FOR SOME COUPLES, assessing treatment options is not that difficult. If you have blocked tubes or your partner has a low sperm count, your doctor will recommend an aggressive treatment like IVF. But if you have open fallopian tubes, functioning ovaries, and your partner has a reasonable sperm count, then you can bypass IVF and opt for a less invasive and less expensive treatment. If you’re in this category, then you’re faced with do-it-yourself (DIY) or something less invasive than IVF, like intrauterine transfer (IUI), which we’ll discuss a little later. Age is also a red flag if you want to use your own eggs, so you need to roll this into your treatment plan.
Essentially, you should weigh your likelihood of success against procedure costs, time available, your fertile window, and the emotional aspects of being infertile. Everyone places a different value on these variables. If you’re in your late 30s, time is more valuable to you than it would be if you were in your late 20s.
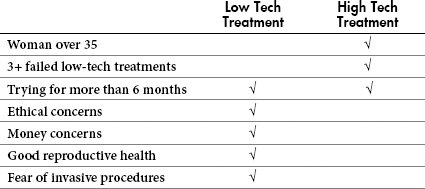
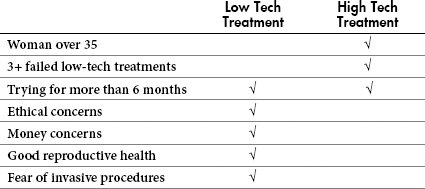
Table 6.1. Selecting your treatment options
There are a number of factors you need to consider before committing to a fertility treatment. For instance, if you’re over 35 and you attempted three or more low-tech procedures that failed (treatments covered in this chapter), your best bet is to opt for a high-tech method like IVF. If time is a concern because you have poor egg quality or you’re older and want to make sure you can use your own eggs instead of a donor’s, then you’ll also want to opt for IVF.
But what if you have your hopes set on options outside of IVF? The most important thing to know is that any low-tech intervention will increase your odds of getting pregnant over intercourse alone. If you have concerns over money or ethics or if you’re not ready for an invasive treatment, then low-tech options can provide you with a golden opportunity. But that doesn’t mean that low-tech (or even high-tech) treatments work for everyone.
Matching Your Treatment with Your Situation
IVF was way out of our reach cost-wise. We opted for insemination instead.
—Lydia, 43, pediatric nurse practitioner
So what will give you the best odds of getting pregnant? If you’re over 38, you should opt for the most aggressive treatment available, especially if you have a good prognosis. This is because your odds of getting pregnant increase with an aggressive treatment. The same recommendation goes if you have a poor prognosis since aggressive treatments may be the only way you even have a chance at getting pregnant.
Your chances of getting pregnant rest on a number of biological factors that you have little or no control over. These include the results from your joint workups, your reproductive system working normally, proper release of your egg, ability of your partner’s sperm to fertilize your egg, and the ability of your fertilized egg to develop into a viable embryo, implant into your uterine wall, and continue to develop as it should. Add your values, hopes, and concerns to the mix, and then assign a value to time to help you choose an ideal treatment for your situation.
Many times tossing your birth control pills is the first step to becoming pregnant. This whole notion of waiting until estrogen is out of your system before trying to have a baby is nonsense. If you want to get pregnant, you’re better off trying as soon as you discontinue your pills. Keep in mind that the right thing to do before discontinuing any medication is to consult with your physician first.
Besides the pill, there are other forms of birth control you may use, such as intrauterine devices (IUDs), tubal ligations, or diaphrams. Table 6.2 describes how discontinuing these methods affects your chances of conceiving when you decide you’re ready become a mother.
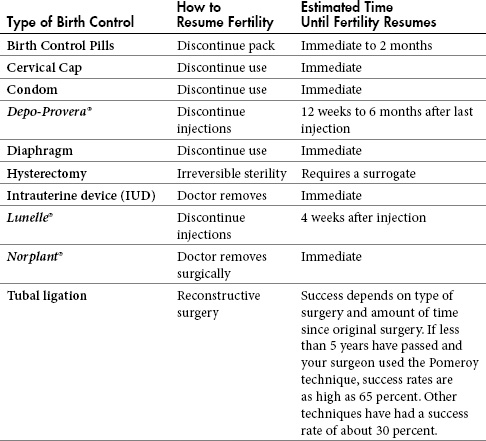
Table 6.2. Reversing common forms of birth control
WHAT ABOUT NATURAL TECHNIQUES?
