TABLE 54.1 Lake Louise Criteria for the Diagnosis of HAPE
BACKGROUND
Altitude illness encompasses a spectrum of clinical entities that occur at elevation as a result of hypobaric hypoxia. While a mild case of acute mountain sickness (AMS)—defined as headache with one of the following: nausea, fatigue, dizziness, anorexia, or poor sleep—may be no more than an inconvenience, high-altitude cerebral and pulmonary edema are true emergencies that require critical intervention and stabilization.
Although the concentration of oxygen remains nearly constant at 20.95% up to an elevation of at least 50 km, the partial pressure of oxygen decreases with increasing altitude in logarithmic fashion. With ascent to higher elevations, the lungs experience a decreasing pressure difference between alveolar and pulmonary arterial capillary beds. Without this pressure difference to drive oxygen across the alveolar membrane, tissue oxygen concentrations fall and, with extended time at altitude, result in hypoxia. This decrease begins at 1,500 m above sea level—generally referred to as the physiologic starting point of high altitude. Elevations are further classified as high altitude (1,500 to 3,500 m), very high altitude (3,500 to 5,500 m), and extreme altitude (above 5,500 m)—imprecise categories that loosely correlate to physiologic stress and pathology. While altitude determines the presence and extent of hypobaric hypoxia, increasing latitude, winter season, and the presence of storms driven by lower regional barometric pressure can influence local barometric pressure. These effects may combine to raise the effective altitude by hundreds of meters resulting in significant clinical consequences.
HIGH-ALTITUDE PULMONARY EDEMA
High-altitude pulmonary edema (HAPE) is a potentially deadly form of noncardiogenic edema driven by hypobaric hypoxia. Ascent to altitude produces an initial hypoxic pulmonary vasoconstrictor response. Although this adaptive response is believed to be useful in mitigating ventilation–perfusion mismatch in disorders such as pneumonia, a global constriction of the pulmonary vascular bed may lead to a pathologic increase in pulmonary artery pressures.1 While pulmonary artery pressures rise in all individuals with ascent to altitude, HAPE-susceptible individuals manifest an exaggerated response.2–4 One theory purports that uneven pulmonary vasoconstriction leads to overperfusion in select areas of the pulmonary vascular bed.5,6 This unevenly distributed perfusion overloads the pulmonary capillaries, eventually leading to fluid leak and “stress failure” of the alveolar–capillary membrane.7
Susceptibility to HAPE is driven by a complex set of factors, including prior history of HAPE, rate of ascent, sleeping altitude, physical exertion, air temperature, concomitant respiratory illness, and individual genetic predisposition or congenital cardiopulmonary abnormalities.2,8–14 Males were historically considered to be at higher risk for HAPE than females, but this hypothesis may have been influenced by behavioral confounders such as typically faster ascent profiles in males more than innate physiology. One recent study suggests that females may in fact be at higher risk.15 The incidence of HAPE at moderate elevations of 2,500 m (such as the Rocky Mountains of the American West) is 0.01%. Incidence increases to 2% at 3,600 m and may approach 5% at elevations above 4,300 m.16 Despite a relatively low incidence, HAPE is believed to be the most common cause of altitude- related death.
