How the Mind Communicates with the Gut
Imagine you’re on the freeway, and the driver who’s been tailgating you suddenly zips into traffic, swerves abruptly in front of you, and then slams on his brakes. You brake hard to avoid hitting him, causing you to swerve to the next lane. Then you see him laugh. Your neck muscles begin to tense up, your jaw clenches, your lips tighten, your brow furrows. From the passenger seat, your spouse immediately notices your angry expression. In contrast, remember a time when you were depressed. Your face sank, your gaze lowered, and people around you noticed.
Recognizing emotions on other people’s faces comes naturally to us. This skill transcends the barriers of language, race, culture, national origin, and even species, as we can recognize an angry dog or a frightened cat. Nature programmed humans to recognize various emotions easily and gauge our responses accordingly. Your emotions are so apparent because your brain sends out a distinct pattern of signals to the face’s many small muscles, which means that every emotion has a corresponding facial expression. The people around you can discern your facial expressions in the blink of an eye. Each of us is an open book.
But we are literally blind to the gut manifestations of these emotions. When you are fuming in traffic, your brain sends out a characteristic pattern of signals to your digestive system, just as it does to your facial muscles; the digestive system also responds dramatically. As you sat fuming about the driver who cut you off, your stomach went into vigorous contractions, which increased its production of acid and slowed the emptying of the scrambled eggs you ate for breakfast. Meanwhile your intestines twisted and spit mucus and other digestive juices. A similar yet distinct pattern happens when you’re anxious or upset. When you’re depressed, your intestines hardly move at all. In fact, we now know that your gut mirrors every emotion that arises in your brain.
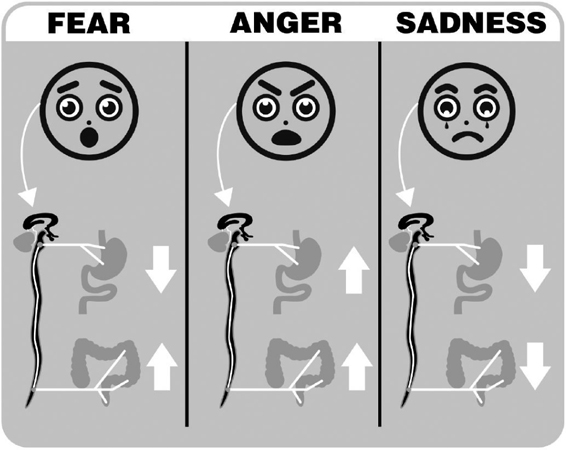
FIG. 3. THE GUT IS A MIRROR IMAGE OF EMOTIONAL FACIAL EXPRESSIONS
Emotions are closely reflected in a person’s facial expressions. A similar expression of our emotions occurs in the different regions of the gastrointestinal tract, which is influenced by nerve signals generated in the limbic system. Signals to the upper and lower GI tract can be synchronous or go in opposite directions. Solid white arrows indicate the increase or decrease in gastrointestinal contractions associated with a particular emotion.
The activity of these brain circuits affects other organs as well, creating a coordinated response to every emotion you feel. When you’re stressed, for example, your heartbeat speeds and your neck and shoulder muscles tighten, and the reverse happens when you’re relaxed. But the brain is tied to the gut like no other organ, with far more extensive, hardwired connections. Because people have always felt emotion in their gut, our language is rich with expressions that reflect this. Every time your stomach was tied up in knots, you had a gut-wrenching experience, or you felt butterflies in your stomach, it was the emotion-generating circuits of your brain that were responsible. Your emotions, brain, and gut are uniquely connected.
If a patient with abnormal gut reactions seeks help from the medical system and an endoscopy does not reveal something more serious, such as gut inflammation or a tumor, physicians often dismiss the importance of the patient’s symptoms. Frustrated about their inability to provide effective relief, they tend to recommend special diets, probiotics, or pills to normalize abnormal bowel habits, without addressing the true cause of the gut reaction.
