Delirium and Dementia
Perspective
Emergency physicians are frequently presented with patients exhibiting neurobehavioral abnormalities. These can be a harbinger of a serious medical condition, and critical decisions must be made expeditiously about diagnostic evaluation, therapeutic intervention, and disposition. The first critical action is to recognize the presence of the neurobehavioral abnormality. The second is to distinguish delirium from dementia or some other neuropsychiatric condition.
In the past, terms such as acute confusional state, sundowning, and organic brain syndrome have been used to describe a host of abnormal cognitive states that can be observed in the emergency setting. These terms have loosely defined a group of neurobehavioral disorders that are caused by a physiologic disturbance. Organic brain syndrome is a nebulous term that the Diagnostic and Statistical Manual of Mental Disorders (fourth edition, text revision) eschews because the “organic” connotation implies that so-called functional mental disorders are without a biologic basis.1
Several key features best distinguish delirium from dementia: the time course of disease evolution, the presence of autonomic system involvement, the level of consciousness, and the presence of an underlying disease processes. Delirium is characterized by a fluctuating level of neurobehavioral disturbance typically progressing during minutes to hours to days. Delirium is a direct consequence of an acute systemic or central nervous system (CNS) stressor. Dementia, on the other hand, tends to follow a more gradual course, with evolution during months to years. Although patients with dementia exhibit confusion, disturbance in level of consciousness usually is not a feature, and manifestations of autonomic nervous system abnormalities are minimal or absent.
The evaluation of patients who present to the emergency department (ED) with a disturbance of neurobehavioral state is best conducted in accordance with the following basic guidelines:
1. The first step is to determine whether this state represents delirium or dementia. The clinical findings may be subtle, and establishment of the diagnosis can be challenging, especially because delirium may be superimposed on dementia and dementia remains an independent risk factor for delirium.2,3 Early symptoms and signs may go unrecognized unless an adequate history is obtained from the patient, family members, and caregivers. A careful examination must include memory and cognitive assessment with a mental status screening examination.
2. Supportive care must be provided. This care may range in extent from aggressive airway and cardiovascular support to pharmacologic or physical restraint to simply placing the patient in a quiet room with appropriate environmental support.
3. A diligent search must be initiated for the underlying precipitating stressors in patients presenting with delirium.
Delirium
Delirium is a syndrome that can be defined as an acute or subacute state of cognitive dysfunction caused by an underlying physiologic condition. Terms that have been used interchangeably with delirium include acute organic brain syndrome, acute confusional state, reversible cerebral dysfunction, metabolic encephalopathy, toxic encephalopathy, and febrile delirium. The word delirium is derived from the Latin delirare, which literally means “to go out of the furrow” (in a more modern sense, “to derail”), but it is used figuratively to mean “crazy” or “deranged.”
Several key features are necessary for a diagnosis of delirium (Box 104-1). Patients with delirium have disturbances in consciousness, memory, cognition, and perception. These disturbances tend to develop during a short time (hours to days). The disturbance in consciousness may be manifested initially as an inability to focus attention. The fluctuating course of symptoms and inattention are the hallmarks of delirium. Deficiencies in cognition may be manifested by disorientation and memory deficits. Perceptual disturbances include hallucinations and delusions. The delirious patient may be somnolent or agitated, and the thought process may range from mildly disturbed to grossly disorganized. The clinical presentation may be subdued or explosive. The patient's sleep-wake cycle may be altered or reversed; agitation often is present during the night. Historically, delirium referred to a hyperactive state marked by agitation and emotional lability (e.g., delirium tremens). An important point, however, is that delirium has several psychomotor subtypes: hyperactive (mania), hypoactive (depressed), and mixed type.4
The exact incidence of delirium in the overall ED population is unknown. However, the prevalence of delirium among elders who present to the ED is approximately 10 to 20%.5 Geriatric patients are at particularly high risk for the development of delirium. Advanced age, dementia, and underlying medical illness are strongly associated with delirium. Multiple medications, drugs, and alcohol also are associated with delirium.6 Severe psychological stress and sleep deprivation may facilitate the development of delirium.
Pathophysiology
At a cellular level, delirium is the result of widespread alteration in cerebral metabolic activity, with secondary deregulation of neurotransmitter synthesis and metabolism. Both the cerebral cortex and the subcortical structures are affected, producing changes in arousal, alertness, attention, information processing, and the normal sleep-wake cycle.
Although the exact pathophysiologic process is not well understood, multiple neurotransmitters have been implicated in causing delirium. One theory is that delirium is associated with a derangement of central cholinergic transmission. Serum anticholinergic activity is increased, and low levels of acetylcholine are seen in older patients with delirium.7 Increased serotonin levels have been found in hepatic encephalopathy, serotonin syndrome, sepsis, and psychedelic drug ingestion.8 Some of the disturbances that occur in delirium are deficiencies of substrates for oxidative metabolism (e.g., glucose, oxygen); disturbances of ionic passage through excitable membranes; increase in cytokines; imbalance of normal noradrenergic, serotoninergic, dopaminergic, and cholinergic homeostasis; and, in some cases, synthesis of false neurotransmitters.9 Drugs and exogenous toxins can produce delirium through direct effects on the CNS. Although the limbic system appears to be particularly vulnerable to the effects of these drugs, the cerebral hemispheres and the brainstem also can be profoundly affected.
Tricyclic antidepressants can cause delirium by cholinergic inhibition; sedative-hypnotics depress activity in the CNS, especially in the limbic system, thalamus, and hypothalamus. Narcotics affect CNS activity primarily by interacting with various opioid receptor sites. Depending on the opioid receptor type affected, the physiologic response may be analgesia, euphoria, sedation, dysphoria, delusions, or hallucinations. Psychedelic drugs probably act as agonists at serotonin receptor sites. Phencyclidine (PCP) inhibits reuptake of dopamine, norepinephrine, serotonin, and α-aminobutyric acid and also may act as a false neurotransmitter.
Hyperthermia and hypothermia can cause delirium, probably as a result of changes in the cerebral metabolic rate. In hypothermia, cerebral metabolism decreases 6 to 7% for each 1° C decrease in temperature from 35 to 25° C. In hyperthermia, cellular damage with uncoupling of oxidative phosphorylation begins to occur at temperatures higher than 42° C. Patients suffering from heatstroke may have cerebral edema, degenerative neuronal changes (especially involving Purkinje cells of the cerebellum), and petechiae in the walls of the third and fourth ventricles. Delirium occurring at temperatures below 40° C is multifactorial in origin and not caused solely by increased core temperature.
Delirium caused by metabolic abnormalities, such as hyponatremia, hypernatremia, hyperosmolarity, hypercapnia, and hyperglycemic disorders, is associated with a variety of metabolic disturbances at the neuronal and astrocyte levels. Such disturbances may include impairments in energy supplies, changes in resting membrane potentials, changes in cellular morphology, and changes in the brain water volume.
Most patients with delirium have reduced cerebral metabolic activity. This reduction in cerebral metabolism is reflected by a decrease in the frequency of background electrical activity on the electroencephalogram (EEG). Exceptions are hyperthermia, sedative-hypnotic withdrawal, delirium tremens, and certain drug-induced states, in which the cerebral metabolism is either normal or increased.
Etiology
The causes of delirium are legion (Table 104-1). Within the geriatric population, medications are a common cause of delirium, whereas drugs (including ethanol) are the most common cause of delirium in the younger adult population. Acute cognitive dysfunction may be secondary to drug overdose, withdrawal syndromes, and adverse or idiosyncratic reactions.
Table 104-1
Causes of Delirium: “I Watch Death” Mnemonic
| CAUSE | FORM |
| Infectious | Sepsis, encephalitis, meningitis, syphilis, central nervous system abscess |
| Withdrawal | Alcohol, barbiturates, sedative-hypnotics |
| Acute metabolic | Acidosis, electrolyte disturbance, hepatic or renal failure, other metabolic disturbances (↑ or ↓ glucose, magnesium, calcium) |
| Trauma | Head trauma, burns |
| CNS disease | Hemorrhage, stroke, vasculitis, seizures, tumor |
| Hypoxia | Acute hypoxia, chronic lung disease, hypotension |
| Deficiencies | Vitamin B12, hypovitaminosis, niacin, thiamine |
| Environmental | Hypothermia, hyperthermia, endocrinopathies (diabetes, adrenal, thyroid) |
| Acute vascular | Hypertensive emergency, subarachnoid hemorrhage, sagittal vein thrombosis |
| Toxins or drugs | Medications, street drugs, alcohol, pesticides, industrial poisons (e.g., carbon monoxide, cyanide, solvents) |
| Heavy metals | Lead, mercury |
Modified from Wise MG: Delirium: Differential diagnosis for delirium: Critical items (I WATCH DEATH). In: Yudofsky SC, Hales RE (eds): The American Psychiatric Press Textbook of Neuropsychiatry, 2nd ed. Washington, DC, American Psychiatric Publishing, 1992.
