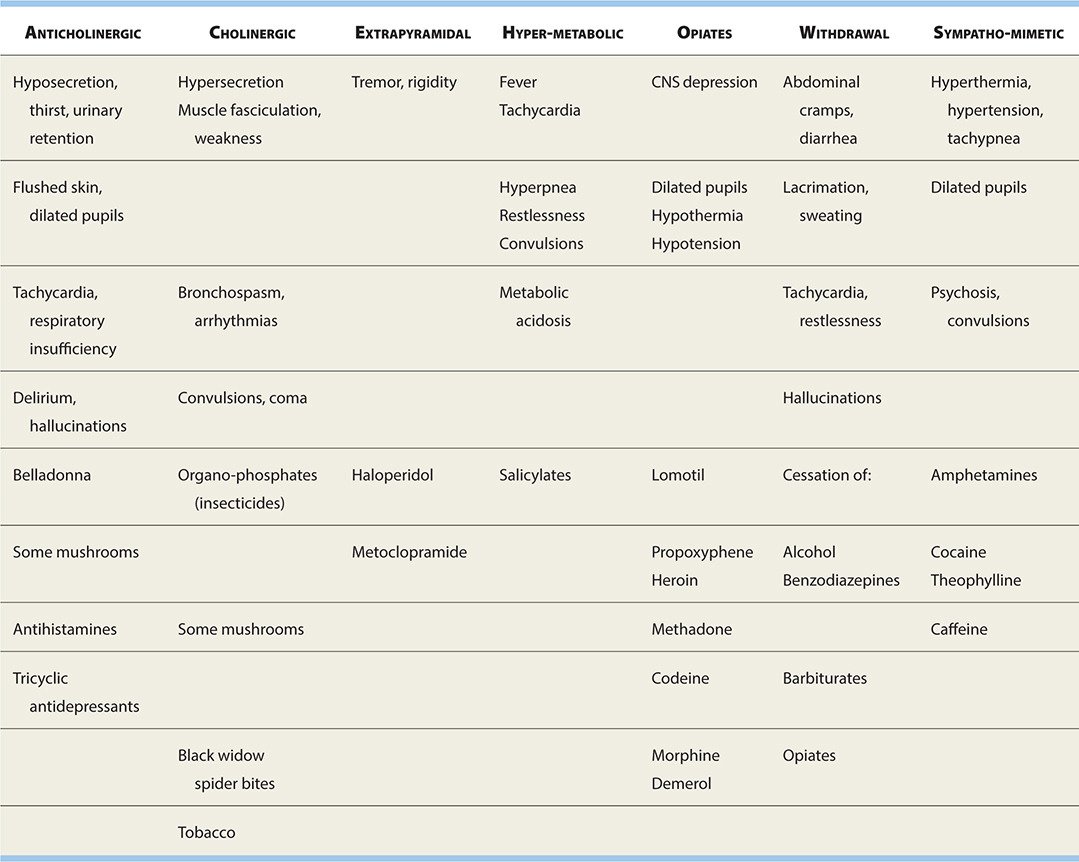
See Table 6-2.
TABLE 6-2. “Toxidromes,” Symptoms, and Some Causes
PREVENTION
 Childproof home, including cabinets and containers.
Childproof home, including cabinets and containers.
 Store toxic substances in their original containers and out of children’s reach.
Store toxic substances in their original containers and out of children’s reach.
 Supervise children appropriately.
Supervise children appropriately.
 Have poison control center number easily accessible.
Have poison control center number easily accessible.
MANAGEMENT
 Frequently, ingested substances are nontoxic, but if symptoms arise or there is
any question, a poison control center should be contacted.
Frequently, ingested substances are nontoxic, but if symptoms arise or there is
any question, a poison control center should be contacted.
 History:
History:
 Precise name of product (generic, brand, chemical—bring container or extra substance/pills).
Precise name of product (generic, brand, chemical—bring container or extra substance/pills).
 Estimate amount of exposure, time of exposure.
Estimate amount of exposure, time of exposure.
