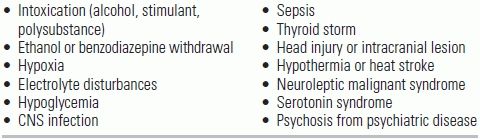
TABLE 57.1 Differential Diagnosis for Acute Undifferentiated Agitation
BACKGROUND
Emergency physicians are frequently called upon to provide care to agitated, violent, and combative patients. These patients pose a significant safety threat to themselves and to the providers who care for them; furthermore, their agitation can impede the diagnostic workup and delay potentially lifesaving care. Chemical sedation is often necessary in order to ensure patient and provider safety and to expedite the diagnostic workup.
Acute undifferentiated agitation can be classified broadly into medical, toxicologic, or psychiatric etiologies (Table 57.1). It may present with a wide spectrum of severity; patients may be agitated but cooperative or dangerously combative. Excited delirium syndrome (ExDS), also referred to as agitated delirium, is a recently-recognized syndrome that represents the most severe form of agitation. ExDS can be precipitated by almost any psychiatric or medical condition, drug, toxin, or biochemical or physiologic alteration.1 Patients with ExDS are typically young males; they present in a hyperadrenergic autonomic state characterized by hyperthermia, tachycardia, insensitivity to pain, and superhuman strength.1 ExDS is associated with an increase in mortality and represents a true medical emergency that requires immediate attention.
TABLE 57.1 Differential Diagnosis for Acute Undifferentiated Agitation
MANAGEMENT GUIDELINES
Although sedation is a critical component of the management of acute agitation in the emergency department (ED), health care professionals should be mindful that these patients are experiencing personal, psychological, and medical crises and that they deserve respect and dignity. Prior to administering sedative agents, de-escalation techniques both verbal and environmental (i.e., turning the lights down, minimizing ambient noise) should be attempted. Such techniques may fail in the severely agitated (or combative) patients, some of whom may require physical restraint prior to chemical sedation. If physical restraint is used, it should be for the shortest time possible; positioning a restrained patient in the prone position should be avoided as this has been associated with increased mortality.2
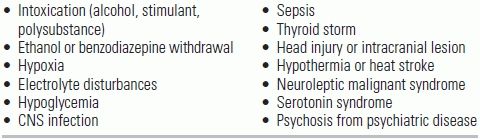
Benzodiazepines and antipsychotic medications are the most commonly-used pharmacologic agents for the sedation of the agitated patient (Table 57.2). Although intravenous (IV) administration of these medications allows for rapid onset, this dosing route may be challenging and unsafe in the combative and uncooperative patient. For this reason, intramuscular (IM) formulations are often used initially until an IV can be established. Oral administration of benzodiazepines and antipsychotics is rarely given in acutely agitated patients, but can be considered in those who are cooperative.3
TABLE 57.2 Agents for Acute Undifferentiated Agitation in the Emergency Department
IV, intravenous; IM, intramuscular; PO, oral. Consider using lower doses for elderly patients. Adapted from Vilke GM, et al. J Forensic Leg Med. 2012;19:117–121; and Wilson MP, et al. West J Emerg Med. 2012;13:26–34.
MEDICATIONS USED FOR SEDATION OF THE SEVERELY AGITATED EMERGENCY DEPARTMENT PATIENT
Benzodiazepines have a long history of use in the treatment of agitation. This drug class binds to the gamma–aminobutyric acid β (GABA-β)-subtype receptor—the primary inhibitory neurotransmitter of the central nervous system—and exerts sedative, hypnotic, anxiolytic, anticonvulsant, amnestic, and muscle relaxant effects.4 Lorazepam and midazolam are the most commonly used and best studied benzodiazepines for the management of acute agitation because they have predictable onset of action when given in the IM form. Diazepam, chlordiazepoxide, and clonazepam are infrequently used in the acute management of agitation because they have longer half-lives and have inconsistent IM absorption.5 Midazolam has a faster onset and shorter duration of action than lorazepam, especially when given IM; however, patients receiving midazolam may require more frequent redosing because of its shorter half-life.6,7
The dosing of IM and IV midazolam and lorazepam is listed in Table 57.2. Protocols recommend dosing midazolam 2 to 5 mg IV every 5 to 10 minutes.8,9 Serial dosing, however, must be used cautiously, as it may increase the risk of respiratory depression, which was reported to be as high as 13% with use of this protocol.9 Fortunately, this serious side effect is usually transient;5,9,10 it may, however, be more common in patients with ethanol or opiate intoxication and so should be used with caution in this population. Additional side effects of benzodiazepines include ataxia, dizziness, and decreased blood pressure, especially in patients who are hypovolemic.
