
Human beings share an innate desire to reproduce. Obviously, survival of our species depends on it. Unfortunately for many, pregnancy is no longer a certainty. Nearly 15 percent of reproductive couples (men with female partners age 20 to 45) suffer from infertility.

![]() Improving Your Odds
Improving Your Odds
Fertility treatments do not make impossible pregnancies possible; they make improbable pregnancies probable.
If you’re a couple in your late 30s trying to get pregnant, Mother Nature isn’t cutting you any slack. Your monthly chance of conceiving, sad as it sounds, may be less than 10 percent (see chapter 4). Although this sounds discouraging, give yourself (and your partner) credit for seeking help.
With recent advances in assisted reproductive technology, your monthly conception rate can increase considerably. No matter what prompted you to pick up this book, within these covers you’ll find practical solutions to eliminate the “in” in infertility. Depending on your health and that of your partner, your monthly odds can increase to anywhere from 25 to 80 percent. Is this enough to make a difference? Once you gaze into your newborn’s eyes, it will make all the difference in the world.
TIPS TO INCREASE YOUR CHANCES OF GETTING PREGNANT
1. If you’re not satisfied with your fertility clinic, consider one with a higher success rate.
2. If you’re happy with your current clinic, discuss changing protocols.
3. Consider transferring more embryos.
4. Ask if genetic screening like PGS or PGD is warranted in your situation.
5. Try complementary therapies like acupuncture, yoga, or others in chapter 5.
6. Get fit, exercise, and confirm your BMI is in the right range for your height.
7. Find extracurricular activities to reduce your stress.
8. Eat healthy, well-balanced meals.
9. Avoid environmental toxins and those found in cleaning supplies.
10. Get plenty of sleep.
For many people, trying to get pregnant can be “trying.” By now you’ve attempted all the tricks you know to get pregnant, and you’ve heard all the suggestions from well-meaning friends with children, but still nothing. Friends keep asking if you’ve had any luck, but the answer remains the same. A look of concern washes over their faces after you reply with a weak “no,” and without warning your head throbs with the question you feel they’re holding back: Are you infertile?
Infertility is a medical condition, a misunderstood condition that touches both genders equally. A condition so common that it affects over 100 million people worldwide. In this country infertility is still a concern. While over seven million Americans have been diagnosed as infertile, experts believe the actual number is easily triple that.
Since our culture leans toward delaying childbearing in order to build a career first, fertility problems such as blocked or damaged fallopian tubes, ovulation failure, fibroids, endometriosis, poor sperm production, and damage from sexually transmitted diseases are often revealed only when a couple in their 30s or early 40s finds out they can’t conceive.
Regardless of your age, if you’ve tried to get pregnant for a year without any luck, you need a fertility evaluation. Eighty-five percent of couples who achieve pregnancy without medical intervention succeed within this time frame. Earlier treatment is advisable if you have one or more risk factors, such as the following:
• You’re over 35 years old.
• You have a history of irregular or absent menstrual periods.
• You know or suspect you have uterine/tubal disease, endometriosis, fibroids, or hormonal imbalance like polycystic ovarian syndrome (PCOS).
• Your partner is known to be subfertile.
• Your doctor has previously diagnosed you with an STD.
Many couples try on their own, only to find out that if had they sought help earlier, they may have saved themselves years of heartache.
I tried to get pregnant as a newlywed at age 21. But nothing happened. Years went by, and we didn’t know anything was wrong. Once we saw a fertility specialist, we got some answers. Besides thin uterine lining, one of my fallopian tubes was blocked, and Cesar had a low sperm count. Knowing this earlier would have saved us years of heartache.
—Christine, 32, human resources specialist
We kept trying to do it ourselves, but months went by with no pregnancy. Before we knew it years had lapsed, and we were still childless. Once we had our workup, we found out why. I had a mild case of endometriosis and John had a low sperm count. Now we tell all our friends to see a specialist early on.