The list of commonly prescribed drugs causing delirium is extensive and includes antibiotics (antifungal, antimalarial, and antiviral agents; numerous antibacterial agents, including the quinolones and macrolides), anticholinergic drugs (antihistamines, antispasmodics, muscle relaxants, tricyclic antidepressants), anticonvulsants, anti-inflammatory agents (corticosteroids, salicylates, and other nonsteroidal anti-inflammatory drugs), various cardiovascular medications (beta-blockers, antidysrhythmics, antihypertensives, cardiac glycosides), sympathomimetics (phenylpropanolamine), sedative-hypnotics, narcotics (transdermal fentanyl [Duragesic], morphine sulfate [Roxanol], hydromorphone HCl [Dilaudid], oxycodone HCl [OxyContin]), miscellaneous drugs (aminophylline, cimetidine, lithium, chlorpropamide), over-the-counter medications with anticholinergic properties, and caffeine-containing products.6
Many “street drugs” with significant abuse potential, such as hallucinogens, amphetamines, PCP, cocaine, and methylenedioxymethamphetamine (MDMA, ecstasy), can cause delirium, as can intoxication with any of the alcohols (e.g., ethanol, methanol, ethylene glycol).
Exposure to industrial chemicals (e.g., carbon disulfide, heavy metals, insecticides, cyanide, carbon monoxide) can cause a wide range of symptoms that include acute delirium. In addition, ingestion of certain plants (e.g., nutmeg, foxglove, jimsonweed, psilocybin-containing mushrooms) can cause delirium.
Delirium can be one of the protean manifestations of a metabolic or nutritional abnormality. The most common metabolic disorder causing acute cognitive changes is diabetes mellitus. Hypoglycemia is the most common and readily reversible cause of acute confusion in the diabetic patient. Other causes of acute cognitive impairment in the diabetic patient are hyperglycemia, hyperosmolarity, and acid-base abnormalities. Severe metabolic abnormalities, including electrolyte disturbances, hypoxemia, hepatic insufficiency, renal insufficiency, and dysfunction of various endocrine glands (hyperthyroidism, hypothyroidism, Cushing's syndrome, hyperparathyroidism, and other endocrine disorders), can cause delirium. Deficiency of niacin, pyridoxine, folic acid, or vitamin B12 may be associated with an acute confusional state.
Delirium can be a prominent feature of any systemic infection, particularly in the very young, elders, and immunocompromised patients. Infectious and host factors together determine the degree of cognitive impairment. Extracranial infections that are associated with delirium include sepsis (particularly gram-negative sepsis), subacute bacterial endocarditis, Legionnaires' disease, Rocky Mountain spotted fever, malaria, typhoid fever, toxic shock syndrome, and several viral infections including influenza. Patients with CNS infections, including meningitis, encephalitis, and intracerebral abscess, may have acute cognitive dysfunction.
Another less common cause of delirium is CNS infarction in the distribution of the nondominant middle cerebral artery and the posterior cerebral artery. In patients who have a collagen vascular disease with CNS vasculitis, neuropsychiatric manifestations, including acute delirium, may be prominent. Paraneoplastic syndromes may include encephalopathy, with symptoms of confusion, catatonia, and dementia.
Patients who are immunocompromised may have multiple and unusual causes of acute delirium. Patients with immunosuppression secondary to malignant disease, drugs, or human immunodeficiency virus type 1 (HIV-1) infection may have acute brain dysfunction secondary to infection, complications of drug therapy, or the underlying disease itself.
Acute confusional states have been reported to be a more common herald of the onset of physical illness in the elderly than are fever, pain, and tachycardia.2,3,10 Factors that predispose elders to delirium include the effects of aging on the brain, reduced capacity for homeostatic regulation, impaired vision and hearing, and age-related changes in the pharmacokinetics and pharmacodynamics of drugs.11 The etiology of delirium in elders is usually multifactorial.
Clinical Features
The clinical manifestations of delirium are as variable as the causes. The clinical presentation can be so subtle as to go unrecognized or may be dramatic enough to disrupt the entire ED. The natural history of a patient's delirium can progress from apathy to marked agitation in the course of hours (see Box 104-1). Nonspecific prodromal symptoms such as anxiety, restlessness, and insomnia typically emerge during hours to days.
Key aspects of cognitive impairment should become evident during a careful history and examination. Disturbance in attention is central to the diagnosis of delirium. The patient is easily distractible and has difficulty remaining focused on a particular topic or interacting with a single person. Disorientation often accompanies the deficit inattention but is not an invariable feature. The patient usually is disoriented with respect to time and occasionally to place; in extreme cases, disorientation to person also may be noted. Delirium, however, may be present in a patient who is completely oriented to person, place, and time. A mental status examination that consists solely of questions that assess orientation will not detect delirium in these instances.
The patient with delirium always has some degree of memory impairment, with the greatest impact on short-term memory. Thought processes and speech may be disorganized. Disturbance in the sleep-wake cycle often occurs early in the course of delirium. Perceptual disturbances, including misperception of the environment, poorly formed delusions, and hallucinations, are common. The delirious patient may experience visual, auditory, tactile, gustatory, or olfactory hallucinations, in contrast to patients with acute functional psychosis, who typically experience only auditory hallucinations. In addition, the delirious patient has a reduced capacity to modulate fine emotional expression and may demonstrate extreme emotional lability.
The cognitively impaired patient may provide an unreliable history. Valuable information often can be obtained from family, friends, and out-of-hospital personnel. Specific inquiry should be made about the patient's current medical problems and previous medical history, including diabetes, hypertension, kidney or liver disease, and any neurologic or psychiatric problems. It is important to determine whether the patient is immunosuppressed or has risk factors for immunosuppression. A detailed medication history, including the use of prescribed and over-the-counter medications, dietary supplements, and alcohol or other substances, is essential. Out-of-hospital personnel should be able to provide information about the home environment, medication bottles belonging to the patient or found near the patient, and the possibility of trauma.
The physical examination should begin with a careful assessment of vital signs including pulse oximetry and a pain assessment. The delirious patient often exhibits abnormalities on such evaluation, including elevated or decreased pulse, blood pressure, respiratory rate, and temperature. The examination includes assessment of the head for signs of trauma and the pupils for symmetry of light reflex; funduscopic examination for hemorrhage or papilledema; examination of the ears for hemotympanum; evaluation of the neck for nuchal rigidity, bruits, and thyroid enlargement; assessment of the heart and lungs; evaluation of the abdomen for organomegaly and ascites; and examination of the extremities for cyanosis. The skin should be carefully examined for rashes, petechiae, ecchymosis, splinter hemorrhages, and needle tracks. The neurologic examination includes assessment of the cranial nerves, motor strength, sensation, and presence of abnormal movements (e.g., tremor, asterixis, myoclonus). The reflexes are assessed for symmetry and presence of hyperreflexia or hyporeflexia. Findings that typically suggest either a metabolic or a structural neurologic problem are not necessarily specific for that category of disorder. For example, asterixis is a hallmark of metabolic encephalopathy but can be seen in focal brain disease. Likewise, focal neurologic signs that typically are associated with structural CNS lesions also can be present in various metabolic abnormalities, such as hypoglycemia, hyperglycemia, hepatic encephalopathy, uremia, and hypercalcemia.
The physical examination is not often helpful in determining the specific drug or class of drugs causing acute cognitive impairment. The one exception to this rule is toxidromes, which are constellations of signs and symptoms characteristic of intoxication with certain drugs or classes of drugs (see Chapter 147).
A brief mental status examination should be performed in all patients thought to have acute brain dysfunction. Although the concept is rather obvious, few physicians proceed beyond questions about the patient's orientation to person, place, and time when assessing mental status. Failure to diagnose subtle forms of delirium when they are present is directly related to omission of mental status testing.12
Several standardized tools for assessment of mental status have been successfully applied in the ED.12–14 Mental status testing includes assessment of orientation, memory, attention, and concentration; several tests also incorporate assessments of constructional tasks, spatial discrimination, arithmetic ability, and writing. Cognitive functioning can be rapidly assessed in approximately 7 to 10 minutes. Memory assessment requires testing of the patient's ability to repeat short series of words or numbers (immediate recall), to learn new information (short-term memory), and to retrieve previously stored information (long-term memory). Constructional apraxia is assessed by having the patient perform tasks such as drawing interlocking geometric figures or clock faces and connecting dots. Dysnomia (inability to name objects correctly) and dysgraphia (impaired writing ability) are two of the most sensitive indicators of delirium. Almost all acutely confused patients exhibit writing impairments, including spatial disorganization, misspelling, and tremor.13,15
No single bedside cognitive test that can be administered quickly is ideal. The Mini-Mental State Examination (MMSE) developed by Folstein and colleagues has been validated more than any other test and most frequently is recommended as a rapid screening tool.10,13,15,16 For hospitalized patients, this test has a sensitivity of 87% and a specificity of 82% for detection of organic brain syndrome. Some investigators report slightly better results when the test is modified and age is added as a variable in the analysis.16 The MMSE does not measure executive function and is insensitive for detection of early signs of mild cognitive impairment (without dementia) or early dementia.17
The MMSE consists of a short series of questions that test orientation, registration (memory), attention, calculation, recall, and language (Fig. 104-1). The time for the test to be administered can be reduced to 5 minutes by elimination of the writing and drawing components with only a modest reduction in sensitivity. The registration section tests both immediate and short-term memory; the recall section also assesses short-term memory. The ability to recall two of three objects has 81% sensitivity and 74% specificity for exclusion of organic brain syndrome. Asking the patient to subtract “serial sevens” backward from 100 assesses attention, concentration, and arithmetic ability. This test is specific but not sensitive for absence of an organic brain syndrome; up to 40% of nondelirious, nondemented people fail to perform the tasks of this test correctly, reflecting limitations due to language ability and education. A total score of 23 or less is considered markedly abnormal and indicates an organic brain syndrome. As a general rule, patients with mild cognitive impairment have a score of 18 to 26 of 30, those with moderate impairment have a score of 10 to 18, and those with severe impairment have a score of less than 10.
