

• Blackheads: dilated skin follicles with central dark, horny plugs
• Whiteheads: red, swollen follicles with or without white pustules
• Nodules: tender collections of pus deep in the skin that discharge to the surface of the skin
• Cysts: deep nodules that fail to discharge contents to surface
• Large deep pustules: cysts that contain inflammatory compounds that break down adjacent skin tissue, leading to scar formation
Acne is the most common of all skin problems. There are two major forms: acne vulgaris and acne conglobata. Acne vulgaris is characterized as a superficial disease that affects the hair follicles and oil-secreting glands of the skin; it is manifested as blackheads, whiteheads, and inflammation (redness). Acne vulgaris is the least severe form of acne. On the other hand, acne conglobata is a more severe form, with cyst formation and subsequent scarring. Rosacea is a chronic acne-like eruption on the face of middle-aged and older adults, associated with facial flushing (see the chapter “Rosacea”). In both superficial (acne vulgaris) and cystic (acne conglobata) acne, the lesions occur predominantly on the face and, to a lesser extent, on the back, chest, and shoulders.
Causes
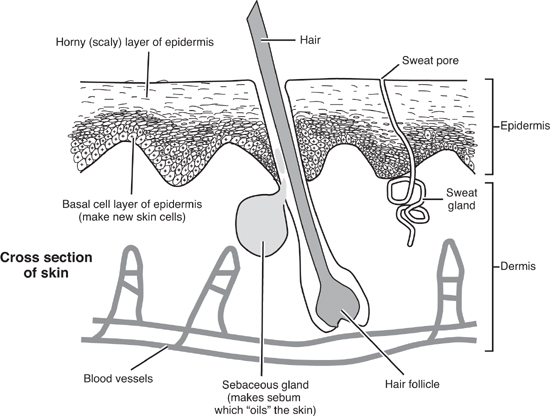
Acne has its origin in the skin pore or, to use a more accurate term, the pilosebaceous unit. Such units usually consist of a hair follicle and the associated sebaceous glands, which are connected to the skin by the follicular canal through which the hair shaft passes. The sebaceous glands produce sebum, a mixture of oils and waxes that lubricates the skin and prevents the loss of water. Sebaceous glands are concentrated most highly on the face and to a lesser extent on the back, chest, and shoulders.
Acne is more common among males, and onset is typically at puberty (somewhat later for the cystic form). This occurs because male sex hormones, such as testosterone, stimulate the cells that line the follicular canal to produce keratin, a fibrous protein that is the main component of the outermost layer of skin as well as of hair and nails. Overproduction of keratin can block skin pores. In addition, testosterone causes the sebaceous glands to enlarge and produce more sebum. So higher testosterone levels increase the likelihood that pores will become blocked by either excessive keratin or too much sebum. While boys are at greater risk, there is an increase in testosterone level in girls during puberty, making them susceptible as well.
While the onset of acne usually reflects an increase in testosterone level, the severity and progression of acne are determined by a complex interaction among hormonal factors, keratin-producing cells, sebum, and bacteria. Here is the basic scenario: Pimples begin forming near the surface of the skin pore when the cells that line the canal start producing an excess of keratin; this eventually leads to blockage of the canal, resulting in ballooning and thinning. Eventually a white-head or blackhead is formed. A blackhead will form if the blockage is incomplete, allowing the sebum to make its way to the surface, thereby avoiding the inflammation of a white-head (discussed below), and a whitehead will form if the blockage is complete.
With the blockage of the canal, a bacterium known as Propionibacterium acnes (Corynebacterium acnes) can overgrow and release enzymes that break down sebum and promote inflammation. The redness of pimples is a result of this inflammation. If the bacterium grows out of control or if the inflammation is severe, the condition can result in the rupture of the wall of the hair canal and damage to surrounding tissue. If this happens at the skin surface, it simply causes superficial redness and pustules. However, if it occurs deeper within the skin, a nodule or cyst can form, leading to more significant damage and possibly scar formation.