—Devon, 35, court reporter
How do you know if you’re infertile? If you have been having unprotected intercourse for one year without conception, you’re officially infertile. As you’ll find later in this book, it’s often beneficial to begin your fertility evaluation (workup) and even your treatment well before meeting this definition. The fact remains that every individual is unique. You’ll do yourself and your partner a favor if you rely less on rigid definitions and more on your own situation. Couples rarely regret getting treatment early but often regret delaying treatment.
Most physicians who specialize in reproductive medicine recommend that couples schedule a fertility evaluation as soon as they realize they have a problem. Getting help early is especially important if you have any of the following:
• history of sexually transmitted disease
• ovarian cysts
• painful periods
• irregular cycles
• ectopic pregnancies
• miscarriages
Or if your partner has any of the following:
• low sperm count
• sluggish sperm
• abnormally shaped sperm.
So what exactly does this mean? Infertility is a disease of the reproductive system that impairs one of the body’s most basic functions: conceiving babies. Conception is a complicated process that relies on many factors. Like instruments in an orchestra, your reproductive system requires that all processes work in sync to achieve perfect harmony.
Delayed childbearing is the main reason for the recent rise in infertility. As you age, you experience a clear decline in fertility. Numerous studies support this decline. The classic study, published in 1957 by Christopher Tietze, researched a religious sect called the Hutterites. The Hutterites raise children communally and encourage their sons and daughters to have as many children as possible. They forbid contraception, follow strict monogamy, and have virtually no sexually transmitted disease. Tietze studied them over time and noted their incidences of infertility for various age groups. In their commune only 7 percent of women under age 30 suffered from infertility. This number rose to 11 percent at age 35, 33 percent at age 40, and 87 percent at age 45. Tietze selected Hutterites for study, of course, because their society provided ideal circumstances for promoting fertility.
How does this study relate to you? It provides baseline data on infertility and aging that is still applicable today. In fact, incidence of infertility at a given age in the general population nearly always exceeds the numbers mentioned above. So yes, in the real world more than one-third of women are infertile at 40 years of age.
Yet age has little effect on male infertility. Age-related infertility in men usually stems from diminished sexual function and increased incidence of systemic diseases like coronary disease. Documented male fertility has occurred well beyond the age of 80. These days it’s not uncommon to hear of men over 60 becoming fathers.
Infertility is difficult to grasp because it’s a disease that you can’t see or feel. Couples often wonder if they’re infertile or if they have timed their lovemaking incorrectly. To recognize infertility, you need to be aware of subtle (or sometimes obvious) signals that your body sends you. Most of the time, detection requires fertility tests.
One of the most important indicators of potential fertility is regular menstrual cycles. If you’re having irregular menstrual cycles, chances are you’re not releasing an egg every month (ovulating) or you’re ovulating very infrequently. Ovulation is necessary for pregnancy to occur. Without ovulation you’ll have no egg to fertilize. If your cycle is regular, you can expect to menstruate at intervals ranging from 21 to 35 days. And if you’re ovulatory, you’ll have 26 to 32 days between onset of consecutive menstrual cycles. Increased vaginal mucous production suggests ovulation. You can expect to see this clear mucous around the middle of your cycle (see page 8).
While I sustained an injury from a car accident that doctors said could cause fertility issues, the main reason I decided to seek fertility treatment was due to the fact that my spouse and I are the same gender. I came from an extremely fertile family background. My grandmother had twenty-two pregnancies, and my mom had five pregnancies. I felt certain that getting pregnant wouldn’t be an issue, but we needed a little help with the actual process of conceiving. We initially met with Dr. Potter to discuss our options for sperm and to find out what he advised. Initially we wanted to use a “known” donor and started that process, but after having issues with scheduling, my wife and I both agreed that it was most likely better to go with an anonymous “Open ID” donor. That was pretty much the hardest part about the conceiving process. From there we were met step by step with the most amazing staff, and any question I had was quickly and beautifully answered.
It made getting pregnant fun, informative, and extremely personal, which is something we were afraid we’d lose in the process.
—Tabby, 33, software engineer
WHAT HAS TO HAPPEN FOR FERTILIZATION TO OCCUR?
In order to understand infertility, you must first understand what happens when all your conditions are right. First, we’ll discuss what occurs in your reproductive system.
Figure 1.1. Female reproductive system
Source: EMD Serono, Inc.