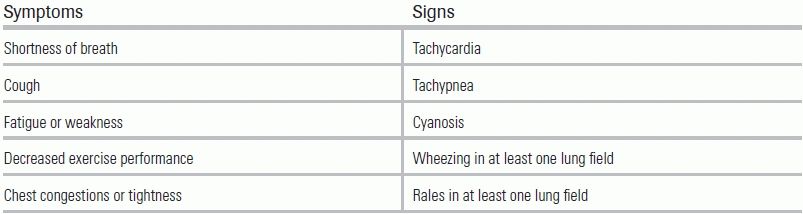
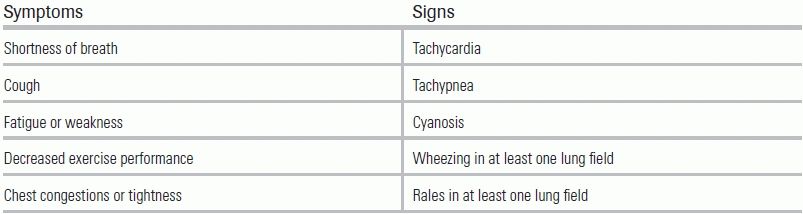
The classic victim of HAPE is a young, healthy person who is fit enough to rapidly ascend to high altitude. Symptoms typically develop on the second night of a new and higher sleeping altitude. Development of HAPE after 4 days at a given altitude is rare and should prompt the consideration of alternative diagnoses. Early (and possibly subtle) symptoms include a dry cough and reduced exercise performance. Symptoms may then progress to the more classic findings of dyspnea at rest and cough productive of pink, frothy sputum. The Lake Louise Criteria for the diagnosis of HAPE are based on the patient exhibiting a combination of two cardinal signs along with two symptoms17 (Table 54.1).
TABLE 54.1 Lake Louise Criteria for the Diagnosis of HAPE
While AMS is present in half of cases, it may notably be absent.18 Fever is common and does not preclude a diagnosis of HAPE, even in the presence of productive sputum. On chest radiograph, patchy lung infiltrates in the setting of a normal-sized heart confirms the diagnosis. EKG findings suggestive of right heart strain may also be observed. Arterial blood gas analysis reveals respiratory alkalosis with severe hypoxia. Partial pressures of arterial oxygen are typically between 30 and 40 mm Hg.19 The differential diagnosis for HAPE includes:
As with all altitude illness, the mainstays of treatment are descent and supplemental oxygen. In the field, individuals should descend 500 to 1,000 m or until symptoms resolve.20 If oxygen is available and symptoms are mild, oxygen may be given to maintain saturations above 90% in lieu of descent.21 While not systemically studied, simulated descent using a portable hyperbaric chamber can be considered if evacuation and oxygen are unavailable.22 Clinicians not experienced with these devices should be forewarned that their use may limit ongoing patient contact. More generally, patients should be kept warm and should avoid exertion, as both hypothermia and exercise lead to increased pulmonary artery pressures.23
Should weather or logistics preclude the provision of oxygen or descent, pharmacologic pulmonary vasodilators exist that can be used to bridge a patient until evacuation or oxygen is available. These agents are known to reduce pulmonary artery pressures; however, rigorous controlled studies are lacking regarding their efficacy in improving outcome. One study assessed nifedipine in a small cohort and demonstrated a reduction in pulmonary artery pressures and an improvement in arterial oxygenation, albeit with only modest clinical improvement.24 More recently, phosphodiesterase inhibitors and beta-agonists have shown efficacy in the prevention of HAPE and are commonly used in the field; however, no systematic trials have been performed to demonstrate their use in the acute treatment of HAPE.25,26 More work is currently needed to determine best pharmacologic practice for the treatment of HAPE; in the interim, it is reasonable to consider use of a pulmonary vasodilator if oxygen and descent are not available.
Once a patient is evacuated to an appropriate medical facility, oxygen should be delivered to maintain saturations above 90%. Positive airway pressure devices may be used to improve oxygenation if available; obtundation due to concomitant high-altitude cerebral edema (HACE) would be a relevant contraindication.27,28 The need for intubation is rare, but may be necessary for unstable patients with altered mental status or severe hypoxemia not responsive to supplemental oxygen. Patients will typically show clinical improvement within hours after the provision of oxygen. In the acute setting, the addition of a pharmacologic agent to oxygen therapy is reasonable if the patient has stable hemodynamics.
