66
Critical incidents
A survey in the US showed that medical errors were responsible for 98 000 deaths per year, i.e. more people die in a year in the US from medical errors than from motor vehicle accidents or breast cancer.
In a prospective study of pediatric admissions to hospital, potential adverse events were highest in the NICU (neonatal intensive care unit):
- 91% of admissions had a medication error
- 46% of admissions had a potential adverse event
- 74% of errors involved physician ordering.
Neonatal critical incidents which may relate to fetal or obstetric care will need to be considered in conjunction with maternal–fetal medicine, e.g. hypoxic–ischemic encephalopathy or seizures within 48 hours of birth. Other aspects of quality improvement involving neonatal care are considered in Chapter 65.
The most common critical incidents are medication errors and extravasation injuries, but a selection of frequent or important examples follows. Some approaches to their prevention are given, but each critical incident will need to be considered by the multi-disciplinary risk management team.
Prevention of critical incidents requires a culture of safety throughout the unit (Fig. 66.1). Being honest and open with parents is vital.
Fig. 66.1 Requirements of a culture of safety in the neonatal unit.
(Adapted from J. Horbar, Vermont–Oxford Network.)
Extravasation of intravenous infusions (Figs 66.2 and 66.3)

Fig. 66.2 Extravasation injury.

Fig. 66.3 Scarring from extravasation injury.
Cause
- Fragile tissues.
- Small catheter, difficult to fix securely.
- Movement by infant.
- Irritant infusion – e.g. calcium, high concentration of dextrose, parenteral nutrition.
Prevention
- Expert fixation of catheters.
- Leave potential extravasation area visible.
- Avoid occluding limb with tape.
- Regular checks, pressure-sensitive alarms.
- Give irritant infusions via central lines if possible.
What to do if extensive extravasation
- Aspirate cannula.Flush affected area with saline via several skin punctures. Some centers inject hyaluronidase into extravasation site. Elevate affected limb.
- Consult plastic surgeons if concern about long-term scarring.
Excessive fluid volume infused
Cause
- Incorrect settings on pump.
- Malfunction of pump.
Prevention
- Electronic ‘guard-rails’ built into pumps (max and minimum rate based on infusion).Check and monitor infusion.
Giving wrong breast milk to wrong patient
Cause
- Similar patient names.
- Poor labeling.Multiple milk containers kept in same fridge.Inadequate checking procedures.
Prevention
- Clear labeling.
- Double-checking.
- Warning mechanism (name alert tags) for staff if babies have similar names.
- Electronic milk storage and dispensing systems.
What to do if occurs
- Inform parents.
- Test donor mother for blood-borne viruses.
Complications of umbilical arterial catheters (UAC)
Incorrect vessel
- Inserted into umbilical vein instead of artery.
Prevention
- Check for presence of arterial pulsation to confirm in artery and arterial waveform on monitor.
- Check position on abdominal X-ray (Fig. 66.4).
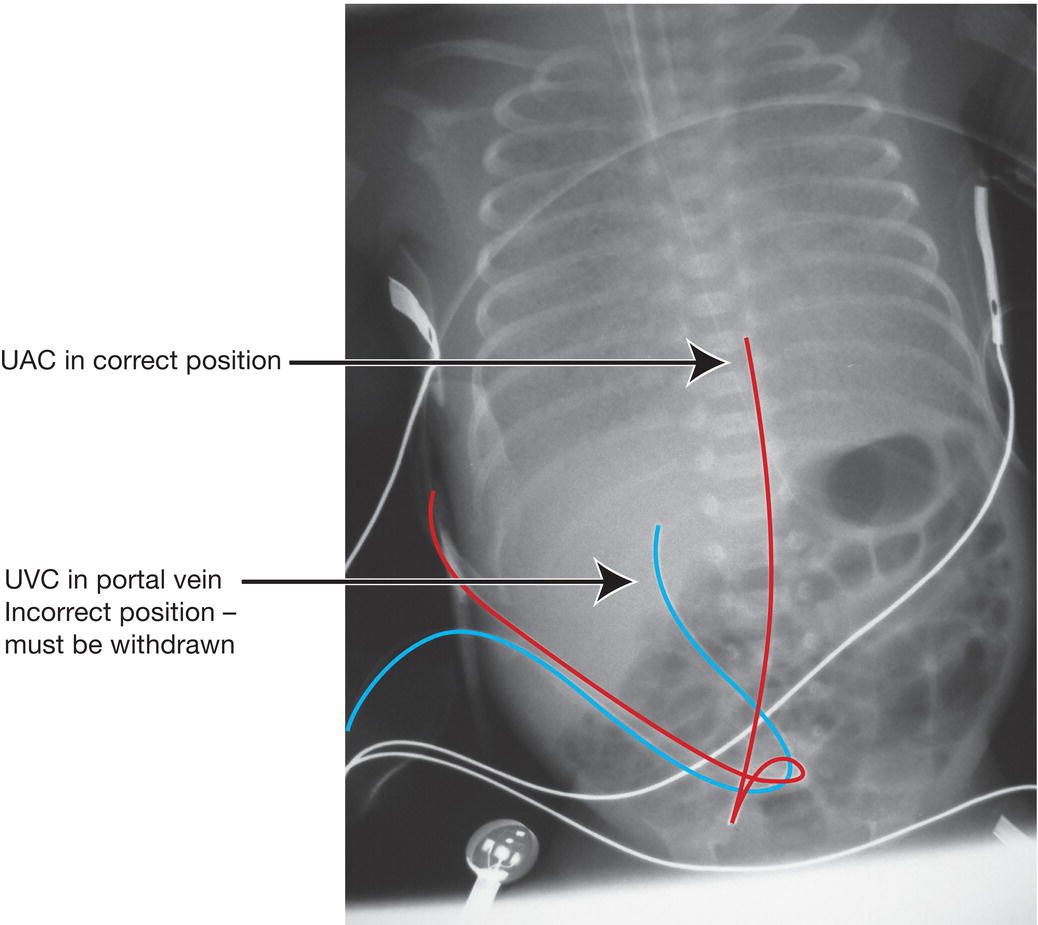