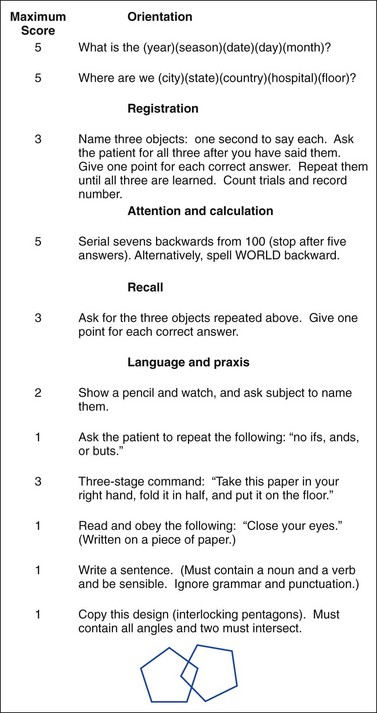
Figure 104-1 Mini-Mental State Examination. (Adapted from Folstein MF, Folstein SE, McHugh PR: “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189, 1975.)
The Quick Confusion Scale represents another attempt to quantify the attention aspects of mental status (see Chapter 17, Fig. 17-2). It has significant correlation with the MMSE, can be administered more quickly, and does not require constructional tasks.18 Another useful diagnostic tool is the Confusion Assessment Method; it has a sensitivity of 93 to 100% and specificity of 90 to 95%.19 This simple tool has four key features used for screening of delirium: acute onset and fluctuating course, inattention, disorganized thinking, and altered level of consciousness. For a definitive diagnosis of delirium, the first two features and one of the last two must be present. It has proved to be a valuable tool because of its ease and interobserver reliability. In addition, it has been shown to be more sensitive than clinical impression alone.18,20 The Six-Item Screener is another brief test of cognition that was found to be 94% sensitive and 86% specific in identifying disturbance of cognition in older patients.15
All bedside tests of cognition have limitations and can miss mild degrees of impairment. The patient's level of education and general intelligence can substantially affect the outcome. Furthermore, a single bedside test reflects a patient's cognitive functioning at only one point in time. For a diagnosis of delirium (or dementia) to be established, an essential criterion is a documented decline from the patient's baseline level of cognitive functioning, and the sensitivity of these tests increases when they are repeated over time.
Diagnostic Evaluation and Ancillary Studies
Some reversible causes of delirium can be diagnosed by a number of basic, readily available tests. The following laboratory tests can be helpful in evaluation of the delirious patient: a complete blood count (CBC; hemoglobin, leukocyte count with differential, platelet count, and mean corpuscle volume), serum electrolyte values, glucose concentration, calcium concentration, and urinalysis. The CBC may suggest unusual but potentially treatable abnormalities, such as thrombotic thrombocytopenic purpura, megaloblastic anemia, hyperviscosity from myelogenous leukemia, and unsuspected infection. The anion gap should be determined in all patients with altered mental status. An elevated anion gap (>15 mEq/L) may indicate the presence of unmeasured anions, such as sulfate in renal failure; keto acids in diabetic or alcoholic ketoacidosis; lactate in postictal states or associated with hypotension; and exogenous toxins, such as ethylene glycol, methanol, and salicylates. A pulse oximetry measurement should be obtained in all patients to screen for hypoxemia, and an arterial blood gas analysis is warranted in those patients at risk for respiratory failure with carbon dioxide retention. Suspected occult infection warrants urinalysis and chest radiography. In elders, an electrocardiogram should be obtained to exclude a silent acute coronary syndrome. Ammonia level should be considered in patients with cirrhosis, ascites, or asterixis. Despite these diagnostic evaluations, no cause is found for delirium in up to 16% of patients.6
Toxicology screens are overused as diagnostic tests and have limited usefulness in the evaluation of most patients with delirium. Additional laboratory studies outside the scope of the ED evaluation that may be appropriate when the cause of delirium remains unknown include thyroid function studies, vitamin B12 and folic acid assays, rapid plasma reagin test, measurement of serum antinuclear antibodies, urinary porphobilinogen assay, and screens for heavy metals.
Patients with a history of trauma (especially those taking anticoagulant medications), previous neurosurgical procedures, immunodeficiency, or focal neurologic signs require a head computed tomography (CT) scan to detect structural lesions causing delirium. Early infarctions, small brainstem lesions, meningitis or encephalitis, closed head injuries, sagittal vein thrombosis, and small isodense subdural hematomas may be missed on a CT scan. In addition, approximately 2 to 8% of acute subarachnoid hemorrhages are not detected by head CT scan and require lumbar puncture for diagnosis. The role of magnetic resonance imaging (MRI) in the evaluation of the delirious patient has not been clearly established. MRI is superior to CT for detection of small intercerebral and brainstem lesions, small brain contusions, certain encephalitides, and abnormalities of white matter (e.g., leukoencephalopathy). MRI perfusion scans are more sensitive in detecting an acute vascular event.
Cerebrospinal fluid (CSF) analysis is an essential part of the evaluation in selected patients with delirium. In patients with fever and cognitive dysfunction, even without meningismus, a lumbar puncture should be performed to rule out meningitis. This test is particularly important in the very young, elders, and immunocompromised patients, who are less likely to show classic signs of meningitis. Patients with focal neurologic deficits, immunocompromised states, or evidence of increased intracranial pressure should undergo head CT before lumbar puncture, and they should receive antibiotics before the CT scan.
Although it is rarely practical in the ED setting, the EEG can be a valuable diagnostic tool in determining the presence of delirium. Bilateral diffuse symmetrical electroencephalographic abnormalities are a relatively consistent feature of delirium. In most cases, the changes consist of a nonspecific generalized slowing from the baseline activity and can be useful in distinguishing delirium from other neurobehavioral abnormalities.
Differential Diagnosis
Considerations in the differential diagnosis for apparent delirium include functional psychiatric disorders and dementia. Depression, mania, paranoia, and schizophrenia all may resemble delirium. Several clinical features are helpful in distinguishing between organic and functional syndromes (Table 104-2).
Table 104-2
Comparison of Delirium and Acute Psychosis
| CHARACTERISTIC | DELIRIUM | ACUTE PSYCHOSIS |
| Onset | Acute | Acute |
| Vital signs | Typically abnormal (fever, tachycardia) | Normal |
| Prior psychiatric history | Uncommon | Common |
| Course | Rapid, fluctuating | Stable |
| Psychomotor activity | Variable | Variable |
| Involuntary activity | Possible asterixis, tremor | Absent |
| Cognition function | ||
| Orientation | Usually impaired | Occasionally impaired |
| Attention | Globally impaired | May be disorganized |
| Concentration | Globally impaired | Impaired |
| Hallucinations | Visual, visual and auditory | Primarily auditory |
| Delusions | Transient, poorly organized | Systematized |
| Speech | Pressured, slow, possibly incoherent | Usually coherent |
| Course | Typically resolves | Responds to therapy, recurrence common |
Dementia, like delirium, is characterized by global cognitive impairment. Unlike delirium, dementia tends to be an insidious process that develops during months to years with little fluctuation during hours or days. Typically, the patient's vital signs are normal. Dementia occurs primarily in the elderly. A point worthy of emphasis is that patients with dementia are five times more likely to develop delirium.2,3,5,6
Management
Delirium constitutes a medical emergency. The outcome depends on the cause of the delirium, the patient's overall health status, and the timeliness of treatment. The presence of hyperactive or hypoactive delirium has some prognostic significance.2 The hypoactive form of delirium tends to be more common in elders and carries a worse overall prognosis, perhaps because it often goes unrecognized. Acute recognition and management of delirium in elders are essential because delirium in this population is associated with increased risk of long-term institutionalization, development of dementia, and increased overall mortality.21
Patients who present with acute delirium should be screened quickly for readily reversible causes, such as hypoglycemia, hypoxia, and narcotic overdose. Acute intoxication from a number of drugs or chemical agents, including tricyclic antidepressants, ethylene glycol, cholinesterase inhibitors, anticholinergic agents, carbon monoxide, and cyanide, requires prompt attention. Although supportive measures are the mainstay of treatment in most poisonings and intoxications, most of these toxins have specific antidotes.
