7
The Lancer Anti-Aging Method for Acne-Prone Skin
If you are lucky, you might wonder why an anti-aging book has a chapter on acne. You might assume that pimples are a thing of the past, a bad memory from adolescence. The fact is that 30 percent of women and 20 percent of men from the ages of twenty to sixty are troubled by acne breakouts. Though teenage boys have more acne scarring than girls, women are more likely than men to have adult acne.
Though a bad case of acne can have a negative impact on the self-esteem of an already self-conscious teenager, a breakout or even a single pimple can be a major source of distress and embarrassment for an adult. Adolescent acne lesions tend to appear on the upper half of the face. Adult acne is usually concentrated in the central part of the face and along the jawline. Adults get isolated pimples, but they are whoppers. Teenage breakouts are mostly superficial. In contrast, acne lesions in adults are deep under the skin and become cystic. Adult skin can develop enlarged pores and ruddiness along with acne blemishes.
For some, acne has been a constant state since their teenage years. Others experience a recurrence after years of clear skin. Breakouts can occur for the first time during pregnancy, perimenopause, menopause, or times of extreme stress. Many women and men are dealing with acne at the same time they are trying to combat the effects of aging on their skin. Of the sixty million Americans who have acne, twenty million have it severely enough to cause scars.
It might surprise you to know that acne and aging are on the same spectrum. The mechanisms and physical processes that cause your skin to age are also responsible for acne. Changes in the balance of the epidermis create the conditions that result in clogged pores, the root of this common skin disorder. Acne is associated with abnormalities in epidermal barrier functions. The Lancer Method works to heal acne in the same way it revitalizes and restores aging skin. Before we get to the cure, we have to understand the problem.
THE MAKING OF A PIMPLE
Acne is a disorder of the pilosebaceous unit or PSU. This unit consists of sebaceous or oil glands connected to a follicle that may or may not produce a shaft of hair. For every hair on your body, there is a corresponding skin pore, but not every pore houses a hair. Pores are found everywhere except the palms, soles of the feet, lower lip, and parts of the genital area. PSUs are densest on the face, neck, chest, back, and shoulders. That is where the skin disruptions of acne occur.
When canals and pores become plugged with oil and dead skin cells, acne develops. A pimple forms when the sebaceous glands produce too much sebum. The severity of acne corresponds to the amount of oil produced. Normally, sebum keeps skin and hair moisturized. The oily skin of adolescence results from the hormone surge typical of that period of life, which leads to excessive amounts of sebum. After the age of twenty, sebum production begins to decrease. Hormonal imbalance caused by the menstrual cycle, pregnancy, perimenopause, and menopause leads to the reduction of estrogen and the relative increase of male hormones in women. That is why more women experience adult-onset acne. The proportion of male hormones becomes higher, creating an excess of sebum that leads to acne for some people.
Microcomedone
- The sebum combines with keratinocytes within the canal and cells ready to be sloughed off from the stratum corneum. The corneocytes become too sticky to shed and accumulate in the pores.
- The mix of dead cells and oil can form a plug in the canal. As the material builds up, a bottleneck is formed, called a microcomedone, a precursor to an acne lesion that is not yet visible. Microcomedones can develop into full-blown comedones that can be inflamed or not.
Inflammatory Immune Response
- P. acnes (Propionibacterium acnes) bacteria that normally live on the skin feed on the mixture of sebum and dead skin cells, thrive, and can set off an inflammatory immune response, drawing white blood cells to fight the bacteria.
Bursting of Follicle
- When the plugged follicle canal can no longer hold its contents, the pus bursts and spills into the dermis, resulting in a spreading inflammation and more tissue destruction.
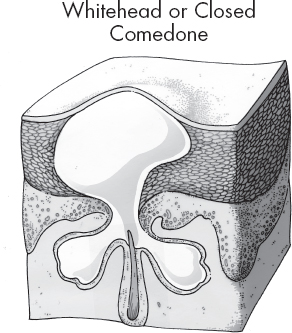
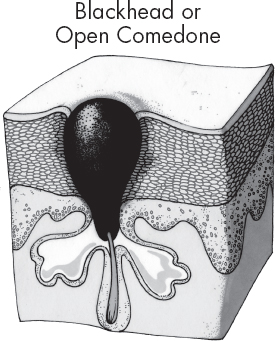
A microcomedone can evolve into a number of different lesions that represent the stages of acne. Whiteheads and blackheads are comedones that are not inflamed.
