CHAPTER 19
Traumatic Dental Injuries: Follow‐Up and Long‐Term Prognosis
Eva Fejerskov Lauridsen, Simon Storgård Jensen, and Jens O. Andreasen
Long‐term prognosis after traumatic dental injury mainly depends on the type and extent of injury, correct initial treatment, and systematic clinical and radiographic follow‐up that allows early identification and appropriate handling of potential healing complications.
A traumatic dental injury represents acute transmission of energy to the tooth and supporting structures, which can result in fracture and/or displacement of the tooth, separation or crushing of the supporting tissues [gingiva, periodontal ligament (PDL), and bone] and damage to the neurovascular supply to the pulp. A variety of healing complications may occur after traumatic dental injury. The type and severity of complications depend upon the tissues involved.
Wound healing events
Wound healing events comprise revascularization of ischemic tissue or formation of new tissue in the case of tissue loss (Figure 19.1). In both instances, wound healing takes place by a coordinated migration of cells into the traumatized area, where macrophages form the healing front, followed by endothelial cells and fibroblasts. Vascular loops are formed in a stroma of tissue dominated by immature collagen (Type III) and proliferating fibroblasts. These cells are synchronized via chemical signals released by the involved cells and the surrounding tissue. This phenomenon has been termed the wound healing module [1].

Figure 19.1 Later wound healing events; macrophages (m) form the healing front, followed by endothelial cells (e) and fibroblasts (f).
Source: Andreasen 1995 [9]. Reproduced with permission of F. Andreasen.
In the following, wound healing responses will be described as they appear in the case of simple luxation injuries, with only a separation injury of the PDL and the pulp, and subsequently with more complicated luxation trauma accompanied by crushing injuries [2] (Figures 19.2 and 19.3).
- Separation injuries (Figure 19.2). In the case of separation injury (e.g., extrusive luxation), the major part of the injury consists of cleavage of intercellular structures (collagen and intercellular substance), while there is limited damage to the cells in the traumatized area. This implies that wound healing can occur from existing cellular systems with a minimum of delay [2]. After 1 week, new collagen formation starts to unite the severed PDL fibers which results in initial consolidation of a luxated or a replanted tooth. After 2 weeks, repair of the principal fibers is advanced to a degree where approximately two‐thirds of the mechanical strength of the PDL is regained. In luxated teeth with a severed vascular supply, ingrowth of new vessels into the pulp starts 4 days after injury and proceeds at a speed of approximately 0.5 mm per day in teeth with open apices. Revascularization is usually markedly influenced by the size of the pulpo‐periodontal interface, being almost complete and predictable in teeth with open apices (≥1.0 mm). The chance of revascularization is decreasing with the diameter of the apical foramen and becomes rare with an apical foramen of <0.5 mm [2].
- Crushing injury (Figure 19.3). In complicated luxation injuries with crushing (e.g., intrusion) or other damage of the PDL (e.g., dissection after avulsion), there is extensive damage to both cellular and intercellular systems; and damaged tissue must be removed by macrophages and/or osteoclasts before the traumatized tissue can be restored. Such damage adds several weeks to the healing process. If the protecting cementoblast layer and the epithelial rests of Malassez along the root surface have been destroyed due to the trauma, there is free access for osteoclasts and macrophages to remove damaged PDL and cementum on the root surface leading to root resorption [2].
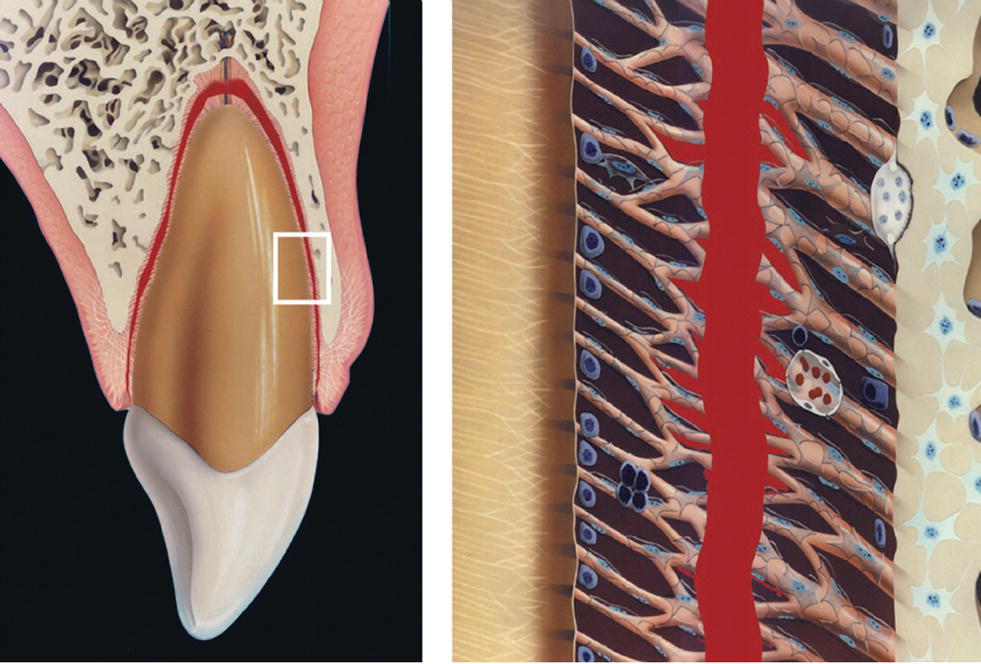
Figure 19.2 Nature of trauma in the case of separation injury.
Source: Andreasen 1995 [9]. Reproduced with permission of F. Andeasen.
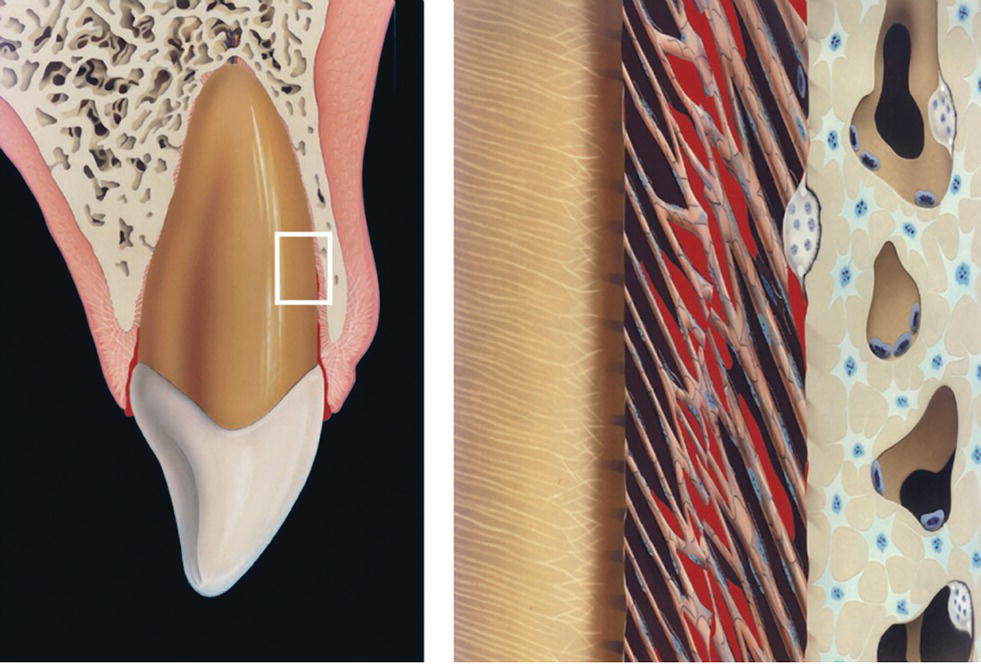
Figure 19.3 Nature of trauma in the case of crushing injury.
Source: Andreasen 1995 [9]. Reproduced with permission of F. Andreasen.
To ascertain the progress of healing and/or the initiation of complications, detailed clinical and radiographic examination must be carried out at specific intervals where complications have become diagnosable.
