

Introduction
The immune system is one of the most complex and fascinating systems of the human body. Its primary function is to protect the body against infection and the development of cancer. Too often conventional medicine overlooks the importance of susceptibility to infection or disease. Support and enhancement of the immune system are perhaps the most important and vital steps in reducing susceptibility to colds, flu, and cancer.
Determining Immune Function
The criteria that we use to determine whether the immune system is going to be an area of focus is an answer of yes to any of the following questions:
• Do you catch colds or flu easily?
• Do you get colds or flu more than three times a year?
• Are you suffering from chronic infection?
• Do you get frequent cold sores or fungal nail infections, or do you have genital herpes?
• Are your lymph glands sore and swollen at times?
• Do you have now or have you ever had cancer?
Recurrent or chronic infections, even very mild colds, happen only when the immune system is weakened. What makes it difficult for susceptible people to overcome their tendency for infection is a repetitive cycle: a weakened immune system leads to infection, and chronic infection leads to depletion of the immune system, further weakening resistance. Enhancing the immune system by following the guidelines in this chapter may provide the means of breaking the cycle.
Components of the Immune System
The immune system is composed of the lymphatic vessels and organs (thymus, spleen, tonsils, and lymph nodes), white blood cells (lymphocytes, neutrophils, basophils, eosinophils, monocytes, etc.), specialized cells residing in various tissue (macrophages, mast cells, etc.), and specialized serum factors.
The thymus is the major gland of our immune system. It is composed of two soft pinkish gray lobes lying like a bib just below the thyroid gland and above the heart. To a very large extent, the health of the thymus determines the health of the immune system. Individuals who get frequent infections or suffer from chronic infections typically have impaired thymus activity. Also, people affected with hay fever, allergies, migraine headaches, or rheumatoid arthritis usually have altered thymus function. The thymus is responsible for many immune system functions, including the production of T lymphocytes, a type of white blood cell responsible for cell-mediated immunity (immune mechanisms not controlled or mediated by antibodies). Cell-mediated immunity is extremely important in the resistance to infection by mold-like bacteria, yeast (including Candida albicans), fungi, parasites, and viruses (including herpes simplex, Epstein-Barr, and viruses that cause hepatitis). If an individual is suffering from an infection from these organisms, it is a good indication that his or her cell-mediated immunity is not functioning up to par. Cell-mediated immunity is also critical in protecting against the development of cancer, autoimmune disorders such as rheumatoid arthritis, and allergies.
The thymus gland releases several hormones, such as thymosin, thymopoeitin, and serum thymic factor, which regulate many immune functions. Low levels of these hormones in the blood are associated with depressed immunity and an increased susceptibility to infection. Typically, thymic hormone levels will be very low in the elderly (thymus function decreases with age), individuals prone to infection, cancer and AIDS patients, and individuals exposed to undue stress.
Approximately one-sixth of the entire body is the space between cells. Collectively this space is referred to as the interstitium and the fluid contained within the space is referred to as the interstitial fluid. This fluid flows into the lymphatic vessels and becomes the lymph.
Lymphatic vessels usually run parallel to arteries and veins. The vessels serve to drain waste products from tissues. The lymphatic vessels transport the lymph to lymph nodes, which filter the lymph. The cells responsible for filtering the lymph are macrophages. These large cells engulf and destroy foreign particles, including bacteria and cellular debris.
The lymph nodes also contain B lymphocytes, white blood cells capable of initiating antibody production in response to the presence of viruses, bacteria, yeast, and other organisms.
The spleen is the largest mass of lymphatic tissue in the body. Weighing about 7 oz, the spleen is a fist-sized, spongy, dark purple organ that lies in the upper left abdomen behind the lower ribs. The spleen’s functions include producing white blood cells; engulfing and destroying bacteria and cellular debris, and destroying worn-out red blood cells and platelets. The spleen also serves as a blood reservoir. During times of demand, such as hemorrhage, the spleen can release its stored blood and prevent shock.
Like the thymus, the spleen also releases many potent immune-system-enhancing compounds. For example, tuftsin and splenopentin, two small proteins secreted by the spleen, have been shown to exert profound immune-enhancing activity.
There are several types of white blood cells, including neutrophils, eosinophils, basophils, lymphocytes, and monocytes.
Neutrophils
These cells actively phagocytize—engulf and destroy—bacteria, tumor cells, and dead particulate matter. Neutrophils are especially important in preventing bacterial infection.
