This chapter was written by Heidi H. Pfeifer, RD, LDN, the ketogenic dietitian at Massachusetts General Hospital in Boston and co-creator of the LGIT diet.
The Low Glycemic Index Treatment (LGIT) for epilepsy was developed in 2002 at the Massachusetts General Hospital by dietitian Heidi Pfeifer and Dr. Elizabeth Thiele as a liberalized alternative to the ketogenic diet. Although effective, the ketogenic diet can be difficult to tolerate due to restrictiveness and poor palatability. To meet the therapeutic ketogenic ratio (4:1 fats to protein and carbohydrates), fats must comprise an extremely high percentage of the daily caloric intake (90%). However, the LGIT is lower in fat (60%) and higher in carbohydrates with a therapeutic ratio that is closer to 1:1. The modified Atkins diet approximates a 2:1 ratio.
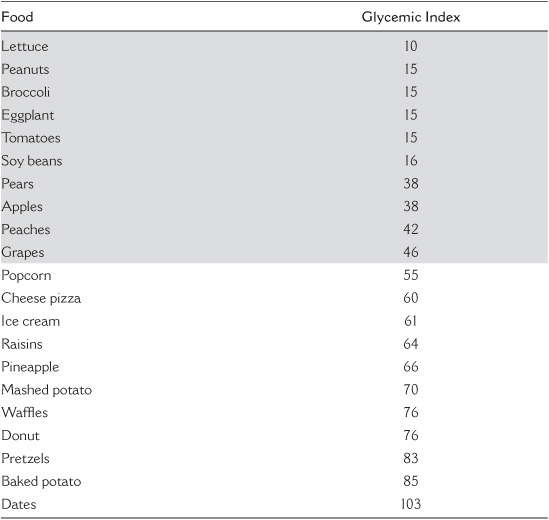
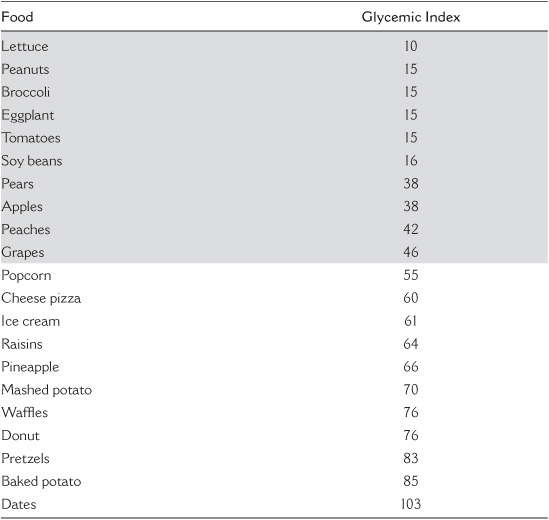
The concept of low glycemic index treatment is new to the field of neurology. However, similar therapies have been used over the past 20 years for diabetes, heart disease, obesity, and polycystic ovary syndrome. A specific food’s glycemic index refers to its effect on blood sugar level as compared to a reference food, like sugar. A number of different variables, such as acidity or fiber levels, can affect a food’s glycemic index; for a given food, the higher these levels, the lower the glycemic index. The glycemic index can be modified by adding fats or proteins to carbohydrates, slowing digestion, and, therefore, lowering the glycemic index. For example, adding butter to bread lowers its glycemic index. A sample of common glycemic index values is listed in Table 21.1. More detail can be found on the Internet (www.glycemicindex.com)
The LGIT is similar to the modified Atkins diet and ketogenic diet as it regulates the quantity of carbohydrates consumed, typically to 40–60 grams per day. A main difference compared to the modified Atkins diet and ketogenic diet is that other than the higher carbohydrate count per day, carbohydrate-rich foods are limited to those with a glycemic index of <50 relative to glucose. On the modified Atkins diet, the type of carbohydrate is not specified, although with only 10–20 grams per day, most patients may tend to gravitate toward the lower glycemic index carbs naturally.