 Progression of symptoms.
Progression of symptoms.
 Other medical conditions (e.g., pregnancy, seizure disorder).
Other medical conditions (e.g., pregnancy, seizure disorder).
 Gastric decontamination: Emesis (induced by syrup of ipecac) and gastric lavage
remove only one third of stomach contents and are not generally recommended, though
the combination of the latter with activated charcoal may be most effective.
Gastric decontamination: Emesis (induced by syrup of ipecac) and gastric lavage
remove only one third of stomach contents and are not generally recommended, though
the combination of the latter with activated charcoal may be most effective.
 Activated charcoal is effective for absorbing many drugs and chemicals, though
it does not bind heavy metals, iron, lithium alcohols, hydrocarbons, cyanide. It may
be used in conjunction with cathartics such as sorbitol or magnesium sulfate.
Activated charcoal is effective for absorbing many drugs and chemicals, though
it does not bind heavy metals, iron, lithium alcohols, hydrocarbons, cyanide. It may
be used in conjunction with cathartics such as sorbitol or magnesium sulfate.
 WARD TIP
WARD TIP
Can only administer activated charcoal if ingestion was <1 hour prior
 Dilution of stomach contents with milk has limited value except in the case of
ingestion of caustic materials.
Dilution of stomach contents with milk has limited value except in the case of
ingestion of caustic materials.
 Skin decontamination: Remove clothing, use gloves, flood area with water for 15
minutes, use other mild material such as petroleum or alcohol to remove substances
not removed by water.
Skin decontamination: Remove clothing, use gloves, flood area with water for 15
minutes, use other mild material such as petroleum or alcohol to remove substances
not removed by water.
 Ocular decontamination: Rinse eyes with water, saline, or lactated Ringer’s for
> 15 minutes; consider emergency ophthalmologic exam.
Ocular decontamination: Rinse eyes with water, saline, or lactated Ringer’s for
> 15 minutes; consider emergency ophthalmologic exam.
 Respiratory decontamination: Move to fresh air; bronchodilators may be effective,
inhaled dilute sodium bicarbonate may help acid or chlorine inhalation.
Respiratory decontamination: Move to fresh air; bronchodilators may be effective,
inhaled dilute sodium bicarbonate may help acid or chlorine inhalation.
 Antidotes: See Table 6-3.
Antidotes: See Table 6-3.

 Treat seizures, respiratory distress/depression, hemodynamics, and electrolyte
disturbances as they arise.
Treat seizures, respiratory distress/depression, hemodynamics, and electrolyte
disturbances as they arise.
Adolescence
 Adolescence comprises the ages between 10 and 21 years.
Adolescence comprises the ages between 10 and 21 years.
 The most common health problems seen in this age group include unintended pregnancies,
sexually transmitted diseases (STDs), mental health disorders, physical injuries,
and substance abuse.
The most common health problems seen in this age group include unintended pregnancies,
sexually transmitted diseases (STDs), mental health disorders, physical injuries,
and substance abuse.
PREVENTION
 WARD TIP
WARD TIP
The leading causes of death for adolescents are accidents, homicide, and suicide.
 Be on the lookout for adolescents at high risk for health problems, including physical,
mental, and emotional health.
Be on the lookout for adolescents at high risk for health problems, including physical,
mental, and emotional health.
 Screen for depression. Suicide is the third leading cause of death in adolescents.
Depression in the adolescent can manifest as irritability, anger, new drug use, and
drop-off in school performance.
Screen for depression. Suicide is the third leading cause of death in adolescents.
Depression in the adolescent can manifest as irritability, anger, new drug use, and
drop-off in school performance.
 Look for:
Look for:
 Decline in school performance, excessive school absences, cutting class.
Decline in school performance, excessive school absences, cutting class.
 Frequent psychosomatic complaints.
Frequent psychosomatic complaints.
 Changes in sleeping or eating habits.
Changes in sleeping or eating habits.
 Difficulty in concentrating.
Difficulty in concentrating.