Maybe you picked up this book because you know you need to see a fertility doctor. If so, don’t count yourself out yet. There still are a number of things you can do to improve your chances in the baby department besides throwing out your birth control pills, condoms, or other contraceptives. The most important of these is knowing your body’s ovulation signs better than you ever thought you’d need to.
If you have a history of regular menstrual cycles and you know your cycle length, subtract 16 days. For instance, if your cycle is 28 days, this would be day 12 or if your cycle is 30 days, this would be day 14. Whatever day you come up with is the day you should begin having sex for three days in row.
If your partner has low sperm count and you’ve heard you should have sex every other day, don’t believe it. The last thing you want to do is miss your window. You’re better off ensuring that some sperm goes to the right place at the right time. Remember, getting pregnant requires only one sperm. And finding and fertilizing your egg is all about timing.
Identifying the time of the month you ovulate is vital if you want to increase your chances of conception. Whether you do this yourself (natural methods) or your doctor controls it for you (IVF) is entirely up to you.
There are three methods you’ll need to employ to determine your “fertile window.” Initially you should take your basal body temperature daily. Next you’ll need to verify the consistency of your cervical mucous. And finally you should use an ovulation predictor kit. But before we discuss each in detail, there are some obvious symptoms of ovulation that you should have no problem identifying:
• regular menstrual periods
• breast tenderness prior to menstruation
• abdominal cramps, twinges, bloating, or tenderness prior to menstruation
• increased vaginal wetness around midcycle
If you don’t have any of these symptoms and you haven’t had a fertility evaluation, you should have one before proceeding. Stress can occasionally make your menstrual period irregular, but this is normal. An absence of any or all of these basic symptoms may indicate that you’re not ovulating. Before we discuss ways to pinpoint the days you’re fertile, visualize your cycle divided into four major components: menstruation, infertile days, fertile days, and more infertile days.
These four components fall within three phases: follicular (phase when your follicles grow), ovulatory (phase when you ovulate), and luteal (phase that makes up majority of your infertile days).
Figure 6.1. Fertility cycle
Illustrator: Adam Hanin
Searching for a cheap, low-tech way to pinpoint your fertile time of the month? One of the oldest fertility awareness methods around is charting your basal body temperature (BBT) and cervical mucous. If you want modern technology, you can confirm those results with an in-home ovulation predictor kit (OPK). While tons of fertility books (even best sellers) have instructed women to check their cervical position, this is not useful. Contrary to popular belief, the cervix doesn’t move much. Your best indicators of ovulation are BBT and cervical mucous.
Couples who are not ready to dive into fertility treatment, those waiting for a consultation with an RE, or those taking a breather after a failed attempt often find natural fertility methods useful.

![]() What to Look for with Your BBT
What to Look for with Your BBT
You’re looking for a fluctuation of at least 0.4 degrees Fahrenheit after ovulation that makes your chart show low temperatures followed by higher ones. Low temperatures signal your follicular phase and higher temperatures signal your luteal phase. The day you move from one phase to the other is the day you ovulate.
Proponents of natural family planning claim this process is simpler than reading headlines off a weekday newspaper while lying in bed (without walking outside to retrieve it). All you need is a BBT thermometer (available at any drugstore), an ovulation chart, and a pen. BBT thermometers are ultrasensitive, measuring within a tenth of a degree, whereas regular thermometers measure within a half a degree. Most in-store BBT thermometers cost between $12 and $15, though some are more. If you’re buying online, expect a competitive price break, and remember that most will include a shipping fee. If you’re considering a glass thermometer, you’ll want to find one that’s nonmercury, though it doesn’t have to be one marketed specifically for fertility. BBT is the temperature of your body at rest, so keep your thermometer handy at your bedside so you can take your BBT while you’re still lying flat on your back.
