Anyone can get old. All you have to do is live long enough.
Groucho Marx, comedian
As we saw in chapter 1 – and as any good genie will tell you – most human beings wish to live a long, healthy life. Regardless of doctors, some people believe that it all depends on your parents. But it’s not as simple as that. Whereas our parents’ height explains some 80 to 90% of how tall we are, their longevity only accounts for 3% of how long we live. Even identical twins die, on average, some ten years apart.1 In the next two chapters, we’ll look at what determines health and longevity. In particular, we’ll emphasize the uncertainty in medical knowledge and how to deal with it. To get us started, here are three stories about the medical profession.
Let’s go back in time to 1685, when the British king Charles II was treated by fourteen of the best physicians available. He had uremia, a clinical syndrome caused by kidney dysfunction. The medical historian H.W. Haggard gives a vivid description of events.
The King was bled . . . to the extent of a pint from his right arm. Next [the physician] drew eight ounces of blood from his left shoulder . . . gave an emetic to make the King vomit, two physics, and an enema containing antimony, rock salt, marsh-mallow leaves, violets, beet root, camomile flowers, fennel seed, linseed, cardamom seed, cinnamon, saffron, cochineal, and aloes. The King’s head was then shaved and a blister raised on his scalp. A sneezing powder of hellebore root was given to purge his brain, and a powder of cowslip administered to strengthen it, for it was the belief in those days that nasal secretion came from the brain. The emetics were continued at frequent intervals and meanwhile a soothing drink given, composed of barley water, licorice, and sweet almonds, light wine, oil of wormwood, anise, thistle leaves, mint, rose, and angelica. A plaster of pitch and pigeon dung was put on the King’s feet. Next there was more bleeding followed by the administration of melon seeds, manna, slippery elm, black cherry water, extract of lily of the valley, peony, lavender, pearls dissolved in vinegar, gentian root, nutmeg, and cloves. To this mixture were added forty drops of the extract of human skull. Finally, in desperation a bezoar stone was tried. The King died.2
It’s hard not to believe that Charles II would have lived longer without the treatment of the celebrated physicians.
Back in the modern world and across the Atlantic, our second story is even more tragic. Ben Kolb was seven years old when he arrived at the Martin Memorial Hospital in Florida for a routine ear operation in December 1995. Doctors administered a general anesthetic that started to take effect – as planned – within about twenty minutes. The next step was to give an injection of lidocaine, a local anesthetic that reduces bleeding. It was shortly afterwards that things started to go wrong. First, Ben’s heart rate and blood pressure increased to alarming levels. The emergency anesthesiologist was summoned and managed to stabilize his condition briefly. However, nine minutes later, his heart rate and blood pressure plunged dramatically, his lungs filled with fluid, and he went into cardiac arrest. For nearly two hours, doctors and nurses fought to get his heart working again, but their efforts were futile. Ben remained in a coma for nearly twenty-four hours, until his parents gave permission for the life-support machine to be switched off.
The post-mortem showed that Ben had died from human error. The syringe that was supposed to contain lidocaine in fact contained a massive dose of concentrated adrenaline. If only the mistake hadn’t been made, we would probably never have heard of Ben Kolb, who would now be old enough to attend college with a great life ahead of him.
Now, fast forward six years or so for our third story. A federal district court in Wyoming rules that GlaxoSmithKline should pay $6.4 million in compensation to surviving family members of Donald Shell. On February 13, 1998, Shell, while on the antidepressant Paxil (also known as Seroxat), went on a killing spree in Gillette, Wyoming, shooting dead his wife, daughter, and nine-month-old grand-daughter with his .22-calibre pistol, before turning the gun on himself. On June 2, 2004, New York Attorney General Eliot Spitzer sued GlaxoSmithKline for consumer fraud, charging the company with concealing negative information about the popular antidepressant – which had huge annual revenues.
Although the company conducted three trials on Paxil, it published the results of only the one favorable trial. Worse, despite marketing the drug as suitable for adolescents, the company had no significant evidence from any of the three trials that Paxil was effective for depression in children. Finally, as the court heard, while the published study showed that the only adverse side-effect was headaches, the complete data set revealed that 6.5% of patients treated showed “emotional liability,” including suicidal thoughts, compared with only 1.4% of those on a placebo. Actual suicide rates in the two unpublished studies were also higher for those on Paxil than for those not taking the drug.3
These stories illustrate three important points. First, the beliefs of even the most distinguished practitioners are often proven wrong at a later date. Medicine is not an exact science. Second, mistakes happen. Despite good intentions, human error prevails. Third, not all intentions are good. As in other fields, some blunders are caused by vested interests.
