CHAPTER 18
Traumatic Dental Injuries: Examination, Diagnosis, and Immediate Care
Eva Fejerskov Lauridsen, Simon Storgård Jensen, and Jens O. Andreasen
It is well documented that the majority of traumatic dental injuries occur in children. Thus, in a Swedish study, 83% of all individuals with acute dental trauma were younger than 20 years of age [1]. Injuries to primary or permanent teeth can appear rather severe, particularly when associated with trauma to supporting tissues (Figures 18.1 and 18.2). The situation is distressing for both the child and parents. It is important that the dentist and the other members of the dental team are well prepared to meet the many complex and challenging problems in the care of dental emergencies (Box 18.1).
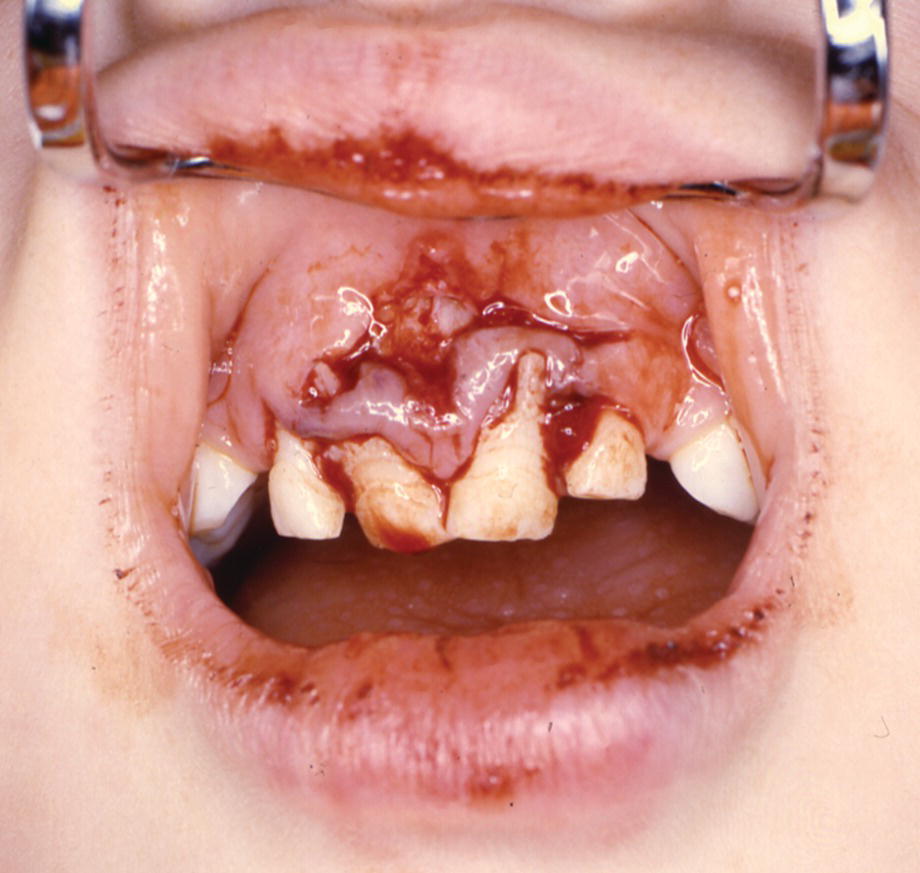
Figure 18.1 A 4‐year‐old boy with lateral luxation of three primary incisors and extensive gingival laceration.

Figure 18.2 The patient has had an impact where the force has been transmitted through the upper lip to the teeth and the alveolar process. Note the lip laceration and abrasion and the displacement of the right central and lateral incisors.
Epidemiology
Traumatic dental injuries are frequent. A Danish study showed that 30% of children had suffered traumatic dental injuries in the primary dentition and 22% in the permanent dentition [2]. The incidence of injuries to primary teeth increases from 1 year of age, and most traumas involve children younger than 4 years of age. In the permanent dentition, the most accident‐prone time is between 8 and 10 years of age (Figure 18.3). Boys appear to sustain injuries to permanent teeth twice as often as girls. Traumatic dental injuries usually affect one or two of the anterior teeth, and especially the maxillary central incisors (Figure 18.4) [3].
Figure 18.3 Percentage distribution of 1275 children with traumatic dental injuries related to age at the time of injury.
Source: Skaare & Jacobsen 2003 [3]. Reproduced with permission of John Wiley & Sons.
Figure 18.4 Distribution of injuries of the most frequently injured permanent teeth: 97% of all injuries affected the incisors.
Source: Skaare & Jacobsen 2003 [3]. Reproduced with permission of John Wiley & Sons.
Etiology
In a young child learning to walk and to run, muscle coordination and judgment are incompletely developed and falling injuries frequently occur. Trauma to the orofacial area may also be part of child physical abuse. The characteristics of this unfortunate condition are presented in Box 18.2.
A Norwegian study of children aged from 7 to 18 years reported that 48% of all dental traumas occurred during school hours and 52% during leisure time. Nearly half of the leisure‐time injuries occurred when children were playing. Ten percent happened in traffic, and half of these were bicycle accidents. Twenty‐five percent occurred while partying or visiting bars and clubs [4].
In contrast to common belief, only 8% of all injuries were sports related. Finally, in the age group 16–18 years, 23% of all orofacial injuries resulted from violence [4].
Examination
To ensure that all relevant data are recorded, a standardized trauma form is recommended [5]. This form serves as a checklist for the dentist at the initial visit and at subsequent appointments.
History
When the patient is received for treatment, the first step is to gain an initial impression of the extent of the injury. Is there a need for immediate medical care? Is the patient’s general condition affected? If not, the following questions should be asked to end up with a correct diagnosis, and allow treatment planning:
- When did the injury occur? The time interval between injury and treatment can influence both the treatment procedure and the expected outcome. Thus, optimal repositioning of a displaced permanent tooth is difficult if treatment is delayed. The time factor is also very critical for the prognosis of avulsed teeth.
- Where did the injury occur? This information is important for insurance and social security purposes. The place of accident also provides information on the need for tetanus prophylaxis in replantation cases.
- How did the injury occur? The nature of the blow may provide clues as to the type of injury to be expected. For example, when a blow hits the chin, the mandibular arch is forced against the maxillary arch, with jaw fracture or crown–root fractures in the premolar or molar regions as possible resulting injuries.
- Was there a period of unconsciousness? If so, for how long? Is there headache? Amnesia? Nausea? Vomiting? Excitation or difficulties in focusing the eyes? These are all signs of brain concussion and require medical attention.
- Is there any disturbance in the occlusion? Can imply luxation injury, alveolar fracture, jaw fracture, or luxation or fracture of the temporomandibular joint. Limitations of mandibular movement or mandibular deviation on opening or closing the mouth indicate that the jaw may be fractured.
- Have there been previous injuries to the teeth? Answers to this may explain radiographic findings, such as pulp canal obliteration and incomplete root formation in a dentition with otherwise completed root development.
Medical history
A short medical history should include information about medication, allergies, bleeding disorders, and other conditions that could interfere with treatment or prognosis. Ask also if the patient is covered by antitetanus vaccination.
Extraoral examination
Palpation of the facial skeleton and mandible and note is taken of soft tissue swelling, bruises, or lacerations to the face and lips. Deep lip wounds are examined closely with respect to tooth fragments or other foreign bodies (Figure 18.5).
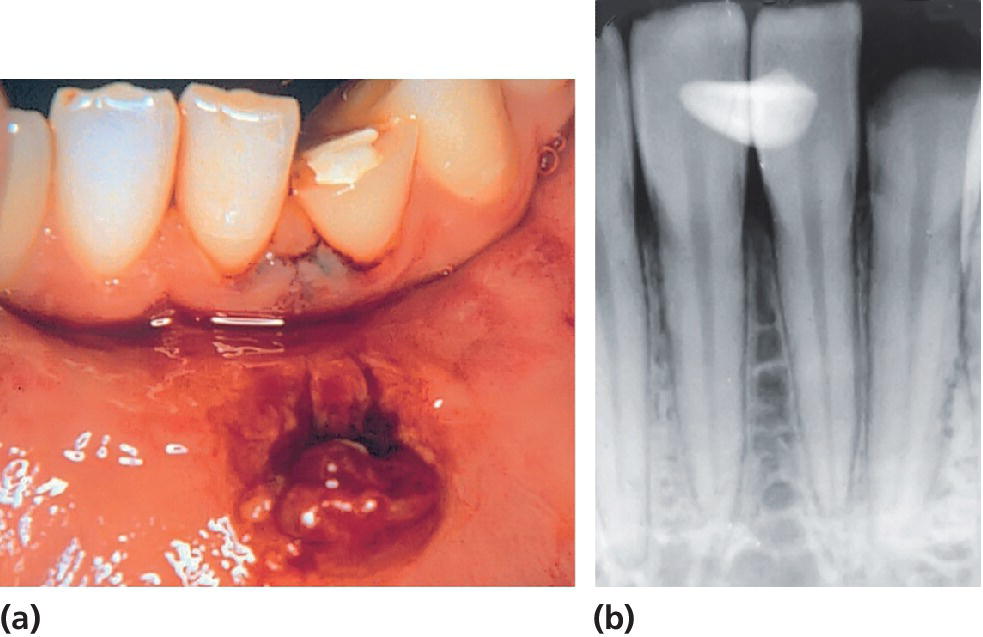
Figure 18.5 (a) Crown fracture of mandibular lateral incisor and mandibular lip lesion. (b) A radiograph reveals the fractured tooth fragment hidden in the lip lesion.
Intraoral examination
The examination must be systematic and include the recording of:
- swelling, laceration, and hemorrhage of the oral mucosa and gingiva
- abnormalities in occlusion
- missing, displaced or mobile teeth, fractured crowns, or cracks in the enamel.
It is important to examine all teeth within a traumatized area and, in close bite situations, also teeth in the opposite jaw. Particular note is taken of the following factors:
- Displacement. The direction (intrusion, extrusion, retrusion or protrusion) as well as the extent (in millimeters) of displacement should be recorded. Minor displacements can be difficult to detect. In such cases it is helpful to examine the occlusion as well as radiographs taken at various angulations.
- Mobility. The degree of mobility is assessed in both a horizontal and vertical direction, keeping in mind that immature permanent teeth and primary teeth undergoing root resorption may have quite extensive physiologic mobility. When several teeth move together en bloc, a fracture of the alveolar process should be suspected.
- Reaction to percussion. The handle of a mouth mirror is tapped gently against the teeth in both a horizontal and vertical direction. Tenderness to percussion indicates damage to the periodontal ligament. A high metallic tone implies that the injured tooth is locked in bone.
- Color of the tooth. Discoloration may appear almost immediately after the injury. Special attention should be paid to the palatal surface in the gingival third of the crown.
- Reaction to sensibility tests. It is usually not possible to obtain reliable information from a young, frightened child. However, in the permanent dentition electrometric sensibility testing should be performed whenever possible. It gives important information about the neurovascular supply to the pulp, and provides a baseline value for comparison at follow‐up examination. The contralateral uninjured tooth or another comparable tooth serves as a control. The most reliable response is obtained when the electrode is placed upon the incisal edge. It is important to explain the purpose of the test and the type of reaction to be expected.
Radiographic examination
A detailed radiographic examination is mandatory in order to obtain an impression of the injury to the teeth, supporting tissues, the stage of root development and, in the case of primary tooth injuries, the relation to permanent successors (Figure 18.6). Before a radiographic examination is carried out, a clinical examination should establish the extent of the trauma region. This area is then radiographed; ideally, the injury site should be viewed from different angulations [6].