If more doctors and patients realized that the gut is in fact a theater in which the drama of emotion plays out, that drama might be less likely to become a painful melodrama for patients. Nearly 15 percent of the U.S. population suffers from a range of aberrant gut reactions, including irritable bowel syndrome, chronic constipation, indigestion, and functional heartburn, which all fall into the category of brain-gut disorders. They suffer from symptoms that range from queasiness, gurgling, and bloating all the way to unbearable pain. Amazingly, the majority of patients suffering from abnormal gut reactions have no idea that their gut problems reflect their emotional state.
Even more amazingly, most of the time neither do their doctors.
The Man Who Could Not Stop Vomiting
Of the many patients I have seen in my long career as a gastroenterologist, Bill stands out in my memory more than any other. Bill was twenty-five and otherwise healthy when he came to my office with his fifty-two-year-old mother. Surprisingly, it was she who started the conversation: “I really hope you can help Bill. You are our last resort. We are desperate.”
Over the previous eight years, Bill had spent countless hours in various emergency rooms, suffering from excruciating stomach pain and unstoppable vomiting. During particularly difficult periods, he would visit the ER several times a week. Usually the ER physicians prescribed painkillers and sedatives to treat his discomfort, but none of them seemed to have any idea what was actually wrong with him. Even worse, some labeled him a drug-seeking patient because nothing in the diagnostic tests they ran matched the severity of his symptoms.
Bill had also been to several gastrointestinal (GI) specialists who performed extensive diagnostic tests but without finding a cause for his miserable symptoms. His continued pain and vomiting forced him to drop out of college and move back in with his concerned parents.
His mother, a businesswoman, was frustrated that Bill’s doctors had not been able to diagnose Bill accurately, so she began searching online for answers. “I think he has all the symptoms of cyclical vomiting syndrome,” she told me.
As Bill’s doctor, I wanted to see for myself.
As happens often with brain-gut disorders, many unusual theories have been proposed to explain the unique constellation of symptoms in cyclical vomiting syndrome. But based on decades of research that my team has done with several other research groups at UCLA, I believed that the most plausible explanation was an exaggerated gut reaction triggered by an overactive stress response in the brain.
In patients with cyclical vomiting syndrome, stressful life events generally spark the attacks. A wide range of seemingly unrelated stimuli including strenuous exercise, menstruation, exposure to high altitudes, or simple prolonged psychological stress can cause enough of an imbalance in the body to trigger an attack. When the brain (not necessarily our conscious brain) perceives such a threat, it signals the hypothalamus, an important brain region coordinating all our vital functions, to crank up release of a critical stress molecule called corticotropin-releasing factor, or CRF for short, which functions as a master switch that sends the brain (and the body) into stress-response mode. Patients with this disorder may be completely symptom-free for several months or even years, even though their CRF system is primed all the time. But when they experience additional stress, a recurrence of symptoms is triggered.
When CRF levels rise high enough, it switches every organ and cell in your body, including the gut, into stress mode. In a series of elegant animal experiments, my UCLA colleague Yvette Tache, who’s one of the world’s experts in stress-induced brain-gut interactions, revealed the many shifts in the body that CRF induces.
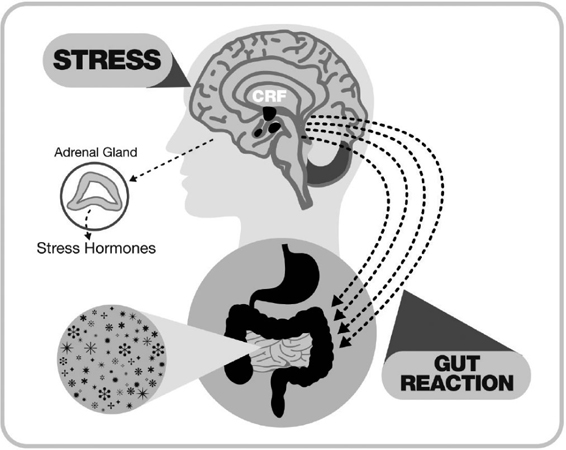
FIG. 4. GUT REACTIONS IN RESPONSE TO STRESS
In response to any perturbations of an individual’s normal balanced state such as stress, the brain mounts a coordinated response aimed at optimizing the organism’s well-being and survival. The corticotropin releasing factor (CRF) is the chemical master switch that sets this stress response in motion. It is secreted by the hypothalamus and acts on closely adjacent regions of the brain. Stress-induced CRF in the brain is associated with an increase in stress hormones (such as cortisol and norepinephrine) in the body. This process also stimulates a stress-induced gut reaction that impacts the composition and activity of the gut microbiota.