 Signs of depression, stress, or anxiety.
Signs of depression, stress, or anxiety.
 Conflict with parents.
Conflict with parents.
 Social withdrawal.
Social withdrawal.
 Sexual acting-out.
Sexual acting-out.
 Conflicts with the law.
Conflicts with the law.
 Suicidal thoughts, preoccupation with death.
Suicidal thoughts, preoccupation with death.
 Substance abuse.
Substance abuse.
SCREENING
 WARD TIP
WARD TIP
One percent of adolescents have made at least one suicide gesture.
 Routine health care should involve audiometry and vision screening, blood pressure
checks, exams for scoliosis.
Routine health care should involve audiometry and vision screening, blood pressure
checks, exams for scoliosis.
 Breast and pelvic exams in females may also be necessary, and self-exams should
be emphasized.
Breast and pelvic exams in females may also be necessary, and self-exams should
be emphasized.
 Likewise, examination for scrotal masses is necessary in males with emphasis on
self-examination.
Likewise, examination for scrotal masses is necessary in males with emphasis on
self-examination.
 STDs (gonorrhea and chlamydia), including HIV should be considered in those adolescents with high-risk behaviors.
Counsel sexually active adolescents on contraception and protection against STDs.
STDs (gonorrhea and chlamydia), including HIV should be considered in those adolescents with high-risk behaviors.
Counsel sexually active adolescents on contraception and protection against STDs.
 Screen with Pap smears within 3 years of the onset of sexual activity or at 21
years of age.
Screen with Pap smears within 3 years of the onset of sexual activity or at 21
years of age.
 Adolescents who are engaged in one risk-taking activity such as smoking cigarettes
are at greater risk for experimenting with drugs and alcohol.
Adolescents who are engaged in one risk-taking activity such as smoking cigarettes
are at greater risk for experimenting with drugs and alcohol.
 Mental health screening at each yearly visit.
Mental health screening at each yearly visit.
PHYSICAL EXAM
 Sexual maturity should be assessed at each visit.
Sexual maturity should be assessed at each visit.
 Assess for scoliosis at each visit until Tanner stage 5 is achieved.
Assess for scoliosis at each visit until Tanner stage 5 is achieved.
PREGNANCY
EPIDEMIOLOGY
 In 2014, a total of 249,078 babies were born to women aged 15–19 years, for a birth
rate of 24.2 per 1,000 women in this age group. This is another historic low for U.S.
teens and a drop of 9% from 2013(CDC).
In 2014, a total of 249,078 babies were born to women aged 15–19 years, for a birth
rate of 24.2 per 1,000 women in this age group. This is another historic low for U.S.
teens and a drop of 9% from 2013(CDC).
CONTRACEPTION
 EXAM TIP
EXAM TIP
An ↑ in the number of years of schooling for a woman delays the age at which a woman marries and has her first child.
EPIDEMIOLOGY
Among U.S. high school students surveyed in 2015:
 41% had ever had sexual intercourse.
41% had ever had sexual intercourse.
 30% had had sexual intercourse during the previous 3 months, and, of these
30% had had sexual intercourse during the previous 3 months, and, of these
 43% did not use a condom the last time they had sex.
43% did not use a condom the last time they had sex.
 14% did not use any method to prevent pregnancy.
14% did not use any method to prevent pregnancy.
 21% had drunk alcohol or used drugs before last sexual intercourse (CDC).
21% had drunk alcohol or used drugs before last sexual intercourse (CDC).
RISK FACTORS
Factors associated with early sexual activity include poor academic performance, lower expectations for education, poor perception of life options, low school grades, and involvement in other high-risk behaviors such as substance abuse.
FORMS OF CONTRACEPTION
 Abstinence, condoms (male and female), diaphragm, cervical cap, spermicides, or
some combination of these.
Abstinence, condoms (male and female), diaphragm, cervical cap, spermicides, or
some combination of these.
 Hormonal methods include oral contraceptive pills and injectable or implantable
hormones, and hormone patches.