If this sounds a bit negative, don’t be put off. We – like you and your doctor – have your well-being at heart. It’s just that, if we’re all going to manage the “health” dimension of your personal Fortune effectively, we need to be aware of the limitations of medical science and, as in other aspects of life, the significant role of luck.
We stress throughout this chapter that medicine is an inexact, evolving science. Thus, the fact that a well-meaning physician provides advice based on the best available knowledge of the day does not mean that he or she necessarily has the right answer (remember Charles II). Typically, patients do not perceive the uncertainty inherent in medical practice. But it’s still there and to assume otherwise is to fall victim – once again – to the illusion of control. Doctors cannot eliminate uncertainty and, indeed, their advice tends to change (perhaps with very good reason) over the years or vary from one country to another. And quite apart from this inconsistency over time and place, scientists and physicians are human. They make mistakes for good (and sometimes bad) reasons. Some studies have even concluded that medical error is the third biggest cause of death in the USA, behind cancer and heart disease, killing more than 225,000 people every year.4 The UK and Canada report similar results.
But there’s another – more serious – problem with medicine. And this one is not entirely the medical profession’s fault. Let’s illustrate it by way of a couple of stories again.5 Again, they’re both true, but we won’t name any names this time.
Over a two-year period in the 1990s, one doctor convinced ninety women with positive test results from mammography screening to have radical surgery. It was the only sure way, or so he claimed, to save their lives and protect their loved ones from grief. What he didn’t know (or worse, didn’t explain) is that 93% of those who test positive with this kind of screening don’t develop breast cancer.6 That means approximately eighty-four of his patients had painful, expensive, intrusive surgery that, on the best possible reading of this story, brought them absolutely no benefits.
Around the same time a single mother was diagnosed HIV-positive after a screening program. At that point AIDS wasn’t properly understood and none of today’s powerful drugs had been developed. The woman lost her friends and her job, as everyone was scared to touch her. She too was afraid to cuddle her son or prepare his food. Then, nine months later, she caught bronchitis. She thought it was the beginning of the end, but her doctor recommended another AIDS test. “What’s the point?” she thought, but – believing that doctors’ advice should always be followed – she didn’t argue. The test was negative. It turned out that her original results had been mixed up with someone else’s. Although great news, it didn’t erase the psychological scars suffered by both the woman and her affection-starved son. Meanwhile, the other person involved in the mix-up was about to get some very bad news – and too late to prevent possibly infecting other people with the HIV virus.
The point of both stories is that test results are not 100% reliable. And yet, both doctors and patients tend to treat them as such. The German psychologist Gerd Gigerenzer refers to this as the “illusion of certainty,” a close relative of the “illusion of control” that we’ve already met. The lesson here for the patient? Simple: if you have an unexpected test result, take the test again. It’s unlikely to be wrong twice in a row.
Another lesson is for doctors and those who train them. To make a sweeping generalization, they need a better understanding of the uncertainties involved in their profession and more training in statistics. Unfortunately, we their patients don’t help. We tend to have strongly deferential attitudes toward medical practitioners. We also have mistaken beliefs that physicians are all-knowing and that tests are infallible. We let doctors absorb our uncertainties. As we shall see throughout this book, by trusting experts, we create our own illusions of control. Perhaps we simply get the expert advice we deserve?
Now let’s turn our attention to life expectancy. We are, of course, grateful to the medical profession for the amazing gains in life expectancy made over the last two centuries. However, that doesn’t mean to say that today’s doctors are all-knowing. When it comes to advice about how to live longer, it turns out that many modern assumptions are based on dodgy data or ropey reasoning. Unfortunately, this can lead to some pretty depressing conclusions. But bear with us at least until the next chapter, where we will return to a more upbeat position.
