♦ Know where your lungs are
♦ Lung structure
♦ How the lungs work
♦ Healthy lungs compared with COPD lungs
♦ The muscles involved in breathing
♦ The oxygen demand of breathing
♦ The control of breathing
The vast majority of people go throughout life without ever having to consider their breathing. For some, the first time they pay any attention to their lungs is when they get close to their last breath. As I work almost daily with people with COPD, I find that breathing can preoccupy their minds for considerable periods of the day. What amazes me is how little most of these COPD patients know about the workings of their lungs, so I always take time to explain the basic structure and function of the respiratory system so that they get a gist of what I will be asking them to aim towards throughout the Brice Method. There are certain structures of the body that play pivotal roles in healthy breathing, and others that can contribute to breathlessness. You will need to be able to identify these structures as you go through this book, and you will eventually be able to feel yourself using parts of your body in a way that will help, not hinder, your breathing.
Not all the COPD patients I see are completely oblivious to how they can control their breathing. Many people will have learnt particular breathing techniques through activities they have done throughout their lives. Some people will have sung, or played a wind instrument, and learned how to control their breath to make music. Others may have played a sport where the manner of breathing is pivotal to performance, and others may have had a job where activities have required them to breathe in a certain way. I find this reference point can be very useful; if you can cast your mind back to an activity in your life where you have had to control your breathing to some degree, this may help you take on board the information in this book more readily. If you have never done anything where you have had to think about your breathing, don’t worry. This book is designed to take you through each stage of the process. One of my ex-patients, who was in his late nineties, put into words what I was thinking when he learned to breathe in a stress-free way: ‘You have taught an old dog a new trick!’
Important reminder
If you decide not to do Landmark 1 (self-test, page 13) prior to reading on, you are highly unlikely to recognise what improvements you are making as you progress through the programme. If you are serious about learning how to breathe more effectively, you will need to do the self-test and record the outcomes, so you can refer back to it at a later date.
I have found that the first thing you need to do to help you improve your breathing is to understand where your lungs are, and how they are designed to work. It is my experience that it is only when you know this information that you can fully understand where you could be going wrong and what you can do to improve your breathing.
Know where your lungs are
Strange though it may seem, the vast majority of patients that I see have absolutely no idea of where their lungs are located, and have almost no concept of their size and capacity. Once I have asked patients about their medical history and their breathing has settled down, I ask them to take a deep breath and tell me where their lungs are positioned. Most simply gesture to the general area of the chest, looking at me as if I am a bit daft bothering to ask them such an obvious question. It is a couple of seconds later when they struggle to explain exactly where their lungs are, that they realise that, even though they have a lung condition, they know very little about the organ that limits their lives so dramatically.
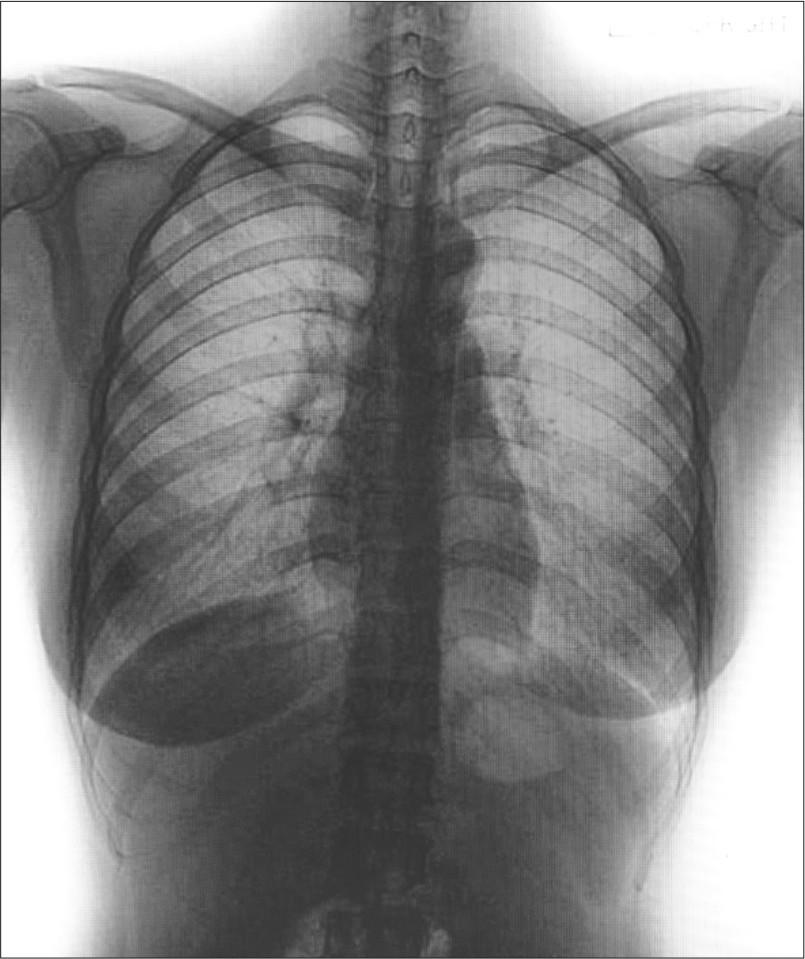