Other conditions requiring immediate medical intervention include infections. Patients with signs of acute meningitis or sepsis should receive antibiotics within 30 minutes of arrival to the ED along with appropriate fluid resuscitation. Other emergent conditions that may be manifested with delirium and necessitate immediate intervention include severe hypothermia, hyperthermia, and CNS vascular conditions, including hypertensive encephalopathy, acute epidural or subdural hematoma, subarachnoid hemorrhage, and stroke. Patients with Wernicke's encephalopathy require immediate treatment with 100 mg of intravenous thiamine, with titration of additional doses until the ophthalmoplegia resolves. Resistance to thiamine may result from hypomagnesemia because magnesium is a cofactor for thiamine transketolase. Glucose administration in patients with severe thiamine deficiency may precipitate Wernicke's encephalopathy. The specific treatment of delirium tremens (and other alcohol withdrawal syndromes) involves the substitution of a long-acting drug that is cross-tolerant with the alcohol. Benzodiazepines are the agents of choice to induce sedation. Delirium secondary to dehydration, hyponatremia, hypernatremia, hypercalcemia, and hepatic or renal disease gradually resolves during hours to days with appropriate treatment.
Supportive care for all patients with delirium includes provision of an appropriate environment with adequate lighting, minimization of sensory overload, placement of the patient in an area that can be easily observed by staff, and use of stretcher side rails to prevent falls. Use of “sitters” may be necessary because patients may require constant supervision. It is important to protect the patient from self-harm or from injuring other patients or staff. In cases of hyperactive delirium, the patient may need to be initially restrained physically until pharmacologic control takes effect. Restraints should be viewed only as a temporizing action because they can increase agitation and the risk of injury to the patient. Physical restraints in agitated patients have been associated with significant injuries and even death by asphyxiation and are not a substitute for pharmacologic control.22,23
Pharmacologic restraint has become the cornerstone of behavioral management. Classes of drugs that have been used for management of delirium include the antipsychotics and benzodiazepines. The ideal sedating drug should have the following characteristics: low toxicity with minimal anticholinergic effects, ease of administration, short half-life, minimal effects on the cardiovascular and respiratory systems, and no effect on the seizure threshold. Antipsychotic medications used to treat delirium include the butyrophenones and the newer atypical antipsychotic agents.24–29 Although no one drug is ideal, the butyrophenones, specifically haloperidol (Haldol), are considered the agents of choice for control of agitation in acute delirium on the basis of extensive clinical experience.23,24 Increasing evidence indicates that compared with haloperidol, the newer atypical antipsychotic agents (risperidone, olanzapine, ziprasidone, aripiprazole) may have equal or better efficacy and fewer side effects (especially akathisia and dystonia) for management of acute agitation.25–29 In addition, the atypical antipsychotic agents received a black box warning from the U.S. Food and Drug Administration (FDA) in 2005 for use in elderly demented patients with agitation because of the increased mortality noted in this special population of patients (although this is associated with long-term use).30 Phenothiazines and droperidol, a butyrophenone pharmacologically similar to haloperidol, can cause orthostatic hypotension, lower the seizure threshold, and have anticholinergic effects, making them unacceptable for the treatment of delirium. The use of droperidol for management of agitation has been significantly curtailed since the FDA gave this drug a black box warning because of the association of droperidol use with QT prolongation and torsades de pointes; however, many clinicians think that the warning is unjustified.31,32 The opioids morphine and meperidine (Demerol) are capable of inducing dysphoria and can exacerbate respiratory depression and hepatic encephalopathy and should not be used for behavior control in the agitated delirious patient.
Benzodiazepines are the drugs of choice for management of delirium caused by withdrawal from alcohol or sedative-hypnotics, for which a long duration of action is desirable. Lorazepam, a shorter-acting benzodiazepam that undergoes glucuronide conjugation with rapid renal clearance, is the preferred agent for treatment of withdrawal symptoms. In general, they are not indicated in the management of symptoms of delirium caused by other conditions.33 Although limited data exist, the benzodiazepines may be helpful with ingestion of stimulants such as hallucinogens, cocaine, and PCP. The benzodiazepine diazepam (Valium) should be avoided as an agent for treatment of agitated behavior in most delirious patients because of its long half-life, respiratory depressant effect, and risk of drug accumulation with repeated dosing. Benzodiazepines can worsen confusion, and use of this class of drugs is an independent risk factor for delirium, especially in the elderly.34,35
As the primary drug for control of hyperactive delirium, haloperidol is a potent dopamine-blocking medication with virtually no anticholinergic and minimal hypotensive effects. The main effect of the drug acutely is tranquilization. The drug can be easily titrated with intravenous administration. The incidence of extrapyramidal side effects in patients receiving intravenous haloperidol for management of delirium with agitation is relatively low. Studies of the acute administration of haloperidol report an 8 to 30% incidence of extrapyramidal side effects, with akathisias being most common and acute dystonia occurring in less than 10% of patients.36 Haloperidol can prolong the QTc interval, but this effect is clinically insignificant in most patients and does not require a pretreatment electrocardiogram. Caution is warranted with use of this agent in patients taking medications that prolong the QTc (e.g., class IA and class III antiarrhythmics, certain antibiotics, inhibitors of the cytochrome P450 system) and in patients with acute coronary ischemia, uncompensated congestive heart failure, or hepatic dysfunction.37 Dosing should vary with the patient's level of agitation, age, weight, and response to treatment. In most patients, 5 to 10 mg intravenously or intramuscularly is well tolerated as an initial dose, and levels can be titrated as needed. Higher doses may be required for younger patients. Daily doses in excess of 200 mg for 15 consecutive days have been given safely to agitated patients in the critical care setting.35 For elders, a lower initial dose of 0.50 to 1.0 mg is recommended.38
Several well-controlled studies have shown that the combination of haloperidol and lorazepam (given by either the intramuscular or intravenous route) can achieve more rapid control of agitated behavior than is possible with haloperidol alone and can reduce the already low incidence of extrapyramidal neuromuscular symptoms.39,40
The atypical antipsychotics can be used acutely for management of agitation. These drugs have multiple mechanisms of action including antagonism of alpha2-adrenergic, serotonin, muscarinic, dopamine, and histamine receptors. These drugs block the reuptake of dopamine and serotonin, and the newer drugs also have dopamine agonist effects (aripiprazole).41–44 Compared with haloperidol, several of these atypical agents (ziprasidone, risperidone, clozapine, and olanzapine) have been shown in nonrandomized case series to control agitation as effectively with less sedation and fewer extrapyramidal side effects.41–44 Because of the limited dopamine antagonism effect, atypical antipsychotics are the preferred agent for patients with parkinsonism and agitation. Atypical antipsychotic agents for management of acute agitation have been slow to be adopted in clinical practice because of the limited studies (no randomized controlled studies in the ED setting) and the significant clinical experience with haloperidol and lorazepam.
It is not possible to obtain informed consent for proposed diagnostic and therapeutic interventions from a patient suffering from delirium. In such cases, implied consent exists when a true emergency is present or clinically suspected because common law recognizes that a reasonable person would want to receive treatment in a true emergency even if impaired awareness at the time of treatment precludes giving of informed consent. Thus it is appropriate to render treatment without informed consent to a patient who lacks decision-making capacity in a life-threatening emergency situation unless an advanced directive is available indicating the patient's desire to forgo treatment.45
Disposition
Patients with delirium secondary to acute drug intoxication may be discharged from the ED, provided the process readily reverses itself during a short period of observation and the drug has no potentially serious delayed toxicity. For most patients delirious from metabolic, infectious, or CNS processes, admission to the hospital is necessary for further diagnostic evaluation and treatment. The only readily reversible metabolic problem associated with delirium that can be completely managed in the ED is hypoglycemia.
For most patients without significant underlying medical illness who have delirium, the outcome is full recovery. After an episode of acute delirium, younger patients may experience mild cognitive dysfunction that lasts weeks to months. Geriatric patients, on the other hand, often experience persistent decline in their baseline level of functioning, with loss of at least one activity of daily living after acute delirium.46 Delirium in elders hospitalized without baseline dementia is associated with higher 1-year mortality rates, higher rates of institutionalization, and a greater risk for development of dementia.21,47 For elders, an episode of delirium, especially for those with baseline cognitive impairment, can have significant long-term consequences despite good supportive multidisciplinary care.48
Dementia
Dementia is not a single disease entity but rather a highly variable clinical syndrome characterized by a gradually progressive deterioration of cognitive function. As with delirium, potential causes are varied and numerous, and the prognosis depends on the underlying cause. A particular dementia can be classified as either potentially reversible or irreversible. Most patients with dementia have an irreversible disease process; during the past several years, the prevalence of reversible dementia has fallen to between 3 and 10%, with depression, hydrocephalus, subdural hematomas, drugs, and alcohol dependence syndrome accounting for a majority of cases.49,50 The goals of ED evaluation for suspected dementia are (1) to recognize the signs and symptoms of potentially reversible forms of dementia, (2) to identify the manifestations of acute illness in the demented patient promptly, and (3) to assess the findings for congruency with the normal progression of the irreversible dementias.