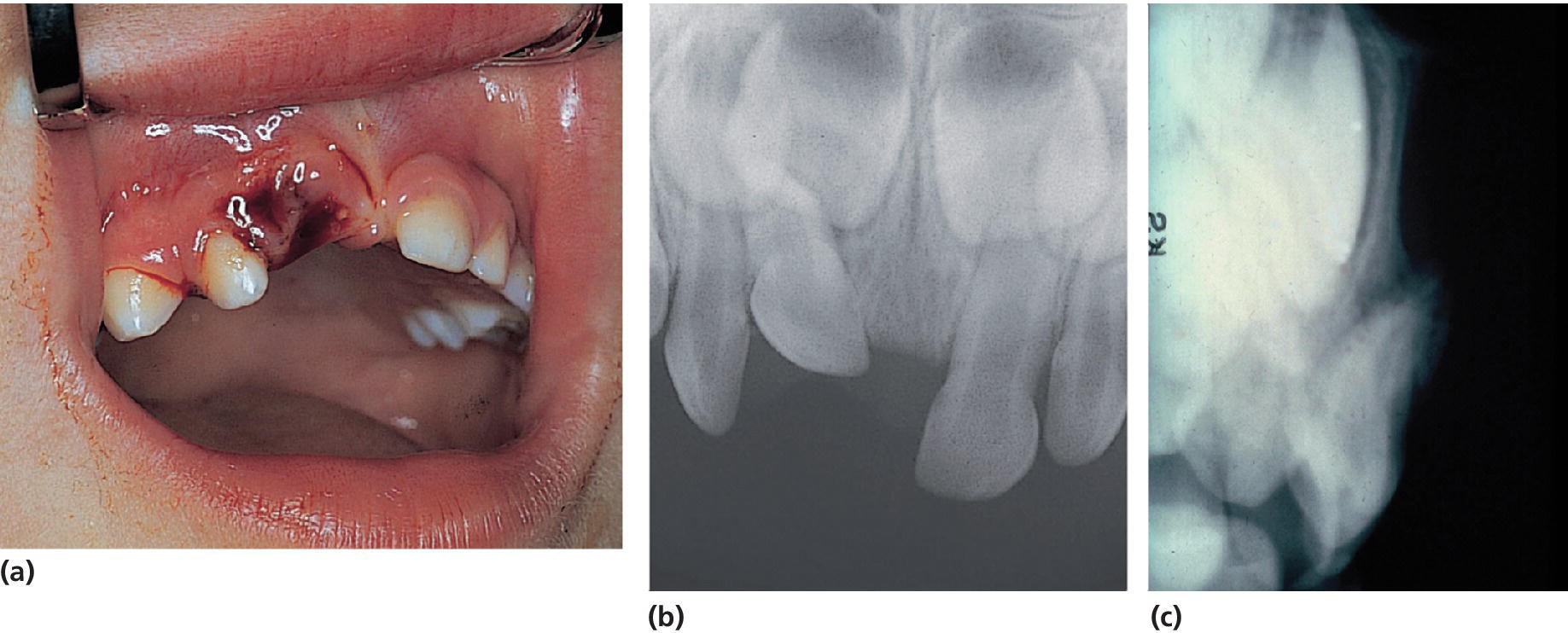
Figure 18.6 (a) Clinical condition immediately after severe intrusive luxation of the primary right central incisor. (b) The occlusal exposure shows foreshortening of the intruded tooth, indicating buccal displacement away from the permanent follicle. (c) This is evident in the lateral radiograph, since the apex of the intruded incisor is forced through the buccal bone plate.
Permanent teeth
For an injured anterior front with all incisors involved, four exposures should be taken (one occlusal and three bisecting angle exposures), where the central beam is directed interdentally between the incisors. This combination of radiographs results in each traumatized tooth being seen from different angulations, which increases the likelihood of diagnosing even minor dislocations (Figure 18.7).

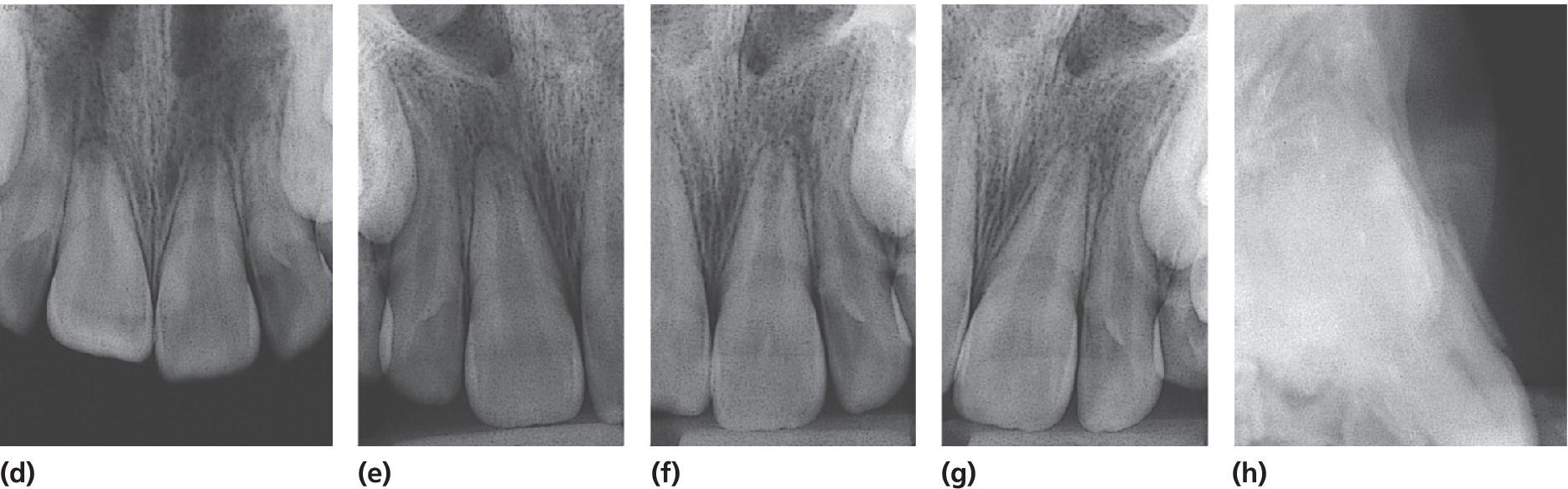
Figure 18.7 (a–c) Clinical appearance after lateral luxation of the right central incisor. (d–g) One occlusal and three periapical radiographs. Note that the occlusal exposure is optimal for showing the buccal displacement of the root. (h) The lateral radiograph illustrates where the fracture of the buccal bone plate has occurred (arrow).
In deep lip wounds a soft tissue radiograph is essential to diagnose embedded tooth fragments or other foreign bodies. A film is placed between the lips and the alveolar process, and the exposure time should be approximately 25% of a dental exposure time.
Primary teeth
A young child is often difficult to examine radiographically because of fear or lack of cooperation. However, with the parents’ help, it is usually possible to obtain a radiograph of the traumatized area (see also Chapter 8). In these instances an occlusal film held by the parents and a steep exposure angle should be used. This will normally show the position of the displaced tooth and its relation to the permanent successor. However, an extraoral lateral exposure may give additional information in case of suspicion of collision between the primary tooth and the permanent tooth germ.
Diagnosis
With combined information from the clinical and radiographic examination, a diagnosis is made and the injury is classified as a guide to the treatment required. In this chapter the classification recommended by the World Health Organization (WHO) will be used. The code numbers are according to the International Classification of Diseases [7].
Injuries to the hard dental tissues and the pulp
- Enamel infraction (S 02.50). An incomplete fracture (crack) of the enamel without loss of tooth substance.
- Enamel fracture (uncomplicated crown fracture) (S 02.50). A fracture with loss of tooth substance confined to the enamel.
- Enamel–dentin fracture (uncomplicated crown fracture) (S 02.51). A fracture with loss of tooth substance confined to enamel and dentin, but not involving the pulp.
- Complicated crown fracture (S 02.52). A fracture involving enamel and dentin, and exposing the pulp.
Injuries to the hard dental tissues, the pulp, and the alveolar process
- Crown–root fracture (S 02.54). A fracture involving enamel, dentin, and cementum. It may or may not expose the pulp (uncomplicated and complicated crown–root fracture).
- Root fracture (S 02.53). A fracture involving dentin, cementum, and the pulp. Root fractures can be further classified according to displacement of the coronal fragment and localization of the fracture.
- Fracture of the mandibular (S 02.60) or maxillary (S 02.40) alveolar socket wall. A fracture of the alveolar process that involves the alveolar socket.
- Fracture of the mandibular (S 02.60) or maxillary (S 02.40) alveolar process. A fracture of the alveolar process that may or may not involve the alveolar socket.
Injuries to the periodontal tissues
- Concussion (S 03.28). An injury to the tooth‐supporting structures without abnormal loosening or displacement of the tooth, but with marked reaction to percussion.
- Subluxation (S 03.28). An injury to the tooth‐supporting structures with abnormal loosening, but without displacement of the tooth.
- Extrusive luxation (S 03.21). Partial displacement of the tooth out of its socket.
- Lateral luxation (S 03.20). Displacement of the tooth in a direction other than axially. This is accompanied by comminution or fracture of the alveolar socket.
- Intrusive luxation (S 03.21). Displacement of the tooth into the alveolar bone. This is accompanied by comminution or fracture of the alveolar socket.
- Avulsion (exarticulation) (S 03.22). Complete displacement of the tooth out of its socket.
Injuries to gingiva or oral mucosa
- Laceration of gingiva or oral mucosa (S 01.50). A shallow or deep wound in the mucosa resulting from a tear; usually produced by a sharp object.
- Contusion of gingiva or oral mucosa (S 01.50). A bruise usually produced by impact with a blunt object and not accompanied by a break in the mucosa, usually causing submucosal hemorrhage.
- Abrasion of gingiva or oral mucosa (S 01.50). A superficial wound produced by rubbing or scraping of the mucosa, leaving a raw, bleeding surface.
The distribution of various dental diagnoses in the primary and permanent dentition is shown in Figures 18.8 and 18.9, respectively. In the permanent dentition uncomplicated crown fractures are very common [3]. In contrast, luxation injuries dominate in the primary dentition [8]. This is probably due to resilience of the alveolar bone in young children, favoring loosening or displacement rather than fractures of the hard dental tissues.
Figure 18.8 Percentage distribution of diagnoses for traumatized primary teeth.
Source: Heintz 1968 [25]. Reproduced with permission of Elsevier.

Figure 18.9 Distribution of 2019 traumatized permanent teeth according to diagnosis in 1275 children aged 7–18 years.
Source: Skaare & Jacobsen 2003 [3]. Reproduced with permission of John Wiley & Sons.
Immediate care: primary teeth
During its early development, the permanent incisor is located palatally and in close proximity to the apex of the primary incisor (Figure 18.10). Consequently, with injuries to primary teeth, the dentist must always be aware of possible damage to the underlying permanent teeth.
Figure 18.10 Schematic drawing illustrating developmental disturbance of permanent tooth bud at the age of 2 years. The crown of the primary incisor is displaced buccally, forcing the root into the crown of the developing permanent incisor.
A young child is often unable to cooperate, and the following procedure is suggested for clinical examination (Figure 18.11):
- The parent is seated on a chair with the child on his or her lap, facing the parent.
- The dentist, who is seated behind the child, receives and steadies the child’s head in the lap.
- The parent gently restrains the child’s arms and legs.