Benzodiazepines should be reserved for patients whose agitation is severe and who present an immediate threat to themselves or others. They may also be useful in patients who are withdrawing from ethanol or benzodiazepines or those who have taken stimulants such as amphetamines or cocaine.11 For agitated patients with delirium, the risks and benefits of benzodiazepine use, which can exacerbate delirium, must be carefully weighed.12
Typical, or first-generation, antipsychotics have a long history of use in the treatment of agitation. Haloperidol and droperidol are high-potency butyrophenone antipsychotics that primarily antagonize the D2 dopamine receptor. Despite their side effects (discussed below), and the availability of newer generation atypical antipsychotics, haloperidol and droperidol are still widely used for the management of agitation. They have relatively little effect on hemodynamics13 and can be given orally, intramuscularly, and intravenously.
Although haloperidol is more commonly used for agitation, droperidol offers several advantages. Droperidol may have a more rapid onset of action and a shorter half-life when given intramuscularly.14 In one randomized controlled study comparing droperidol 5 mg IM with haloperidol 5 mg IM, droperidol achieved more rapid control of the patient's agitation without any relative increase in side effects.15 Compared with IM haloperidol, IM droperidol may also last longer and be less likely to require repeat dosing.16 The dosages for haloperidol and droperidol are listed in Table 57.2. Serial dosing (i.e., every 5 to 10 minutes) can be required to achieve adequate sedation; total doses exceeding 20 mg are associated with increased side effects and have limited incremental benefit.6,17,18
One of the most feared side effects of both droperidol and haloperidol is QT prolongation and torsades de pointes, especially when theses drugs are given intravenously and at higher doses.19,20 Because of reports of cardiac death secondary to torsades de pointes, the FDA issued a black box warning on droperidol in 2001 that has curtailed its use in the clinical setting. This warning is not without controversy. Many have argued that the adverse events observed with droperidol were at doses much higher than typically used for agitation. Several studies have also shown droperidol to be safe for use at doses typically administered for agitation.21,22 Regardless, special care should be taken when using either haloperidol or droperidol in patients with a known prolonged QT interval, who take other QT prolonging medications, or have medical conditions that cause QT prolongation. A 12-lead electrocardiogram should be obtained if possible prior to IV administration. If the patient's QTc interval is >500 milliseconds, the IV route should be avoided.
Haloperidol and droperidol can also cause extrapyramidal symptoms (EPS)—including acute dystonic reactions, akathisia, and pseudoparkinsonism—due to their blockade of dopamine receptors in the basal ganglia. Because haloperidol and droperidol have relatively little anticholinergic activity, EPS occurs in up to 20% of patients treated with these medications.23 Anticholinergic agents such as diphenhydramine (25 to 50 mg), benztropine (1 to 2 mg), and promethazine (25 to 50 mg) are usually effective in treating acute EPS, though severe akathisia may require benzodiazepines.
Droperidol and haloperidol have also been shown to decrease seizure threshold and should be used with caution in patients with a history of seizures. Finally, neuroleptic malignant syndrome (NMS) is a rare but potentially fatal complication of these medications.
