TABLE 52.1 AWS Precipitants and Exacerbating Factors

BACKGROUND
Chronic alcoholism and alcohol withdrawal syndrome (AWS) are serious disorders that affect millions of people worldwide. AWS is frequently encountered in hospitalized patients and contributes significantly to patient morbidity and mortality. AWS also imposes a considerable financial burden on hospitals, as these patient visits are often prolonged and not fully reimbursed. In spite of the high volume of medical admissions for moderate to severe AWS, relatively little evidence-based literature addresses its management. This is particularly true in the intensive care unit (ICU), where management varies significantly among institutions.
PATHOPHYSIOLOGY
When the central nervous system is exposed to long-term ethanol use, compensatory changes occur to counter ethanol's depressant effects on the inhibitory centers of the cerebral cortex. The net effect of these compensatory changes is to restore cerebral homeostasis despite the near-constant presence of ethanol. Tolerance to ethanol is an example of such a compensatory changes change. Alcohol potentiates γ-aminobutyric acid (GABAA) signaling by increasing the GABAA chloride channel opening. With chronic ethanol use, the persistently stimulated inhibitory GABAA receptors become down-regulated and less sensitive to ethanol.1–5 Ethanol also inhibits glutamate, the excitatory neurotransmitter that binds to and activates the excitatory N-methyl- D-aspartate (NMDA) receptor. In chronic ethanol use, NMDA receptor systems are up-regulated and become more sensitive to glutamate.6–9 Ethanol use is also associated with increased brain dopamine; this is thought to be a contributing factor to some of its acutely pleasurable effects and addictive qualities.9–11
When ethanol exposure is abruptly terminated, there is a loss of homeostasis, and these neurotransmitter systems become imbalanced. This absence of ethanol's depressant effects on the already desensitized, down-regulated GABA system combined with the enhanced NMDA excitatory system and dysregulation of the dopaminergic system is primarily responsible for the development of unopposed CNS excitation and the hyperexcited state associated with AWS.12–14
Chronic ethanol use is also thought to desensitize α2 receptors. The increased dopamine seen with ethanol use is metabolized to norepinephrine (NE) by dopamine-β-hydroxylase, resulting in an increase in available NE. Chronically impaired α2 receptor activity in the face of increased NE results in adrenergic receptor up-regulation and adrenergic hypersensitivity. These effects may explain the increased sympathetic nervous system activity observed in alcohol withdrawal.15–17
HISTORY AND PHYSICAL EXAM
Initial steps in the successful treatment of adult patients at risk of or actively experiencing AWS include early recognition of AWS, appropriate patient disposition, early initiation of symptom-triggered therapy (STT),18–25 and/or front-loading with benzodiazepines.26 Early recognition of AWS requires detailed history taking and an awareness of the stages of withdrawal.
Clinical manifestations of alcohol withdrawal occur along a spectrum and often coexist with other pathophysiologic states. Psychological symptoms range from mild anxiety, insomnia, craving, irritability, and labile emotions to significant agitation, trouble thinking clearly, and altered mental status (AMS) or frank delirium. Physical symptoms include headache, diaphoresis, nausea and vomiting, tachycardia, hypertension, tremor, tongue fasciculations, hyperthermia, and seizures.
The typical withdrawal timeline after a patient's last drink is as follows:
Although AWS tends to occur in a temporal progression, there is no fixed sequence. Completion of alcohol withdrawal typically lasts 4 to 7 days; however, significant withdrawal can last up to 2 weeks.27 Historically, approximately 5% of all patients with AWS will progress to DTs28; this number jumps to over 30% for patients who experience withdrawal seizures.29 In modern times, advances in medical therapy and ICU care have decreased the mortality from AWS with DT from 37% to 5%.30–33
DIFFERENTIAL DIAGNOSIS
It is important to consider the complete clinical picture when caring for a patient with AWS. Not only does AWS frequently exist as a result of or in parallel with another pathophysiologic process, but its signs and symptoms can also be masked or complicated by other processes (Table 52.1). Occasionally, symptoms such as isolated tachycardia are wrongly attributed to AWS in the ethanol-dependent patient. Similarly, confounding AWS with other diagnoses (encephalopathy, psychosis, delirium from another cause, CNS injury, infection) can lead to wrong diagnoses, inappropriate sedation, and withheld treatments.34
TABLE 52.1 AWS Precipitants and Exacerbating Factors

DIAGNOSTIC EVALUATION
A history of physiologic tolerance to ethanol from years of heavy use, coupled with recent cessation or reduction in ethanol intake, places patients at risk for developing AWS, severe AWS, and/or DT. Risk factors for the development of severe AWS and/or DT include duration of ethanol abuse; quantity of ethanol consumed; history of repeated episodes of AWS, DTs, or seizures; withdrawal symptoms with a positive BAL; mild intoxication with BAL >300 to 400 mg/dL; and comorbid infections.27,35–38 Hypokalemia, thrombocytopenia, and presence of structural brain lesions are additional independent predictors of more severe withdrawal.36 Certain populations may also be predisposed to severe AWS, and there may be a genetic or racial component (Whites appear more at risk than Blacks for severe AWS).33,39 When admitted to the hospital, high-risk patients should undergo careful risk assessment, followed by management using an established clinical care pathway. Unrecognized or undertreated withdrawal may progress to more severe withdrawal and exacerbate future episodes of AWS, underscoring the importance of early recognition and treatment.