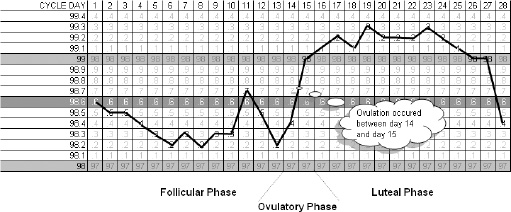
Figure 6.2. Sample fertility forecasting chart
Illustrator: Adam Hanin
This means you shouldn’t sit up, get out of bed, go to the bathroom, drink, eat, or do anything before you take your morning temperature. Any activity at all raises your temperature. Although it may sound awkward, if you use this technique over several months, it becomes as routine as brushing your teeth upon waking. After you take your resting temperature each morning, plot it on your chart (we’ve provided a full-size fertility forecasting chart in the Appendix).
While this method works if done correctly, critics say it’s time consuming and tedious. But if this is all it takes to get you pregnant, chances are you won’t mind the inconvenience. Here are a few tips to help you get an accurate BBT.
• Take your temperature at the same time each day (set an alarm if needed).
• Your BBT is more accurate after at least five hours of sleep.
• Take it three times in a row just to be sure.
• Plot your temperature on the chart in the back of this book.
The closer you can take your BBT to your waking time (before your feet touch the floor) each day, the better. BBT temperature variation is 0.2 degrees per hour (lower if you take it earlier and higher if you take it later). So every change in time (earlier or later) can skew your results, causing you to possibly misjudge your ovulation date.

![]() What Sexual Position Is Conducive to Getting Pregnant?
What Sexual Position Is Conducive to Getting Pregnant?
Finding the “right” sexual position is not as important as making sure your partner ejaculates deep within your vagina. It’s also not important that your partner stay engaged afterward, but it can’t hurt. To ensure gravity works for you, lie on your back for at least five minutes longer. No need to hang your feet from the ceiling or prop your feet on pillows, though.
Did you think trying to have a baby meant you needed to have intimate knowledge of the fluid your cervix secretes? If this is unappetizing to you, you’re not alone. Many women feel this way, but once they begin checking for these signs they find it’s no stranger than inserting a tampon or strapping on a pad with wings.

![]() Consistency of Fertile Mucous
Consistency of Fertile Mucous
Cervical mucous during your fertile window has the consistency of raw egg whites. Fertile mucous is clear and stretches more than an inch. At any other time of the month your mucous is thick, opaque, and does not stretch.
When you’re on the lookout for what we call “purposeful mucous,” you need to look for it every time you go to the bathroom. Here’s the best way to spot it.
• Wipe your vaginal area (front to back) with toilet tissue and check it before urinating.
• Examine your panties for discharge (mucous) during bathroom breaks.
• Give your mucous a stretch test by pressing it between your finger and thumb and then pulling them apart. If the mucous is clear (egg-white consistency) and stretches more than an inch, grab your partner for a steamy rendezvous.
The lining of your cervical canal produces purposeful mucous, and its consistency changes throughout your cycle. Charting will help you determine which phase your mucous is in: dry (no mucous), wet (some mucous), slippery (fertile mucous), or tacky (sticky mucous). When you’re fertile, this mucous helps your partner’s sperm swim toward your cervix so it can find your egg.
One step up from charting your natural fertility signs is using store-bought OPKs that are less complicated, more user-friendly, and help eliminate human error. OPKs come packaged with test sticks similar to in-home pregnancy test kits except instead of testing for human chorionic gonadotropin (hCG), they measure the amount of luteinizing hormone (LH) in your urine. But don’t be fooled into thinking these kits work for everyone.
WHAT CRITICS SAY ABOUT OPKs
• Can’t confirm that you actually ovulated.
• Not reliable if you’re taking certain injectable fertility drugs like Pergonal or hCG.
• Harder to use if your cycle is irregular.
• Some tests are more difficult to read than others.
• Anything but cheap, ranging between $15 and $50, depending on the brand and number of test sticks. Each stick is good for only a single use.
• Inaccurate for women whose eggs fail to release from their follicles following LH surge (luteinized unruptured follicle syndrome, or LUFS).
• Less accurate for women with PCOS because their LH is higher than normal, giving them a false positive.
• Less accurate for women over 40 with premature ovarian failure (POF) because they secrete more LH (and FSH), giving them a false positive.
OPKs work by measuring the LH surge that precedes ovulation. Normally your LH elevates 24 to 36 hours before you ovulate until it peaks. This peak is your LH surge. To improve your chance of getting pregnant, you’ll want to have sex with your partner a day or two before and the day of ovulation.