Olanzapine, risperidone, aripiprazole, and ziprasidone have been extensively evaluated for the treatment of acute agitation in the psychiatric patients; their role in the ED patient with undifferentiated agitation is less clear. Most atypical antipsychotics have oral and IM formulations, although the IM formulation may be less readily available in the ED.
Compared to typical antipsychotics, second-generation, or atypical, antipsychotics have a favorable side effect profile. Atypical antipsychotics also antagonize the dopamine D2 receptor, but unlike typical psychotics, they also antagonize the serotonin 5-HT2, histamine, alpha, and muscarinic receptors to variable degrees. They are less likely to cause oversedation, EPS, QT prolongation, and vital sign abnormalities. Some concerns, however, have been raised about hypotension and oxygen desaturation caused by parenteral olanzapine used in combination with benzodiazepines, especially in patients intoxicated with ethanol.25–27 Similar to typical antipsychotics, NMS has also been reported in patients receiving atypical antipsychotics.28
CHOICE OF MEDICATION FOR SEDATION OF THE AGITATED PATIENT
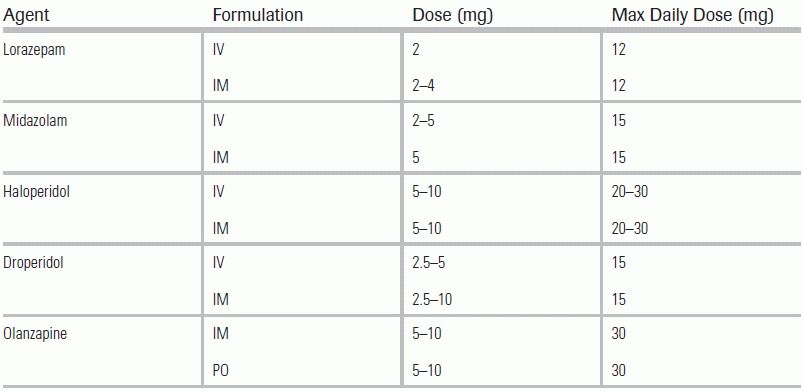
The choice of medication for sedating the agitated ED patient can depend on how quickly sedation needs to be achieved and on the desired length of sedation. Several randomized controlled trials of typical antipsychotics have explored how they compare with benzodiazepines as monotherapy for controlling agitation. In one study, 111 ED patients with severe agitation were treated with either midazolam 5 mg IM, lorazepam 2 mg IM, or haloperidol 5 mg IM; midazolam was reported as having the shortest time to adequate sedation and shorter times to awakening compared with haloperidol and lorazepam.7 A second study compared midazolam 5 gm IV with droperidol 5 mg IV in 153 agitated ED patients and allowed these medications to be redosed every 5 minutes until adequate sedation was achieved.8 The study observed that more patients in the midazolam group achieved adequate sedation within 5 minutes (45% vs. 17%), suggesting that midazolam may have faster onset of action than droperidol. Both medications had side effects; there was a trend toward increased respiratory depression in the midazolam group (4.1% vs. 0.0%) and dystonic reactions in the droperidol group (0.0% vs. 3.8%). A third study compared droperidol IV (2.5 mg for patients <50 kg, 5.0 mg for patients >50 kg) with lorazepam IV (2.0 mg for patients <50 kg, 4.0 mg for patients >50 kg) in 202 agitated ED patients; repeat dosing was allowed in 30 minutes.28 Though sedation was similar for both medications at 5 minutes, a larger proportion of the droperidol group achieved adequate sedation at subsequent time intervals. In addition, more patients in the lorazepam arm required redosing compared with the droperidol arm. No major adverse events occurred in either group.
The role of atypical antipsychotics in the management of the acutely agitated ED patient is less well established. To date, most research has been conducted in patients whose agitation has a psychiatric cause; in this population, atypical antipsychotics such as olanzapine, aripiprazole, and risperidone are as effective as haloperidol and show a lower incidence of EPS.29–31 Only one randomized controlled trial has evaluated the role of atypical antipsychotic medications in the ED patient with undifferentiated agitation. This study randomized 144 agitated ED patients to receive midazolam 5 mg IM, droperidol 5 mg IM, or ziprasidone 20 mg IM.17 Only 39% of the ziprasidone group achieved adequate sedation within 15 minutes compared to 69% of the midazolam group and 60% of the droperidol group.17 As result, IM ziprasidone is not recommended for rapid sedation of the agitated patient.