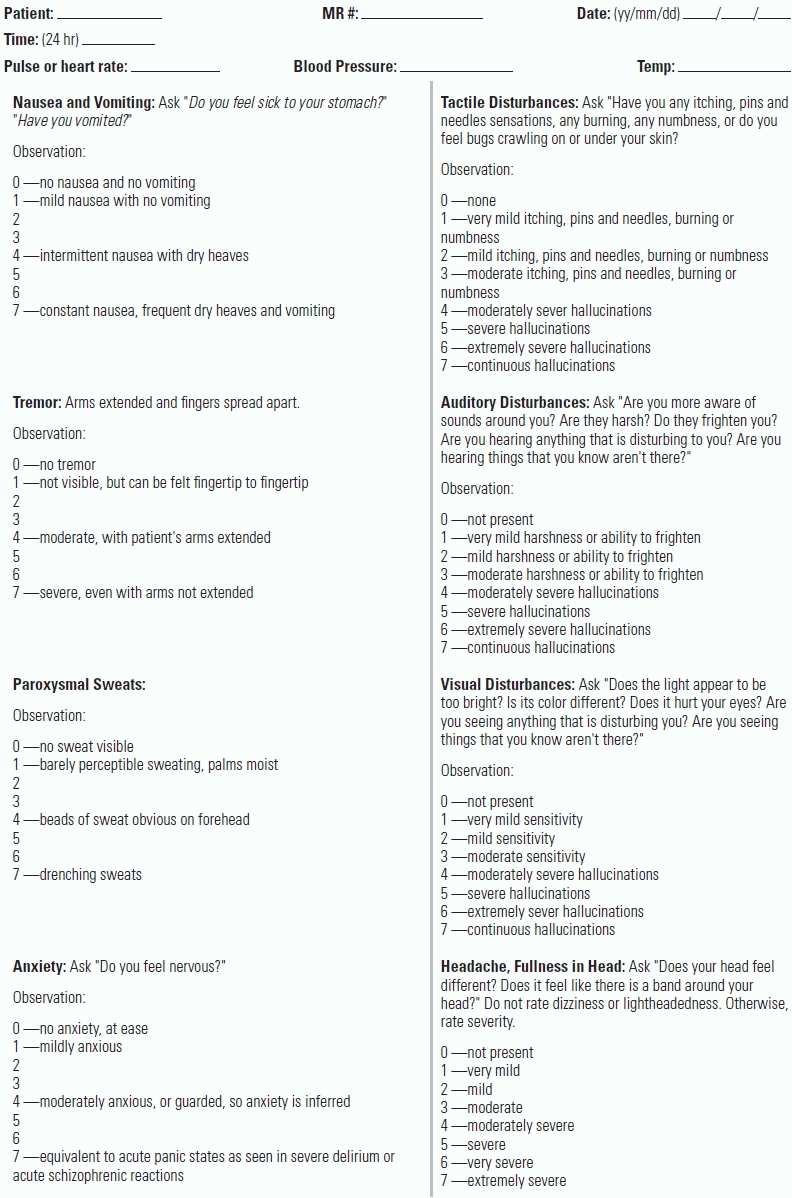
The most commonly used and highly validated scoring systems for the assessment and STT of AWS are the Clinical Institute Withdrawal Assessment—Alcohol (CIWA-Ar, Ar: Alcohol-revised, and, where available, a new version CIWA-Ad) (Table 52.2).22,24,26,27,34,40–44 Care must be taken to apply the CIWA score correctly to at-risk patients to avoid erroneous attribution of symptoms to patients not in AWS.34 Some centers use abridged, institution-specific assessment tools; these may be convenient at a local hospital level but have not been extensively validated.
TABLE 52.2 Clinical Institute Withdrawal Assessment - Alcohol (CIWA-Ar)

The strength of the CIWA tools is the ability to detect AWS at an early stage, when treatment will be maximally beneficial. The CIWA-Ar/Ad score becomes more difficult to evaluate in patients with very high scores, DTs, or benzodiazepine-resistant AWS. In these cases, the goal of STT is to maintain light sedation, and an agitation/sedation score such as the Richmond Agitation Sedation Score (RASS) may be a more useful assessment tool (Table 52.3).
TABLE 52.3 Richmond Agitation Sedation Scale (RASS)

Initial patient classification into mild, moderate, or severe AWD should be based on CIWA-Ar score and clinical picture. At initiation of treatment, CIWA-Ar/Ad/RASS (the latter for ICU patients) should again be assessed. The result of these scores, along with clinical picture, should then guide medication dosing; scoring should be repeated as indicated by the degree of AWS and frequency of medication dosing. No single guideline exists for managing this process; a sample protocol is provided in Figures 52.1–52.3.

FIGURE 52.1 AWS initial assessment guideline. AWS guidelines codeveloped with Dr. Amy Dzierba, Pharm.D., Columbia University Medical Center.

FIGURE 52.2 Suggested AWS guideline for mild, moderate, and severe AWS. AWS guidelines codeveloped with Dr. Amy Dzierba, Pharm.D., Columbia University Medical Center.

FIGURE 52.3 AWS guideline for RAW and DT. AWS guidelines codeveloped with Dr. Amy Dzierba, Pharm.D., Columbia University Medical Center.
MANAGEMENT GUIDELINES
Moderate to severe AWS is most commonly treated with benzodiazepines. Ideal pharmacologic management is tailored to the individual patient and controls hyperadrenergic symptoms, anxiety, agitation, and delirium while minimizing adverse effects. Drug selection and dosing strategy should be informed by the desired pharmacodynamic and pharmacokinetic properties of the drugs, as well as by individual patient characteristics (existing symptoms, underlying illnesses, and/or past episodes of AWS). Ongoing subjective assessments using CIWA-Ar/Ad and RASS scores are essential.
When compared to standing doses or continuous infusions of benzodiazepines, well-executed STT with benzodiazepines plus adjunctive agents can decrease total benzodiazepine dose, incidence of intubation and admission to the ICU, and hospital and ICU length of stay (LOS).18,20–25,42,45–47 In one study, well-executed STT was shown to be comparable to front-loading, an approach in which patients are typically titrated to lid lag, a low CIWA score (<8), or a state of calm.26 In front-loading, the use of long-acting benzodiazepines with active metabolites can lead to heavier sedation but confers the advantage of autotapering. In the emergency department (ED), front-loading followed by SST is often used in the initial control phase for patients in AWS.48 Generally speaking, institutional clinical guidelines and individual patient parameters should guide the practitioner's choice of approach.
The five most commonly used benzodiazepines are diazepam, chlordiazepoxide, lorazepam, clonazepam, and oxazepam. There are several important considerations when choosing a pharmacologic agent for a patient in AWD (Table 52.4).