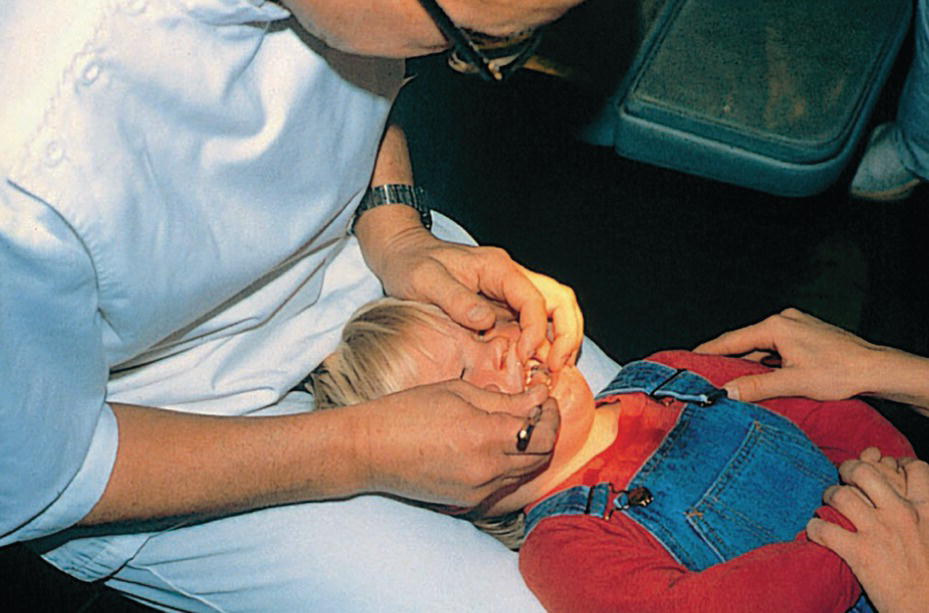
Figure 18.11 Procedure for examination of a young child’s mouth (see text).
In this way, a thorough examination of the oral structures can easily be done in a few minutes.
With the assistance of a parent or another adult, it is also possible to obtain radiographs of the traumatized area. However, active treatment such as splinting of loosened teeth or endodontic therapy may be extremely difficult. Therefore, in the majority of cases, the dentist has to decide whether the traumatized tooth is best treated by extraction, or whether it can be maintained without any extensive treatment.
A primary incisor should always be removed if its maintenance will jeopardize the developing permanent tooth bud, i.e., if the displaced primary tooth has invaded the follicle of the permanent successor [9]. If treatment is required in a young child, the use of conscious sedation should be considered (Chapter 9).
Enamel and enamel–dentin fracture
Most crown fractures consist of enamel or superficial enamel–dentin fractures. In both situations, slight grinding of sharp edges is sufficient. If the fracture is extensive, and the child cooperative, the tooth can be restored with glass‐ionomer cement or composite [9].
Complicated crown fracture
Normally, extraction is the treatment of choice. However, if full cooperation of the child can be achieved, the same procedure as outlined for permanent teeth can be followed [9].
Crown–root fracture
These cases involve fracture of enamel, dentin, and cementum. Frequently, the pulp is also exposed. Restorative treatment is extremely difficult and the tooth is best extracted [9].
Root fracture
If the coronal fragment is severely dislocated, extraction is the treatment of choice. No effort should be made to remove the apical fragment, as such intervention might damage the underlying permanent tooth. After removal of the coronal fragment, uncomplicated resorption of the apical fragment should be expected (Figure 18.12). Without evident displacement, the coronal fragment may show little mobility, and no immediate extraction is required. The tooth should be kept under observation. Sometimes necrosis develops in the coronal fragment, whereas the apical portion nearly always remains vital. In these cases the coronal fragment only should be extracted [9].
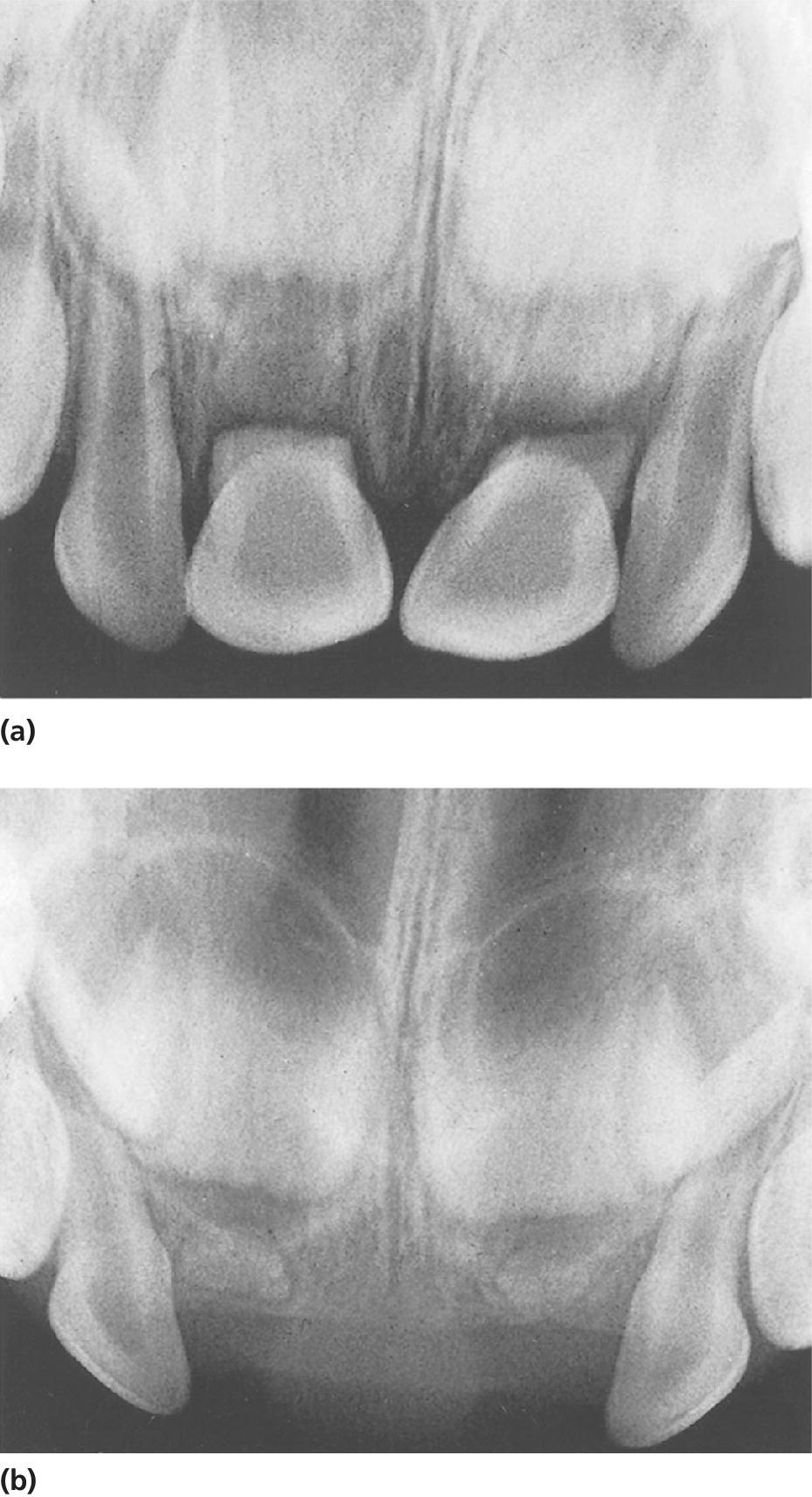
Figure 18.12 (a) Fractured roots of both central incisors with dislocation of the coronal fragments. (b) Normal resorption of the apical fragments after removal of the coronal fragments.
Luxation injuries
These injuries dominate in the primary dentition. Most often, the patients also have extensive soft tissue damage such as swollen lips, lacerations, and hemorrhage of the oral mucosa and gingiva (Figure 18.13). The parents are instructed to clean the traumatized area gently with 0.1% chlorhexidine solution, using cotton swabs (twice daily for a week). Normally the soft tissue heals quickly. Swelling will usually subside within a week.

Figure 18.13 Severe soft tissue damage with extensive hemorrhage. Both central incisors and the right lateral incisor are extruded and extremely mobile.
Concussion
Most concussions are not seen by the dentist at the time of the accident. The parents may see no need to seek dental treatment, or they may not be aware of the injury until tooth discoloration appears.
Subluxation
The parents are advised to keep the traumatized area as clean as possible, and to feed the child on a soft diet for a few days [9]. Mobility should diminish within 1–2 weeks.
Extrusive luxation
An extruded tooth may be repositioned by digital pressure. However, if the tooth is severely displaced and shows considerable mobility, the tooth is best treated by immediate extraction [9].
Lateral luxation
- Palatal displacement of the crown is most common. This implies that the apex is forced in a buccal direction and thus away from the permanent tooth germ. If there is no interference with the occlusion these teeth can be left untreated. Over a period of 1–2 months, tongue pressure will usually reposition the tooth (Figure 18.14).
- In the case of minor occlusal interference, slight grinding is indicated. When there is more severe occlusal interference, the tooth can be gently repositioned by combined labial and palatal pressure after the use of local anesthesia or the tooth may be extracted [9].
- Buccal displacement of the crown (Figures 18.10 and 18.15). The root will be displaced palatally in the direction of the permanent tooth bud. In case of collision with the permanent tooth germ, extraction is the treatment of choice [9].

Figure 18.14 (a) Severe palatal luxation of the right central incisor. No treatment other than observation was performed. (b) Two months later, the tooth is back in normal position due to tongue pressure.
Figure 18.15 Clinical condition immediately after buccal displacement of the left central incisor in an 8‐month‐old girl.
Intrusive luxation
An intruded tooth often shows severe displacement. Sometimes it will be completely intruded into the alveolar process and mistakenly assumed to be lost, until a radiograph shows the intruded position (Figure 18.16). With all intrusions, it is essential to clarify whether the root is forced in a palatal or buccal direction. The diagnosis should be based on a combined clinical and radiographic examination.


Figure 18.16 (a) Clinical examination after trauma of an 18‐month‐old child. The parents assumed that the right central incisor was lost. (b) The radiograph reveals severe intrusive luxation. Additional radiographs should be taken to disclose the exact direction of the intrusion (see Figure 18.6).
Clinical examination
Due to a buccal curve of the apex, the primary root tends to be displaced through the buccal bone plate. It is advisable to palpate the buccal sulcus. If part of the crown is visible, the tooth crown axes will also indicate the direction.
Radiographic examination
A foreshortened appearance of the intruded tooth implies buccal displacement of the root and thus away from the permanent tooth germ, whereas an elongated image suggests palatal displacement towards the permanent successor (Figure 18.6).
Treatment
In most cases the root will be displaced in a buccal direction and the primary tooth can be left to re‐erupt spontaneously [9]. The parents are instructed to clean the traumatized area with 0.1% chlorhexidine solution for a week. During the re‐eruption phase, there is a risk of infection, and the patient should therefore be seen for follow‐up a week after the injury. Signs of infection include swelling, spontaneous bleeding, and abscess formation. There may also be a rise in body temperature. In these cases, the traumatized tooth must be removed and antibiotic therapy instituted. Without signs of infection, re‐eruption will generally take place within 2–6 months (Figure 18.17). If re‐eruption fails to occur, ankylosis should be suspected. If the ankylosed tooth interferes with eruption of the permanent successor, it must be removed [9].