Your reproductive tract consists of a vagina (birth canal), a uterus (womb), two fallopian tubes, and two ovaries. Ovaries contain small cyst-like structures called follicles. Each follicle houses a single egg. Around the time menstruation begins (in a normal cycle) your hypothalamus (a region of your brain) sends a signal to your pituitary gland. This signal instructs your pituitary gland to secrete a substance called follicle-stimulating hormone (FSH). Once secreted, FSH travels through the bloodstream, and when it reaches your ovaries—just as the name implies—it stimulates your follicles.

![]() Problems with FSH Production
Problems with FSH Production
Stress and mental and physical illness interfere with signals between the hypothalamus and your pituitary gland. This interference can decrease your fertility.
After stimulation a group of follicles grows on each of your ovaries. Usually only one follicle develops beyond the early stages. This follicle is termed the dominant follicle. The dominant follicle grows larger and larger with FSH stimulation. Besides containing your egg, follicles produce the female hormone estrogen (estradiol).
Estrogen serves two primary purposes. First, it causes the lining of your uterine (endometrial) cavity to grow thicker. This is important because ultimately your fertilized egg (embryo) will implant in this lining. Second, estrogen serves as a signal between the follicle and the brain. As your follicle grows larger and matures, estrogen levels rise. When levels of estrogen reach a certain threshold, your brain signals your pituitary gland to release a second hormone called luteinizing hormone (LH). This process is your LH surge.
All over-the-counter ovulation predictor kits that analyze urine test for the LH surge. LH is another protein that travels through your bloodstream to your follicles. It causes your egg cell to break free from your follicle’s wall and float freely in follicular fluid. LH then sets off a chain of events called ovulation, which causes your follicle to rupture and release your egg.

![]() Where Does Ovulation Occur?
Where Does Ovulation Occur?
Ovulation occurs in your cul-de-sac (pouch of Douglas). This small sac-like structure of the abdominal cavity occupies the space between your rectum and uterus.

Table 1.1. Key reproductive glands and organs
The fallopian tube then grasps your egg with small finger-like projections called fimbria. Cilia, small hair-like structures on the fimbria and in the tube, pulse and sweep in a rhythmic motion, moving your egg (ova) into the tube.

Figure 1.2. A frozen natural egg

![]() Why Can’t Your Partner’s Sperm Pass Your Cervix?
Why Can’t Your Partner’s Sperm Pass Your Cervix?
Men mass-produce sperm at the rate of millions per day with very poor quality control. In fact, most semen samples have only 14 to 20 percent normal sperm under strict parameters. A normal sperm has an appropriate-size head, normal tail, and normal movement (motility).
The next step involves fertilization. It occurs toward the end of the fallopian tube (distal fallopian tube) near your ovary. First, your partner’s sperm has to enter your vagina. His sperm is in the ejaculatory fluid released during his orgasm. Typical healthy ejaculations will contain about 80 to 100 million moving sperm. Of this number, only a small fraction (less than 1 percent) arrives at your distal fallopian tube.
Another important role of estrogen is to cause glands that line your cervical canal to produce large amounts of clear, stretchy mucous. If you are fertile, your mucous looks similar to raw egg whites. This mucous lasts for several days each cycle, and its consistency permits your partner’s sperm to penetrate it and pass through the cervix. Keep in mind that your partner’s sperm can only penetrate your cervical mucous midcycle. Even in this ideal mucous, most of your partner’s sperm will never pass your cervix. The few that do will propel themselves through your uterine cavity and into your fallopian tubes. Uterine contractions that occur during orgasm may accelerate this.
Once your partner’s sperm reach your fallopian tubes, they undergo a process called capitation, in which they become hyperactivated. This is where your partner’s sperm pursue your egg. Once one sperm penetrates your egg, your egg becomes impermeable to other sperm. The newly fertilized egg is now an embryo (zygote). It begins as a single cell and contains combined genetic material from both sperm and egg. The zygote then divides progressively into a multicell embryo. While the embryo is dividing, cilia continue to sweep it toward the uterus. When the embryo contains about 12 to 16 cells, it’s a morula.