WHAT SUPPORTERS SAY ABOUT OPKs
• more than 97 percent accurate if used correctly
• easy to use
• relatively inexpensive, from under $20 (generic) to under $40 and up (brand name)
• readily available at just about any drugstore
• convenient and small enough to carry in your purse
Just like home pregnancy test kits, OPKs require you to urinate on a test stick for a specified number of seconds (check directions carefully) before reading results. The results are displayed by two lines, one of which turns darker (result line) than the first (control line) when your test is positive. Keep in mind that sometimes the lines will darken if left for several hours, so don’t assume you have a LH surge if you don’t read your test as its directions specify. There are an array of OPK brands to choose from, including Clearblue™, First Response™, generic brands, and many others.

![]() What If You Have a Vacation Planned?
What If You Have a Vacation Planned?
One of the benefits of OPKs is that they’re fast travel companions—small enough to place several weeks’ supply in your garment bag without compromising packing space.
What is the best day to start testing? If your cycles are regular, you’ll want to test 16 days before your next period. But if your cycles are irregular, you’ll want to test every few days to make sure you capture the big event.
These high-tech devices give you a little more reassurance than an OPK. Fertility monitors work similarly to scuba diving computers except instead of storing data about your dives, they store information about your cycle. They measure estrogen and LH levels and are able to detect onset of ovulation five days before it occurs. Couples with hectic schedules rave about these devices because they give more time to plan sexual interludes. But even with their increased capabilities they’re not without flaws.
WHAT CRITICS SAY ABOUT FERTILITY MONITORS
• Labor intensive—requires you to test every morning at the same time beginning with the first day of your menstrual period.
• Less effective if you’re menopausal or breastfeeding or if you have impaired liver or kidney function or are taking antibiotics containing tetracycline.
• Expensive, ranging from price tags just over $150 to $200 and up, not including test sticks.
• Like OPKs, they can’t confirm you’ve released an egg.
What’s the process for using a fertility monitor? Simply turn on the monitor first thing each morning, take a urine test if it prompts you to, and read your daily fertility status on the display window. You should begin using it on or before the fifth day of your cycle, but to ensure accuracy, read the instructions carefully. There are an array of fertility monitors to choose from. Each requires a different level of LH to register a positive surge, so compare your options before making a purchase. Some actually give you three separate readings.
• low fertility: very small chance of conceiving
• high fertility: increased chance of conceiving
• peak fertility: highest chance of conceiving
WHAT SUPPORTERS SAY ABOUT FERTILITY MONITORS
• about 98 percent accurate
• able to find your fertility window days in advance
• give a greater sense of confidence
• able to plan sex ahead of time
• can be used when taking injectable fertility drugs
Did you ever think predicting ovulation could be as simple as licking a lens? Probably not, but this is exactly what you’ll get if you buy a saliva fertility monitor. This lipstick-sized gem is actually a minimicroscope and works by magnifying the way your saliva reacts days before ovulation. Have you ever studied frost on a windowpane? The pattern that emerges on the microscope’s lens when you’re fertile resembles what you might see on window pane in chilly weather.
WHAT CRITICS SAY ABOUT SALIVA FERTILITY MONITORS
• May not work on all women.
• Ferning (see the following paragraph and illustration) may not be distinct.
• Women may not fern on every fertile day.
Just before you ovulate you have an “estrogen surge” that increases the salt content in your saliva. This increase in salt forms a distinct crystalline pattern called “ferning” that you can see through a microscope lens. When you see this fern-like pattern in your saliva, it’s the best time to have sex with your partner.

Figure 6.3. Saliva fertility monitor
Illustrator: Adam Hanin
The best time to test is before you eat, drink, or brush your teeth in the morning, because doing so will interfere with your results. Simply lick the removable slide (or viewing window if built in), then insert it into the monitor and allow it to dry for about five minutes. When you turn it on, look through the eyepiece for the result. If you test on infertile days, you’ll see dots and circles with no particular pattern. On fertile days you’ll see a pattern that emulates fronds of a fern. Once you see the results, you can record them on your fertility chart.