In the brain, spiking CRF levels raise anxiety and make people more sensitive to a range of sensations, including signals from the gut, which are experienced as severe belly pain. The gut itself contracts more and its contents are evacuated, resulting in diarrhea. The stomach slows down and even reverses itself to empty its contents upward. The gut wall becomes leakier, the colon secretes more water and mucus, and the amount of blood flowing through the lining of our stomach and intestine increases.
In Bill’s case, just a few key questions about his symptoms would help me make a diagnosis. I asked Bill if he was completely symptom-free in between his bouts of vomiting, which was the case. I asked him and his mother whether there was a family history of migraine headaches, a chronic pain disorder genetically related to cyclical vomiting syndrome. And indeed, both his mother and grandmother suffered from migraines.
“What kind of symptoms do you experience in the period immediately before an attack?” I asked. Bill told me that a full-blown attack was usually preceded by about fifteen minutes of intense anxiety, sweating, cold hands, and pounding of his heart—all symptoms of a stresslike reaction in his body. What’s more, these symptoms woke him up very early in the morning—another identifying feature of the syndrome. (This feature is probably caused by the diurnal increase in the activity of our central stress system.) A hot shower or an Ativan pill could prevent the attacks, but most of the time that didn’t help. “Once the vomiting begins, and I can’t stop it, I have to rush to the emergency room.”
“What happens in the emergency room?” I asked. Bill told me that his doctors reluctantly gave him narcotic painkillers, which usually put him right to sleep, and he’d wake up symptom-free an hour later. Bill’s many previous diagnostic tests, including endoscopies and CT scans of his belly, had not revealed any abnormalities that could explain his symptoms, and a brain scan had ruled out a brain tumor.
Bill’s mother’s Internet diagnosis was indeed correct—he was suffering from cyclical vomiting syndrome. The sad thing was that despite his doctors’ repeated failure to diagnose him correctly, making the correct diagnosis was actually simple, and his mother, who had no medical training, did it on the Internet.
You don’t have to suffer from the crippling symptoms of cyclical vomiting syndrome to experience the limited knowledge that many physicians have about gut reactions gone wrong, and the resulting lack of effective therapies. Nearly 3 in 20 people in the United States suffer from symptoms or syndromes caused by problems from altered brain-gut interactions, including irritable bowel syndrome, functional heartburn, or functional dyspepsia. However, those of you who are not bothered by nasty and unpleasant gut sensations should be aware that you don’t have to have any of these disorders for gut reactions to occur.
Cyclical vomiting syndrome is one of the most dramatic examples of gut reactions gone awry, but it is not the only one. Altered brain-gut interactions can have powerful effects on all of us.
The Little Brain in Your Gut
Imagine that you’re out to dinner with a good friend. The waiter has just served you a medium-rare ribeye and you are reveling in the deliciousness of the meal. Here is a short account of what happens the minute you put the first piece of steak in your mouth—though you may want to avoid making what follows a part of your dinner conversation.
Even before you chew and swallow your food, your stomach fills with concentrated hydrochloric acid that can be as acidic as battery acid. When the partially chewed bites of steak get there, your stomach exerts grinding forces so intense that they break up the steak into tiny particles.
Meanwhile, your gallbladder and pancreas are preparing the small intestine to do its job, by injecting bile to help digest fat, and a variety of digestive enzymes. When your stomach passes the tiny steak particles to the small intestine, the enzymes and bile break them down into nutrients that the gut can absorb and transfer to the rest of the body.