Figure 1.3. Frozen morula
During morula stage (about three to four days after ovulation) the developing embryo descends through the tube and into your uterus. After five to seven days the embryo contains hundreds of cells and forms a cavity within its center. At this stage the embryo is a blastocyst. The blastocyst implants in your uterine lining so that it develops a blood supply (placenta) that allows it to grow into a fetus and then a baby.
Figure 1.4. Blastocyst

![]() Human Reproduction Is Amazing
Human Reproduction Is Amazing
All these reproductive processes occur nine months before your baby takes his (or her) first breath. And even more astonishing, you don’t even have to think about them to make them happen.
As you can imagine, sperm and egg are unique cells. They contain only 23 chromosomes each whereas all other cells in the body contain 46. This is so that when your egg and your partner’s sperm unite, they’ll reconstitute the normal chromosomal count of 46.
These cells are also distinctive in another way. Egg cells are the largest cell in the human body. Once a follicle containing your egg is stimulated, the egg matures to its final diameter of about 120 to 150 microns. About 15 to 16 eggs would fit on the head of a straight pin. Sperm cells (spermatozoon) are the smallest cells in the human body, at about 2.5 to 3.5 microns with tail lengths of 5 to 7 microns. About 600 to 800 sperm cells would fit on the head of a straight pin. Although your eggs are about 50 times larger than your partner’s sperm, both cells are highly specialized to accomplish specific tasks.
You are born with all the eggs you’ll ever have. Initially, your egg supply was around 5 million. This occurred when you were still developing at about six months gestation inside your mother’s womb. From this point onward, you experienced a relentless and irreversible decline in eggs. At birth, your egg supply had already dwindled to around 2 million. And once you began menstruating at age 11 or so, only 400,000 to 600,000 eggs remained. Throughout your lifetime you’ll ovulate between 400 to 450 eggs. Although this number may sound abundant, it’s not. This is because 99.9 percent of your eggs will undergo atresia (die).
To understand why most of your eggs die you need to know how this process works. Before you ovulate, a group of eggs develop independently of FSH. These eggs mature only when your body signals them with FSH. As they mature, their follicles (the structures that house them) release estrogen signaling your body to slow FSH production. As FSH declines, some eggs stop maturing. Ultimately, only one egg matures enough to ovulate. To picture this, think of your eggs as troops marching toward the edge of a cliff. As your body fails to warn the majority of impending danger, it may warn some. The troops that your body fails to warn have no other choice but to march over the edge. But the troops that receive the FSH signal from your body begin maturing.
Discovering a Hidden Time Clock
I was in no hurry to have children. I was enjoying traveling, working, and spending time with my family. I had no idea there was a time issue with my eggs. As funny as it sounds now, I thought I could have children at any time.
—Claudia, 34, teacher
Ovarian reserve is the number of eggs that you have at any given time. You’ll continue to lose eggs whether you use birth control, carry a child to term, or nurse a baby.
Keep in mind that your eggs are one of the longest-lived cells in your body, which may account for the increased number of genetic abnormalities found in older mothers (see chapter 13). By the time you reach menopause (on average around 51) your egg supply is exhausted.
Prior to losing your final egg, there is a long period (five to ten years) during which you might experience marginal fertility. During this period you may experience increased variability in your menstrual cycle length and have occasional missed cycles. Reduction in fertility is due to diminished quality and competence of your remaining eggs. This decreased competency manifests itself in reduced fertility as you age and increases your likelihood of miscarriage and chromosomal abnormalities like Down syndrome (see chapter 13).
Giving up control is one of the hardest challenges couples face. But now you can rest easier knowing that what happens with your reproductive system is out of your hands. You wouldn’t expect an orchestra that never played together to perform well in Carnegie Hall; the same concept applies to your reproductive system. It’s nearly impossible to have a baby if any one reproductive process is disharmonious with the rest—the result is utter chaos. And it doesn’t stop there. Once everything is in harmony, you still face challenges. Your embryo must be healthy, and your hormonal environment must facilitate its development. By understanding how your reproductive system works, one can easily understand how having a baby is a miracle. Getting help from a fertility specialist makes it even more of a miracle.