Hormonal methods include oral contraceptive pills and injectable or implantable
hormones, and hormone patches.
 Intrauterine devices are not recommended for adolescents because of the ↑ risk
of sexually transmitted infections.
Intrauterine devices are not recommended for adolescents because of the ↑ risk
of sexually transmitted infections.
COMBINATION ORAL CONTRACEPTIVES
Usually consist of either 50, 35, 30, or 20 μg of an estrogenic substance such as mestranol or ethinyl estradiol plus a progestin.
SIDE EFFECTS
 WARD TIP
WARD TIP
Adolescents who smoke may ↑ their risk for side effects from oral contraceptives.
 Short-term effects may include nausea and weight gain.
Short-term effects may include nausea and weight gain.
 Other possible effects include thrombophlebitis, hepatic adenomas, myocardial infarction,
and carbohydrate intolerance.
Other possible effects include thrombophlebitis, hepatic adenomas, myocardial infarction,
and carbohydrate intolerance.
POTENTIAL BENEFITS
Long-range benefits may include ↓ risks of benign breast disease and ovarian disease.
HIV/AIDS
See the Infectious Disease chapter.
EPIDEMIOLOGY
 HIV/AIDS is the sixth leading cause of death among adolescents aged 15–24 years.
HIV/AIDS is the sixth leading cause of death among adolescents aged 15–24 years.
 One half of all new infections in the United States occur in people younger than
25 years of age.
One half of all new infections in the United States occur in people younger than
25 years of age.
SCREENING
Screening should include adolescents with risk factors such as previous STD, unprotected sex, practicing insertive or receptive anal sex, trading sex for money or drugs, homelessness, intravenous drug or crack cocaine use, being the victim of sexual abuse.
Child Abuse
 WARD TIP
WARD TIP
If the story doesn’t make sense, suspect abuse.
DEFINITION
Child maltreatment encompasses a spectrum of abusive actions, and lack of action, that result in morbidity or death. Forms of child abuse include:
 Physical abuse
Physical abuse
 Sexual abuse
Sexual abuse
 Neglect
Neglect
RISK FACTORS
 WARD TIP
WARD TIP
Mongolian spots can be confused with bruises.
 Parental risk factors:
Parental risk factors:
 Low socioeconomic status.
Low socioeconomic status.
 Mother’s age (young).
Mother’s age (young).
 History of being abused as a child.
History of being abused as a child.
 Alcoholism, substance abuse, psychosis.
Alcoholism, substance abuse, psychosis.
 EXAM TIP
EXAM TIP
A baby should never be shaken for any reason.
 Social isolation.
Social isolation.
 Child risk factors:
Child risk factors:
 Children with special needs, handicapped children (chronic illness, congenital
malformation, mental retardation).
Children with special needs, handicapped children (chronic illness, congenital
malformation, mental retardation).
 Prematurity.
Prematurity.
 EXAM TIP
EXAM TIP
The most common reason for shaking a baby is inconsolable crying.
 Age <3 years.
Age <3 years.
 Nonbiologic relationship to the caretaker.
Nonbiologic relationship to the caretaker.
 “Difficult” children.
“Difficult” children.
 Family and environmental factors:
Family and environmental factors:
 Unemployment.
Unemployment.
 Intimate partner violence.
Intimate partner violence.
 Poverty.
Poverty.
PHYSICAL ABUSE
 WARD TIP
WARD TIP
Sometimes abusive parents “punish” their children for enuresis or resistance to toilet training by forcibly immersing their buttocks in hot water.
Suspect if:
 Injury is unexplained or unexplainable.
Injury is unexplained or unexplainable.
 Injury is inconsistent with mechanism suggested by history.
Injury is inconsistent with mechanism suggested by history.
 History changes each time it is told.
History changes each time it is told.
 There are repeated “accidents.”
There are repeated “accidents.”
 There is a delay in seeking care.
There is a delay in seeking care.
