
Nonalcoholic Fatty Liver Disease (NAFLD)/Nonalcoholic Steatohepatitis (NASH)

• Most patients with NAFLD have few or no symptoms.
• Patients may complain of fatigue, malaise, and dull right-upper-quadrant abdominal discomfort.
• Liver enzymes may be elevated.
• On ultrasound exam of the liver, the presence of fatty accumulations can be seen.
Non-alcoholic fatty liver disease (NAFLD) is one cause of a fatty liver, occurring when fat is deposited in the liver (steatosis), though not because of excessive alcohol use. It ranges in severity from a rather benign impairment of liver function to an inflammation of the liver referred to as nonalcoholic steatohepatitis (NASH), which may advance to cirrhosis and end-stage liver disease.
Simple steatosis is associated with obesity, occurring in 70% of patients who are 10% above ideal body weight and nearly 100% of those who are obese. In addition to obesity, NASH is also associated with other factors that impair liver function, including nutritional abnormalities, drugs, and occupational exposure to toxins.
NAFLD is thought to affect more than 20% of Americans, making it the most common liver disease in the United States. NASH affects roughly 2 to 3% of those with NAFLD, making it a major cause of cirrhosis of the liver. Almost 20% of patients with NASH progress to cirrhosis over a decade.
Causes
NAFLD is associated with insulin resistance, which may be evident as obesity, type 2 diabetes, and elevations in blood triglycerides.1–3 When the liver is exposed to damaging compounds, such as the pro-oxidants that are seen with the inflammation accompanying insulin resistance, the first reaction is the infiltration of fat into the liver. NAFLD can also be caused by some medications:
• Amiodarone
• Antiviral drugs (nucleoside analogues)
• Aspirin (rarely, as part of Reye’s syndrome in children)
• Corticosteroids
• Methotrexate
• Nifedipine
• Tamoxifen
• Tetracycline
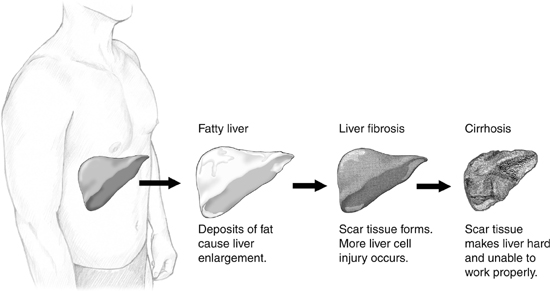
Progression of NAFLD/NASH
Therapeutic Considerations
The primary goal in most cases is improving insulin sensitivity through diet and supplementation. Weight loss is the most effective treatment for NAFLD in overweight individuals4 (see the chapter “Obesity and Weight Management”). NAFLD patients with diabetes will need to follow the recommendations in the chapter “Diabetes.”
Treatment in lean individuals with NAFLD, and a secondary treatment in overweight individuals, involves the use of liver-protecting compounds and herbal compounds that promote the flow of bile and fat to and from the liver (choleretics).
All individuals with NASH should follow the recommendations below as well as those given in the chapter “Hepatitis.”
Elimination of high-glycemic-index foods is a critical step in both the prevention and the treatment of NAFLD. It is interesting to note that in one study 80% of NAFLD patients drank enough soft drinks and juices to add the equivalent of 12 tsp sugar or more to their diet.5 The recommendations in the chapter “A Health-Promoting Diet” should be followed. In addition, special foods rich in factors that help protect the liver from damage and improve liver function include high-sulfur foods such as garlic, legumes, onions, and eggs; good sources of soluble fiber such as pears, oat bran, apples, and legumes; vegetables in the brassica family, especially broccoli, brussels sprouts, and cabbage; artichokes, beets, carrots, and dandelion; many herbs and spices such as turmeric, cinnamon, and cilantro; and green leafy vegetables that enhance detoxification processes in the liver.
Considerable research indicates an increase in iron concentration in the liver in people with NAFLD.6–8 Given its ability to generate pro-oxidants, iron should be avoided unless there is a medical reason for iron supplementation (e.g., iron-deficiency anemia). Follow a low-iron diet and avoid iron supplements.
Betaine and Other Lipotropic Factors
Betaine, choline, methionine, vitamin B6, folic acid, and vitamin B12 are important lipotropic agents, compounds that promote the flow of fat and bile to and from the liver. Lipotropic agents have a long history of use in naturopathic medicine; in essence, they produce a “decongesting” effect on the liver and promote improved liver function and fat metabolism. Lipotropic formulas appear to increase the levels of two important liver substances: SAM-e and glutathione.
Betaine as a single agent has been shown to be quite helpful in NAFLD when given at dosages up to 10 g twice a day.9 However, we feel that taking a lower dosage in conjunction with other lipotropic agents is a more rational approach. Most major manufacturers of nutritional supplements offer lipotropic formulas. The important thing in taking a lipotropic formula is to take enough to provide a daily dose of 1,000 mg betaine, 1,000 mg choline, and 1,000 mg methionine and/or cysteine. Alternatively, SAM-e can be used at a dosage of 200 to 400 mg per day.
Carnitine
Our bodies can make carnitine, but sometimes we may not manufacture sufficient quantities—NAFLD may be an example. Carnitine plays an extremely important role in the utilization and metabolism of fatty acids in the liver as well as in the function of mitochondria, the energy-producing part of cells. Low levels of carnitine in the liver can increase susceptibility to NAFLD. Carnitine supplementation has been shown to significantly inhibit and even reverse alcohol-induced fatty liver disease.10
![]()
QUICK REVIEW
• Insulin resistance is the primary risk factor for NAFLD.