All factors previously mentioned may ultimately determine whether you’ll achieve full-term pregnancy. The following are critical factors for successful conception:
• eggs and sperm that are healthy
• fallopian tubes that are open and undamaged
• sperm’s determination to reach egg
• sperm’s tenacity to fertilize egg
• embryo’s ability to divide and implant into uterus
• continued development of the implanted embryo
Now you can toss all those well-meaning but frustrating books on “how to conceive naturally” and tackle your real problem: boosting your fertility. These tips will help you get started (see chapter 5 for more information on maximizing your fertility and living a fertile lifestyle):
• Reduce or eliminate alcohol use.
• Eliminate tobacco use (it can destroy your eggs).
• Reduce caffeine intake.
• Stay physically fit.
• Eat a well-balanced diet.
• Get plenty of rest.
• Have well-timed, frequent intercourse.
There are also plenty of activities that you or your partner may engage in frequently, but they can be deterrents when it comes to getting pregnant.
Activities to Avoid
Sleeping with tight underwear. Consider this the ideal time to gift your spouse boxers at bedtime or suggest he sleep in the buff.
Excessive exercise. Now is not the time for you and your partner to participate in a triathlon or the Ironman. If this is your hobby or ambition, put it on hold for the next three to six months while you’re trying to get pregnant. Easing up on exercise also applies to serious athletes, cyclists, runners, and so on.
Horseback riding and dirt bikes. Heat, pressure, and repeated trauma are not kind to sperm production, so it’s best to put these activities on hold for three to six months while trying to get pregnant.
Jacuzzi. Soaking in a hot tub raises body temperature and can affect your partner’s ability to create healthy sperm. Avoid jacuzzis three months prior to trying to get pregnant and also during pregnancy, as it also raises your body temperature and can cause birth defects or miscarriage.
For years both men and women have worried about infertility, blindly assuming that it’s a female problem. Myths like this often create a great deal of anxiety in women who, month after month, greet another unwelcome menstrual period.
If you’re a woman and you feel inadequate over what you perceive as your fertility problem, know that it takes two people to have a baby. Recent statistics prove that infertility is not overwhelmingly a female problem. Approximately 40 percent of infertility has a primary male factor, and 40 percent is due to a female factor. Of the remaining cases, 10 percent is due to a combined problem in both partners, and 10 percent is unexplained.
Work activities such as standing for long periods or chronic exposure to dust or loud noises may decrease fertility. Studies suggest that infertility may be higher in women who frequently switch from working day to night shifts. Job-related exposure to high temperatures, chemicals, radiation, pesticides, and other toxic substances can also increase infertility in women.
Although some risk factors like sexually transmitted diseases, multiple sex partners, drug use, certain medications, extreme fluctuations in weight, and occupational and environmental toxins are similar for both sexes, others fail to cross genders. For example, exposure in utero to DES (diethylstilbestrol, taken to prevent miscarriage in the early 1970s) has reduced fertility in women, but it does not present a significant risk for men. If any of these risk factors apply to you, you’ll need to inform your doctor prior to discussing your fertility options (see chapter 5).
WHAT KIND OF DOCTOR SHOULD YOU SEE?
Scheduling your initial appointment can bring an onslaught of feelings and emotions. Fear, ambivalence, sadness, joy, and anxiety are some of the most common. Most physicians understand the emotional and psychological aspects associated with infertility and can recommend where you can go to receive guidance or counseling.
Whereas you may begin addressing infertility with your gynecologist or family physician, patients who seek advice from physicians who specialize in reproductive medicine may get answers faster. How can you find one? The best way to do this is to interview potential candidates. Like finding any service, it’s always best if you know someone who has undergone fertility treatments. If any of your friends, family, colleagues, or neighbors have experienced successful treatments, ask them first. Otherwise, begin your search using the list provided in the appendix.