HIGH-ALTITUDE CEREBRAL EDEMA
HACE is the most critical manifestation of the AMS spectrum. Change in mental status in travelers at high altitude has been observed and documented for over a century,29 but the first comprehensive review of HACE was not published until 1983.30 The diagnosis of HACE is most often made clinically and requires mental status changes in individuals exhibiting symptoms of AMS.31 HACE has been reported to occur in just 1% to 2% of all high-altitude trekkers and in 3.4% of those suffering from AMS.32,33 Climbers who have developed HAPE have a much higher risk of concomitant HACE while at altitude, with a reported incidence of 13% to 20%; autopsy studies of patients who died of HAPE have shown that up to 50% of those had concurrent HACE.34
Although its exact pathophysiology remains unclear, HACE is believed to occur through a cascade of cytotoxic and vasogenic responses resulting in increased cellular permeability, vasoconstriction, and a deleterious rise in intracranial pressure.35 HACE most commonly occurs at altitudes above 4,700 m; however, it may present at lower altitudes in those already affected by HAPE.36 It is not known why some individuals are more susceptible than others to developing HACE—rapid ascent, heavy exertion at altitude, and a past history of AMS or HACE remain the most relevant risk factors.30,31
Altered mental status and ataxia are pathognomonic for HACE.30 Typically, individuals report progressively worsening AMS over the preceding 24 to 48 hours. Headache is usually, but not always, present. Early symptoms include drowsiness and subtle psychological and behavioral changes including apathy, social withdrawal, and confusion.31,37 Ataxia has been reported in approximately 40% to 60%, and papilledema is present in up to 50%.30 Gastrointestinal symptoms, including anorexia, nausea, and vomiting, may also occur. Visual and auditory hallucinations and seizures are rare. Retinal hemorrhages are associated with HACE but may also be present in climbers unaffected by HACE at higher altitudes. Level of consciousness may progress rapidly to coma, so alertness is a poor prognosticator of disease severity.
In 1991, the International Hypoxia Symposium established a set of guidelines for the clinical diagnosis of HACE. The Lake Louise Criteria for HACE are “the presence of a change in mental status or ataxia in a person with AMS” or “the presence of both a change in mental status and ataxia in a person without AMS.”17 It is critical to maintain a broad differential diagnosis, especially in patients with atypical presentations or those who are not responding to conventional therapy. The differential diagnosis for HACE is broad and includes:
HACE is primarily a clinical diagnosis, with laboratory and imaging studies primarily used to rule out potentially confounding disease processes. Appropriate laboratory studies include an electrolyte panel, complete blood count, glucose, ethanol level, carboxyhemoglobin level, and toxicology screen.37 Patients with HACE may have a mild leukocytosis, so clinical correlation is necessary to exclude an infectious etiology.30 A lumbar puncture may be performed if there is sufficient concern for CNS infection or subarachnoid hemorrhage. Typical findings include normal cell counts, but markedly elevated opening pressures as high as 44 to 220 mm H2O in affected individuals.38,39 Head computed tomography will show an attenuation of signal in the white matter with compression of sulci and flattening of gyri consistent with cerebral edema. Magnetic resonance imagings (MRIs) will demonstrate increased T2 signaling in the corpus callosum without changes in the gray matter, consistent with the white matter effects of vasogenic edema.40 Importantly, imaging findings lag behind clinical recovery and can be used to confirm the diagnosis of HACE even after clinical improvement.
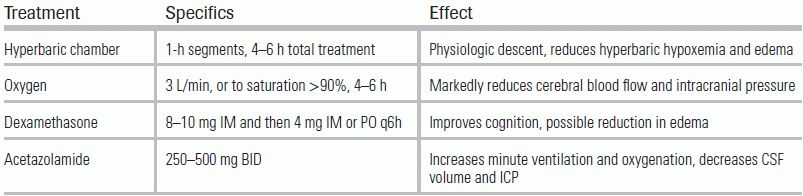
There is a saying that there are three treatments for HACE: “descent, descent, and descent.” All altitude illnesses should be treated primarily by descent to a lower elevation. Current field guidelines recommend descending at least 500 m or to the last known elevation at which the patient was asymptomatic.41 Delaying descent to wait for aeromedical rescue or to institute pharmacologic treatment can be fatal. If physical descent is impossible due to weather, geography, or severity in a patient's condition, achieving physiologic descent via a portable hyperbaric chamber is also effective.42 This cylindrical, inflatable pressure bag can simulate descent of over 1,500 m.
