9
Intestinal Flora and Infectious Diseases
Understanding the Relationship
As we’ve discussed, ailing intestinal flora will not protect the body as well as it should against exogenous infections, and it can even become a source of infection itself. It is therefore in your best interest to learn how to keep this flora healthy and how to restore it if it becomes imbalanced. But let’s first take a look at just what the intestinal flora is.
THE INTESTINAL FLORA
Our entire digestive tract is completely sterile at birth, meaning that no microbial flora is present. Microorganisms enter it quite quickly, however, and colonize it. Some are transported by the air that is inhaled and travel through the upper respiratory tract into the digestive tract; the majority make their way there, however, through food. In the beginning, these microbes are essentially the bifidus bacteria contained in a mother’s milk. Later, there will be a full variety of bacteria and other germs coming from water, fruits, vegetables, dairy products, and so forth.
The digestive tract does not provide a favorable environment for all the germs that enter it with food. Some of these germs perish quickly because the living conditions there are too adverse for them. Others, to the contrary, find ideal living conditions there and multiply in large numbers. This multiplication can attain vertiginous heights; the four hundred to five hundred different species of germs that make up the intestinal flora—the word germ can, in fact, be used instead of microbe when discussing this environment—form a population of several hundred billion individuals (1014), a figure that is larger than the number of cells in the entire human body!
The germs of the intestinal flora are not divided up uniformly. Their number varies depending on the part of the digestive tract in which they are located. The germ content of the mouth is average, in comparison to the other parts of the digestive tract, while germs are practically nonexistent in the stomach because the high acidity of the gastric juices (which range from pH 1.5 to 5) kills the vast majority of the germs that travel through it. Only a small number survive to reach the intestines. These germs will then multiply to form the intestinal flora.
In the first half of the small intestine, the flora is quite abundant, with between one thousand and one million germs per 0.04 inch. Germs are even more numerous in the second half of the small intestine and the ascending colon that extends from it, but the numbers diminish somewhat in the descending colon. (See figure 8.) Like all living beings, these germs die and their cadavers must be expelled from the body. Their number is so high that they represent around half the weight of the stools.
The different kinds of bacteria that make up the intestinal flora do not all colonize the same parts of the intestines. Aerobic germs (which require free air and oxygen) are naturally located in the upper half of the small intestine, at the level of the duodenum and the jejunum, because the air held by the stomach can easily enter there. Among these germs we find the enterococci, the colon bacilli (E. coli), the streptococci, the staphylococci, pseudomonads, citrobacteria, and so forth.
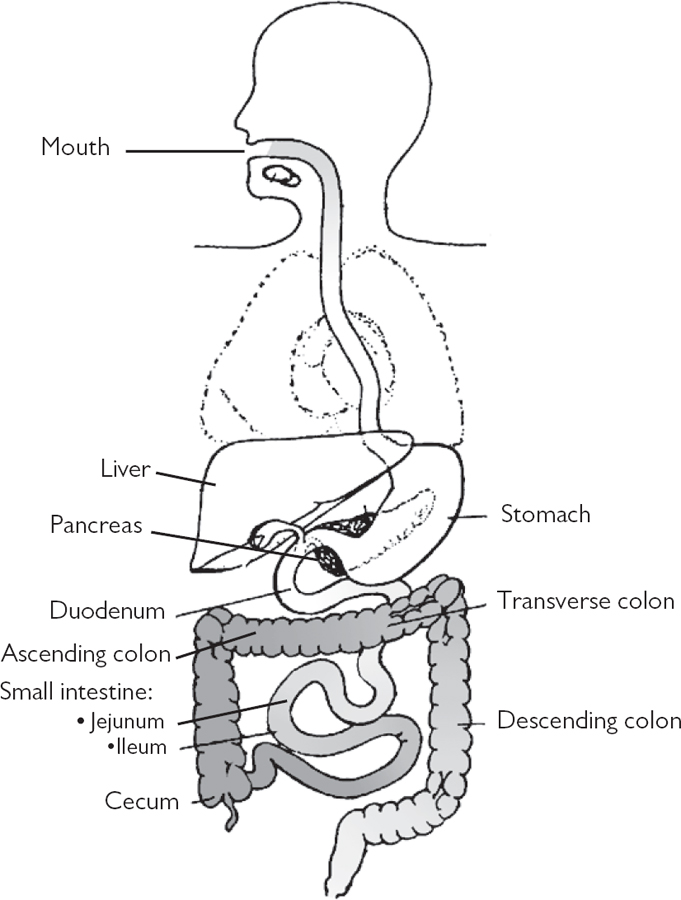
Figure 8. Distribution of the microbial flora
Anaerobic germs (which have no need of oxygen) inhabit the enclosed spaces that are oxygen poor, including the second half of the small intestine (the ileum) as well as the colon. These germs include the fusobacteria, anaerobic streptococci, and clostridia; the aspergillus and Candida albicans fungi; and also the well-known lactic acid–producing lactobacilli and bifidobacteria, which contain a number of varieties.