As digestion proceeds, the muscles in your intestinal walls execute a distinct pattern of muscular contractions called peristalsis, which moves food down and through your digestive tract. The strength, length, and direction of peristalsis depend on the type of food you have ingested, ensuring, for example, that the gut has more time to absorb fat and complex carbohydrates, and less for a sugary drink.
At the same time, parts of your intestinal walls contract to steer the food being digested to the lining of the small intestine, where nutrients are absorbed. In your large intestine, powerful waves of contraction move contents back and forth to enable the organ to extract and absorb 90 percent of the water in intestinal contents. Another powerful wave of contraction then moves contents toward the rectum, typically triggering an urge to have a bowel movement.
Between meals, a different pressure wave—the migrating motor complex—serves as your gut’s housekeeper, sweeping out anything else your stomach couldn’t dissolve or break down into small enough pieces such as undissolved medications and unchewed peanuts. This wave slowly travels from the esophagus to your rectum every ninety minutes, generating enough pressure to crack a Brazil nut and sweeping undesirable microbes from your small intestine into the colon. Unlike the peristaltic reflex, this housekeeping wave operates only when there’s no food left to digest in your GI tract—when you’re sleeping, for example—and it switches off as soon you take your first bite of breakfast.
The gut can coordinate all this and more without any help from your brain or spinal cord, and it is not the muscles making up your gut wall that know how to do it. Instead, managing digestion is largely the work of your enteric nervous system (ENS)—a remarkable network of 50 million nerve cells wrapped around the intestine from the esophagus to the rectum. This “second brain” may be smaller than its three-pound counterpart in your head, but when it comes to digestion, it’s brilliant.
Michael Gershon, a prominent anatomist and cell biologist at Columbia University Medical Center, a pioneer in studying the role of the gut’s serotonin system, and author of the popular book The Second Brain, likes to show a video clip that demonstrates the enteric nervous system’s ability to operate independently. In it, a section of guinea pig intestine sits in a bath of fluid, and on its own propels a plastic pellet from one side of the intestine to the other—all without any connection to the brain. In all likelihood, the human gut can operate just as independently.
It’s remarkable that all of these complex digestive functions are coordinated autonomously by hardwired circuits—anatomic connections between millions of nerve cells—within your enteric nervous system, and that this is accomplished without much help from your brain or the rest of your central nervous system—as long as everything goes well.
On the other hand, your emotional brain can mess up just about every one of those seemingly automatic functions. If your dinner conversation takes a wrong turn and you get into an argument with your friend, your stomach’s wonderful meat-grinding activity is quickly turned off and instead goes into spastic contractions that no longer allow it to empty properly. Half of that tasty steak you ate will remain in your stomach without further digestion. Long after you have left the restaurant, your stomach will still be in spasms as you lie awake. Because there is still food in your stomach, the nocturnal migrating contractions won’t happen, preventing the usual overnight cleansing of your gut. In patients like Bill, who have a hyperactive brain-gut axis to start out with, stress-related or emotional triggers that won’t cause much harm to a healthy individual will forcefully inhibit stomach peristalsis and even reverse it, while at the same time creating spastic contractions in his colon. It is as if the set points on the warning system in his brain are off, triggering frequent false alarms, with devastating consequences for his well-being.
Gunshots and Gut Reactions
Humans have always experienced emotion via their guts, and over the years, many curious individuals have tried to learn more about this phenomenon. When army surgeon William Beaumont was presented with the opportunity to learn more about the gut-brain connection in 1822, he didn’t hesitate.
It was early summer, and Beaumont was stationed at Fort Mackinac on Mackinac Island, Michigan, in the upper reaches of Lake Huron. A fur trapper named Alexis St. Martin had been accidentally shot with a musket from less than a yard away. When Dr. Beaumont first saw him a half hour after the accident, St. Martin had a hole the size of a man’s hand in his upper left abdomen. Looking into the wound, Beaumont could see the man’s stomach, which had a hole large enough to fit an index finger.
