Our epitaph [as a species] may well read: “They died of a peculiar strain of reductionism, complicated by a sudden attack of elitism, even though there were ready natural cures close at hand.”
—Gary Paul Nabhan, Cultures of Habitat
Most herbalists, irrespective of culture or country, do know of the antibacterial activity of plants and they do use them to heal bacterial disease on a regular basis, but, in general, our understanding of herbal antibiotics has been thin. By thin I mean we’ve been stuck in a paradigm of “take this for that” or “what’s that plant good for” or even (among the reductionist herbal schools that have adopted the medical model; that is, the phytorationalists) “the active constituent of Hypericum perfoliatum should be standardized in order for the plant to be effective in the treatment of mild depression.” Given the seriousness of the emerging bacterial diseases, we need to have a more comprehensive paradigm in place, one that takes into account the potential sophistication of herbal medicine as a very ancient art form of healing, one that uses both perceptual and intellectual awareness, as well as a focus on outcomes, in its expression.
The importance of systemic herbal antibacterials cannot be overstated.
Many resistant diseases, such as staph, are widely spread throughout the body. They can affect internal organs, invade difficult-to-reach parts of the body, or, very commonly, infect the skin (from the inside rather than outside), appearing as skin ulcerations in various locations. To treat a systemic infection like staph, an herbal antibiotic that is systemically spread throughout the body is necessary.
I remember the first time someone told me she had a community-acquired systemic staph infection; it was a woman who’d come to hear me teach. She said that she had undergone numerous courses of antibiotics, and that after the last one failed the physicians had told her, “Well, let’s just observe it and see what happens.” Her furious response was, “I know what’s going to happen, I’m going to lose my foot.”
I began to understand then just how important systemic antibacterials are in herbal practice. With resistant bacterial infections spreading at the rate they are, we need systemics—we need to know them as a category and we need to really know how to use them. We need to move from herbalism as a kind of “let’s-eat-organic-today” choice (unless we’re really sick; then we’ll go to the emergency room) to a “we-can-depend-on-this-for-our-life” form of healing.
When herbs are taken into the body, some just stay pretty much in the GI tract, whereas others cross the intestinal membranes and circulate in the body, often concentrating in particular locations; the liver or kidneys, for instance. But one class of herbs is always broadly systemic. Once ingested they concentrate in the bloodstream (and sometimes the liver) and are widely circulated, reaching every cell that needs a constant blood supply, which is pretty much every cell in the body. These are the herbs that have traditionally been used to treat malaria. Many, if not most of them, also tend to possess rather strong antibacterial actions, sometimes broadly so. It is important, however, to make a distinction between the two common types of malarial herbs, for not all malarial herbs are true antimalarials.
Some malarial herbs are widely systemic and actually do kill the parasites responsible for malaria, but others only treat some of the symptoms of the disease such as fever or chills. Many researchers have not understood the distinction and so they may list an herb as being used for malaria when in fact it is only being used as an adjunct herb to treat one of the symptoms of malaria; for instance, when yarrow is used to treat malarial fevers.
Yarrow isn’t a systemic antimalarial (even though it does have some mild actions against the parasite) but, rather, is a diaphoretic adjunct. It helps reduce fevers because it induces sweating, which cools the body. When researching the ethnobotanical literature, it is crucial to understand this distinction between the different kinds of malarial herbs. Once you do, their study begins to open up the wider world of systemic antibacterials. Systemic antibacterial herbs have often been used for centuries in the treatment of malaria simply because one of their antimicrobial actions is against malarial organisms. But they are often widely active against other organisms and can be very powerful. (Systemic antibacterials may also be found in a particular category of Chinese medicine—plants for toxic blood.)
The first systemic herbal antibiotic I began to understand was Cryptolepis sanguinolenta, a traditional herbal medicine from Ghana. I was introduced to it by a healer from Ghana, Nana Nkatiah, and it was this herb that I recommended to the woman who approached me at the workshop. Her family had become infected through exposure to her and at this point they were all ill. They used cryptolepis and it worked very well. Since then I have used cryptolepis on numerous occasions to treat systemic staph infections that have not responded to multiple antibiotic regimens. It has, so far, never failed. I consider this plant, along with alchornea, sida, and bidens, to be the primary systemic herbal antibiotics for use in treating resistant organisms at this time.
While cryptolepis is sometimes hard to find, many of the other herbs in this section are not—at least in the wild. They are often widely distributed throughout the world; a number of them are considered invasive plants, which is a plus.
Invasive plants—Earth’s way of insisting we notice her medicines.
Family: In flux, given the propensity of botanical PhD students to write dissertations on minutiae; probably Apocynaceae (subfamily Periplocoideae) or perhaps Asclepiadaceae
Common Names: Cryptolepis (in the West) • delboi • gangamau (among the Hausa) • Ghanian quinine • kadze (among the Ewe) • koli mekari (among the Mpiemo peoples in the Central African Republic and the eastern part of Cameroon) • nibima (among the Twi-speaking people of Ghana) • ouidoukoi • yellow dye root
Species Used: There are about 20 or maybe 30 (taxonomists are so irritating) species of cryptolepis, 10 or more in Africa, two in Madagascar, four in Asia, three in Papua New Guinea, and one in Australia, and probably others elsewhere if that larger number is accurate. The primary systemic antibacterial among the genus is Cryptolepis sanguinolenta.
The potency of C. sanguinolenta has generated a lot of interest in this genus of plants. C. triangularis, native to Angola, Lagos, Belgian Congo, and Gambia, has, like C. sanguinolenta, been found to contain cryptolepine, one of the more potent antimalarial alkaloids known. (Some sources consider these two to be the same plant; others list them as distinct species.) Some sources say that all the members of this genus contain the antibacterial alkaloids cryptolepine, quindoline, and neocryptolepine. I have been unable to verify this by finding any in-depth chemical analysis of the other species. A number of sources do list cryptolepine and similar alkaloids as present in C. buchanani, a traditional Ayurvedic plant, commonly used as a medicinal in Thailand, Nepal, and India. It may be true; the traditional uses of C. buchanani show the same range of action as that of C. sanguinolenta, so I tend to give the reports credence. C. hypoglauca is reported in one study to contain cryptolepine, but I can’t find anything definitive on that either.
Of all the plants in the genus, C. buchanani and C. obtusa have stimulated the most interest outside C. sanguinolenta. Given the importance of C. sanguinolenta, in-depth chemical research needs to be done on the entire genus to determine whether the other species within it can be used as effectively.
The root is usually the part used medicinally (or in dyeing). The leaves can be used medicinally (see the description of the plant’s chemistry below) but rarely are. The root of the plant is generally about the thickness of a pencil, appears to be fairly consistent in thickness over long lengths, and has a light tannish color on the thin exterior bark and a brilliant yellow on the interior. It’s pretty. The root is exceptionally bitter due to the many alkaloids present.
Cryptolepis can be prepared as powder, capsules, tea, or tincture.
For bacterial infections of the skin and wound sepsis, liberally sprinkle cryptolepis powder on the site of infection as frequently as needed.
1:5, 60 percent alcohol, 20–40 drops, up to 4x daily
For resistant staph: In the treatment of severe systemic staph infection, the usual dose is ½ tsp–1 tsp, 3x daily. In very severe cases increase the dose to 1 tbl, 3x daily. (I prefer to not use dosages this high for longer than 60 days. That is usually sufficient.)
For malaria: 1 tsp–1 tbl, 3x daily for 5 days, repeat in 14 days
Use 1 teaspoon cryptolepis in 6 ounces water to make a strong infusion.
As a preventive: Drink 1 or 2 cups daily.
In acute conditions: Drink up to 6 cups daily.
Note: While the herb will work if infused in cold water, studies have found that the hot-water extraction is more effective. It is nearly as strong as the alcohol tincture.
As a preventive: Take 3 “00” capsules 2x daily.
In acute conditions: Take up to 20 capsules daily.
None noted. Considerable research has taken place to determine the potential adverse reactions from using the plant, and none have been found, either in human clinical use or with in vivo testing on mice, rats, and rabbits. The herb is taken as a regular tonic for years at a time in some parts of Africa and India. One or two cups of the tea or two or three droppers of the tincture (60 to 90 drops) a day are fine for extended, long-term use.
Researchers in some instances have noted that people taking cryptolepis have elevated levels of ALP (alkaline phosphatase) and uric acid, which return to normal after the herb is discontinued. There have been no reported side effects from this. And though there is one report in the literature of adverse effects of cryptolepis in mouse pregnancy, I can find nothing in traditional use that substantiates an extrapolation to humans nor any studies in the literature that show negative effects in pregnancy in people.
Cryptolepine has been found to be cytotoxic, which raises concerns in some people. A few points:
• Cryptolepine is an isolated constituent, and like most isolated constituents that are made into pharmaceuticals, it produces side effects that don’t appear when the whole herb is used. Cryptolepis itself has not been found to be cytotoxic to people.
• The word cytotoxic, when used in reports, generally means it kills cancer cells, and indeed, cryptolepine does.
• Cryptolepine is cytotoxic because it intercalates DNA. DNA is a double helix, two joined twisted ladders. Cryptolepine inserts itself between the two ladders—that is, intercalates—and as a result interferes with cellular division, which is why it is useful in cancer treatment. Cryptolepine is a potent inhibitor of topoisomerase II, which it inhibits once it intercalates. The function of topoisomerase II is to allow DNA replication by unwinding the DNA helix, using it as a template, then winding it again after replication. If topoisomerase is inhibited, DNA replication, and cellular division, can’t occur.
None noted. However … cryptolepis has been used in traditional medicine to help rectify insomnia. One mouse study has supported that effect of the plant. There is some potential for the plant to synergize with hypnosedatives or central nervous system depressants. Caution should be exercised, although there have been no reported adverse effects in these situations to date.
Actions
Antibacterial
Anticomplementary activity
Anti-inflammatory
Antimalarial
Antimicrobial
Antimuscarinic
Antiparasitic
Antiprotozoal
Antipyretic
Antithrombotic
Antiviral (mild)
Hypoglycemic
Hypothermic
Noradrenergic
Renal vasodilator
Active Against
Aspergillus spp.
Babesia spp.
Bacillus subtilis
Campylobacter spp.
Candida spp.
Entamoeba histolytica
Enterobacter cloacae
Escherichia coli
Herpes simplex
Klebsiella spp.
Mycobacterium spp.
Neisseria gonorrhoeae
Plasmodium spp.
Proteus mirabilis
Proteus vulgaris
Salmonella spp.
Shigella dysentariae
Staphylococcus aureus
Streptococcus pyogenes
Tests have found the plant to be a stronger antibacterial than the pharmaceutical antibiotic chloramphenicol. Generally, it is more broadly active against Gram-positive bacteria (which are usually easier to treat due to their cellular structure), but it does have potent activity against a number of Gram-negative bacteria.
A number of studies have found cryptolepis active against Pseudomonas aeruginosa; other studies have found it ineffective. A balanced review of the journal papers, in my opinion, indicates that it is active against Pseudomonas. Examination of the studies does not give an easy clue as to the discrepancy in findings, but preparation differences seem to be involved.
Cryptolepis possesses little antifungal activity, though again, some studies have found it effective against candida while others have not. Again, a review of the studies, in my opinion, indicates that it is effective against candida and that preparation problems are the source of the discrepancy.
Systemic infections, especially malaria, MRSA, streptococcus, babesia, campylobacter, urinary tract infections, tuberculosis, wound sepsis. It is very good for several Gram-negative bacterial infections: klebsiella, salmonella, shigella, E. coli, enterobacter, gonorrhea, and most likely pseudomonas
Other Uses
The root has long been used as a brilliant yellow dye in the regions in which it grows; hence its common name, yellow dye root. The dye is usually used for dying leather, generally goat skins. The roots are gathered, dried, then ground in a wooden mortar. The powdered root is blended with hot water in a large vessel. The goat skin is coated with groundnut oil and then dipped in the dye bath. The extract is hand-rubbed into the leather during soaking. Then a tamarind fruit paste is added and rubbed in. The skin is exposed to air for a few minutes, then reimmersed in the bath and rubbed once more. The fruit paste purifies the color.
Though the roots are the primary part of the plant used (both for dye and medicine), the leaves are used as a vegetable in Burkina Faso.
Cryptolepis sanguinolenta is a slender, thin-stemmed climbing shrub whose stem produces a blood-red to deep orange juice when cut (sanguinolenta means “tinged or mixed with blood; bloody”). Essentially it’s a tropical plant that likes it hottish and a bit humid. It is common from sea level to 2,500 feet (800 m) in altitude in savanna, dry forest, and gallery forest—that is, the riparian forests that develop along rivers and wetlands.
From reports, though it is usually wildcrafted, cryptolepis seems fairly easy to cultivate from seed and root cuttings. The seeds can be broadcast if desired. Due to its climbing nature, the plant needs a trellis to do well. Because of the growing international interest in the plant, commercial planting in Africa is on the increase.
The seeds are collected when semi-ripe and red/black in color. Normally they are then planted in raised mounds to facilitate harvesting of the roots. The seeds lose viability fairly quickly; they have a 90 percent to 100 percent germination rate for 4 weeks after harvesting and then begin to decline.
Roots can be collected after the plant is 1 year old, at any time of year. The side of the mounds are dug into and the root harvested. Up to one-third of the root from an individual plant can be taken without damaging the plant or its growth.
Cryptolepis would probably grow well in the American South, the northwest Olympic Peninsula, and parts of the West, or in any climate similar to its natural home. Given its importance, it should be cultivated wherever and whenever it can grow.