The anaerobic intestinal flora can be subdivided into two distinct groups of germs, each of which has a different role in the digestive process: the germs of fermentation and the germs of putrefaction.
The Fermentation Flora
The flora of fermentation inhabits the second half of the small intestine, the ascending colon, and the transverse colon, with the bulk of their population at the cecum and in the ascending colon (see figure 9). The lactobacilli acidophilus and bifidobacteria are the most widely present germs of this flora.
As their categorization indicates, the role played by these germs is to trigger the process of fermentation. They work primarily on long carbohydrate chains (complex carbohydrates) that form the hard fibers that make up the framework of plant tissues: the ribs of salad leaves and the skin of fruits, for example. Their purpose is to break down these fibers in order to free their nutrients. In fact, fibers like pectin, inulin, and lignin cannot be digested by the digestive juices released by the stomach, the liver, and the other digestive glands of the human being.
So these fibers arrive intact in the intestine. Their transformation can be realized, however, by the microorganisms of the intestinal flora, in a way similar to that which takes place in the digestive tract of herbivores.
The fermentation produces a variety of acidic substances: lactic acids, acetic acids, propionic acids, butyric acids, succinic acids, and carbonic acids. These substances acidify the part of the intestines in which they are released. They thereby create a slightly acidic environment (pH 6 to 6.8), which, far from being a threat to the intestinal flora, actually encourages its survival and sustains its development. A welcome side effect of this slight acidification is the intestinal peristalsis it stimulates.
The Putrefaction Flora
This flora is located in the terminal portion of the colon—that is, the small portion at the end of the transverse colon—and in the entire descending colon (see figure 9), where its concentration is strongest.
The role of the putrefaction flora is to break down food particles that have not yet been digested. At this stage of digestion, these particles consist primarily of protein residues: meats, fish, eggs, and so forth. The carbohydrates—even those that are hard to break down—will have been already digested a little higher in the tract by the flora of fermentation.
This decomposition through putrefaction creates more or less toxic wastes that will be neutralized by the liver. These include ammonia, phenols, indoles, skatoles, and hydrogen sulfide, as well as ptomaines, formed from the breakdown of amino acids. Because these are alkaline substances, they make the descending colon an alkaline environment (pH 8), which encourages the development of putrefaction germs.
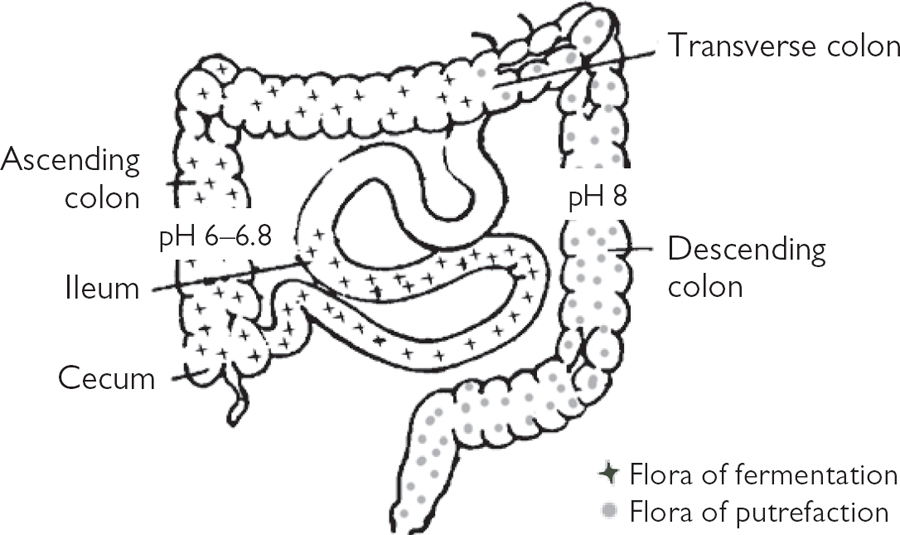
Figure 9. Distribution of the intestinal flora
IMBALANCES IN THE INTESTINAL FLORA
Together, the flora of fermentation and the flora of putrefaction make up the intestinal flora of the human being. The quality of the entire intestinal flora is dependent upon the balance between these two groups of germs. It is clear that the fermentation flora are the predominant group, as these germs colonize a much larger portion of the intestines than the germs of putrefaction, including the entire small intestine (16+ feet) and a large part of the colon (around 3 feet), compared to the descending colon (around 1½ feet) for the germs of putrefaction. We can therefore accept that a healthy intestinal flora would consist of 85 percent flora of fermentation and 15 percent flora of putrefaction. These proportions are normal and guarantee health. Any alteration in these figures, in contrast, is a sign of imbalance and poor quality in the intestinal flora.