Skin Manifestations
Bruises
 EXAM TIP
EXAM TIP
Skeletal injuries suspicious of abuse: “Some Parents Are Maliciously Mean” (or Parents Should Manage Anger)
 Most common manifestation of physical abuse
Most common manifestation of physical abuse
 Suspicious if:
Suspicious if:
 Seen on nonambulatory infants.
Seen on nonambulatory infants.
 Have geometric pattern (belt buckles, looped-cord marks).
Have geometric pattern (belt buckles, looped-cord marks).
Burns
 Suspicious if:
Suspicious if:
 Involve both hands or feet in stocking-glove distribution or buttocks with sharp
demarcation line (forced immersion in hot water).
Involve both hands or feet in stocking-glove distribution or buttocks with sharp
demarcation line (forced immersion in hot water).
 Cigarette burns—if nonaccidental, usually full-thickness, sharply circumscribed.
Cigarette burns—if nonaccidental, usually full-thickness, sharply circumscribed.
 “Branding” injuries (inflicted by hot iron, radiator cover, etc).
“Branding” injuries (inflicted by hot iron, radiator cover, etc).
Skeletal Injuries
Suspicious if:
 Spiral fractures of lower extremities in nonambulatory children (see Figure 6-2A and B).
Spiral fractures of lower extremities in nonambulatory children (see Figure 6-2A and B).
FIGURE 6-2. (A) Spiral fracture (arrow) of the femur in a nonambulatory child, consistent with nonaccidental trauma. (B) Same child 2 months later. Note the exuberant callus formation at all the fracture sites in the femur and proximal tibia and fibula.
 Posterior rib fractures (usually caused by squeezing the chest).
Posterior rib fractures (usually caused by squeezing the chest).
 Fractures of different Ages.
Fractures of different Ages.
 Metaphyseal “chip” fractures (usually caused by wrenching).
Metaphyseal “chip” fractures (usually caused by wrenching).
 Multiple fractures.
Multiple fractures.
 Scapular and clavicle fractures.
Scapular and clavicle fractures.
 EXAM TIP
EXAM TIP
CNS injuries suspicious of abuse: “Mothers, Refuse Shaking!” (Metaphyseal fractures, Retinal hemorrhages, Subdural hematoma)
Central Nervous System (CNS) Injuries
 WARD TIP
WARD TIP
Epiphyseal-metaphyseal injury is virtually diagnostic of physical abuse in an infant, since an infant cannot generate enough force to fracture a bone at the epiphysis.
 Most common cause of death in child abuse: “Shaken baby syndrome.”
Most common cause of death in child abuse: “Shaken baby syndrome.”
 Occurs due to violent shakes and slamming against mattress or wall while an infant
is held by the trunk or upper extremities.
Occurs due to violent shakes and slamming against mattress or wall while an infant
is held by the trunk or upper extremities.
 Findings include:
Findings include:
 Retinal hemorrhages.
Retinal hemorrhages.
 Subdural hematoma (from rupturing of bridging veins between dura mater and brain cortex).
Subdural hematoma (from rupturing of bridging veins between dura mater and brain cortex).
 Symptoms include:
Symptoms include:
 Lethargy or irritability
Lethargy or irritability
 Vomiting
Vomiting
 Seizures
Seizures
 Bulging fontanelle
Bulging fontanelle
ABDOMINAL INJURIES
 WARD TIP
WARD TIP
Shaken baby syndrome can mimic meningitis or sepsis.
 Second most common cause of death in child abuse.
Second most common cause of death in child abuse.
 Usually no external marks. Most commonly, liver or spleen is ruptured.
Usually no external marks. Most commonly, liver or spleen is ruptured.
 Symptoms include vomiting, abdominal pain or distention, shock.
Symptoms include vomiting, abdominal pain or distention, shock.
SEXUAL ABUSE
 Includes genital, anal, oral contact; fondling; and involvement in pornography.
Includes genital, anal, oral contact; fondling; and involvement in pornography.
 Most common perpetrators—fathers, stepfathers, mother’s boyfriend(s) (adults known
to child).