There is some confusion in the naming of some of the more potent alkaloids in C. sanguinolenta, as researchers in different parts of the world named them with different names at about the same time. It still isn’t sorted out. However, the primary ones are cryptolepine, neocryptolepine (a.k.a. cryptotackieniene, quinindoline), several other forms of neocryptolepine, hydroxycryptolepine, cryptolepine hydrochloride, isocryptoline (a.k.a. cryptosanguinolentine), quindoline, cryptoheptine, biscryptolepine, cryptoquindoline, cryptospirolepine, and cryptomisrine.
Most cryptolepis species contain phenolic compounds but C. sanguinolenta does not. Screening has found alkaloids (numerous), polyuronoides, and reducing sugars but little else. Polyphenols, saponins, flavonoids, and cyanogenic glycosides have been reported in at least one study. Cryptolepine is considered to be the strongest constituent (see the sida monograph, page 102, especially the “Scientific Research” section), though many of the others are nearly as potent.
An analysis of the leaves has found many of the same alkaloids that are present in the root, including cryptolepine. Aqueous and ethanolic extracts of the leaves are highly active against malaria (and presumably other microorganisms), giving a 90 percent inhibition of multidrug-resistant malarial strains in vitro. The leaves contain at least two novel alkaloids not present in the roots: cryptolepinoic acid and methyl cryptolepinoate, as well as the usual cryptolepine, hydroxycryptolepine, and quindoline.
C. buchanani, C. hypoglauca, and C. triangularis have all been listed as containing similar alkaloids as C. sanguinolenta. The research is thinner than I would like and triangularis may be a synonym of sanguinolenta. Buchanani has been studied in the most depth. It’s a traditional herb in Ayurvedic practice (see that description, page 98). Several sources list it as containing cryptolepine and quindoline as well as sarmentogenin, sarmentocymarin, nicotinoyl glucoside, glucopyranose, buchananine, buchanin, n-triacontanol, n-triacontanoic acid, alpha-amyrin, beta-sitosterol glucoside, cryptosin, cryptanoside A-D, germinocol, cryptolepain, sarverogenin, and isosaverogenin. These latter two compounds appear to have potent antibacterial and antiparasitic properties. Given its traditional uses in India, it appears that C. buchanani may in fact be a good substitute for sanguinolenta.
C. obtusa contains some novel steroidal alkaloids, but not much work has been done on this plant—and on the rest of the family even less.
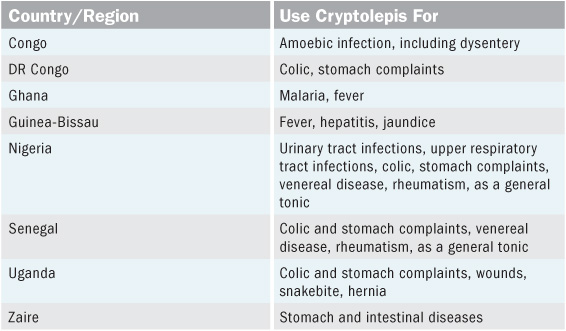
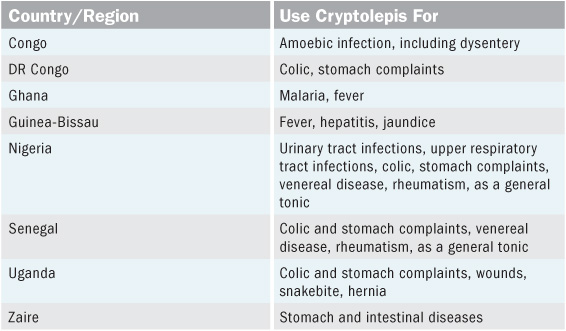
Cryptolepis has been successfully used for centuries by traditional African healers in the treatment of malaria, fevers, and diarrhea, as shown in the chart below.
Cryptolepis buchanani has been used in traditional Ayurvedic practice for millennia. It is widely distributed throughout Pakistan, India, Nepal, Bhutan, Myanmar, China, Thailand, and Sri Lanka. It is considered an invasive weed in many areas (a useful sign of medicinal importance). There are a multitude of local names for the plant in those regions, 60 that I have identified so far. Maranta is a common one. It’s been used as an antidiarrheal, antibacterial, anti-inflammatory, antiulcerative, blood purifier, demulcent, diaphoretic, and diuretic, and for treating paralysis and rickets and as a general tonic for overall health. It is commonly used for urinary tract infections, for coughs as an expectorant, as a febrifuge (antipyretic), and for abdominal disorders such as dysentery.
In Thailand alcohol extracts of the plant have been used as a primary anti-inflammatory in the treatment of arthritis, muscle and joint pain, and rheumatism.
Scientific studies of C. buchanani conducted in India and based on traditional use have found it is strongly antibacterial, effective against Staphylococcus aureus, E. coli, Salmonella typhimurium, Klebsiella pneumoniae, Proteus vulgaris, and Bacillus subtilis. Research has found it to possess immunopotentiating properties (useful in immunodeficiency), to act as a cardiotonic and cardio-protector, to be hepatoprotective, and to be strongly anti-inflammatory. It has shown some hypotensive actions and is considered to be, in one study, antiamphetaminic (a truly strange category—I gave him the amphetamines but they didn’t work because …).
Given the plant’s presence in China and nearby countries, it is certain that it is used in TCM, but none of my sources, though rather extensive in places, give a listing for the plant.
Until recently, this plant was not known to Western practice.
Cryptolepis was discovered by the West because of the resurgence of pharmaceutically resistant plasmodial parasites. In an attempt to find new treatments for malaria, researchers began looking at traditional treatments. Initial studies revealed both Cryptolepis sanguinolenta and Artemisia annua (see monograph, page 140) to be powerfully active against resistant strains. Artemisia was the first to be developed into a drug (with the same predictable problems ensuing). Cryptolepis lagged behind, but in the past 15 years a tremendous amount of research has been conducted on the plant. Initially, most of it was concerned with malaria.
Cryptolepis is potently active against the malarial parasite, Plasmodium falciparum. (It is also active against other members of the genus: P. berghei berghei, P. berghei yoelii, and P. vinckei petteri.) Scores of studies have found it to be effective against the malarial parasite no matter the degree of its resistance to pharmaceuticals. Five of the plant’s constituents—cryptolepine, cryptolepine hydrochloride, hydroxycryptolepine, cryptoheptine, and neocryptolepine—have been found to be exceptionally active against the parasite, and one other, quindoline, is also active, though not as strong. Studies looking solely at inhibition of beta-haematin formation, which is one of the primary ways that antimalarials deal with malarial infection of blood cells, have found that seven compounds in cryptolepis are active in that respect.
The herb has been remarkably potent against malaria in human clinical trials. One such trial compared the effectiveness of cryptolepis (a hot water infusion of the powdered root) with chloroquine, the usual synthetic drug for malaria treatment, in comparative patient populations at the outpatient clinic of the Centre for Scientific Research into Plant Medicine at Mampong-Akuapem in Ghana, West Africa. Clinical symptoms were relieved in 36 hours with cryptolepis, and 48 hours with chloroquine. Parasitic clearance time was 3.3 days in the cryptolepis group, and 2.3 days in the chloroquine group—a remarkably comparable time period. Forty percent of the patients using chloroquine reported unpleasant side effects necessitating other medications, whereas those using cryptolepis reported no side effects.
Because many of the antimalarial compounds in cryptolepis are water soluble, and water-soluble extracts have worked well in clinical trials, a local company in Ghana hopes that a premade tea of cryptolepis will work well against malaria. Using 2.5 grams of powdered root per tea bag, the preparation is called Phyto-Laria and can be purchased over the counter in Ghana. (Similar products, Malaherb and Herbaquine, are also available in Ghana, and one called Malarial is sold in Mali.)
Pharmaceutical companies have created a number of cryptolepine analogues in an attempt to generate a patented drug they can control. Side effects from these analogues are unknown (isolated cryptolepine, unlike the plant it comes from, has shown a number of serious side effects during in vitro and in vivo studies), and like artemisinin and artesenuate (constituents isolated from Artemisia annua; see monograph, page 140), these analogues are likely to prove futile in the long run since the malarial parasite does develop immunity to single chemical compounds with regularity. Even though the analogues are molecularly close to cryptolepine, studies have found their mode of action to be different from cryptolepine’s—the researchers really don’t know what they do in the body or the likely long-term impacts. Because the herb itself is so tremendously safe and effective, I would not recommend the use of analogues if they do in fact ever come on the market.
Cryptolepis is also broadly antibacterial. It has been tested against over 100 strains of campylobacter bacteria and found strongly effective against all of them. The tincture is more effective than co-trimoxazole and sulfamethoxazole, and equal to ampicillin. Cryptolepis is active against cholera but is not as strong in its effects as tetracycline. It has been found to be broadly active against a number of enteropathogenic microorganisms including Shigella dysentariae, Entamoeba histolytica, and E. coli. It is especially potent in the treatment of resistant staph, Streptococcus pyogenes, numerous strains of tuberculosis (Mycobacterium spp.), and urinary tract infections caused by enterobacter and klebsiella bacteria. The activity against such a wide range of organisms bears out its traditional use for many of the diseases that these organisms cause.
Cryptolepis also possesses anti-hyperglycemic properties, making it a potential antidiabetic herb. The isolated constituent cryptolepine lowered glucose levels in mouse models of type 2 diabetes, caused a decline in insulin levels, and enhanced glucose uptake. Several patents have been granted in this area.
The herb is strongly hypothermic, which means it lowers body temperature, a main reason why it has been found so effective in the treatment of fevers. It is also hypotensive due to its vasodilating effects, and it has been found to be active against a number of cancer lines and is stimulating interest as a potential anticancer agent.
Family: Malvaceae
Common Names: Most of the species in this genus are commonly called something to do with “fanpetals,” and in fact the sidas are sometimes referred to as the fanpetals. S. cordata, for example, is heartleaf fanpetals, S. neomexicana is New Mexico fanpetals, S. spinosa is prickly fanpetals, and so on. If it has fanpetals as part of its common name, it is probably a sida.
Oddly, the most medicinally inclined tend to be called something else: S. cordifolia is country mallow, S. rhombifolia is Cuban jute, S. acuta is common wireweed or teaweed or ironweed—all of which give an indication as to its nature, as does the Australian common name: spinyhead sida. Sometimes it is called hornbeam-leaved sida, morning mallow, or broomweed (the immensely durable branches are used everywhere the plant grows to make brooms), but most prefer a nastier name.
The sidas are so widely distributed around the world and used in so many medicinal traditions that their non-English common names are legion. (See the Traditional Uses section on page 113 for some examples.)
Species Used: There are 125 or 150 or 200 species of the genus Sida (taxonomy is an exact science). They are distributed throughout the world, mostly in the tropics and subtropics, but some species extend into temperate regions.
The main medicinal species that has been studied is Sida acuta. However, as research has deepened on this species, other sidas are coming to light as similarly potent, particularly S. rhombifolia and S. cordifolia. Two other species, S. tiagii and S. spinosa, have not been studied as extensively, but their traditional uses, and some research, indicate they may possess the same medicinal actions.
Given the potency of some of this genus, it makes sense for more research to occur. As far as I can determine, little has been done along this line, but it may well be that many sidas contain similar constituents. If so, given their wide range, they would be one of the world’s most accessible systemic herbal antibacterials.
This section will primarily concentrate on where the most research has been done: Sida acuta, with some depth on S. rhombifolia, S. cordifolia, S. spinosa, and S. tiagii.
Note: Sida carpinifolia is considered to be a synonym of S. acuta.
The whole plant—roots, leaves, stems, seeds. Most people tend to just use the aerial parts for the simplicity of harvest and ecological soundness. More practically, harvesting the root of a mature plant in this genus is as difficult as conveying to a politician the meaning of the word integrity. It is a tough, tough root to dig up. Nevertheless, S. acuta is considered an invasive botanical in many countries and most people are happy if you just take the whole damn thing.
The tincture and the hot-water extract are the strongest medicinal forms of sida for internal use. The plant can be prepared as powder, capsules, hot tea, or alcohol tincture. Most people use the leaves.
For bacterial infections of the skin, wound sepsis, and eczema, liberally sprinkle the powder on the site of infection as frequently as needed.
As a preventive: Take 3 “00” capsules 3x daily.
In acute conditions: Take up to 30 capsules daily. Or you can just use 1–3 tablespoons powder in water or juice.
1:5, 60 percent alcohol, 20–40 drops, up to 4x daily
For resistant staph: In the treatment of severe systemic staph infection the usual dose is ½ tsp–1 tbl, 3–6x daily. (I prefer to not use dosages this high for longer than 60 days. That is usually sufficient.)
Use 1–2 teaspoons of the powdered leaves in 6 ounces water; let steep 15 minutes.
As a preventive: Drink 1 or 2 cups daily.
In acute conditions: Drink up to 10 cups daily.
For eye infections: Use the cool tea as eyedrops, 1–3 drops as needed, 3–6x a day.
Note: While the herb will work if infused in cold water, studies have found that the hot-water extraction is more effective. It is nearly as strong as the alcohol tincture. Also, because the plant’s primary active constituents are alkaloids, the water used for the infusion must be acidic; see the box on page 92.
None noted, known, or reported; however …
• The herb is traditionally used to prevent pregnancy. It does interfere with egg implantation in mice. The herb should not be used in patients who are trying to get pregnant or are newly pregnant.
• Even though the herb is traditionally used in later pregnancy, caution should be exercised with pregnant patients. I would be uncomfortable using it if I were pregnant, but then I would be uncomfortable anyway if I were pregnant.
• Since the herb contains cryptolepine, it is a DNA intercalator and interferes with DNA replication. (See page 93 in the cryptolepis monograph, for more.)