What are the circumstances that bring about such changes? To answer this question, it is necessary to remember that the germs of the intestinal flora, as saprophytes, depend for their survival on the food we eat, as this food is what they themselves feed on. Their numbers increase, therefore, when the foods they require are present in abundant amounts and decrease when the quantity of these foods is reduced.
It so happens that the typical diet of most people today has insufficient levels of fruits, vegetables, and whole grains, and thus is low in the fibers that the germs of fermentation need. To the contrary, it has high levels of meat and various proteins, the preeminent foods of the germs of putrefaction. The consequence of this imbalanced intake is that the flora of fermentation population shrinks while that of the flora of putrefaction increases. These changes can become so drastic that it is estimated that more than 90 percent of the world’s population actually has directly reversed proportions of these germs. In other words, in the majority of the populace, there is a ratio of 15 percent flora of fermentation to 85 percent flora of putrefaction.
When the proportions are reversed in this way, the germs of putrefaction become too abundant to remain confined in the descending colon. In order to survive, they must expand their living space. They will therefore spread out beyond their normal territory in the direction of the transverse and ascending colons. This expansion is possible and made even easier due to the fact that the flora of fermentation that should be abundant in that space is now widely scattered because of the imbalance. It therefore no longer has a strong presence to block the advance of the germs of putrefaction, as it would with a healthy balance. Furthermore, because their numbers are reduced, the acidity the germs of fermentation should produce—which is another barrier against invasion by the germs of putrefaction—no longer exists. The environment will have become more alkaline, which offers favorable conditions to the invading putrefaction germs, as they need an alkaline environment in order to multiply.
THE HARMFUL EFFECTS OF AN IMBALANCED INTESTINAL FLORA
The harmful consequence of the demographic explosion of the flora of putrefaction is that an excessive amount of ptomaines and other poisons is produced during the digestive process. That production is so excessive that it exceeds the liver’s capability to neutralize these poisons. These substances begin spreading into the tissues and gradually poison them. The organic terrain deteriorates more and more, which paves the way for a host of illnesses because of the clogging and overload.
The growing volume of toxic substances assaults the intestinal mucous membranes. These poisons eventually carve microlesions into the intestinal walls. It so happens that one of the roles played by these walls is to prevent entry into the bloodstream and tissues of anything except useful substances like vitamins and minerals. Once they have been made porous by microlesions, they can no longer perform their job as a filter. The door is therefore open not only to toxins but to germs as well, with all the adverse consequences this can cause (we will address this topic in greater detail later in this chapter).
In addition to insufficient plant-based foods and excessive meat and other proteins in the diet, other imbalancing factors for the intestinal flora include the consumption of too much white sugar, coffee, tea, chocolate, and alcohol, but the primary culprit is taking conventional antibiotics.
Although the purpose of antibiotics is to kill pathogenic germs, they also destroy all other microbes with which they come into contact, or inhibit their development. Among these germs are those of the intestinal flora that are sensitive to their effect, which is primarily the case for the flora of fermentation: lactobacilli and bifidobacteria. These germs are all the easier to destroy because antibiotics are generally taken orally. Consequently, their action first appears in the upper digestive tract—the small intestine, headquarters for the flora of fermentation—and much less in the terminal portions—the colon, in which the flora of putrefaction is located. Taking conventional antibiotics therefore has the consequence of weakening the flora of fermentation to the benefit of the flora of putrefaction.
From the perspective of infections, an imbalance in the intestinal flora gives birth to two harmful consequences:
- A greater vulnerability to infection because the intestinal flora is no longer playing its protective role
- A greater risk that the intestinal flora can itself become a source of infection
THE PROTECTIVE ROLE OF THE INTESTINAL FLORA
Under normal circumstances, the four hundred to five hundred varieties of germs that make up a healthy intestinal flora cohabitate harmoniously. A balance exists between the various populations, the surfaces of the territories they occupy, the parts of the intestines they colonize, and the parts of the food to which each has a right.