Most common perpetrators—fathers, stepfathers, mother’s boyfriend(s) (adults known
to child).
 Suspect if:
Suspect if:
 Genital trauma.
Genital trauma.
 STDs in small children.
STDs in small children.
 Sexualized behavior toward adults or children.
Sexualized behavior toward adults or children.
 Unexplained decline in school performance.
Unexplained decline in school performance.
 Runaway.
Runaway.
 Chronic somatic complaints (abdominal pain, headaches).
Chronic somatic complaints (abdominal pain, headaches).
 Symptoms include:
Symptoms include:
 May be totally absent.
May be totally absent.
 Tears/bleeding in female or male genitalia.
Tears/bleeding in female or male genitalia.
 Anal tears or hymenal tears (not very reliable symptoms).
Anal tears or hymenal tears (not very reliable symptoms).
EVALUATION OF SUSPECTED ABUSE
 WARD TIP
WARD TIP
Children too young to talk about what has happened to them (generally younger than 2) should have a complete skeletal survey if you suspect abuse.
Physical Abuse
 Bleeding disorders must be ruled out in case of multiple bruises.
Bleeding disorders must be ruled out in case of multiple bruises.
 X-ray skeletal survey (skull, chest, long bones) in children < 2 years of age (to
look for old/new fractures).
X-ray skeletal survey (skull, chest, long bones) in children < 2 years of age (to
look for old/new fractures).
 Computed tomographic (CT) scans of the head/abdomen as indicated.
Computed tomographic (CT) scans of the head/abdomen as indicated.
 Ophthalmology consult.
Ophthalmology consult.
Sexual Abuse
 Sexual abuse includes any sexual activity (nonconsensual and consensual) between an adult and a child.
Sexual abuse includes any sexual activity (nonconsensual and consensual) between an adult and a child.
 Cultures for STDs, test for presence of sperm, if indicated (usually within 72
hours of assault).
Cultures for STDs, test for presence of sperm, if indicated (usually within 72
hours of assault).
MANAGEMENT
 WARD TIP
WARD TIP
A child who presents with multiple fractures at multiple sites and in various stages of healing should be considered abused until proven otherwise.
 If abuse is suspected, it must be reported to child protective services (CPS) (after
medical stabilization, if needed).
If abuse is suspected, it must be reported to child protective services (CPS) (after
medical stabilization, if needed).
 All siblings need to be evaluated for abuse, too (up to 20% of them might have
signs of abuse).
All siblings need to be evaluated for abuse, too (up to 20% of them might have
signs of abuse).
 Disposition of the child (i.e., whether to discharge the patient back to parents
or to a CPS worker if medically cleared) has to be decided by CPS in conjunction with
treating physician.
Disposition of the child (i.e., whether to discharge the patient back to parents
or to a CPS worker if medically cleared) has to be decided by CPS in conjunction with
treating physician.
 Family must receive intensive intervention by social services and, if needed, legal
authorities.
Family must receive intensive intervention by social services and, if needed, legal
authorities.
 Remember: If sent back to abusive family without intervention, up to 5% of children can be
killed and up to 25% seriously reinjured.
Remember: If sent back to abusive family without intervention, up to 5% of children can be
killed and up to 25% seriously reinjured.
NEGLECT
 WARD TIP
WARD TIP
Management of abuse:
Suspect
↓
Report
↓
Disposition
↓
Family counseling
DEFINITION
 Neglect is the most common form of reported abuse.
Neglect is the most common form of reported abuse.
 Neglect to meet nutritional, medical, and/or developmental needs of a child can
present as:
Neglect to meet nutritional, medical, and/or developmental needs of a child can
present as:
 Failure to thrive.
Failure to thrive.
 Poor hygiene (severe diaper rash, unwashed clothing, uncut nails).
Poor hygiene (severe diaper rash, unwashed clothing, uncut nails).
 Developmental/speech delay.
Developmental/speech delay.
 Delayed immunizations.
Delayed immunizations.
 Not giving treatment for chronic conditions.
Not giving treatment for chronic conditions.