• The herb contains ephedrine, although not in large quantities (see Plant Chemistry, page 111, for an explanation of just how minute those amounts are). There has been a lot of inaccurate, hysterical reporting on ephedra, even among researchers who should know better. Weight loss and “natural energy” companies marketed supplements containing the herb (usually along with caffeine and other stimulants). People wanting to lose weight or increase their energy took the supplements—often in huge doses, far beyond sanity. Herbalists did not support this use of the herb. Ephedra is very safe when used properly; it really didn’t need to be banned. The companies using it improperly just needed to be prohibited from doing so. Nevertheless, be aware that sida contains minute amounts of ephedra and that a mild raciness or wakefulness may occur from using the herb—but it probably won’t. (See more in Finding Sida, page 108.)
None known or reported; however …
• Since the herb is hypoglycemic, it may affect medications for diabetes. Just watch blood sugar levels of diabetic patients.
• Since the herb contains ephedrine, it probably should not be used with pharmaceuticals that possess similar effects.
Actions
Adaptogenic
Analgesic
Anthelmintic (fresh leaf juice)
Antiamoebic
Antibacterial
Anticancer (antineoplastic, antiproliferative)
Antifertility activity (inhibits egg implantation in mice)
Anti-inflammatory
Antimalarial
Antimicrobial
Antioxidant (mild)
Antiprotozoal
Antipyretic
Antiulcerative
Antivenin activity
Hematoprotectant
Hematoregenerator
Hematotonic
Hepatoprotective
Hypoglycemic
Insecticidal
Active Against
Sida acuta is active against:
Babesia spp.
Bacillus spp.
Escherichia coli
Herpes simplex
Listeria innocua
Mycobacterium phlei
Pasteurella multicocida
Plasmodium spp.
Salmonella typhimurium
Shigella boydii
Shigella dysentariae
Shigella flexneri
Staphylococcus aureus
Streptococcus pyogenes
The plant is apparently less active against Pseudomonas aeruginosa, Candida spp., Aspergillus niger, and A. fumigatus (however, see the Scientific Research section on page 116).
Sida rhombifolia is active against:
Aspergillus niger
Bacillus spp. (various)
Candida albicans
Entamoeba histolytica
Escherichia coli
Klebsiella pneumoniae
Micrococcus luteus
Morganella morganii
Proteus vulgaris
Pseudomonas aeruginosa
Salmonella enteritidis (mildly)
Salmonella paratyphi
Salmonella sonnei
Salmonella typhi
Shigella boydii
Shigella dysentariae
Staphylococcus aureus
Vibrio mimicus
Vibrio parahaemolyticus
Anemia
Cancer of the blood
Diarrhea
Dysentery
Eye infections (as eyedrops)
Fevers
Infected wounds
Malaria
Skin rashes such as eczema and impetigo
Systemic staph infections
Tuberculosis
Early indications are that sida is moderately virucidal against herpes viruses and can help prevent outbreaks. It is also useful as an adaptogenic in long-term debilitating infections such as Lyme, malaria, and dysentery.
Sida is very high in protein, being 16 percent to 25 percent protein depending on how it is grown. Some cultures use it as a pot herb; it is possible to use it as a primary protein source, especially if you are an “invasivore.” Yes, they do exist. Invasivores eat only invasive species—though none have yet (publicly) admitted to consuming Homo sapiens.
I have not eaten sida, but the tincture is delicious, one of the few that delights the tongue. If you do try the herb as a vegetable, let me know what you think.
Many cultures use the plant’s twigs in making brooms. From all reports they are exceptionally long lasting and useful given the hardiness of the wood. The bark from the stems of most species has been used for making cords, ropes, and twine; the bark from S. acuta can be used for making canvas and fishnets as well, hence the “jute” designation for some of the species.
Many of the sidas are typical-looking mallow-like plants with the usual five-lobed pale yellow to orange flowers. They get their name from the spreading or fanning of their flower petals. Some of the species are ground covers, while others grow into sturdy bushes as much as 6 feet (2 m) tall. They can be perennials, annuals, or biennials—and I am talking about the same plant here; they alter their behavior depending on where they are growing and the climate. They are often considered wasteland weeds irrespective of the species.
Sida acuta grows from 3 to 6 feet tall and may appear as either an annual or a perennial. It is a potently invasive medicinal wherever it gets established. In general, when the sidas get loose, they just keep on going, and they don’t like to be controlled once they’re established.
S. acuta has a very deep and strong taproot that endures droughts, mowing, and tillage with impunity. The plant easily survives extensive foraging by animals. With age the stem gets tough and woody, which helps the plant resist the phytopolice who wish to send it back to Mexico. Once established, the plant is highly competitive, loves and spreads easily into disturbed ecosystems, and doesn’t share or play well with others. It can be found as high as 5,000 feet (1,500 m) and is often found in pastures, wastelands, cultivated farmland, roadsides, lawns, forests, and any human-planted or disturbed environment. It grows well in clay soils and desert as well as your typical black humus and survives heavy rainfall as well as drought. The seeds (spinyhead) adhere well to clothing and animals, are picked up in mud on tires and shoes, hide in hay and grass bales, and germinate easily wherever they end up. They are very sharp and puncture the skin, and feet, with abandon.
Truly one of the great invasives.
Sida acuta can be grown in much of the United States and should be cultivated wherever it can be. It has been reported in Alabama, Florida, Georgia, Hawaii, Louisiana, Mississippi, New Jersey, Pennsylvania, South Carolina, Texas, Puerto Rico, and the U.S. Virgin Islands. Although it is said to grow most easily in zones 8 to 11, given that it grows in New Jersey and Pennsylvania, there is no reason it cannot grow throughout that region as well as in Northern California, Oregon, and the Olympic Peninsula and most likely other regions as well.
Sida cordifolia grows in Alabama, Hawaii, Florida, Texas, Puerto Rico, and the U.S. Virgin Islands.
Sida rhombifolia is widely distributed: Alabama, Arizona, Arkansas, California, Florida, Georgia, Hawaii, Kansas, Kentucky, Louisiana, Maryland, Mississippi, New Jersey, North Carolina, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, Puerto Rico, and the U.S. Virgin Islands.
Sida spinosa grows throughout those states and also in Connecticut, D.C., Delaware, Illinois, Indiana, Iowa, Maine, Massachusetts, Missouri, Nebraska, New York, Ohio, West Virginia, and Ontario, Canada.
Sida acuta is considered to be native to Mexico and Central America, but it has spread around the world with great abandon (the seeds are great hitchhikers—the Spanish colonizers in South America and Mexico took some with them everywhere they traveled). In Australia’s northern territories biological control has been instituted to try to stop its spread, with only mixed success.
This species is common in China, Japan, Taiwan, the Philippines, Malaysia, Singapore, Indonesia, Papua New Guinea, Fiji, Tonga, Tahiti—it’s common throughout the entire Pacific Rim and Pacific Islands, in fact—India, Sri Lanka, Thailand, Cambodia, Vietnam, Burkina Faso, Togo, Nigeria, Kenya, Peru, western Colombia, Panama, Honduras, El Salvador, Guatemala, Mexico, and other similar places and regions around the world. In most places where it has been introduced it is considered invasive and noxious and is often deeply disliked (the seeds, rather nasty, contribute to its poor reputation). It is considered a plant threat to Pacific ecosystems. However, in some regions (Florida) people grow it as an ornamental. Go figure.
Sida rhombifolia is even more widespread than S. acuta. It is invasive throughout the Pacific Rim and Islands, Australia, and New Zealand. It is widely found in China, Japan, Taiwan, Thailand, Cambodia, Vietnam, Malaysia, Indonesia, the Indian Ocean chain, Peru, Ecuador, Colombia, Costa Rica, Nicaragua, Honduras, El Salvador, Guatemala, and Mexico.
Sida cordifolia also grows widely throughout the Pacific Rim and Islands (invasive status) as well as in Japan, Taiwan, Australia, El Salvador, and Honduras.
Sida spinosa is invasive throughout the Pacific Rim and Islands and grows widely in Japan, Australia, Chile, Peru, and Mexico.
Sida acuta grows well from seed. In fact, its seeds are very hardy, with at least a 30 percent survival rate over several seasons of drought. Each plant produces several hundred seeds every year. They attach to any passing animal and drop off later to spread the plant even further. The seeds need a period of high temperature to break their seed coat and do best if there is a period of alternating high and low temperatures.
The seeds are collected in the fall and can be top-seeded where you want them to grow, with average watering.
Note: Sida acuta is as good at healing damaged land as it is ill people; it is exceptionally good at detoxifying polluted soils. It removes cadmium, lead, nickel, iron, zinc, cobalt, mercury, molybdenum, copper, manganese, arsenic, and chromium from industrially polluted or dump sites. It is particularly good at scavenging lead, zinc, iron, nickel, cadmium, chromium, molybdenum, and arsenic. The plant should not be harvested for medicine from such sites as it will contain high levels of heavy metals.
Sida acuta (and several others in the genus) is one of the few medicinals known besides Cryptolepis sanguinolenta to contain cryptolepine. This is one of the more potent constituents in the plant. The plant, like C. sanguinolenta, also generates a number of cryptolepine derivatives: quindoline, quindolinone, cryptolepinone, and 11-methoxy-quindoline.
Other constituents include ecdysterone, beta-sitosterol, stig-masterol, ampesterol, evofolin A and B, scopoletin, loliolide, 4-ketopinoresinol, ephedrine, beta-phenethylamine, quinazoline, carboxylated tryptamine alkaloids, alpha-amyrin, hentriacontane, hypolaetin-8-glucoside, campesterol, heraclenol, acanthoside B, daucoglycoside, choline, betaine, trans-feruloyltyramine, vomifoliol, ferulic acid, sinapic acid, syringic acid, syringaresinol, vanillic acid, swainsonine, vasicine, vasicinol, vasicinone, and peganine.
The seeds of both Sida acuta and Sida rhombifolia contain numerous ecdysteroids including ecdysone and 20-hydroxyecdysone. Sida filicaulis seeds contain lesser amounts. There is some indication that the plants, as opposed to the seeds, contain these compounds as well. This is the presumed source of the adaptogenic actions of the sidas when used as medicine. Sida acuta plants also contain alkaloids, flavonoids, steroids, tannins, cardenolides, polyphenols, terpenoids, and cardiac glycosides.
Sida acuta and Sida rhombifolia contain a number of cyclopropenoid fatty acids.
The same alkaloids present in Sida acuta have been found in Sida humilis, S. rhombifolia, and S. spinosa.
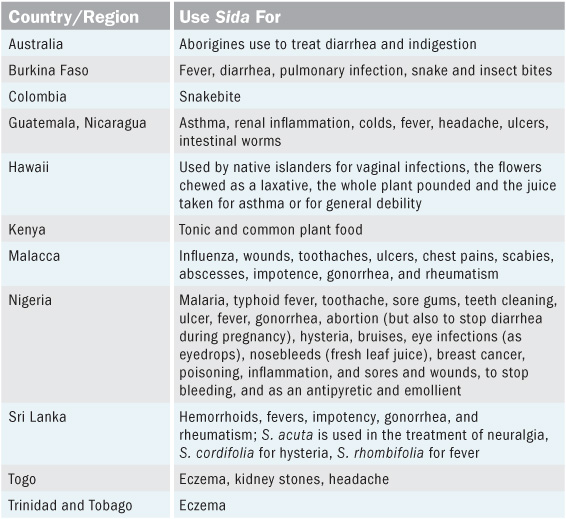
Sida acuta is widely used in traditional medicinal practice around the world to treat malaria, fevers, headache, skin diseases, infected wounds, diarrhea, dysentery, snake bites, asthma, GI tract problems, systemic infections. James Duke’s database lists 12 species of sida that have been used in traditional medicine, all for a similar range of complaints. The heaviest hits occurred with acuta, cordifolia, rhombifolia, and veronicaefolia. S. acuta and rhombifolia are sometimes smoked in Mexico for their euphoric effects.
Various sida species have been used in India for over five thousand years; some species are native, others were introduced from the Americas. The primary species used is Sida cordifolia, but all are common medicinals. Sida acuta is considered an invasive menace by some and listed as such in some government writings. Practitioners in India commonly use the various species interchangeably, which has led to calls for stricter identification of which sidas are being used and for what. Species commonly used are S. acuta, S. carpinifolia, S. cordifolia, S. humilis, S. indica, S. rhombifolia, and S. spinosa.
Bala is the primary term in Sanskrit for the main medicinal species—acuta and cordifolia—while lesser species are distinguished by a linguistic modification of that term: S. carpinifolia is bala phani-jivika, S. rhombifolia is atibala (or mahabala), S. spinosa is nagabala, S. humilis is bhumibala. However, every local ethnic group that uses the genus for medicine has its own local name for the plants. There are scores of them. The plants, again, are considered to be interchangeable for the most part in practice; the roots, leaves, seeds, and stems are all used.
Sida cordifolia is considered to be cooling, astringent, stomachic, tonic, aromatic, bitter, febrifuge, demulcent, diuretic. The seeds are used as an aphrodisiac and to treat gonorrhea, cystitis, hemorrhoids, colic, and tenesmus. The leaves are used for strangury, hematuria, gonorrhea, cystitis, leukorrhea, chronic dysentery, nervous diseases, facial paralysis, and asthma, and as a cardiac tonic. They are cooked with rice and used for bloody diarrhea and bleeding hemorrhoids. An infusion of the roots is effective for nervous and urinary diseases and disorders of the blood and liver, while a decoction of the root (with ginger) is used for fever accompanied by cold shivering fits (essentially malarial fevers). The root juice is good for wounds, and an infusion of the dried root for bloody diarrhea, dandruff, and scalp problems. The juice of the plant is used for spermatorrhoea, rheumatism, and gonorrhea. All parts of the plant are used as a stomachic and cardiac tonic.
Sida acuta is used as a diaphoretic and antipyretic and to treat fevers, dyspepsia, and lingering debility from previous illnesses. The juice of the root is used for intestinal worms, an infusion of the root for intermittent fever and chronic bowel complaints and for asthma, and the powdered root is made into a paste and applied to boils and abscesses. The leaves are used as a demulcent and diuretic and to treat chronic diarrhea and dysentery, rheumatic conditions, and gonorrhea. It is a common food plant in some districts.