When the pore becomes clogged and bloated with the oil, dead skin cell, and bacteria mixture that stays beneath the skin, a whitehead or closed comedone forms. The area becomes a slightly raised bump on the skin.
With an open comedone, the mixture is exposed to air at the skin’s surface through an open pore, and the plug darkens. The pores become black spots or blackheads.
Comedones
Inflammatory Papule
If bacteria enter the picture, acne lesions become inflamed. The simplest form is called a papule, which is a small pink bump on the skin that is tender. The sebum-corneocyte mix builds up pressure on the cells surrounding the pore. Enough pressure will rupture the sides of the pore; the sebaceous material will leak into the surrounding skin, which gets infected when the P. acnes bacteria are released. The small red bump that appears is an inflammatory papule.
Pustule
An acne pustule, commonly known as a pimple, is the next stage. White blood cells have appeared at the site to fight off the P. acnes infection. White blood cells pile up and create pus at the tip of the bump, which is red at the base. Pustules are often mistaken for whiteheads for this reason.
Nodule
A more troublesome lesion is the nodule, a large, painful, solid lesion that is lodged deep within the skin like a boil at the level of the dermis. Nodules cause serious scarring.
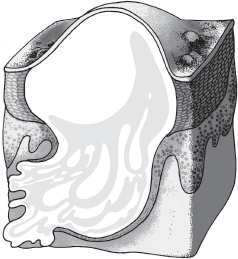
Cyst
Finally, inflamed, pus-filled cysts can form deep in the skin. Cysts are painful and also lead to scarring.
Cyst
If you want to stop acne from intensifying and doing serious damage to your skin, you need to consult a dermatologist. Over-the-counter remedies might help the occasional breakout, but you need the help of a board-certified dermatologist to avoid scarring and to stop acne’s progress.
WHAT IS BEHIND ADULT ACNE FLARE-UPS
Genetics
Whether or not you develop acne largely depends on your genes. Though being acne-prone is an inherited trait, the rising statistics indicate that the cause obviously goes beyond genetics. Lifestyle has a lot to do with it.
Hormones
An overproduction of androgens, or a change in the overall hormone balance in women and men, can cause breakouts. Large amounts of testosterone overstimulate the sebaceous glands, which produce an excess of sebum. During puberty, that hormonal surge causes real problems for male and female skin. As males mature, there is less fluctuation in their hormones than those of the opposite sex.
Females have a monthly cycle of shifting hormone levels. The premenstrual time is a red-hot flare-up zone, because androgens and oil production are high. Androgen-based birth control pills can cause increased oiliness and consequent breakouts. Hormonal fluctuations during pregnancy can also wreak havoc on a woman’s skin, resulting in pregnancy acne. The decrease of estrogen with age during perimenopause and menopause reduces the protective function of the female hormones, estrogen in particular. The balance shifts, and androgens have a more powerful effect, resulting in increased oiliness and breakouts.
Stress
Stress makes your skin more sensitive and reactive. It is a leading aggravating factor in acne flare-ups. In general, the body’s ability to resist infection is lowered by stress. Stress interrupts the healing process, causing new lesions to form and the breakdown of lesions that had begun to heal. Stress exacerbates any disease by setting an inflammatory cascade into motion. A chronically inflamed body is the ideal environment for the development of acne lesions. When you are stressed, your body produces cortisol and other stress hormones that trigger the production of more oil in your skin. Sudden stress can turn a non-inflammatory lesion into a painful nodule in less than twenty-four hours.
Diet and Acne
The role food plays in the formation of acne is surrounded by controversy. In the past, chocolate, french fries, other fried foods, and sweets were the suspected culprits. Then the thinking changed, and the link between diet and acne was treated as a myth. Now research is taking a broader view of the relationship between diet and acne flare-ups. With the rise in the incidence of acne in the United States, scientists have been studying the impact of the modern Western diet on the skin. They have found an association between obesity and acne. The consumption of dairy products, refined sugar, salt, and foods high on the glycemic index has been found to promote and aggravate acne.
Studies have found that obese people have higher levels of testosterone than people with a normal body mass index (BMI). That alone is enough to stimulate the overproduction of oils that can clog pores. Cow’s milk may contain steroid hormones and other components that precipitate a hormonal cascade, overstimulating the pilosebaceous unit described earlier. Processed food, so prevalent in the Western diet, is packed with refined sugar and salt. If you study the labels of processed foods, you will see sucrose, high fructose corn syrup, and salt close to the top of the list. Highly processed food is broken down quickly and converted to glucose, which causes spikes in blood sugar levels. High levels of glucose in the blood trigger the production of more insulin, which leads to inflammation and increased androgen levels. A high-carbohydrate diet can make you acne-prone.