Primary teeth: follow‐up and prognosis
If it is decided to preserve a traumatized primary tooth, it should be carefully observed for clinical and radiographic signs of pulpal or periodontal complications. Radiographs must also be examined closely to disclose any damage to the permanent successor (Figure 19.4). The patient should always be evaluated one week after the injury to assure initial healing has taken place. Thereafter the intervals between re‐examinations will depend on the type of injury, the expected type of complication and the age of the child. Hence, if there is a low risk of healing complications (e.g., concussion, subluxation or enamel–dentin fracture) and good parental support, then it may be sufficient to evaluate the traumatized teeth once a year. However, parents must then be carefully instructed to contact the dentist if there is any sign of infection such as discoloration of the crown, swelling or pain. In severe cases where there is a high risk of complications (e.g., intrusions or lateral luxation) it is recommended to see the child after 1 week, 4 weeks, 3 months, 6 months, and 1 year, and then annually until the primary tooth is shed and the permanent successor is in place.
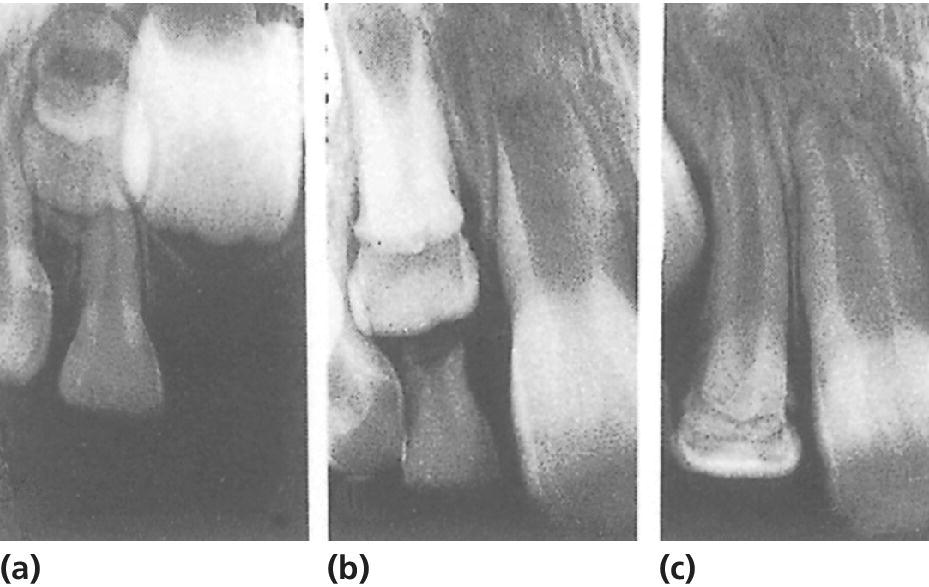
Figure 19.4 Severe malformation of permanent lateral incisor following intrusive luxation of predecessor at the age of 2 years. (a) Condition 1 year after trauma. (b,c) Further development of deformed incisor and uncomplicated eruption, respectively.
Pulpal and periodontal complications
Pulp necrosis
Pulp necrosis is the most common complication [3]. In evaluating pulpal status in primary teeth, sensitivity testing is of limited value, due to the difficulty in obtaining adequate cooperation from the child. Most often, diagnosis of necrosis is based on inspection of tooth color, response to percussion testing, radiographic observation of a periapical lesion or the presence of a fistula or abscess in relation to the traumatized tooth.
Discoloration of the tooth crown is an important sign of the condition of the pulp. It is observed that traumatized teeth with a normal color only rarely develop periapical inflammation. A discolored tooth, on the other hand, is not necessarily indicating the necrotic state of the pulp. A grayish discoloration recorded shortly after a trauma frequently reflects intrapulpal bleeding. On further examination, the gray hue may gradually fade, and return to normal or almost normal. In this case, the pulp will retain its vitality. However, if the grayish color persists, necrosis should be suspected. Information on the pulpal condition can also be obtained by evaluation of the size of the pulp cavity. If pulp necrosis has occurred, normal physiologic reduction in size will not take place. At the first sign of infection, i.e., formation of a periapical radiolucency (Figure 19.5), fistula or abscess formation, extraction is the treatment of choice to prevent possible sequelae to the permanent successor [4].
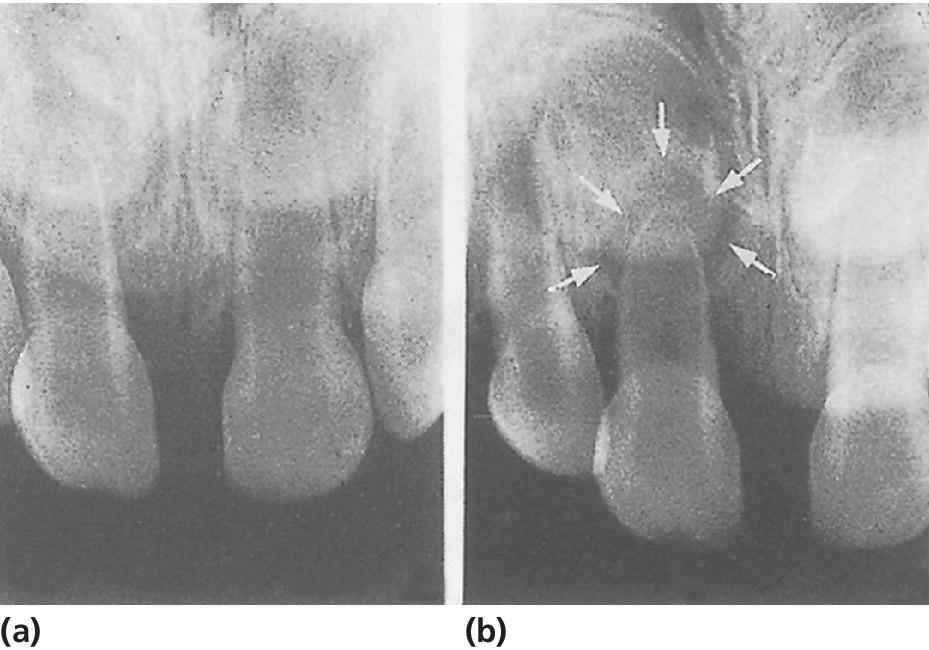
Figure 19.5 (a) Radiograph taken 1 week after slight intrusive luxation of right central incisor. (b) Three months after the trauma there is marked periapical inflammation (arrows).
Pulp canal obliteration
Obliteration of the pulp chamber and canal is a frequent reaction to trauma [3]. The radiograph reveals either partial or total mineralization of the pulp cavity (Figure 19.6). Clinically, the tooth crown gradually assumes a yellowish hue. In the majority of cases, obliterated teeth remain unaffected up to the time of shedding [4].

Figure 19.6 Subluxation of both central incisors leading to pulp canal obliteration. (a) At time of injury. (b) Two years later, there is almost total obliteration of the pulps.
Root resorption
The etiology and pathogenesis of root resorption in primary teeth are identical to root resorption in traumatized permanent incisors. External infection‐related root resorption is usually seen after intrusive luxation, whereas internal resorption may develop as a result of both subluxation and luxation injuries [3]. Extraction is the treatment of choice with all types of pathologic root resorption [4].
Injuries to developing permanent teeth
It is well documented that trauma to a primary tooth is easily transmitted to its permanent successor [5,6]. The highest frequencies of developmental disturbances are found after intrusions, avulsions, and alveolar fractures. Most disturbances occur when the apex of the primary tooth directly traumatizes the permanent tooth bud (Figure 19.7). However, periapical inflammation of the primary tooth may also have harmful effects. The type and severity of disturbances found among permanent incisors are also closely related to the age at the time of injury. A tooth germ is especially vulnerable during its early developmental stages. Thus, the most serious disturbances are seen when the damage occurs before the age of 2 years. Changes in morphology or mineralization of the crown of the permanent incisor are the most common types of complications. These lesions range from small enamel opacities to severe malformations [5,6]. Small enamel opacities on the buccal surface of the incisors is the most frequent sequelae. This type of defect will occur in a case of disturbed enamel maturation in a localized area of the crown. If the ameloblasts are affected during an earlier stage it may result in localized yellow‐brown discoloration and hypoplasia of the enamel (Figures 19.8, 19.9, and 19.10). In case of displacement of a primary tooth directly into the follicle of the permanent successor, dislocation of the mineralized part of the tooth may occur in relation to the soft part of the tooth germ whereby a crown dilaceration will occur (Figure 19.4). A permanent incisor with malformation of the crown has a high risk of pulp necrosis because bacteria can gain access to the pulp through microscopic defects in enamel and dentin. It is therefore recommended to seal the enamel shortly after eruption of the tooth [7]. Trauma may also interfere with root formation, leading to bending of the root or partial arrest of the development [5,6]. Severe malformations of the permanent incisors have been reported in less than 5% of the patients [7]. In these cases it is recommended to monitor the patients closely around the time of eruption. The malformed tooth may fail to erupt due to the damage that has been inflicted on the dental follicle. It can be important to preserve a malformed incisor, in order to secure a normal development of the alveolar bone in the region.