WHAT SUPPORTERS SAY ABOUT SALIVA FERTILITY MONITORS
• 98 percent accurate
• safe and easy to use
• no urine handling
• lens is washable and reusable, so it’s a one-time purchase
• predicts ovulation up to five days in advance
• convenient, portable, fits in any small tote
• you can test anytime, anywhere, unlike OPKs
• relatively inexpensive
Keep in mind that smoking, human error, or even the environment can affect your test results. For instance, if you’re taking your test while lounging on a beach, you run the risk of collecting more salt crystals on your lens than what is normally present in your saliva.
There are many brand names to choose from, including Clearblue, Ovu-test, Ovucue, Fertile Focus, and Ovulook. If you’re looking for one that stores and analyzes data similarly to a fertility monitor, prepare to shell out up to $150 to $200 and up.

![]() Options That Make Sense
Options That Make Sense
OPKs or fertility monitors are excellent if you want to pinpoint ovulation, have religious or ethical concerns, or are not ready to dive into high-tech fertility options. But remember that they don’t work for everyone. Always consult with a trained RE (or urologist if your partner is diagnosed with male infertility) so you know exactly what you’re dealing with.
Does the thought of producing a sperm sample in a public bathroom give your partner the heebie-jeebies? The idea of producing anything “on demand,” especially if it involves a tiny plastic cup and half your child’s genetic makeup, is enough to give any man performance anxiety. This is when an in-home sperm test can be helpful.
WHAT CRITICS SAY ABOUT IN-HOME SPERM TESTS
• less accurate than a Kruger or WHO—only 78 percent
• lacks in-depth information on sperm quality, movement, shape, and percentage of normal cells
There are a couple of options for in-home sperm tests. The first FDA-approved home sperm count tests, SpermCheck and FertilCount, are two of the most common. They sell for $30 to $40, depending on the retailer. This simple test allows you to evaluate two semen samples to confirm whether your partner’s sperm concentration is within normal range of 20 million/ml. It works by staining cells in your partner’s sperm sample to produce a color. Once time has elapsed, he simply compares his sample’s color intensity to a color reference contained in a test stick.
You can find this kit at just about any drugstore, or to save him what could be an embarrassing trip, you can purchase it online and have it shipped to your front door by an online pharmacy.
WHAT SUPPORTERS SAY ABOUT IN-HOME SPERM TESTS
• easy-to-use
• convenient
• reduces embarrassment and anxiety associated with producing a sample on demand
• can buy it online without ever leaving your home
• relatively inexpensive
While in-home sperm tests are convenient and do give you some information about sperm count, they don’t provide in-depth information about sperm quality, movement, shape, and percentage of normal cells (see page 25). If your partner’s sperm test is low or he has one or more risk factors for infertility (see page 43), then he’ll need to see a urologist for a more in-depth analysis.
Clomid
Most people have heard of the fertility drug Clomid and its potential for causing multiple pregnancies. But what you may not know is that Clomid doesn’t work for everyone. While 80 percent of women who use it do ovulate within the first three months of treatments, only 40 percent actually get pregnant. This attrition rate is due to a wide range of factors (i.e., your age, quality of your partner’s sperm, if fertilization doesn’t occur, or if your follicle fails to release your egg) that prevent pregnancy.

![]() Clomid by Any Other Name . . .
Clomid by Any Other Name . . .
Clomid and Serophene® are brand names for clomiphene citrate. Women who take either brand ovulate irregularly, don’t ovulate at all, or have PCOS. Doctors also prescribe clomiphene citrate to fertile women in hopes of producing multiple eggs (superovulation) to increase their chances for conception.
INTRAUTERINE INSEMINATION (IUI)
If you have unexplained infertility, “unfriendly” cervical mucous, or your partner has a low sperm count or sluggish sperm, you may want to consider an option that gives his sperm a head start. Intrauterine insemination (IUI) is a solution in all these areas and also works well for same-sex female couples. It allows sperm to bypass your cervix without encountering hostile cervical mucous that could deter them. In IUI your doctor introduces a quantity of “washed” sperm into your uterus via a catheter to increase the likelihood that your egg fertilizes.