Sida rhombifolia is used as a diuretic and aphrodisiac and to treat hemorrhoids, gonorrhea, rheumatism, kidney stones, fever, and scorpion sting. An infusion of the root is used for asthma.
Sida spinosa is used for cooling fevers (as a decoction, 2x daily) and to treat gonorrhea, gleet, scalding urine, debility. It was used as a primary trauma medicine in Chhattisgarh, India, during the wars of the twentieth century. The leaf juice was used to stop bleeding, decrease pain, prevent infection, and hasten healing time.
Other Ayurvedic uses of sida include the treatment of eye problems (infections), sinusitis, cramps, joint pain, fracture, swelling, Parkinson’s disease, colic, whooping cough, uterine problems, vaginal infection, bronchitis, TB, emaciation, and cystitis. All the sidas are used as veterinary medicine for treating diarrhea in farm animals throughout India.
Sida acuta—huanghuaren or huang hu aren—is used in Chinese medicine, as is Sida rhombifolia—huan hua mu—and presumably other sidas as well. I can find little on the plants even though they seem to have a longish history of use there. The plants are usually used as decoctions, with a dosage range of up to 30 grams, or about 1 ounce. The Chinese consider sida to clear heat and benefit dampness. They have found it to be antibiotic, anti-inflammatory, analgesic, diuretic, and tonic.
Sidas are commonly used for depression, bronchitis with cough and wheezing, and urinary tract inflammations. Less common uses are for dermatosis, itching, eczema of the scrotum, sores and boils, stomach pain, dysentery, gastritis, enteritis, tonsillitis, liver problems, jaundice, cervical tuberculous lymphadenitis, malaria, colds and flu, and kidney stones.
Sida (S. rhombifolia primarily) was apparently introduced into the United States in the nineteenth century as a fiber plant, but it wasn’t much used as a medicinal. The Eclectics listed it in a tiny reference under Althea, a.k.a. marsh mallow, as being highly mucilaginous, useful as a poultice, and effective for respiratory complaints.
The recent focus on cryptolepine-containing plants as well as traditional malarial plants has stimulated a lot of interest in Sida acuta and some of the more commonly used Asian sidas. Most of the scientific studies have focused on phytochemical analysis and in vitro studies of the plants’ antimicrobial actions, with a smattering of in vivo studies. The scientific exploration of these plants is still in its infancy and no clinical trials have been conducted that I am aware of.
There have been a number of studies of the antimicrobial activity of Sida acuta, and while they do give a good indication of its potency, nearly all the studies are flawed. Inexplicably, very few of the researchers appeared aware of the importance of proper preparation of the plant extracts. Looking only at the ethanol and water extract preparations in the studies, the problems are twofold. First, they tended to use 90 percent to 95 percent pure alcohol to make the ethanol extracts. This means that only the alcohol-soluble constituents would be present in the extract. (There would be a tiny amount of water-soluble constituents from the 5 percent to 10 percent water that was present in the alcohol.) Many of the most potent constituents in the plant, such as cryptolepine, are only water soluble, so the preparation method will affect the impact of the extract on microorganisms.
Second, when making the water-based extracts many of the researchers used a neutral-pH distilled water. Additionally, some made it as a cold maceration. This is problematical for several reasons. Firstly, the alkaloids in the plant, most importantly cryptolepine and its derivatives, are primarily soluble in water that is somewhat acidic. Secondly, the plant constituents are less soluble in cold water than in hot. For the studies to be truly relevant, the water extracts should have used water with a pH of from 1 to 6 to make sure they were acidic enough to extract the alkaloids and the water should have been hot. With the ethanol extracts, preparation should have been made using half water and half pure grain alcohol; the water should have been hot, the herb inserted, the mixture allowed to cool, and then the alcohol added. The differences in preparation techniques are the most likely reason that the antimicrobial actions of the plant vary as much as they do from study to study.
Nevertheless, in all studies Sida acuta has been shown to be potently active against malarial parasites, staph bacteria, and TB, though beyond that there is a lot of variance. The best study took these factors into account but was exploring only alkaloid activity.2 That study found more activity from the alkaloids against Gram-negative bacteria than previous research, which makes sense, as cryptolepis has been found to be active against Gram-negative bacteria simply due to the presence of cryptolepine and its derivatives. In fact the alkaloidal extract of Sida acuta was nearly as effective against Gram-negative as Gram-positive bacteria.
A close examination does indicate, however, that both cryptolepis and sida more easily kill Gram-positive organisms than Gram-negative. This does not mean they are not active, it simply means that the dose needs to be higher if you are dealing with Gram-negative organisms, an observation confirmed by studies on both plants. The plant should also be taken for a longer duration—the Gram-negative bacteria did need a longer exposure to the herb than the Gram-positive. The use of a synergist that enhances antibacterial activity against Gram-negative bacteria would be helpful. (See piperine monograph, page 236.)
In spite of the problems in the in vitro studies, tests for antimicrobial activity have borne out the traditional uses of the plants against microbial diseases. They have found sida strongly active against Plasmodium spp., Staphylococcus aureus, and Mycobacterium phlei, resistant and nonresistant strains. It is highly active against Streptococcus pyogenes, E. coli, Bacillus subtilis, Pasteurella multicocida, and Salmonella typhimurium. It is also active against herpes simplex, Shigella boydii, S. flexneri, S. dysentariae, and Listeria innocua and less active against Pseudomonas aeruginosa, Candida spp., Aspergillus niger, and A. fumigatus, but still effective, especially if the dosage is increased. In many instances the plant was more effective against the bacterial strains than pharmaceutical antibiotics.
Sida increases glutathione levels in the blood, increases red blood cell numbers (making it good for treating anemia), and increases total white blood cell count, indicating an immune potentiation effect that may tie in with its reported adaptogenic actions in traditional practice.
In vivo studies have found Sida acuta to have a strong and reliable antiulcerative effect; that is, it protects the stomach lining from the formation of induced ulcers. In vivo research has also found a strong analgesic action.
Another in vivo study found sida hepatoprotective against induced liver damage (the plant is used in India for liver disease among other things). Several compounds from the plant have been found to inhibit induced preneoplastic lesions in mouse mammary tissue. In vivo studies have also found sida to be hypoglycemic, lowering blood sugar concentrations in diabetic mice, and to be antihyperlipidemic, lowering blood cholesterol and triglyceride levels, again in diabetic mice.
An analysis of four sidas—S. acuta, humilis, rhombifolia, and spinosa—found them to have similar alkaloidal constituents, including cryptolepine.
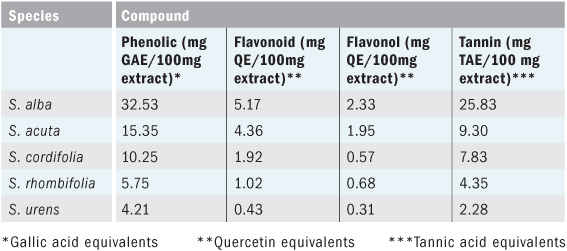
An analysis of five sidas—S. acuta, alba (a synonym of spinosa), cordifolia, rhombifolia, and urens—found varying levels of polyphenols in the plants (see chart at bottom of page).
The antioxidant activity of the plants followed that order as well, with Sida alba having the highest, S. urens the lowest. The plants were tested for anti-inflammatory activity, exploring their lipoxygenase (LOX) and xanthine oxidase (XOX) inhibition. For LOX, alba inhibited 80 percent, acuta 79 percent, cordifolia 21 percent, rhombifolia 52 percent, urens 47 percent; for XOX alba inhibited 47 percent, acuta 43 percent, cordifolia 13 percent, rhombifolia 46 percent, urens 35 percent.
All these species of sida are successfully used to treat liver diseases including hepatitis B in Burkina Faso; the authors of the study were exploring some of the mechanisms that might explain their effectiveness.
Sida alba (i.e., S. spinosa) is fairly high in ecdysteroids, which are adaptogenic and explain, in part, the plant’s use for debility in traditional practice.
Numerous studies have found Sida cordifolia to possess very potent anti-inflammatory and analgesic activities. An alkaloid with a tremendously long name, one of the quinazoles—a group of which cryptolepine is a member—was found to be the most potent source of the activity. In vivo studies: An aqueous extract of cordifolia stimulated liver regeneration in 67 percent partial hepatectomy in rats; birds treated with cyclophosphamide, which causes immunosuppression, experienced a reversal of that condition when given cordifolia. In vitro studies: The plant is strongly antimicrobial and acts as an antistressor/adaptogenic in stressed mice; use of the plant after myocardial injury showed significantly increased endogenous antioxidants in heart tissue; other studies found evidence of a protection from neurotoxicity caused by quinolinic acid.
Sida tiagii during in vivo research has been found to have antidepressant and antiseizure effects in mice.
Family: Euphorbiaceae
Common Name: Christmas bush
Species Used: The genus Alchornea is a pan-tropical group of plants comprising some 60 species, six of which are indigenous to Africa. Alchornea cordifolia is the main medicinal species, though A. laxiflora is a reliable substitute. Regrettably, there has been little study on the members of this genus other than A. cordifolia.
Mostly the leaves, but the stem bark, pith, root bark, roots, and fruits are all used.
Add 7 ounces of herb to 1 quart of water and boil for 20 minutes. Strain, then drink 6–8 ounces of the tea every 4 hours. Studies have shown that the tea takes about 3 hours to begin getting into the blood, and it tends to hit peak presence 1 to 2 hours after that depending on the dose; dosage presence lasts about 4 hours. This means that if you are using the tea you need to have another cup every 4 hours or so. Recommended dosage times: 8 A.M., 12 P.M., 4 P.M., 8 P.M., or beginning whenever you rise and then going to a 4-hour period.
For eye disease: Use the cool tea as eyedrops, 1–3 drops every 3–4 hours.
1:5, 50 percent alcohol, 50 percent water; take ¼ teaspoon of the tincture every 4 hours
For wounds and infected skin, liberally sprinkle the powder on the site as frequently as needed.
None noted, and no toxicity has been found. There are no reports in the literature or by traditional practitioners of side effects, although large doses may have a sedative or depressant effect on the central nervous system.
None noted; however, large doses should not be taken along with CNS depressants or sedatives.
Note: Some people indicate that Alchornea castaneifolia can be used interchangeably but I can’t see this as accurate—I would never recommend using it interchangeably. See Beware of A. castaneifolia, opposite page.
Alchornea cordifolia is a common plant throughout much of the largish middle of Africa, from Senegal to Kenya and Tanzania and from just north of South Africa to Angola. It’s a straggly shrub or small tree up to 25 feet in height. It is widespread in secondary forest and likes riparian habitat and marshy areas but does spread into drier ecosystems, especially in disturbed soils. It will grow in terrain up to 5,000 feet (1,524 m) in altitude. It likes acid soils and is an active soil modulator, restoring calcium levels to depleted soils. Alchornea laxiflora grows in the same regions and has virtually the same appearance.
Propagates well from cuttings; they root solidly in a few months. The seeds are considered to be difficult germinators, needing to be scarified and tended diligently. Germination takes up to 3 months.
The plant can be harvested at any time. The leaves are taken when healthy and vital in appearance. The plant is normally wildcrafted as it is widespread and vigorous once established. It is not yet an agricultural crop.
Actions
Amoebicidal
Anthelmintic
Antiamoebic
Antianemic
Antibacterial
Antidiarrheal
Antidrepanocytary
Antifungal
Anti-inflammatory
Antimalarial
Antimicrobial
Antioxidant
Antiprotozoal
Antiseptic
Antitumor
Antiviral
Bronchial relaxant
Smooth muscle tissue relaxant
Trypanocidal
Active Against
Aspergillus spp.
Babesia spp.
Bacillus subtilis
Candida albicans
Entamoeba histolytica
Escherichia coli
Helicobacter pylori
Klebsiella pneumoniae
Plasmodium spp.
Proteus mirabilis
Proteus vulgaris
Pseudomonas aeruginosa
Salmonella enteritidis
Salmonella typhi
Shigella flexneri
Staphylococcus aureus
Streptococcus pyogenes
Use to Treat
Malaria, systemic staph infections, pseudomonas, anemia, fevers, infections from Streptococcus pyogenes, and diarrhea and dysentery from such things as severe E. coli, Salmonella, Entamoeba, Shigella, or amoebic organisms. Generally, resistant Gram-positive and Gram-negative infections, systemic or of the GI tract. Infected wounds. Sickle cell anemia, sleeping sickness, resistant respiratory infections, conjunctivitis (as an eyewash), UTIs.
Other Uses
Alchornea is a potent alley-cropping plant and soil restorer: Rows of the trees are planted as windbreaks to protect other crops while returning calcium to depleted soils. The fruits produce a black dye traditionally used for fishing nets, cloth, pottery, and leather. The wood is used for construction and crafts.
It coppices well and is very hard to get rid of once established.
A. cordifolia contains the usual terpenes, sterols, flavonoids, tannins, carbohydrates, glycosides, saponins, and alkaloids. It also has alchorneine, alchornine, and alchornidine (all are imidazopyrimidine alkaloids), several guanidine alkaloids, allic acid, gentisic acid, anthranilic acid, protocatechuic acid, ellagic acid, hyperoside, various quercitrins, daucosterol, acetyl aleuritolic acid, beta-sitosterol, epoxy fatty acids (in the seeds, lots), and a lot of other stuff no one has discovered yet.
A. cordifolia is widely used throughout every region of Africa in which it grows. It is used as a wash for eye infections and powdered for ringworm and other skin infections. It is an anti-inflammatory, a carminative, an anodyne, a diuretic, an emmenagogue, a blood purifier, and a tonic and has antitumor actions. See chart on next page for a comprehensive list of traditional uses.