Figure 19.7 Disturbance of development of permanent tooth bud due to intrusion of primary incisor. Due to laceration of the follicle, disturbances in enamel formation will develop.
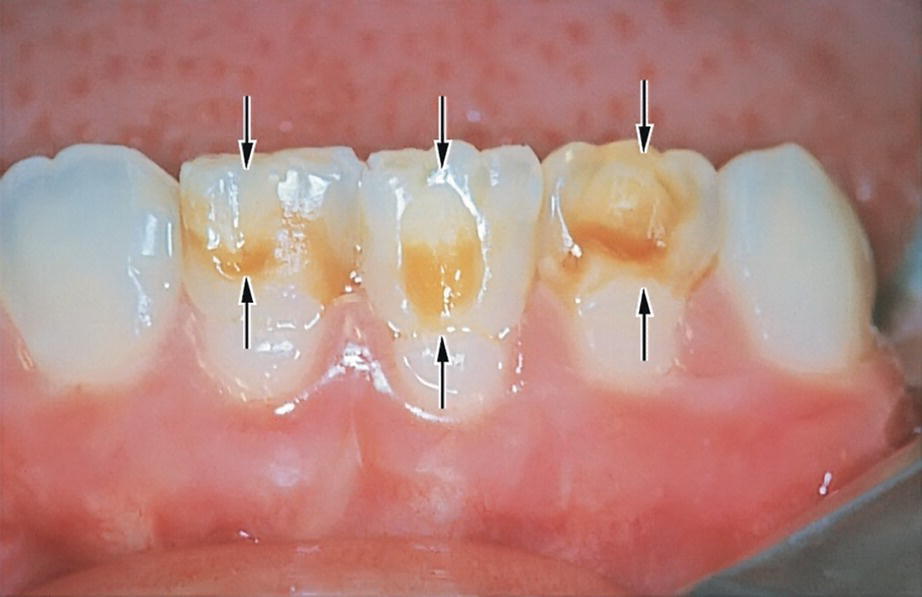
Figure 19.8 Enamel defects in three mandibular incisors (arrows) resulting from avulsion of corresponding predecessors at the age of 2 years.

Figure 19.9 External enamel hypoplasia of right central incisor caused by intrusion of predecessor at the age of 18 months. The hypoplastic area is covered with composite.

Figure 19.10 A simplified model of the different stages of amelogenesis. The secretory stage where the ameloblasts are secreting the enamel matrix and the early and late maturation fases where the enamel crystals are growing and the mineral content reaches 96% prior to tooth eruption. The reduced enamel epithelium is fusing with the oral epithelium when the tooth is erupting.
Source: Lauridsen et al. 2014 [7]. Reproduced with permission of Danish Dental Journal.
Permanent teeth: follow‐up and prognosis
Due to the variability of dental tissue involved, each specific traumatic injury has an individual prognosis (www.dentaltraumaguide.org). Trauma patients should therefore be recalled with intervals that allow timely diagnosis and treatment of potential complications. Re‐examinations should thus be individualized. Most complications are observed within the first year after trauma. However, the follow‐up evaluation of permanent teeth should continue until treatment of all complications is completed, or until a lost or extracted permanent tooth has been adequately replaced. The following time schedule may serve as a guide for trauma types with moderate or high frequencies of complications: 1 week, 3 weeks, 6 to 8 weeks, 3, 6, and 12 months; thereafter, once a year for 5 years.
The follow‐up examinations should include testing of pulp sensibility, percussion and mobility, and inspection of the tooth color.
A standardized radiographic technique should be used, whereby the tooth is visualized in several projection angles, which are identical during the follow‐up period [8]. The use of film holders is highly recommended.
Pulpal and periodontal complications
Pulp canal obliteration
Pulp canal obliteration is the term used to describe the progressive hard tissue formation within the pulp cavity. A gradual narrowing of the pulp chamber and root canal is observed on radiographs, leading to either partial or total obliteration (Figures 19.11, 19.12, and 19.13). Reduced electrometric response and even loss of sensibility may be recorded as a result of the mineralization. Another clinical observation is a yellowish color of the crown.
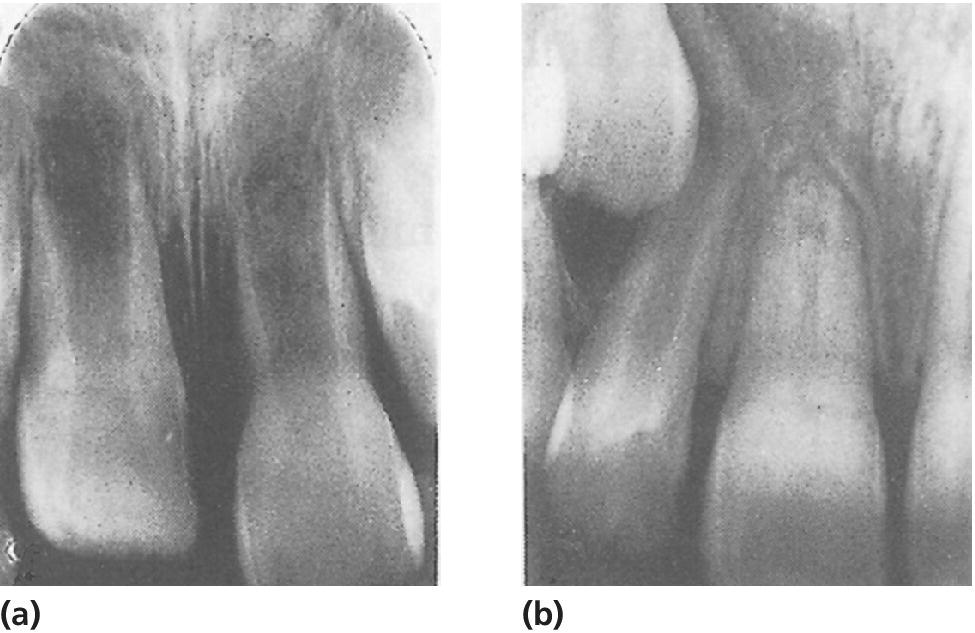
Figure 19.11 (a) Intrusive luxation of immature right central incisor. (b) Spontaneous re‐eruption, closure of apical foramen, and pulp canal obliteration have occurred.

Figure 19.12 Partial pulp canal obliteration in left central incisor. (a) At time of injury. (b) Condition 15 years later. Pulp chamber completely obliterated and root canal slightly reduced in size (arrow).

Figure 19.13 Obliteration after successful replantation of right central incisor. The tooth was replanted within a few minutes. (a) Normal findings 3 weeks later. (b) A radiograph taken 6 months later shows apical closure. (c) Seven years after replantation, there is total pulp canal obliteration and no sign of root resorption.
It is not fully understood what stimulates odontoblasts to start the formation of hard tissue on the root canal walls. However, obliteration appears to be significantly related to teeth with incomplete root formation. Obliteration is also more frequent after extrusion, lateral luxation, and intrusion than after concussion and subluxation, which indicates that the disturbance in dentin formation may be related to the revascularization of the pulp [9,10].
Although a radiograph gives the illusion of complete mineralization of the pulp cavity, a minute strand of pulp tissue always remains. In about 13% of these teeth the pulp becomes necrotic and periapical inflammation develops [11,12]. This is a late complication, usually seen 5–20 years after the injury. In a long‐term follow‐up study these pulp necrosis events were found to increase at about 1% per year [13]. Despite the excessive mineralization, the root canal is nearly always accessible for conventional endodontic treatment.