If you reduce your consumption of simple carbohydrates, you will reduce acne symptoms. If you stay away from white foods—potatoes, white bread, white pasta, cakes, cookies, rice—and processed foods and refined sugars, you will reduce acne symptoms. Replace processed foods with whole foods that are high-fiber sources of carbohydrates, such as nuts, vegetables, beans, and fruits. Eat small meals and snacks often during the day to keep your blood sugar level stable. This will improve your acne while fighting aging. Chapter 11 will go more deeply into the right way to eat to look young and feel great, including foods that will stimulate estrogen production.
Medications and Drugs
Certain medications and drugs are known to aggravate acne conditions or cause them. Corticosteroids, mood elevators, anti-anxiety drugs, anti-depressants, certain cold and flu medications, recreational drugs, and DHEA can cause acne breakouts. Discuss the medications you are taking with your dermatologist.
Grooming Products
A major contributing factor for breakouts involves the products you use on your skin and hair. Many cosmetic products—shampoo, conditioner, soap, makeup—are comedogenic, meaning they are acne causing. There is even a form of acne popularly called pomade acne that is caused by hair products that seep into the forehead and trap bacteria in the hair ducts. Your hairstyle can cause or aggravate acne. For example, wearing bangs puts hair care products in direct contact with your skin. If you use products with spray applicators, the chemicals wind up on your face as well as your hair. It is best to keep products away from your hairline and to rinse your face to remove any styling product that remains on your face.
If you change your skin care products or add a new one, you are challenging your skin with new active ingredients, preservatives, and other additives. Your skin can react and break out. Introducing too many new acne products at once can cause blemishes. You should add new products to your regimen gradually, one or two at a time, and give your skin enough time to adjust. About four to six weeks is average.
Even products that are labeled non-comedogenic, water-based, or oil-free might still have irritating ingredients. You will find recommendations for skin care products for blemished skin later in the chapter.
EVERYDAY ACNE TRIGGERS
Genetics, hormones, stress, diet, medications, and cosmetic products constitute the big picture when it comes to the causes of acne, but there are myriad things that can negatively affect acne-prone skin. Making some small adjustments in your life and raising your awareness of situations that can bring on breakouts will help you to keep your skin clear and flawless. Sweat, dirt, and bacteria are major causes of breakouts, so limiting your skin’s exposure to these elements is a great place to start.
Here are a few ways to protect your skin from breakouts:
- Do not mess with pimples and blemishes yourself! This can spread bacteria and make the problem worse, or cause scarring.
- Change your pillowcase every few nights to avoid trapped bacteria.
- Avoid the use of fabric softeners on your towels and sheets—they can clog pores and cause irritation.
- Limiting your caffeine intake will reduce breakout-causing inflammation in the skin.
Facial Hair Removal
Waxing, tweezing, depilatories, and laser removal can make skin tissues swell, sending bacteria and skin cells deeper into the pore and follicle shaft. You might be trading facial hair for bumpy skin that itches. Use 1 percent hydrocortisone before and after you defuzz.
Telephone Acne
The surfaces of cell phones and phones in general collect bacteria. The warmth and moisture from your mouth create a perfect environment for bacteria to thrive. Phones are held close to your face and can cause friction acne. It is a good idea to clean your phones with an alcohol wipe or hand sanitizer daily. While you are at it, clean your eyeglasses and sunglasses.
Do Not Wear Makeup at the Gym or When You Are Sweating and Other Workout Tips
Makeup will block your pores and prevent elimination of toxins. It will also suffocate your skin. Wear wicking fabrics for a hard workout. Sweating in tight clothing can lead to excessive oil production and cause acne on your chest and back. Skin swells from freshly oxygenated blood sent to feed working muscles. Perspiration produces acids and salts to cool the body. Combined with the swelling, this is a perfect formula for skin irritation and dryness. Sports glasses, helmets, hats, and headbands should be cleaned well and often if you want to avoid breakouts.
Be Mindful of the Stresses of Travel
Aside from the ordeal of security checks, catching trains and planes, and traffic, the change in your environment created by traveling can affect your skin. If you are going to a tropical climate, heat and humidity can cause acne flare-ups. You sweat to cool off your body, and the acids and salts in perspiration can dry your skin and increase inflammation. If you are traveling to a place that is frigid, cold and ice cause your skin to get thinner. That can be a good thing if you have lesions.
