61
ED Evaluation of the Critically Ill Patient
Geoffrey K. Lighthall and John E. Arbo
BACKGROUND
Risk assessment and disposition of the critically ill patient is guided by impression of clinical trajectory as well as presumed diagnosis. While diagnosis is often based on historical information and on physician experience and intuition, the clinical trajectory is dictated by the state of tissue perfusion and the patient's ability to compensate for physiologic perturbations. For example, a patient with a positive troponin, ST changes, and a mean pressure of 65 mm Hg may be having a simple myocardial infarction, while another patient with similar findings may be in cardiogenic shock. Similarly, low blood pressure (BP) in one patient may result from therapeutic lowering of vascular tone (e.g., heart failure), while the same BP in a different individual may signify distributive shock. Differentiating these possibilities enables appropriate disposition and treatment and is essential to the practice of acute care medicine. This chapter focuses on the pathophysiologic roots of organ dysfunction, and demonstrates how an understanding of these principles permits efficient identification of likely diagnoses, institution of timely therapy, and safe patient disposition. Fluency with these principles also enhances communication with other health care providers.
PATHOPHYSIOLOGY OF SHOCK AND ORGAN DYSFUNCTION
Organ dysfunction arising from critical illness can be traced to abnormalities in either one or both of the following physiologic relationships:
1.The autoregulatory curve describing the relationship between organ blood flow and mean arterial pressure (MAP)1
2.The relationship between the supply of oxygen to tissues (oxygen delivery or DO2) and consumption (demand or VO2)2–4
Evaluating these two key homeostatic relationships—MAP/blood flow and oxygen supply/demand (VO2/DO2)—is essential in any patient exhibiting distress, organ dysfunction, or hemodynamic instability. Failure to do so commonly results in misdiagnosis and delayed recognition of clinical deterioration.5–7
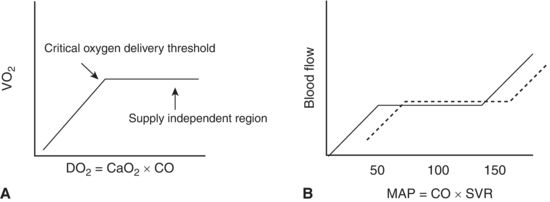
Oxygen consumption or demand (VO2) is determined by physical activity, temperature, and body mass, while oxygen delivery (DO2) is the product of cardiac output (CO) and the content of arterial oxygen (CaO2). CO is in turn the product of stroke volume (SV) and heart rate (HR), while arterial oxygen content is primarily determined by hemoglobin concentration and saturation. The graphic representation of these relationships is presented in Figure 61.1. For both curves, the down-sloping limb on the left indicates a region where the patient is at risk for organ failure. Specifically, in curve A, DO2 below the critical threshold signifies a loss of physiologic reserve and a transition to anaerobic metabolism; in curve B, a MAP below the autoregulatory threshold signifies the inability to maintain a constant blood flow to metabolically active regions with an organ. Appreciating the implication of these curves is essential to understanding the impact of different categories of shock.
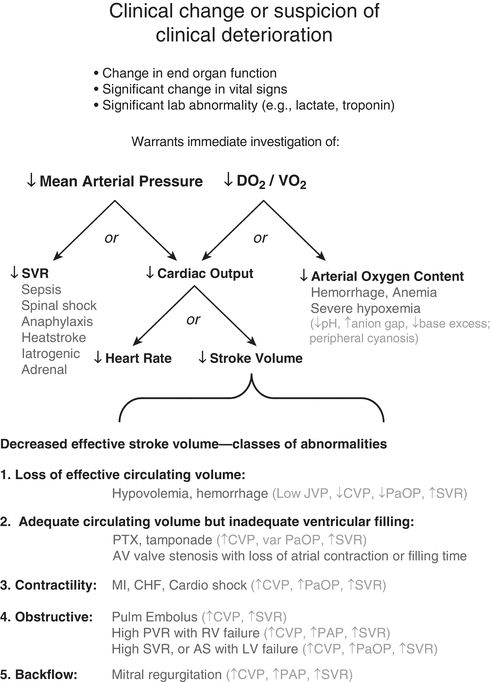
For example, the low MAP typically seen in distributive shock becomes life threatening when vascular resistance is unable to maintain MAP above the autoregulatory threshold. Cardiogenic shock may have borderline or low MAP but is differentiated from a simple myocardial infarction by a loss in CO to levels insufficient to meet tissue oxygen demand. Hemorrhagic shock involves both a loss in hemoglobin content and a related loss in ventricular volume—and hence a loss in CO. In severe hemorrhage, these “two hits” on DO2 can result in huge derangements in oxidative metabolism. The hemodynamic indices associated with the prototypic shock states are displayed in Table 61.1. As will be shown throughout the chapter, detection of abnormalities in either maintenance of MAP or DO2 is followed by further differentiation of these parameters as described in Figure 61.2.