Pulp necrosis
Pulp necrosis is the most common post‐traumatic complication [9]. If the neurovascular supply to the pulp is severed at the time of injury, pulp healing may occur due to ingrowth of new blood vessels and nerve fibers. Revascularization of the pulp is most likely to occur in teeth with immature root development; but in children and adolescents it may also occur in teeth with mature root development. However, it is only possible in the absence of bacteria in the root canal. The long‐term prognosis of the pulp is therefore primarily related to the extent of damage to the neurovascular supply (related to the type of luxation), and the possibility of revascularization of the pulp (reflected by the stage of root development) [9]. Bacteria may gain access to the pulp through exposed dentin, e.g., in case of fracture of the crown or damage to the root surface. Hence, teeth with combination injuries (luxation injury and a crown fracture) have an increased risk of pulp necrosis [14–16].
Clinical signs of pulp necrosis
While some pulp necroses can be diagnosed within the first 3 months after injury, years may pass before signs of necrosis become apparent. Diagnosing pulp necrosis usually implies the use of pulp sensibility testing, evaluation of color changes, and radiographic examination for signs of pathosis such as periapical radiolucency, root resorption, and/or arrested root development.
Pulp sensibility testing. Sensibility testing can be performed with an electric pulp test, cold test, or by blowing air on exposed dentin. It is important to bear in mind that it is a measure of the sensory nerve activity and not a measure of the vitality of the pulp. In case of revascularization after complete severance of the pulp, the regeneration of the sensory nerves takes longer than the ingrowth of new blood vessels [2]. The tooth may therefore not respond to sensibility test until 3–12 months after injury. A negative test alone should, therefore, not be regarded as proof of necrosis. Endodontic treatment should always be postponed until at least one other clinical and/or radiographic sign of necrosis appears. In addition, teeth with immature root development may have a higher threshold for reaction to sensibility test because the sensory nerves are not yet fully developed.
Tooth discoloration. An almost immediate pinkish discoloration indicates intrapulpal bleeding caused by the trauma. In the following weeks the red color may turn gray but in case of pulp healing, the discoloration will gradually fade away (Figure 19.14). However, if the tooth crown turns progressively gray, necrosis should be suspected. A grayish color that appears for the first time several weeks or months after trauma is regarded as a sign of necrosis. In this case, the gray color signifies decomposition of necrotic pulp tissue. Teeth with pulp canal obliteration may appear yellow [8].
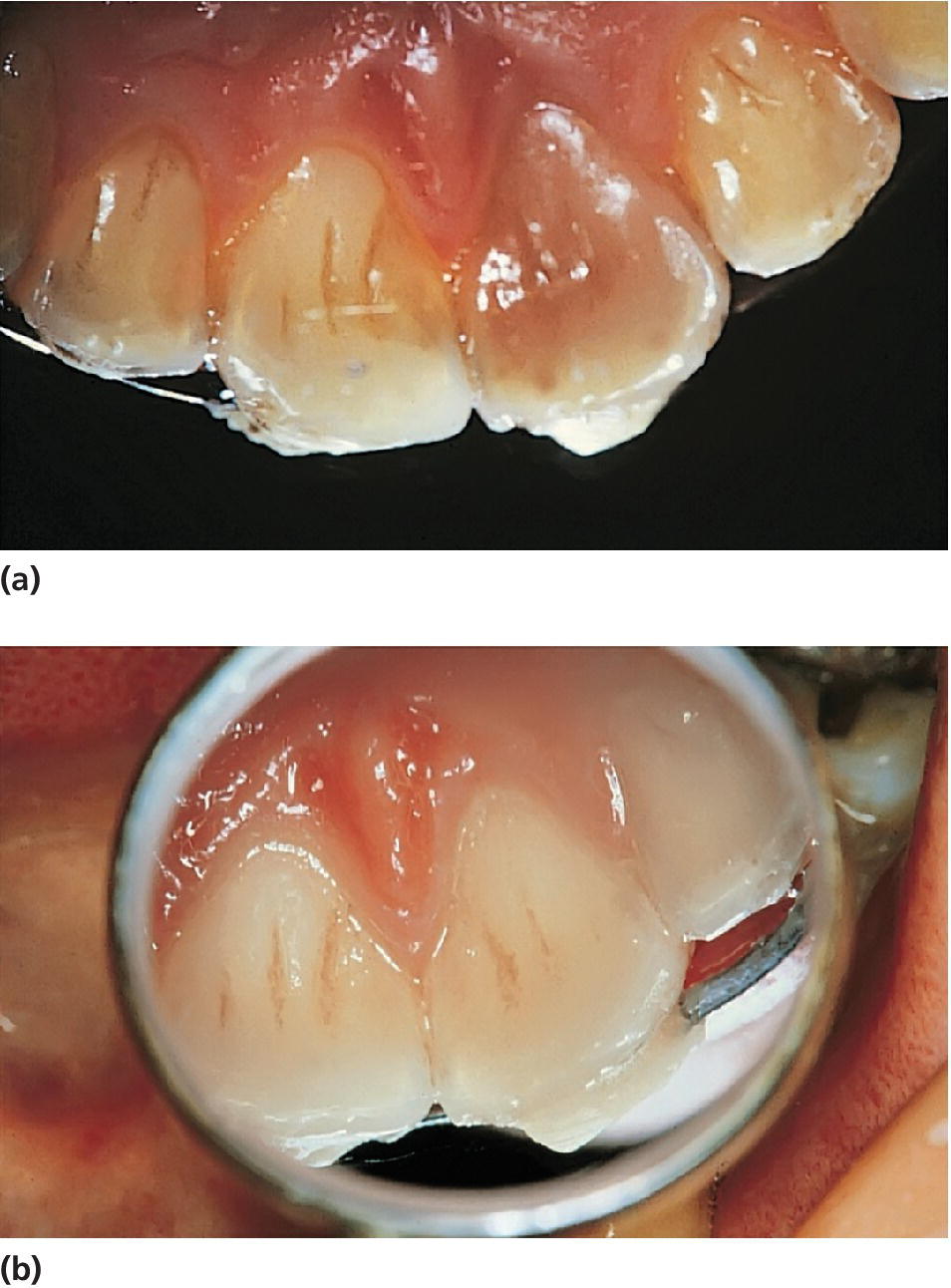
Figure 19.14 (a) Left central incisor in 10‐year‐old boy discolored within 1 week after subluxation injury. (b) Three months later. Discoloration has disappeared and the tooth responds normally to electrometric pulp testing.
Radiographic signs of pulpal necrosis
To get maximum information from a radiographic follow‐up it is mandatory that a standardized radiographic technique is used to ensure that series of radiographs may be adequately compared. The use of filmholders is therefore recommended.
Periapical radiolucency. An increased width of the periodontal ligament and loss of lamina dura in the apical area, may be a sign of pulp healing seen in relation to revascularization of the pulp. However, increasing size of the defect and development of a persistent apical radiolucency indicate periapical inflammation in respond to bacteria in the root canal [8].
Arrest of root development. If necrosis involves the epithelial root sheath before root development is complete, no further root growth takes place. It should be borne in mind that necrosis may progress from the coronal to the apical part of the pulp. In this way, vitality may apparently persist for a while apically, resulting in the formation of a calcified barrier across the wide apical foramen [2] (Figure 19.15).