At this point, I take the opportunity to show my patients a picture of a normal set of lungs (see Figure 1.1). When patients see that their lungs take up almost the entirety of the inside of the rib cage, some start to get an inkling of where their problems might lie, especially if they can feel the air going only a little way into the chest in the self-test exercise, Landmark 1. (Hopefully you will have done this exercise, recorded your 1–10 score, and written down a short description of how the breath felt to you. Sorry to keep on about this, but it really is important.)
Lung structure
The next step I take is to teach a patient how the lungs are structured, and how this structure affects their proper functioning. I will quickly run through this using a diagram of the anatomy of the respiratory system (see Figure 1.2). The area occupied by the lungs is known as the thorax, and the parts of the spine associated with this area (the thoracic spine) are called the thoracic vertebrae.

Figure 1.2: Anatomy of the respiratory system
Looking at Figures 1.1 and 1.2, probably the first thing you will notice is how enormous the lungs actually are. I find it useful to compare the lungs to sponges that almost completely fill the inside of the rib cage. Also inside the rib cage there is a gap for the heart, plus the tube that leads to the gut (the oesophagus), and a few blood vessels and nerve bundles (not shown here). The rib cage is designed to protect the fragile lungs, but to do so whilst still allowing the chest to be mobile enough for the lungs to work effectively. This structure is also flexible enough to assist with relatively complex body movements like walking, throwing, lifting and carrying, not to mention maintaining an upright stance.
You are already likely to know that the primary role of the lungs is to draw air into the body, extract the oxygen from the air, and make it available to the bloodstream to circulate round the body. The lungs also help get rid of carbon dioxide as well as heat, both of which are waste products of the body, as it uses up the oxygen. Oxygen is essential to help power every living cell in your body, transforming glucose into energy. Every cell requires oxygen to function effectively, and this is why the respiratory system is so important – ultimately it is key to our survival.
I feel it is vital to emphasise that the overall capacity of the lungs is ultimately linked to the expansion and contraction of the rib cage and the cavity that houses the lungs. This will be explored many times throughout this book. The lungs sit above the abdominal mass of the liver, stomach, gut and other organs. They are physically separated from the abdominal mass by an extremely strong dome-like muscle called the diaphragm.
Inhalation (breathing in) causes air to be drawn in through the nose via the nasal cavity, or directly in through the mouth. This air passes the pharynx inside the head, and then into the larynx, and down the windpipe. The windpipe, or ‘trachea’, is a thick cartilage-ringed pipe that takes the air down the neck into the main structure of the lungs. The trachea splits into two primary bronchi that allow air into the left and right lungs. These in turn split into ever-smaller pipes until the air reaches the minute bronchioles. Oxygen does not transfer into the bloodstream directly from these pipes; they merely transport the air into the active part of the lungs. The active part, where the oxygen is absorbed into the bloodstream, is made up of structures called ‘alveoli’.
All of these structures are shown in Figure 1.3.
There are literally millions of alveoli in an adult lung, and they have the ability to expand and contract rather like a sponge. If you were to take a healthy lung from a small adult, and spread out all the alveoli on the floor, the surface area would take up the size of a badminton court. Do the same for a large adult, and the surface area would be closer to the size of a tennis court. Once you understand that such large surface areas are involved in transferring oxygen into the bloodstream, is it little wonder that the human body can do extraordinary feats of physical activity?