In the meantime, let’s go back twelve to fourteen millennia. In those far-from-good old days, life expectancy was little more than twenty years. Then human beings started to domesticate animals, which provided a more reliable supply of food than hunting. A few thousand years later, people began to cultivate the land, a further innovation in the survival stakes. Life expectancy began to rise steadily and has been climbing ever since. By about 2,000 years ago it had reached twenty-five (a huge 25% increase). Another 1,000 years later, and in England at least, it had risen to thirty (another 20% increase). By 1750, when Britain started harnessing the benefits of the industrial revolution and growing economically faster than any other country, life expectancy increased by another five years to about thirty-five. After that, it grew exponentially, doubling to seventy in only two centuries. So, already, we can see the effects of luck on longevity: how long you live depends on when you are born.
It also depends where you are born and live. Today, if you rank countries by life expectancy estimates for those born in 2007, the top fourteen nations come out at over eighty years, while the next sixteen are above seventy-nine. At the other end of the scale, there are ten countries where life expectancy is between forty and forty-five and a further five where babies born in 2007 will be lucky to make it to forty. The difference – from Andorra at 83.5 years to Swaziland at 32.2 – is dramatic.
Even within developed countries, on the basis of life expectancy alone, you are lucky if you’re born female. Japanese men, for example, can live on average to 74.2 years of age, while their sisters have a life expectancy of eighty-five (the highest national figure for women in the world). Similarly, there are big differences within countries and ethnic groups. In the USA, women of Asian origin living in Bergen County, New Jersey, have a life expectancy of ninety-one years, while male Native Americans from South Dakota average only fifty-eight.7
Whether we call it luck or fate, none of us have any control over our ethnicity, nationality, gender, and date of birth. So, apart from moving to Andorra, what can we do to improve our life expectancy and health? Unfortunately, not a lot. Beyond the obvious advice to avoid excesses – of tobacco, alcohol, drugs, food, and even exercise – there are few straightforward steps to longer, healthier living.
Scientists nonetheless have a way of analyzing the possible negative effects of certain activities on life expectancy. Based on observation, they’ve identified a number of so-called “risk factors” – an obvious example being smoking. They then ask, for instance, how life expectancy varies between people who smoke and those who don’t. If it turns out that non-smokers live about one year longer on average than smokers then the scientists conclude that smoking reduces life expectancy by that amount.
One problem is that this is all they can hope to conclude. Some smokers – and even some scientists – interpret this (wrongly) as: “Quit smoking and you can expect to live one year longer.” But to reach such conclusions, you have to look at the various studies which have compared groups of people who started and stopped smoking at different ages. Another problem is that people sometimes have complicated combinations of risk factors. Many smokers also drink alcohol to excess and fail to exercise. How do scientists and statisticians unravel the combined effects of different life choices?
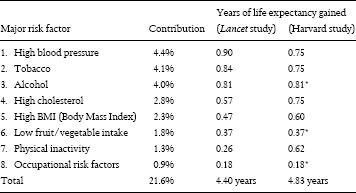
In one major study, published in the prestigious international medical journal, The Lancet,8 researchers set out to identify gains in life expectancy across twenty selected risk factors and many countries. They concluded that these twenty factors accounted on average for 16.1 years in sub-Saharan Africa and 4.4 years in the developed world. Many of the risk factors in the developing world – infant malnutrition, unsafe water, inadequate hygiene – are beyond the control of individuals, so we’ll look only at the subset of eight risk factors relevant to developed countries.
We’ll also compare the results of the Lancet research with those of another study from the Harvard School of Public Health.9 The latter used the statistical technique of “meta-analysis” to estimate differences in life expectancy due to various risk factors. This involves aggregating all the available information from all previously published research. The figures in the last column of table 1 show the results of both studies (cheating a little, as the Harvard study didn’t include alcohol, fruit and vegetable consumption, or occupational risk).
Table 1 Major risk factors: Contributions and life expectancy gains
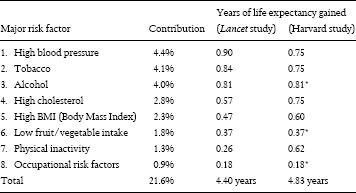
* Numbers from the Lancet study since there was no data for these risk factors in the Harvard study
Table 1 shows us two ways of looking at the effects of risk factors. The first – labeled “contribution” – captures the percentage of variability in total life expectancy associated with each factor in the Lancet study. The big surprise here is that the sum of all eight “major” factors accounts for only 21.6% of the total. In other words, almost 80% remains unexplained and therefore beyond our control. The second and third columns of results (numbers) show the estimated years of life expectancy saved by eliminating each factor – and offer a similar surprise: the maximum expected improvement in life expectancy is only 4.4 or 4.8 years, with high blood pressure, tobacco, and alcohol having the greatest negative effects. The implication is that, in developed countries, all of which have eliminated the biggest risk factors such as malnutrition and poor sanitation, we’re left with little room for improvement!