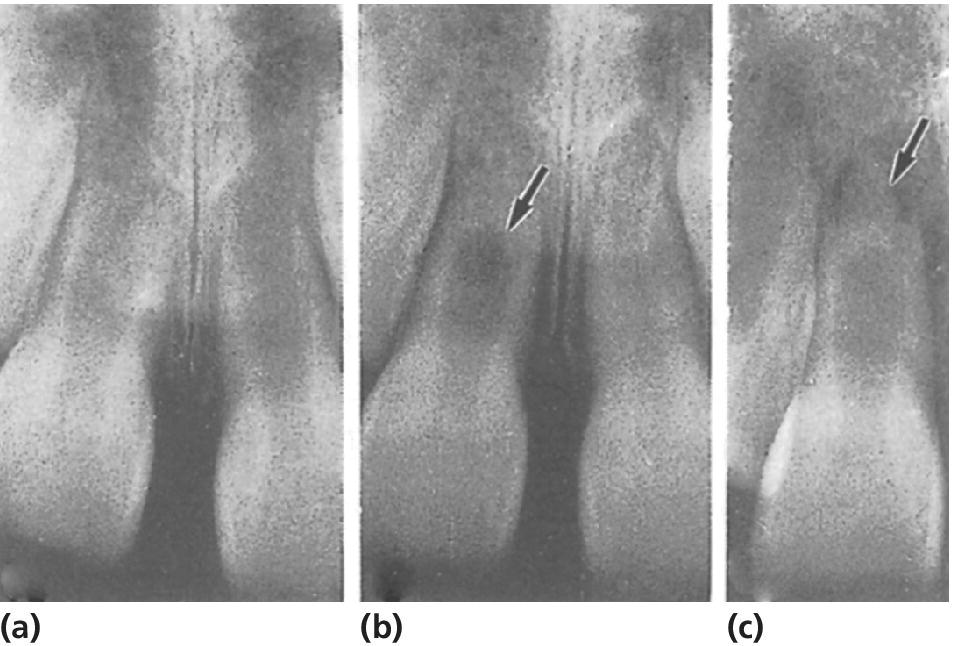
Figure 19.15 Pulp necrosis of right central incisor following intrusion. (a) Re‐eruption took place 3 months after injury. (b) No further root development. Hard tissue formation (arrow) is found together with continued vitality. (c) Pulp necrosis is diagnosed from a periapical radiolucency (arrow), which developed 1 year after injury.
Cervical root fractures after endodontic treatment
Endodontic treatment of nonvital immature teeth is reported to be highly successful (see Chapter 17). However, it is important to realize that success refers to the primary goal: a tight apical seal. Necrosis in a developing tooth results in arrested dentin formation, often resulting in thin dentinal walls. These fragile walls are susceptible to fracture particularly in the cervical area (Figure 19.16). The frequency of cervical root fracture is reported to range from 2% in an 11‐year‐old to 77% in a 6‐year‐old (Box 19.1) [17]. The thin dentinal walls are the main reason for cervical fractures. However, it has been reported that long‐term use of calcium hydroxide for apexification of immature roots increases the risk of these cervical fractures [18]. This finding has led to a shift in the endodontic procedure for teeth with immature root formation, and formation of an apical plug with MTA is therefore now the recommended procedure. However, the prognosis should still be regarded as doubtful to poor with pulp necrosis in children 6–10 years of age, and an alternative long‐term treatment plan should be considered. This is of particular importance in malocclusion cases where extraction of premolars is part of the orthodontic treatment plan. The question is whether a nonvital immature incisor with doubtful prognosis should be kept for as long as possible for later prosthetic replacement, or whether the traumatized tooth should be removed and the space closed orthodontically or by premolar autotransplantation.

Figure 19.16 Spontaneous root fracture of nonvital immature central incisor. (a, b) During long‐term treatment with calcium hydroxide. (c) The fracture was observed 1 year after completed endodontic treatment.
Root resorption
Root resorption is a frequent complication subsequent to luxation injuries with tooth displacement [19–21].
Repair‐related resorption (surface resorption)
This resorption entity is characterized by small cavities on the root surface surrounded by a periodontal ligament space of normal width. In the case of multiple cavities affecting the root apex, repair‐related resorption may appear as a shortening of the apex (Figure 19.17). This resorption type is self‐limiting and requires no treatment. It may be considered as a remodeling of the tissues in case of mild to moderate damage to the root surface. Repair‐related resorption is especially frequent in teeth with lateral luxations and extrusions [2,22].

Figure 19.17 External repair related resorption along the root surface and the apex of an extruded central incisor. (a‐c) Clinical and radiographic appearance at the time of injury. (d‐f) Repair related resorption is diagnosed after one year (arrows).
Infection‐related resorption (inflammatory resorption)
Infection‐related resorption is a pathologic and very progressive type of root resorption. It is most frequently seen after severe luxation injuries such as intrusions and avulsions. The development is due to cell damage of the periodontal ligament and the cementum induced by the trauma, and the simultaneous presence of infected necrotic pulp tissue. Bacterial products from the infected root canal will penetrate through the dentin tubules into the periodontal ligament. It is the resulting inflammatory response that causes resorption of the root surface [2,22].
The diagnosis is made radiographically where this resorption appears as bowl‐shaped areas on the root surface associated with radiolucencies in adjacent bone. Hence, the width of the periodontal space is increased. Most frequently, infection‐related resorption is identified in the middle or coronal third of the root (Figures 19.18 and 19.19). Teeth with infection‐related resorption will always respond negatively to pulp sensibility testing.
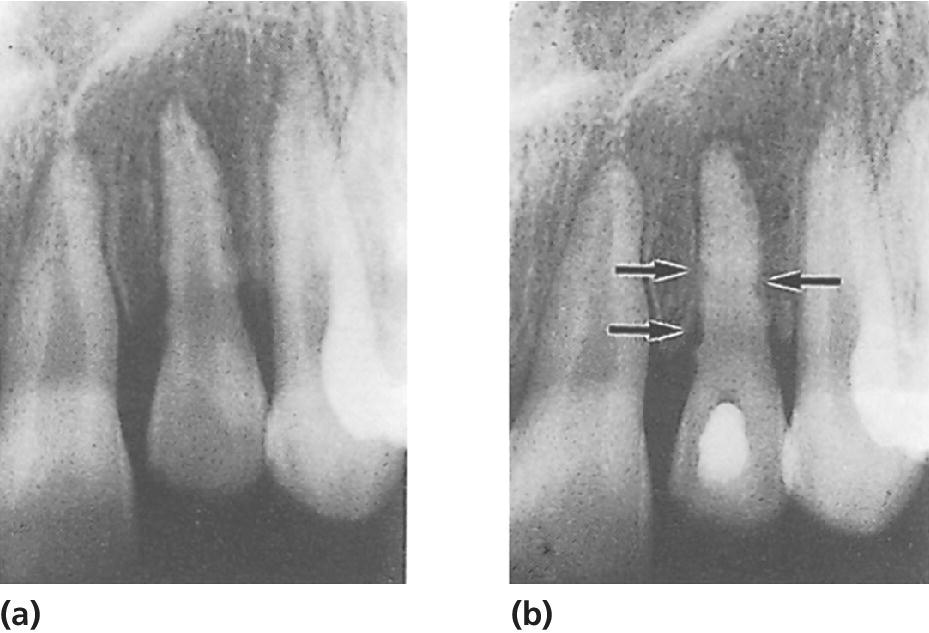
Figure 19.18 External infection‐related root resorption along root surface of an intruded lateral incisor. (a) Six weeks after injury. (b) During endodontic treatment, the pulp cavity was temporarily filled with calcium hydroxide. Persistent defects are seen on the root surface (arrows), but no further progression has taken place.