Not known as far as I can tell.
Not known as far as I can tell.
Not known as far as I can tell, though some species have been used for a long time in South American indigenous practice. They don’t seem to be similar in action to the two African species discussed here.
In vitro studies have found Alchornea cordifolia active against 15 MRSA isolates and to be strongly active against Pseudomonas aeruginosa. Low concentrations of the herb are active against E. coli, P. aeruginosa, Staphylococcus aureus; it is as or more active than pharmaceutical antibiotics such as gentamicin and ampicillin. In vivo studies have confirmed the MRSA action in mice. A 50 percent ethanol extract (normal tincture) of alchornea was tested against 74 microbial strains: aerobic, facultative, anaerobic, and fungi. It was active at low concentrations against all except three strains, all filamentous fungi. Like most systemic antibacterial herbs, it was a bit stronger against Gram-positive strains than Gram-negative. It has been found to be active against Helicobacter pylori, Salmonella typhi, Shigella flexneri, Salmonella enteritidis, and enterohemorrhagic E. coli (EHEC), bearing out its traditional uses for treating dysentery and diarrheagenic bacterial pathogens. Ethanolic and water extracts have been found to be equally active except that only the ethanolic extract was active against EHEC. Other studies have found the ethanolic extract reliably effective in vitro for E. coli, Pseudomonas aeruginosa, Staphylococcus aureus, Klebsiella pneumoniae, Proteus mirabilis—at the proper dosage, it is as effective as ciprofloxacin.
In vitro screening of 45 Congolese medicinal plants found alchornea to be highly antiamoebic, with strong activity against Entamoeba histolytica. Other studies have confirmed this, including finding a strong spasmolytic action. The plant exhibited a more than 70 percent reduction of spasms in guinea pig ilea.
A. cordifolia has been found to produce its activity in the treatment of dysentery and diarrheal diseases through three mechanisms: antibacterial, antiamoebic, and antispasmodic actions that are apparently synergistic. In vivo study has found the plant to be highly antidiarrheal against castor-oil-induced diarrhea in mice.
Given the traditional use of alchornea for treating malaria across Africa, it is odd that only two in vitro studies have been conducted on its activity against Plasmodium falciparum. One study found it potently active, the second mildly so. A. cordifolia is fairly high in ellagic acid, which has been found to be strongly active, in vivo and in vitro, against the malarial parasites. The former study also found it strongly active against Trypanosoma brucei. (A. cordifolia is used in ethnoveterinary practice to treat that disease, and studies have found it active against both resistant and nonresistant forms.)
Like a number of plants in this chapter, Alchornea appears to be hemotonic, a hemoregenerator, and hemoprotectant, but the research has not focused that broadly. It does have a long history of use against anemia, malaria, and sickle cell anemia, as well as for trypanosomiasis (a.k.a. African sleeping sickness), which is also a parasitic disease of the bloodstream, similar in some respects to malaria and babesia.
The research on Alchornea laxiflora is limited, but both its traditional use and the studies that exist seem to confirm that its actions are very similar to those of A. cordifolia. It grows in the same eco-ranges and is considered interchangeable by the traditional practitioners. In vitro studies have found that the plant has anticonvulsant and sedative actions (in vivo studies have found this action in A. cordifolia as well) and is strongly anti-oxidant, anti-inflammatory, antimicrobial, and antibacterial against both Gram-positive and Gram-negative bacteria. The chemistry of the two plants is very similar.
One study found A. laxiflora strongly active against HIV-1 and HIV-2 in vitro, more so than AZT. Another found the plant to possess immune modulatory and stimulant actions. It generates a lymphoproliferative effect on naive murine splenocytes and thymocytes and modulates the effects of the phagocytic and lysomal enzyme activities of murine macrophages. It increases phagocytosis and intracellular killing capacity. Lysosomal phosphatase activity of peritoneal macrophages increased significantly.
Of 42 plants tested in one study, Alchornea cordifolia was found to have the most potent antioxidant effects. In vitro study found that the plant was highly protective of rat liver against hepatotoxins. In vivo study in mice found the same.
A number of in vivo studies have found the plant to be strongly anti-inflammatory and very effective in the treatment of induced edema in rats. In vitro studies have found Alchornea cordifolia strongly anti-inflammatory by inhibiting human neutrophil elastase and superoxide anion.
Histological changes occur in rat pancreas after use of an ethanolic extract of the plant—28 days of use resulted in regenerative alterations. Islet cells in the pancreas of rats with induced type 1 diabetes regenerated. Quiescent cells proliferated and replaced lost cells. The plant also decreased blood glucose levels and increased B-cell levels in other studies.
The plant is used as an antiasthmatic in Ghana, and an in vivo study found it to act similarly to isoprenaline, which is sometimes used in bronchial inhalers for asthma. Another study found the plant to have a marked effect on the aorta of Wistar rats, essentially inducing elastogenesis.
Family: Asteraceae (Compositae)
Common Names: Spanish needles, beggarticks, demon spike grass, needle grass, *$%#*%!, and a lot of other names in hundreds of languages. It appears to grow everywhere and people either hate it or loathe it or both. They certainly do name it.
Species Used: There are 200 species in the Bidens genus. Maybe. Anal-retentive phytospecific maniacs are continually messing about with which species belong in the genus and, as usual, making problems for everyone. In consequence, the taxonomy of Bidens is considered “unsatisfactory,” which is a massive understatement.
Bidens pilosa is the main species used medicinally (or at least on which most of the studies have been done), but there do seem to be a number of others in the genus that historical use and early research indicate can almost certainly be used similarly: B. frondosa, B. tripartitus, B. ferulaefolia, B. alba are all fairly potent, frondosa and tripartitus more so than pilosa in their antimalarial effects. B. maximovicziana, B. pinnata, and B. campylotheca are all fairly strong as well but, in terms of impact on the malarial organism, a bit less strong than pilosa.
Note: Bidens leucantha is a synonym for B. pilosa.
Usually the aerial parts, but the entire plant is active, and in some instances the roots seem to be a bit stronger as a medicinal. Normally, however, the leaves tend to be the most potent part of the plant, followed by the roots. The fresh leaves are often used and a number of studies show the fresh leaves and juice of the plant to be the most antimicrobial. Drying the plant reduces its antimicrobial action considerably.
There are some important things to know about using and preparing bidens:
• The most potent forms of this herb are alcohol tinctures and the fresh juice.
• The most potent constituents are considerably more soluble in alcohol than in water. Water infusions have a decent range of potency (as can be seen from the plant’s traditional uses as a tea in Africa) but are not nearly as effective as a cold alcohol/water maceration.
• Some of the plant’s most potent constituents oxidize easily and begin to degrade as soon as the plant is dried. Heat also destroys them.
• Expect about a two-thirds reduction in antimicrobial activity if the plant is not prepared fresh.
• The older the dried plant is, the less potent it will be in either water or alcohol. The fresher the dried plant material, the better.
• Water infusions lose potency fairly rapidly; they should be made and used daily. The rapidity of degradation of the plant chemicals is, in part, why so many cultures that don’t normally make alcohol tinctures resort to using the juice of the leaves of this plant, internally and externally, for disease.
• Water extractions of the plant (teas, infusions, decoctions), especially if it is dried, possess about half the antibacterial activity of an alcohol tincture (depending on how old the extractions are), but they do possess most or all of the other actions described in this material (anti-inflammatory, antiallergenic, immune-modulating, and so on), especially the anti-inflammatory and antipyretic actions.
• A tincture is the strongest form of the herb as medicine. The use of piperine as a synergist will increase the potency of the plant considerably.
Fresh plant, 1:2, 95 percent alcohol, 45–90 drops in water, up to 4x daily. Tincture made from the dried plant, if you must, would be 1:5, 50 percent alcohol, triple the dose.
For acute conditions (malaria, systemic staph):¼–1 tsp and up to 1 tbl in water, up to 6x daily for up to 28 days, depending on severity. The tincture can also be used topically on infected wounds.
Possible, but not really recommended.
Tea: 1 teaspoon herb in 8 ounces hot water; let steep 15 minutes. Drink 2–4 cups daily.
Decoction: Not recommended; heat degrades the herb. But if you must: For external use, boil 1 ounce herb in 1 quart water for 20 minutes, then strain. Cool and use on skin inflammations. For internal use, boil 2–4 ounces herb in 1 quart water for 20 minutes, then strain. Drink by the cup 2–4x daily.
Cold infusion: Steep 2–4 ounces herb in 1 quart cold water overnight. Drink by the cup 2–4x daily.
You can run the leaves through a juicer to obtain a decent quantity of the fresh juice—the plants are pretty prolific. Be aware that they have strong fibers that will bind the juicer and you’ll have to clean it often. Use the juice on infected wounds, for eye infections, or internally for systemic infections. If you want, you can stabilize the juice with the addition of 20 percent alcohol so that it will keep (see page 227). It can then be taken internally much like the tincture, though it will be more potent in its actions. Dosages are similar to those listed for the tincture.
Actions
Antibacterial
Antidiabetic
Antidysenteric
Anti-inflammatory
Antimalarial
Antimicrobial
Antiseptic
Astringent
Blood tonic
Carminative
Diuretic
Galactagogue
Hepatoprotective
Hypoglycemic
Hypotensive
Immunomodulant
Mucous membrane tonic
Neuroprotectant
Prostaglandin synthesis inhibitor
Styptic
Vulnerary
Active Against
Bacillus cereus
Bacillus subtilis
Candida albicans
Human cytomegalovirus
Entamoeba histolytica
Enterococcus faecalis (Streptococcus faecalis)
Escherichia coli
Herpes simplex 1 and 2
Klebsiella pneumoniae
Leishmania amazonensis
Mycobacterium tuberculosis
Neisseria gonorrhoeae
Plasmodium spp.
Pseudomonas aeruginosa
Salmonella spp.
Serratia marcescens
Shigella flexneri
Staphylococcus aureus
Staphylococcus epidermidis
Bidens is not very active against Aspergillus.
Like a lot of studies for antimicrobial activity, a number of those on Bidens are contradictory. For every study that finds it active against E. coli, another says it is not. Same for Pseudomonas, Klebsiella, Streptococcus, and Candida. Some studies show very strong activity, others mild, others none at all.
The differences come from the time of year the plant was gathered, the ecosystem in which it was found, whether wild or domesticated plants were used (wild plants have been found to be much stronger antibacterials), and differences in how the plants were prepared—the main problem being preparation. (See Preparation and Dosage, page 128.)
For this plant to act as a potent antimicrobial, it must be prepared as a tincture of the fresh plant or the fresh juice must be used.
In order of potency:
1) Any systemic infections that are accompanied by problems in the mucous membranes anywhere in the body, especially chronic diarrhea, dysentery, UTI, vaginitis, and inflamed respiratory passages
2) Systemic staph
3) Malaria, babesia, leishmania
4) Any of the other resistant organisms bidens is active against
Other Uses
As a pot herb. The plant comes up early in the spring, is very hardy, and is used by many cultures as a food staple. However, see Side Effects and Contraindications (page 132) for a caveat on the plant as food.
None noted; however, be aware that Bidens pilosa’s leaves have numerous sharply pointed microhairs around the margins that are very high in silica. This kind of silica formation has been linked to esophageal cancer in certain domesticated animals (cows) and humans. Tribal cultures that eat large quantities of the plant as a primary food source show increased levels of that type of cancer. Cultures that use the plant only sporadically for food do not have an increased incidence of cancer. Exercise caution if using bidens as a food plant; it appears fine for occasional use but not as a steady diet.
Note: Bidens pilosa is a toxic-waste reclamation plant. Unless you want more heavy metals in your body, be careful where you get the plant. It should not be harvested from sites where there is heavy metal contamination. Numerous studies have found it to be a potent phyto-remediation plant for cadmium and one study showed the same for arsenic; another indicates it may have an affinity for heavy metals in general.
None noted, although one study does show it potentiating tetracycline.
Caution should be exercised when using the plant with people on diabetic medications as it will alter blood glucose and insulin levels.
A native of South America, Bidens pilosa is a world-class invasive species. Spread by the Spanish during colonization, it is now widespread seemingly everywhere. If it does not currently grow someplace, it eventually will.
Bidens grows from sea level to 10,000 feet (3,600 m) in altitude. It tolerates moist soil, sand, clay, lime rock, infertile soil, drylands. It thrives best in high sunlight, dry soils, and disturbed areas but has been found in nearly every type of eco-range on the planet. It can withstand long periods of drought and survives temperatures as low as 5°F (–15°C). It isn’t fire tolerant but rapidly invades burned areas and is quite happy about any opportunity to do so.
It loves the southern and southwestern United States and has spread up the West and East Coasts into eastern Canada.
It is found throughout the Caribbean, Central America, South America, Europe, Russia, China, most of Africa, Southeast Asia, southern India, Japan, the Pacific Islands, and Australia. It may not grow in Ulan Bator or Nebraska, but then again, it may.
At its initial appearance in spring, bidens is quite a beautiful ground-coverish sort of plant, but as the season develops and it grows taller, it develops a rather straggly, weedy appearance. The flowers are the usual white, five-petaled things with an orange interior. The seeds are longish, thin, black needles with a sharp, extended pronged tip. There are often three or four prongs in spite of the fact that Bidens means “two-toothed” (bi means two and dens—as in dental—being tooth). The seeds can attach themselves to about anything, hence the name beggarticks. If you walk through a patch of bidens during seeding season, your shoelaces and pants to the knees will be covered with hundreds of the hard-to-remove seeds—a thousand seeds weigh only about 1 gram. They take hours to pick out, hence the name *$%#*%!