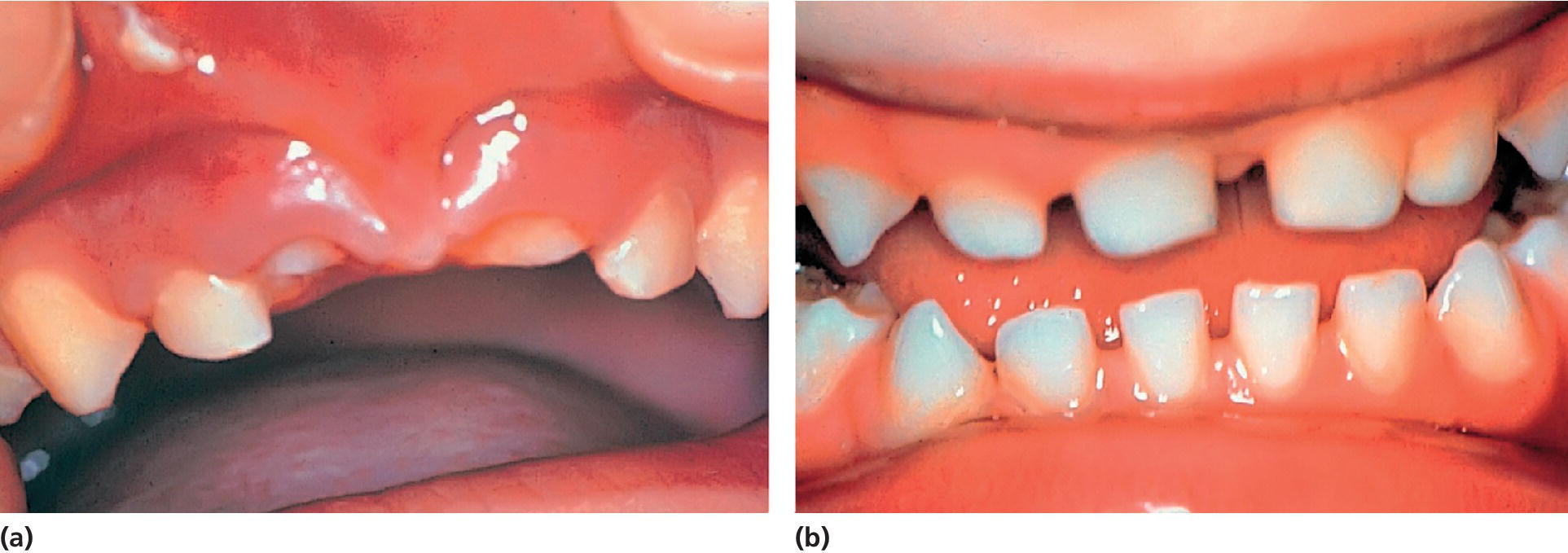
Figure 18.17 (a) Condition immediately after intrusive luxation of both central incisors. (b) Re‐eruption is evident 6 months later.
If the primary root is displaced palatally, into the follicle of the developing tooth germ, extraction is recommended [9]. Extraction is performed to minimize the risk of bacterial invasion into the follicle which could cause further damage to the developing permanent tooth. Elevators should never be used to luxate the intruded incisors. Forceps should be the only instrument employed for this purpose. The intruded tooth should be grasped mesiodistally and lifted out of its socket in an axial direction. Thereafter digital pressure should be applied to the buccal and palatal aspects of the socket to reposition the displaced bone plates.
Avulsion
A radiographic examination is essential to ensure that the missing tooth is not intruded (Figure 18.16). Replantation is contraindicated, as pulp necrosis is a frequent complication. Moreover, there is a risk of further injury to the permanent tooth germ by the replantation procedure, whereby the coagulum from the socket can be forced into the follicle [9].
Immediate care: permanent teeth
The most common age of trauma to the permanent dentition is between 8 and 10 years (Figure 18.3). This implies that a traumatized tooth often has an open apical foramen, a wide root canal, and fragile dentinal walls in the cervical area. If pulp necrosis develops, no further dentin apposition occurs, and there is a considerable risk of spontaneous root fracture cervically with subsequent loss of the injured tooth (see Chapter 19). Consequently, the primary concern is to maintain pulp vitality to allow continued root formation including physiologic dentin apposition in the critical cervical area. The following recommendations for treatment of acute traumatic injuries is based on the treatment guidelines developed by the International Association of Dental Traumatology [10,11].
Crown fractures
It is most important to diagnose concomitant periodontal injuries, since the risk of complications to crown fractures is significantly increased with an additional luxation injury (Figures 18.18 and 18.19) [12–14].
- Enamel infraction. Infractions are incomplete fractures without loss of tooth substance. The fracture line usually stops at the enamel–dentin junction. Infraction lines are best seen when the light beam is directed parallel to the long axis of the tooth. In case of concomitant luxation injury sealing of the infraction line with resin is recommended.
- Enamel fracture. Minimal tooth substance is lost, and restoration is normally not needed. Often, a slight contouring of the fractured angle will provide an esthetically satisfactory result.
- Enamel–dentin fracture. Some typical examples are shown in Figures 18.18 and 18.19. Crown fractures involving dentin result in exposure of dentinal tubules to the oral environment. If the dentin is left unprotected, bacteria or bacterial toxins may penetrate the tubules, resulting in pulpal inflammation. Although the inflammation may be reversible, pulp necrosis is also a possible outcome. The pulp should therefore be protected against external irritants as quickly as possible, and the tooth crown restored by one of the following restorations.
- Temporary crown restoration. There are situations in which a temporary restoration should be preferred over a period of time. One example is when the child’s general health condition is also affected. A temporary restoration may then be the most practical solution until the child has recovered. Another example is when an associated luxation injury requires immediate fixation, as shown in Figure 18.19. The procedure is to cover exposed dentin with calcium hydroxide. After etching, rinsing, and drying of the enamel, a layer of light‐curing composite resin is applied. Alternatively, the whole fracture surface can be covered with a glass ionomer cement “bandage.”
- Reattachment of a crown fragment. A tooth fragment from a traumatized incisor may be reattached. Dehydration of the fragment will decrease the bonding strength and lead to an inferior cosmetic result and must therefore be avoided. A dry fragment can be rehydrated before bonding. If a temporary restoration is indicated for a period of time, the fragment can be stored in physiologic saline in the delay period. The broken fragment can then be bonded to the tooth with a flowable composite (Figure 18.20) [15].
- Composite crown build‐up. If the fractured fragment is not found, or if it is too small to be reattached, a composite build‐up has been shown to be successful both functionally and esthetically in the young patient (Figure 18.21). The treatment procedure is summarized in Box 18.3.
- Complicated crown fracture. This fracture involves enamel and dentin, with exposure of the pulp (Figure 18.22). The overall aim of the treatment is preservation of a vital noninflamed pulp. The pulp must be sealed from bacteria so that it is not infected during the period of repair. In most cases this can be achieved by either pulp capping or partial pulpotomy. The indications and techniques for these two treatment procedures are presented in Boxes 18.4 and 18.5 (see also Chapters 16 and 17).
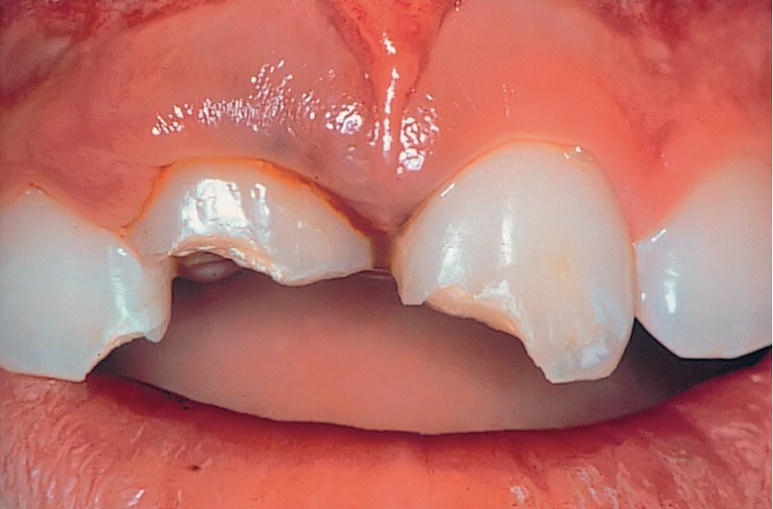
Figure 18.18 Uncomplicated crown fracture involving either mesial corners or entire incisal edge. The gingival bleeding indicates that intrusive luxation has also occurred in the right central incisor.
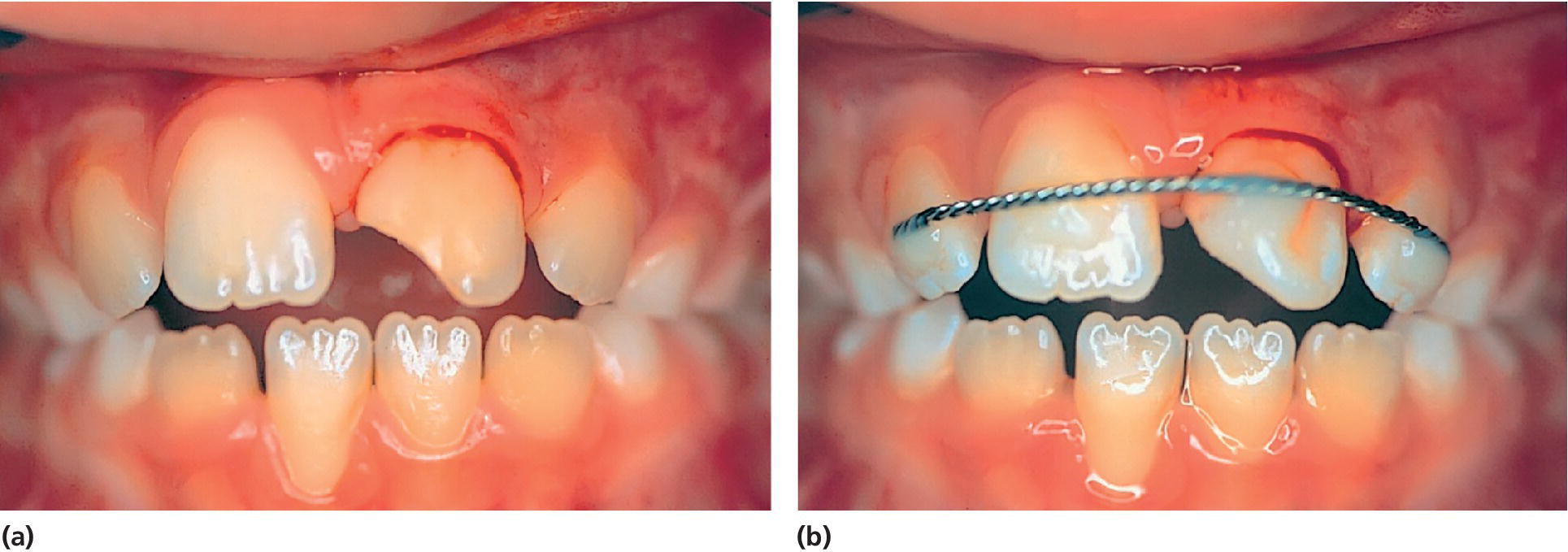
Figure 18.19 (a) Both subluxation and uncomplicated crown fracture have occurred in the left central incisor. (b) The tooth is stabilized with a splint, and a temporary crown restoration is applied.