MANAGEMENT
If nonorganic (i.e., due to insufficient feeding) failure to thrive is suspected:
 Patient should be hospitalized and given unlimited feedings for 1 week; 2 oz/24
hours of weight gain is expected.
Patient should be hospitalized and given unlimited feedings for 1 week; 2 oz/24
hours of weight gain is expected.
 All suspected cases of neglect must be reported to CPS.
All suspected cases of neglect must be reported to CPS.
MUNCHAUSEN SYNDROME BY PROXY
DEFINITION
 Parent/caregiver either simulates illness, exaggerates actual illness, or induces
illness in a child.
Parent/caregiver either simulates illness, exaggerates actual illness, or induces
illness in a child.
 Psychiatrically disturbed parent(s) gain satisfaction from attention and empathy
from hospital personnel or their own family because of problems created.
Psychiatrically disturbed parent(s) gain satisfaction from attention and empathy
from hospital personnel or their own family because of problems created.
EPIDEMIOLOGY
 EXAM TIP
EXAM TIP
Baron von Munchausen was an 18th-century nobleman who became famous because of his incredible stories, which included travel to the moon and flying atop a cannonball over Constantinople, as well as visiting an island made of cheese. His name became a synonym for gross confabulations.
 Affected children are usually < 6 years old.
Affected children are usually < 6 years old.
 Parent (usually mother) has some medical knowledge.
Parent (usually mother) has some medical knowledge.
SIGNS AND SYMPTOMS
 Vomiting (induced by ipecac).
Vomiting (induced by ipecac).
 Chronic diarrhea (from laxatives).
Chronic diarrhea (from laxatives).
 Recurrent abscesses or sepsis (usually polymicrobial, from injecting contaminated
fluids).
Recurrent abscesses or sepsis (usually polymicrobial, from injecting contaminated
fluids).
 Apnea (from choking the child).
Apnea (from choking the child).
 Fever (from heating thermometers).
Fever (from heating thermometers).
 Bloody vomiting or diarrhea (from adding blood to urine or stool specimens).
Bloody vomiting or diarrhea (from adding blood to urine or stool specimens).
DIAGNOSIS
Diagnosis is difficult, but is initiated by removing child from parent via hospitalization. Usually, child without access to parent will have all/most symptoms resolved; testing will also usually be normal.
MANAGEMENT
 Admission to the hospital for observation, possibly using hidden video cameras.
Admission to the hospital for observation, possibly using hidden video cameras.
 All cases of suspected Munchausen syndrome by proxy must be reported to CPS.
All cases of suspected Munchausen syndrome by proxy must be reported to CPS.
SUDDEN INFANT DEATH SYNDROME (SIDS)
DEFINITION
 Sudden death of an infant (< 1 year old) that remains unexplained after thorough
case investigation, autopsy, and review of the clinical history.
Sudden death of an infant (< 1 year old) that remains unexplained after thorough
case investigation, autopsy, and review of the clinical history.
 SIDS is one of the leading causes of death of infants.
SIDS is one of the leading causes of death of infants.
ETIOLOGY
Apnea hypothesis.
DIAGNOSIS
Difficult to differentiate from intentional harm.
PREVENTION
 WARD TIP
WARD TIP
Infants unable to roll over should be placed on the back while sleeping.
 There has been a vast ↓ in the number of cases since the trend of having infants
sleep on their backs (supine).
There has been a vast ↓ in the number of cases since the trend of having infants
sleep on their backs (supine).
 The number one preventive measure to date is parental education, though the use
of cardiorespiratory monitoring in the home is being debated.
The number one preventive measure to date is parental education, though the use
of cardiorespiratory monitoring in the home is being debated.
 Limiting passive smoke exposure.
Limiting passive smoke exposure.
 Do not use soft bedding, pillows, stuffed animals, loose blankets.
Do not use soft bedding, pillows, stuffed animals, loose blankets.
 Co-sleeping with the parent increases the risk.
Co-sleeping with the parent increases the risk.