In 1907, Alzheimer described the clinical history and postmortem findings for a 50-year-old woman with progressive dementia.51 For decades, Alzheimer's disease was considered to be an uncommon dementia of younger patients known as presenile dementia. The more common dementia of elders was believed to be caused by atherosclerotic cerebrovascular disease and was referred to as senile dementia. During the past several decades, research has shown that the neuropathologic changes in the two entities are identical. Today, these two categories of primary degenerative dementias are collectively referred to as Alzheimer's disease. Alzheimer's disease accounts for 60% of all dementias; vascular dementia (with or without Alzheimer's disease) accounts for 20%, and the remaining 20% of cases are attributable to more than 50 known causes.52
Worldwide, approximately 24.3 million persons suffer from dementia, and 4.6 million new cases are diagnosed yearly.52 The prevalence is approximately 1% at the age of 60 years but doubles every 5 years until it reaches 30 to 50% by the age of 85 years. The National Institutes of Health calculates that by 2030 there will be approximately 10 million people with Alzheimer's disease in the United States.53,54
The American Psychiatric Association has defined criteria necessary for the diagnosis of dementia (Box 104-2). There must be impairment in both memory and cognitive function. Several clinical features deserve emphasis. Intellectual impairment must involve both short-term and long-term memory. The cognitive impairment commonly involves abstract thinking, judgment, and other higher cortical functions. The cognitive disturbance must significantly interfere with interpersonal relationships, work, and social activities of the affected person. Although mild decline in intellectual functioning can be part of the normal aging process, gross intellectual impairment and confusion should not be considered part of normal aging. Mild cognitive impairment is distinct from early dementia in that impairment involves mild memory deficits; some believe that mild cognitive impairment is a precursor to the development of Alzheimer's disease.55
Dementia can be classified according to the degree of cognitive impairment. Mild dementia implies some impairment of work and social activities; however, the capacity for independent adequate personal hygiene and independent living remains intact. With moderate dementia, independent living is hazardous, and some degree of supervision is necessary. With severe dementia, continual supervision and often custodial care are needed.
Demented patients often have longer hospitalizations for the same acute medical illness compared with those without dementia, and the life expectancy of demented patients is 6 to 8 years less than that of nondemented age-matched control subjects.56
Etiology
Dementia may be caused by more than 50 different disease states (Box 104-3). Dementia may be broadly classified as either primary degenerative dementia or secondary dementia; the secondary dementia category includes the potentially reversible dementias. Primary degenerative dementias include Alzheimer's disease, dementia with Lewy bodies, subcortical dementias involving the basal ganglia and thalamus (e.g., progressive supranuclear palsy, Huntington's chorea, Parkinson's disease), and dementia of the frontal lobe type, which includes Pick's disease. Dementia with Lewy bodies, clinically manifested by persistent, well-formed visual hallucinations and prominent extrapyramidal movements, has been found to be the third most common type of dementia. With advanced aging, dementia may have mixed causes, with Alzheimer's disease and vascular dementia frequently coexisting. A smaller percentage of dementias are attributable to causes such as anoxic encephalopathy, hepatolenticular degeneration, tumors, and slow virus infections.
Adverse drug reactions and metabolic abnormalities in patients can cause either an acute delirium or a gradual progressive dementia. Drug-induced dementia occurs primarily in elders and can be caused by various psychotropic drugs, antihypertensive medications, anticonvulsants, anticholinergics, and miscellaneous medications such as L-dopa. Dementia also may be caused by heavy metals and other exogenous agents, such as carbon monoxide, carbon disulfide, and trichloroethylene.
Endocrinopathies that can cause secondary dementia include hypothyroidism, hyperthyroidism, parathyroid disease, Addison's disease, Cushing's disease, and panhypopituitarism. Nutritional deficiencies that cause dementia include thiamine deficiency (Wernicke's syndrome), niacin deficiency (pellagra), vitamin B12 deficiency, and folate deficiency. Dementia can be caused by intracranial space-occupying lesions and hydrocephalus. Repetitive intracranial trauma resulting from contact sports can produce a chronic organic brain syndrome without evidence of hematoma or significant contusion (dementia pugilistica).57,58 Intracranial processes that may eventually lead to a chronic organic brain syndrome include infections with slow viruses, HIV-1 infection, chronic meningitis (tubercular or fungal), brain abscess, and neurosyphilis. In addition to primary HIV-1 CNS infection, toxoplasmosis, cryptococcal meningitis, malignant disease, and infections due to herpesvirus, cytomegalovirus, varicella-zoster virus, and papovavirus (progressive multifocal leukoencephalopathy) can cause progressive cognitive impairment in this compromised group of patients and must be excluded.59
Depression in elders may closely mimic dementia. Diagnosis of pseudodementia or depression masquerading as dementia can be difficult and may require therapeutic interventions to confirm the clinical diagnosis of depression. Confounding the issue, depression often coexists with dementia; one study found that 40% of patients with dementia were depressed.60 Depression, anxiety, and apathy are common in the prodrome and course of Alzheimer's disease.60,61
Pathophysiology
Alzheimer's disease is the best-understood dementia and involves several characteristic anatomic, pathologic, and neurochemical changes. The predominant change is cortical atrophy most prominent in the temporal and hippocampal regions caused by progressive synaptic and neuronal loss in the cerebral gray matter. This atrophy generally is followed by loss of white matter (subcortical atrophy). Cell loss does occur with the normal aging process but not to the extent seen in dementia. Not all patients with dementia have gross cerebral atrophy. There is no ischemic component to Alzheimer's disease.
Histologic features characteristic of Alzheimer's disease include extracellular deposition of β-amyloid protein and intracellular neurofibrillary tangles contributing to neuron loss. The abnormal processing of β-amyloid protein probably is central to the pathogenesis of Alzheimer's disease. The neurofibrillary tangles are intraneuronal paired helical filaments composed of the abnormally phosphorylated protein tau, the structural protein involved in the regeneration of neurites. In demented patients, these tangles occur in great numbers throughout the cerebral cortex; only limited numbers can be seen in nondemented elders (primarily in the hippocampus region) and in a variety of other diseases. The density of neocortical tangles correlates with the severity of dementia.56 Mounting evidence suggests that Aβ protein accumulation triggers activation of cysteine aspartyl proteases (caspases) with cleaving of the tau protein, leading to neurofibrillary tangles and apoptosis. Senile plaques are extracellular lesions composed of degenerating neuronal processes and abnormal β-amyloid protein. These plaques are extensively spread throughout the cerebral cortex and do not correlate with the severity of dementia.62 Other consistent neurohistopathologic changes in Alzheimer's disease include granulovascular degeneration, Hirano bodies, β-amyloid deposition in the small cortical blood vessels, and neuronal loss in the limbic area.63
Many biochemical abnormalities have been described in patients with Alzheimer's disease. A decrease in the neurotransmitter acetylcholine is characteristic. Levels of the enzyme choline acetyltransferase, which synthesizes acetylcholine in the brain, can be reduced to 20% of that in age-matched control subjects.64
Several risk factors for Alzheimer's disease are recognized, including advancing age, family history, low education level, hypercholesterolemia, and head trauma. The apolipoprotein E epsilon 4 allele on chromosome 19 has been associated with both familial and sporadic late-onset Alzheimer's disease. Apolipoprotein E is responsible for transporting of the cholesterol and phospholipids necessary for dendritic and synaptic repair. There are several allelic variants, but those homozygous or heterozygous for the E4 variant have an increased risk for the development and expression of the disease.64 Abnormalities on chromosomes 1 and 14 also have been associated with Alzheimer's disease.
The frontotemporal dementias are less prevalent than Alzheimer's disease and are categorized by a frontal and temporal atrophy caused by cell death.65 The most common histologic finding in the frontotemporal dementias is the combination of prominent cell loss and gliosis in frontal and temporal regions of the cortex, termed dementia lacking distinctive histology.66
Approximately 15 to 20% of dementias are caused by multiple vascular insults to the CNS; the resulting deficit is termed multi-infarct dementia. The multiple infarcts typically involve the cerebral hemispheres and basal ganglia. Multi-infarct dementia often has an earlier age at onset than Alzheimer's disease and occurs more often in adult men and patients who have risk factors for atherosclerosis. Approximately 29% of dementias are a mixed variety, with components of both ischemic cerebrovascular disease and Alzheimer's dementia.64,67
Inflammatory conditions of the CNS caused by conventional viruses include subacute sclerosing panencephalitis from measles virus infection, progressive multifocal leukoencephalopathy from infection by the JC virus (a papovavirus), progressive rubella encephalitis, and infection associated with HIV disease. The unconventional viral infections include kuru, Creutzfeldt-Jakob disease (CJD), and variant CJD (which appears to be linked to bovine spongiform encephalopathy, the pathologic process in “mad cow disease”) and are associated with minimal inflammatory histopathologic changes in the CNS; these diseases cause a fine vacuolation of the nervous tissue and hence are referred to as subacute spongiform viral encephalopathies.68
Slow virus infections of the CNS can cause a progressive dementia that is irreversible. With these infections, months to years pass between infection with the virus and the appearance of clinical illness. Slow virus infections of the CNS are caused by both conventional viruses and unconventional viruslike agents known as prions. A prion is a proteinaceous infectious particle with the apparent ability to start a chain reaction that changes the shape of benign protein molecules into abnormal, slowly destructive forms. Prions are present in CJD and variant CJD.68
One of the most prevalent slow virus infections causing progressive dementia is HIV-1 infection. HIV may produce a primary neurotrophic disorder in addition to causing the immunologic compromise that permits other viruses to replicate and damage nervous tissue.