What characteristics should you look for when selecting a specialist? First, you’ll want to confirm that the specialist you find has your best interest at heart: pinpointing the cause of your infertility and correcting it. How can you tell? The specialist you want has incredible listening skills. While interviewing her, be sure to check if she’s making eye contact with you. If she seems disorganized, overworked, or uninterested, then you’ll want to interview other doctors. You’ll also want to look elsewhere if she’s got her head stuck in another patient’s file. Before leaving her office you’ll want to take note of her responses. Is she compassionate? Does she have a good success rate? Is she someone you’d recommend to family and friends?
Next, you’ll want a specialist who can provide accurate information and dispel any misinformation about fertility that you or your partner may have. Finding a specialist who can offer emotional support, or direct you to a group who can, is also beneficial.
Finally, you’ll want your specialist to give you her professional opinion, even if that means it’s time to move on (keep in mind that this can occur only when you’re ready). It’s also important that she shares the same philosophy as you and adheres to similar ethics. Whereas these are only a few suggestions to narrow your choices, you’ll want to make sure the specialist you choose meets your criteria.
Why It’s Important to Find the Right Doctor
We did months of fertility drugs through our OB/GYN. He never told us that we needed to see a fertility specialist. We wasted six months with him. Then we saw a reproductive endocrinologist.
—Mark, 40, professor
There are many types of health care professionals who can assist you on your fertility journey. Here are the main players.
Reproductive Endocrinologist
Are you searching for a specialist who is trained to tackle every imaginable aspect of your infertility (and your partner’s), from preconception to pregnancy and beyond? Then you’re looking for a reproductive endocrinologist (RE).
An RE has completed a four-year residency in general obstetrics and gynecology and an additional two- to three-year fellowship in reproductive endocrinology and infertility. He has passed written and oral examinations in both obstetrics and gynecology as well as reproductive endocrinology/infertility, and he should hold certifications in both specialties from the American Board of Obstetrics and Gynecology.
An RE limits his practice strictly to treatment of infertile couples and women with reproductive abnormalities (glandular and structural). Once you achieve pregnancy, he’ll follow you for the first eight to ten weeks of pregnancy, but he does not deliver your baby. You’ll need a general OB/GYN to follow you the remainder of your pregnancy. REs routinely receive referrals from obstetricians and can easily refer you to one in your area.
Urologist
A urologist is a surgeon who specializes in treating both the male and female urinary tract. They’re the ultimate experts in issues affecting men’s reproductive health. A urologist completes a five- to six-year residency after medical school. They take board examinations in urology and should be fellows of the American College of Surgeons. The initials FACS after their name indicate this distinction.
Only a few urologists hold a subspecialty in male infertility. This means they completed a one- to two-year fellowship in male infertility after residency. These subspecialists are usually limited to large metropolitan areas, and there are not many of them, as only a few complete training each year in the United States.
Obstetrician/Gynecologist
An obstetrician/gynecologist (OB/GYN) is a female health specialist who is able to diagnose and treat disorders of the female reproductive system and pregnancy. OB/GYNs complete a four-year residency after medical school and hold board certifications in obstetrics and gynecology. Being a fellow of the American College of Obstetricians and Gynecologist is an indication of board certification. The initials FACOG after their name indicate this credential.
OB/GYNs have received training in basic workup and treatment of infertility. They also received training in laparoscopy and surgery of the female reproductive tract. OB/GYNs can perform surgery to remove uterine fibroids and polyps as well as endometriosis. They have not been trained to perform in vitro fertilization or other advanced fertility treatments. The OB/GYN should be the first stop for most patients who think that they’re infertile. That’s where you’ll get a basic workup and treatment, including medications that can boost egg production, if needed.
Family Practitioner
A family practitioner (FP) is a general physician trained to take care of a variety of common ailments in adults and children. FPs have three years of training after medical school. Those that specialize in specific areas of medicine should hold a certification from the American Board of Family Practice. They’re the “gatekeepers” because many health maintenance organizations (HMOs) require you to see your FP before accessing specialized care. Most FPs will refer you to an OB/GYN or an RE. They may order tests at the time of your referral, like a semen analysis (for your partner) or a hysterosalpingogram (for you) to speed up the process. You’ll want a referral because your FP probably knows specialists in your area and can make a qualified referral. If your FP doesn’t know an OB/GYN or RE, you can contact one out of network.