• Weight loss is the most effective treatment for NAFLD in overweight individuals.
• Elimination of high-glycemic foods is a critical step in both prevention and treatment of NAFLD.
• A diet low in iron and avoidance of iron supplements is indicated in NAFLD.
• Betaine, choline, methionine, vitamin B6, folic acid, and vitamin B12 are important lipotropic agents.
• Carnitine supplementation has been shown to significantly inhibit and even reverse alcohol-induced fatty liver disease.
• Prescription bile acid therapy with ursodeoxycholic acid is a very important consideration, especially in NASH.
• Milk thistle extract protects the liver from damage, enhances detoxification processes, and increases the liver’s content of glutathione—a key compound in liver function that is low in patients with NAFLD.
Since carnitine normally facilitates fatty acid transport and oxidation in the mitochondria, a high carnitine level may be needed to handle the increased fatty acid load produced by alcohol consumption or other liver injury. In addition to studies in NAFLD, supplemental carnitine has been shown to reduce free fatty acid levels in patients with cirrhosis and to reduce serum triglycerides and liver enzyme levels while elevating HDL cholesterol in patients with alcohol-induced fatty liver disease.10,11
In a recent study, 45 NAFLD patients were given either carnitine (600 mg per day) or placebo. Results demonstrated significant improvements in the carnitine group, including improvement in liver function and evidence of improved mitochondrial function.12
Carnitine’s use in liver disorders associated with fatty infiltration, including NAFLD, is very important, especially when these changes are due to the ingestion of alcohol or exposure to toxins such as pesticides and herbicides.
Bile Acids
Bile acids are naturally occurring compounds such as ursodeoxycholic acid and tauroursodeoxycholic acid that, like the liptropic agents described above, are effective in promoting the flow of bile and fat to and from the liver. Bile acid preparations are available by prescription, but mixtures of bile acids from ox bile are available in health food stores and may prove to be suitable alternatives. Bile acids appear to be a very useful treatment for NASH. Normally, the daily dosage of ursodeoxycholic acid is 13 to 15 mg/kg.9 However, a recent study assessed the efficacy and safety of high-dose ursodeoxycholic acid in patients with NASH.13 This 12-month double-blind study used a daily dosage of 28 to 35 mg/kg in 126 patients with biopsy-proven NASH and elevated liver enzymes (alanine aminotransferase, ALT). The results showed that treatment with high-dose ursodeoxycholic acid was safe and improved ALT levels and other markers of liver function.
Botanical Medicines
There is a long list of plants that have beneficial effects on liver function. However, the most impressive research is with the extract of milk thistle (Silybum marianum) known as silymarin. The flavonoids in silymarin effectively protect the liver from damage and enhance detoxification processes, including increasing the liver’s content of glutathione—a key compound in liver function that is low in patients with NAFLD. For more information on silymarin, see the chapter “Detoxification and Internal Cleansing.”
TREATMENT SUMMARY
Follow the guidelines in the chapter “A Health-Promoting Diet.” In addition, the recommendations in the chapter “Obesity and Weight Management” are very important.
Certain foods are particularly helpful because they contain the nutrients the liver needs to produce and activate the dozens of enzymes involved in the various phases of detoxification or aid in the effective elimination of toxins. Such foods include:
• Garlic, legumes, onions, eggs, and other foods with a high sulfur content.
• Good sources of soluble fiber, such as pears, oat bran, apples, and legumes or soluble fiber supplements such as PGX (PolyGlycopleX)
• Vegetables in the brassica family, especially broccoli, brussels sprouts, and cabbage because they aid in detoxification reactions
• Artichokes, beets, carrots, dandelion greens, and many herbs and spices such as turmeric, cinnamon, and cilantro
• Green leafy vegetables as well as green foods such as wheatgrass, barley grass, chlorella, and spirulina
• A high-potency multiple vitamin and mineral formula as described in the chapter “Supplementary Measures”
• Fish oils: 1,000 mg EPA + DHA
• One of the following:
![]() Grape seed extract (>95% procyanidolic oligomers): 100 to 300 mg per day
Grape seed extract (>95% procyanidolic oligomers): 100 to 300 mg per day
![]() Pine bark extract (>95% procyanidolic oligomers): 100 to 300 mg per day
Pine bark extract (>95% procyanidolic oligomers): 100 to 300 mg per day
![]() Some other flavonoid-rich extract with a similar flavonoid content, super greens formula, or another plant-based antioxidant that can provide an oxygen radical absorption capacity (ORAC) of 3,000 to 6,000 units or higher per day
Some other flavonoid-rich extract with a similar flavonoid content, super greens formula, or another plant-based antioxidant that can provide an oxygen radical absorption capacity (ORAC) of 3,000 to 6,000 units or higher per day
• One of the following:
![]() Lipotropic formula providing 1,000 mg betaine, 1,000 mg choline, and 1,000 mg cysteine and/or methionine
Lipotropic formula providing 1,000 mg betaine, 1,000 mg choline, and 1,000 mg cysteine and/or methionine
![]() SAM-e: 200 to 400 mg per day
SAM-e: 200 to 400 mg per day
![]() Bile acids (mixed, from ox bile): 500 mg with meals
Bile acids (mixed, from ox bile): 500 mg with meals
• PGX (PolyGlycopleX): 1,500 to 5,000 mg before meals
• Milk thistle (Silybum marianum): Dosage is based on silymarin content (standardized extracts are preferred) and the best results are achieved at higher dosages, i.e., 140 mg to 210 mg silymarin three times per day; dosage for silymarin phytosome is 120 mg two to three times per day between meals.