TABLE 52.4 Benzodiazepines for treatment of AWS

Chlordiazepoxide and diazepam have a longer duration of action due to the presence of active metabolites. This may decrease the rate of breakthrough symptoms and have an autotapering effect.49,50 Parenteral diazepam has a short onset and is preferred for rapid titration in severe cases; doses of 5 to 20 mg can be given every 5 to 10 minutes. Higher bolus doses can be used if the patient demonstrates tolerance. Oral chlordiazepoxide can be used effectively in moderate withdrawal and can be rapidly titrated at doses of 50 to 100 mg/hour. Patients may also be managed with aggressive oral dosing of chlordiazepoxide. The experience of recent national drug shortages established the efficacy of this approach in patients previously thought to require parenteral medications.51–53
Lorazepam, which has a longer time to peak effect (15 to 20 minutes), may lead to iatrogenic oversedation if titrated too rapidly. Lorazepam can be titrated in doses of 1 to 4 mg every 15 to 30 minutes. If higher doses are used, a longer dosing interval is preferred. Due to lorazepam's lack of active metabolites, nondependence on renal or hepatic mechanisms for clearance and predictable t1/2, it is preferred over diazepam and chlordiazepoxide for use in patients with COPD, hepatic dysfunction (INR > 1.6), renal dysfunction (CrCl < 30 mL/min, SCr > 2 mg/dL), or age > 65 years.54 Prolonged lorazepam infusions carry a risk of toxicity from propylene glycol (the diluent in lorazepam infusions) with associated metabolic acidosis and renal failure. Lorazepam is also incompatible with numerous other infusions.
In general, it is recommended to avoid using different benzodiazepines together (e.g., oral chlordiazepoxide and intravenous benzodiazepines), except during the initial control phase when a patient is progressing from mild to more severe symptoms, or to provide a basis for autotapering (when chlordiazepoxide is added). The deliberate and measured use of different classes of medications based on mechanism of action and synergy can yield good results. Haphazard polypharmacy with benzodiazepines and other sedatives in difficult-to-control patients increases the chances of unexpected synergy and oversedation.
Patients with resistant alcohol withdrawal (defined below) require ICU-level monitoring and a more aggressive pharmacotherapeutic approach. Such patients often require adjunctive therapies like phenobarbital or propofol (see below).
Resistant Alcohol Withdrawal (RAW) is defined as the following:
1.Failure to respond to 200 mg of IV diazepam (or 30 mg lorazepam) in the first 3 hours
2.Failure to respond to 400 mg of IV diazepam (or 60 mg lorazepam) in the first 8 hours
3.Requirement of repeated doses of more than 40 mg of diazepam for control of agitation
4.Persistent CIWA scores of >25 despite aggressive therapy
Barbiturates are GABAA agonists and have been employed as monotherapy and, more commonly, as adjuncts in severe DT or RAW.20,51,52,55–59 The most studied barbiturate in the setting of AWS is phenobarbital, which is typically initiated in a monitored setting when high-dose benzodiazepines have failed to control symptoms. A standard starting dose of phenobarbital of 30 mg can be used, titrated to effect every 30 minutes. As the onset of barbiturates' effect can be delayed, it is prudent to wait approximately 30 minutes before adding an additional agent. The long half-life of barbiturates also confers a beneficial self-tapering effect. One study showed decreased ICU admissions with phenobarbital given as a single dose of 19 mg/kg (vs. placebo) early in the course of treatment.58 It is unclear, however, whether this outcome demonstrates superiority of loading with a barbiturate, or the benefit of a front-loaded approach in general paired with a less aggressive institutional protocol. In times of nationwide benzodiazepine shortages, the use of barbiturates in the treatment of AWS should be considered a reasonable therapeutic option.51,52
Propofol is a GABAA agonist and an NMDA antagonist. It is highly effective at controlling severe AWS symptoms and is generally reserved for cases refractory to high-dose benzodiazepines and barbiturates. Intubation is generally recommended because of propofol's potency and the narrow window between an effective and toxic dose. Propofol's short half-life makes it unsuitable as a primary or exclusive agent. Intubated patients on propofol infusions can be started on a benzodiazepine or chlordiazepoxide via nasogastric tube, in an effort to wean from propofol and establish a base of long-acting benzodiazepines that permit autotapering (see Tapering section).60,61 Propofol infusions are susceptible to tachyphylaxis and should only be used in a highly monitored setting.62
In historical studies of AWS, benzodiazepines have been shown far superior to monotherapy with antipsychotics in controlling symptoms and preventing seizures or DT's.41,63,64 Bolus therapy with the antipsychotic haloperidol, given with clonidine and benzodiazepines, has been described as a successful combination when compared to continuous monotherapy infusions.24,41,42 It is not clear whether the strength of the treatment reported was the result of attentive STT/bolus therapy, or the combination of the medications used, or both. As a general rule, while there may be a role for antipsychotics in patients in AWS with comorbid psychiatric disorders or pronounced hallucinations, monotherapy with these agents should be avoided.
Some studies have suggested that benzodiazepine use in the treatment of AWS can lead to more craving—of both ethanol and benzodiazepines—and that alternative, non–benzodiazepine-based regimens—such as anticonvulsants—may decrease craving and relapse after detoxification.65–69 Since these studies considered only short-term outcomes, it is difficult to know whether the effect on craving continues beyond the initial period following detoxification.
The anticonvulsant topiramate is an antiglutaminergic and GABA-enhancing drug, and studies have shown it to attenuate AWS in rodents.70 Human studies have shown a benefit over placebo for preventing AWS and suggest a possible role for treating ethanol dependence.9,10,70 Valproic acid,71–73 gabapentin,67,74 and carbamazepine66,71,75 have also been evaluated in the treatment of AWS, primarily in mild to moderate cases in the settings of inpatient and outpatient detoxification units. Studies suggest them to be inadequate as sole agents but potentially more useful in combination therapy.33,71,76
A 2010 Cochrane review of anticonvulsants for AWS concluded that there was insufficient evidence in their favor, excepting the use of carbamazepine, which may outperform benzodiazepines in treating some aspects of AWS.77 Compared to benzodiazepines, carbamazepine appears to have more benefit in symptom control and craving in less medically severe cases and in the outpatient setting, but less benefit in preventing seizures and DTs.75
Gamma-hydroxybutyric acid (GHB), also a GABAA agonist, was found to be comparable, but not superior, to benzodiazepines.78 GHB has been used more widely in Europe, but concerns for GHB addiction have tempered its use in the United States.79 Phenytoin has not been shown to be beneficial in seizures related to AWS.80–82
Of note, in 2013, an unpublished case series was presented at a national meeting regarding the use of valproic acid or gabapentin with clonidine patches. The investigator described successful detoxification of medically moderate to severe AWS without the use of a benzodiazepine.53,83 Since the findings remain unpublished, it is difficult to comment on the results, except to say that alternative regimens to benzodiazepines are being explored and discussed.