For the less healthy lung, smoking, pollution, disease or illness may have had the effect of damaging some areas of the alveoli, even affecting the elasticity of some of the smaller tubes that feed the alveoli. These damaged areas reduce the amount of space that is useable for the transfer of oxygen from the lungs into the bloodstream. The good news is that whilst areas of the lung may have been damaged, the remaining space is usually large enough to allow for day-to-day activities in all but the most severe cases of COPD.
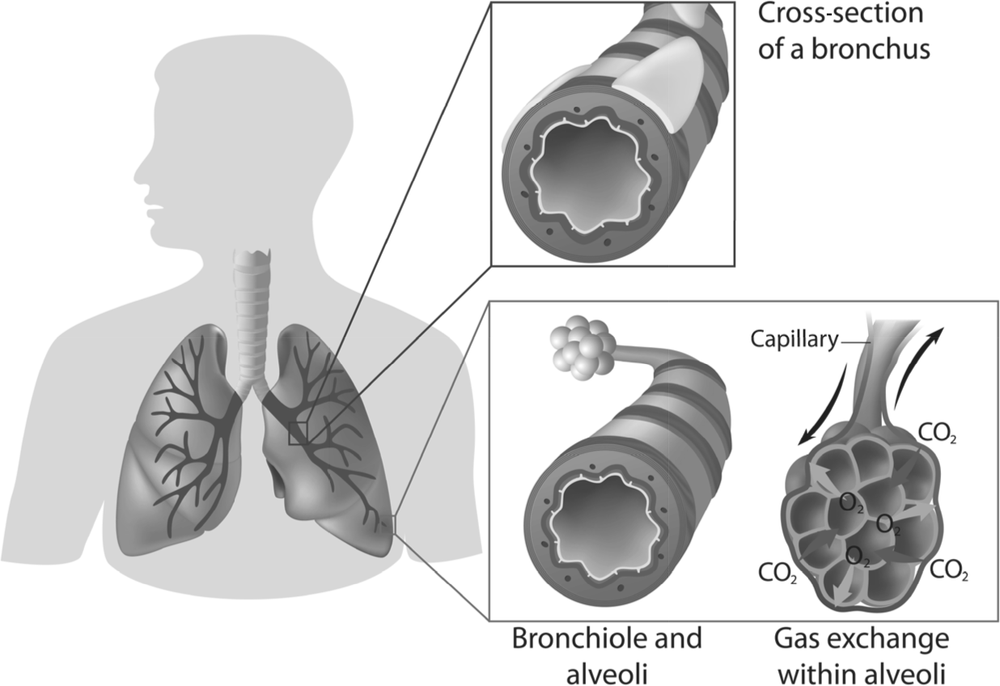
Figure 1.3: Bronchi, bronchial tree and alveoli
I find it is reassuring to tell my patients that whilst their badminton court- or tennis court-sized space may be damaged because of their illness, they are likely to still have plenty of lung remaining. Visualising the tennis court, they are probably still going to be able to play on the smaller singles court, rather than the full doubles court. Whilst adventurous humans may need the badminton/tennis court-sized surface area of lungs to do extreme activities, like climbing Mount Everest or winning the Tour de France cycle race, much less ‘floor space’ is required to climb a flight of stairs or take the train to Paris. Most COPD patients have much simpler objectives.
How the lungs work – the pressure gradient
The air we breathe is a gas, and gases have properties that enable them to be moved simply from one area to another without using up very much energy. Gases move from areas of high pressure to areas of relative low pressure, and the speed at which the flow takes place depends, in the main, on the variation between the two pressures. Think about how the expansion of the chest cavity would cause the air pressure in the lungs to drop, and once the pressure is lower than the outside air, the gas will be sucked in automatically.
A COPD patient’s lungs are usually as sensitive to small variations in air pressure as a barometer. Many COPD patients have yet to realise that their breathing becomes laboured when the external air pressure is low. This can help explain to some extent why on some days you can breathe more easily and on others you may not. Just as hill walkers will notice the reduction in the air pressure as they ascend a mountain, COPD patients will struggle when the air pressure is low.
It is important to understand that the structure of a healthy lung is extremely spongy and malleable. It is this sponginess that enables lung tissue to expand and contract with the chest cavity, drawing air in, and also helping push the air out with relatively little effort. Until you developed COPD it is likely that you rarely thought about the fact you were taking approximately 15 breaths a minute, every minute of every day. As it makes sense that anything which prevents the lungs from expanding or contracting will ultimately restrict a person’s ability to breathe, I feel it should be the first thing to be looked at before other forms of treatment or medication are recommended.