The conclusions vary slightly, but broadly the studies agree that these eight risk factors – all of which involve some degree of human control – account for around four to five years of extra life expectancy. This might be lower than we’d hoped. But not many people are going to argue about having an additional four or five happy, healthy years.
Hang on a minute, though. If we accept findings like these uncritically, aren’t we falling into the same trap as those people who didn’t dare question their unexpected test results? And shouldn’t we also investigate the quality of medical data available? It’s time to follow our own advice and get some second or third opinions.
In fact, if we look at the other available research, we find that the data on risk factors varies enormously. Let’s start with the effects of cholesterol reduction on life expectancy. A study published in The Journal of the American Medical Association in 2000 underlines the differences in opinion between different researchers.
An assessment of all the cholesterol-lowering dietary trials published in 1987 showed an aggregate 6% more deaths in those who adopted a cholesterol-lowering diet over those on a free diet. A similar review of drug trials showed an aggregate of over 13% more deaths in those taking cholesterol-lowering drugs. At the other extreme, a study analyzing data from 81,488 men between the ages of 18 and 39 years demonstrated a continuous graded association between elevated serum cholesterol and risk of coronary heart disease, cardiovascular disease, and all-cause mortality. Individuals with baseline cholesterol levels of less than 200 mg/dL had a greater life expectancy of 3.8 to 8.7 years.10
The relation between levels of cholesterol, the taking of cholesterol-reducing drugs, and mortality rates is clearly quite confusing. It’s no wonder there’s talk of a “cholesterol myth.”11 In addition, some studies have shown that some cholesterol-lowering drugs are not only ineffective but may even increase the risk of heart attacks while also producing serious, negative side effects.12 There are also concerns about conflicts of interest as drug companies may not be releasing negative evidence about the value of their drugs.13
Surely, though, there’s less controversy about smoking, which has long been accepted as a killer? Research published recently in the British Medical Journal gives non-smokers as much as ten years longer than smokers. That’s nine years more than the Lancet’s estimate.
The excess mortality associated with smoking chiefly involved vascular, neoplastic, and respiratory diseases that can be caused by smoking. Men born in 1900–1930 who smoked only cigarettes and continued smoking died on average about ten years younger than lifelong non-smokers.14
Similarly, those who never exercise would be advised not to read the 2005 back-catalogue of the Archives of Internal Medicine.
Moderate and high physical activity levels led to 1.3 and 3.7 years more in total life expectancy and 1.1 and 3.2 more years lived without cardiovascular disease, respectively, for men aged fifty years or older compared with those who maintained a low physical activity level. For women the differences were 1.5 and 3.5 years in total life expectancy and 1.3 and 3.3 more years lived free of cardiovascular disease, respectively.15
As for the overweight, the Annals of Internal Medicine painted a bleak picture in 2003.
Large decreases in life expectancy were associated with overweight and obesity. Forty-year-old female nonsmokers lost 3.3 years and forty-year-old male nonsmokers lost 3.1 years of life expectancy because of overweight. Forty-year-old female nonsmokers lost 7.1 years and forty-year-old male nonsmokers lost 5.8 years because of obesity.16
Finally, the cheerily titled journal Hypertension had bad news in 2005 for those with high blood pressure.
Irrespective of sex, fifty-year-old hypertensives compared with normotensives had a shorter life expectancy, a shorter life expectancy free of cardiovascular disease, myocardial infarction, and stroke, and a longer life expectancy lived with these diseases. Normotensive men (22% of men) survived 7.2 years (95% confidence interval, 5.6 to 9.0) longer without cardiovascular disease compared with hypertensives and spent 2.1 (0.9 to 3.4) fewer years of life with cardiovascular disease. Similar differences were observed in women.17
Now let’s put the results of these separate studies together in our own table (table 2).
On these five risk factors alone, we get a total potential gain in life expectancy of over thirty-two years! How can this be? Was there something wrong with the way the studies were conducted? Or is there a flaw in the statistical reasoning? Which, if any, studies can we trust? We’ll return to these questions later. For now, let’s look at a few other well-known life-expectancy brain-teasers.