In the agitated patient with a psychiatric etiology, several studies have demonstrated that a butyrophenone in combination with a benzodiazepine results in improved sedation with less EPS than monotherapy.23,32,33 In ED patients, the role of combination therapy in the patient with undifferentiated agitation remains unclear. One randomized controlled trial compared droperidol 10 mg IM, midazolam 10 mg IM, and the combination of droperidol 5 mg IM + midazolam 5 mg IM in 91 violent and agitated ED patients.34 The study did not observe any differences in the duration of agitation between the three groups. However, the midazolam group required more redosing to maintain adequate sedation; this group also experienced a nonsignificant tendency to develop oxygen desaturations, especially in patients with ethanol intoxication. A second randomized controlled trial compared midazolam IV alone with midazolam IV used in conjunction with either droperidol 5 mg IV or olanzapine 5 mg IV.24 The combination of droperidol + midazolam or olanzapine + midazolam was associated with significantly shorter times to adequate sedation compared with midazolam alone. More patients in the midazolam-only group required additional sedation within 60 minutes. There were no differences in adverse events or ED length of stay. Several retrospective studies, however, raise concerns that combining olanzapine with a benzodiazepine may result in lower oxygen saturations when given to patients with ethanol intoxication.35,36 As a result, additional research is needed to determine the safety and efficacy of combining antipsychotics and benzodiazepine in the treatment of agitation in the ED.
SUMMARY RECOMMENDATIONS
Based on the abovementioned studies, the following general conclusions can be made:
Ketamine is a dissociative anesthetic that antagonizes the N-methyl-D-aspartate receptor. It is commonly used in the ED for procedural sedation and induction of intubation and minimally affects respiratory drive. Several case reports have shown that ketamine may be useful in the treatment of severe agitation refractory to antipsychotics or benzodiazepines.37–39
Dexmedetomidine is an alpha-2 agonist sedative that produces minimal respiratory depression; an advantage of this agent is that patients remain easily arousable, even while their agitation is adequately controlled. The evidence supporting its use is limited to case reports in patients with delirium tremens.40 Further research is needed to establish the role and safety of both ketamine and dexmedetomidine in treating agitation in the ED.
CHOICE OF SEDATIVES BASED UPON CAUSE OF AGITATION
Recently, the American Association for Emergency Psychiatry released a consensus statement on the management of agitation in the ED including specific types of agitation that may warrant specific sedatives.11 In a busy ED, however, it is often challenging to determine the cause of agitation, especially early in a patient's course. With this caveat, for agitation secondary to stimulants, benzodiazepines are considered the first-line agent. Benzodiazepines should also be used for agitation secondary to alcohol and benzodiazepine withdrawal. For alcohol-intoxicated patients, benzodiazepines should be avoided because of increased risk of respiratory depression; haloperidol or a second-generation antipsychotic should be used instead. For agitation secondary to a psychiatric illness, antipsychotics are preferred over benzodiazepines, and atypical antipsychotics are preferred over typical antipsychotics. Benzodiazepines may be used if the initial dose of antipsychotic medications is insufficient to control agitation. For agitation secondary to hyperactive delirium not caused by a stimulant, ethanol withdrawal, or benzodiazepine withdrawal, haloperidol is recommended if immediate pharmacologic control is required. Benzodiazepines can exacerbate the delirium component of hyperactive delirium and should be avoided in those instances.41
CONCLUSION
The management of severe acute agitation in the ED is challenging and requires a coordinated effort between emergency physicians, nurses, and staff. When non-pharmacological methods fail to calm the patient, intervention with chemical sedation can to ensure patient and staff safety and facilitate the diagnostic workup. Familiarity with the summary recommendations provided in this chapter can help guide selection of the most appropriate sedative agent.