Table 1.2. Doctors who treat infertility
WHEN SHOULD YOU SEEK A SUBSPECIALIST?
If you’re having any of the fertility problems mentioned in the list that follows, chances are you need to see a reproductive endocrinologist (RE):
• inability to achieve pregnancy after trying for one year
• female age greater than 35
• tubal blockage
• low ovarian reserve
• Clomid failure
• unexplained infertility
• male-factor infertility
If you’re a male and you’re experiencing any of the infertility issues in the following list, you need to see a urologist who has a subspecialty in male infertility:
• low or absent sperm count
• abnormal male physical findings or symptoms
It doesn’t hurt to consult with an RE to bypass your infertility with methods like IVF and ISCI (see chapter 8), but only a urologist can treat your partner’s underlying conditions.
COMMUNICATING WITH YOUR PRACTITIONER
Chances are you assume it takes two to make a baby, and this is true, except when undergoing fertility treatments. Once you and your partner decide to seek an expert, there is a third and equally critical component to your planned pregnancy: your fertility specialist. The specialist you select will play many essential roles during your treatment. First, he’ll serve as an investigator, uncovering all possible causes of your infertility. It’s critical that you’re confident about the capabilities of whomever you select. This expert must not only inspire confidence but also needs to have one ultimate goal in mind: seeking the truth.
You’re Your Best Advocate
Don’t be afraid to ask questions, but trust your body, ladies. You know your body better than anyone else. Trust everything about it. Next to that, trust the doctor and the staff, because they are there to make your dream a reality. If you have a bad experience with a staff member, just be up-front and ask for it to be improved, but I can’t imagine that happening at the clinic we went to. Think positively—it really helps! And finally, your life will start to creep by slowly in two-week intervals. Try to keep yourself busy during each two-week interval to avoid mental looping processes. Seek help from a therapist if it helps. Also, I would highly recommend couples therapy to anyone trying.
—Tabby, 33, software engineer

![]() Know Your Biological Clock
Know Your Biological Clock
Women over age 45 trying to conceive naturally have less than a 1 percent monthly chance of getting pregnant.
By this point you may have tried all kinds of natural remedies to get pregnant, but nothing seems to work. Whether you began a fitness program with a balanced diet or quit smoking, you still greet each month with some level of dissatisfaction. This is why it’s even more important that you find a fertility specialist who is board certified and interested in finding the primary (and, in some cases, secondary) cause(s) of your infertility.
Once your specialist has eliminated what’s not causing your infertility, the real work begins. This new triangular relationship, if a pregnancy occurs, will last through your first trimester (8 to 12 weeks) and possibly beyond. During this time you’ll have weekly or biweekly appointments with your specialist and a chance to form a significant bond. In many cases patients see their specialist so much that they begin to feel like he’s an extended family member. This is another reason it’s crucial that you and your partner both feel comfortable with your doctor. It’s no time for personality conflicts.
Once you’ve decided on the type of physician you want, your next hurdle is choosing the type of practice that best suits your lifestyle. Depending on what size city you live in, whether it’s a bustling metropolis or a quaint town near a mid- to large-size urban area, you’ll have several choices. If finding a practice with a high success rate is important to you, check out the yearly report issued by the Centers for Disease Control at www.cdc.gov/reproductivehealth. Here’s what you need to know to make an informed decision on what type of practice you want.
Solo Medical Practice
This type of practice houses a single doctor, who works independently and typically uses another doctor to act in her absence when on vacation or making hospital rounds. Whereas a reproductive endocrinologist, urologist, or family practitioner might work in a solo practice in a small- to mid-size town, this is rarely the case in larger metropolitan areas, especially with the advent of managed health care.
The major disadvantage with this type of practice is that there is only one doctor. If a tragedy occurs and the doctor is away indefinitely or closes her doors permanently, you’re out of luck. If this is a concern of yours, you may want to ask the physician what you can expect if she is away for an extended period. Chances are she’ll arrange for another doctor to handle your needs. But if the answer fails to reassure you, consider keeping a second choice in mind in case you run into any snags. Although this may never occur, it’s wise to have a backup plan in case of an emergency or if you decide you and your doctor are from two different planets.