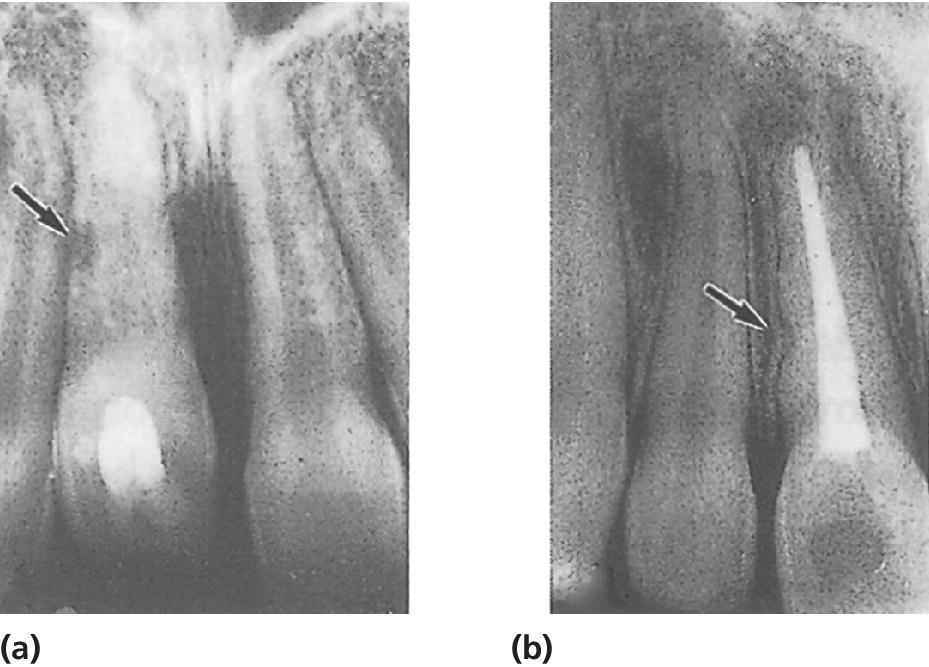
Figure 19.19 External infection‐related root resorption following intrusive luxation of a right central incisor. (a) An area of resorption (arrow) was seen 8 weeks after injury. The pulp canal was temporarily filled with calcium hydroxide. (b) Two years later, there is a persistent defect (arrow), but no further progression of resorption.
The first sign of resorption may be observed as early as 3 weeks after trauma, and most cases are disclosed within the first 3 months. If not present within the first year after the injury, infection‐related resorption is unlikely to occur. If allowed to progress, the resorptive process may destroy the tooth completely within a few months [22]. Immediate endodontic treatment is indicated including removal of necrotic pulp tissue, canal debridement, and treatment with calcium hydroxide followed by a guttapercha root canal filling or MTA filling. In the majority of cases this approach will arrest the process, and cement repair will follow in the resorption cavities (Figure 19.19).
Ankylosis‐related resorption
This type of resorption is significantly related to intrusion and to replantation of avulsed incisors after an extended dry extra‐alveolar period, both instances which represent extensive damage to the PDL. A bony union (ankylosis) is established between the alveolar bone and the root surface, followed by continuous resorption of cementum and dentin replaced by and formation of new bone (Figure 19.20). Radiographically, the normal periodontal space disappears and the tooth substance is gradually replaced by bone. Clinical examination may reveal this type of resorption before it can be seen on X‐ray. A typical finding is a high, metallic percussion sound differing clearly from an uninjured tooth. It appears that most ankylosis‐related resorptions are evident within 2 months to 1 year after the accident [22].

Figure 19.20 Progression of replacement resorption after avulsion and subsequent replantation of left lateral incisor. (a–c) Radiographs taken 6 months, 2 and 4 years after injury. (d) Condition at time of removal of lateral incisor 7 years after replantation.
Unfortunately, there is presently no effective treatment for an ankylosed tooth and eventually the entire root will be substituted by bone. However, the substitution rate is often very low, and the tooth may be maintained for several years. It may take 3–10 years before the root is completely resorbed. The progression rate is strongly age related (Figure 19.20).
Ankylosis disturbs vertical growth of the alveolar process in growing individuals (Figure 19.21). The resulting deficient vertical bone and soft tissue volume may compromise later prosthetic rehabilitation significantly. The moment ankylosis is suspected, an alternative treatment plan should be made. In young patients where abundant alveolar growth is anticipated, decoronation is recommended. In decoronation, the crown is separated from the resorbed root 1–2 mm beneath the marginal bone level. The ankylosed root will then gradually be transformed into bone during the remodeling process, preserving the width and allowing continuous vertical growth of the alveolar process [23]. Both processes are essential for the later tooth replacement whether by a conventional bridge, an autotransplantation of a premolar, or a dental implant. Concerning timing of the decoronation procedure it is essential that it is carried out when the tooth has gone only 2–3 mm in infraposition and there is still more residual growth (and thereby infraposition) to be expected.

Figure 19.21 Infraposition of a left central incisor due to replacement resorption (ankylosis).
In cases where the infraposition is diagnosed late or when little additional vertical growth is anticipated, an osteotomy may be performed around the ankylosed tooth concomitant with placement of an interpositional bone grafting material and rigid fixation. Using this technique, the width and height of the alveolar process is also preserved and the ankylosed tooth may serve as a long‐term fixed provisional space maintainer until the growth has ended, and the final prosthetic treatment can be performed.
Ridge preservation (or socket preservation), where a bone substitute material with a low substitution rate is placed into the extraction socket after removal of the ankylosed tooth, is well documented to preserve the dimensions of the alveolar ridge in adults. However, it is not recommended in growing individuals, since this technique has led to arrested alveolar growth as seen with the ankylosed teeth and early placed implants [24].
Root canal resorption (internal resorption)
Internal root resorption is a rare complication in traumatized teeth. It is probably caused by a chronic pulpal inflammation due to a partial pulp necrosis. Internal resorption is usually present without clinical symptoms, and is first diagnosed radiographically. The diagnosis is usually made years after trauma. The process may progress very rapidly, and endodontic treatment should be started as soon as the diagnosis is made. The prognosis is good if endodontic treatment is initiated before the resorption becomes extensive, with perforation of the root surface.
Prognosis following trauma to permanent teeth
Infraction and uncomplicated crown fracture
Traumatized teeth without associated periodontal injuries suffer remarkably few complications. High‐risk teeth with respect to pulp necrosis after crown fractures appear to be those with untreated deep corner fractures [25].
Treatment of uncomplicated crown fractures in childhood often consists of rebonding of the tooth fragment or a composite restoration (see Chapter 18). These procedures usually represent only a semi‐permanent solution, whereas a definitive restoration with porcelain laminate onlays or porcelain crowns normally has to wait until adult age has been reached.
Complicated fracture
The two standard treatments—pulp capping and partial pulpotomy—appear to result in successful healing in more than 90% of cases (see Chapters 12 and 18).
Crown–root fracture
No studies have compared the results of the different treatment procedures described in Chapter 18. It appears, though, that orthodontic extrusion of apical root fragment leads to a stable periodontal condition, whereas surgical exposure of the palatal fracture site has been found to lead to chronic inflammatory changes within the palatal gingiva in some cases. After some time, this may result in slight migration of the restored tooth in a buccal direction. Surgical repositioning of an apical fragment has been found to have a good long‐term survival [26].
Root fracture
In about 80% of all root fractured teeth the pulp remains viable or becomes revascularized, and repair occurs in the fractured area [9,27–29]. In this regard, four main types of healing events have been found (Figure 19.22 and Box 19.2).

Figure 19.22 Radiographs and diagrams illustrating various modalities of healing after root fractures. (a) Healing with calcified tissue. (b) Interposition of connective tissue. (c) Interposition of bone and connective tissue. (d) Interposition of granulation tissue.
Source: Andreasen 1995 [9]. Reproduced with permission of F. Andreasen.
Pulp necrosis is caused by an infected pulp in the coronal fragment. This condition can often be diagnosed within 6 months after injury. Severe dislocation of the coronal fragment and mature root formation at the time of injury significantly increases the risk of pulp necrosis [27,28].
Concerning therapy, it is important to realize that the apical fragment almost always contains viable pulp tissue. Endodontic treatment can therefore be confined to the coronal fragment. After completion of endodontic treatment, repair between the two fragments with connective tissue (PDL) is a consistent finding [30] (Figure 19.23). If the infection has spread to the apical fragment, it may have to be removed surgically.