Beaumont’s excellent surgical care saved St. Martin’s life, but he wasn’t able to close the man’s stomach wound, and St. Martin ended up with a gastric fistula—a permanent hole in his stomach that opened to the outside of his body. After St. Martin recovered, he was no longer able do the physical work of a fur trader, so when Beaumont relocated from Michigan to Fort Niagara in New York State, he hired St. Martin to work with his family as a live-in handyman, and the two became an unusual team of investigator and study subject.
Before long, Beaumont became the first person in history to observe human digestion in real time. He conducted an experiment with St. Martin in which he tied small pieces of boiled beef, raw cabbage, stale bread, and other foods to a silk string and then dangled them in St. Martin’s stomach, pulling them out at different times to test how “gastric juice” from the stomach digested food. The experiments were difficult and uncomfortable for St. Martin, who sometimes became upset and irritable. By directly observing the changes that occurred in St. Martin’s gastric activity, Beaumont concluded that the man’s anger slowed his digestion. In this way, Beaumont became the first scientist in history to report that your emotions can influence the activity of your stomach.
Emotions impact not just the stomach, but your entire digestive tract. As reported by Weeks in 1946, an army physician working in a field during World War II observed a wounded soldier who had suffered extensive combat-related damage to the wall of his abdomen, exposing large portions of his small and large intestine. Doctors observed that when this unfortunate soldier’s injured compatriots began to arrive in the same hospital ward, causing the wounded soldier even more distress, the movement in both his small and large intestine became more active.
It took some twenty years from these graphic early wartime observations to more scientific laboratory studies of mind-gut connections. In the 1960s, an accomplished gastroenterologist at Dartmouth College’s school of medicine, Thomas Almy, examined a larger number of patients under more controlled conditions. He conducted emotionally charged interviews with healthy people and patients with irritable bowel syndrome and monitored the colonic activity of both groups. When subjects reacted with hostility and aggression, their colons contracted quickly, whereas when they felt hopeless, inadequate, or self-reproaching, their colons contracted more slowly. Later, other scientists confirmed these results and found that colonic activity was increased only when topics discussed were personally relevant to the subjects.
Today, scientists agree that the brain is hardwired to link the emotions you experience every day with specific bodily responses. And when push comes to shove, hardwiring directs our gut reactions.
Here is an analogy that I like to use with my patients to help them understand how the brain, enteric nervous system, and gut interact.
Imagine that a hurricane is approaching. The federal government doesn’t send emergency instructions to every individual citizen in the country. Instead, it sends instructions to a network of local agencies, which can broadcast and implement the plans if needed. In the absence of a major threat like a natural disaster, these local agencies can regulate most everything on their own. But when a clear directive comes down from the federal government during an emergency, it overrides many routine activities going on at the local level. Once the threat has passed, the country returns quickly to its regular activities.
Similarly, your enteric nervous system can handle all routine challenges related to digestion. However, when you perceive a threat and feel afraid or angry, the emotional brain center does not send individual instructions to every single cell in the gastrointestinal tract. Instead, the brain’s emotional circuits signal the enteric nervous system to divert from its daily routine. The digestive system switches back to local control once the emotion has passed.
Your brain implements these motor programs in the gut through a variety of mechanisms. It releases stress hormones such as cortisol and adrenaline (also known as epinephrine) and dispatches nerve signals to the enteric nervous system. The brain sends two sets of nerve signals: those that stimulate (carried by the parasympathetic nerves, including the vagus nerve) and those that inhibit gut function (the sympathetic nerves). Usually activated in tandem, the two nerve pathways do a remarkable job of adjusting, fine-tuning, and coordinating the activities of the enteric nervous system to shape gut activity reflecting a particular emotion.