LITERATURE TABLE
RCT, randomized control trials; IV, intravenous; IM, intramuscular; ED, emergency department; 95% CI, 95% confidence intervals; LOS, length of stay.
1.Vilke GM, DeBard ML, Chan TC, et al. Excited Delirium Syndrome (ExDS): defining based on a review of the literature. J Emerg Med. 2012;43:897–905.
2.Chan TC, Vilke GM, Neuman T, et al. Restraint position and positional asphyxia. Ann Emerg Med. 1997;30:578–586.
3.Gault TI, Gray SM, Vilke GM, et al. Are oral medications effective in the management of acute agitation? J Emerg Med. 2012;43:854–859.
4.Mihic SJ, Harris RA. Chapter 17. Hypnotics and sedatives. In: Goodman LS, Brunton LL, Chabner B, et al., eds. Goodman and Gilman's the Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill; 2011.
5.Battaglia J: Pharmacological management of acute agitation. Drugs. 2005;65:1207–1222.
6.Rund DA, Ewing JD, Mitzel K, et al. The use of intramuscular benzodiazepines and antipsychotic agents in the treatment of acute agitation or violence in the emergency department. J Emerg Med. 2006;31:317–324.
7.Nobay F, Simon BC, Levitt MA, et al. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004;11:744–749.
8.Knott JC, Taylor DM, Castle DJ. Randomized clinical trial comparing intravenous midazolam and droperidol for sedation of the acutely agitated patient in the emergency department. Ann Emerg Med. 2006;47:61–67.
9.Spain D, Crilly J, Whyte I, et al. Safety and effectiveness of high-dose midazolam for severe behavioural disturbance in an emergency department with suspected psychostimulant-affected patients. Emerg Med Australas. 2008;20:112–120.
10.Alexander J, Tharyan P, Adams C, et al. Rapid tranquillisation of violent or agitated patients in a psychiatric emergency setting. Pragmatic randomised trial of intramuscular lorazepam v. haloperidol plus promethazine. Br J Psychiatry. 2004;185:63–69.
11.Wilson MP, Pepper D, Currier GW, et al. The psychopharmacology of agitation: consensus statement of the American association for emergency psychiatry project Beta psychopharmacology workgroup. West J Emerg Med. 2012;13:26–34.
12.Breitbart W, Marotta R, Platt MM, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. Am J Psychiatry. 1996;153:231–237.
13.Foster S, Kessel J, Berman ME, et al. Efficacy of lorazepam and haloperidol for rapid tranquilization in a psychiatric emergency room setting. Int Clin Psychopharmacol. 1997;12:175–179.
14.Cressman WA, Plostnieks J, Johnson PC. Absorption, metabolism and excretion of droperidol by human subjects following intramuscular and intravenous administration. Anesthesiology. 1973;38:363–369.
15.Thomas H Jr, Schwartz E, Petrilli R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21:407–413.
16.Resnick M, Burton BT. Droperidol vs. haloperidol in the initial management of acutely agitated patients. J Clin Psychiatry. 1984;45:298–299.
17.Martel M, Sterzinger A, Miner J, et al. Management of acute undifferentiated agitation in the emergency department: a randomized double-blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med. 2005;12:1167–1172.
18.Baldessarini RJ, Cohen BM, Teicher MH. Significance of neuroleptic dose and plasma level in the pharmacological treatment of psychoses. Arch Gen Psychiatry. 1988;45:79–91.
19.Lawrence KR, Nasraway SA. Conduction disturbances associated with administration of butyrophenone antipsychotics in the critically ill: a review of the literature. Pharmacotherapy. 1997;17:531–537.
20.Hassaballa HA, Balk RA. Torsade de pointes associated with the administration of intravenous haloperidol: a review of the literature and practical guidelines for use. Expert Opin Drug Saf. 2003;2:543–547.