When you are traveling, wash your face with bottled water, because your skin may react to different minerals in the tap water. Avoid using hotel soaps, shampoos, and conditioners, because introducing new products can cause your skin to react.
Pick the Right Non-Irritating Sunscreen for Your Skin
The chemical agents that protect your skin from harmful UV rays either are absorbed by your skin or rest on the skin’s surface to create a sun shield. The physical agents that stay on the surface can be bad for acne-prone skin. The ingredients zinc oxide and titanium oxide may sit on the surface and cause sweating that becomes irritating. Use products with avobenzone, oxybenzone, methoxycinnamate, or octocrylene in combination with physical blocks.
Limit Your Caffeine Intake
Drinking coffee or highly caffeinated beverages launches your body into a stressed-out state. What you perceive as energy is created by the fight-or-flight hormones that kick in and create inflammation. To keep your energy high, switch to a diet rich in complex carbohydrates.
THE LANCER METHOD TO THE RESCUE
The basic three-step Lancer Method—polish, cleanse, and nourish—works wonders for acne-prone skin. You will have to use products created specifically for blemished skin. They are formulated to be gentle and non-irritating and to neutralize the bacteria that cause inflammatory acne. You should not use the same products teenagers use. Those products are designed to reduce extreme oiliness. Older skin can be dry and still have acne breakouts. If your skin gets too dry, you will exacerbate acne lesions.
The fine-tuned Lancer Method for skin with problems will require some judgments from you. You will have to observe how your skin behaves and respond accordingly when introducing new products to your regimen. You want to prevent your skin from becoming seriously inflamed and to calm it if it is. For example, if your skin is oily, large-pored, and inflamed, you will want to ease into the three steps. You do not want to risk irritating your skin more. I suggest that you polish just once every other evening the first week and then every evening, five days a week. When your skin is used to that, polish every night. Then repeat introducing the polish step in the morning, so that you will eventually be exfoliating gently twice a day. If your skin gets red, irritated, and dried, cut back on the polishing. You have to judge how much your skin can benefit from this polishing to reach maintenance.
Active Ingredients in Acne Treatment Products
You should be familiar with the five ingredients that you will find in most acne products:
- Benzoyl peroxide is used in over-the-counter and prescription products for acne. Benzoyl peroxide dries up excess oil, kills bacteria by flooding them with oxygen, and mildly exfoliates. It can soften up plugs in a couple of weeks and keep more from forming. It is available in strengths from 2.5 to 10 percent. Unless your skin is extremely oily, you should use the lowest strength for adult acne; otherwise, it can cause dryness, scaling, redness, burning, and stinging. Available in gels, lotions, and pads, benzoyl peroxide is sold under various brand names. For older skin, I recommend using mild formulated products that contain this effective blemish fighter. You do not want to dry out your skin. Use it carefully, because it can bleach clothing and hair.
- Salicylic acid prevents the pores from clogging by gently increasing cell shedding inside the skin pores. When applied, it can sting and cause irritation. Over-the-counter acne products are available in strengths of 0.5 to 2 percent. Brand names change. Look at the label. Some products are better suited to younger skin.
- Two alpha hydroxy acids will appear on the labels of over-the-counter acne products: glycolic acid and lactic acid. Not only do they remove dead skin cells and help to reduce inflammation, but they also stimulate the growth of new, smooth skin that reduces the appearance of acne scars.
- Sulfur is combined with other ingredients, like salicylic acid, benzoyl peroxide, or resorcinol. It works to remove pore-clogging dead skin cells and excess oil. Sulfur may have an unpleasant odor, which is unmistakable, but it can be masked.
These ingredients can irritate the skin initially. It can take up to four weeks before the skin improves.
Polish for Blemished Skin
Exfoliating is especially important for blemished skin. Acne lesions form when pores are blocked by a plug composed of dead skin cells mixed with sebum. Bacteria can feed on the mixture, and your skin becomes inflamed. Keeping those pores open and exfoliating the dead cell buildup will prevent acne. Sloughing off dead skin cells from the surface of your skin will keep them from blocking pores and preventing the flow of sebum to the skin’s surface, where it moisturizes and makes the skin look fresh. Polishing also brings oxygen to the skin, increasing metabolism, which speeds up blemish healing.
If you have inflammatory acne and large pores when you begin using the Lancer Anti-Aging Method for Acne-Prone Skin, ease into it. Polish only one night the first week. Work your way up until you are polishing morning and night. You have to be very gentle if you have acne lesions. You do not want them to burst under the skin and infect surrounding areas.