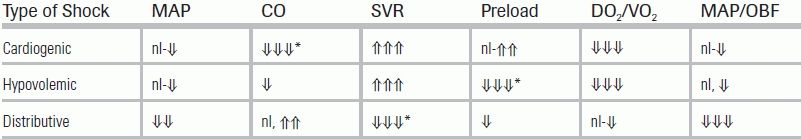
TABLE 61.1 Typical Hemodynamic Changes Associated with Three Accepted Categories of Shock
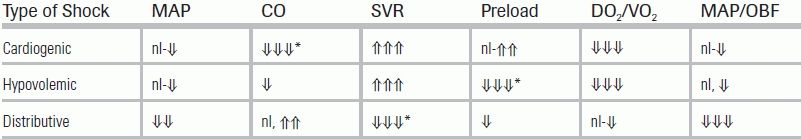
Arrows show degree of change from baseline in mean arterial pressure (MAP), cardiac output (CO), systemic vascular resistance (SVR), and cardiac preload. Additionally, alterations in the relationship between oxygen delivery and demand (DO2/VO2) and mean arterial pressure and organ blood flow (MAP/OBF) are indicated. The asterisk indicates the primary abnormality associated with each shock state.
nl, normal range, arrows showing increases or decreases.
EVALUATION OF THE ADEQUACY OF BLOOD PRESSURE
From classic studies, we know that the normotensive brain autoregulates at MAPs between 50 and 150 mm Hg. This corresponds to the flat portion of the curve in Figure 61.1B. A baseline hypertensive patient would operate on a right-shifted antiregulatory curve and may not have normal organ perfusion at mean pressures <65 to 70 mm Hg. Retrospective analyses of trauma registries support the existence of age-related relative hypotension8 and have demonstrated poorer outcomes in these individuals at MAP values previously considered normal.9 Based on an aggregate data on patients with septic shock, studies propose that previously normotensive patients should be considered hypotensive if, after receiving 30 mL/kg crystalloid infusion, they still exhibit a decreased systolic pressure (a drop >40 mm Hg) or a decrease in MAP >30 mm Hg.10 Determination of adequacy of MAP, therefore, often depends upon understanding a patient's usual BP range and the magnitude of acute change. Review of vital signs obtained in the outpatient setting or preoperative visit are helpful in this regard. Patients without clinic notes and charts may be more difficult to evaluate, but the patient history, as well as the presence of renal disease or left ventricular hypertrophy, can provide clues. Pressures noted on admission or obtained in the emergency department are not likely to reflect a patient's true baseline.
EVALUATION OF THE ADEQUACY OF OXYGEN DELIVERY RELATIVE TO DEMAND (VO2/DO2)
In many cases, a critically ill patient may arrive at the ED with a BP close to his or her baseline value. It is important to remember that for these patients, evaluation of DO2/VO2 is still required. The key question surrounding the status of this relationship is whether the patient's oxygen extraction is abnormally high (a falling DO2 for a given VO2—moving right to left on that flat portion of the cure in Fig. 61.1A) or whether anaerobic metabolism is already present (an inadequate DO2 for a given VO2—the left side downward slope in Fig. 61.1A). Metabolic acidosis, an elevated anion gap, and elevated lactate levels are associated with an oxygen debt and subsequent anaerobic metabolism and can be rapidly identified with point-of-care blood gas analysis. A fall in DO2 and subsequent abnormal increase in oxygen extraction may be identified by a central venous oxyhemoglobin saturation of <70%. Typically, perturbations in the economy of oxygen extraction result from impaired delivery.
MAKING THE DIAGNOSIS
Evaluation of Low Blood Pressure
A low MAP results from either a low CO or low systemic vascular resistance (SVR). Thus, the etiology of a low MAP can often be inferred by an exam that differentiates between high and low SVR. Cold extremities, weak pulses with narrow pulse pressures, and delayed capillary refill suggest a low CO and a high SVR. Warm extremities with brisk capillary refill and bounding pulses indicate a normal or high CO and a low SVR.