This distribution, however, cannot tolerate the intrusion of a number of foreign germs. All the microbial resources in the intestines have already been judiciously exploited and will support no more. Furthermore, the intestines represent the ideal living milieu for all the germs of the intestinal flora, and none of them would be ready to surrender their place to invaders. They will fight against invasions, and to do so, either they will secrete antibiotic substances that kill the aggressors or they will occupy the terrain as vigorously as possible. In this way, the intestinal flora serve as a barrier to microbial pathogens.
A pathogenic germ that enters a digestive tract whose intestinal flora is healthy will find itself confronted by an entire series of obstacles: since the living space it needs to develop is absent, it will not have the food it needs, and the pH of the intestinal environment will not be suitable for it because it was established by different kinds of germs.
On the other hand, the situation is entirely different when the intestinal flora is deficient. Because they do not have to confront a strong and abundant population of germs, the pathogenic germs will find numerous spaces to conquer in the intestines and a sufficient supply of food. They will then establish themselves at a site where the living conditions are favorable, start multiplying, and drive out the existing germs, if only by imposing a pH balance that is harmful to them. Because these pathogenic germs have been given an opportunity to multiply, they will trigger an infection that would never have happened if the intestinal flora had been healthy.
The various diarrheas that Europeans and North Americans—or, more specifically, some Europeans and North Americans—catch so easily when they travel in the tropical regions of the world are due, at least for the more benign cases, to a deficiency of their intestinal flora. Germs enter the digestive tract of these travelers with the food they eat and the water they drink, and because their intestinal flora is not healthy enough to act as a protective barrier against those germs, the germs are able to multiply without any resistance.
INTESTINAL FLORA AS A SOURCE OF INFECTION
It is not necessary for a germ to enter the intestines for an infection to be triggered by an insufficient intestinal flora. It can also be caused by a germ that is part of the intestinal flora itself. In fact, this flora necessarily includes various pathological germs that perform their own specific role in the digestive process. Normally, their dangerous character is not given an opportunity to display itself because their numbers are limited. They will always remain in the minority as long as the intestinal flora is healthy.
The situation is, of course, entirely different when the intestinal flora has been weakened or partially destroyed. As it can no longer fulfill its role as a brake or protective barrier in these conditions, some pathogenic germs will multiply and trigger an infection.
Candida albicans, for example, is a normal resident of the intestine. Customarily, its population is extremely small and it plays an insignificant role. It would probably have remained completely unknown to the general public if the destruction of the intestinal flora by antibiotic therapy had not permitted its disproportionate multiplication in a large number of people. When virulent, candida colonizes the digestive tract, where it creates various disorders (gas, bloating, colitis, etc.), but it can also invade the rest of the body. A large number of fungal infections, as well as certain nerve disorders, can be traced back to this invader.
Other regular residents of the intestine that are potentially dangerous are the staphylococci and streptococci, germs that are well known for causing a wide variety of infections such as boils, sore throats, rhinopharyngitis, otitis, septicemia, pneumonia, arthritis, urinary infections, and so on.
Among the other pathological germs that can normally be found in the intestinal flora are Escherichia coli (which, when virulent, can cause enteritis and urinary infections), klebsiella (respiratory infections, digestive tract infections, and infections of the urogenital system), shigella (dysentery), salmonella (typhoid), and so forth. As can be seen, the infections they cause are not confined to the intestines. When the intestinal milieu is not healthy, these germs can travel to other organs. They can climb up the digestive tract to reach the upper respiratory tract, or they may colonize the genitourinary tract. Some of them leave the intestinal milieu through tiny lesions in the intestinal walls, and the bloodstream then carries them to other parts of the body.
By losing its role as a protector, the intestinal flora can become a source of infection not only through the pathogenic germs it contains but also through those that appear from time to time as mutations.
The transmission of hereditary characteristics takes place rapidly and frequently in germs, as a new generation can appear every twenty to sixty minutes. The risk of a transmission error, and thereby the possible appearance of a mutant, is therefore much higher here than elsewhere. A mutant germ possesses a characteristic different from those of its parent line. Sometimes that new characteristic may be resistance to antibiotics (see chapter 5); in other cases, it may be a virulent nature—in other words, it initiates a germ lineage that is not peaceful but pathogenic.
Normally, a germ like this does not manage to establish a presence in the overpopulated milieu of the intestines. It will perish quickly, destroyed by the other germs or weakened by the adverse conditions of the environment. However, it can sometimes happen that because of deficient intestinal flora it manages to survive or, worse, to multiply and cause an infection.
This flora can also become a source of infection when the digestive processes do not perform properly. Insufficiently digested foods and the poisons produced by abnormal fermentations and putrefactions attack and injure the intestinal walls. Although little, these lesions allow nonpathogenic germs to leave the intestinal milieu and make their way into other parts of the body. It so happens that a germ that is harmless in the intestines is not necessarily so in another organ. The body can be extremely vulnerable to its presence because, by multiplying, it will attack our tissues and make us sick.