We Opted for IUI
My treatment initially started with a month of taking metformin, regulating my diet to drop carbs and eat more often during the day, and just generally get my body into a stable state. Once I was ready to actually start the cycle, I was given clomid. I took clomid for five days to increase the number of follicles that would possibly mature into eggs (to increase the number of eggs released during ovulation). The next step happened two weeks later, when I went in for an ultrasound to measure the follicles. We had five follicles of a nice size. Dr. Potter told us we were ready. We replied, “WE’RE ready!” So later that day I gave myself two injections of ovidrel. This caused my body to ovulate within the next 36 hours. The next day my wife and I went to the clinic, and I was inseminated via IUI. The following day we went in for a second insemination, at which point Dr. Potter let my wife push the button. That was a really special moment for me because she was involved.
—Tabby, 33, software engineer

![]() Do I Have to Take Fertility Drugs When Opting for IUI?
Do I Have to Take Fertility Drugs When Opting for IUI?
Fertility drugs will increase your success rate by stimulating your ovaries and helping you produce eggs, but it’s not necessary to take them. With IUI you have the option of IUI only, IUI with Clomid therapy, or IUI with fertility injections. It’s wise to discuss each of these with your doctor before you commit to a treatment.
Preparation for your IUI is straightforward. Most states require infectious disease testing for both you and your partner prior to treatment. These tests check for HIV, hepatitis, and other transferable diseases (see page 34). Once you’ve passed these tests, your doctor will give you an ultrasound to measure the size of your follicles. When they reach 18 to 20 mm, your doctor will administer human chorionic gonadotropin (hCG) to signal your body to release eggs (OPKs or fertility monitors also work). Next, hCG triggers your LH surge, which causes your follicles to release eggs. This happens 34 to 40 hours after your doctor administers it.

![]() Why Wash Sperm?
Why Wash Sperm?
Semen is a mixture of sperm cells, seminal fluid, and debris (dead sperm, white blood cells, mucous, and fat globules). You probably didn’t realize it, but semen contains prostaglandins, which cause menstrual cramping. Although sperm behaves fine in the vaginal environment, if your doctor injects raw sperm directly into your uterus, you would experience severe pain. So the goal of sperm washing is to separate healthy sperm from toxic seminal fluid. One method of doing this involves a specialized lab tech who layers sperm on top of a nutrient medium and spins it in a centrifuge. Spinning forces sperm cells to the bottom of the tube. Once spun, he draws this purified sperm into a syringe so your doctor can inseminate you.
Because we learned in chapter 1 that only a fraction of sperm reaches your distal fallopian tube, IUI gives your partner’s sperm a boost by injecting the healthiest ones directly into your uterus. Instead of sending in the “second string,” your doctor places the “elite runners” near the finish line so they can unite with your egg easily.
IUI Helps Bypass Low Sperm Count

Figure 6.4. Intercourse vs. IUI
Illustrator: Adam Hanin
Have you ever wondered what challenges your partner’s sperm must overcome to reach your egg? Quite a few to be exact. Sperm must travel about six inches, or fifteen centimeters. This journey sounds miniscule until you realize it’s 3,750 times the length of a sperm cell. A similar comparison would be if you swam forty miles to reach your work.
So what are the odds that your partner’s sperm will reach your egg? For instance, if your partner has 100 million sperm, 100 or less will reach your egg. But if your partner has only 10 million moving sperm, only about ten will find your egg. If you proceed with an IUI and your doctor takes that same sample of swimmers, he can probably isolate about 7 million and place those directly into your uterus. This increases your chance of fertilization by 70 times.
WHAT TO KNOW BEFORE GOING LOW OR HIGH TECH
This is how you get the most mileage from your fertility workup. Discuss your treatment options with your partner and your doctor. Thousands of couples have wasted years going low tech before learning that they either need to see a specialist or were never candidates for treatments to begin with. This is not the situation you want to find yourself in if you consider your time, effort, and money precious.
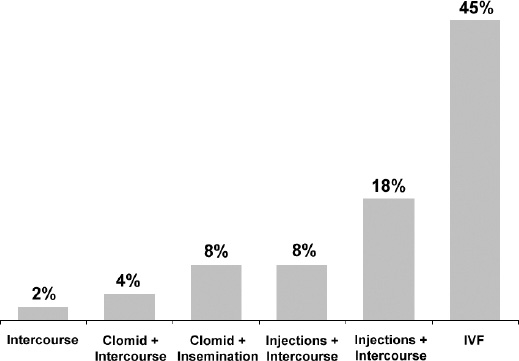
Figure 6.5. Chance of conception
Gauge your treatment by your chance of success. Each method has its benefits and risks. For instance, no method beats IVF when it comes to unexplained infertility. But it’s also expensive, invasive, and requires a multitude of medications.