Table 2 Major risk factors: Summary of years of life expectancy saved
Major risk factor |
Years of life expectancy saved |
1. Smoking |
10.0 |
2. High blood pressure |
7.2 |
3. Obesity (average of men/women) |
6.45 |
4. High cholesterol (average) |
6.25 |
5. Physical activity (average of men/women) |
2.5 |
Total |
32.4 years |
Medical researchers and statisticians have always had problems explaining the data for certain countries. Take Japan, for instance. The Japanese per capita consumption of cigarettes is among the highest in the world, yet Japanese life expectancy is also the highest (at least for larger countries). If the British results, which – if you remember – give non-smokers a ten-year edge over smokers, were applicable, Japanese women, 41% of whom smoke, could expect to live an extra four years on average. That would take them up to an incredible eighty-nine-year life expectancy. Overall life expectancy in Japan would exceed eighty-six, if both men and women didn’t smoke. And if we could rule out all the other risk factors, Japanese life expectancy would rise to well over 100 on the basis of table 2.
In the international smoking league tables, the first place goes to Greece, while Norway has the smallest per capita cigarette consumption in the developed world. Yet life expectancy in Norway is only three and a half months longer than in Greece, a country where physical exercise is famously unpopular and where hospital access is patchy – many islands don’t have hospitals at all.
What about high-fat diets and cholesterol intake? France is perhaps the most well-known paradox in this respect. Life expectancy in Metropolitan France is more than eighty years – the tenth highest in the international rankings – although the French diet is notoriously rich in fat. If we go into further detail, we find that deaths from cardiovascular disease are lower than in other nations (39.8 per 100,000 as opposed to 196.5 per 100,000 in the USA). In particular, Périgord, the region in south-west France famous for producing the high-cholesterol delicacy foie gras, has a particularly fatty diet, with plenty of butter, and duck and goose products. Yet life expectancy is higher than in the rest of France and cardiovascular death rates even lower. Back on the national scale, if we compare France to Norway, we find that per capita cigarette consumption is 2.8 times higher in the former, and fat intake significantly lower in the latter. But – you guessed it – the French live on average about a year longer than Norwegians. The only possible conclusion is that there must be factors other than smoking and cholesterol to explain the difference in life expectancy between France (and in particular Périgord) and the USA, Norway, or many other developed nations, where public health campaigns against these two “vices” have had more effect.
By focusing entirely on the negative aspects of the risk factors – and the worst-case scenarios at that – these public health campaigns tend to raise falsely positive expectations about how we individuals can improve our chances of living longer. The message may be that “doctor knows best.” But the deeper we dig into the evidence, the most charitable interpretation is the “doctor is telling us to be on the safe side.” And, strangely, there’s been comparatively little medical research about why the Japanese, Greeks, and French live longer than medical research suggests they ought to. If we’re going to make reasoned choices about how to live our lives, we need more objective and accurate cost-benefit analyses of the many different activities that influence longevity.
The plot thickens yet further, when we begin to look at changes in medical advice over time. Nor do we have to go back to 1685 and the eccentric treatment of Charles II (where we started this chapter), to find doctors changing their minds. If we look at just a few examples from living memory, we see radical and inexplicable shifts in the positions taken by the medical profession.
Take coffee, for instance. Is it good or bad for you? Since the 1950s, coffee has been linked with heart disease and cancer. But the most recent studies – and the resulting hundreds of newspaper articles across the world – suggest that drinking coffee can prolong life, reducing the risk of conditions as diverse as heart problems, type-two diabetes, Parkinson’s disease, cirrhosis of the liver, asthma, and even ovarian cancer.18 Coffee is no longer a guilty pleasure, but a beneficial dietary supplement . . . at least until next year.