As noted above, male hormones control sebaceous gland secretion and exacerbate the development of abnormal growth of the hair-follicle cells. But excessive secretion of male hormones is not necessarily the cause, since there is only a poor correlation between blood levels of these hormones and the severity of the disease.1–3 What may be more important is that the skin of patients with acne shows greater activity of an enzyme called 5-alpha-reductase, which converts testosterone to a more potent form known as dihydrotestosterone (DHT).4,5
One key factor in acne is genetics. It is inherited in an autosomal dominant pattern. What this means is that if both parents had acne, three of four children will have acne. If one parent had acne, then one of four children will have acne.6
Dietary factors also play a major role in acne, from both a preventive perspective and a therapeutic one, and are discussed below. Another contributor to acne that is seldom recognized is intestinal toxemia. One study showed that 50% of patients with severe acne had increased blood levels of toxins absorbed from the intestines.7 This situation has not yet been fully evaluated, but it is an interesting finding given that naturopathic physicians in the early 1900s viewed acne as largely a condition reflecting poor colon health.
In 1948, Dr. M. B. Sulzberger stated, “There is no single disease which causes more psychic trauma and more maladjustment between parents and children, more general insecurity and feelings of inferiority and greater sums of psychic assessment than does acne vulgaris.” Acne has always been associated with emotional stress and depression, but it is possible that the emotional stress also plays a role in the disease progression. In the 1940s dermatologists John H. Stokes and Donald M. Pillsbury first proposed a gastrointestinal mechanism for the overlap between depression, anxiety, and skin conditions such as acne. These doctors hypothesized that emotional states might alter the normal intestinal microflora, increase intestinal permeability, and contribute to systemic inflammation and increased sebum production. They also noted that as many as 40% of those with acne have hypochlorhydria, and they hypothesized that inadequate stomach acid would set the stage for migration of bacteria from the colon toward the distal portions of the small intestine, as well as an alteration of normal intestinal micro-flora. The remedies these authors discussed as a means to cut off the stress-induced cycle included administration of Lactobacillus acidophilus cultures (long before they were known as probiotics) and also cod liver oil. Many aspects of this gut-brain-skin unifying theory proposed by Stokes and Pillsbury have recently been validated. The ability of the gut microflora and oral probiotics to influence systemic inflammation, oxidative stress, glycemic control, tissue lipid content, and even mood itself, may have important implications in acne.8 In addition, probiotic supplementation is often indicated, given that a common treatment for acne is antibiotics, which kill off the important healthful bacteria in the intestines.
If a person appears to have acne, it is important to make sure that it truly is acne. Exposure to a variety of compounds can produce the characteristic lesions of acne.
Agents That Cause Acne-like Lesions
Drugs: steroids, diphenylhydantoin, lithium carbonate
Industrial pollutants: machine oils, coal tar derivatives, chlorinated hydrocarbons
Local actions: use of cosmetics or pomades, excessive washing, repetitive rubbing
Therapeutic Considerations
Pilosebaceous Unit
Acne requires an integrated therapeutic approach. Also, because many individuals have undergone long-term treatment with broad-spectrum antibiotics, they often develop intestinal overgrowth of the yeast Candida albicans. This chronic yeast infection may actually make acne worse and must be treated when present. (See the chapter “Candidiasis, Chronic.”)
In addition to orally administered antibiotics, another acne treatment is oral isotretinoin (Accutane), a derivative of vitamin A. It is approved only for severe acne and recalcitrant nodular acne. This drug has received a lot of attention regarding its safety. Specifically, reports of intracranial hypertension, depression, and suicidal ideation have prompted an examination of Accutane’s life-threatening potential. It is also not to be taken by pregnant women. A warning was added to its product label with regard to signs of depression and suicidal ideation, and a U.S. Food and Drug Administration–mandated registry is now in place for all individuals prescribing, dispensing, or taking isotretinoin, to help decrease the risks associated with isotretinoin therapy.
Another popular treatment for acne is the use of over-the-counter preparations containing benzoyl peroxide (e.g., Oxy 5/Oxy 10, Clearasil, Benoxyl). Benzoyl peroxide acts as a skin antiseptic to keep the growth of bacteria down. It is most effective for superficial pimples that are inflamed. In order to be effective, benzoyl peroxide preparations must be applied on a daily basis. The primary side effect of benzoyl peroxide preparations is a tendency to dry out the skin and/or cause redness and peeling. The prescription topical medicine most often used is tretinoin (Retin-A). Side effects are more common with Retin-A than with benzoyl peroxide. The peeling and drying can be quite severe, as Retin-A improves acne by chemically burning the skin.