These cells are involved in allergic conditions. They secrete histamine and other compounds designed to break down antigen-antibody complexes, but they also promote allergic mechanisms.
Lymphocytes
There are several types of lymphocytes, including T cells, B cells, and natural killer cells.
T cells are thymus-derived lymphocytes. These cells orchestrate many immune functions and are the major components of cell-mediated immunity (discussed above). There are different types of T cells, including helper T cells, which help other white blood cells to function; suppressor T cells, which inhibit white blood cell functions; and cytotoxic T cells, which attack and destroy foreign tissue, cancer cells, and virus-infected cells.
The ratio of helper T cells to suppressor T cells is a useful determinant of immune function. If the ratio is low, immunodeficiency is present. For example, AIDS is characterized by a very low ratio of helper T cells to suppressor T cells. If the ratio of helper T cells to suppressor T cells is high, most often allergies or autoimmune disorders such as rheumatoid arthritis or lupus are present. Both high and low T cell ratios have been found in chronic fatigue syndrome.
B cells are responsible for producing antibodies, which are large protein molecules which bind to foreign molecules (antigens) on bacteria, viruses, other organisms, and tumor cells. After the antibody binds to the antigen it sets up a sequence of events that ultimately destroys the infectious organism or tumor cell.
Natural killer cells or NK cells received their name because of their ability to destroy cells that have become cancerous or infected with viruses. They are the body’s first line of defense against cancer development. The level of activity of natural killer cells in chronic fatigue syndrome, cancer, and chronic viral infections is usually low.
Monocytes
Monocytes are the garbage collectors of the body. These large white blood cells are responsible for cleaning up cellular debris after an infection. Monocytes are also responsible for triggering many immune responses.
Macrophages
As stated earlier, the lymph is filtered by specialized cells known as macrophages. Macrophages are actually monocytes that have taken up residence in specific tissues such as the liver, spleen, and lymph nodes. These large cells phagocytize or engulf foreign particles including bacteria and cellular debris. Macrophages are essential in protecting against invasion by microorganisms as well as against damage to the lymphatic system.
Mast Cells
Mast cells are basophils that have taken up residence primarily along blood vessels. The mast cell, like the basophil, is responsible for releasing histamine and other compounds involved in allergic reactions.
There are a number of special chemical factors that enhance the immune system (interferon, interleukins, complement, etc.). These compounds are produced by various white blood cells—for example, interferon is produced primarily by T cells, interleukins are produced by macrophages and T cells, and complement fractions are manufactured in the liver and spleen. These special chemical factors are extremely important in activating the white blood cells to destroy cancer cells and viruses.
Supporting the Immune System
There really isn’t any single magic bullet that can immediately restore immune function. The immune system is a complex integration of parts that are continuously protecting the body from microbial and cancerous attack. The immune system is truly holistic, as evidenced by the close association of psychological, neurological, nutritional, environmental, and hormonal factors with immune function. Supporting the immune system is critical to good health. Conversely, good health is critical to supporting the immune system. The best approach to supporting immune function is a comprehensive plan involving lifestyle, stress management, exercise, diet, nutritional supplementation, avoidance of toxins, and the use of botanical medicines.
The first step in supporting immune function is employing the healing power of the mind and attitude. Psychoneuroimmunology (PNI) is the term used to describe the interactions between emotional state, nervous system function, and the immune system.1 Investigations into these interactions have documented that the mind and attitude play a significant role in the functioning of the immune system. However, a complete and detailed account of the many facets of PNI, or behavioral immunology, is beyond the scope of this chapter, so we will focus on the basics.
Our mood and attitude have a tremendous bearing on the function of our immune system. When we are happy and up, our immune system functions much better. Conversely, when we are depressed, our immune system tends to be impaired. Employing measures outlined in the chapter “A Positive Mental Attitude” can be quite useful in improving the immune system.
It was easily accepted by conventional medical authorities that negative emotional states adversely affect the immune system, but for some reason the medical community initially scoffed at the notion that positive emotional states can actually enhance immune function.