Fig. 66.4 X-ray showing umbilical arterial and venous catheters. Catheter in umbilical artery (red line) – initial course caudally towards groin, then cranially up middle of spine. Catheter in umbilical vein (blue line) – cranial course to right of spine. This catheter is in the portal vein, a potentially dangerous position, and must be withdrawn. In addition, overlapping catheters, as shown here, can easily lead to misinterpretation.
This is important – if in umbilical vein by mistake, excessively high oxygen could be given, which could damage eyes (retinopathy of prematurity, ROP) if preterm.
Thrombosis/emboli/vasoconstriction
Consequences
- Occlusion of the artery causes mottling of skin, loss of pulses, cool limb and cyanosis in one or both legs. May result in gangrene/amputation of limb.
- Emboli may affect distant organs.
Prevention
- Regular observation. If skin becomes discolored, reposition or remove catheter.
- Position catheter either high at T6–10 or low at L3–4 to avoid catheter tip near renal vessels to reduce risk of renal artery thrombosis (hematuria, renal failure, hypertension).
- Flush catheter gently, heparin infusion.
- Ensure infant’s intravascular volume is adequate.
Blood loss from arterial catheters
Cause
- Disconnection of catheter.
Prevention
- Clear labeling that catheter is arterial.
- Connections screwed together.
- Pressure-sensitive alarm.
Ischemic damage from peripheral artery catheters
Cause
- Small size of vessel.Inadequate collateral supply.
Prevention
- Choose suitable artery:
- use radial artery only if ulnar artery shown to be patent (Fig. 66.5) (see Chapter 76 for Allen test).
- avoid superficial temporal artery as can cause ischemia of parietal lobe.
- avoid brachial artery as end artery and occlusion may result in loss of distal limb, and median nerve may be damaged.
- Only use for sampling, not injecting.
- Remove if any significant blanching, other than transient.

Fig. 66.5 Ischemic damage from radial artery catheter.
Portal vein thrombosis from umbilical venous catheters
Cause
- Catheter in portal vein causing portal vein thrombosis.
Prevention
- Check on X-ray that catheter is in the inferior vena cava and not the portal vein (Fig. 66.4).
Extravasation of parenteral nutrition (PN) from central venous lines
Cause
- Catheters may migrate and PN may be infused into:
- – the tissues, causing swelling and inflammation
- – the lungs, causing pleural effusion
- – the pericardium, causing pericardial effusion and tamponade the liver, causing hepatitis.
Prevention
- Check catheter tip is in the inferior or superior vena cava, not the right atrium or portal vein.
Burns and scalds
Cause
- Overheating of humidifier in CPAP/ventilator circuit.
- Disconnection of temperature probe or malfunctioning of radiant warmer (Fig. 66.6).
- Failure to move transcutaneous O2/CO2 probes regularly.

Fig. 66.6 Scalding of skin from excessive heat from radiant warmer after dislodging of skin temperature probe. It resolved within a few hours.
Prevention
- Temperature alarms.
Scarring of skin
Cause
- Poorly keratinized skin prone to long-term scarring, especially if black ethnicity (keloid formation).
Prevention
- Minimize skin damage:
- – care with adhesive tape, regularly reposition probes and avoid undue pressure from attachments for tracheal tubes, nasal CPAP, etc.
- – if transcutaneous O2/CO2 electrodes used, rotate to different skin sites regularly
- – procedures, e.g. chest tube for pneumothorax, avoid breast-bud area (Fig. 66.7).