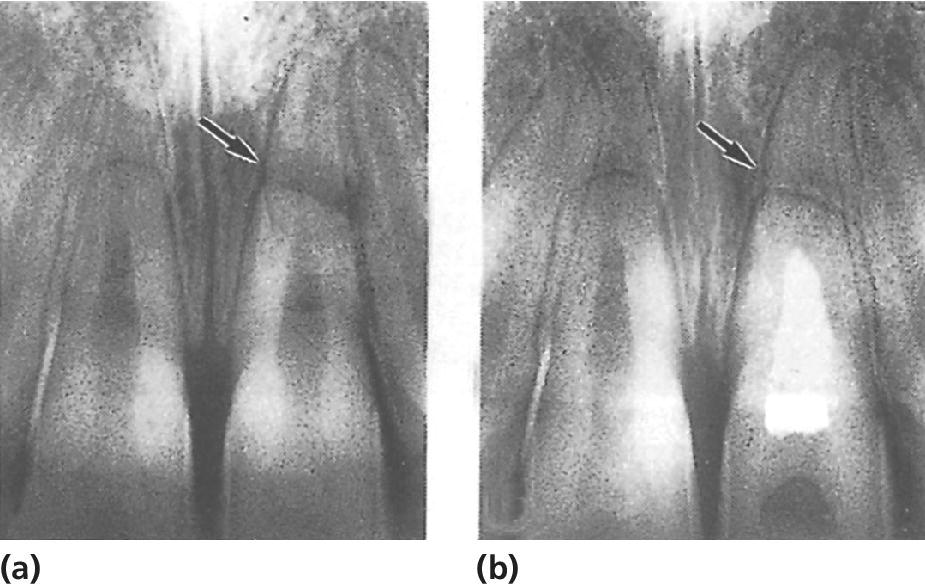
Figure 19.23 Root fractures of both central incisors. (a) Retained pulpal vitality and calcified tissue repair in the right incisor, whereas radiolucency corresponding to fracture line (arrow) indicates necrosis in the left incisor. (b) Two years after completed root filling of left incisor PDL union between segments is evident.
When teeth with fractures in the cervical third of the root develop necrosis, the following procedure should be considered: extraction of the coronal fragment with subsequent orthodontic extrusion of the apical fragment or a decoronation procedure.
Irrespective of healing type, root fractured teeth have a reasonably good long‐term prognosis, especially fractures located in the mid or apical position of the root [30].
Luxation injuries
The long‐term prognosis of luxated teeth without displacement (concussion and subluxation) is very good with a very low risk of healing complications [31]. Pulp necrosis is frequent in mature teeth with extrusion and lateral luxation whereas pathologic root resorption is rare. Intrusions represent a very severe injury type, which may lead to tooth loss due to progressive root resorption. Teeth with combination injuries, where the tooth has suffered both a fracture and a luxation injury, have an increased risk of pulp necrosis and infection‐related resorption [14–16].
Avulsion followed by replantation
In teeth with a wide‐open apical foramen, revascularization of the pulp may occur (Figure 19.24). The pulp tissue of an avulsed tooth apparently has the potential to survive for up to 3 hours out of the socket. Therefore, in teeth replanted within 3 hours, endodontic treatment is postponed until pulp necrosis is evident. These teeth must be followed closely. With signs of necrosis, such as infection‐related resorption, endodontic treatment should be started immediately. It is recommended that a replanted tooth with incomplete root formation is examined radiographically every second week until pulp necrosis is confirmed or until continued root formation is evident.
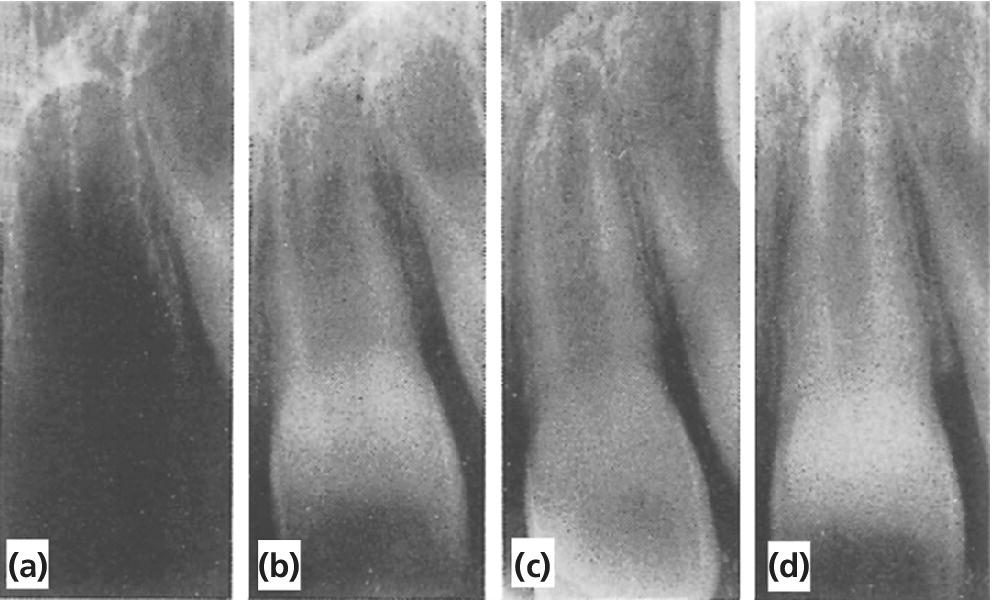
Figure 19.24 Successful replantation of a left central incisor (arrows). The tooth was stored in the mouth of the child’s mother for 45 min. (a–c) Radiographs taken before, 12 days and 6 months after replantation, respectively. (d) One year after injury, with continued root development and narrowing of pulp canal.
Pulp revascularization is not likely to take place in teeth with a closed apical foramen, and endodontic treatment must be started within 1–3 weeks after replantation to prevent the onset of infection‐related resorption. Root resorption is very frequent following avulsion, and all three types of resorption may occur.
Dental Trauma Guide
The Dental Trauma Guide (www.dentaltraumaguide.org) provides detailed prognosis estimates for all the different types of traumatic dental injuries and also for teeth with a combination of injuries. The risk of pulp necrosis, pulp canal obliteration, repair‐related resorption, infection‐related resorption, ankylosis‐related resorption, marginal bone loss, and tooth loss is given for teeth with mature and immature root development [31].
Treatment options in case of trauma related loss of permanent teeth
In cases where traumatized teeth are lost or have a doubtful prognosis (e.g., due to progressive root resorption), several factors need to be addressed before the final treatment plan is determined:
- age of the patient
- remaining craniofacial growth including vertical growth of the alveolar process
- available space between crowns and roots of teeth adjacent to the traumatized area
- occlusal relations
- hard and soft tissue conditions of the alveolar process
- compliance of the patient including oral hygiene.
Evaluation of these factors assist in determining the treatment plan, which may include orthodontic space closure, acid‐etched or conventional fixed prosthetics, autotransplantation of premolars or placement of dental implants. Study casts and radiographs including periapical, lateral cephalometric, and panoramic radiographs are essential. To aid in the choice between these treatment possibilities, study casts are essential.
Orthodontic space closure may be performed at any age. Treatment with conventional fixed prosthetics usually has to be postponed until adult age due to risk of devitalizing the pulp by preparing teeth with large pulp cavities. Acid‐etched fixed bridges (Rochette or Maryland bridges) are less destructive to intact adjacent teeth. However, they may interfere with growth and cause displacement of anterior abutment teeth in case of ideal interincisal support. Another treatment procedure that can be used in adolescents is autotransplantation of premolars to the region of the tooth loss. Due to the unique osteogenic capacity of a tooth graft, this procedure offers a treatment alternative in which both the lost tooth and the atrophied alveolar ridge may be replaced [32]. Recent studies have demonstrated good long‐term survival of these transplants, thus providing a realistic treatment alternative for tooth replacement in young individuals [33]. A full orthodontic analysis is indispensable before autotransplantation is planned. Autotransplantation may predictably replace a missing tooth. However, the price of the replacement should not be malocclusion. The key factors for success with tooth transplantation include proper selection of donor tooth with 2/3 to ¾ root development, as well as low‐trauma surgical techniques to harvest the donor tooth, and to prepare the recipient site.
Placement of dental implants is another well‐documented way to replace teeth lost as a consequence of dental trauma, with favorable long‐term prognosis. The direct and functional bond between alveolar bone and titanium implant surface is termed “osseointegration.” After a healing period of up to 3 months, the final prosthetic rehabilitation can be performed without engaging adjacent intact teeth. In the early days, osseointegration was also called “functional ankylosis,” which implies that the implant in some ways will behave like an ankylosed tooth. As a consequence, dental implants are contraindicated in individuals where maxillofacial growth is not yet complete. The implant will stay in its original position and progressive infraocclusion can be anticipated in case of ongoing alveolar growth or continued eruption of the adjacent teeth. Minor infraocclusion may be treated by renewal of the implant‐retained crown. However, in more extreme cases, the implant has to be removed, followed by augmentation of bone and soft tissue, before placement of a new implant can be performed. Chronological age cannot be used as a determinant for cessation of growth. Methods to monitor growth include superimposition of lateral cephalometric radiographs taken one year apart, height measurements, and hand‐and‐wrist radiographs. In addition the presence of interincisal support is believed to reduce the chance of continued eruption of adjacent teeth, and thereby minimize the risk of implant infraposition.