Although a stressor does not have to be a major life event to cause depressed immune function, it is safe to say that the more significant the stressor, the greater the impact on the immune system. The loss of a spouse, perhaps the most stressful life event, was strongly associated with increased sickness and death well before a link between the mind and immune function was documented. In fact, it was not until 1977 that a study of 26 bereaved spouses documented that grief led to a significant depression in immune function (natural killer cell activity was significantly reduced).2 Subsequent studies have further demonstrated that bereavement, depression, and stress significantly diminish important immune functions.1,3
Positive Emotional State and Immune Function
By the end of the 1970s, several studies had shown that negative emotions suppress immune function. But in 1979, Norman Cousins’ popular book Anatomy of an Illness caused a significant stir in the medical community. Cousins’s book provided an autobiographical anecdotal account that positive emotional states can cure the body of even a quite serious disease.4 Cousins watched Candid Camera and Marx Brothers films and read humorous books.
Originally physicians and researchers scoffed at Cousins’s account. But they soon demonstrated in numerous studies that laughter and other positive emotional states can in fact enhance the immune system.5,6 In addition, guided imagery, hypnosis, and other meditative states have been shown to enhance immune system function.1,7
If you want to have a healthy immune system, you need to laugh often, view life with a positive eye, and put yourself in a relaxed state of mind on a regular basis.
Stress
Many clinical and experimental studies have clearly demonstrated that stress, personality, attitude, and emotion are etiologic or contributory in suppressing the immune system as well as leading to the development of many and diverse diseases.1 Reaction to stressful stimuli is entirely individual, reinforcing the fact that people differ significantly in their perceptions of and responses to various life events. The variations in response help account for the wide diversity of stress-induced illnesses. Stress causes increases in blood levels of the adrenal hormones adrenaline and cortisol, leading to an immune-suppressed state and leaving the host susceptible to infectious and carcinogenic illnesses. This immune suppression is proportional to the level of stress, and although the effects are numerous, they appear to involve a common mechanism: increases in cortisol, pro-inflammatory compounds known as cytokines, and adrenaline, resulting in significant decrease in white blood cell function, thymic function, and the formation of new white blood cells. More than 150 clinical studies have now shown that stress can alter immune function and contribute to the development of significant disease and poor health.1,3 Stress not only disrupts the immune system’s ability to fight infection but also can lead to the development of allergies and/or autoimmune disease.8–10
Studies have documented the relationship between psychosocial stress and the development of infectious illness. Research studies often use the response to a vaccine to simulate the response to an infectious organism as a measure of immune system function. For example, the chronic stress associated with caring for a spouse with Alzheimer’s disease or, for younger people, experiencing stressful life events was associated with a poorer antibody response to an influenza virus vaccine than was the case in well-matched control subjects.11,12 The premise is that the production of a delayed, weaker, and shorter-lived immune response to a vaccine is the same as an impaired immune responses to disease-causing organisms in the real world. Consistent with this concept, subjects who show poorer responses to vaccines also experience higher rates of clinical illness as well as longer-lasting infectious episodes.
Fortunately, the effects of stress on the immune system can be attenuated or even overcome with positive mood, effective stress reduction techniques, humor, laughter, and guided imagery.1,13 For more information on dealing with stress, see the chapter “Stress Management.”
A healthful lifestyle, as detailed in the chapter “A Health-Promoting Lifestyle,” goes a long way in establishing a healthy immune system. This benefit is perhaps most obvious when one looks at the effects of lifestyle on natural killer cell activity.14–16 Below is a list of the lifestyle practices associated with higher natural killer cell activity. One particular lifestyle factor that is absolutely critical to healthy immune function is adequate sleep. In healthy humans, sleep deprivation has consistently been demonstrated to impair different components of immune function and mood. Interestingly, the deterioration of immune function precedes the plummeting of subjective well-being and psychosocial performance in sleep-deprived subjects.17
Lifestyle Practices Associated with Higher Natural Killer Cell Activity
Not smoking
Increased intake of green vegetables
Regular meals
Maintaining proper body weight
Getting more than seven hours of sleep per night
Exercising regularly
A vegetarian diet
Diet
The health of the immune system gland is greatly affected by a person’s nutritional status. Dietary factors that depress immune function include nutrient deficiency, excessive consumption of sugar, consumption of allergenic foods, and high cholesterol levels in the blood. Dietary factors that enhance immune function include all essential nutrients, antioxidants, carotenes, and flavonoids. Consistent with good health, optimal immune function requires a healthy diet that:
• Is rich in whole, natural foods, such as fruits, vegetables, grains, beans, seeds, and nuts
• Is low in fats and refined sugars
• Contains adequate but not excessive amounts of protein
In addition, individuals are encouraged to drink five or six 8-fl.-oz glasses of water per day. These dietary recommendations, along with a positive mental attitude, a good high-potency multivitamin and mineral supplement, a regular exercise program, daily deep breathing and relaxation exercises (meditation, prayer, etc.), and at least seven hours of sleep per day, will go a long way in helping the immune system function at an optimal level.