So how about salt? The website of the American Food and Drug Administration (FDA), part of the US Department of Health and Human Services, documents the controversial history of medical advice on salt intake and its harmful effects, notably high blood pressure. As early as 1998, a meta-analysis published by the Journal of the American Medical Association suggested that “restricting dietary sodium intake” has only a minimal effect on blood pressure.19 However, the study was immediately attacked as having methodological flaws. The debate rages on right up to the present day. Indeed, the FDA is currently not making any recommendations on how high or low Americans’ daily intake of salt should be. They talk instead about moderation and point out that eating less salt is clearly not harmful for the healthy, normal adult. Whether this advice is evading the issue or a tacit admission of the lack of evidence, it at least has the merit of being honest.20
And so to surgical procedures. Tonsillectomy was a very common practice up until the 1980s. Millions of people (mostly children) had their tonsils whipped out if they regularly became infected and swollen. Back in the 1920s some general practitioners even treated it as a preventive measure, performing tonsillectomy on toddlers in the same way that we vaccinate today. Nowadays, however, the surgical removal of tonsils is rare and only recommended for those with severe throat problems or sleep apnea (a disorder that involves lapses in breathing during sleep). The reason for the decline is that researchers noticed the health of children in geographical areas where the operation was common was no better than in those regions where it was rarely performed.21 Not that this has stopped the debate. Much of the literature for throat specialists is for removing tonsils, while pediatricians are generally against. If this conflict comes as a surprise, remember what we said earlier about vested interests.
At least vitamins are still good for you. Or are they? There’s certainly a huge international industry devoted to dietary supplements – and people say the market is usually right (even if the medical profession sometimes gets it wrong). However, a new meta-analysis of forty-seven research projects, involving 180,938 people who were randomly assigned real vitamins in varying doses or dummy pills, questions prevailing belief. It concludes that the three antioxidant supplements, vitamin A, vitamin E, and beta-carotene, can’t be recommended and that taking them may even increase mortality rates!22
Another more recent study of nearly 300,000 men showed that taking multivitamins more than seven times a week increased the risk of advanced and fatal prostate cancer. The study concluded that heavy multivitamin users were almost twice as likely to get fatal prostate cancer as men who never took the pills.23
In order to figure out whom to trust in these shifting sands of advice, we should probably ask why the medical profession changes its mind so often. Let’s try to find the answer by looking at one particularly extreme example. In 2004, USA Today typified the press coverage of a major study about obesity in America with a story entitled “Obesity on Track as No.1 Killer”. The tabloid cited a study from the Journal of the American Medical Association stating that poor diet and physical inactivity had accounted for 400,000 deaths in 2000 compared with 435,000 deaths from tobacco.24
However, just one year later, a study by different researchers also appeared in the Journal of the American Medical Association. This study estimated that the effect of obesity was only 26,000 more deaths per year – one-fifteenth of the original estimate.25 Although publicity raged on using the old numbers, a spokesperson for the Centers for Disease Control and Prevention (whose researchers were involved in both studies) told The New York Times that the agency wouldn’t take an official position on the new paper, because “We’re too early in the science.”26 One reason for the difference between the two studies was that the second also took into consideration the lower mortality risk rate of people who are overweight (but not obese) compared to those who are normal/thin. In other words, there are advantages to not being thin. As stated in an editorial in The New York Times, “excess pounds may have prevented some 86,000 deaths annually. That estimate has exploded like a bombshell amid the health officials struggling to control the undeniable upsurge of obesity here and abroad. It leaves the CDC, in particular, with a lot of explaining to do . . . The whole notion of what constitutes normal weight and overweight may have to be rethought.”27
Another recent study on the topic, published in the American Journal of Public Health found:
The mortality risk among ‘normal’ weight men (i.e., those in the BMI ‘Body Mass Index is used to define normal, overweight and obese people’ range of 20 to 25 kg/m2) was as high as that among men in the mild obesity category (BMIs of 30–35 kg/m2), with a minimum risk observed at a BMI of approximately 26 kg/m2. Among women, the mortality risk was smallest at approximately 23 to 24 kg/m2, with the risk increasing steadily with BMIs above 27 kg/m2. In each specification, the slope of the line was small and volatile through the BMI range of 20 to 35 kg/m2, suggesting negligible risk differences with minor differences in weight for much of the population.28
In other words, this study found negligible differences in life expectancy between people considered to be of normal weight and those overweight, or even in the mild obesity category. The study also found that even fully obese people could expect to live longer than previous research had indicated. The conclusions are startling and have far-reaching consequences, since overweight and mild obesity are all associated with high cholesterol, high blood pressure, and inactivity:
The present results highlight previous findings indicating that mild obesity and overweight are not strongly related to mortality. In addition, one cannot assume that a risk measured for a person with a BMI of 35 (a person with a BMI of 35 is considered to be in the mild obese category) should concern a person with a BMI of 30, especially when the personal and economic costs of weight loss are high. It would be more reasonable to focus on the smaller group of people in the severely obese category (BMIs of 40 and over; 3.3% of adults in 2002), which has a clearer relationship to mortality; however, some of this association, too, might be contaminated by omitted variables.