The chief advantage to having a solo practitioner is that you see the same doctor each time. This is a real plus for couples who prefer to see a familiar face during each visit. Keep in mind that not everyone becomes pregnant with their first treatment, so visits to your practitioner could continue anywhere from six months to a year or more. This is when knowing your personality and, in some cases, comfort zone comes in handy. For some couples a solo practitioner will completely suit your needs, whereas others will opt for a practitioner or specialist in a partnership or group practice.
Partnership or Group Medical Practice
If you’re seeing a specialist in a partnership or group medical practice, chances are you’ll see the same practitioner each time even though there are multiple physicians within the practice. When you’re shopping for practices, you may want to inquire whether that practitioner will see you each visit. Some practices rotate physicians, particularly health maintenance organizations (HMOs), in which each time you may see a different doctor.
More often than not, seeing a familiar face each visit will give you additional reassurance. Only you can decide whether seeing a different doctor each time bothers you. Obviously the advantage of seeing several doctors is that you may benefit from each physician’s expertise and training. The disadvantage is that you may not bond with certain doctors in the group.
Couples worried about infertility may research up-to-date information via the Internet. About 294 million Americans already do. But when you’re surfing for facts, making appointments, or purchasing medical products online, how do you know which sources to trust and which to be wary of?
Unfortunately this is one drawback of the Internet. Along with the volume of helpful information lies a vat of misinformation. Lack of online content regulation forces consumers to become e-savvy.
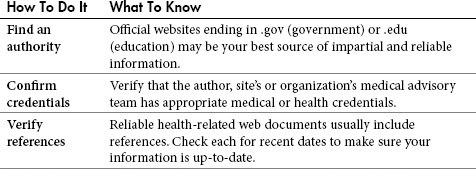
Table 1.3. Evaluating online sources
If you’re interested in learning more about your infertility or want a second opinion, here are tips for finding the most reliable, up-to-date information.
After you’ve decided on the type of practitioner and practice you desire, how can you find the right match? This is a tough one, because the experience you have with your physician can either make your journey worthwhile or turn it into one that’s forgettable.
WHAT QUESTIONS SHOULD YOU ASK?
Now that you’ve narrowed your choices of possible fertility centers, what questions should you ask during your initial consultation? Although there are no right or wrong questions, it’s important that you feel comfortable asking anything that comes to mind. Because infertility can take you and your partner on an emotional, psychological, spiritual, and financial roller-coaster ride that can last anywhere from three months to a year or longer, knowing what you can expect is essential.
• When did your program open its doors?
• How many babies are born yearly through your program’s fertility and IVF procedures?
• How many treatment cycles have you initiated? What are your success rates?
• How many egg retrieval procedures has your clinic performed?
• How many embryo transfer procedures has your clinic performed?
• How many pregnancies have resulted from your clinic’s efforts?
• How many pregnancies resulting from your clinic’s efforts were twins or multiple births?
• How many selective reductions occurred as a result of your clinic’s efforts?
• Does your clinic transfer embryos after three or five days? What is the benefit to either?
• What happens if the first cycle doesn’t work?
• What happens to our leftover embryos (should we have any)?
• What are our options if our own eggs and sperm fail to achieve a viable pregnancy?
• Couples rarely regret getting treatment early but often regret delaying treatment.
• Talk with all the people you trust who have undergone fertility treatments, and ask for physician recommendations. Family, friends, colleagues, and neighbors are great places to start.
• If you don’t know any couples who have had fertility treatments, check the resources listed in the appendix or try the Internet to locate your prime candidates for physicians, medical centers, and support groups.
• Eliminate tobacco use and reduce alcohol, caffeine, and other risk factors to help you conceive.
• Be proactive about your fertility. Help uncover obstacles you and your partner face, and find out what your options are.
• Make an appointment now if you have tried to get pregnant for a year, have preexisting conditions, or are over 35.
• Search for the ideal physician and practice for you, your lifestyle, and your personality. Keep one as a backup, as it never hurts to have a plan B.
• Communicate well with your fertility specialist—it will make your journey more meaningful.
• Take charge! Do not wait for a miracle—create your own.