For blemished skin, you have to find an exfoliant with larger, spherical buffing particles without rough edges to avoid irritating your skin further. If possible, try to sample an exfoliator before buying to be certain that the product is gentle enough for your sensitive skin.
Lancer Ethnicity Scale Guidelines for Acne Home Care
You have to become aware of your own biology and the way your skin responds to treatment. If you have acne, your skin is already overstimulated. Your goal is to calm inflammation, not to aggravate it. Be patient. Your skin will improve.
Introduce new products to your skin care routine gradually. See how your skin reacts. Slow down if your skin turns red or burns.
LES I or II: If you have very fair, sensitive, inflamed skin, you should begin the program by polishing your skin on alternate nights. Gradually work up to polishing in the morning and at night.
LES III or IV: If your skin is in the medium-tone range, polish nightly five out of seven nights.
LES IV or V: Olive and darker skins have a highly amped-up scarring response. Add the polish step to your regimen very slowly. Begin by exfoliating just one evening a week. There is no hurry. You do not want to irritate your skin further.
Sometimes home care can take you only so far. If acne breakouts persist after two or three months, it is essential for you to see a dermatologist. There are many treatment options that can be tailored to your condition.
When Home Care Is Not Enough: Medications to Clear Up Your Skin
If your acne persists and you see scarring and discoloration, you will need more than over-the-counter remedies to heal your skin. A dermatologist will prescribe one or more of the following medications for you:
- Topical retinoids, containing vitamin A derivatives, are the first-line therapy to treat inflammatory and non-inflammatory acne. Retinoids prevent pimples from forming by decreasing inflammation and helping the oil move out of the hair follicle/pore channel.
- Another topical approach is to use topical anti-microbials to act on P. acnes bacteria. They are often used in combination with other medications.
- Lightening creams are sometimes used to bleach the hyperpigmentation that can result after inflamed acne lesions heal. These reddish purple marks will fade eventually, but you can speed the process. Make certain to use an oil-free sunscreen and avoid the sun.
- Hormone therapy in the form of oral contraceptives can clear adult acne in pre-menopausal women. Sometimes the contraceptives are used with an anti-androgen drug such as spironolactone. Acne clears up because the overactive sebaceous glands are suppressed.
- Taken orally or applied topically, antibiotics reduce bacteria and inflammation. Treatment usually begins with a high dose that is reduced as the skin improves. I am not a big fan of this approach, as overuse of antibiotics can lead to a weakened immune system, and can cause damage to the digestive system. Antibiotic resistance is another issue.
Procedures to Deal with Acne and Its Effects
If you are under the care of an experienced dermatologist, there are a number of procedures that can speed the healing process and reduce the evidence of acne on your skin.
Chemical peels: A series of light chemical peels of glycolic acid and other chemical agents can loosen blackheads, decrease pimples, and help to fade spots that remain on the skin. Usually four to six treatments are needed to improve the skin.
Microdermabrasion: This treatment removes the surface layer of the stratum corneum with a handheld device that blows crystals onto the skin. These crystals polish the stratum corneum. A vacuum device then removes the crystals and the sloughed-off skin cells. The procedure should be supervised by a dermatologist. Too aggressive a treatment could discolor acne-affected skin further. A series of treatments is necessary to restore the skin. If your skin forms exaggerated scar tissue or keloids, chemical peels and microdermabrasion could make your complexion worse.
Extraction: Removing comedones by extraction can be helpful. Dermatologists use a sterile device the size of a pen to extract whiteheads and blackheads. The procedure should only be done by a dermatologist or a trained medical professional under the close supervision of a dermatologist. Never try to do this or drain a cyst on your own by picking or squeezing, which can make your acne, scarring, and infection worse. Your injured tissue can become infected by staph, strep, and other bacteria.
Drainage and extraction: When large cysts do not respond to medication, drainage and extraction, also known as acne surgery, may be required. In the hands of a dermatologist under sterile conditions, this procedure will reduce the pain of a cyst and decrease the likelihood of scarring. Trying to do this yourself could lead to serious infections and disfiguring scars.
Light therapy: In some cases, light therapy, also known as photo-rejuvenation, may be an option for treating skin discolored by acne. A variety of methods involving light can improve acne. Exposing your skin to different types of light can kill P. acnes bacteria. One method uses a chemical that makes the oil gland and follicle sensitive to light; a bright light in the form of a laser, intense pulsed light, or an LED lamp is then applied. Blue light is the most commonly used wavelength, but a combination of blue light and red light has proven to be effective. There are many at-home devices available in a broad range of prices. In the office, intense pulsed light is used with a suction apparatus to clear plugged-up follicles before applying laser energy.