When your emotions play out in the theater of your gut, a large ensemble of specialized cells are at work. The actors include various types of gut cells, cells of the enteric nervous system, and the gut’s 100 trillion microbes—and the play’s emotional overtones will alter their behavior and their chemical conversations. The plots rotate throughout your day, and include both negative and positive stories. On the one hand, there are worries about your children; irritation when the guy in the next lane cuts you off on the highway; anxiety when you’re running late to the meeting; fear of layoffs and financial stress.
On the other, there’s also a hug from your spouse, kind words from a friend, or a pleasant family meal. While we have learned a lot about the gut reactions associated with such negative emotions as anger, sorrow, and fear, we know virtually nothing about the gut reactions to positive emotions such as love, bonding, and happiness. Does the brain refrain from interfering with the activities of the enteric nervous system when everything is fine? Or does it send a distinct set of nerve signals that reflect your state of happiness? And what effect would such happy signals have on the gut microbes, on gut sensitivity, and on the digestion of a meal? What happens in your gut when you sit down for a meal with your family to celebrate the graduation of your daughter from college, or when you are in a blissful state during a meditation retreat? These are important questions that science will need to answer if we want to fully grasp the impact of gut reactions on our well-being.
For some people, the plays performed in the gut include more thrillers and horror stories than romantic comedies. Gut cells in a chronically angry or anxious person, using a script that dates back to childhood, may play out dark plots day after day. Many gut cells in these people over time adapt to accommodate the stage directions: nerve connections in the enteric nervous system change, the sensors in the gut become more sensitive, the gut’s serotonin-producing machinery shifts into higher gear, and even gut microbes become more aggressive. It’s no surprise that when scientists study the gut in patients with functional GI disorders, anxiety disorders, depression, or autism, they find changes in the makeup and behavior of many of these gut players, and the scientific literature is filled with such observations. However, developing therapies targeted at such gut changes has generally failed to provide symptomatic relief for patients with these disorders. On the other hand, one would expect that changing the playbook of the brain to more positive stories, with the goal of altering the gut reactions and thereby reversing the cellular changes in the gut, is more promising. Studies are currently under way to determine if gut microbial changes are associated with positive mind-based interventions, such as hypnosis and meditation, and if these changes lead to symptom improvements in such disorders as irritable bowel syndrome.
How the Brain Programs the Gut’s Emotional Responses
Today, we know a great deal about how emotion affects our bodies, including our GI tract. To understand how it works, you first need to know about the limbic system, a primitive brain system that we share with other warm-blooded animals and that plays a major role generating your emotions. Deep in your gray matter, emotion-specific circuits within the limbic system get activated when you’re angry, scared, feel sexually attracted, or hurt—and also when you feel hungry or thirsty.
Like a miniature supercomputer, these circuits aim to adjust our bodies to respond optimally to changes both inside and outside our bodies. When we face a life-threatening situation, it can turn on a dime, quickly rearranging thousands of messages to individual cells and organs throughout the body, which shift their behavior just as quickly.
We’re all familiar with what happens next. The emotion-related brain circuits send signals to the stomach and intestine to rid themselves of contents that might otherwise drain energy required for action, which is why you might need to head to the bathroom before your big presentation. Our cardiovascular system reroutes oxygen-rich blood from the gut to the muscles, slowing digestion and preparing us to fight (or flee).
We’re not alone in the animal kingdom in these experiences: For millions of years, mammals have needed to bond, fight, assess potential threats, and sometimes flee. Evolution has bestowed upon us a collective wisdom about how to best respond to these situations, and has packaged that wisdom into specific circuits and programs that execute our reactions to threats automatically. This saves time and energy in a moment of crisis because without such hardwired responses, we’d have to start from scratch each time. These programs, known as emotional operating programs, can activate within milliseconds, implementing a coordinated set of behaviors that allow us to survive, thrive, and reproduce.