Clonidine and dexmedetomidine are centrally acting α2 agonists. α2 agonists decrease NE release and reduce symptoms of sympathetic overdrive. These agents have been studied in rodent models for the treatment of AWS84–87 as well as in a limited number of human trials. The surgical literature has reported the successful use of clonidine with haloperidol and benzodiazepines in the treatment of surgical intensive care unit (SICU) and trauma patients with AWS;24,41,42,88,89 one randomized controlled trial found transdermal clonidine to be as effective as chlordiazepoxide in the management of mild AWS;90 and a case series reported using high-dose clonidine patches in combination with valproic acid or gabapentin in the treatment of moderate to severe AWS.83 Most studies (case reports and uncontrolled case series) of dexmedetomidine in AWS have focused on its use as an adjunctive agent.91–101 Both clonidine and dexmedetomidine can produce sedation as well as hypotension and bradycardia, and acute withdrawal from dexmedetomodine has been described in patients on prolonged infusions.102 There is likely a role for clonidine and dexmedetomidine as adjuncts in the treatment of AWS, but more studies are required to fully comment on appropriate case selection, outcomes, and patient safety.103 At this time, neither agent is recommended for use as monotherapy in AWS.
Baclofen is a stereo-selective agonist of GABAB. It has been shown to be effective in suppressing AWS in rodents104,105 and, in a small number of human trials, to be comparable, but not superior, to benzodiazepines.106–108 It is notable that the benzodiazepine doses were low in the human trial comparison groups, suggesting that the study population was experiencing less severe withdrawal. A recent Cochrane review concluded that there were insufficient data to make outcome or safety conclusions regarding baclofen's use for AWS.109 Baclofen has shown some effect in supporting efforts at alcohol abstinence in alcohol-dependent patients with liver cirrhosis. This application has gained popularity, particularly in Europe, and warrants further study.106,107,110–113
Ethanol therapy for AWS (IV or PO) is not recommended due to a high failure rate and potential for complications.114–117 In both PO and IV forms, alcohol has large free water content, an association with electrolyte and behavioral disturbances, and a tendency to cause hypoglycemia. These factors, as well as difficulties in titration to adequate blood levels, make it an unsuitable choice.115 In a randomized trial of IV ethanol versus scheduled-dose diazepam in a trauma ICU, IV ethanol was found to be inferior to diazepam and was associated with greater treatment failures.117 Prophylaxis with ethanol in patients, particularly for elective surgical admissions, is practiced in some centers.115 A discussion of this is beyond the scope of this chapter, and it remains a controversial practice.
Beta-adrenergic agents should not be used to control the hypertension and tachycardia associated with AWS until the underlying cause (i.e., the hyperadrenergic AWS state) is treated. Once fluid status and appropriate sedation are administered, vital sign abnormalities usually normalize. If hypertension coexists, beta-blockers and other antihypertensive agents can be used to control blood pressure. Beta-blockers, by masking abnormal vital signs, can also obscure the diagnosis of delirium tremens.118
Once initial control of withdrawal symptoms is achieved with benzodiazepines and/or phenobarbital/propofol and a stable clinical trend is established for 24 to 28 hours, a plan for tapering must be implemented. A recommended approach is to taper by approximately 20% per day of total daily benzodiazepine equivalent dose. Taper with chlordiazepoxide when possible (anticipate starting with ≥100 mg chlordiazepoxide PO q2–8h in severe cases). For example, if a patient had a total of 700 mg chlordiazepoxide PO and 8 mg lorazepam IV over 24 hours (equivalent to ~900 mg chlordiazepoxide), then the next day's dose would be 720 mg/day (divided q6–8h). Patients treated with long-acting agents with active metabolites may exhibit varying degrees of an “autotaper” effect while still receiving STT. If during tapering, a patient's CIWA-Ar scores increase to >10, give supplemental medication for breakthrough symptoms and consider a slower taper by increasing the daily dose, that is, tapering by 10% per day. Propofol infusions should be tapered as early as possible (after 2 to 3 days) because of the associated risk of infection and hypertriglyceridemia. Tapering from nonbenzodiazepines is not well described in moderate to severe AWS.
The following additional supportive care measures for the patient with AWS should be considered, particularly if the patient is heavily sedated or bedbound.
A.Daily × 7 days: thiamine 100 mg PO/IV, folate 1 mg PO/IV, and MVI PO/IV
B.Careful electrolyte repletion
c.Docusate 100 mg PO/NG/DT/PEG TID and Senna two tablets PO/NG/DT/PEG daily
D.Lacrilube each eye BID or artificial tears two drops each eye QID
E.NPO if compromised mental status, severe agitation, and risk for aspiration
F.Early mobilization from bed whenever possible per ICU/SDU care plan
G.Avoidance of daily interruption of sedation as is routine with other ICU patients
H.Restraints and continuous observation as per hospital policy
I.MICU and psychiatry consult for difficult cases
J.Social Work consult for after care and outpatient detox/rehab follow-up
CONCLUSION
STT with benzodiazepines is currently accepted as best practice in the management of mild to severe AWS. This approach provides the greatest advantage in patients with severe AWS, benzodiazepine-resistant AWS, and DT's, resulting in shorter lengths of stay, decreased complication rates, and lower total medication dose requirements when compared to lower bolus doses or those placed on continuous infusions (especially of benzodiazepines).35 Propofol and dexmedetomidine are not supported as sole agents or first-line agents, but show promise as rescue medications in benzodiazepine-resistant cases or when intubation is considered imminent. Resource utilization and complications rates remain high for patients with severe AWS, and providers should exercise a low threshold for transfer to the MICU in concerning cases (Figs. 52.2 and 52.3).
LITERATURE TABLE

1.Cagetti E, Liang J, Spigelman I, et al. Withdrawal from chronic intermittent ethanol treatment changes subunit composition, reduces synaptic function, and decreases behavioral responses to positive allosteric modulators of GABAA receptors. Mol Pharmacol. 2003;63:53.