Diode lasers: This laser treatment reduces sebum production by destroying some of the sebaceous glands that exist in the dermis. This approach combines an infrared laser with skin cooling to target oil gland production. This type of treatment can help to even out skin discoloration and resurface acne scarring by removing the outer layers of the stratum corneum. Diode lasers stimulate collagen and elastin production as well.
High-intensity lasers: CO2 lasers, for example, reduce or resurface acne scarring by removing the outermost layer of skin. Laser treatments can be painful. Topical painkillers are used during the procedure. You have to plan some downtime for laser treatments, because redness can result, which usually subsides within a week. Lasers are usually used on darker skin only when nothing else works, because the treatment can intensify hyperpigmentation.
ACNE SCARS AND WHAT TO DO ABOUT THEM
Whether or not acne lesions leave scars is primarily up to your genetics. If you have any family members with severe acne, you should be certain to get early treatment the minute you experience acne symptoms, because your risk of developing severe acne may be high.
Your acne has to be under control before you tackle its lasting effects. Treatment of scars is based on where the scar is located, how big it is, and how long it has been there. Scars left behind by acne lesions are either depressed or raised and call for different treatments. With age, both types of scars become more noticeable.
Depressed Scars
Depressed scars are soft, saucer-like pits in the skin. These depressions are formed when the skin has lost its underlying support. There are three types of depression scars: rolling scars, boxcar scars, and ice pick scars. Rolling scars give the skin a wavy texture. Boxcar scars look like large pores with box-like walls. Ice pick scars are deep pits with narrow openings that look as if the skin has been punctured.
For depressed scars, acne surgery removes, raises, and fills the pit by separating the scar tissue from the underlying skin. This procedure replaces a large, deep scar with one that is smaller, flatter, and generally less noticeable. After healing, the procedure is followed by skin resurfacing. Surgery involves downtime for healing, and bandages must be changed at home. The bruising can last one or two weeks.
Ablative laser treatment can be effective for ice pick and shallow boxcar scars. Antibiotic soaks must be used after this procedure. Recuperation is usually about two weeks, after which people begin to see improvements that can continue up to eighteen months.
Fillers have become popular because they can diminish depressed acne scars immediately. Collagen; hyaluronic acid; polymethyl methacrylate (PMMA); poly-L-lactide acid (PLLA); calcium hydroxyapatite (CHA); or your own fat is injected to plump up the scars. Most fillers are temporary, lasting about three to six months. When scars are filled with your own fat, extracted by liposuction, the results can last up to three years. PMMA is a semi-permanent filler.
Chemical peels and microdermabrasion can be part of the treatment plan to resurface the skin.
Raised Scars
Raised scars come in two varieties. A keloid scar grows beyond its original border. This type of scar is extremely thick, rubbery, and large. Keloids tend to form on the chest, shoulders, upper back, and sometimes earlobes. They are more common in LES IV and V. Keloid scars often require more than one type of procedure. A hypertrophic scar does not grow beyond its border.
A series of intralesional injections can help to reduce raised scars. The injections are made one lesion at a time. Anti-inflammatory agents can often shrink the keloid and make it feel smoother. Corticosteroid injections have the same effect. Some patients have an injection every two or three weeks, others every three to six weeks. If the scar does not respond by the fourth week, scar surgery might be recommended. Most keloids have a high risk of returning if the surgery is not combined with other treatments, including pressure garments, injections of corticosteroids once a month for a few months, and radiation, which can prevent the return of raised scars.
Pulsed dye lasers (PDLs) can be effective for treating both types of raised scars. Treatment can help to reduce the itch and pain, flatten a raised scar, and diminish the color. For people with fair skin, intense pulsed light (IPL) also may be a treatment option.
Cryotherapy, a treatment that freezes scar tissue, causes the tissue to die and fall off. Combined with corticosteroid injections, cryotherapy can diminish hypertrophic scars and flatten some keloids.
So much can be done now to treat acne and to reduce scarring that with persistence, you will be able to control outbreaks and erase some of the scarring acne might leave behind. Lifestyle adjustments can make a big difference.
Next on the scale of inflammation is rosacea, a disorder that can take many forms and varies from person to person. Rosacea is often misdiagnosed as acne or dry skin because various types of its symptoms are similar to those conditions. Rosacea is a physically uncomfortable disorder that requires special attention.