Nutrient Deficiency. Nutrient deficiency is the most common cause of a depressed immune system. Although research relating nutritional status to immune function has historically concerned itself with severe malnutrition states (i.e., kwashiorkor and marasmus), attention is now shifting toward marginal deficiencies of single or multiple nutrients and the effects of too many calories. The large body of clinical and experimental data has made inevitable the conclusion that a single nutrient deficiency can profoundly impair the immune system.
Given the widespread problem of multiple marginal (subclinical) nutrient deficiencies in Americans, it can be concluded that many people are suffering from impaired immunity that would be amenable to nutritional supplementation. This statement is particularly true of the elderly. Numerous studies have shown that almost all elderly Americans are deficient in at least one nutrient, and most are deficient in many. Likewise, numerous studies show that taking a multivitamin and mineral supplement enhances immune function in elderly subjects (whether they suffer from overt nutritional deficiency or not).18–20 These findings have considerable fundamental, clinical, and public health significance.
Sugar. The oral administration of 100 g portions of carbohydrate as glucose, fructose, sucrose, honey, or orange juice significantly reduces neutrophil phagocytosis, while starch has no effect. As can be seen in the figure below, effects start within half an hour and last for more than five hours, and typically there is a 50% reduction in phagocytic activity at the peak of inhibition (usually two hours after ingestion).21,22 Because neutrophils constitute 60 to 70% of the total white blood cell (WBC) count and are a major portion of the defense mechanism, impairment of phagocytic activity leads to an immune-compromised state. Oral administration of increasing amounts of glucose progressively lowers neutrophil phagocytosis, with maximal inhibition corresponding to maximal blood glucose levels.
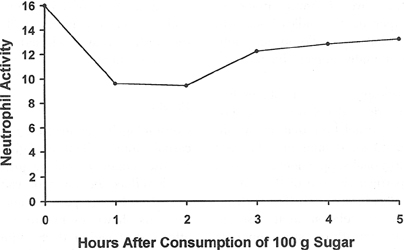
The Effects of Sugar on White Blood Cell Function
In addition, oral ingestion of 75 g glucose has been shown to depress lymphocyte response; lymphocytes are the primary white blood cells that fight viruses.23 Other parameters of immune function are also undoubtedly affected by sugar consumption.
It has been hypothesized that the ill effects of high glucose levels are a result of elevation of insulin values and competition with vitamin C for membrane transport sites.24,25 This hypothesis is based on evidence that vitamin C and glucose appear to compete for absorption into white blood cells, which requires insulin to happen. Once inside the white blood cell, glucose and vitamin C appear to have opposite effects on immune function.
Considering that the average American consumes 125 g sucrose plus 50 g other refined simple sugars each day, the conclusion that most Americans have chronically depressed immune systems is inescapable. It is clear, particularly during an infection, that the consumption of simple sugars, even in the form of fruit juice, is harmful to the host’s immune status.
Fasting during the first phase of an infection might be helpful because it results in a significant increase (up to 50%) in the phagocytic index.21 The fast should not be continued beyond the first 24 hours, however, because eventually the white blood cells’ energy sources will become depleted.
Obesity
Obesity is associated with decreased immune status, as evidenced by the reduced ability of the white blood cells of obese individuals to destroy bacteria. Obesity is also associated with higher infection rates as well as an increase in risk for certain cancers.26 Obesity also increases the risk of asthma and autoimmune diseases by inducing decreased immunological tolerance, a consequence of immunological changes brought about by hormones known as adipokines and cytokines, secreted by fat cells.27 In addition, cholesterol and lipid values are usually elevated in obese individuals; this may explain their impaired immune function. Increased blood levels of cholesterol, free fatty acids, triglycerides, and bile acids inhibit various immune functions, including:28,29
• Formation of new white blood cells
• Response to infectious agents
• Antibody response
• Movement of white blood cells to areas of infection
• Phagocytosis
Optimal immune function therefore depends on control of these serum components. Interestingly, carnitine, even at minimal concentrations, has been shown to neutralize lipid-induced immunosuppression.30 This effect is probably due to carnitine’s role as a rate-limiting factor in the removal of fatty substances from the blood. Individuals with elevations in blood lipids experiencing frequent infections may want to supplement with carnitine (900–1,500 mg per day).