Low MAP and physical exam findings consistent with low vascular tone (i.e., low SVR) are suggestive of distributive shock. In these patients, attention centers on differentiating neurologic injury from the other etiologies of low vascular tone, such as anaphylaxis and sepsis (Fig. 61.2).
Evaluation of Low Oxygen Delivery
Low MAP and physical exam findings consistent with a high SVR and low CO (i.e., increased vascular tone, cool extremities) should prompt the provider to consider the determinants of CO—specifically either a low HR or diminished SV. A key point differentiating causes of low SV is the overall volume status of the patient. Low SV can result from frank hypovolemia as in hemorrhage and severe dehydration, or can exist in the setting of euvolemia or hypervolemia where the low SV results from precardiac obstruction of ventricular filling, poor pump function, postcardiac obstruction, or valvular regurgitation. With hypovolemia, central veins will be collapsed, and peripheral veins may be difficult to locate; findings of hypovolemia should prompt a search for sources of volume loss, particularly bleeding. Low SV from all other causes will be accompanied by normal to large central veins; enlarged central veins should prompt a thorough examination of the chest and echocardiographic examination of the heart. The use of transthoracic echocardiography is increasingly common in ICUs and EDs for focused assessment of these conditions.11,12 Figure 61.2 provides a systematic approach to the evaluation of the patient with evidence of clinical deterioration or the onset of organ dysfunction. The physiologic parameters incorporated into Figure 61.2 allow consideration of all possibilities for a given category of abnormality, which offers advantages in evaluation of the unstable patient.
Evaluation of Hemorrhage
In a patient in whom blood loss has occurred more than 30 minutes prior to laboratory analysis, interstitial-to-vascular fluid shifts will result in hemodilution and produce an accompanying drop in hematocrit. In this setting, the presence of an elevated lactate or evidence of an imbalance in DO2/VO2 would clearly be due to hemorrhage. In hemorrhage, physical exam findings include a weak pulse, narrow pulse pressure, delayed capillary refill, and cold extremities, which suggest that MAP is being maintained by abnormally high vascular resistance. With more rapid or immediate hemorrhage, isovolemic blood loss prior to fluid shifts will fail to reveal a depressed hematocrit, while still yielding findings of increased vascular tone and inadequate DO2. In the case of low CO suspected to be due to occult hemorrhage (e.g., a retroperitoneal bleed, contained aneurysm rupture, etc.), clinical assessment could still uncover the presence of hemorrhage through exam findings suggestive of a low SV (e.g., flat neck veins).
PROVIDING EMPIRIC THERAPY
Therapy for any shock state involves both targeted interventions as well as empiric resuscitation. The utility of a physiologic evaluation as presented here is its ability to direct therapy appropriate to the class of abnormality while more definitive diagnostic data are being obtained—thereby avoiding undesirable delays in patient care. A hypotensive patient with findings consistent with distributive shock will always require vasopressors and fluids. This intervention can safely take place while the possibilities of allergy and sepsis are investigated and, if present, treated. In a patient with evidence of low CO and compensatory vasoconstriction, the physiologic analysis might encourage use of inotropes and avoidance of additional vasopressors while possibilities of heart failure or outflow tract obstruction are investigated.
END POINTS OF RESUSCITATION
Much controversy exists regarding the desirable end points for resuscitation from shock.13–17 Rather than target specific numeric indices of DO2 and CO, a “bare minimum” goal should be to ensure that an adequate MAP has been restored and that DO2 is not limiting consumption. The concepts presented in this chapter provide a balanced and physiologic approach to achieving these resuscitative goals. From the determinants of MAP, one can see that a MAP that is disproportionately supported by a high vascular resistance will do so at the expense of CO, which can have disastrous consequences DO2. Similarly, optimization of SV and DO2 does not guarantee a MAP sufficient to maintain renal and other solid organ function; vasopressors to ensure an adequate SVR may be necessary and may help avoid fluid overload.18 To achieve these minimum goals, the Society of Critical Care Medicine19,20 recommends a target MAP of >65 mm Hg and the normalization of central venous oxygen saturation or lactate. Some individualization of the MAP goal may be indicated in patients with known hypertension.