The plant loves disturbed places, especially agriculturally disturbed fields, and actively tries to colonize cultivated land. It is allelopathic (toxic to other plants) and can reduce domesticated crops up to 50 percent once it invades a planted field. It is considered highly noxious in scores of countries just for that reason. The plant has very few natural predators.
I like it.
Bidens grows best from sea level to 10,000 feet (3,600 m) within a temperature range of 75°–90°F (25°–30°C) during the growing season. The edges of its growing temperature are from about 55° to 115°F (15° to 45°C).
Bidens grows easily from seed and is a tenacious grower. The seeds can still be viable after 3 years. The plant grows very fast, flowering as few as 6 weeks after its emergence from the ground. The first seeds mature just 4 weeks after flowering. Each plant produces a minimum of three thousand seeds a year and in some climates will reproduce four times before dying back.
The seed germinates best if buried about 4 cm in the soil; deeper than 6 cm and it won’t germinate at all. Soaking the seed in water prior to planting increases germination rate and numbers. The seed can be broadcast or sown in rows.
The plant is an annual and can be harvested within 4 to 6 weeks of its emergence in the spring; it is generally considered to be harvestable until it sets seed (unless of course you are interested in making medicine from the seeds). The older the leaves, the more bitter and astringent they become. If you are using it for its astringency, gather late in the year. If you are gathering it for food, get it early in the year.
If you are growing it as a medicinal, remove the flowers to retard old age and stimulate leaf growth. The leaves can be harvested throughout the year as long as you don’t allow the plants to go to seed early on. If the plants are topped, you can get up to six harvests a year depending on your climate.
If you must dry bidens, do so out of the sun. And collect a lot of it, as it dries to almost nothing; a big bag of the fresh plant will give you a handful of dried powder. The plant will oxidize, so keep it in paper bags or, if well dried, in plastic, inside a plastic bin out of the sun. Replace every year or two, depending on how you store it. But ideally it should be used fresh.
A great deal of research has found that the plant leaves if used fresh or tinctured fresh possess significantly stronger antimicrobial activity than if dried. The herb’s ability to inhibit malarial parasites drops from 90 percent in the fresh leaf tincture to 38 percent in the dried (in vivo studies). If you are using the plant as an antimicrobial for resistant pathogens, harvest the leaves before flowering and tincture them fresh.
If you do grow bidens intentionally, you may irritate your neighbors. Nevertheless, its ease of growth, widespread habitat, and medicinal nature make it an essential herb to know, grow, and use for the treatment of resistant pathogens.
There has been a lot of work on the constituents of Bidens pilosa, and around 100 different plant chemicals have been identified so far. There are numerous aurone flavonoids, butoxy lipids, coumaric acids, and erythronic acid phenylpropanoids, a number of heptaphenyl and phenylheptatriyne benzenoids, a lot of okanin flavonoids, numerous stigmasterol steroids, a lot of quercetin flavonols, daucosterol, and a whole lot more. A very comprehensive plant in terms of flavonoids, terpenes, phenylpropanoids, lipids, and benzenoids.
The most active constituents are thought to be the polyacetylene compounds and the flavonoids. The acetylenes have shown the broadest-spectrum antimicrobial activity.
The plant is one of the great easily available systemic antibacterial herbs. It does not appear to have as wide a range of action as Sida or Cryptolepis and is definitely not as strong. But it is reliable for the treatment of a number of resistant bacterial infections and is very simple to use. Because it grows so easily and is so prevalent in so many countries, it is a crucial herb to know about as resistant organisms extend their reach.
Wherever the plant grows it is often used by the local peoples for similar problems: to treat mouth and stomach ulcers, headaches, ear infections, hangovers, diarrhea, kidney problems, malaria, jaundice, dysentery, burns, arthritis, ulcers, abdominal problems, swollen spleen, coughs, colds and flu, rheumatism, boils, diabetes, skin rashes, and infected wounds. It is also used as an anesthetic, a coagulant, a poison antidote (especially for snakebite), and to ease childbirth.
Bidens pilosa grows primarily in the south of India, where it is known as ottrancedi. It is frequently used for glandular sclerosis, wounds, colds, flu, acute or chronic hepatitis, and urinary tract infections. Another species, Bidens trifada, is used for chronic dysentery, eczema, skin problems, ulcers, headache, earache and ear problems, toothache, cough, inflammation, and leprosy.
Called xian feng cao (abundant weed), gui zhen cao (demon needle grass), or nian shen cao (I don’t know but probably unflattering) by the locals, all parts of the plant are used to clear heat and toxins. Dosage runs from 15 to 60 grams (½ to 2 ounces) per day, or as high as 120 grams (4 ounces) in acute conditions such as appendicitis.
It is used for treating cardiac spasm, itching, gastroenteritis, appendicitis, colitis, irritable bowel syndrome, hemorrhoids, diarrhea, dysentery, difficulty swallowing, sore throat, tonsillitis, esophageal enlargement, jaundice, acute or chronic hepatitis, malaria, boils, abscesses, infections, fever, chills, joint pain, traumatic injury, sprains, swelling, contusions, rheumatoid arthritis, gastric and esophageal cancer, epilepsy in children, infantile fever with convulsions, malnutrition in infants, colds and flu, bronchitis, chest congestion, hemoptysis, allergies, lung irritation, pneumonia, insect bites, scorpion sting, and snakebites.
Herbalists in the United States have consistently failed to understand this species, generally listing it as of little importance and having only minimal medicinal uses. The Eclectics knew it but used it little, primarily as an emmenagogue and expectorant, for amenorrhea, dysmenorrhea, uterine problems, severe cough, asthma, and as an infusion. An infusion of the seeds sweetened with honey was used for whooping cough. The plant was thought useful for heart conditions including palpitation, for colds, and for acute bronchial and laryngeal attacks.
The Seminole tribe used bidens similarly, as did the native Hawaiians. Numerous tribes used it as a pot herb.
Michael Moore was the first contemporary herbalist to begin to understand its actions and he wrote about it extensively in the early 1990s. He didn’t explore its antimicrobial activity but rather focused on its potency as a mucous membrane tonic. In his words, bidens “is probably the best herbal therapy we have for irritation, inflammation, pain, and bleeding of the urinary tract mucosa.”3
The plant is a mucous membrane tonic and not only stops the inflammation and acts as a potent antibacterial in UTI infections but also heals the mucous membranes themselves. Moore felt it good for recurrent UTI infections and inflammations that didn’t respond to antibiotics. The pain will usually go away in a day or two if you use bidens; he recommends using it an additional few days to completely clear up the problem.
Moore also considered bidens specific for reducing elevated levels of uric acid in the blood; i.e., for treating gout or urate-based kidney stones. It is a decent diuretic and does in fact stimulate uric acid elimination in the urine.
Because it is a mucous membrane tonic and is astringent, powerfully anti-inflammatory, and strongly antibacterial, it is specific for a number of troublesome diseases caused by resistant pathogens: UTIs, chronic diarrhea and dysentery, gastritis and ulcers (anywhere in GI tract, from mouth to anus), inflamed mucous membranes in colds and flu and respiratory infections of any sort, sore throats from coughs or infection or even overuse of the throat, and vaginal infections.
Moore notes that bidens has the “ability to tighten, shrink, and tonify the structural cells of the mucus membranes, thereby preventing congestion and edema, while simultaneously increasing the circulation, metabolism, and healing energy of the functional cells of those tissues.”4
It’s a good plant, too often overlooked.
Bidens pilosa is highly active against the malaria parasite in in vivo and in vitro studies, bearing out its traditional use for that disease. The linear polyacetylenic diol extracted from bidens was found to be highly active against the malarial parasite in vivo and in vitro, especially in the fresh plant. The constituent is unstable in the dried state.
It is generally felt that the polyacetylenes in the plant are the most active constituents, the most potent antimicrobials. The research seems to bear this out. Alcohol tinctures of the fresh plant showed a 90 percent inhibition of the malarial parasite in vivo, while dried plant tinctures ran about 65 percent and water extracts about 38 percent. That activity is the same whether resistant or nonresistant strains are tested. In comparison, chloroquine-susceptible strains, when treated with chloroquine, will show a 99.2 percent inhibition of the malarial parasite. So the plant is nearly as strong as the pharmaceutical but not quite. It is definitely not as potent a plant as sida or cryptolepis, so larger doses need to be taken and for longer if you are using this plant for malaria.
An interesting in vivo study comparing the effectiveness of wild bidens versus domesticated found the wild species to be consistently stronger in its actions (the domesticated worked, just not as well).
As noted earlier, bidens possesses good antibacterial activity, as many antimalarials do. It has been found active against a wide range of microbial organisms, but some of the results are contradictory. (See Active Against, page 130, for more depth.)
Several of the plant’s isolated polyacetylenes were found to be more active than ampicillin, tetracycline, norfloxacin, and amphotericin B during in vitro studies. Ciprofloxacin and ofloxacin were more potent than the plant extracts. In one study, water extracts of the plant were found to be more effective against E. coli and Bacillus cereus than gentamicin.
Bidens has been found to potentiate the activity of tetracycline if taken along with that pharmaceutical.
It is effective against herpes simplex 1 and 2 in in vitro studies, being nearly as strong as acyclovir but without the side effects.
Bidens pilosa during in vitro testing was found more active than metronidazole in the treatment of Entamoeba histolytica, a cause of amoebic dysentery around the world. The organisms weren’t completely inhibited but were significantly reduced in number. B. pilosa was also found to be highly active in the treatment of the parasite Leishmania amazonensis. An ethanolic extract inhibited both the intracellular amastigotes and the promastigote form. The extract had very low toxicity.
Bidens pilosa is as effective as atropine, promethazine, neostigmine, and hydrocortisone in protecting mice from the venom of Dendroaspis jamesoni, a snake in Cameroon whose venom contains a potent neurotoxin. The plant extract also potentiated the antivenom normally used to treat those snakebites (as did atropine and promethazine). It is a very potent protector against neurotoxins. However, the plant is only weakly effective against viper venom, which causes hemorrhage and necrosis.
A number of in vivo studies reveal the herbal tincture to be highly antiulcerogenic, inhibiting gastric lesions induced by alcohol, and to be more effective than sucralfate. The herb significantly protected gastric mucosa and initiated mucosal healing through a number of mechanisms. (See Western Botanic Practice, page 136.)
A number of studies have found the plant to possess antitumor activity. It inhibits angiogenesis (the formation of abnormal blood vessels, common in cancer and certain forms of macular degeneration), is antiproliferative, and directly reduces viable tumor cells (stimulates apoptosis). It possesses a strong antileukemic activity and numerous cell regulatory actions that normalize cellular function and growth.
The plant also has a strong antipyretic effect, comparable to acetaminophen. It is specific for lowering fever during acute infections.
Bidens has been found to be a strong antioxidant and anti-inflammatory. A double-blind, randomized crossover trial with 20 participants found the herb effective in the treatment of allergic rhinitis. In vitro and in vivo studies have found it highly effective in protecting erythrocytes from oxidative damage. The water-soluble fractions are more antioxidative than the ethanol-soluble fractions. The plant inhibits COX-2 expression (similarly to ibuprofen) and prostaglandin production by inhibiting prostaglandin synthesis. It’s a significant free-radical scavenger, comparable to alpha-tocopherol. It inhibits histamine release.
A number of in vivo studies note bidens to be an effective hepatoprotector. It protects the liver from chronic obstructive cholestasis and decreases the rate of necrosis and liver fibrosis. It normalizes liver enzyme levels and restores superoxide dismutase and glutathione peroxidase levels in liver-injured mice. It is strongly protective against induced liver damage.
The plant possesses oxytocic-like actions on the uterus, tones the uterine muscle, and helps in labor contractions (in vivo studies).
It possesses relaxant activity on vascular tissue, is a vasodilator, and relaxes cardiac action. It reduces the aorta resting tone and inhibits KCL-and CaCl2-induced contractions by 95 percent. The effects are relatively long lasting. It attenuates high-fructose and salt-loaded hypertension in rats and reduces insulin levels in their blood. The effects are marginal in normotensive rats, but marked in hypertensive ones.
The plant possesses antidiabetic properties: It lowers glucose levels in the blood of mice, increases insulin sensitivity, and stimulates the release of insulin from the pancreas. A single daily dose for 28 days (in mice) also was found to protect islet structure in the pancreas and potentiate its activity. It was successfully used to reverse type 2 diabetes in mice. It reduces hypoglycemia. One of the herb’s constituents, cytopiloyne, a polyacetylene, has been found to prevent type 1 diabetes in nonobese mice.
Bidens pilosa is a strong and reliable immune modulator. It has been found to modulate the differentiation of helper T cells and prevent Th1-mediated autoimmune diabetes in nonobese diabetic mice. This has been attributed to a number of polyacetylenic compounds and a butanol fraction. The butanol fraction also reduces Th2-mediated airway inflammation in mice. Hot-water extracts of the plant stimulate interferon-gamma expression. The plant will increase immune action if such action is low, and decrease it if it is high.
Family: Asteraceae
Common Names: Sweet Annie • sweet wormwood
Species Used: There are around 400 artemisias in the genus, but Artemisia annua contains the most artemisinin—a potent antiparasitic—and this section will focus primarily on that species. Artemisinin is famous for its effectiveness in treating malaria. Many other artemisias contain artemisinin (contrary to earlier reports saying they did not) and I will discuss some of them in this section.
All the plants in the genus do have some antibacterial and antimicrobial actions; however, those constituents are not nearly as systemic as those in the other plants in this chapter. Artemisia annua, artemisinin, and its related constituents are best thought of as systemic antihematoparasiticals; that is, specific for killing blood parasites, rather than systemic antibacterials. Nevertheless, for treating diseases in their range of action, they are great.
The aerial parts, including the flowers, which have the highest artemisinin content.
The whole herb has a much broader range of actions than the isolated constituent artemisinin.