Alcohol
Alcohol consumption increases the susceptibility to experimental infections in animals, and alcoholics are known to be more susceptible to infections, especially pneumonia. Studies of immune function in alcoholics show a profound depression in most indicators of immunity.31
Vitamin A and Carotenes
Vitamin A plays an essential role in maintaining the integrity of the skin and linings of the respiratory and gastrointestinal tract as well as their secretions. These tissues constitute a primary nonspecific host defense mechanism. Vitamin A has also been shown to stimulate and/or enhance numerous immune processes. Also, vitamin A deficiency may predispose an individual to an infection, and during the course of an infection vitamin A stores typically plummet. Vitamin A may be helpful in boosting immune function beyond reversal of vitamin A deficiency, because many immune functions are further enhanced by the administration of (supposedly) excessive levels of vitamin A.20,32 In addition, vitamin A prevents and reverses stress-induced thymus gland shrinkage (involution), and additional vitamin A can actually promote thymus growth.33
Carotenes have also demonstrated a number of immune-enhancing effects. In addition to being converted into vitamin A, carotenes function as antioxidants. Because the thymus gland is so susceptible to damage by free radicals, beta-carotene has advantages in enhancing the immune system that are different from vitamin A (retinol) through its ability to protect the thymus. However, taking sufficient vitamin A is still important, as about 25% of the population does not effectively convert beta-carotene to vitamin A.
Vitamin C
Vitamin C (ascorbic acid) plays an important role in the natural approach to immune enhancement. Although vitamin C has been shown to be antiviral and antibacterial, its main effect is improvement of host resistance. Many different immunostimulatory effects have been demonstrated, including enhancing lymphoproliferative response to mitogens and lymphotrophic activity and increasing interferon levels, antibody responses, immunoglobulin levels, secretion of thymic hormones, and integrity of ground substance.20,34 Vitamin C also has direct biochemical effects similar to those of interferon.35
Numerous clinical studies support the use of vitamin C in the treatment of infectious conditions and possibly even cancer at very high intravenous dosages. In addition to its effects on the common cold, vitamin C has also been shown to be useful in other infectious conditions.36 Vitamin C levels are quickly depleted during the stress of an infection as well as in chronic disease.37
It is useful to supplement vitamin C concurrently with flavonoids, which raise the concentration of vitamin C in some tissues and potentiate its effects as well as exert their own effects.38
Vitamin D
The importance of vitamin D to the regulation of cells of the immune system has gained increased appreciation over the past decade with the discovery of the vitamin D receptor on white cells and key vitamin D metabolizing enzymes expressed by cells of the immune system. Vitamin D has been shown to produce a wide range of immune-enhancing effects, including:39–43
• Upregulation of antimicrobial peptides, to enhance clearance of bacteria at various barrier sites and in immune cells
• Modulation of the immune system by direct effects on T cell activation
• Protection against the development of autoimmune diseases (e.g., Crohn’s disease, type 1 diabetes, multiple sclerosis, asthma, and rheumatoid arthritis)
• Reduction of the frequency of viral upper respiratory infections
Vitamin D appears to be especially important in protection against viral or bacterial upper respiratory infection.44
Vitamin E
Vitamin E enhances both antibody production and cell-mediated immunity. A vitamin E deficiency results in atrophy of lymphoid tissue and decreases white blood cell response and function. Vitamin E supplementation (30–150 IU) has been shown to:45
• Increase white blood cell response
• Prevent free-radical-induced thymus atrophy
• Enhance helper T cell activity
• Increase antibody response and phagocytosis
Elderly subjects may benefit from even higher dosages of vitamin E. One study sought to determine the effect of vitamin E supplementation at different dosages on immune function in 88 patients older than 65 years.20,46 The researchers measured T cell function by a number of assessments. Vitamin E was given at 60, 200, or 800 IU for 235 days. Although the placebo group experienced only an 8% increase in T cell function, the 60 IU group had a 20% increase, the 200 IU group a 58% increase, and the 800 IU group a 65% increase. With regard to antibody production, the best results were observed in the patients receiving 200 IU per day. No effect on autoimmune antibodies was noticed. No adverse effects were observed at any of the three dosage schedules of vitamin E.