Although there is some controversy about diet in the etiology of acne, there is clear evidence of an association. In westernized societies, acne vulgaris is a nearly universal skin disease, afflicting 79 to 95% of the adolescent population. In men and women older than 25 years, 40 to 54% have some degree of facial acne, and clinical facial acne persists into middle age in 12% of women and 3% of men. In contrast, epidemiological evidence shows that acne incidence rates are considerably lower in non-westernized societies.9
A number of dietary factors have been identified. Milk is a significant problem for many acne sufferers. In addition to trans-fatty acids, milk contains hormones, including precursors to DHT, and it promotes an increase in insulin-like growth factor 1 (IGF-1). Receptors for IGF-1 are present on the sebaceous gland. When IGF-1 binds to these receptors it stimulates sebum production. Elimination of all milk and dairy products and high-sugar foods is recommended.10–13
For those who are iodine sensitive, foods high in iodine should be eliminated (including foods with a high salt content, as most salt is iodized). Also, foods containing trans-fatty acids (milk and milk products; margarine, shortening, and other synthetically hydrogenated vegetable oils) or oxidized fatty acids (fried food) should be avoided, as these may aggravate acne by increasing inflammation in sebaceous glands.
A diet high in refined carbohydrates is associated with acne. In the early 1940s dermatologists reported that insulin is effective in the treatment of acne, suggesting impaired skin glucose tolerance, insulin insensitivity, or both.14,15 The insulin was either given systemically (5 to 10 units two to three times a week) or injected directly into the lesion. Interestingly, one study comparing the results of oral glucose tolerance tests in acne patients showed no differences from controls in blood glucose measurements. However, repetitive skin biopsies revealed that the acne patients’ skin glucose tolerance was significantly disturbed.11 One researcher even coined the term skin diabetes to describe acne.16 Acne sufferers generally have a diet higher in glycemic load than that of even the typical American.17 This is problematic for several reasons, including the influence dietary ratios of carbohydrates, protein, and fat have on the metabolism of testosterone in the skin. Basically, a high-carbohydrate diet increases the conversion of testosterone to the more potent DHT in the skin, which in turn increases sebum production and worsens acne. In contrast, a diet in the range of 45% protein, 35% carbohydrate, and 20% fat produces substantially less DHT formation and enhances the elimination of estrogen, both therapeutic goals.18
High-chromium yeast is known to improve glucose tolerance and enhance insulin sensitivity;19 it has been reported in an uncontrolled study to induce rapid improvement in patients with acne.20 Other forms of chromium may offer similar benefits.
Vitamin A (Retinol)
Many studies have demonstrated that oral vitamin A in the retinol form can reduce sebum production and the overproduction of keratin. Retinol has been shown to be effective in treating acne when used at high—and potentially toxic—dosages (i.e., 300,000 to 400,000 IU per day for five to six months).21 Although dosages of vitamin A below 300,000 IU per day for a few months rarely cause toxic symptoms, we do not recommend this therapy unless it is conducted under the direct supervision of a physician. In fact, we do not recommend dosages greater than 150,000 even under a physician’s supervision. And high dosages of vitamin A should never be ingested by anyone with significant liver disease.
The first significant toxic symptom is usually headache followed by fatigue, emotional volatility, and muscle and joint pain. Laboratory tests appear unreliable for monitoring toxicity, since serum vitamin A levels correlate poorly with toxicity, and liver enzymes are elevated only in symptomatic patients. Of far greater concern is the risk of birth defects caused by high dosages of vitamin A. Women of childbearing age must have at least two negative pregnancy test results prior to the initiation of vitamin A therapy, and they should use effective birth control during treatment and for at least one month after discontinuation. Women who are pregnant or may become pregnant need to limit their daily intake of vitamin A to 3,000 IU, as higher dosages increase the risk for birth defects. The baseline laboratory examination should also include cholesterol and triglyceride assessment, liver enzymes, and a CBC (complete blood count). These tests should be repeated monthly during treatment. Again, we recommend that this therapy be used only under strict physician supervision.