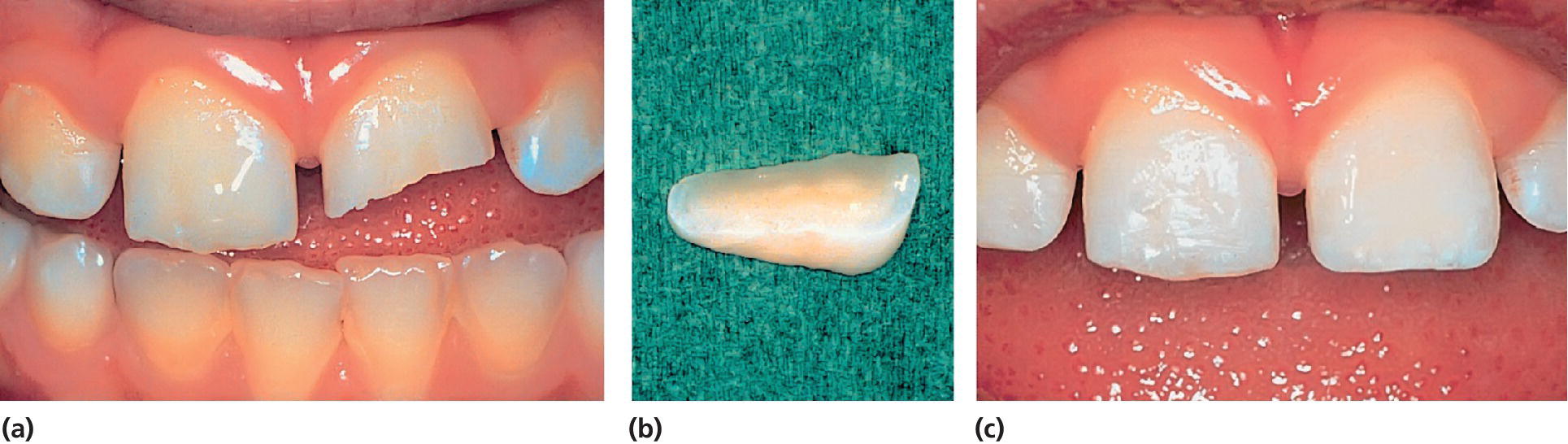
Figure 18.20 (a) Enamel–dentin fracture of the left central incisor in an 8‐year‐old boy. (b) The fractured crown fragment. (c) Condition immediately after reattachment of the fragment.
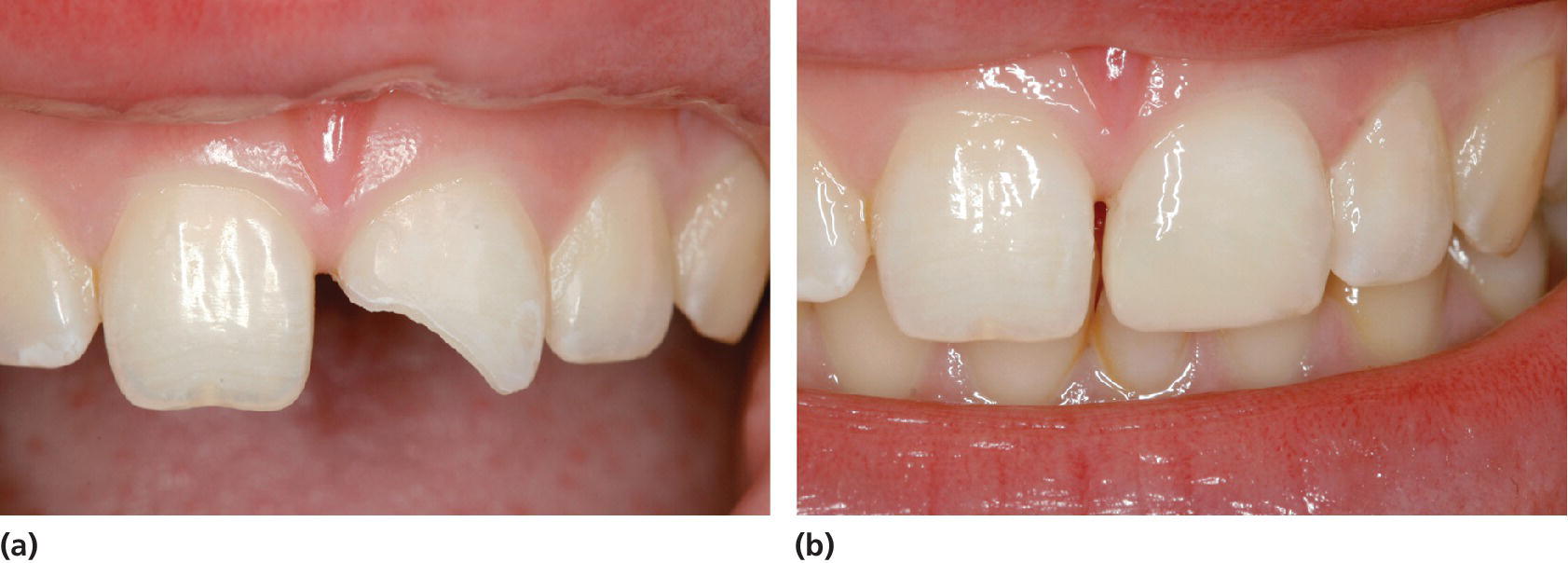
Figure 18.21 (a) A 12‐year‐old girl with enamel–dentin fracture of the left central incisor. (b) Condition shortly after the composite crown build‐up.
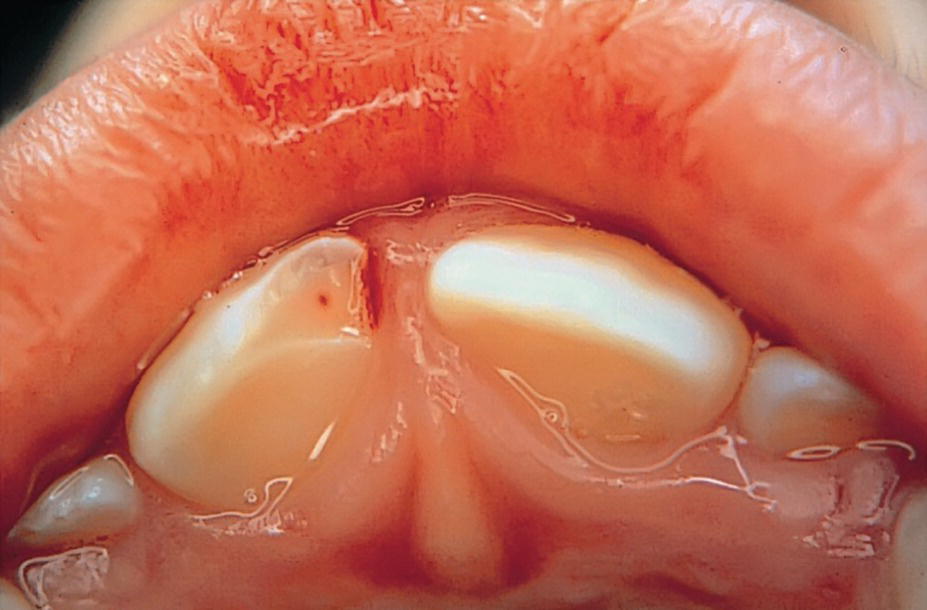
Figure 18.22 Right central incisor with a small pulpal exposure, but with loosening and marked tenderness to percussion. Partial pulpotomy was decided to be the treatment of choice.
Both capping and partial pulpotomy have shown favorable prognoses. However, if in doubt as to the treatment of choice, partial pulpotomy should be performed, since it results in better wound control and ensures a bacteria‐tight seal of the pulp cavity [16,17].
Crown–root fracture
These injuries involve enamel, dentin, and cementum, and are often complicated by pulpal exposures. The fracture is sometimes vertical with the fracture line in the same direction as the long axis of the root. A more typical finding is an oblique course of the fracture line, as shown in Figure 18.23. The fracture is then usually located a few millimeters incisally to the gingival margin on the buccal surface. Palatally, the fracture is found to extend below the cemento–enamel junction.
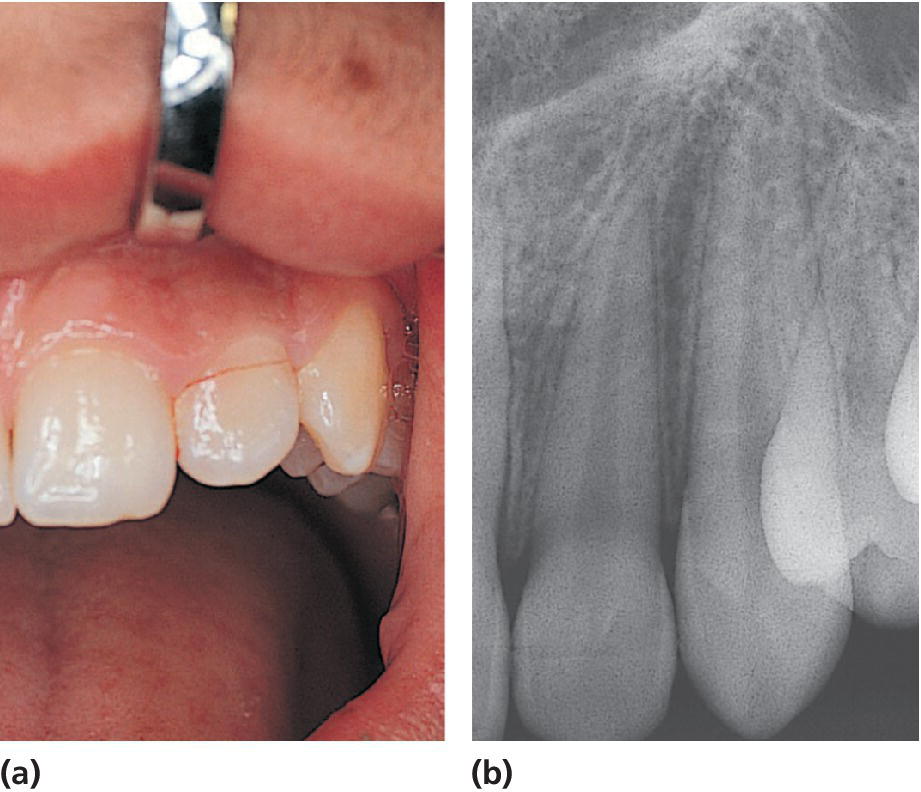
Figure 18.23 Crown–root fracture of the left lateral incisor. (a) Buccally, the fracture line is located close to the gingival margin. (b) The radiograph only demonstrates the position of the buccal part of the fracture, whereas the palatal part cannot be seen.
In some cases, loose fragments can be stabilized by bonding as a temporary measure. However, the prognosis is rather doubtful. In fractures communicating with the oral cavity, periodontal breakdown is most likely to occur. Thus, with most crown–root fractures, the treatment is to remove the loose fragment or fragments. Any pulpal involvement must be determined. If the pulp is exposed, treatment should follow recommendations given in Box 18.4 and 18.5. Further treatment depends on how deeply the fracture extends into the root surface. The goal is to create a situation where the tooth can be restored after removal of the coronal fragment. If the root portion is of sufficient length, one of the following procedures is suggested:
- Fragment removal and gingival reattachment. The coronal fragment is removed and the gingiva is allowed to reattach to the exposed dentin (i.e., by formation of a long junctional epithelium). After some weeks, the tooth can be restored above the gingival level.
- Fragment removal and surgical exposure of subgingival fracture. After removal of the coronal fragment, the subgingival fracture is exposed by gingivectomy and/or osteotomy if the fracture extends below the alveolar crest. After gingival healing, the tooth is restored with a post‐retained crown. While this procedure might appear to be most direct, long‐term esthetic success may be compromised due to an accumulation of granulation tissue in the gingival sulcus palatally, which can lead to buccal migration of the restored tooth.
- Fragment removal and orthodontic extrusion. The coronal fragment is initially stabilized to adjacent teeth. Pulp extirpation and canal obturation with guttapercha and sealer can be performed at a later appointment. The coronal fragment is then removed and the tooth extruded over a 4–6‐week period. The tooth should be slightly overextruded (0.5 mm), due to risk of relapse [18]. A buccal gingivectomy is performed, whereafter the tooth can be restored.