2.Kumar S, Porcu P, Werner DF. The role of GABA receptors in the acute and chronic effects of ethanol: a decade of progress. Psychopharmacology (Berl). 2009;205:529.
3.Mihic SJ, Ye Q, Wick MJ, et al. Sites of alcohol and volatile anaesthetic action on GABA(A) and glycine receptors. Nature. 1997;389:385.
4.Morrow AL, Suzdak PD, Karanian JW, et al. Chronic ethanol administration alters gamma-aminobutyric acid, pentobarbital and ethanol-mediated 36Cl− uptake in cerebral cortical synaptoneurosomes. J Pharmacol Exp Ther. 1988;246:158.
5.Whittemore ER, Yang W, Drewe JA, et al. Pharmacology of the human gamma-aminobutyric acid A receptor alpha 4 subunit expression in Xenopus laevis oocytes. Mol Pharmacol. 1996;50:1364–1365.
6.Hoffman PL, Grant KA, Snell LD, et al. NMDA receptors: role in ethanol withdrawal seizures. Ann N Y Acad Sci. 1992;654:52.
7.Tsai G, Gastfriend DR, Coyle JT. The glutamatergic basis of human alcoholism. Am J Psychiatry. 1995;152(3):332–340. PMID: 7864257.
8.Tsai G, Coyle JT. The role of glutamatergic neurotransmission in the pathophysiology of alcoholism. Annu Rev Med. 1998;49:173–184. PMID: 9509257.
9.Johnson BA, Ait-Daoud N, Bowden CL, et al. Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. Lancet. 2003;361(9370):1677–1685. PMID: 12767733.
10.Johnson BA, Swift RM, Ait-Daoud N, et al. Development of novel pharmacotherapies for the treatment of alcohol dependence: focus on antiepileptics. Alcohol Clin Exp Res. 2004;28(2):295–301. PMID: 15112937.
11.Swift RM. Topiramate for the treatment of alcohol dependence: initiating abstinence. Lancet. 2003;361(9370):1666–1667. PMID: 12767727.
12.Finn DA, Crabbe JC. Exploring alcohol withdrawal syndrome. Alcohol Health Res World. 1997;21(2): 149–156. PMID: 15704352.
13.Lingford-Hughes A, Nutt D. Neurobiology of addiction and implications for treatment. Br J Psychiatry. 2003;182(2):97–100. PMID: 12562734.
14.Nutt D. Alcohol and the brain: pharmacological insights for psychiatrists. Br J Psychiatry. 1999;175(2): 114–119. PMID: 10627792.
15.Borg S, Kvande H, Sedvall G. Central norepinephrine metabolism during alcohol intoxication in addicts and healthy volunteers. Science. 1981;213(4512):1135–1137. PMID: 7268421.
16.Linnoila M, Mefford I, Nutt D, et al. NIH conference: alcohol withdrawal and noradrenergic function. Ann Intern Med. 1987;107(6):875–889. PMID: 2825572.
17.Sellers EM, Degani NC, Zilm DH, et al. Propranolol-decreased noradrenaline excretion and alcohol withdrawal. Lancet. 1976;1(7950):94–95. PMID: 54619.
18.Cassidy EM, O'Sullivan I, Bradshaw P, et al. Symptom-triggered benzodiazepine therapy for alcohol withdrawal syndrome in the emergency department: a comparison with the standard fixed dose benzodiazepine regimen. Emerg Med J. 2012;29:802.
19.Daeppen JB, Gache P, Landry U, et al. Symptom-triggered vs fixed-schedule doses of benzodiazepine for alcohol withdrawal: a randomized treatment trial. Arch Intern Med. 2002;162:1117. PMID: 12020181.
20.Gold JA, et al. A strategy of escalating doses of benzodiazepines and phenobarbital administration reduces the need for mechanical ventilation in delirium tremens. Crit Care Med. 2007;35(3):724–730.
21.Jaeger TM, et al. Symptom-triggered therapy for alcohol withdrawal in medical inpatients. Mayo Clin Proc. 2001;76(7):695–701.
22.Saitz R, Mayo-Smith M, Roberts MS, et al. Individualized treatment for ethanol withdrawal. JAMA. 1994;272:519–523.
23.See S, Nosal S, Barr WB, et al. Implementation of a symptom triggered benzodiazepine protocol for alcohol withdrawal in family medicine inpatients. Hosp Pharm. 2009;44(10):881–887.
24.Spies CD, Otter HE, Hüske B, et al. Alcohol withdrawal severity is decreased by symptom-orientated adjusted bolus therapy in the ICU. Intensive Care Med. 2003;29:2230. PMID: 14557857.
25.Stanley KM, Amabile CM, Simpson KN, et al. Impact of an alcohol withdrawal syndrome practice guideline on surgical patient outcomes. Pharmacotherapy. 2003;23:843–854. PMID: 12885097.
26.Maldonado JR, Nguyen LH, Schader EM, et al. Benzodiazepine loading versus symptom-triggered treatment of alcohol withdrawal: a prospective, randomized clinical trial. Gen Hosp Psychiatry. 2012;34: 611–617. PMID: 22898443.
27.Maldonado JR. An approach to the patient with substance use and abuse. Med Clin North Am. 2010;94:1169–1205. PMID: 20951277.
28.Victor M, Adams RD. The effect of alcohol on the central nervous system. In: Metabolic and Toxic Disease of the Nervous System. Baltimore, MD: Lippincott Williams & Wilkins. 1953:526–573.
29.Victor M, Brausch C. The role of abstinence in the genesis of alcoholic epilepsy. Epilepsia. 1967;8:1–20.
30.Boston LN. Alcohol withdrawal. Lancet. 1908;1:18.
31.DeBellis R, Smith BS, Choi S, et al. Management of delirium tremens. J Intensive Care Med. 2005;20:164. PMID: 15888905.
32.Pristach CA, Smith CM, Whitney RB. Alcohol withdrawal syndromes—prediction from detailed medical and drinking histories. Drug Alcohol Depend. 1983;11:177. PMID: 6861616.