HIV dementia or AIDS dementia complex occurs in approximately one fourth of patients with AIDS. It is believed to be caused by the HIV-1 virus targeting the microglial cells and the macrophages, which may produce cytotoxic substances such as tumor necrosis factor and interleukins. Pathologic changes occur mostly in the hippocampus and basal ganglia and include atrophy, ventricular dilation, and fibrosis.69,70
Several of the potentially reversible causes of dementia also are associated with neuropathologic or neurochemical abnormalities. Normal-pressure hydrocephalus generally affects younger people; 50% of patients are younger than 60 years. Most of the conditions that cause hydrocephalus involve a defect in uptake of CSF by arachnoid villi, which results in gradual ventricular dilation.
Chronic, heavy ethanol consumption is associated with dementia. The neurotoxicity of ethanol appears to be independent of thiamine deficiency. Heavy chronic alcohol consumption causes cerebral cortical atrophy, but no single alcohol-related dementia syndrome exists. It is estimated that approximately 20% of chronically demented patients have a history of alcoholism.
Clinical Features
The symptoms, signs, and progression of chronic cognitive impairment rarely are so diagnostic as to permit identification of the specific cause of the dementia. Alzheimer's disease begins insidiously. Signs and symptoms of cognitive dysfunction may be present for months to years before the diagnosis is made. The earliest symptoms and signs of Alzheimer's disease often are vague and nonspecific; patients manifest anxiety, depression, insomnia, frustration, and somatic complaints that often are more prominent than the memory loss. Patients often deny any cognitive deficits and change the subject of the conversation frequently rather than admit their increasing forgetfulness. Physicians often overlook the subtle signs of dementia in this phase of the disease.71
Depression often is the initial manifestation of Alzheimer's disease and is present in up to 40% of cases. Early in the illness, short-term memory is affected, with forgetfulness of recent events such as appointments and names of new acquaintances. Patients often repeat questions. The memory impairment may cause them to withdraw from social situations and recreational pursuits. Attempts to perform complex tasks may produce anxiety and confusion. The patient often has difficulty with interpersonal relationships. Affect may be shallow and labile, and minor events may trigger inappropriate laughter or tears. Compensation for early deficits includes excessive orderliness and avoidance of situations in which the defects may be observed. Patients in this early phase who are treated with antidepressants with anticholinergic properties may experience worsening of their symptoms. Sedative-hypnotics prescribed for anxiety also may accelerate cognitive dysfunction.
As the dementia progresses, cognitive deficits are more obvious and should be readily apparent on a mental status examination. Problems with recent memory, impairment of remote memory, language deficits, and difficulty with spontaneous speech may be noted. With moderate severity of the disease, patients have difficulty naming objects (dysnomia). As many as 50% of patients have delusions, usually of the paranoid type. Atypical presentations of Alzheimer's disease include aphasia, visual agnosia, right parietal lobe syndrome, focal neurologic findings, extrapyramidal signs, gait disturbances, and pure memory loss. In the final stage of dementia, patients exhibit marked cognitive impairment, apraxia, and significant personality changes. They often are bedridden and unable to perform any of the routine activities of daily living.
Because Pick's disease dementia affects the frontal and temporal lobes, patients often have frontal lobe release signs, including dramatic behavioral changes of disinhibition and social inappropriateness. Basal ganglia degenerative disorders that have dementia as a prominent feature are Huntington's chorea, Parkinson's disease, and Wilson's disease. One of several features that distinguish cortical from subcortical dementias is a prominent movement disorder, including posturing, ataxia, tremor, and chorea, that tends to occur early in the illness. Other features of these dementias include slowness of speech, hypotonia, and dysarthria, which can progress to mutism.72
Patients with vascular dementia have a stepwise deterioration in memory and cognitive function with each cerebrovascular insult. The clinical presentation may follow one of two scenarios. In the more common scenario, the patient suffers several strokes that involve large volumes of cortical and subcortical structures in both hemispheres. The patient then exhibits dementia along with other neurologic disabilities (e.g., focal weakness, hyperreflexia, extensor plantar response). In a second group of patients, the presentation is more subtle. These patients characteristically are hypertensive and suffer multiple tiny infarcts (lacunae) that involve deep subcortical structures. There may be no focal neurologic residua except progressive dementia with psychomotor retardation. Aggressive antihypertensive therapy in the very elderly does not reduce the incidence of dementia.73
The clinical manifestations of slow virus CNS infections are protean. After an insidious onset of mental deterioration in subacute sclerosing panencephalitis, a rapid progression ensues that is associated with myoclonic jerks, incoordination, and ataxia. In progressive multifocal leukoencephalopathy, neurologic signs and symptoms reflect diffuse asymmetrical involvement of both cerebral hemispheres. Sporadic CJD, of unknown etiology, tends to affect older people, with a rate of disease among those 50 to 70 years of age of 1 case per million. Among these patients, rapidly evolving dementia with myoclonus is characteristic. The hallmarks of the disorder are mental deterioration, multisystem neurologic signs, myoclonus, and typical electroencephalographic changes that evolve during months. Variant CJD affects younger patients (median age of 24 years), with key features that include early affective symptoms progressing to cognitive impairment and gait disturbances and ultimately leading to progressive neurologic deterioration. The incubation period appears to be in the range of 10 to 15 years, and most patients die within 14 months after the clinical onset of symptoms.68
The most common treatable dementia is pseudodementia, or depression. The clinical distinction between depression and dementia is difficult, and the coexistence of depression and dementia is common in people with mild dementia. A number of distinguishing features suggest that the problem is depression rather than dementia: the onset of cognitive changes in pseudodementia often can be pinpointed, and symptoms usually are of short duration before medical help is sought. The progression of symptoms is rapid, and the family usually is aware of the severity of the dysfunction. A history of psychiatric illness is common. Patients with pseudodementia usually complain of cognitive dysfunction and emphasize their failures and disabilities. The affective change often is pervasive, and the patient makes little effort to perform simple tasks. Loss of social skills usually occurs early in the illness, and patients communicate a strong sense of distress and inability to function. Intellectual functioning in pseudodementia often is difficult to assess because of lack of patient cooperation or inconsistent findings on neuropsychometric testing. Attention and concentration often are intact, but patients commonly give answers such as “I don't know” on tests of orientation, concentration, and memory. Memory losses for recent and remote events usually are equally severe, and variability in the performance of tasks with similar degrees of difficulty may be marked. Tasks of high capacity (e.g., testing of delayed memory with distraction) may be helpful in identifying the depressed patient.74
The classic triad of progressive dementia, ataxia, and urinary incontinence occurs in patients with normal-pressure hydrocephalus, which typically affects patients who are younger than those with primary degenerative dementia. More than half of the reported cases are in persons younger than 60 years. Hydrocephalus secondary to previous head trauma or infection carries a more favorable prognosis than that for primary hydrocephalus.
In approximately 20% of the reversible cases, dementia is secondary to an intracranial mass. Patients may exhibit focal or nonfocal neurologic signs.75 Of the reversible dementias, 10 to 15% are secondary to medications or chemical intoxications, frequently compounding a history of heavy alcohol use. Geriatric patients have increased susceptibility to the toxicities owing to polypharmacy and age-related changes in metabolism. The clinical presentation of a patient with a drug-related or toxin-related dementia may be indistinguishable from that of a patient with a primary degenerative process.
Family or friends usually bring the patient to the ED because of a sudden worsening in mental status, a change in the patient's activities (e.g., refusal to eat), or a change in the ability of the caregiver to manage the patient. Presentations vary by the cause of the dementia and the stage of progression. Many elders with dementia have a superimposed delirium on presentation.
Differential Considerations
Subacute or chronic cognitive decline may be secondary to a dementing illness or can be a manifestation of senescent forgetfulness, delirium, or depression. Senescent forgetfulness is an almost inevitable reality of aging. Mild impairment of both short-term and long-term memory is usual. Unlike in dementia, the cognitive disturbance in senescent forgetfulness does not interfere with work or customary social activity. The distinction between senescent forgetfulness and mild cognitive impairment is not well defined.
In most cases, the clinical distinction between delirium and dementia is obvious. As stated previously, the onset of symptoms, progression of signs and symptoms, perceptual disturbances, possible presence of abnormalities on assessment of vital signs, and fluctuations in the level of consciousness are key distinguishing features.
Diagnostic Strategies
The evaluation of the patient with possible dementia should include a focused medical and psychiatric history and medication history plus a collateral history from family and friends. Physical examination should include a detailed neurologic examination with mental status evaluation. Dementia often goes unrecognized in the patient who is alert, pleasant, and cooperative. A validated cognitive evaluation test can play a key role in the early identification of dementia in patients who have maintained social and conversational ability.