Jaak Panksepp, a neuroscientist at Washington State University who has made important contributions to the field of affective neuroscience (which applies neuroscience to the study of emotion), has concluded from his experiments on animals that our brains have at least seven emotional operating programs that direct the body’s response to fear, anger, sorrow, play, lust, love, and maternal nurturance. They execute the appropriate set of bodily responses quickly and automatically—even when you don’t know you’re feeling a particular emotion. They make your face flush when you feel embarrassed, give you goose bumps when you watch a scary movie, make your heart beat faster when you’re scared, and make your gut more sensitive when you are worried.
Our emotional operating programs are written in our genes. This genetic coding is, in part, inherited from our parents, and it is also influenced by events we experience early in life. For example, you may have inherited genes that predispose your fear or anger program to overreact to stressful situations. If you also experienced emotional trauma as a child, your body added chemical tags to these key stress-response genes. The net result is that as an adult, you will most likely experience exaggerated gut reactions to stress. This explains the common observation that two individuals exposed to the same stressful situation may show very different reactions to it: while one does not experience any noticeable gut reaction, the other one is incapacitated by nausea, stomach cramps, and diarrhea. While this early programming for trouble may be a good thing for surviving in a dangerous world, it is a liability if you live in the safety of a protected environment.
When the Gut Gets Stressed
Of all of our emotional operating programs, the one engaged by stressful events is among the best studied. When you feel anxious or fearful, your stress response is at work, trying to maintain a state of homeostasis, or internal balance, in the face of internal or external threats.
When we talk about stress, we usually talk about stress from daily living pressures, or larger stressors such as trauma or natural disasters. But your brain also perceives many bodily events as stressful, including infections, surgeries, accidents, food poisoning, sleep deficits, attempts to stop smoking, or even something as natural as a woman’s menstrual period.
Let’s pull back the curtain on what happens in your body when you’re stressed. But first, you need to know more about the emotional brain’s impressive abilities. Life-threatening situations showcase them best.
If the brain decides there’s a threat, it activates the stress program in the brain, which then orchestrates the most appropriate response in our bodies, including the gastrointestinal tract. Each of our emotional operating programs uses a specific signaling molecule, so the release of a particular substance in the brain can trigger the engagement of the entire program with all its consequences on the body and the gut. The brain’s dedicated signaling molecules include a few hormones you’ve probably heard about before—endorphins, which act as a painkiller in the body and promotes a feeling of well-being; dopamine, which triggers desire and motivation; and oxytocin, which is sometimes called the “love hormone” and stimulates feelings of trust and attraction. They also include the molecule mentioned earlier known as corticotropin-releasing factor, or CRF, which acts as the stress master switch.
Even if you’re perfectly healthy and relaxing on a beach, CRF plays a crucial role for your well-being by regulating the amount of the hormone cortisol that is produced by your adrenal glands. Through its normal daily fluctuations, cortisol maintains proper fat, protein, and carbohydrate metabolism and helps keep the immune system in check.
However, when the stress program is activated, there is a dramatic increase in this CRF-cortisol system. When you are stressed, the first responder in your brain is the hypothalamus, a small brain region that controls all your vital functions and is the main production site for CRF. Through a chemical intermediary, the CRF release is followed by activation of the adrenal gland, which starts pumping out cortisol, thereby increasing its level in the bloodstream and preparing the body for the expected increased metabolic demand.
As the stress master switch, CRF released from the hypothalamus also spreads locally to another brain region, the amygdala, which triggers a feeling of anxiety or even fear. This activation of the amygdala plays out in the body as heart palpitations, sweaty palms, and the urge to eliminate any contents from the GI tract.
These stress-induced changes in your digestive system may not sound like the ideal way to enjoy a meal, and they’re not. The next time you’re in the midst of a particularly stressful day, just remember that you might not want to eat a large lunch.
Even if you eat when you’re more relaxed, there’s still a chance you could experience an unpleasant gut reaction to your meal. Once an emotional motor program has been triggered, its effects may linger for hours—or sometimes for years. Our thoughts, memories of past events, and expectations of the future can influence the activities within our brain-gut axis, and the consequences can sometimes be painful.