Because the studies are few and plant preparation differs from study to study, the outcomes in the antibacterial studies of the artemisias are contradictory. They do find a range of antibacterial activity across the artemisias—bearing out traditional uses of the genus—but the studies tend to vary on which bacteria the species are active against, leading to confusion. There is a tendency to extrapolate the clinical use of the plant based on its in vitro antibacterial activity, but that is a mistake, as it is with numerous other plants.
This same problem exists with goldenseal. Goldenseal is highly active against a number of bacterial organisms, but berberine, the strongest constituent, does not make it across the GI tract membrane in any quantity so the plant (and the constituent) is not a systemic antibacterial; it is mostly limited to the GI tract. Artemisinin, and some of the other antiparasitics in artemisia, are strongly systemic, but they have limited antibacterial activity. They are primarily antiparasitics for the blood and liver and antitumor agents.
The activities of the essential oils are more broadly antibacterial, but they are primarily confined to the GI tract when the plant is taken internally. This makes them useful for GI tract infections—or for use directly on the skin—but useless as systemic antibacterials. The traditional use of Artemisia annua, which gives a very good indication of its range of medicinal activity, has been primarily:
• For reducing fever—the plant stimulates sweating
• For topical use—it’s useful for infected wounds and skin infections
• For GI tract problems and infections
• For female reproductive problems—primarily as an emmenagogue
• For liver problems
• As a steam inhalant for respiratory problems—which utilizes the essential oils
• For parasitic diseases of the blood and liver
Most of the antibacterial studies have been on the essential oils of various species but again, these oils do not disseminate widely in the bloodstream, which means they will be useful only for respiratory infections when used as steam, internally in the GI tract when prepared as a cold infusion (which keeps the oils in the liquid), or topically when used as a poultice or cold infusion wash. Nevertheless, when used in these ways the artemisias are very good medicines for resistant organisms other than blood parasites.
A study of Artemisia nilagirica leaf extracts found the plant active against a range of both Gram-positive and Gram-negative organisms: Bacillus subtilis, Clavibacter michiganensis, Enterobacter aerogenes, Pseudomonas aeruginosa, Pseudomonas syringae, Salmonella typhi, Shigella flexneri, and Yersinia enterocolitica. It was not active against Enterococcus faecalis, E. coli, Klebsiella pneumoniae, or Staphylococcus aureus. A number of studies have found most artemisias inactive against E. coli, Klebsiella, Pseudomonas, and staph, but others, such as one looking at the activity of Artemisia anomala against Bacillus subtilis, E. coli, Proteus vulgaris, Salmonella typhi, and Staphylococcus aureus, have found the plant to be active. In that example a methanol extract was used. Given the solubility dynamics of artemisia constituents (including artemisinin), it seems likely that the variability in the studies is coming from solubility differentials (hexane, for example, is a much better solvent for artemisia constituents than anything else and artemisinin is much more highly soluble in fat—whole milk—than water).
Artemisinin: The effective dosage for malaria is 500 to 1,000 mg on the first day and 500 mg daily thereafter for 2 to 4 more days. This will completely clear the malarial parasite from the blood. However, at 400 mg per day for 5 days, the recrudescence rate is 39 percent. Dosage at 800 mg drops the rate nearer to 3 percent. Chinese dosage runs from 500 mg to 1,600 mg for 3 days, repeated in 2 weeks (to treat newly hatching parasites). I do think there is some evidential support for 800 to 1,200 mg for 5 to 7 days, repeated for another 5 to 7 days in 2 weeks. The relapse rate is definitely smaller at the higher dose.
Note: Artemisinin becomes less present in the blood the longer it is taken, so that by day 7 the constituent is present at only 24 percent of its day-1 levels. The isolated constituent is not very effective if taken for longer than 7 days at a time for parasitical infections. If it doesn’t work for babesia, for instance, within a few weeks, it is not going to. Pulsing will not help.
There are several things to keep in mind when preparing the whole herb for use:
• The fresh plant is the strongest.
• Whether fresh or dried, the plant should never be boiled.
• Fat helps extraction of the active constituents.
• The plant, while still potent for blood parasites, loses a lot of its antioxidant activities if dried.
• Dosage and length of use are crucial.
Traditional Chinese texts, thousands of years old, recommend preparation of the fresh herb, infused in room-temperature water, then pounded and wrung out to extract the plant juice as well. Examination has indeed shown that this produces the most potent infusions.
Many of the constituents in artemisia are not very water soluble, including the artemisinin. However, they are highly soluble in fats and alcohol.
Place 100 grams (about 4 ounces) of fresh herb (leaves and flowers) cut into pieces in a container, pour ½ quart (2 cups) hot water over the herb, cover, and let stand 12 hours. Wring out; drink it all. Do this daily for 7 days. Repeat after 2 weeks.
Run the fresh plant through a juicer. Take 1 tablespoon of the fresh juice every day for 7 days—you can stabilize the juice with the addition of 20 percent alcohol (see page 227). Repeat after 2 weeks. Note: The fresh juice is 6 to 17 times more potent than pure artemisinin; this and the tincture are the two most potent forms of the herb.
Actions
Antibacterial
Antifungal
Anti-inflammatory
Antimalarial
Antiparasitical
Antitumor
Antiviral
Calcium antagonist
Immunomodulant
Plasmodicide
Schizonticide
Active Against
Babesia spp.
Bovine diarrheal virus
Clonorchis sinensis
Eimeria acervulina
Eimeria tenella
Epstein-Barr virus
Fasciola hepatica
Hepatitis B and C
Leishmania spp.
Neospora caninum
Opisthorchis viverrini
Plasmodium spp.
Schistosoma spp.
Toxoplasma gondii
Trypanosoma spp.
Also active against various cancer cell lines. Broadly active against dermatophytes—fungi that cause infections in hair, skin, and nails. A. annua is active against a number of bacteria in vitro, but the data in the various studies is contradictory, as usual. Specific for parasitic infections in the blood and liver and to some extent in the GI tract.
Decoctions of the herb are active against Bacillus cereus, Bacillus subtilis, Bordetella bronchiseptica, E. coli, Klebsiella pneumoniae, Micrococcus flavus, Proteus vulgaris, Pseudomonas aeruginosa, Salmonella typhi, Salmonella typhimurium, Sarcina lutea, Staphylococcus aureus, Staphylococcus epidermidis, and Streptococcus mutans.
A different extract (type not stated) was found to be active against Mycobacterium avium. Methanol extracts were found active against Bacillus cereus, Bacillus pumilus, Bacillus subtilis, E. coli, Micrococcus luteus, Pseudomonas aeruginosa, Salmonella spp., and Staphylococcus aureus.
The essential oil has been found active against Candida albicans, Enterococcus hirae, E. coli, and Staphylococcus aureus but not Pseudomonas aeruginosa.
The oil of Artemisia tschernieviana has been found active against Bacillus cereus, Bacillus subtilis, Candida albicans, Enterobacter aerogenes, E. coli, Klebsiella pneumoniae, and Staphylococcus aureus. This same antibacterial activity has been found in other artemisias: A. absinthium, A. douglasiana and A. ludoviciana (also Helicobacter pylori), A. echegarayi (also active against Proteus mirabilis and various Listeria species), A. gilvescens (also MRSA), A. giraldii (also Aspergillus spp., Proteus spp., Sarcinia lutea, Trichoderma viride), A. herba-alba, A. iwayomogi, A. kulbadica, A. leucodes, A. monosperma (also TB and staph), and A. princeps var. orientalis (also Bacteroides fragilis, Bifidobacterium, Clostridium perfringens, and staph), A. vulgaris (also Streptococcus mutans).
The artemisias in general are considered to be active against intestinal parasites, but again, little actual study has occurred. A. absinthium is often considered the most potent against intestinal parasites in historical practice. Leaf extracts are active against Syphacia parasites, nematodes that infect the intestinal tracts of mice; the plant is also active against multi-drug-resistant malarial parasites in vivo.
Artemisia maciverae is active in vivo against Trypanosoma brucei, showing complete clearance after 7 days of treatment (10 mg/kg body weight). The same plant is also strongly antiplasmodial at the same dosage, clearing the parasites from mice in 3 days.
Various artemisias have been found active against plant pathogens (which is why artemisias are used to protect crops in some locations) and various fungi.
Use to Treat
Any parasitic infection in the blood and liver or for systemic cancers (artemisinin does have good activity as an antitumor drug). These are the real strengths of the plant if it is being used as a systemic. There is nothing else comparable in potency for these uses. The plant, if properly prepared, is also active against microbial and parasitic infections, especially in the GI tract (see Preparation and Dosage, page 142) and on the skin.
Pour 1 quart hot water over 100 grams of dried herb (leaves and flowers), and let stand 12 hours. Strain and drink. Do this daily for 7 days. Repeat after 2 weeks.
Pour 1 quart hot, whole milk over 100 grams fresh or dried herb, cover, and let stand 4 hours.
Note: This will extract 80 percent of the artemisinin in the herb while water infusions extract much less (about 25 percent in dried herb formulations).
Chop fresh herb finely, and measure its weight in ounces. Place the herb in twice that amount (now using liquid ounces) of pure grain alcohol. (For example, you’d mix 1 ounce of herb with 2 ounces of alcohol; see Fresh Plant Tinctures, page 339, for more depth on this). Let stand 2 weeks. Press out the liquid. Take 1 tablespoon twice daily for 7 days. Repeat after 2 weeks.
Take 2 ounces each of the tinctures of sida, cryptolepis, and Artemisia annua and combine together. Take 2 tablespoons of the mix each day for 7 days. Repeat in 2 weeks.
The herb is very effective if used properly. The dose can be increased fairly high, as it is a very safe herb. Remember: The reason that this herb was discovered was that in the region of China where it is used there were few or no incidences of malaria. The secret is in the dose, as with all medications.
About 25 percent of people using Artemisia annua as an antimalarial report a mild nausea, which does not progress to vomiting. It may also cause occasional dizziness, tinnitus, pruritus, and mild abdominal pain.
Artemisinin itself can cause gastrointestinal upset, loss of appetite, nausea, cramping, diarrhea, vomiting. About 4 percent of people who take it experience these symptoms, usually in a more severe form than that experienced from ingesting the herbal infusion. Very high doses (5,000 mg per day of artemisinin for 3 days) have caused liver inflammation, which corrects upon stopping the supplement. Artemisinin has a slightly chronotropic effect on the heart. It causes mild hypotension. This has not been, apparently, a problem in any users.
Both the herb and the constituent should be used with caution in pregnancy, especially in the first trimester. In vivo studies have found a number of adverse effects in rats and mice if the herb is used in the first trimester. However, one clinical trial with 16 patients in the first trimester of pregnancy taking the herb found the miscarriage rate to be the same as that for the general population.
Artemisia annua, like many antimicrobial plants, contains synergists that make its compounds more active against microbial organisms. In this instance, chrysospenol-D and chrysophlenetin, two flavonols in the plant, have been found to potentiate the activity of berberine and norfloxacin against resistant staph. Artemisinin does induce certain liver enzymes and may interact with drugs such as omeprazole.
A. annua is native to China, western Asia, northern India, Japan, Korea, Vietnam, Myanmar, southern Siberia, and southeastern Europe. An emerging invasive plant species, it is naturalized in the United States and many other countries. It loves waste places—roadsides, fallow fields, neglected gardens—especially in eastern North America. It can grow pretty much anyplace but is stronger and more aromatic when grown in poor, dry soil. Its artemisinin content is about 20 percent higher when it grows in mildly potassium-deficient soils.
The plant, once established, grows into a large straggly bush. The leaves look a bit like celery’s leaves, though A. annua’s are much broader, bushier, and more extensive in their growth. The plant grows 4 to 6 feet (1.2 to 2 m) tall with a typical attractive, weedy, bushy look. It blooms in late summer.
Artemisia annua is an annual (hence its species name) and cultivates easily from seed. Sow the tiny seeds outdoors in the fall or seed them indoors before the last frost. They like it best on top of well-aerated soil; they need light to germinate. Once established, the plant self-sows and will never go away.
The aerial parts should be harvested just after flowering. The flowers and leaves both contain artemisinin. The artemisinin content is higher in the fall than in spring; it takes the plant time to create the chemical. The longer you wait, the better the yield, so take even the older, dying-back leaves. The stems and root contain only very low amounts of the compound and aren’t generally worth the trouble.
Once the plant is picked, let it dry in the sun for a week. The light helps the artemisinin precursors keep producing after the plant is harvested. After a week, the sun does more harm than good, so finish drying in a dry, dark spot inside.
Several hybrid plants (Artemisia annua var. artemis, var. campinas, var. anamed) have been bred for higher artemisinin content. They are available from Anamed (www.anamed.org) as part of an artemisia antimalarial starter kit that includes a lot of useful information on growing and using the plant. One problem with the hybrids is that they don’t reseed themselves well and the artemisinin content of those that do is poor (so it is not as sustainable an alternative as it should be). If you want a continual supply of the plant, non-hybrids are the way to go.
Artemisia annua contains a great many chemical constituents, over 150 at last count, and that is most likely just a tiny fraction of the total. There are a minimum of 28 monoterpenes, 30 sesquiterpenes, 12 terpenoids and steroids, 36 flavonoids, 7 coumarins, 4 aromatics, and 9 aliphatic compounds.
Artemisinin is considered to be the active antiplasmodial compound but numerous other compounds with malarial activity have been found. Others, such as arteannuin B and artemisinic acid, are antibacterial and antifungal. Arteannuin B, while found to be ineffective against malarial parasites, strongly potentiates the activity of artemisinin. Many of the flavonoid compounds have been found to be antimalarial in vitro. Some of them (artemetin, casticin, chrysophlenetin, chrysosplenol-D, and cirsilineol) have been found to also potentiate artemisinin’s ability to kill plasmodial parasites. Many of these flavonoids are abundant in the plant; they induce a three- to five-fold reduction in the amount of artemisinin needed to kill malarial organisms. Some of the sesquiterpene lactones are also antiplasmodial, with ridentin, some of the guainolides, and germacranolides being the most important.