33.Saitz R, O'Malley SS. Pharmacotherapies for alcohol abuse. Withdrawal and treatment. Med Clin North Am. 1997;81:881. PMID: 9222259.
34.Hecksel KA, Bostwick JM, Jaeger TM, et al. Inappropriate use of symptom-triggered therapy for alcohol withdrawal in the general hospital. Mayo Clin Proc. 2008;83:274–279. PMID: 18315992.
35.Awissi DK, Lebrun G, Coursin DB, et al. Alcohol withdrawal and delirium tremens in the critically ill: a systematic review and commentary. Intensive Care Med. 2013;39:16–30. PMID: 23184039.
36.Eyer F, Schuster T, Felgenhauer N, et al. Risk assessment of moderate to severe alcohol withdrawal—predictors for seizures and delirium tremens in the course of withdrawal. Alcohol Alcohol. 2011;46:427–433. PMID: 21593124.
37.Monte R, Rabuñal R, Casariego E, et al. Risk factors for delirium tremens in patients with alcohol withdrawal syndrome in a hospital setting. Eur J Intern Med. 2009;20(7):690–694. PMID: 19818288.
38.Thiercelin N, Rabiah Lechevallier Z, Rusch E, et al. Risk factors for delirium tremens: a literature review. Rev Med Interne. 2012;33:18–22. PMID: 21920639.
39.Chan GM, Hoffman RS, Gold JA, et al. Racial variations in the incidence of severe alcohol withdrawal. J Med Toxicol. 2009;5(1):8–14. PMID: 19191209.
40.Nuss MA, Elnicki DM, Dunsworth TS, et al. Utilizing CIWA-Ar to assess use of benzodiazepines in patients vulnerable to alcohol withdrawal syndrome. W V Med J. 2004;100:21–25. PMID: 15119493.
41.Spies CD, Dubisz N, Neumann T, et al. Therapy of alcohol withdrawal syndrome in intensive care unit patients following trauma: results of a prospective, randomized trial. Crit Care Med. 1996;24:414–422. PMID: 8625628.
42.Spies CD, Rommelspacher H. Alcohol withdrawal in the surgical patient: prevention and treatment. Anesth Analg. 1999;88(4):946–954. PMID: 10195555.
43.Sullivan JT, Sykora K, Schneiderman J, et al. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989;84:1353.
44.Sullivan JT, et al. Benzodiazepine requirements during alcohol withdrawal syndrome: clinical impressions using a standardized withdrawal scale. J Clin Pharmacol. 1991;11:291–295.
45.Mayo-Smith MF; for the American Society of Addiction Medicine Working Group on Pharmacological Management of Ethanol Withdrawal. Pharmacological management of ethanol withdrawal: a meta-analysis and evidence based practice guideline. JAMA. 1997;278:144–151.
46.Mayo-Smith MF, Beecher LH, Fischer TL, et al. Management of alcohol withdrawal delirium. An evidence-based practice guideline. Arch Intern Med. 2004;164:1405.
47.Repper-DeLisi J, Stern TA, Mitchell M, et al. Successful implementation of an alcohol-withdrawal pathway in a general hospital. Psychosomatics. 2008;49(4):292–299. PMID: 18621934.
48.Stehman CR, Mycyk MB. A rational approach to treatment of alcohol withdrawal in the ED. Am J Emerg Med. 2013;31:734–742. PMID: 23399338.
49.Amato L, Minozzi S, Vecchi S, et al. Benzodiazepines for alcohol withdrawal. Cochrane Database Syst Rev. 2010;3:CD005063. doi: 10.1002/14651858.CD005063.pub3.
50.Amato L, Minozzi S, Davoli M. Efficacy and safety of pharmacologic interventions for the treatment of the alcohol withdrawal syndrome. Cochrane Database Syst Rev. 2011;CD008537.
51.Hoffman RS. Management of moderate to severe alcohol withdrawal syndromes. UptoDate. http://www.uptodate.com. Accessed September 11, 2013.
52.Miller DG, Weinstein E, Hunter BR. Alcohol, meet benzodiazepine shortage; How to effectively treat alcohol withdrawal during nationwide shortages of benzodiazepines. Emerg Physic Monthly. 2012; June.
53.Otto AM. Benzodiazepines discouraged for alcohol withdrawal. Clinical Psychiatry News. March 15, 2013. http://www.clinicalpsychiatrynews.com/index.php?id=2407&cHash=071010&tx_ttnews[tt_news]=141547. Accessed April, 2014.
54.Kumar CN, Andrade C, Murthy P. A randomized, double-blind comparison of lorazepam and chlordiazepoxide in patients with uncomplicated alcohol withdrawal. J Stud Alcohol Drugs. 2009;70(3):467–474. PMID: 19371497.
55.Hayner CE, Wuestefeld NL, Bolton PJ. Phenobarbital treatment in a patient with resistant alcohol withdrawal syndrome. Pharmacotherapy. 2009;29(7):875–878. PMID: 19558262.
56.Hjermø I, Anderson JE, Fink-Jensen A, et al. Phenobarbital vs Diazepam for delirium tremens: a retrospective review. Dan Med Bull. 2010;57:A4149.
57.Kramp P, Rafaelsen OJ. Delirium tremends A double blind comparison of diazepam and barbital treatment. Acta Psychiatr Scand. 1978;58:174–190.
58.Rosenson J, Clements C, Simon B, et al. Phenobarbital for acute alcohol withdrawal; A prospective randomized double-blind placebo controlled study. J Emerg Med. 2013;44:592–598.
59.Young GP, Rores C, Murphy C, et al. Intravenous phenobarbital for alcohol withdrawal and convulsions. Ann Emerg Med. 1987;16(8):847–850. PMID: 3619162.
60.Coomes TR, Smith SW. Successful use of propofol in refractory delirium tremens. Ann Emerg Med. 1997;30:825. PMID: 9398758.
61.McCowan C, Marik P. Refractory delirium tremens treated with propofol: a case series. Crit Care Med. 2000;28:1781. PMID: 10890619.
62.Currier DS, Bevacgua BK. Acute tachyphylaxis to propofol sedation during ethanol withdrawal. J Clin Anesth. 1997;9:420–423. PMID: 9257211.
63.Blum K, Eubanks JD, Wallace JE, et al. Enhancement of alcohol withdrawal convulsions in mice by haloperidol. Clin Toxicol. 1976;9:427. PMID: 986285.