For example, if you return to the restaurant where you argued with your spouse over dinner, your memories may trigger your anger operating program, despite a friendly dinner conversation this time around. If that restaurant was an Italian restaurant, any Italian restaurant or even the mere thought of risotto di mare may trigger the anger program. I often explain this scenario to my patients, who are quick to blame certain foods for causing digestive distress. I ask them to explore whether it’s the food or in fact a recollection of an earlier event that’s responsible for their symptoms. When they start paying attention to the circumstances that trigger their symptoms, they often realize the incredible power of the brain-gut connection.
The Mirror in Your Gut
One of the most important pieces of information I can give to a patient like Bill, with cyclical vomiting syndrome, or to patients with other disorders of the brain-gut axis, is a simple, scientific explanation of what causes their distressing symptoms, and how this information determines the treatment of this condition. This simple explanation generally relieves the uncertainty about the diagnosis, which tends to ease the patient’s mind as well as the family’s. Science also forms the rational basis for tailoring an effective therapy.
In the clinic, I told Bill that his brain was releasing too much CRF. Excess CRF in his brain was prompting not just his feeling of anxiety, but also the associated heart palpitations, sweaty palms, exaggerated stomach contractions that reversed peristalsis and sent his stomach contents upward, and excessive contractions of his colon, which were associated with cramping pain and sent his stomach contents downward. Bill and his mother were visibly relieved by the information, as it was apparently the first time that anyone had given them a scientific explanation for his symptoms.
“But why do the attacks always happen in the early morning hours?” Bill’s mother wanted to know. I told her that the normal secretion of CRF in the brain naturally peaks in the early morning hours, and gradually declines until midday. So in patients with cyclical vomiting syndrome, brain CRF would most likely reach unhealthy levels early in the morning.
I told them about how CRF declares an emergency and shifts the body from peacetime to war, to teach them how our brain and our gut’s nervous system work together to direct gut function. “This makes total sense,” Bill said, “but why does it happen in my case without any major stresses in the middle of my sleep?”
“That’s exactly where the problem is,” I responded, explaining how the normal brakes on his brain’s emergency mechanisms were faulty, which caused trivial events to trigger his fear-related program. “This will result in many false alarms,” I said.
“I am so glad that we finally know what’s going on,” said his mother. But an explanation only gets you halfway to a solution. She asked what they could do to prevent the attacks from happening in the first place.
To help Bill prevent the vicious attacks that were keeping him from living a full life, I prescribed several medications that calm hyperactive stress circuits and the hyperarousal associated with the excessive CRF release. Some of these aimed to reduce the frequency of his attacks, others to stop an attack in its tracks should one occur. Fortunately, with proper treatment, most cyclical vomiting patients improve dramatically—they have fewer attacks, and they get better at stopping a developing attack. Over time, patients lose the fear of recurring attacks that had held them back, which often allows them to reduce or discontinue the medication.
This was exactly what happened with Bill. When I saw him three months later, he had only had a single episode, and he had stopped it by taking Klonopin, an antianxiety medication I had prescribed. After years of suffering and enduring humiliating comments from emergency room physicians, he was excited to finally be able to rebuild his life. Other cyclical vomiting patients I’ve seen have required additional treatments to recover, including cognitive behavioral therapy and hypnosis. But Bill did not. He resumed his college classes and was even able to greatly reduce his medication over time.
We can all learn from patients like Bill, as I do every day in the clinic. Normal gut reactions, such as worrying about a job interview, or transient upsets from being stuck in traffic or running late to an appointment are never a major problem. However, we should be mindful of the detrimental effects of such emotions on our gut and its many residents when they occur chronically, in the form of anger, sorrow, or recurrent fear. Remember, the stage on which these gut reactions play out is large, and the number of actors is huge. This may not be such a big deal in the case of a feeling of thirst, which we can easily quench with a glass of water, or an acute pain that only lasts a few minutes. It is of greater concern when we recall that emotions always have a mirror image in our gut, and speculate about the detrimental effects that chronic anger, sorrow, or fear may exert not only on our digestive health but on our overall well-being.