The artemisinin content of A. annua, if the leaves and flowers are harvested in the fall before the plant goes to seed, can run anywhere from 0.75 percent to 1.4 percent (several high-yield varieties are in development or are just on the market).
A relatively new development is the finding of another strongly active antiplasmodial constituent, tehranolide, in a number of artemisia species. In vivo studies show it to be strongly antiplasmodial. Treatment with the tehranolide extracts of Artemisia diffusa resulted in complete clearance of parasites from the blood in mice at similar dosages to artemisinin.
Artemisia annua (and many of the other artemisias) is somewhat unusual in its actions. The systemic constituents of the plant primarily act in two ways: 1) as highly potent antiparasitics for blood and liver parasites; and 2) as antitumor agents. These same constituents have two other actions that are useful: 1) they stimulate sweating and thus help reduce fever; and 2) they are emmenagogues; that is, they stimulate menstruation. The emmenagogue action is why the plant is generally not recommended in the first trimester of pregnancy. Caveat: Artemisia annua has much less emmenagogue activity than some of the other artemisias; the stimulatory activity has been found to be only minimal.
Although other artemisias have been used to effectively treat malaria and other blood parasites, the most potent species for this, at this time, is Artemisia annua.
The plant has been used in Chinese medicine for over two thousand years, but its current status as an antimalarial emerged from its use by the North Vietnamese during the Vietnam War. Malarial infections were exceptionally high among the North Vietnamese troops. Appeals to the Chinese leader Mao for help resulted in the discovery of Artemisia annua for use as an antimalarial.
Chinese researchers had discovered that in one region of China the people had little incidence of malaria infection. Looking closer they discovered that the local people took the herb at the first sign of symptoms. In 1972 Chinese researchers isolated artemisinin.
This plant is unknown in India, though a number of other artemisias are used. Artemisia absinthium is used for intermittent fevers, for stomach complaints (as a bitter and digestive), as a vermifuge for intestinal worms, and for nervous system complaints (from hysteria to depression). Artemisia maritima (wormseed) is specific for intestinal worms, especially ascarides and oxyuris. Most of the other artemisias are used similarly.
Called qing-hao in traditional Chinese medicine, Artemisia annua is used for clearing fevers from the blood, especially in conditions with headache, dizziness, low fever, and a stifling sensation in the chest. Also for febrile diseases, for malaria, and for scabies, pruritus, and malignant ulcers.
For many years A. annua was unknown, although many other artemisias have long been used. Artemisia absinthium was a primary herb among the Eclectics in the late ninteenth century in the United States. The herb was used for intermittent fevers, for malaria, as a vermifuge in the treatment of intestinal worms, for dyspepsia, nervous conditions, diarrhea and liver complaints, for amenorrhea and leukorrhea, for jaundice. Other artemisias were used similarly.
The indigenous peoples throughout the United States used the plants similarly.
There have been hundreds of in vitro and in vivo studies and clinical trials on the antiparasitical actions of artemisinin (and its analogues), most on malaria and schistosomiasis. I will just touch on them here.
Every one of the several hundred clinical trials shows the effectiveness of artemisinin in the treatment of malaria. (There have been a number of clinical trials with the whole herb as well; see Whole Herb vs. Artemisinin, page 154.)
Artemisinin has become the choice for malarial treatment worldwide because it is effective against resistant strains of the organism. Ninety-eight percent of malarial parasites are generally killed within 24 hours with use of the herb or its isolated constituent. If low, short-term doses are used (less than 5 days), however, relapse rates can be as high as 39 percent. Higher dose ranges for a longer period of time (5 instead of 3 days) lower the relapse rate considerably. Clinical trials with as many as 2,000 people (with both low and high dosages) have found 100 percent clearance rates for all participants if artemisinin is taken for 5 to 7 days. There are very few side effects when used properly in short-term treatment.
The constituents of the herb that are antiparasitic are exceptionally systemic in that they spread quickly throughout the body and easily cross the blood-brain barrier. Artemisinin is considered specific for cerebral malaria. Because it infuses the blood, it is carried throughout the body to every cell, all of which need blood to live.
A slightly modified form of artemisinin—artesenuate—has been found effective for babesia organisms in vitro. Relatively low concentrations of the compound are effective; complete inhibition of Babesia equi and B. caballi occurred at 0.2 and 1.0 micrograms/ml respectively. (To make artesenuate, artemisinin is modified slightly in order to get patent protection.)
Use of artemisinin in clinical practice, however, has shown only moderate success for this organism; it seems to be effective in about half the people who use it for babesia. Sida and cryptolepis appear to be better alternatives.
A number of clinical trials have occurred with a synthetic form of artemisinin, artemether, in the treatment of schistosoma infections. Schistosoma are a type of blood fluke—and are a major infectious parasitic organism, second only to malaria in numbers of those infected, totaling hundreds of millions worldwide.
Artemether is normally given in a single dose of 6 mg/kg every 2 weeks. It is primarily active against the juvenile form of the parasite rather than the adult. Repeated dosing results in parasite reductions of 90 percent to 98 percent. Artesenuate has been found just as effective.
Artemisinin is also effective against Neospora caninum, another type of protozoa that affects both endothelial cells and macrophages. CNS involvement and carditis are common. Artemisinin is effective against a number of other organisms such as Eimeria tenella, Leishmania major (which infects macrophages), Toxoplasma gondii, Schistosoma mansoni (liver flukes), and Clonorchis sinensis (liver flukes), all parasitical organisms. It is antispirochetal against leptospire organisms, killing them in vitro. Artemisinin does appear to possess broad antiparasitical actions.
Artemisinin is also stimulating interest as an antitumor and anti-cancer compound. It has shown effectiveness as an anticancer agent both in vitro and in vivo. In vitro studies have found artemisinin effective against human leukemia cells, breast cancer, and colon cancer. Treatment of both bone cancer and cancer of the lymph nodes in dogs was effective with 10 to 15 days of treatment. The use of artemisinin in people with cancer has shown effectiveness as well; Vietnamese doctors have found it successful in curing 50 percent to 60 percent of several different types of cancer patients.
Clinical practice reports indicate the use of artesenuate in the successful treatment of non-Hodgkin’s lymphoma (60 mg IM for 14 days), artemisinin for small-cell lung carcinoma (500 mg BID for 4 months), artesenuate (IV) and artemisinin (300 mg BID) for 4 months in the treatment of stage 4 breast cancer with metastases, topical artemisinin in the treatment of multiple skin cancers, oral artemisinin in the treatment of breast cancer with metastases to the spine, and artesenuate in the treatment of stage 4 uveal melanoma.
A number of studies have found the herb to possess anti-inflammatory and antioxidant activity.
Artemisinin is immunostimulatory in vivo. It stimulates phagocytosis, and macrophages become more potent; they are better at phagocytosing malarial-infected erythrocytes.
There is increasing evidence that using the single compound artemisinin or any of its derivatives is stimulating resistance in the organisms it is being used to treat. Resistant malarial organisms have been found in Cambodia and are beginning to spread worldwide.
A recent study found that malarial organisms go into a dormancy state upon encountering artemisinin and then recover after dosing has ceased.
In consequence, many groups are beginning to use combination therapies to treat susceptible parasites, essentially artemisinin plus a pharmaceutical. It’s known as artemisinin combination therapy or ACT.
The increasing resistance to artemisinin and its synthetic derivatives is a problem that cannot be solved through multidrug therapy: single constituent pharmaceuticals will always end up promoting resistance in disease organisms. A different approach is essential.
As I have already mentioned, there is a conflict between two ideologies in health care and medicine: 1) sustainable, affordable health care that empowers the people who use it; and 2) health care controlled by corporations for their own profit, a model that is designed to keep the people who use it dependent on specialists and corporate manufacturers. There is no way to avoid encountering, or dealing with, this conflict in some form if you explore the use of herbal medicines for your own health.
While the cost of artemisinin is low when viewed from Western, industrialized perspectives, in Africa it is prohibitively high. In 2004 the cost of a course of artemisinin was $2.40, more than most people in Africa can afford. As a result artemisinin forgery has become a lucrative business in Africa. Products that contain no artemisinin are widely available; they do nothing to cure malaria.
A number of NGOs (nongovernmental organizations) such as ANAMED (Action for Nature and Medicine), of which I am an admirer, have begun to address the problem in a simple and direct manner—they are providing artemisia seeds to anyone in Africa who wants them, teaching them how to grow the plant and how to use it to treat malaria. This has resulted in rather predictable responses from Western researchers, physicians, and corporate scientists. They oppose it and sometimes work quite strongly to stop it.
The primary argument being made is that the plant is not very effective against malaria, which of course ignores the reason artemisinin was discovered in the first place—people who used it for medicine had little or no incidence of malaria in their communities. Some researchers go so far as to say the plant does not work at all, only the isolated constituent is effective. Jansen (2006) is a perfect example. He comments, “The herbal tea approach to artemisinin for malaria is totally misleading and should be forgotten as soon as possible.”5
Thankfully, the reaction to such antiquated thinking has been strong.
RITAM (Research Initiative on Traditional Antimalarial Methods), a partnership between the Global Initiative for Traditional Systems of Health at Oxford University and hundreds of international researchers from over 30 countries who are exploring malaria treatment with traditional plants, responded to Jansen’s comment this way: “We believe that this statement is totally misleading and should be forgotten as soon as possible.”6 Their article then explains in depth how most Western researchers, in looking at Artemisia annua tea formulations, consistently fail to understand the plant or how it should be used in practice to be effective. It points out, as well, how Hansen’s comments are fatally flawed.
Extensive work by RITAM and ANAMED has resulted in comparable tea preparations that are as effective in use as artemisinin.
The artemisinin content in the plant is strongly stable if it is properly stored (out of the sun in foil or plastic bags inside plastic tubs). Even after 1 year in storage, the artemisinin content is nearly identical to that in the freshly harvested plant. (Ceiling-hung plants will begin to degrade after 3 months.) The artemisinin is held in the glandular trichomes of the plant’s leaves and flowers, where the essential oils of the plant are also held. These oils protect the artemisinin from degradation, oxidation, fungi, and molds.
Numerous researchers are suggesting that artemisinin combination therapy (ACT) is the best approach to treating malaria as the recrudescence rates are smaller and the parasite has a harder time developing resistance. But the plant already is an ACT substance. Researchers, using identical tiny amounts of Artemisia annua and artemisinin, found that these tiny amounts of A. annua reduced parasitemia in vivo by 50 percent at day 4, while the artemisinin was no more effective than placebo.
Other researchers, removing the artemisinin from the plant, found it still effective for malaria treatment.
There are other constituents in the plant that have been found to be synergists with artemisinin. Several flavonols have been found to be potentiating synergists with both berberine and norfloxacin in the treatment of MRSA, for instance. They apparently act as a multidrug-resistance efflux pump inhibitor (see chapter 6). These same flavonols have also been shown to potentiate the action of artemisinin against the malarial parasite. And both Artemisia annua and Artemisia dracunculus contain an essential oil, piperitone, that acts as a potentiator of nitrofurantoin against Enterobacter cloacae.
The number of synergists and potentiators in the artemisias seems large. The complex combination of multiple antiplasmodium constituents and synergists makes the plant a potent choice for an, essentially, free treatment for those who need it, or want it as the treatment of choice.
There have been a number of clinical trials in the use of the tea (or whole herb or tincture) in treating malaria. Studies have shown that the pharmacokinetics of the herb’s artemisinin when taken as a tea are identical to those of artemisinin taken as an isolated constituent:
Clinical trial with tincture: 72 grams of crude extract in divided doses over 3 days in the treatment of 485 cases of Plasmodium vivax and 105 cases of P. falciparum. Clearance rate was 100 percent, but the patients were not followed for recrudescence.
Clinical trial with whole-herb infusion: 93 percent clearance rate in 254 patients using a 7-day course of whole herb infusion (tea) in the treatment of P. falciparum. Recrudescence rate was 13 percent after 1 month.
Clinical trial with capsules: Clinical trial of 165 people infected with Plasmodium vivax. Fifty-three were given capsules of A. annua that also contained oil (COEA) for 3 days (the oil enhances absorption of the artemisinin). Another 50 received the herb capsules with oil (COEA) for 6 days. Forty-one received capsules without the oil (QHET). Twenty-one received chloroquine. Dosage was 36.8 grams on the first day, 18.4 on subsequent days. Parasite clearance and fever reduction were faster with the capsules than with chloroquine. There was a 30-day follow-up with blood checks every 10 days. About one-third of those who took the COEA herb capsule for only 3 days or who took the non-oil capsules (QHET) experienced recrudescence. Those who took COEA for 6 days experienced about 8 percent recrudescence. There was no recrudescence in the chloroquine group.
Clinical trial with infusion: An aqueous infusion for 5 days in a small trial of five people found 100 percent clearance; no follow-up occurred to check for recrudescence.
Clinical trial with infusion and decoction: A trial using infusions (254 people) and decoctions (48 people) with 5 grams herb in 1 liter of hot water, infused for 15 minutes or boiled for 5 minutes, found both forms effective. Dose was 250 ml (about 8 ounces) four times daily for 7 days in the infusion group and 4 days in the decoction group. Clearance rate was 93 percent and 92 percent respectively. There was a 13 percent recrudescence rate in the infusion group. Recrudescence in the decoction group was not checked.
Early indications are that if the plant is properly prepared and used it can be as effective as artemisinin or its analogues in the treatment of malaria and other blood parasites. It will be especially effective if combined with other plants described in this chapter, especially sida and cryptolepis.