In another double-blind study of 451 elderly participants in a nursing home, vitamin E supplementation (200 IU per day) demonstrated a protective effect against upper respiratory tract infections, particularly the common cold.47
Vitamin B6
Vitamin B6 deficiency results in depressed cellular and humoral immunity; the thymus, spleen, and lymph nodes shrink; the number of white blood cells plummets; there is a tremendous reduction in the quantity and quality of antibodies produced; and there is decreased activity of thymus hormones. Factors predisposing to vitamin B6 deficiency are low dietary intake, excess protein intake, high consumption of yellow (hydralazine) food dyes, alcohol consumption, and use of oral contraceptives.
Folic Acid and Vitamin B12
A deficiency of vitamin B12 and/or folate results in significantly reduced production of white blood cells and abnormal white blood cell responses. Folic acid deficiency (the most common vitamin deficiency in the United States) has been shown to result in shrinkage of the thymus and lymph nodes and impaired white blood cell function. A B12 deficiency produces identical findings and is especially harmful to the ability of white blood cells to engulf and destroy infecting organisms.
Other B Vitamins
Thiamine, riboflavin, and pantothenic acid deficiencies lead to reduced antibody response, decreased white blood cell response, and atrophy of the thymus and lymph tissue.
Iron
Iron deficiency is a common nutritional deficiency state that causes immune dysfunction in large numbers of people, in particular menstruating women, elderly individuals taking aspirin and other drugs that can cause gastrointestinal bleeding due to ulcer formation, and children. Marginal iron deficiency, even at levels that do not lower blood values, can influence the immune system. Thymus and lymph node atrophy, decreased white blood cell response and function, and decreased ratio of T cells to B cells are common findings.
Iron is an important nutrient to bacteria as well as humans. During infection, one of the body’s nonspecific defense mechanisms to limit bacterial growth is to reduce plasma iron, and in vitro studies have shown that the natural protectors in the blood against bacterial infection are eliminated by the addition of iron to the serum.48 As body temperature rises, plasma iron levels drop, and when temperature is raised to fever levels the growth of bacteria is inhibited, though not at high iron concentrations.
These observations lead us to the conclusion that iron supplementation is probably contraindicated during acute infection, especially in patients with low transferrin levels. However, in patients with impaired immune function, chronic infections, and subnormal iron levels, adequate supplementation is essential.
Zinc
The hereditary zinc deficiency disease acrodermatitis enteropathica (AE) offers an excellent model for understanding the role of zinc in immunity. In AE, the number of T cells is reduced, white blood cell function is significantly impaired, and thymic hormone levels are lower. All of these effects are reversible upon adequate zinc administration and absorption.
Some studies have shown that zinc serves a vital role in many immune system reactions. For example, it promotes the destruction of foreign particles and microorganisms, acts as a protectant against free radical damage, acts synergistically with vitamin A, is required for proper white blood cell function, and is a necessary cofactor in activating serum thymic factor.49,50
Zinc also directly inhibits the growth of several viruses, including common cold viruses and the herpes simplex virus.51,52 Throat lozenges containing zinc have become popular in the treatment of the common cold for good reason—they work (as discussed further in the chapter “Common Cold”).
Selenium
With the vital role it plays in the antioxidant enzyme glutathione peroxidase, selenium affects all components of the immune system, including the development and expression of all white blood cells. Selenium deficiency results in depressed immune function, whereas selenium supplementation results in augmentation and/or restoration of immune functions. Selenium deficiency has been shown to inhibit resistance to infection as a result of impaired white blood cell and thymus function, while selenium supplementation (200 mcg per day) has been shown to stimulate white blood cell and thymus function.53–56
The ability of selenium supplementation to enhance immune function goes well beyond simply restoring selenium levels in selenium-deficient individuals. For example, in one study selenium supplementation (200 mcg per day) to individuals with normal selenium concentrations in their blood resulted in a 118% increase in the ability of lymphocytes to kill tumor cells and an 82.3% increase in the activity of natural killer cells.56 These effects were apparently related to the ability of selenium to support the expression of the immune-enhancing compound interleukin-2 and, consequently, the rate of white blood cell proliferation and differentiation into forms capable of killing tumor cells and micro-organisms. The supplementation regimen did not produce significant changes in the blood selenium levels of the participants. The results indicated that the immune-enhancing effects of selenium in humans require supplementation above the normal dietary intake.
Perhaps the most effective method of reestablishing a healthy immune system is employing measures to improve thymus function. Promoting optimal thymus gland activity involves the following:
• Prevention of thymic involution or shrinkage by ensuring adequate dietary intake of antioxidant nutrients
• Use of nutrients that are required in the manufacture or action of thymic hormones
Antioxidants
The thymus gland shows maximum development immediately after birth. During the aging process, the thymus gland undergoes a process of shrinkage, or involution. The reason for this involution is that the thymus gland is extremely susceptible to free radical and oxidative damage caused by stress, radiation, infection, and chronic illness.