Often, alveolar bone is lost concomitant with dento‐alveolar trauma. Unlike autotransplantations, dental implants do not have the capacity to induce new bone formation. However, predictable methods exist to augment bone in the horizontal dimension using autogenous bone blocks or guided bone regeneration techniques [34]. Vertical bone augmentation is at present less predictable. However, alveolar distraction osteogenesis or local segment osteotomies with interpositional bone grafts may provide sufficient conditions for the later implant‐retained prosthetic rehabilitation.
References
- 1. Gottrup G, Storgard JS, Andreasen JO. Wound healing subsequent to injury. In: Andreasen J.O., Andreasen FM, eds. Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th edn. Oxford: Blackwell, 2007; 1–61.
- 2. Andreasen JO, Løvschall H. Response of oral tissues to trauma. In: Andreasen JO, Andreasen FM, Andersson L, eds. Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th edn. Oxford: Blackwell Munksgaard, 2007.
- 3. Borum MK, Andreasen JO. Sequelae of trauma to primary maxillary incisors. I. Complications in the primary dentition. Endod Dent Traumatol 1998;14:31–44.
- 4. Flores MT, Holan G, Borum MK, Andreasen JO. Injuries to the primary dentition. In: Andreasen J.O., Andreasen FM, Andersson L, eds. Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th edn. Oxford: Blackwell, 2007; 516–41.
- 5. Andreasen JO, Ravn JJ. The effect of traumatic injuries to primary teeth on their permanent successors. II. A clinical and radiographic follow‐up study of 213 injured teeth. Scand J Dent Res 1970;79:284–94.
- 6. Andreasen JO, Sundstrøm B, Ravn JJ. The effect of traumatic injuries to primary teeth on their permanent successors. I. A clinical, radiographic, microradiographic and electronmicroscopic study of 117 injured permanent teeth. Scand J Dent Res 1970;79:219–83.
- 7. Lauridsen E, Yousaf N, Andreasen JO. Udviklingsdefekter på de permanente incisiver som følge af traume i det primære tandsæt. Tandlægebladet. Særnummer November 2014.
- 8. Andreasen FM, Andreasen JO. Diagnosis of luxation injuries: the importance of standardized clinical, radiographic and photographic techniques in clinical investigations. Endod Dent Traumatol 1985;1:160–9.
- 9. Andreasen FM. Pulpal healing after luxation injuries and root fracture in the permanent dentition. Thesis, Copenhagen University, 1995.
- 10. Robertson A. Pulp survival and hard tissue formation subsequent to dental trauma. Swed Dent J 1997; Suppl 125.
- 11. Cvek M, Granath L‐E, Lundberg M. Failures and healing in endodontically treated non‐vital anterior teeth with post‐traumatically reduced pulpal lumen. Acta Odont Scand 1982;40:223–8.
- 12. Jacobsen I, Kerekes K. Long‐term prognosis of traumatized permanent anterior teeth showing calcifying processes in the pulp cavity. Scand J Dent Res 1977;85:588–98.
- 13. Robertson A, Andreasen FM, Bergenholtz G, Andreasen JO, Norén JG. Incidence of pulp necrosis subsequent to pulp canal obliteration from trauma of permanent incisors. J Endod 1996;22:557–60.
- 14. Lauridsen E, Hermann N, Gerds TA, Ahrensburg SS, Kreiborg S, Andreasen JO. Dental trauma. Combination injuries 1. The risk of pulp necrosis in permanent teeth with concussion injuries and concomitant crown fractures. Dent Traumatol 2012;28:364–70.
- 15. Lauridsen E, Hermann N, Gerds TA, Ahrensburg SS, Kreiborg S, Andreasen JO. Dental Trauma. Combination injuries 2. The risk of pulp necrosis in permanent teeth with subluxation injuries and concomitant crown fractures. Dent Traumatol 2012;28:371–8.
- 16. Lauridsen E, Hermann N, Gerds TA, Ahrensburg SS, Kreiborg S, Andreasen JO. Dental trauma. Combination injuries 3. The risk of pulp necrosis in permanent teeth with extrusion or lateral luxation injuries and concomitant crown fractures without pulp exposure. Dent Traumatol 2012;28:379–85.
- 17. Cvek M. Prognosis of luxated non‐vital maxillary incisors treated with calcium hydroxide and filled with gutta‐percha. A retrospective clinical study. Endod Dent Traumatol 1992;8:45–55.
- 18. Andreasen JO, Munksgaard EC, Bakland LK. Comparison of fracture resistance in root canals of immature sheep teeth after filling with calcium hydroxide or MTA. Dent Traumatol 2006;22:154–6.
- 19. Andreasen JO. Review of root resorption systems and models. Etiology of root resorption and the homeostatic mechanisms of the periodontal ligament. In: Davidovitch D, ed. The biological mechanisms of tooth eruption and root resorption. Birmingham: EBSCO Media, 1988; 9–21.
- 20. Andreasen JO. Experimental dental traumatology: development of a model for external root resorption. Endod Dent Traumatol 1987;3:269–87.
- 21. Andreasen JO, Andreasen FM. Root resorption following traumatic dental injuries. Proc Finn Dent Soc 1991;88:95–114.
- 22. Andreasen JO, Andreasen FM, Bakland LK, Flores MT. Traumatic Dental Injuries—a Manual, 3rd edn. Oxford: Wiley‐Blackwell, 2011.
- 23. Malmgren B. Ridge preservation/decoronation. Pediatr Dent 2013;35:164–9.
- 24. Sandor GKB, Kainulainen VT, Queiroz JO, Carmichael RP, Oikarinen KS. Preservation of ridge dimensions following grafting with coral granules of 48 post‐traumatic and post‐extraction dento‐alveolar defects. Dental Traumatol 2003;19:221–7.
- 25. Ravn JJ. Follow‐up study of permanent incisors with enamel‐dentin fractures after acute trauma. Scand J Dent Res 1981;89:355–65.
- 26. Kahnberg K‐E. Surgical extrusion of root fractured teeth—a follow‐up study of two surgical methods. Endod Dent Traumatol 1988;4:85–9.
- 27. Andreasen JO, Andreasen FM, Mejare I, Cvek M. Healing of 400 intra‐alveolar root fractures. 1. Effect of pre‐injury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent Traumatol 2004;20(4):192–202.
- 28. Andreasen JO, Andreasen FM, Mejare I, Cvek M. Healing of 400 intra‐alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent Traumatol 2004;20(4):203–11.
- 29. Jacobsen I. Traumatized teeth. Clinical studies of root fractures and pulp complications. Thesis. Oslo, 1981.
- 30. Cvek M, Mejare I, Andreasen JO. Conservative endodontic treatment of teeth fractured in the middle or apical part of the root. Dent Traumatol 2004;29:261–9.
- 31. Andreasen JO; Lauridsen E, Gerds T.A, Ahrensburg SS. Dental Trauma Guide: A source of evidence‐based treatment guidelines for dental trauma. Dent Traumatol 2012;28:345–50.
- 32. Andreasen JO., Andersson L, Tsukiboshi M. Autotransplantation of teeth to the anterior region. In: Andreasen J.O., Andreasen FM, Andersson L, editors. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 4 ed. Oxford: Blackwell; 2007. p. 740–60.
- 33. Czochrowska EM, Stenvik A, Bjercke B, Zachrisson BU. Outcome of tooth transplantation: Survival and success rates 17–41 years posttreatment. Am J Orthod Dentofacial Orthop 2002;121:110–19.
- 34. Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone‐substitute materials. Int J Oral Maxillofac Implants 2009;24 Suppl:218–36.