Zinc
Zinc is an important nutrient in the treatment of acne. It is involved in local hormone activation, retinol-binding protein formation, wound healing, immune system activity, and tissue regeneration.
Zinc supplementation in the treatment of acne has been the subject of much controversy and many double-blind studies. Inconsistent results may be due to the differing absorbability of the various zinc salts used. For example, studies using effervescent zinc sulfate show efficacy similar to that of the antibiotic tetracycline, with fewer side effects from chronic use,22 while those using plain zinc sulfate have shown less beneficial results.23 The majority of patients required 12 weeks of supplementation before good results were demonstrated, although some patients experienced dramatic improvement immediately.
In another study, 66 patients with inflammatory acne were given zinc gluconate (30 mg elemental zinc) or a placebo for two months.24 On the basis of the number and severity of lesions, an “inflammatory score” was given to each patient. In the placebo group the inflammatory score dropped from 58 to 47, while in the treatment group the score dropped from 49 to 27. Physicians rated 24 of 32 patients in the zinc group as responders, compared with only 8 of 34 in the placebo group. At least two other double-blind studies with zinc gluconate provide additional support.25,26 Unfortunately, there have been no studies to date using better-absorbed forms of zinc, such as zinc picolinate, citrate, acetate, or monomethionine.
The importance of zinc to normal skin function is well recognized, especially in light of the zinc deficiency syndrome called acrodermatitis enteropathica. As noted above, zinc is essential for retinol-binding protein and thus for serum retinol levels.27 Although low levels of zinc increase the formation of DHT, high concentrations significantly inhibit its formation.28 Interestingly, serum zinc levels are lower in 13- and 14-year-old males than in any other age group.29
Vitamin E and Selenium
Serum vitamin A levels in rats on a vitamin-E-deficient diet remain low regardless of the amount of oral or intravenous vitamin A supplementation. Serum levels return to normal after vitamin E is restored to the diet. Vitamin E has been shown to regulate retinol levels in humans.
Male acne patients have significantly decreased levels of the antioxidant enzyme glutathione peroxidase, which normalize with vitamin E and selenium treatment. The acne of both men and women improves with this treatment.30 This improvement is probably due to inhibition of lipid peroxide formation and suggests that the use of other antioxidants may be valuable.
Various topical gels, ointments, and creams containing natural products are available to treat acne. Like benzoyl peroxide, these preparations aim to reduce both the bacteria level and inflammation. Although there are many choices, the most popular natural formulas are those with tea tree oil and azelaic acid.
Tea Tree Oil
Melaleuca alternifolia, or tea tree, is a small tree native to only one area of the world: the northeast coastal region of New South Wales, Australia. The leaves, the portion of the plant that is used medicinally, are the source of tea tree oil.
Tea tree oil possesses significant antiseptic properties and is regarded by many as an ideal skin disinfectant. This claim is supported by its efficacy against a wide range of organisms (including 27 of 32 strains of P. acnes),31 its good penetration, and the fact that usually it does not irritate the skin. The therapeutic uses of tea tree oil are based largely on its antiseptic and antifungal properties.
In a study conducted at the Royal Prince Hospital in New South Wales, a 5% tea tree oil solution demonstrated beneficial effects similar to those of 5% benzoyl peroxide, but with substantially fewer side effects.32 However, this 5% tea tree oil solution is probably not strong enough for moderate to severe acne. Stronger solutions (up to 15%) should provide even better results. Numerous studies have shown that tea tree oil is extremely safe for use as a topical antiseptic, but it can occasionally produce contact dermatitis.
Azelaic Acid
This naturally occurring nine-carbon dicarboxylic acid, extracted from grains such as wheat and barley, has demonstrated much pharmacological activity, including antibiotic activity against P. acnes. Clinical studies with 20% azelaic acid cream have shown it to produce results equal to those achieved with benzoyl peroxide, tretinoin, and oral tetracycline.33 It has been shown to be effective in all of the different forms of acne. In order to achieve benefits, azelaic acid must be applied to affected areas twice per day for a period of at least four weeks. Treatment usually must be continued for at least six months to maintain the benefits produced after the first month.