TABLE 21.1
Glycemic Index of Common Foods (Those Foods Under 50 Are Highlighted in Grey)
Like the ketogenic diet, the LGIT is individualized to each patient’s needs. Goals for protein, fat, and carbohydrate intake are provided before treatment initiation to ensure that each patient’s diet meets his or her nutritional needs. However, unlike the ketogenic diet, the LGIT does not require foods to be weighed, as meals are based on every-day portion sizes. This allows family members to eat similar foods at mealtime, as well as to eat together in restaurants while maintaining treatment compliance. Compared to the ketogenic and modified Atkins diets, there is less fat with the LGIT, but many of the foods do end up having fats in them for satiety.
Breakfast
Scrambled egg—2 eggs, 1 oz cheese, 1 tsp butter
Peach
Heavy cream—2 oz
Lunch
Roast beef sandwich
Low-carb pita pocket—1/2
Roast beef—4 oz
Cheddar cheese—1 oz
Horseradish mayonnaise—1/2 tbsp
Roasted red pepper—1/2 cup
Heavy cream—2 oz
Snack
Cheese stick—1
Apple—1/2
Dinner
Grilled chicken salad
Chicken breast—6 oz
Mixed salad with lettuce, tomato, and cucumber
Heavy cream—2 oz
Blue cheese dressing—1 tbsp
Although less restrictive, the efficacy of the LGIT is similar to that of the ketogenic diet. Recent studies demonstrate that more than half of patients on the LGIT achieve >50% reduction in their seizure activity with some patients achieving seizure freedom. Many patients have also been able to reduce their anticonvulsant medications while on the LGIT. Treatment has proven effective for both generalized and partial onset seizures and for an age range from 2 years through adulthood.
Patients on the LGIT are monitored very closely and, at our center, are seen by a dietitian and a neurologist 1 month after initiating the diet and then at 3-month intervals throughout therapy. During appointments, clinicians assess seizure control, measure height and weight, and obtain labs to monitor for side effects. With this information, the dietitian and neurologist can make necessary adjustments to optimize the LGIT.
No severe side effects have been reported in patients on the LGIT. Minor possible side effects include weight loss, acidosis, and constipation. Those individuals who have experienced weight loss often did so intentionally. Patients with symptoms of acidosis experienced lethargy, nausea, vomiting, and headache. However, acidosis can be monitored with a simple blood test and easily treated with an alkalizing agent. Just as on the ketogenic diet, constipation is an issue but is minimized on the LGIT by a higher fiber intake in combination with optimal fluids.
The therapeutic mechanism of the LGIT remains unknown. However, we do know that the diet alters metabolism with fats used as the primary source of energy instead of carbohydrates. This reduction in glycolytic stress is thought to contribute to the therapeutic mechanism of dietary treatment. Fat metabolism results in the production of ketone bodies. In LGIT, the ketone bodies may be present in the blood or urine at lower levels than seen in the ketogenic diet and may be undetectable. Additionally, the stabilization of glucose levels may provide a therapeutic effect. Studies have demonstrated a positive correlation between over 90% seizure control and lower blood glucose levels.
As with any other seizure therapy, when seizure freedom is achieved, the patient may slowly transition off treatment. In the case of LGIT, larger quantities of carbohydrates with a low glycemic index (GI <50) are slowly introduced into the diet. If seizure freedom is not achieved, the patient, family, and clinicians need to assess the benefits of current dietary therapy, as well as discuss other possible treatment options to determine future care.
• Always balance each meal with a protein source, a fat source, and a carbohydrate source.
• Limit daily carbohydrate intake to 40–60 grams spread evenly throughout the day.
• Use carbohydrate foods that have glycemic index values that are less than 50.
• Increase the amount of protein (chicken, fish, beef, eggs, cheese, tofu, etc.) and fats (butter, oil, margarine, and mayonnaise).
• Transition from milk to cream to decrease the amount of carbohydrates that are consumed.
• Provide appropriate vitamin and mineral supplements to meet individual needs in the setting of decreased carbohydrate intake.
• Ensure close follow up with a dietitian and neurologist well versed in dietary treatment of epilepsy. ALL DIETS need to be done with the help of a ketogenic team!