64.Kaim SC, Klett CJ, Rothfeld B. Treatment of the acute alcohol withdrawal state: a comparison of four drugs. Am J Psychiatry. 1969;125(12):1640–1646. PMID: 4890289.
65.Longo LP, Campbell T, Hubatch S. Divalproex sodium (Depakote) for alcohol withdrawal and relapse prevention. J Addict Dis. 2002;21(2):55–64. PMID: 11916372.
66.Malcolm R, Myrick H, Roberts J, et al. The effects of carbamazepine and lorazepam on single versus multiple previous alcohol withdrawals in an outpatient randomized trial. J Gen Intern Med. 2002;17(5):349–355. PMID: 12047731.
67.Myrick H, Malcolm R, Randall PK, et al. A double-blind trial of gabapentin versus lorazepam in the treatment of alcohol withdrawal. Alcohol Clin Exp Res. 2009;33:1582–1588. PMID: 19485969.
68.Zack M, Poulos CX, Woodford TM. Diazepam dose-dependently increases or decreases implicit priming of alcohol associations in problem drinkers. Alcohol Alcohol. 2006;41(6):604–610. PMID: 17020910.
69.Poulos CX, Zack M. Low-dose diazepam primes motivation for alcohol and alcohol-related semantic networks in problem drinkers. Behav Pharmacol. 2004;15(7):503–512. PMID: 15472572.
70.Cagetti E, Baicy KJ, Olsen RW. Topiramate attenuates withdrawal signs after chronic intermittent ethanol in rats. Neuroreport. 2004;15:207–2010. PMID: 15106859.
71.Eyer F, Schreckenberg M, Hecht D, et al. Carbamazepine and valproate as adjuncts in the treatment of alcohol withdrawal syndrome: a retrospective cohort study. Alcohol Alcohol. 2011;46:177–184. PMID: 21339186.
72.Lum E, Gorman SK, Slavik RS. Valproic acid management of acute alcohol withdrawal. Ann Pharmacother. 2006;40:441–448. PMID: 16507623.
73.Reoux JP, Saxon J, Malte CA. Divalproex sodium in alcohol withdrawal: a randomized double-blind placebo controlled clinical trial. Alcohol Clin Exp Res. 2011;25:1324–1329. PMID: 11584152.
74.Bonnet U, Hamzavi-Abedi R, Specka M, et al. An open trial of gabapentin in acute alcohol withdrawal using an oral loading protocol. Alcohol Alcohol. 2010;45:143–145. PMID: 20019070.
75.Barrons R, Robertss N. The role of carbamazepine and oxcarbamazepine in alcohol withdrawal syndrome. J Clin Pharm Ther. 2010;35:153–167. PMID: 20456734.
76.Hillborn M, Tokola R, Kuusela V, et al. Prevention of alcohol withdrawal seizures in carbamazepine and valproic acid. Alcohol. 1989;6:223–226. PMID: 2500138.
77.Minozzi S, Amato L, Vecchi S, et al. Anticonvulsants for alcohol withdrawal. Cochrane Database Syst Rev. 2010;CD005064.
78.Addolorato G, Balducci G, Capristo E, et al. Gamma-hydroxybutyric acid (GHB) in the treatment of alcohol withdrawal syndrome: a randomized comparative study versus benzodiazepine. Alcohol Clin Exp Res. 1999;23:1596–1604. PMID: 10549990.
79.Addolorato G, Leggio L, Ferrulli A, et al. The therapeutic potential of gamma-hydroxybutyric acid for alcohol dependence: balancing the risks and benefits. A focus on clinical data. Expert Opin Investig Drugs. 2009;18:675–686. PMID: 19379123.
80.Alldredge BK, Lowenstein DH, Simon RP. Placebo-controlled trial of intravenous diphenylhydantoin for short-term treatment of alcohol withdrawal seizures. Am J Med. 1989;87:645. PMID: 2686433.
81.Chance JF. Emergency department treatment of alcohol withdrawal seizures with phenytoin. Ann Emerg Med. 1991;20:520. PMID: 2024792.
82.Rathlev NK, D'Onofrio G, Fish SS, et al. The lack of efficacy of phenytoin in the prevention of recurrent alcohol-related seizures. Ann Emerg Med. 1994;23:513. PMID: 8135426.
83.Maldonado JP. Alcohol Withdrawal Syndrome—Treatment Options Beyond Benzodiazepines. San Juan, Puerto Rico: ACMT Alcohol Abuse Academy; 2013.
84.Jaatinen P, Riihioja P, Haapalinna A, et al. Prevention of ethanol-induced sympathetic overactivity and degeneration by dexmedetomidine. Alcohol. 1995;12(5):439–446. PMID: 8519439.
85.Riihioja P, Jaatinen P, Haapalinna A, et al. Effects of dexmedetomidine on rat locus coeruleus and ethanol withdrawal symptoms during intermittent ethanol exposure. Alcohol Clin Exp Res. 1999;23(3):432–438. PMID: 10195815.
86.Riihioja P, Jaatinen P, Oksanen H, et al. Dexmedetomidine alleviates ethanol withdrawal symptoms in the rat. Alcohol. 1997;14(6):537–544. PMID: 9401667.
87.Riihioja P, Jaatinen P, Oksanen H, et al. Dexmedetomidine, diazepam, and propranolol in the treatment of ethanol withdrawal symptoms in the rat. Alcohol Clin Exp Res. 1997;21(5):804–808. PMID: 9267529.
88.Braz LG, Camacho Navarro LH, Braz JR, et al. Clonidine as adjuvant therapy for alcohol withdrawal syndrome in intensive care unit: case report. Rev Bras Anestesiol. 2003;53(6):802–807. PMID: 19471699.
89.Dobrydnjov I, Axelsson K, Berggren L, et al. Intrathecal and oral clonidine as prophylaxis for postoperative alcohol withdrawal syndrome: a randomized double-blinded study. Anesth Analg. 2004;98(3): 738–744. PMID: 14980929.
90.Baumgartner GR, Rowen RC. Transdermal clonidine vs. chlordiazepoxide in alcohol withdrawal: a randomized controlled clinical trial. South Med J. 2001;84(3):312–321. PMID: 2000517.