Many patients with impaired immune function as well as conditions associated with impaired immunity (e.g., chronic fatigue syndrome, cancer, AIDS) suffer from a state of oxidative imbalance characterized by a greater number of pro-oxidants than antioxidants in their system. This situation is quite detrimental to thymus function. One of the primary ways in which antioxidants affect the immune system, particularly cell-mediated immunity, may be by protecting the thymus gland from damage. The antioxidant nutrients most important for protecting the thymus include the carotenes, vitamin C, vitamin E, zinc, and selenium.
Many nutrients function as important cofactors in the manufacture, secretion, and function of thymic hormones. A deficiency of any one of these results in decreased thymic hormone action and impaired immune function. Zinc, vitamin B6, and vitamin C are among the most important. Supplementation with these nutrients has been shown to improve thymic hormone function and cell-mediated immunity.
Zinc is perhaps the critical mineral involved in thymus gland function and thymus hormone action, taking part in virtually every aspect of immunity. When zinc levels are low, the number of T cells is reduced, thymic hormone levels are lower, and many white blood cell functions critical to the immune response are severely lacking. All of these effects are reversible with adequate administration and absorption of zinc.57,58
Adequate zinc levels are particularly important in the elderly, and zinc supplementation in elderly subjects results in increased numbers of T cells and enhanced cell-mediated immune responses.58
Many herbs have been shown to have antibacterial, antiviral, and immunostimulatory effects. A complete discussion is outside the scope of this chapter, though several immune-enhancing botanicals, such as Echinacea species, goldenseal (Hydrastis canadensis), and umka (Pelargonium sidoides), are discussed in the chapters on upper respiratory tract infections (common cold, bronchitis, sinusitis, and sore throat), as that context reflects their primary use. One herb that will be described in this chapter is the root of Astragalus membranaceus, a traditional Chinese medicine used for infections. Clinical studies in China have shown it to be effective when used as a preventive measure against the common cold.59 It has also been shown to reduce the duration and severity of symptoms in acute treatment of the common cold as well as to raise WBC counts in people with chronic low levels of WBCs.
Research on animals has shown that astragalus apparently works by stimulating several factors of the immune system, including enhancing the phagocytic activity of monocytes and macrophages, increasing interferon production and natural killer cell activity, improving T cell activity, and potentiating other antiviral mechanisms.59–61 Astragalus appears particularly useful in cases in which the immune system has been damaged by chemicals or radiation. In immunodepressed mice, astragalus has been found to reverse the T cell abnormalities caused by an immune-suppressing drug (cyclophosphamide), radiation, and aging.62
In terms of supporting immune function, extracts and preparations of baker’s yeast and medicinal mushrooms such as maitake (Grifola frondosa), shiitake (Lentinus edodes), reishi (Ganoderma lucidum), and Cordyceps sinensis exert significant immune-enhancing effects. Much of this activity is due to the presence of molecules known as beta-glucans. Numerous experimental and clinical studies have shown that yeast and mushroom beta-glucans activate white blood cells by binding to receptors on the outer membranes of neutrophils, macrophages, natural killer (NK) cells, and cytotoxic T cells. Just like a key in a lock, the binding of the beta-glucan to cellular receptors flips white blood cells on and triggers a chain reaction leading to increased immune activity. In addition to increasing the ability of the neutrophils and macrophages to engulf and destroy microbes, cancer cells, and other foreign cells, the binding stimulates the production of important signaling proteins of the immune system, such as interleukin-1, interleukin-2, and lymphokines. These immune activators ramp up defenses by activating immune cells.63,64
One of the best-researched beta-glucan sources is Wellmune WGP—a whole glucan particle composed of 1,3/1,6-beta-glucan derived from the cell walls of a highly purified, proprietary baker’s yeast (Saccharomyces cerevisiae). Once absorbed, Wellmune is taken up by macrophages, digested into smaller fragments, and slowly released over a number of days. The fragments bind to neutrophils via complement receptor 3 (CR3), enhancing their activity. As of 2011, six double-blind clinical studies have been conducted with Wellmune WGP demonstrating positive results in reducing the signs, symptoms, frequency, and duration of upper respiratory infections. In a study of marathon runners (who experience increased infections after long runs like marathons), Wellmune WGP significantly reduced symptoms of upper respiratory tract infection (sore throat, stuffy nose, etc.) in the test subjects. Furthermore, the Wellmune group reported 22% higher scores in vigor, 48% reduction in fatigue, 38% reduction in tension, and 38% reduction in confusion compared with the control groups.65
In a double-blind study during the cold and flu season, the Wellmune WGP group reported (1) no incidence of fever, compared with an incidence of 3.5 in the control group over a 90-day period; (2) no need to take a sick day from work or school, compared with 1.38 days of work or school missed for the placebo group; and (3) an increase in general health, including physical energy and emotional well-being.66
In the latest study of 122 healthy volunteers, participants taking 250 mg Wellmune WGP per day for 12 weeks reported a 58% reduction in upper respiratory tract infection symptoms, compared with individuals taking a placebo. These subjects also experienced improvement in energy levels compared with the placebo group.67

QUICK REVIEW
• The immune system protects the body against infection and the development of cancer.