Healthy lungs compared with COPD lungs
Normal, gentle breathing does not use the full capacity of the lungs, as the lungs have a considerable reserve volume that can be accessed when the body needs additional oxygen. This is even the case for most COPD patients. The approximate capacity of a healthy male lung is compared with that of a typical COPD lung in Figure 1.4. The normal breath we take in at rest, or during very slight movement, is called the tidal volume. This provides enough oxygen for the body’s basic functions and is shown in grey on the diagram. The tidal volume of a healthy lung may be 500 ml, whereas in the COPD lung it may only be 300 ml. Each lung also has to have a certain amount of air in it to prevent it from collapsing in on itself, and this is shown as the residual volume, which is approximately 1200 ml. The vital capacity is the actual amount of air the lungs can use before they collapse on themselves. In a healthy lung, you will see that the vital capacity is approximately 4600 ml. If you compare that with the COPD lung at approximately 1800 ml, you will notice the possible area of lung damage massively limits the overall ability of the COPD lung.

Figure 1.4: Healthy lungs compared with COPD lungs (approximate capacities)
As I mentioned previously in this chapter, the air has to be drawn deep into the lungs to reach the alveoli before the oxygen can be transported across into the bloodstream. The alveoli are like minute bunches of grapes with a network of capillaries (the smallest type of blood vessel) round them. Once the air is in the alveoli, oxygen is drawn from it into the bloodstream, eventually reaching the red blood cells. If the red blood cells have enough oxygen in them, the transfer of oxygen into the blood is generally limited. If there is a demand for oxygen in the body, the oxygen is absorbed into the bloodstream immediately, and carbon dioxide, produced as a waste material, travels in the opposite direction into the alveoli simultaneously. Because oxygen is capable of diffusing across only the cell membranes of the alveoli, you not only need to get the air deep enough into your lungs to reach the alveoli, but you also have to keep the air in the air sacs of the alveoli long enough for the oxygen to be absorbed into the bloodstream. Unfortunately, most COPD patients I meet tend to take quick, short and shallow breaths, especially when they are active, and this will ultimately limit their ability to exercise.
The fast breath rate of most COPD patients is something that needs to be addressed before quiet comfortable breathing can be achieved, again something that will be explored in detail later in the book.
The muscles involved in breathing
Whilst there are numerous muscles that influence breathing to some degree, I find it is best to teach my patients that there are three primary muscle groups involved in breathing. Figure 1.5 shows the location of the main muscles of breathing, along with other, secondary, muscle groups, that assist with breathing to some degree. You can refer back to this diagram as you read on.
The diaphragm
The muscle with the most profound effect on normal breathing is the diaphragm. It is a large, dome-shaped muscle that attaches to the lower ribs, separating the lungs and chest cavity from the abdominal cavity. During inhalation, the diaphragm actively contracts downwards to draw air into the expanding lungs. It relaxes automatically, aiding the lungs to recoil during exhalation (breathing out). When it is working effectively, the diaphragm can be responsible for as much as 80% of air flow. It is, however, easily restricted in its efforts as it relies on both the position of the ribcage to allow it to work effectively, and the muscles surrounding the abdomen to pressurise the abdominal mass for it to work against.
Muscles between the ribs
The next most effective group of muscles involved in breathing are the intercostals. There are two sets of intercostal muscles and they each attach between the individual ribs: the internal and the external intercostals. The internal intercostal muscles pull the ribs down and together pushing air out, and the external muscles have the opposite effect as they pull the ribs upwards. These can contribute as much as 15% of maximal airflow. When we are sedentary for long periods of time, the intercostal muscles need to do very little, so they become untrained, and even start to feel quite rigid.
Muscles in the front of the neck
The third and final group of primary muscles involved in breathing are the smallest and weakest of the three groups. They are located in the neck, and are known collectively as ‘accessory muscles of the neck’. They act by lifting the first and second ribs, and can often be seen clearly as sinewy wires going down the side of the neck in people when they are struggling to breathe.