- Fragment removal and surgical extrusion. The coronal fragment is removed, then the root is loosened with elevators and forceps and repositioned in a more incisal position, so that the entire fracture surface is exposed above the gingival level [19]. The root fragment is then stabilized with sutures or a nonrigid splint. The pulp is extirpated, a guttapercha point is placed loosely in the canal to later facilitate canal location, and the entrance to the root canal is sealed with a temporary cement. After 4 weeks, when the tooth is stabilized in its socket, endodontic treatment is completed; and after a further 4–5 weeks, the tooth can be restored.
Root fracture
A root fracture involves dentin, cementum, and the pulp. The coronal fragment may be extruded or displaced in a palatal direction (Figure 18.24). Treatment consists of immediate repositioning of the coronal fragment and stabilization with a flexible splint (Box 18.6). Fixation should also be carried out in cases without dislocation, as close contact between the fragments is considered essential during the period of initial repair [20–22].
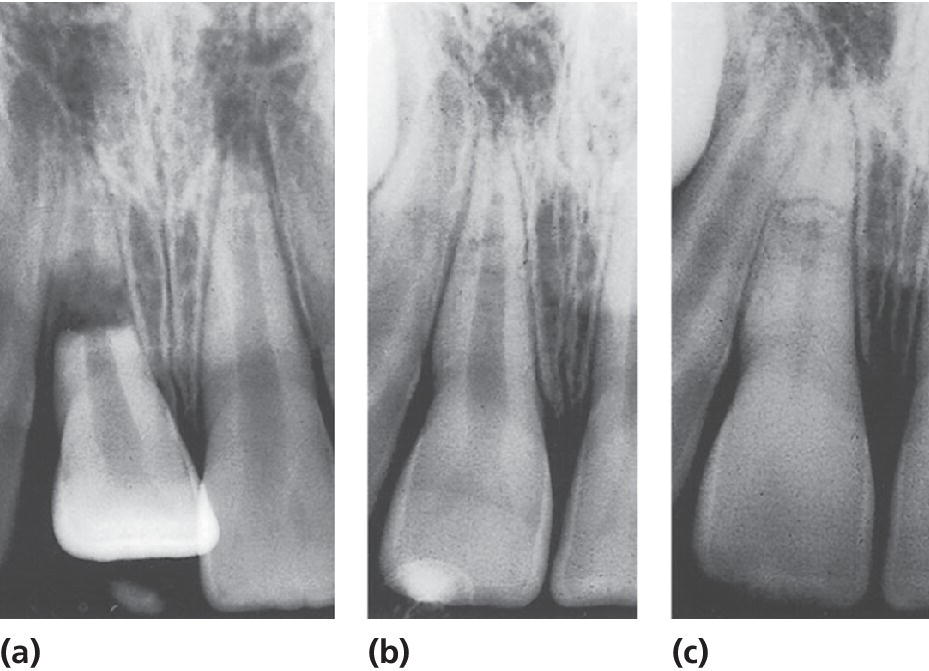
Figure 18.24 (a) Root fracture in the right central incisor with severe dislocation of the coronal fragment. (b) Optimal repositioning performed within 1 hour. (c) Condition 1 year later, with normal findings in the fracture area and partial pulp canal obliteration.
Splinting technique. An acceptable splint should be easy to construct. It should be flexible and neither add further trauma to the periodontal tissues nor interfere with occlusion. The splint should allow sensibility testing and access to the root canal if endodontic treatment is required. Two simple methods based on the etch technique and fulfilling the above‐mentioned requirements are presented in Box 18.7 and Figures 18.19, 18.25, and 18.28.
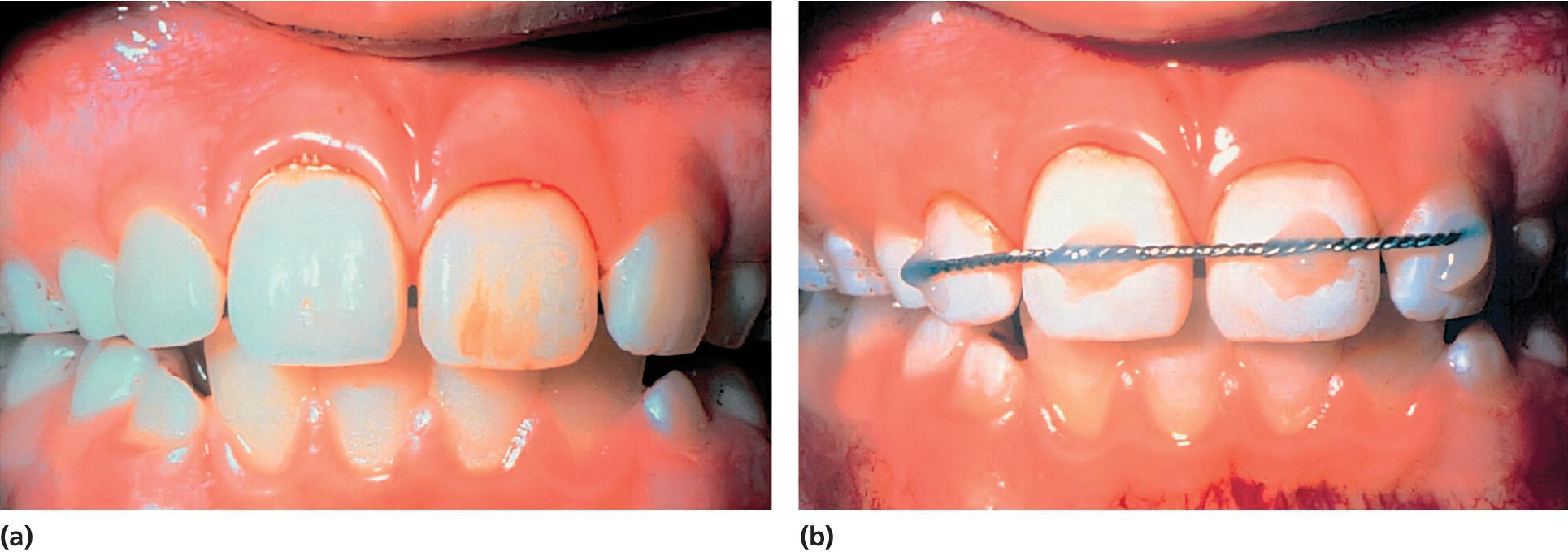
Figure 18.25 (a) Subluxation of both central incisors with mobility in both the horizontal and vertical directions. (b) The teeth are stabilized with an orthodontic twisted wire, resin material, and the acid‐etch technique (see Box 18.7).
Concussion
These lesions are defined as injuries to the periodontal ligament without displacement or loosening of the tooth. Marked tenderness to percussion is the characteristic finding. No immediate treatment is required, but follow‐up examination is important to verify that no associated pulp injury has occurred.
Subluxation
The involved teeth show varying degrees of mobility and there may be bleeding from the gingival margin.
In the case of mobility in both a horizontal and a vertical direction, the tooth may be splinted for 1–2 weeks for the comfort of the patient (Figure 18.25). Should the tooth be only slightly loosened, it is sufficient to recommend a soft diet for 1–2 weeks.
Extrusive luxation
The injured tooth is partially and axially displaced out of the alveolar socket. It appears elongated and is extremely mobile. There is also bleeding from the gingival sulcus (Figure 18.26).
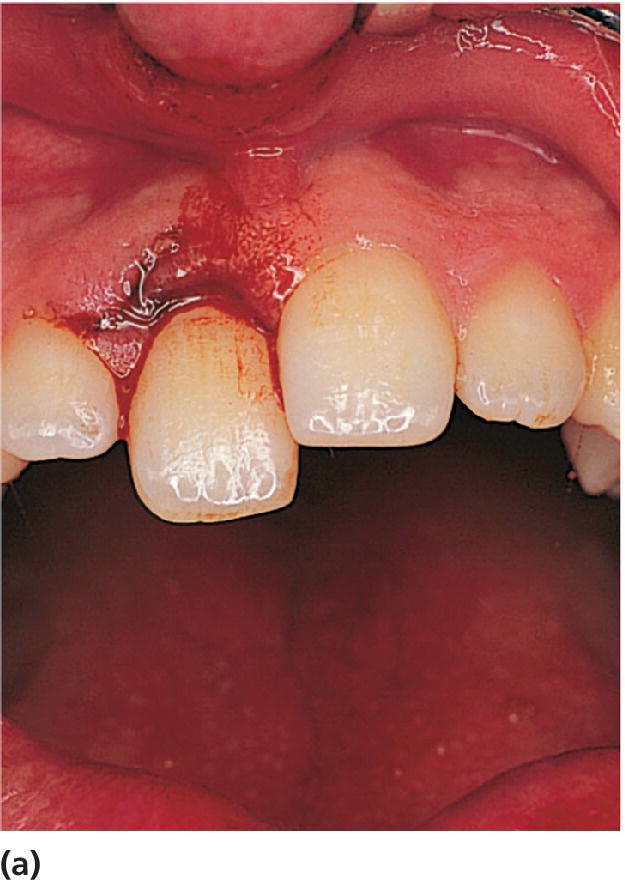


Figure 18.26 (a) Extrusive luxation of the right central incisor. The tooth appears elongated and is also very mobile. (b) The radiograph shows increased periodontal width apically. (c) A radiograph taken after repositioning illustrates optimal position of the tooth in its socket.
The treatment principle implies immediate repositioning and fixation (Box 18.8). Repositioning will facilitate repair of the periodontal ligament. Optimal repositioning is also essential to allow pulp revascularization and continued root development of an immature tooth.
Lateral luxation
Lateral luxation implies displacement in a palatal, buccal, mesial, or distal direction accompanied by comminution or fracture of the alveolar socket. Most often, a palatal luxation occurs (Figure 18.27). The apex is then displaced in the opposite direction and usually forced through the buccal bone. Repositioning requires disengagement of the apex from its bony lock (Box 18.9).
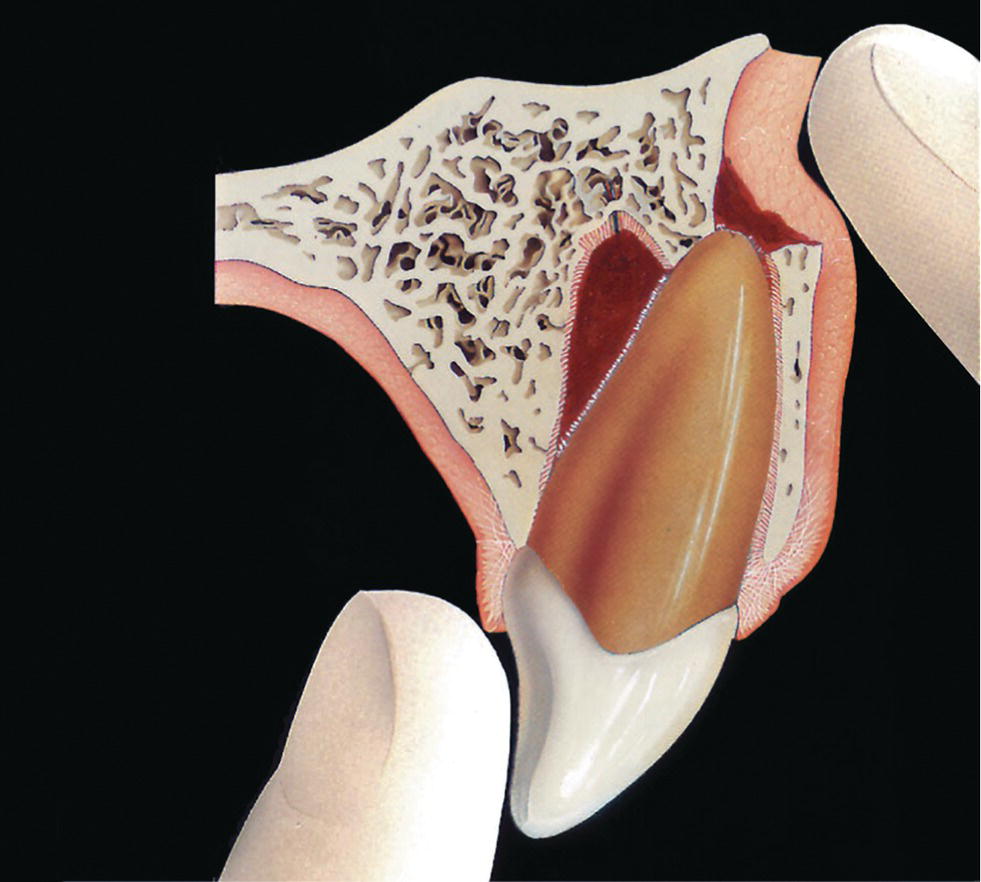
Figure 18.27 Palatal luxation of the crown. The apex is forced through the buccal bone. Repositioning requires disengagement of the tooth from its bony lock. Apply firm digital pressure in an incisal direction, and move the tooth back through the fenestration into the socket. Thereafter, axial pressure will bring the tooth back to its original position.