One review article found a topical cream containing 20% azelaic acid to be as effective as 5% benzoyl peroxide, 4% hydroquinone cream, 0.05% tretinoin, 2% erythromycin, and 0.5 to 1 g per day oral tetracycline in improving acne vulgaris but less effective than oral isotretinoin at a daily dose of 0.5 to 1 mg/kg in reducing acne conglobata. The authors suggested that the few side effects of topical azelaic acid and lack of overt systemic toxicity offer a clear advantage over conventional drugs.34
![]()
QUICK REVIEW
• Acne is the most common skin problem.
• Acne is dependent upon male hormones, especially testosterone, that stimulate the manufacture of sebum.
• Acne is most common among males during puberty, due to hormonal changes.
• Long-term use of antibiotics may result in an overgrowth of the yeast Candida albicans in the intestines.
• The key dietary recommendation is to avoid sugar, trans-fatty acids, milk, fried foods, and iodine.
• Nutrients to aid in the treatment of acne include chromium, vitamin A, vitamin E, selenium, and zinc.
• Topical treatment with tea tree oil or azelaic acid has produced results equal to benzoyl peroxide without the side effects.
![]()
TREATMENT SUMMARY
Acne is a multifactorial disease requiring an integrated therapeutic approach in order to avoid supplement toxicity while attaining the desired clinical results. Patients should be checked for treatable causes and underlying hormonal abnormalities before specific therapies are initiated.
The recommendations given in the chapter “A Health-Promoting Diet” should be the foundation of treatment. In addition, eliminate all refined and concentrated carbohydrates and limit consumption of high-fat and high-carbohydrate foods. Avoid fried foods, iodine, and foods containing trans-fatty acids. Keep the intake of milk and other dairy products low.
• A high-potency multiple vitamin and mineral formula as described in the chapter “Supplementary Measures”
• Key individual nutrients:
![]() Vitamin A: 150,000 IU per day for three months under a physician’s supervision (women who are pregnant or who may become pregnant should not take more than 3,000 IU per day)
Vitamin A: 150,000 IU per day for three months under a physician’s supervision (women who are pregnant or who may become pregnant should not take more than 3,000 IU per day)
![]() Vitamin C: 1,000 mg per day
Vitamin C: 1,000 mg per day
![]() Zinc: 50 mg per day (picolinate is best)
Zinc: 50 mg per day (picolinate is best)
![]() Selenium: 200 mcg per day
Selenium: 200 mcg per day
![]() Chromium: 200 to 400 mcg per day
Chromium: 200 to 400 mcg per day
![]() Vitamin D3: 2,000 to 4,000 IU per day (ideally, measure blood levels and adjust dosage accordingly)
Vitamin D3: 2,000 to 4,000 IU per day (ideally, measure blood levels and adjust dosage accordingly)
• Fish oils: 3,000 mg EPA + DHA per day
• One of the following:
![]() Grape seed extract (>95% procyanidolic oligomers): 100 to 300 mg per day
Grape seed extract (>95% procyanidolic oligomers): 100 to 300 mg per day
![]() Pine bark extract (>95% procyanidolic oligomers): 100 to 300 mg per day
Pine bark extract (>95% procyanidolic oligomers): 100 to 300 mg per day
![]() Some other flavonoid-rich extract with a similar flavonoid content, super greens formula, or another plant-based antioxidant that can provide an oxygen radical absorption capacity (ORAC) of 3,000 to 6,000 units or higher per day
Some other flavonoid-rich extract with a similar flavonoid content, super greens formula, or another plant-based antioxidant that can provide an oxygen radical absorption capacity (ORAC) of 3,000 to 6,000 units or higher per day
• Probiotic (active lactobacillus and bifidobacteria cultures): a minimum of 5 billion to 10 billion colony-forming units per day
• Exposure to sun or ultraviolet lamp
• Fruit acid peels
• Light therapy (blue and red light), intense pulsed light, laser, photodynamic therapy, fractionated light (for acne scars)
• Thorough daily cleansing
• Application of one of the following:
![]() Tea tree oil, 5% to 15% preparation
Tea tree oil, 5% to 15% preparation
![]() Azelaic acid, 20% preparation
Azelaic acid, 20% preparation