The author of the study also refers to previous findings, going back to 1996, indicating that the relation between mild obesity and mortality is not strong. It’s puzzling that we hear so little about this side of the story amidst all the doom and gloom from the media and policy makers.
There is a final twist in the overweight/life expectancy saga. In November 2007, a new article was published in the Journal of the American Medical Association entitled “Cause-specific excess deaths associated with underweight, overweight, and obesity.”29 One of the conclusions of this article is the following:
Overweight was associated with significantly decreased mortality from noncancer, non-CVD causes (-69 299 excess deaths; 95% Confidence Intervals, -100 702 to -37 897) but not associated with cancer or CVD mortality.
Finally, another recent study conducted on older adults concluded the following:
We observed that fit individuals who were obese had a lower risk of all-cause mortality than did unfit, normal weight, or lean, individuals.30
In other words, while in 2003 overweight was considered to decrease life expectancy by more than three years and have little or no influence on life expectancy in 2006, the new studies now suggest that it is now associated with increased life expectancy. These types of contradictory claims over time seem to be unnervingly prevalent in medicine.31
In defense of the scientists, we have to conclude that they’re working in an imperfect world. They’re under pressure to publish their work and publicize their findings. And the chances of doing so are much higher if they can come up with some surprises or dramas. A 400,000 annual death rate, making obesity the number two or three killer in the USA (and on its way to becoming number one in a few years), is much more newsworthy than 26,000 (about the same as chronic liver disease). At the same time, the 26,000 figure is counter to the interests of all those who are advising on the merits of diets and the dangers of high cholesterol. It’s also bad news for the companies which market drugs for weight loss, cholesterol reduction, and heart disease. And if this is happening for obesity and overweight, it’s probably true in many other areas of healthcare.
We’re not here to support the conspiracy theorists. We simply wish to inform reasonable people like you who want to improve your health, live longer and spend less money on doctors and medicines. All we’re saying is that pressures from doctors, the media, the pharmaceutical industry, and society in general are sufficient to explain why the apparent certainty of medical science is just another illusion. Skepticism is not simply justified. It’s advisable.
And that’s before we take errors in scientific and statistical reasoning into account. Back in the 1960s, US scientists carried out the first large-scale study of mammography, involving 62,000 women.32 One half received mammography and physical breast examination by a doctor, while the others weren’t even aware that they were part of the research. During ten years of follow-up, the death rate from breast cancer was 23% lower in the screened women than in the control group. That sounds pretty conclusive! It was certainly enough to inspire an official recommendation of mammography tests for all women.
Yet, when we look at the numbers, doubts begin to creep in. In the tested group there were 147 breast cancer deaths. In the control group there were 192 – that’s 45 extra deaths (and 45 is 23.4% of 192, hence the figure of 23%). Or stated in other terms, the reduction in deaths from breast cancer was about 7 in every 10,000 women. Put it this way and the numbers start to look smaller – and less statistically important. Of course, if you’re an individual woman who believes her life was saved by screening, it’s definitely going to seem worth it. But from a public policy viewpoint, advice recommending mammography tests for all women starts to look questionable, even if we disregard the costs and discomfort of testing.
But the story doesn’t end here. The results of two subsequent studies in Canada, involving 90,000 women, showed that routine mammography testing had no effect on breast cancer mortality, even for the highest-risk age group of fifty to fifty-nine years of age.33 Finally, the Cochrane Collaboration, a respected, international, not-for-profit organization dedicated to providing independent information about healthcare, audited the original 1960s study. It found two major flaws in the research. The corrected results provided no evidence at all that mammography screening reduces breast-cancer-related deaths.34 Yet many doctors still recommend mammography!
Now consider the results of a study published in the prestigious New England Journal of Medicine in March 2009 that investigated the efficacy of screening for prostate cancer.35 It compared 76,693 men split into two groups. Men in the first group were screened regularly; those in the second group were not. After ten years of follow-up, the researchers calculated the numbers of prostate cancer deaths in the two groups. Surprisingly there were slightly more deaths among those in the first group. Regular screening for prostate cancers did not seem to be useful in this large scale study.