Figure 18.28 Resin splint (Protemp®) applied after surgical repositioning of severely intruded left central incisor.
Intrusive luxation
Intrusion is the most severe type of luxation and appears to be most frequent in the 6–12 years age group [32]. The tooth is forced axially into the socket, resulting in damage to the alveolar bone, the periodontal ligament, the cementum, and the pulp (Figure 18.29).

Figure 18.29 Complete intrusion of the left central incisor in a 9‐year‐old boy. (a) The incisal edge is barely visible 5 days after the accident. It was decided to await re‐eruption. (b) Partial re‐eruption is evident a month later. (c) Complete re‐eruption 10 months after trauma. (Delayed eruption of the right incisor is due to a supernumerary tooth.)
In the young permanent dentition with incisors under eruption, the diagnosis is sometimes difficult (Figure 18.18). In these cases a high metallic percussion sound indicates intrusive luxation with the tooth locked in bone.
Different treatment methods are suggested for intruded teeth, e.g., spontaneous re‐eruption, orthodontic extrusion, or surgical repositioning. The recommended treatment depends on the stage of root development and the degree of intrusion.
Guidelines for the treatment are suggested in Box 18.10.
Avulsion
The alveolar bone, cementum, periodontal ligament, gingiva, and the pulp are all damaged when a tooth is completely displaced out of its socket.
Replantation. When avulsion occurs, replantation is the treatment of choice. Due to a frequent occurrence of external root resorption, it is not possible to guarantee long‐term retention of a replanted tooth. However, even when resorption does occur, the replanted tooth can be maintained for years, serving as an ideal space maintainer (Figure 18.30). Moreover, in the young permanent dentition, a replanted tooth that does not go into ankylosis will prevent horizontal and vertical bone loss and facilitate later alternative treatment, e.g., orthodontic closure, premolar transplantation, or dental implants.
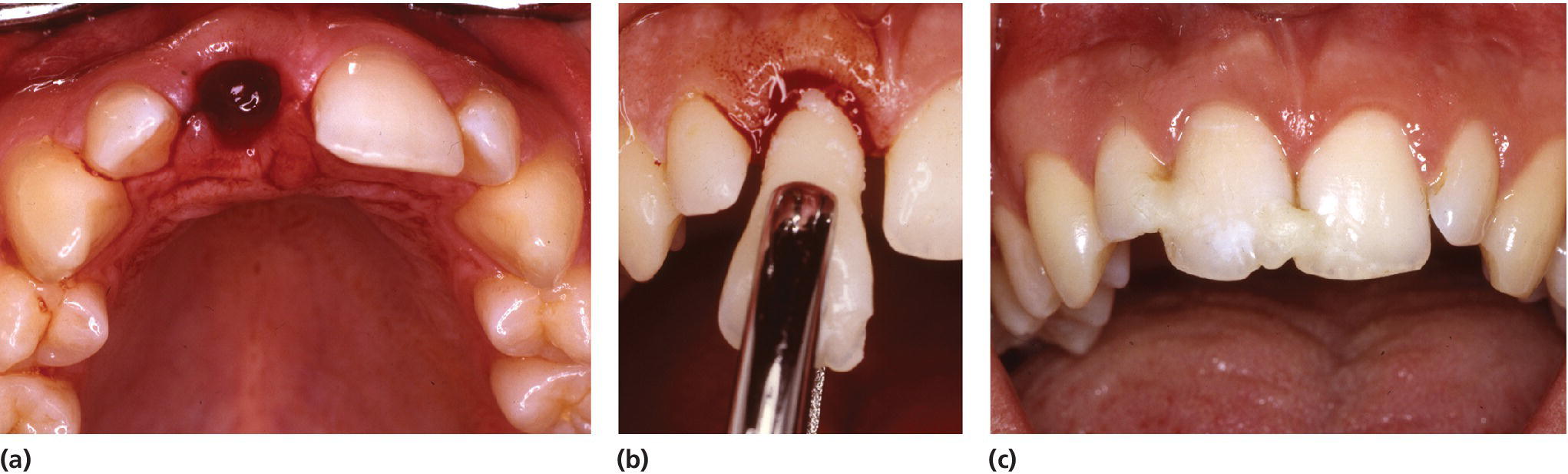
Figure 18.30 (a) A 10‐year‐old girl with avulsion of the left central incisor after a skiing accident. The tooth was found in the snow 4 hours later. (b, c) The avulsed tooth is replaced in the socket with gentle finger pressure and a splint is applied.
Courtesy of S.K. Sundnes.
A number of factors are associated with complications seen after replantation. The most critical factor related to periodontal healing is the extraoral time. A Danish study reported that teeth replanted within 5 minutes had the best prognosis [24]. Consequently, replantation should preferably be done at the site of injury in order to minimize the extraoral period. If immediate replantation is impossible, it is of utmost importance that the periodontal ligament attached to the root is kept moist. Studies have demonstrated that the number of viable cells in the periodontal ligament declines very rapidly with an increase in the drying time. An avulsed tooth should be stored in a physiologic storage medium until it can be replanted. The following storage media have been shown to permit both periodontal and pulpal healing: milk, physiologic saline, tissue culture media, and saliva. However, at the site of injury, only saliva is always available. Recommendations for the treatment of avulsed teeth are presented in Boxes 18.11–18.13.
Should endodontic treatment be performed? Pulp survival is not likely in case of closed apical foramen, and endodontic treatment should always be started after 7–10 days and prior to removal of the splint. The canal may be filled temporarily with calcium hydroxide paste.
In teeth with a wide‐open apical foramen, revascularization of the pulp may occur and endodontic treatment is postponed. However, these teeth must be followed closely. If definite signs of pulp necrosis are observed such as apical radiolucency and/or external infection‐related resorption, endodontic treatment should be started immediately. It is recommended that a replanted tooth with incomplete root formation is examined radiographically every second week until pulp necrosis is confirmed or continued root formation is evident (Figure 18.31).
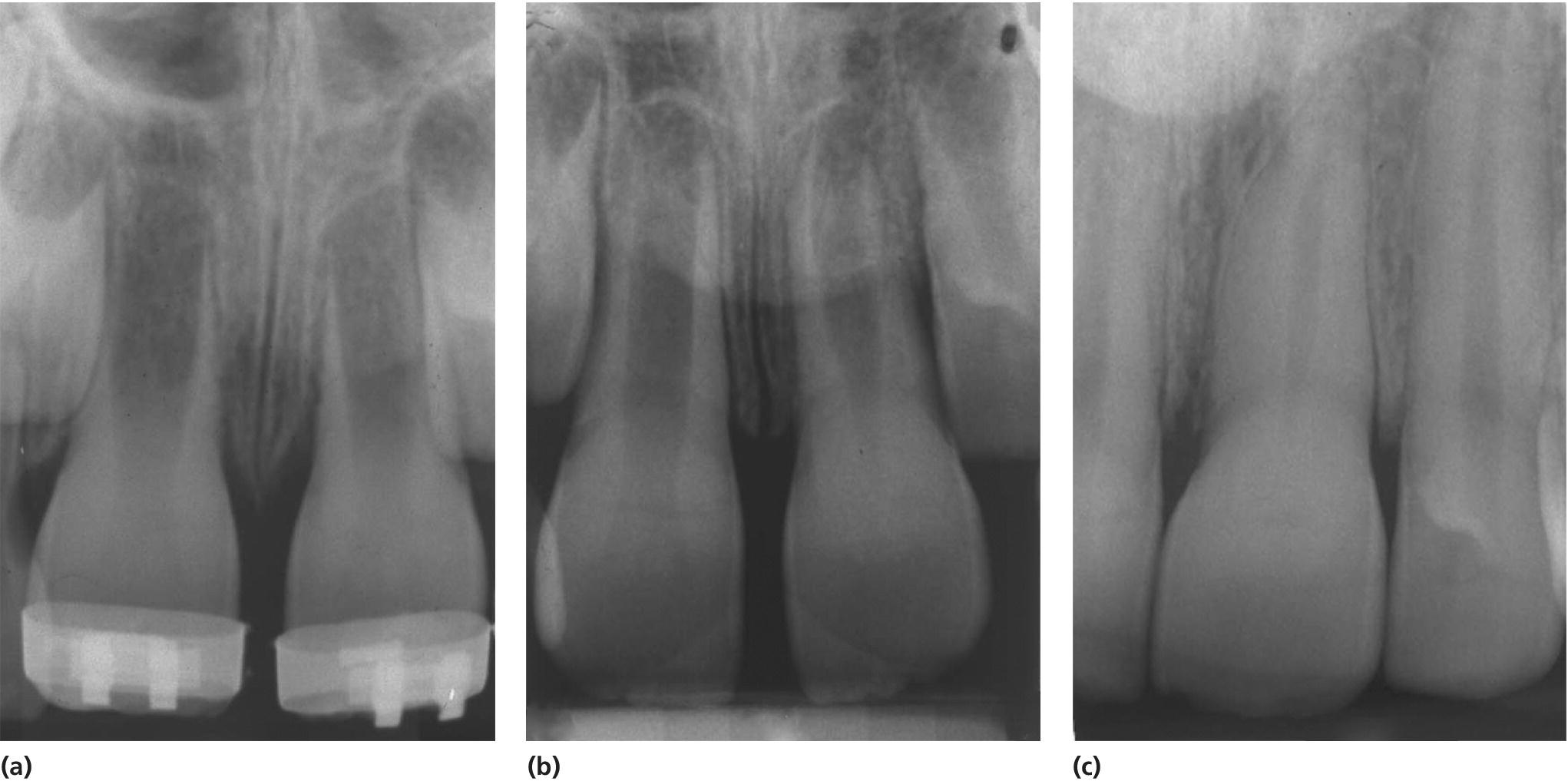
Figure 18.31 Successful replantation of the left central incisor in a 7‐year‐old boy. The avulsed tooth was immediately pushed back in place by the boy’s father. (a, b) Six days and 1 year after replantation, respectively. (c) Four years after the accident with completed root formation and almost total pulp canal obliteration. Note also obliteration in the right central incisor after a subluxation injury.
Courtesy of S.K. Sundnes.