Alzheimer's disease is a clinical diagnosis typically made on probability; no routine available laboratory tests have been found to confirm the presence of the disorder (although MRI scan, functional scans looking at regional blood flow or glucose metabolism, assay for specific biomarkers, and CSF analysis can significantly increase the probability of the presence of the disease). The physical examination is rarely helpful in detecting treatable dementias because of the considerable clinical overlap with irreversible dementias. Data clearly supporting or refuting the ordering of “routine” laboratory studies for evaluation of dementia are lacking; however, a number of studies are recommended to exclude treatable causes (Box 104-4). For patients with suspected undiagnosed dementia presenting to the ED, a baseline laboratory evaluation, including CBC, comprehensive metabolic panel, and urinalysis, is indicated. If neurosyphilis is clinically suspected, a serum fluorescent treponemal antibody absorption test should be performed in addition to a Venereal Disease Research Laboratory (VDRL) test because the serum VDRL assay may yield negative results in patients with tertiary syphilis. The radiologic evaluation should include a non–contrast-enhanced head CT scan. The CT scan is used to diagnose or to exclude the presence of hydrocephalus or space-occupying lesions, and CT findings may support a vascular etiology for the dementia.
Patients require additional laboratory tests on follow-up evaluation; such tests may include determination of serum vitamin B12 and folate levels, thyroid function studies, estimation of erythrocyte sedimentation rate, fluorescent antinuclear antibody assay, measurement of urine corticosteroid levels, and, if indicated by history, urine screens for drugs and heavy metals. Selected patients should undergo a lumbar puncture with CSF analysis, MRI, positron emission tomography scan, electroencephalography (in CJD, characteristic slowing and periodic complexes may be electroencephalographic features), neuropsychological testing, and testing of visual evoked potentials, brainstem auditory evoked potentials, and somatosensory evoked potentials. The EEG rarely is helpful in establishing the diagnosis of senile dementia. An MRI finding of medial temporal atrophy suggests Alzheimer's disease but is not specific or sensitive for diagnosis of this disorder.76
Treatment and Disposition
Reversible dementias and conditions that cause worsening of baseline dementia require early diagnosis and treatment of the underlying disorder if previous cognitive function is to be restored. Determination of reversible causes of dementia during the ED evaluation occasionally is possible on the basis of the history (including medication history), physical examination, and head CT scan. Patients with acute changes in mental status or a relatively rapid onset of symptoms will require hospitalization for comprehensive evaluation. Patients presenting with recent gradual decline in cognitive function without an underlying acute medical condition can undergo further evaluation on an outpatient basis.
Pharmacotherapy approved by the FDA for the treatment of mild to moderate Alzheimer's disease includes the cholinesterase inhibitors donepezil (Aricept), rivastigmine (Exelon), and galantamine (Razadyne). There are multiple randomized, placebo-controlled, large-scale clinical trials with these drugs establishing efficacy in improving cognitive functions, overall evaluation, and activities of daily living in patients with mild to moderate dementia. These drugs are not considered disease modifying, and there are limited data at present on the benefit of these drugs beyond 2 or 3 years (a significant number of patients discontinue medications because of side effects). The most common side effect of these agents is due to the cholinergic effects, including nausea, vomiting, and diarrhea. In 2003, the FDA approved memantine (Namenda), a disease-modifying agent that helps regulate the excitatory effects of glutamate by antagonizing the N-methyl-D-aspartate receptor. Whether this drug alters the underlying disease process is unclear, but short-term studies show improved cognition in patients with moderate and moderate to severe Alzheimer's disease with memantine.77,78 There are conflicting studies on the effectiveness of other agents, such as gingko biloba, vitamin E, nonsteroidal agents, and statins. Estrogen replacement is not indicated for cognitive improvement or maintenance in women with Alzheimer's disease and can be detrimental. Ultimately, the key to altering the course of the disease is halting neuron loss. In severe dementia, the goal of management is supportive care.
Many therapies currently are under investigation for the modulation and early treatment of Alzheimer's disease. These therapies include antibiotics (directed against Chlamydophila pneumoniae), secretase modulators to reduce serum β-amyloid levels, immunization to reduce amyloid plaque burden, chelators to promote dissolution of β-amyloid, nonsteroidal anti-inflammatory medications, supplementation with omega-3 fatty acids, and testosterone.79,80
Increasing evidence suggests that certain nonpharmacologic measures, including behavioral methods and avoidance of environmental triggers, may be effective in reducing agitation and anxiety in patients with dementia.81 On occasion, medications are needed for behavioral symptoms of dementia. Affected patients typically do not improve with anxiolytics. Adverse effects offset the modest advantages in the efficacy of antipsychotic drugs for the treatment of psychosis, aggression, or agitation in many patients with Alzheimer's disease, and these drugs should be avoided when possible.82,83 However, agitation can be controlled with a small dose of the butyrophenone haloperidol.84 The cardiovascular toxicity of this drug is minimal, and it is reasonably well tolerated in elders. Clozapine also has been shown to be effective in treating psychosis associated with both Alzheimer- and Parkinson-type dementias.85 In April 2005, the FDA issued a black box warning that the use of atypical antipsychotics to treat elderly patients with dementia was associated with an increased risk for death compared with placebo. Atypical antipsychotics are relatively contraindicated in this group of patients because of the association with an increased risk of hospitalization and death.86,87 Agitation may occasionally be due to unrecognized depression in dementia, and a trial of selective serotonin reuptake inhibitors may be warranted.88 Temazepam (Restoril) is the drug of choice for sleep disturbance. The half-life of temazepam is 8 to 10 hours for patients of all ages, and the drug bypasses the oxidative hepatic enzyme system.
On occasion, patients are brought to the ED because of a crisis due to family stress from continuous care of the person with dementia. A brief nursing home stay or other institutional stay (respite program) may give the family time to mobilize resources to resume the home care regimen. Social workers can play a vital role in attempting to facilitate management of these patients.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 2000.
2. Inouye, SK, Ferrucci, L. Elucidating the pathophysiology of delirium and the interrelationship of delirium and dementia. J Gerontol A Biol Sci Med Sci. 2006;61:1277–1280.
3. Fick, DM, Agostini, JV, Inouye, SK. Delirium superimposed on dementia: A systemic review. J Am Geriatr Soc. 2002;50:1723–1732.
4. Meagher, DJ, Trzepacz, PT. Motoric subtypes of delirium. Semin Clin Neuropsychiatry. 2000;5:75–85.
5. Hustey, FM, Meldon, SW. The prevalence and documentation of impaired mental status in elderly emergency department patients. Ann Emerg Med. 2002;39:248.
6. Elie, MJ. Delirium risk factors in elderly hospitalized patients. J Gen Intern Med. 1998;13:204.
7. Flacker, JM, et al. The association of serum anticholinergic activity with delirium in elderly medical patients. Am J Geriatr Psychiatry. 1998;6:31–41.
8. Rivera, W, et al. Central nervous system toxicity manifestations of drug toxicity. Emerg Med Rep. 2003;24:12.
9. Inouye, SK. Delirium in older persons. N Engl J Med. 2006;354:1157.
10. Talbot-Stern, JK, et al. Psychiatric manifestations of systemic illness. Emerg Med Clin North Am. 2000;18:199.
11. Hohl, CM, et al. Polypharmacy, adverse drug-related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med. 2001;38:661.
12. Folstein, MF, Folstein, SE, McHugh, PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189.
13. Cullen, B, O'Neill, B, Evans, JJ, Coen, RF, Lawlor, BA. A review of screening tests for cognitive impairment. J Neurol Neurosurg Psychiatry. 2007;78:790–799.
14. American Psychiatric Association Practice Guidelines. Practice guidelines for the treatment of patients with delirium. Am J Psychiatry. 1999;156(Suppl):5.
15. Wilber, ST, et al. An evaluation of two screening tools for cognitive impairment in older emergency department patients. Acad Emerg Med. 2005;12:612.
16. Petersen, RC. Practice parameter: Early detection of dementia: Mild cognitive impairment (an evidenced-based review). Neurology. 2001;56:1133.
17. Duff Canning, SJ, et al. Diagnostic utility of abbreviated fluency measures in Alzheimer disease and vascular dementia. Neurology. 2004;62:556.
18. Huff, JS, et al. The quick confusion scale in the ED: Comparison with the Mini-Mental State Examination. Am J Emerg Med. 2001;19:461.
19. Inouye, SK, et al. Clarifying confusion: The confusion assessment method: A new method for detection of delirium. Ann Intern Med. 1990;113:941.
20. Zou, Y, et al. Detection and diagnosis of delirium in the elderly: Psychiatrist diagnosis, confusion assessment method or consensus diagnosis? Int Psychogeriatr. 1998;10:303.
21. Witlox, J, et al. Delirium in elderly patients and the risk of post-discharge mortality, institutionalization, and dementia: A meta analysis. JAMA. 2010;304:443–451.
22. Schmidt, P, et al. The effects of positional restraint on heart rate and oxygen saturation. J Emerg Med. 1999;17:777.
23. Stratton, SJ, et al. Factors associated with sudden death of individuals requiring restraint for excited delirium. Am J Emerg Med. 2001;19:187.
24. Lonergan, E, Britton, AM, Luxenberg, J, Wyller, T. Antipsychotics for delirium. Cochrane Database Syst Rev. (2):2007.