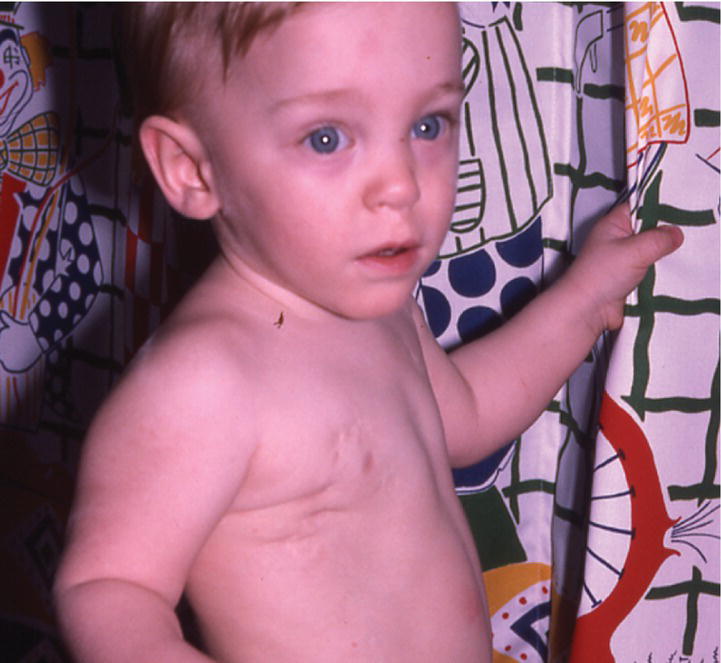
Fig. 66.7 Scarring from chest tubes.
Nasal damage from tracheal tube
Cause
- Dilatation of nostril or damage to the nasal septum by tube.
Prevention
- Avoid excessively large tracheal tubes.
- Avoid leaving in situ for long periods.
- Fix tube securely to prevent leverage.
Nasal damage from nasal CPAP
Cause
- Pressure on nostrils or nasal septum.
Prevention
- Correct positioning, size and fixing of nasal prongs, avoiding excessive pressure on the nostrils or nose, regular repositioning and monitoring.Consider high flow nasal oxygen therapy as causes less nasal trauma.
Tracheal stenosis
Cause
- Damage to subglottic area from tracheal tube (Fig. 66.8).
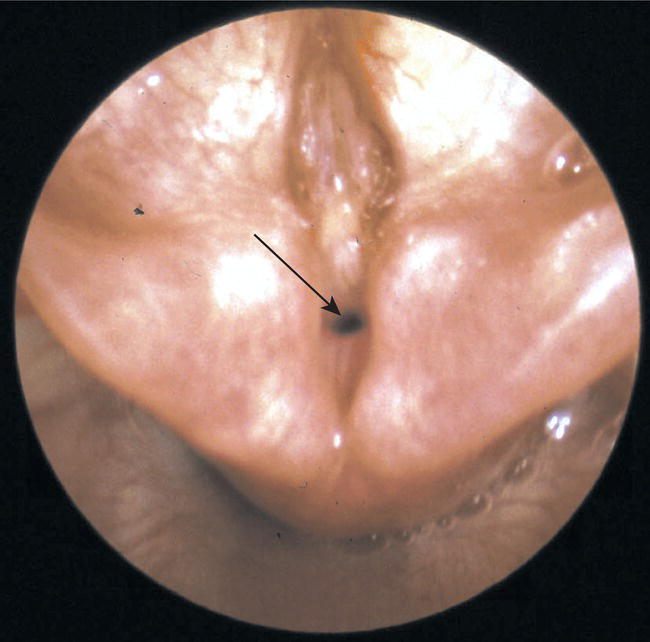
Fig. 66.8 Tracheal stenosis following prolonged mechanical ventilation. The narrowed trachea is shown with an arrow.
Prevention
- Avoid excessively large tubes.
- Minimize time left in place.
- Secure to prevent tube movement and irritation.
Infection
Cause
- Nosocomial infection – inadequate hand-hygiene.
- Catheter related – at insertion or subsequently, e.g. breaking of long line and dressing.
- Procedures – infection where skin denuded from monitor probes or tape.
Prevention
- Meticulous hand hygiene.
- Sterile insertion.
- Minimize interference of lines.
- Remove lines as soon as possible.Care bundles of procedures to minimize infection shown to reduce central line-associated bloodstream infections (CLABSIs).
Aspiration pneumonia from misplaced gavage (nasogastric) feeding tubes
Cause
- Tube inserted into trachea instead of stomach.
Prevention
- Check correct position with pH indicator paper to confirm gastric aspirate is acidic (pH < 5.5).
- If in doubt, X-ray to confirm below the diaphragm and in the stomach to the left of mid-line.