Injuries to the alveolar process
This trauma entity is defined as a fracture of the alveolar process, which may or may not involve the alveolar socket. The typical clinical appearance is where a segment containing one or more teeth is displaced axially or laterally, usually resulting in occlusal disturbance. When mobility testing is performed, the entire fragment is found to be mobile. Gingival lacerations are frequent. Radiographically, a fracture can usually be seen, depending on the angle of the central radiographic beam. The horizontal part of the fracture line may be found in all locations, ranging from the cervical to the apical or periapical region. A differential diagnosis must be made with root fracture. In the case of a root fracture, change in the angulation of the central beam will not alter the fracture position on the root surface. However, in the case of an alveolar fracture, the fracture line will move up or down in relation to the root surface according to the horizontal angulation. The bone fracture may disrupt vascular supply to the teeth, which can result in pulp necrosis. Due to the frequent concomitant luxation injury and damage to the periodontal ligament, progressive root resorption may occur. Furthermore, if the fracture is located next to a developing tooth germ, then the tooth formation may be affected. The treatment principles comprise repositioning and immobilization of the displaced bone‐tooth fragment and monitoring of pulp vitality. Using infiltration or, preferably, a regional block anesthesia, the fragment is repositioned. As with lateral luxation, it is sometimes necessary to disengage the apices of the involved teeth from a bony lock. In the permanent dentition the fractured segment is splinted with a semi‐rigid splint for 4 weeks.
Generally, no measures are taken to stabilize a mobile fragment in the primary dentition, due to lack of sufficient teeth for the splinting procedure. After repositioning of the displaced fragments, the parents are advised to feed the child on a soft diet during the first weeks after the injury. The parents are also instructed to wash the traumatized area twice daily with 0.1% chlorhexidine solution.
Injuries to the gingiva and the oral mucosa
Soft tissue lesions must be adequately treated and recalled for healing control. Minor lacerations of the mucosa, the lip or the tongue should be sutured after careful debridement and cleansing of foreign bodies [5]. With gingival lacerations it is necessary to achieve good tissue positioning to ensure healing. Mouthrinsing or local treatment with 0.1% chlorhexidine solution is recommended to decrease the risk of infection during wound healing.
It is emphasized that if the wound has been contaminated with soil, prophylactic vaccination against tetanus should be administered as soon as possible.
Submucosal hematomas in the vestibular region or the floor of the mouth may indicate a jaw fracture, and careful radiographic examination is indicated.
Patient instruction after dental trauma
Good healing following an injury to the teeth and oral tissues depends, in part, on good oral hygiene. Brushing with a soft brush and rinsing with chlorhexidine 0.1 % twice a day for one week is beneficial to prevent accumulation of plaque and debris. Soft diet is recommended in the initial healing phase for patients with luxation injuries.
Prevention of traumatic injuries
The causes of orofacial injuries in children vary considerably, and there is no easy way to prevent the majority of these injuries. However, although sports are the cause of relatively few orofacial injuries, these are often severe and involve a greater number of teeth than other injuries.
Contact sports, such as ice hockey, football, handball, soccer, and basketball, with their high risk of collisions at high speed, are especially prone to resulting in dental and other injuries (Figure 18.32) [25–27].

Figure 18.32 Frequency of dental and other sports injuries per 10,000 people from 1981 to 1983 in Norway.
Source: Nysether 1987 [27]. Reproduced with permission of Elsevier.
Use of mouthguards
The evidence for the effect of mouthguards for all types of contact sports is incomplete. However, it is apparent that a correctly made mouthguard can reduce both the frequency and the severity of the injuries in many instances. Thus, the use of mouthguards in ice hockey in Canada has reduced the annual rate of dental injuries from 8.3% to 1.2% [28]. A North American study also reported a dramatic decrease in the frequency of orofacial injuries in basketball players using mouthguards [26].
Types of mouthguards include the following:
- Mouth‐formed protectors. Varieties are fitted from a manufactured kit consisting of a fairly rigid outer shell and a soft resilient heat‐cured or self‐cured lining. These protectors have the advantage of a good fit, while still being quite inexpensive.
- Custom‐made protectors are individually processed by a dentist or dental technician on plaster study models of the athlete’s dental arches. These protectors, while significantly more expensive than stock or mouth‐formed protectors, have been found to be acceptable and comfortable for most athletes.
- Stock variety protectors are of latex rubber or polyvinyl chloride, usually made in three sizes, and are supposed to be universally fitting; the advantage being their low cost. However, they have been found to impede both speech and respiration, as they can only be kept in place by occlusion. There is no evidence that they can redistribute forces of impact.
Face masks
Face masks are used in ice hockey. This device has been found to be very effective in protecting players from orofacial injuries and is now mandatory in organized ice hockey in many countries.
Information for the public on dental trauma
Tooth fractures, luxations, and avulsions in the permanent dentition can have an improved outcome if the public are well informed about appropriate first‐aid measures. Often an avulsed permanent tooth can be saved if children, parents, school teachers, and so on have knowledge of first aid for dental injuries.
First aid in the case of trauma to primary teeth
- In the case of bleeding from soft tissue injuries, stop the bleeding by compressing the injured area with gauze or cotton wool for 5 minutes.
- Seek emergency treatment.
- It is not recommended to replant avulsed primary teeth.
First aid in the case of trauma to permanent teeth
Crown fracture
- Find the tooth fragment and place it in a glass of water or milk.
- Seek dental treatment.
Avulsion
- Find the tooth and pick it up by the crown.
- If the tooth is dirty, wash it briefly (10 seconds) under cold running water and put it back into the tooth socket.
- The patient should be instructed to keep the tooth in position by gently pressing with gauze or a handkerchief. If this is not possible then the tooth should be stored in saliva (in the mouth between the teeth and the cheek or in spit in a cup), milk or saline. Avoid storage in water.
- Seek emergency dental treatment immediately.
Dental Trauma Guide
The Dental Trauma Guide is a website (dentaltraumaguide.org) available to all dentists. It has been developed by Dr Jens Ove Andreasen and his research team at the Copenhagen University Hospital, Rigshospitalet, in collaboration with the International Association of Dental Traumatology (IADT). The aim of the website is to help the dentist in diagnosis and treatment of traumatic dental injuries. Through the trauma pathfinder the dentist will be led to the correct diagnosis of luxation injuries, fractures, and the many possible combinations of these. The latest version of the IADT treatment guidelines for the different trauma types are illustrated through text and animations. Furthermore, an estimate of the risk of long‐term complications after trauma is provided, based on important predictors such as stage of root development, additional crown fracture, dry storage of avulsed teeth, etc. (Figure 18.33).

Figure 18.33 www.dentaltraumaguide.org.
Reproduced with permission of University Hospital of Copenhagen.
References
- 1. Glendor U, Halling A, Andersson L, Eilert‐Petersson E. Incidence of traumatic tooth injuries in children and adolescents in the county of Västmanland, Sweden. Swed Dent J 1996;20:15–28.
- 2. Andreasen JO, Ravn JJ. Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. Int J Oral Surg 1972;1:235–9.
- 3. Skaare AB, Jacobsen I. Dental injuries in Norwegians aged 7–18 years. Dent Traumatol 2003;19:67–71.
- 4. Skaare AB, Jacobsen I. Etiological factors related to dental injuries in Norwegians aged 7–18 years. Dent Traumatol 2003;19:304–8.
- 5. Andreasen JO, Andreasen FM, Bakland LK, Flores MT, Andersson L. Traumatic Dental Injuries – a manual, 3rd edn. Oxford: Wiley‐Blackwell, 2011.
- 6. Andreasen FM, Andreasen JO. Diagnosis of luxation injuries: the importance of standardized clinical, radiographic and photographic techniques in clinical investigations. Endod Dent Traumatol 1985;1(5):160–9.
- 7. Application of the International Classification of Diseases to Dentistry and Stomatology. ICD–DA 3rd edn. Geneva: WHO, 1995.
- 8. Skaare AB, Jacobsen I. Primary tooth injuries in Norwegian children (1–8 years). Dent Traumatol 2005;21:315–19.
- 9. Malmgren B, Andreasen JO, Flores MT, Robertson A, DiAngelis AJ, Andersson L, Cavalleri G, Cohenca N, Day P, Hicks ML, Malmgren O, Moule AJ, Onetto J, Tsukiboshi M. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent Traumatol 2012;28:174–82.
- 10. Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, Andersson L, Bourguignon C, Flores MT, Hicks ML, Lenzi AR, Malmgren B, Moule AJ, Pohl Y, Tsukiboshi M. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: Fractures and luxations of permanent teeth. Dental Traumatol 2012;28:2–12.
- 11. Andersson L, Andreasen JO, Day P, Heithersay G, Trope M, Diangelis AJ, Kenny DJ, Sigurdsson A, Bourguignon C, Flores MT, Hicks ML, Lenzi AR, Malmgren B, Moule AJ, Tsukiboshi M. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent Traumatol 2012;28:88–96.
- 12. Lauridsen E, Hermann N, Gerds TA, Ahrensburg SS, Kreiborg S, Andreasen JO. Dental trauma. Combination injuries 1. The risk of pulp necrosis in permanent teeth with concussion injuries and concomitant crown fractures. Dent Traumatol 2012;28:364–70.
- 13. Lauridsen E, Hermann N, Gerds TA, Ahrensburg SS, Kreiborg S, Andreasen JO. Dental Trauma. Combination injuries 2. The risk of pulp necrosis in permanent teeth with subluxation injuries and concomitant crown fractures. Dent Traumatol 2012;28:371–8.
- 14. Lauridsen E, Hermann N, Gerds TA, Ahrensburg SS, Kreiborg S, Andreasen JO. Dental trauma. Combination injuries 3. The risk of pulp necrosis in permanent teeth with extrusion or lateral luxation injuries and concomitant crown fractures without pulp exposure. Dent Traumatol 2012;28:379–85.
- 15. Andreasen FM, Norén JG, Andreasen JO, Engelhardtsen S, Lindh‐Strømberg U. Long‐term survival of fragment bonding in the treatment of fractured crowns: a multicenter clinical study. Quintessence Int 1995;26:669–81.
- 16. Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod 1978;4:232–7.
- 17. Bakland L K, Andreasen JO. Will mineral trioxide aggregate replace calcium hydroxide in treating pulpal and periodontal healing complications subsequent to dental trauma? A review. Dent Traumatol 2012;28:25–32.
- 18. Malmgren O, Malmgren B, Frykholm A. Rapid orthodontic extrusion of crown‐root and cervical root fractured teeth. Endod Dent Traumatol 1991;7:49–54.
- 19. Kahnberg K‐E. Surgical extrusion of root‐fractured teeth – a follow‐up study of two surgical methods. Endod Dent Traumatol 1988;4:85–90.
- 20. Andreasen JO, Andreasen FM, Mejare I, Cvek M. Healing of 400 intra‐alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent Traumatol 2004;20:203–11.
- 21. Andreasen JO, Andreasen FM, Mejare I, Cvek M. Healing of 400 intra‐alveolar root fractures. 1. Effect of pre‐injury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent Traumatol 2004;20:192–202.
- 22. Zachrisson BU, Jacobsen I. Long‐term prognosis of 66 permanent anterior teeth with root fracture. Scand J Dent Res 1975;83:345–54.
- 23. Wigen TI, Agnalt R, Jacobsen I. Intrusive luxation of permanent incisors in Norwegians aged 6–17 years: a retrospective study of treatment and outcome. Dent Traumatol 2008;24:612–18.
- 24. Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM. Replantation of 400 avulsed permanent incisors. 1. Diagnosis of healing complications. Endod Dent Traumatol 1995;11:51–8.
- 25. Heintz WD. Mouth protectors: a progress report. J Am Dent Assoc 1968;77:632–6.
- 26. LaBella CR, Smith BW, Sigurdsson A. Effect of mouthguards on dental injuries and concussion in college basketball. Med Sci Sports Exerc 2002;34:41–4.
- 27. Nysether S. Dental injuries among Norwegian soccer players. Community Dent Oral Epidemiol 1987;15:141–3.
- 28. Castaldi CL. Mouth guards in contact sports. J Conn State Dent Assoc 1974;48:233–41.