At maximal effort, the accessory muscles would only contribute up to 5% of the maximal airflow (see Figure 1.6). Healthy people usually recruit them only at times of real need, such as during high intensity activity. Oddly, this contrasts with the vast majority of the COPD patients I meet. It is common for these people to rely very heavily, sometimes almost entirely, on these small weak muscles for inhalation. Relying upon these small, insignificant muscles groups to drive respiration is a sign of breathing dysfunction and it is also very tiring. Not only do they fatigue very quickly, but they also tend to use up significant amounts of energy with very little effect on breathing efficiency.
The oxygen demand of breathing
The inefficient breathing patterns that COPD patients demonstrate mean that they can often be using between 50% and 70% of their energy expenditure just to drive respiration. This phenomenon may explain why some COPD patients become excessively thin, because their bodies are using up much of their energy intake simply to fuel their inefficient breathing. In comparison, a healthy person will use a negligible amount of energy to breathe, relying on the natural elasticity of the lungs and an open chest to provide the flow of air in and out of the lungs.

Figure 1.6 Approximate percentage contribution of the main muscle groups of respiration
I have purposely simplified the number and extent of muscles involved in normal respiration to help you identify the way in which you breathe currently, and how you might be able to change this. There are a number of additional muscle groups that can influence inhalation and exhalation, especially during physical activity. You will not need to know these muscle groups and what they do to make use of this book, but if you want to read further into this, they are listed in Table 1.1.
Table 1.1: Other muscles that have a part to play in respiration
| Inhalation | Exhalation |
| Latissimus dorsi (arms elevated) | Latissimus dorsi |
| Serratus anterior (arms elevated) | Abdominal muscles |
| Upper trapezius | Quadratus lumborum |
| Serratus posterior superior | Serratus posterior inferior |
| Sternocleidomastoid |
The most recent research done into the actions of the muscular system shows that the muscles do not work alone to provide the tension to move the skeleton and the body. There is another tissue that is understood to have profound effects on the postural positioning of the body in the static positions we adopt whilst at work or at rest. These tissues are known collectively as ‘fascia’. Fascia is essentially connective tissue that helps to support and define the structure of muscles and organs, rather in the same way that the segments of an orange have distinct divisions. The fascia is thought to help take the strain of the muscles when they are overworked consistently over a long period of time. Fascia used to be called sinew. These structures are exceedingly strong and not only attach muscles to bone but can develop under the strains of gravity, caused in the main, by habitually poor posture. They tend to strengthen and tighten when we are inactive and when muscles are being continually overworked. This overuse is thought to cause the fascia to effectively become tight, leathery and dehydrated. The change in the structure of the fascia throughout the body, along with the muscular stiffness and joint rigidity that accompanies it, is thought to limit the natural flow of lymphatic fluids around the body, further increasing the incidence of discomfort or pain.
The control of breathing
Normally, breathing is automatic and subconscious for us all. The body does this by way of the autonomic nervous system. Our autonomic nervous system controls the rate and depth of our breathing, just as it controls other essential bodily functions like heart rate, blood flow, the endocrine system (hormonal), the transit of food through the digestive system, urination and sexual function. Autonomic control enables us to maintain a correct balance in the body from relaxed sleep, right the way through to the most vigorous forms of exercise.
The one time we will definitely have had to think about our breathing is when we have done an active sport or vigorous physical activity. Who remembers the burning-throat sensation of doing a school cross-country or another endurance-based sport that pushed us close to our physical limits? Others will think about the way in which they control their breathing when swimming, sequencing the breath with a stroke to prevent them sucking in water. The more musically minded may have played a wind instrument or sung, where breathing control was essential and required training and practice. Other than in these situations, very few of us continue to challenge our lungs mechanically over our extended lifetime.
In western societies, our modern way of living is becoming more and more sedentary. It is little surprise that most people who develop COPD only really become aware that they have a problem when they can’t do simple daily tasks – tasks that have taken years or even decades to become an issue.
The rate and depth of our breathing are driven in the main by our body’s balancing our blood pH, ensuring the correct levels of acid (oxygen) and alkali (carbon dioxide) are maintained. The lungs themselves have the ability to dilate the larger airways and this action of the smooth muscles around the airways is completely under autonomic nervous system control. The smooth muscles in the lung airways also have pressure receptors in them, and these can feed back directly to the brain informing us how pressurised our lungs are.
Fortunately, we are able to override the rate and depth of breathing by conscious effort, and this book will aim to show you how you can control your breathing in a variety of ways to engage your brain before you ask your body to do anything physically challenging.