As resuscitation proceeds, it is important to continually reexamine VO2/DO2 and adequacy of MAP. If these two physiologic relationships are revisited frequently, missed diagnoses (bleeding, myocardial infarction) and therapeutic mistakes (vasoconstrictors used instead of fluid) can be identified early. For example, in the case of a hypotensive patient given a vasopressor to elevate his or her MAP and subsequently noted to have a rising lactate and falling in pH, evidence would suggest that the initial perception of inadequate vascular tone was incorrect and that correction of MAP would be better served by augmenting CO rather than SVR.
CONCLUSION
The development of shock and organ dysfunction is not a certainty for most medical conditions. Patients progressing to shock are differentiated by the development of abnormalities in at least one of the following two physiologic relationships: (1) the relationship between oxygen supply and demand (DO2/VO2) and (2) the relationship between organ blood flow and MAP. Understanding the derivation of these relationships and their significance to overall organ function enables the provider to effectively implement the diagnostic and therapeutic approach outlined in this chapter. Adherence to this approach also ensures the provision of timely and appropriate care; it is comprehensive, efficient, allows prioritization of diagnostic studies, does not delay treatment, helps define end points of resuscitation, and provides a common physiology-based language for enhanced communication with other health care providers.
REFERENCES
1.Granger HJ, Guyton AC. Autoregulation of the total systemic circulation following destruction of the central nervous system in the dog. Circ Res. 1969;25(4):379–388.
2.Schumacker PT, Cain SM. The concept of a critical oxygen delivery. Intensive Care Med. 1987;13(4):223–229.
3.Shibutani K, Komatsu T, Kubal K, et al. Critical level of oxygen delivery in anesthetized man. Crit Care Med. 1983;11(8):640–643.
4.Bredle DL, Samsel RW, Schumacker PT, et al. Critical O2 delivery to skeletal muscle at high and low PO2 in endotoxemic dogs. J Appl Physiol. 1989;66(6):2553–2558.
5.Bristow PJ, Hillman KM, Chey T, et al. Rates of in-hospital arrests, deaths and intensive care admissions: the effect of a medical emergency team. Med J Aust. 2000;173(5):236–240.
6.Buist MD, Jarmolowski E, Burton PR, et al. Recognising clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care. A pilot study in a tertiary-care hospital. Med J Aust. 1999;171(1):22–25.
7.Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98(6):1388–1392.
8.Edwards M, Ley E, Mirocha J, et al. Defining hypotension in moderate to severely injured trauma patients: raising the bar for the elderly. Am Surg. 2010;76(10):1035–1038.
9.Eastridge BJ, Salinas J, McManus JG, et al. Hypotension begins at 110 mm Hg: redefining “hypotension” with data. J Trauma. 2007;63(2):291–297; discussion 297–9.
10.Marik PE, Lipman J. The definition of septic shock: implications for treatment. Crit Care Resusc. 2007;9(1):101–103.
11.Axler O. Evaluation and management of shock. Semin Respir Crit Care Med. 2006;27(3):230–240.
12.Vieillard-Baron A, Charron C, Chergui K, et al. Bedside echocardiographic evaluation of hemodynamics in sepsis: is a qualitative evaluation sufficient? Intensive Care Med. 2006;32(10):1547–1552.
13.Elliott DC. An evaluation of the end points of resuscitation. J Am Coll Surg. 1998;187(5):536–547.
14.Ivatury RR, Simon RJ, Islam S, et al. A prospective randomized study of end points of resuscitation after major trauma: global oxygen transport indices versus organ-specific gastric mucosal pH. J Am Coll Surg. 1996;183(2):145–154.
15.Gattinoni L, Brazzi L, Pelosi P, et al. A trial of goal-oriented hemodynamic therapy in critically ill patients. SvO2 Collaborative Group. N Engl J Med. 1995;333(16):1025–1032.
16.Shoemaker WC, Appel PL, Kram HB, et al. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94(6):1176–1186.
17.Hayes MA, Timmins AC, Yau EH, et al. Elevation of systemic oxygen delivery in the treatment of critically ill patients. N Engl J Med. 1994;330(24):1717–1722.
18.Liu YL, Prowle J, Licari E, et al. Changes in blood pressure before the development of nosocomial acute kidney injury. Nephrol Dial Transplant. 2009;24(2):504–511.
19.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377.
20.Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. 2008. Crit Care Med. 2008;36(1):296–327.