• Recurrent or chronic infections, even very mild colds and flu, are signs that the immune system is weakened.
• Supporting immune function involves a comprehensive approach.
• The mind and emotions have a tremendous impact on immune function.
• Stress depresses immune function.
• Too much sugar in the diet leads to lowered white blood cell activity.
• Nutrient deficiency is the most common cause of low immune function.
• Key nutrients for supplementation to support the immune system are vitamin A, vitamin C, vitamin E, B vitamins, zinc, and selenium.
• Supporting the thymus, the major gland of the immune system, is one of the primary goals of therapy.
• The herb astragalus exerts broad-spectrum effects on immune function.
• One of the best-researched beta-glucan sources is Wellmune WGP, a whole glucan particle derived from the cell walls of baker’s yeast.
TREATMENT SUMMARY
The regimen given here is meant as a general approach to supporting immune function during an active infection. It is designed to be supportive but is not intended to be a replacement for proper medical care. Though most common infections, such as the common cold, are self-limiting conditions, others can be life-threatening. Proper medical care should be sought when there is any sign or symptom associated with a more serious infection: fever, redness, excessive swelling, severe fatigue, pus formation, etc.
• Rest (bed rest is best).
• Drink large amount of fluids (preferably diluted vegetable juices, soups, and herb teas—no fruit juice).
• Limit your simple sugar consumption (including fruit sugars) to less than 50 g per day.
• High-potency multivitamin and mineral formula as described in the chapter “Supplementary Measures”
• Vitamin C: 500 mg every two hours
• One of the following:
![]() Bioflavonoids (mixed): 1,000 mg per day
Bioflavonoids (mixed): 1,000 mg per day
![]() Grape seed or pine bark extract, 50 to 100 mg per day
Grape seed or pine bark extract, 50 to 100 mg per day
• One of the following:
![]() Vitamin A: 2,500 IU per day
Vitamin A: 2,500 IU per day
![]() Beta-carotene 25,000 IU per day
Beta-carotene 25,000 IU per day
• Vitamin D: 2,000 to 4,000 IU per day (ideally, measure blood levels and adjust dosage accordingly)
• Zinc: 20 to 30 mg per day
• Astragalus membranaceus:
![]() Dried root (or as decoction): 1 to 2 g three times per day
Dried root (or as decoction): 1 to 2 g three times per day
![]() Tincture (1:5): 2 to 4 ml three times per day
Tincture (1:5): 2 to 4 ml three times per day
![]() Fluid extract (1:1): 2 to 4 ml three times per day
Fluid extract (1:1): 2 to 4 ml three times per day
![]() Solid (dry powdered) extract (0.5% 4-hydroxy-3-methoxy isoflavone): 100 to 150 mg three times per day
Solid (dry powdered) extract (0.5% 4-hydroxy-3-methoxy isoflavone): 100 to 150 mg three times per day
• Beta-glucan sources:
![]() Wellmune WGP: 250 to 500 mg per day.
Wellmune WGP: 250 to 500 mg per day.
![]() Maitake: dosage is based upon body weight and beta-glucan content stated as MD- or D-fraction (typically 0.5 mg to 1.0 mg/kg per day).
Maitake: dosage is based upon body weight and beta-glucan content stated as MD- or D-fraction (typically 0.5 mg to 1.0 mg/kg per day).
![]() Shiitake or reishi: equivalent of 6 to 9 g dried mushrooms per day.
Shiitake or reishi: equivalent of 6 to 9 g dried mushrooms per day.