25. Seeman, P. Atypical antipsychotics: Mechanism of action. Can J Psychiatry. 2002;47:27.
26. Daniel, DG, et al. Intramuscular (IM) ziprasidone 20 mg is effective in reducing acute agitation associated with psychosis: A double-blind, randomized trial. Psychopharmacology (Berl). 2001;155:128.
27. Brook, S, et al. Intramuscular (IM) ziprasidone compared with intramuscular haloperidol in the treatment of acute psychosis. J Clin Psychiatry. 2000;61:933.
28. Battaglia, J, et al. Calming versus sedative effects of intramuscular olanzapine in agitated patients. Am J Emerg Med. 2003;21:192.
29. Wright, P, et al. Double blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation. Am J Psychiatry. 2001;158:1149.
30. Kales, HC, et al. Trends in antipsychotic use in dementia 1999-2007. Arch Gen Psychiatry. 2011;68:190–197.
31. Bailey, P, Norton, R, Karan, S. The FDA droperidol warning: Is it justified? Anesthesiology. 2002;97:288.
32. Thomas, H, Schwartz, E, Petrilli, R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21:407.
33. Lonergan, E, Luxenberg, J, Areosa, SA, Wyller, TB. Benzodiazepines for delirium. Cochrane Database Syst Rev. (1):2009.
34. Pandharipande, P, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104:21.
35. Jacobi, J, et al. Clinical practice guidelines for the use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119.
36. Schillevoort, I. Risk of extrapyramidal syndromes with haloperidol, risperidone, and olanzapine. Ann Pharmacother. 2001;35:1517.
37. Sharma, ND, et al. Torsades de pointes associated with intravenous haloperidol in critically ill patients. Am J Cardiol. 1998;81:238.
38. Bergmann, MA, Murphy, KM, Kiely, DK, Jones, RN, Marcantonio, ER. A model for management of delirious postacute care patients. J Am Geriatr Soc. 2005;53:1817.
39. Battaglia, J, et al. Haloperidol, lorazepam, or both for psychotic agitation: A multicenter, prospective, double-blind emergency department study. Am J Emerg Med. 1997;15:335.
40. Cook, IA. Guideline Watch: Practice Guideline for the Treatment of Patients with Delirium. Washington, DC: American Psychiatric Association; 2004.
41. Skrobik, YK, et al. Olanzapine vs haloperidol: Treating delirium in a critical care setting. Intensive Care Med. 2004;30:444.
42. Sipahimalani, A, Massand, PS. Use of risperidone in delirium: Case reports. Ann Clin Psychiatry. 1997;9:105.
43. Ravona-Springer, R, et al. Delirium in elderly patients treated with risperidone: A report of three cases. J Clin Psychopharmacol. 1998;18:171.
44. Sipahimalani, A, Masand, PS. Olanzapine in the treatment of delirium. Psychosomatics. 1998;39:422.
45. Naess, AC. Patient autonomy in emergency medicine. Med Health Care Philos. 2001;4:71.
46. Inouye, SK, et al. Risk factors for delirium at discharge: Development and validation of a predictive model. Arch Intern Med. 2007;167:1406.
47. McCusker, J, et al. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162:457.
48. Cole, MG, et al. Systematic detection and multidisciplinary care of delirium in older medical inpatients: A randomized trial. CMAJ. 2002;167:753.
49. Knopman, DS, et al. Incidence and causes of nondegenerative nonvascular dementia: A population-based study. Arch Neurol. 2006;63:218.
50. Hejl, A, Hogh, P, Waldemar, G. Potentially reversible conditions in 1000 consecutive memory clinic patients. J Neurol Neurosurg Psychiatry. 2002;73:390.
51. Alzheimer, A. Uber eine eigenartige Erkrankung der Hirnrinde. Allerg Z Psychiatr. 1907;64:146.
52. Ferri, CP, et al. Global prevalence of dementia: A Delphi consensus study. Lancet. 2005;366:2112.
53. National Institutes of Health, National Institute on Aging. Progress Report on Alzheimer's Disease 1999. Bethesda, Md: U.S. Department of Health and Human Services; 1999.
54. Kukull, WA. Dementia epidemiology. Med Clin North Am. 2002;86:573.
55. Morris, JC, et al. Mild cognitive impairment represents early-stage Alzheimer disease. Arch Neurol. 2001;58:397–405.
56. Tschanz, JT, et al. Dementia: The leading predictor of death in a defined elderly population: The Cache County Study. Neurology. 2004;62:1156.
57. Roberts, GW, Allsop, D, Bruton, C. The occult aftermath of boxing. J Neurol Neurosurg Psychiatry. 1990;53:373.
58. Mckee, AC, et al. Chronic traumatic encephalopathy in athletes: Progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68:709–735.
59. Belman, AL. HIV-1 infection and AIDS. Neurol Clin. 2002;20:983.
60. Winblad, B. Major depression in a population of demented and nondemented older people: Prevalence and correlates. J Am Geriatr Soc. 2002;46:27.
61. Feldman, H, et al. Behavioral symptoms in mild cognitive impairment. Neurology. 2004;62:1199–1201.
62. Tanzi, RE. Tangles and neurodegenerative disease—a surprising twist. N Engl J Med. 2005;353:1835.
63. Gandy, S. The role of cerebral amyloid beta accumulation in common forms of Alzheimer disease. J Clin Invest. 2005;115:1121.
64. Cummings, JL. Alzheimer's disease. N Engl J Med. 2004;351:56.
65. Knopman, DS. An overview of common non-Alzheimer dementias. Clin Geriatr Med. 2001;17:281.
66. Giannakopoulos, P, Hof, PR, Bouras, C. Dementia lacking distinctive histopathology: Clinicopathological evaluation of 32 cases. Acta Neuropathol (Berl). 1995;89:346.
67. Chui, HC, et al. Clinical criteria for the diagnosis of vascular dementia: A multicenter study of comparability and interrater reliability. Arch Neurol. 2000;57:191.
68. Tyler, KL. Creutzfeldt-Jakob disease. N Engl J Med. 2003;384:681.
69. Bensalem, MK, Berger, JR. HIV and the central nervous system. Compr Ther. 2002;28:23.
70. Sotrel, A, Dal Canto, MC. HIV-1 and its causal relationship to immunosuppression and nervous system disease in AIDS: A review. Hum Pathol. 2000;31:1274.
71. Finkel, SI. Behavioral and psychological symptoms of dementia. Clin Geriatr Med. 2003;19:799.
72. Graham, NL, Bak, T, Patterson, K, Hodges, JR. Language function and dysfunction in corticobasal degeneration. Neurology. 2003;61:493.
73. Peters, R, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): A double-blind placebo controlled trial. Lancet Neurol. 2008;7:683–689.
74. Peters, KR, et al. Characterizing neuropsychiatric symptoms in subjects referred to dementia clinics. Neurology. 2006;66:523.
75. Clarfield, AM. The decreasing prevalence of reversible dementia: An updated meta-analysis. Arch Intern Med. 2003;163:2219.
76. Barnes, J, et al. Measurement of the amygdala and hippocampus in pathologically confirmed Alzheimer disease and frontal lobe degeneration. Arch Neurol. 2006;63:1434.
77. Reisberg, B, et al. A 24-week open-label extension study of memantine in moderate to severe Alzheimer disease. Arch Neurol. 2006;63:49.
78. McShane, R, Areosa Sastre, A, Minakaran, N. Memantine for dementia. Cochrane Database Syst Rev. (2):2006.
79. Sano, M, et al. A controlled trial of selegiline, alpha-tocopherol, or both as treatment for Alzheimer's disease. The Alzheimer's Disease Cooperative Study. N Engl J Med. 1997;336:1216.
80. Siemers, ER, et al. Effects of a gamma-secretase inhibitor in a randomized study of patients with Alzheimer's disease. Neurology. 2006;66:602.
81. Ayalon, L, et al. Effectiveness of nonpharmacological interventions for the management of neuropsychiatric symptoms in patients with dementia: A systemic review. Arch Intern Med. 2006;166:2182.
82. Rochon, PA, et al. Antipsychotic therapy and short-term serious events in older adults with dementia. Arch Intern Med. 2008;168:1090.
83. Kuehn, BM. FDA warns antipsychotic drugs may be risky for elderly. JAMA. 2005;293:2462.
84. Tariot, PN, et al. Pharmacologic therapy for behavioral symptoms of Alzheimer's disease. Clin Geriatr Med. 2001;17:359.
85. Low-dose clozapine for the treatment of drug-induced psychosis in Parkinson's disease. The Parkinson Study Group. N Engl J Med. 1999;340:757.
86. Schneider, LS, et al. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer's disease. N Engl J Med. 2006;355:1525.
87. Schneider, LS, et al. Risk of death with atypical antipsychotic drug treatment for dementia: Meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294:1934.
88. Fickle, SI, et al. A randomized placebo-controlled study of the efficacy and safety of sertraline in the treatment of the behavioral manifestations of Alzheimer's disease in outpatients treated with donepezil. Int J Geriatr Psychiatry. 2004;19:9.