Once evacuated to a medical facility, the patient should be placed on high-flow oxygen with a nonrebreather mask. A 10-mg loading dose of dexamethasone may be given intravenously or intramuscularly, depending on available access. Intubation may be required, either for airway control or if there is significant coexisting HAPE. For obtunded patients, a Foley catheter should be placed for bladder decompression. In an effort to reduce intracranial pressure, hyperventilation (following intubation) and hypertonic saline with diuresis have been used for patients with HACE; however, no controlled studies exist to suggest either of these techniques increase survival or improve neurologic outcome. Summary recommendations for treatment of HACE are listed in Table 54.2.
TABLE 54.2 Treatment Strategies for HACE
CONCLUSION
HAPE and HACE are medical emergencies that require prompt clinical recognition. Dyspnea at rest is an early sign of HAPE, while ataxia is an important indicator of HACE. Treatment for all altitude emergencies includes descent and oxygen; however, pharmacologic treatment strategies and judicious supportive care may also be necessary.
LITERATURE TABLE

CI, confidence interval; OR, odds ratio.
1.Welling KK, et al. Effect of prolonged alveolar hypoxia on pulmonary arterial pressure and segmental vascular resistance. J Appl Physiol. 1993;75:1194–1200.
2.Bartsch P, et al. Prevention of high-altitude pulmonary edema by nifedipine. N Engl J Med. 1991;325(18):1284–1289.
3.Hultgren HN, et al. Physiologic studies of pulmonary edema at high altitude. Circulation. 1964;29:393–408.
4.Grunig E, et al. Stress Doppler echocardiography for identification of susceptibility to high altitude pulmonary edema + AFs-In Process Citation + AF0. J Am Coll Cardiol. 2000;35:980–987.
5.Dawson CA, Linehan JH, Bronowski TA. Pressure and flow in the pulmonary vascular bed. In: Weir KT, Reeves JT, eds. Pulmonary Vascular Physiology and Pathophysiology. New York, NY: Marcel Dekker; 1989:51–105.
6.Hultgren HN. High-altitude pulmonary edema: current concepts. Annu Rev Med. 1996;47:267–284.
7.West JB, et al. Stress failure in pulmonary capillaries. J Appl Physiol. 1991;70:1731–1742.
8.Sophocles AM. High-altitude pulmonary edema in Vail, Colorado, 1975–1982. West J Med. 1986;144:569–573.
9.Reeves JT, et al. Seasonal variation in barometric pressure and temperature in Summit County: effect on altitude illness. In: Sutton JR, Houston CS, Coates G, eds. Hypoxia and Molecular Medicine. Burlington, VT: Queen City Press; 1993.
10.Nuri M, Khan M, Quraishi M. High altitude pulmonary edema. Response to exercise and cold on systemic and pulmonary vascular beds. J Pak Med Assoc. 1988;38:211–217.
11.Yu-Jing S, et al. Endothelial nitric oxide synthase gene polymorphisms associated with susceptibility to high altitude pulmonary edema in Chinese railway construction workers at Qinghai-Tibet over 4 500 meters above sea Level. Chin Med Sci J. 2010;25(4):215–222.
12.Hanaoka M, et al. Association of high-altitude pulmonary edema with the major histocompatibility complex. Circulation. 1998;97(12):1124–1128.
13.Durmowicz AG, et al. Inflammatory processes may predispose children to high-altitude pulmonary edema. J Pediatr. 1997;130(5):838–840.
14.Rios B, Driscoll DJ, McNamara DG. High-altitude pulmonary edema with absent right pulmonary artery. Pediatrics. 1985;75:314–317.
15.Basnyat B, et al. Disoriented and ataxic pilgrims: an epidemiological study of acute mountain sickness and high-altitude cerebral edema at a sacred lake at 4300 m in the Nepal Himalayas. Wilderness Environ Med. 2000;11(2):89–93.
16.Hall DP, Duncan K, Baillie JK. High altitude pulmonary oedema. J R Army Med Corps. 2011;157(1):68–72.
17.Sutton JR, Coates G, Houston CS. Hypoxia and mountain medicine: proceedings of the 7th International Hypoxia Symposium, held at Lake Louise, Canada, February 1991. Advances in the Biosciences. 1st ed. Oxford, NY: Pergamon Press; 1992:xi, 330.