At the same time, there was another, even bigger study involving 162,387 men conducted in several European countries.36 There were 214 men who died from prostate cancer among those in the screened group versus 326 in the second, control group. Since there were 112 (326–214) less deaths among those screened, the relative reduction in deaths was 20.7% (112/540 = 20.7%, where 540 = 326 + 214). This 20.7% seems a huge reduction but this percentage, as with the reduction in breast cancers, is misleading. In absolute terms, the reduction in death rates is tiny as there were 162,387 men in the study and only 112 less deaths between the men in the two groups. In other words, for every 1,000 men there were about 0.7 less cancer related deaths,37 or alternatively 1 death less for each 1,429 screened for prostate cancer. Worse still, it is impossible to know in advance which of the 1,429 is the lucky one.
According to the authors of the study this 0.7 decrease per 1,000 was achieved at a high cost as “1,410 men would need to be screened and 48 additional cases of prostate cancer would need to be treated to prevent one death from prostate cancer”. There is a big cost, therefore, when screening for prostate cancer even if 0.7 lives per 1,000 are saved in doing so. Regrettably, however, as with breast cancer, physicians rarely explain the tiny improvement due to screening and the possible negative consequences involved.
Vested interest and human error aren’t the only grounds for doubt in the field of medicine. Sometimes it’s just impossible to unravel the tangle of different factors at work. Nowhere is this truer than in healthcare research. If we look back to the research on high blood pressure published in Hypertension in 2005 (see above), we find that the authors are honest about the limitations of their data. On the one hand, they say, “Our findings underline the tremendous importance of preventing high blood pressure and its consequences in the population.” On the other hand, they admit the following:
Most of the data used in our analyses were collected at least 3 decades ago. The historic character of the Framingham studies limits the extrapolation of the findings obtained through analyses of the Framingham studies to today’s populations. Great advances in health promotion and in the diagnosis, prevention, and treatment of CVD [Cardiovascular Disease] have occurred since the Framingham studies started.38
Framingham is a town in Massachusetts, where three generations of the population have so far participated in research into cardiovascular disease. It’s a wonderful scientific project that is still underway. Nonetheless, the figures used in the study we’ve quoted date back to the 1970s and simply aren’t representative of the population in general today. Page 283 of the lengthy paper lists the characteristics of the sample. The subjects are divided into three groups: one with normal blood pressure, the second high-to-normal, and the third high. The average height in each group (172 or 173 cm for men and 159 or 160 cm for women) is fairly representative of the current US population. But their weights vary considerably. Less than half of the men with normal blood pressure are overweight, while three-quarters of those in the high-blood-pressure group are overweight. There are similar differences between the groups of women. Even if the authors were able to “adjust” for weight, as they claim, the groups would still fail to be representative.
There’s also something strange about the respective sizes of the three groups. Only 22% of the men and 26% of the women surveyed had normal levels of blood pressure. Is this possible? But the major problem with the data is the number of smokers. Across the sample, smoking rates are more than twice as high as they are in the USA currently. In particular, 81% of the men and 53% of the women in the groups with normal blood pressure were smokers. Even in Greece we don’t find figures that high today! And when we look at the high-blood-pressure group, we find the proportion of current smokers is lower (74% for men and 38% for women). Should we conclude that smoking reduces high blood pressure and can be recommended? Of course not. But you really have to wonder about the relevance of the data.
Now maybe this well-respected study is perfectly good as a self-contained piece of research. What we’re questioning is its suitability as the basis for recommendations made to the general public today. The data are not only thirty years old but highly unrepresentative of the current US population, let alone that of Greece or Périgord. After all, as we’ve seen, even its authors warn against extrapolating from their results. Yet doctors do, terrifying people that their high blood pressure will lead to an early death – a stressful situation which probably makes their blood pressure even higher!
Shifting opinions, human weakness, and statistical minefields all seem to point in the direction of pessimism. It’s starting to look bleak for those who want to take positive action to improve their health. But there’s no need to become fatalistic. Our message is not that there’s nothing you can do – just that received medical wisdom is downright uncertain. So, in the next chapter, we make some positive recommendations – about adopting a more scientific outlook, analyzing what medical tests really mean, gathering different opinions, and incorporating the inherent uncertainty of medicine into your outlook. In other words, we offer a spoonful of sugar to help the medicine go down. At the same time, we insist that you take medical science with the proverbial pinch of salt. After all, who’s to say that a pinch of salt is bad for you?