91.Baddigam K, Russo P, Russo J, et al. Dexmedetomidine in the treatment of withdrawal syndromes in cardiothoracic surgery patients. J Intensive Care Med. 2005;20(2):118–123. PMID: 15855224.
92.Cooper L, Castillo D, Martinez-Ruid R, et al. Am Society of Anesthesiology. Adjuvant use of dexmedetomidine may reduce the incidence of endotracheal intubation caused by benzodiazepines in the treatment of delirium tremens [abstract] Anesthesiology. 2005;103:A317.
93.Darrouj J, Puri N, Prince E, et al. Dexmedetomidine infusion as adjunctive therapy to benzodiazepines for acute alcohol withdrawal. Ann Pharmacother. 2008;42(11):1703–1705. PMID: 18780809.
94.DeMuro JP, Botros DG, Wirkowski E, et al. Use of dexmedetomidine for the treatment of alcohol withdrawal syndrome in critically ill patients: a retrospective case series. J Anesth. 2012;26:601–605. PMID: 22584816.
95.Finkel JC, Elrefai A. The use of dexmedetomidine to facilitate opioid and benzodiazepine detoxification in an infant. Anesth Analg. 2004;98(6):1658–1659. PMID: 15155322.
96.Kandiah P, Jacob S, Pandya D, et al. Novel use of dexmedetomidine in 7 adults with resistant alcohol withdrawal in the ICU. Poster presented at: The 38th Critical Care Congress of the Society of Critical Care Medicine; January 31–February 4, 2009; Nashville, TN.
97.Maccioli GA. Dexmedetomidine to facilitate drug withdrawal. Anesthesiology. 2003;98(2):575–577. PMID: 12552220.
98.Multz AS. Prolonged dexmedetomidine infusion as an adjunct in treating sedation-induced withdrawal. Anesth Analg. 2003;96:1054–1055. PMID: 12651659.
99.Prieto MN, Barr J, Tanaka RN, et al.; Am Society of Anesthesiology. Dexmedetomidine: a novel approach to the management of alcohol withdrawal in the ICU. Anesthesiology. 2007;107:A1313.
100.Rayner SG, Weinert CR, Peng H, et al. Dexmedetomidine as adjunct treatment for severe alcohol withdrawal in the ICU. Ann Intensive care. 2012;23:12. PMID: 22620986.
101.Rovasalo A, Tohmo H, Aantaa R, et al. Dexmedetomidine as an adjuvant in the treatment of alcohol withdrawal delirium: a case report. Gen Hosp Psychiatry. 2006;28:362–363. PMID: 16814639.
102.Kukoyi A, Coker S, Lewis L, et al. Two cases of acute dexmedetomidine withdrawal syndrome following prolonged infusion in the intensive care unit: report of cases and review of the literature. Hum Exp Toxicol. 2013;32:107–110. PMID: 23111887.
103.Muzyk AJ, Fowler JA, Norwood DK, et al. Role of α2-agonists in the treatment of acute alcohol withdrawal. Ann Pharmacother. 2011;45(5):649–657. PMID: 21521867.
104.Colombo G, Serra S, Brunetti G, et al. Suppression by baclofen of alcohol deprivation effect in Sardinian alcohol-preferring (sP) rats. Drug Alcohol Depend. 2003;70:105.
105.Humeniuk RE, White JM, Onh J. The effect if GABAB ligands on alcohol withdrawal in mice. Pharmacol Biochem Behav. 1994;49:561–566.
106.Addolorato G, Leggio L, Ferrulli A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007;370:1915–1922.
107.Addolorato G, Leggio L, Abenavoli L, et al. Baclofen in the treatment of alcohol withdrawal syndrome: a comparative study vs. diazepam. Am J Med. 2006;119:276.e13. PMID: 16490478.
108.Lyon JE, Khan RA, Gessert CE, et al. Treating alcohol withdrawal with oral baclofen: a randomized, double-blind, placebo controlled trial. J Hosp Med. 2011;6:469–474. PMID: 21990176.
109.Liu J, Wang LN. Baclofen for alcohol withdrawal. Cochrane Database Syst Rev. 2013;2:CD008502. PMID: 23450582.
110.Addolorato G, Caputo F, Capristo E, et al. Rapid suppression of alcohol withdrawal syndrome by baclofen. Am J Med. 2002;112:226. PMID: 11893350.
111.Addolorato G, Leggio L, Agabio R, et al. Baclofen: a new drug for the treatment of alcohol dependence. Int J Clin Pract. 2006;60:1003–1008. PMID: 16893442.
112.Gorsane MA, Kebir O, Hache G, et al. Is baclofen a revolutionary medication in alcohol addiction management? Review and recent updates. Subst Abuse. 2012;33:336–349. PMID: 22989277.
113.Leggio L, Garbutt JC, Addolorato G. Effectiveness and safety of baclofen in the treatment of alcohol dependent patients. CNS Neurol Disord Drug Targets. 2010;9:33–44. PMID: 20201813.
114.Eggers V, Tio J, Neumann T, et al. Blood alcohol concentration for monitoring ethanol treatment to prevent alcohol withdrawal in the intensive care unit. Intensive Care Med. 2002;28:1475–1482. PMID: 12373474.
115.Dissanaike S, Halldorsson A, Frezza EE, et al. An ethanol protocol to prevent alcohol withdrawal syndrome. J Am Coll Surg. 2006;203:186–191. PMID: 16864031.
116.Hodges B, Mazur JE. Intravenous ethanol for the treatment of alcohol withdrawal syndrome in critically ill patients. Pharmacotherapy. 2004;24:1578. PMID: 15537562.
117.Weinberg JA, Magnotti LJ, Fischer PE, et al. Comparison of intravenous ethanol versus diazepam for alcohol withdrawal prophylaxis in the trauma ICU: results of a randomized trial. J Trauma. 2008;64(1):99–104. PMID: 18188105.
118.Zechnich RJ. Beta-blockers can obscure diagnosis of delirium tremens. Lancet. 1982;1:1071–1072. PMID: 6122874.
119.Sarff M, Gold JA. Alcohol withdrawal syndromes in the intensive care unit. Crit Care Med. 2010; 38(9 Suppl):S494–S501.