18.Viswanathan R, et al. Further studies on pulmonary oedema of high altitude. Respiration. 1978;36:216–222.
19.Scherrer U, et al. Inhaled nitric oxide for high-altitude pulmonary edema. N Engl J Med. 1996;334:624–629.
20.Marticorena E, Hultgren HN. Evaluation of therapeutic methods in high altitude pulmonary edema. Am J Cardiol. 1979;43:307–312.
21.Zafren K, Reeves JT, Schoene R. Treatment of high-altitude pulmonary edema by bed rest and supplemental oxygen. Wilderness Environ Med. 1996;7(2):127–132.
22.Freeman K, Shalit M, Stroh G. Use of the Gamow Bag by EMT-basic park rangers for treatment of high-altitude pulmonary edema and high-altitude cerebral edema. Wilderness Environ Med. 2004;15(3):198–201.
23.Chauca D, Bligh J. An additive effect of cold exposure and hypoxia on pulmonary artery pressure in sheep. Res Vet Sci. 1976;21:123–124.
24.Oelz O, et al. Nifedipine for high altitude pulmonary edema. Lancet. 1989;2:1241–1244.
25.Maggiorini M, et al. Both tadalafil and dexamethasone may reduce the incidence of high-altitude pulmonary edema: a randomized trial. Ann Intern Med. 2006;145(7):497–506.
26.Swenson ER, Maggiorini M. Salmeterol for the prevention of high-altitude pulmonary edema. N Engl J Med. 2002;347(16):1282–1285; author reply 1282–1285.
27.Schoene RB, et al. High altitude pulmonary edema and exercise at 4400 meters on Mt. McKinley: effect of expiratory positive airway pressure. Chest. 1985;87:330–333.
28.Koch RO, et al. A successful therapy of high-altitude pulmonary edema with a CPAP helmet on Lenin Peak. Clin J Sport Med. 2009;19(1):72–73.
29.Mosso A. Life of Man in the High Alps. London, England: T Fisher Unwin; 1898.
30.Dickinson JG. High altitude cerebral edema: cerebral acute mountain sickness. Semin Respir Med. 1983;5:151–158.
31.Gallagher SA, Hackett PH. High-altitude illness. Emerg Med Clin North Am. 2004;22(2):329–355, viii.
32.Hackett PH, Rennie ID, Levine HD. The incidence, importance, and prophylaxis of acute mountain sickness. Lancet. 1976;2:1149–1154.
33.Hochstrasser J, Nanzer A, Oelz O. Das Hoehenoedem in den Schweizer Alpen. Schweiz Med Wschr. 1986;116:866–873.
34.Ri-Li G, et al. Obesity: associations with acute mountain sickness. Ann Intern Med. 2003;139:253–257.
35.Sutton JR, Lassen N. Pathophysiology of acute mountain sickness and high altitude pulmonary oedema: an hypothesis. Bull Eur Physiopathol Respir. 1979;15:1045–1052.
36.Paralikar SJ, Paralikar JH. High-altitude medicine. Ind J Occup Environ Med. 2010;14(1):6–12.
37.Hackett PH, Roach RC. High altitude cerebral edema. High Alt Med Biol. 2004;5(2):136–146.
38.Milledge JS, West JB, Schoene RB. High Altitude Medicine and Physiology. 4th ed. Hodder Arnold, London; 2007.
39.Houston CS, Dickinson JG. Cerebral form of high altitude illness. Lancet. 1975;2:758–761.
40.Hackett PH, et al. High-altitude cerebral edema evaluated with magnetic resonance imaging: clinical correlation and pathophysiology. JAMA. 1998;280(22):1920–1925.
41.Luks AM, et al. Wilderness Medical Society consensus guidelines for the prevention and treatment of acute altitude illness. Wilderness Environ Med. 2010;21(2):146–155.
42.Zafren K. Gamow bag for high-altitude cerebral oedema. Lancet. 1998;352(9124):325–326.