When Everything Goes Right
The highest point was most likely the day that I got my positive result. I couldn’t believe it. I had tested on the day my cycle was supposed to start and got a negative. I tested again every day for three days with a negative. Finally, on the third day there was an extremely faint second line. My wife was out of town at a wedding, and I couldn’t get in touch with her. . . . I had inadvertently tested RIGHT as the wedding was happening. . . . She was a matron of honor, so there was no way I was going to get her attention. Those few hours were agonizing for me because I wanted to share the news with her. I went into the doctor right away, and at 3 p.m. the coordinator called me and I got my wife on the line and she told us that we tested positive for pregnancy. Neither of us knew what to say next, but we were very excited.
—Tabby, 33, software engineer
Customizing a Treatment to Fit Your Needs
REs, like tailors, customize an end result for their clients. But having your doctor customize a treatment for you is like having a tailor make you a suit without knowing your exact measurements. He may have a good eye and know what usually works for a person in a similar situation, but without knowing what occurs inside your body, there is no way he can know whether a treatment will work or not.
Keep in mind that just because Clomid therapy worked for your best friend doesn’t mean it will work for you. The same goes for injections and intercourse, injections and inseminations, and IVF. Basically, like a game of poker, everyone comes to the table with a different hand. Because so many factors are involved with uniting sperm and egg, it’s an educated guess as to how effective a treatment will be from couple to couple. This is why it’s important to define how long you and your partner are willing to continue trying a low-tech treatment before moving to a more aggressive therapy.
WHAT QUESTIONS SHOULD YOU ASK?
There’s no question that a number of natural methods are available to you to increase your chances of conceiving. From do-it-yourself gadgets like OPKs to fertility monitors to in-home sperm tests to charting daily fertility signs, you have more options today than ever before.
The most important piece of advice you can take away from this chapter is that even with all these new-fangled devices, there is no tradeoff for accuracy and time. While most of these devices work for some people, they’re not accurate on everyone.
If you don’t yet have an RE (for you) or a urologist (for your partner) and you don’t want to waste more time with fruitless measures, now is a good time to schedule those appointments.
Speaking from personal experience, if Jennifer kept charting her fertility signs without seeing an RE, she would have never known that one of her fallopian tubes was blocked. Basically, her chance of getting pregnant was no longer 5 percent per month. With only one functioning tube, it was 5 percent every other month. So instead of twelve chances a year, she and her husband, Adam, had only six. Couple this with Adam’s varicocele and low sperm count, and they had little choice but to pursue an aggressive therapy like IVF.
Answer the questions below. If you have more “yes” answers than “no,” then you’ll want to see a specialist sooner rather than later.
• Are you tired of trying natural methods to get pregnant?
• Is age or time a factor for you?
• Have you and your partner had a fertility workup?
• Have you discontinued your birth control?
• Have you been tracking your body’s natural fertility signs?
• Is charting your daily fertility signs too cumbersome?
• If you have open fallopian tubes, functioning ovaries, and your partner has a reasonable sperm count, then you can bypass IVF and opt for Clomid.
• If you’re a woman over 35 and have attempted three or more low-tech procedures that failed, your best bet is to opt for IVF.
• If you have diminished ovarian reserve and want to make sure you can use your own eggs instead of a donor’s, you’ll want IVF.
• One step up from charting your natural fertility signs is using store-bought OPKs or fertility monitors.
• Saliva-based fertility monitors are lipstick-sized minimicroscopes that allow you to test virtually anywhere.
• While in-home sperm tests are convenient, they don’t provide in-depth information.
• Only about 40 percent of women on Clomid get pregnant.
• With IUI, you have the option of IUI only, IUI with Clomid therapy, or IUI with fertility injections. Discuss your potential success rates with your partner and doctor before committing to a treatment.
• The goal of sperm washing is to separate healthy sperm from toxic seminal fluid.
• Keep in mind that just because Clomid worked for your best friend doesn’t mean it will work on you. The same goes for other fertility treatments.