21.Chase PB, Biros MH. A retrospective review of the use and safety of droperidol in a large, high-risk, inner-city emergency department patient population. Acad Emerg Med. 2002;9:1402–1410.
22.Shale JH, Shale CM, Mastin WD. A review of the safety and efficacy of droperidol for the rapid sedation of severely agitated and violent patients. J Clin Psychiatry. 2003;64:500–505.
23.Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective, double-blind, emergency department study. Am J Emerg Med. 1997;15:335–340.
24.Chan EW, Taylor DM, Knott JC, et al. Intravenous droperidol or olanzapine as an adjunct to midazolam for the acutely agitated patient: a multicenter, randomized, double-blind, placebo-controlled clinical trial. Ann Emerg Med. 2013;61:72–81.
25.Zacher JL, Roche-Desilets J. Hypotension secondary to the combination of intramuscular olanzapine and intramuscular lorazepam. J Clin Psychiatry. 2005;66:1614–1615.
26.Wilson MP, Chen N, Vilke GM, et al. Olanzapine in ED patients: differential effects on oxygenation in patients with alcohol intoxication. Am J Emerg Med. 2012;30:1196–1201.
27.Marder SR, Sorsaburu S, Dunayevich E, et al. Case reports of postmarketing adverse event experiences with olanzapine intramuscular treatment in patients with agitation. J Clin Psychiatry. 2010;71:433–441.
28.Richards JR, Derlet RW, Duncan DR. Chemical restraint for the agitated patient in the emergency department: lorazepam versus droperidol. J Emerg Med. 1998;16:567–573.
29.Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose–response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psychiatry. 2002;59:441–448.
30.Hsu WY, Huang SS, Lee BS, et al. Comparison of intramuscular olanzapine, orally disintegrating olanzapine tablets, oral risperidone solution, and intramuscular haloperidol in the management of acute agitation in an acute care psychiatric ward in Taiwan. J Clin Psychopharmacol. 2010;30:230–234.
31.Tran-Johnson TK, Sack DA, Marcus RN, et al. Efficacy and safety of intramuscular aripiprazole in patients with acute agitation: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2007;68:111–119.
32.Garza-Trevino ES, Hollister LE, Overall JE, et al. Efficacy of combinations of intramuscular antipsychotics and sedative-hypnotics for control of psychotic agitation. Am J Psychiatry. 1989;146:1598–1601.
33.Yildiz A, Sachs GS, Turgay A. Pharmacological management of agitation in emergency settings. Emerg Med J. 2003;20:339–346.
34.Isbister GK, Calver LA, Page CB, et al. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioral disturbance: the DORM study. Ann Emerg Med. 2010;56(4):3920491.e1.
35.Wilson MP, MacDonald K, Vilke GM, et al. A comparison of the safety of olanzapine and haloperidol in combination with benzodiazepines in emergency department patients with acute agitation. J Emerg Med. 2012;43:790–797.
36.Wilson MP, MacDonald K, Vilke GM, et al. Potential complications of combining intramuscular olanzapine with benzodiazepines in emergency department patients. J Emerg Med. 2012;43:889–896.
37.Roberts JR, Geeting GK. Intramuscular ketamine for the rapid tranquilization of the uncontrollable, violent, and dangerous adult patient. J Trauma. 2001;51:1008–1010.
38.Hick JL, Ho JD. Ketamine chemical restraint to facilitate rescue of a combative “jumper”. Prehosp Emerg Care. 2005;9:85–89.
39.Ho JD, Smith SW, Nystrom PC, et al. Successful management of excited delirium syndrome with prehospital ketamine: two case examples. Prehosp Emerg Care. 2013;17:274–279.
40.Muzyk AJ, Fowler JA, Norwood DK, et al. Role of alpha2-agonists in the treatment of acute alcohol withdrawal. Ann Pharmacother. 2011;45:649–657.
41.Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing. 2011;40:23–29.