HOW TO BUILD A STRONG AND BALANCED INTESTINAL FLORA
Imbalances in the intestinal flora are primarily characterized today by an imbalance between the germs of fermentation and those of putrefaction. Now, given the fact that generally the flora of fermentation has become weaker and allowed the flora of putrefaction to grow stronger, it is first and foremost necessary to address the first in order to correct the second. It will be helpful at the same time to reduce the intake of proteins, especially those of meat, which support the germs of putrefaction.
There are two different approaches to strengthening and increasing the flora of fermentation. If it is only slightly below optimal levels, eating correctly is often sufficient to get these bacteria to start multiplying and to win back their rightful place. To do this, prebiotics are the natural choice. These are foods or supplements that contain the most desirable food for the germs of fermentation. However, if the flora of fermentation has been heavily damaged, it is not enough to correctly nourish the remaining germs for their numbers to increase quickly. The competition with the germs of putrefaction, which have gotten the upper hand, is too brutal, and a more radical method should be used. In this case we must import a large number of germs of fermentation. Concretely, this means using probiotics, which are foods or supplements that have a very large number of these germs. In this way the population of the germs of fermentation will increase quickly and rapidly regain their normal proportions.
PREBIOTICS
These are nutritious substances that are necessary for the survival of the germs of fermentation. Providing prebiotics in abundance feeds and supports these germs, allowing them to become stronger and multiply more easily so that they can establish and sustain a more substantial population.
Fruits and Vegetables
Prebiotics are primarily made up of all the foods that have high levels of soluble fibers—in other words, carbohydrate chains of varying length such as pectin or inulin. These substances can be found in fresh or dried fruits, green and brightly colored vegetables, and unrefined grains (though not in the bran, which is too hard). These are all plant foods, the very same ones that the bacteria of fermentation need to transform to facilitate digestion, but they are also the very foods that are most often lacking in the modern diet.
This is why eating a portion of raw or cooked vegetables or green salad every day at the midday and evening meals will have a beneficial effect on the intestinal flora. These portions need to be large, however, so that the germs of fermentation will have enough fiber at their disposal to feed on.
Dosage
- Salad greens and/or raw or cooked vegetables at the midday and evening meal
- One piece of ripe fruit between meals
Whey
Lactose, or milk sugar, is a disaccharide consisting of a molecule of glucose and a molecule of galactose. It is one of the preferred foods of the bacteria of fermentation, which will happily gorge on it. And it provides one other advantage not to be overlooked: the digestion of lactose by the bacteria of fermentation will produce lactic acids, which, by slightly acidifying the small intestine and the first part of the colon, create an environment that is hostile to the multiplication of the germs of putrefaction. Lactose is the only sugar that acts this way.
Milk is 4.7 percent lactose. This is not a very high percentage; you would have to drink a lot of milk for it to have a beneficial effect on the intestinal flora. However, stronger concentrations of this substance can be found in whey.*6 Whey is a by-product of the manufacture of cheese from milk. It is the liquid expressed from the curd, or milk solids. You can find whey supplements in powder or tablet form in health food stores. There are many variations, with or without added flavors, which, when added to water, make a pleasant drink.
Dosage
- Intensive cure: 1 to 2 tablespoons of whey powder mixed with a glass of water, three to six times a day
- Maintenance dose: 1 to 2 tablespoons of whey powder mixed with a glass of water, one or two times a day
Note: Look out for the laxative effect that occurs with high doses of whey!
Lactose
Using modern procedures, it is possible to extract all the lactose from whey and convert it into a concentrate that is sold in health food stores. These concentrates are very pleasant to consume, and they contribute good nutrition for the flora and good acidification of the intestinal environment. It is easy to see how effectively lactose supplementation can regenerate the intestinal microbial balance; thanks to this cure, the production of gas and bloating that accompanies poor digestion due to imbalanced flora will vanish in the space of a few days.
Dosage
- Intensive cure: 1 tablespoon of lactose, mixed with water or a yogurt containing bifidobacteria, three times a day
- Maintenance dose: 1 tablespoon a day of lactose, mixed with water or a yogurt containing bifidobacteria, once a day

The beneficial effects of prebiotics are generally felt gradually, as the regeneration of the intestinal flora is a physiological process that can take some time. Among the prebiotics, fruits and vegetables should be eaten throughout your entire life, for this is in accordance with nature’s plans. This is not quite the case for preparations like whey and milk sugar, which are supplements to the diet. They should be taken in the form of month-long cures, two times a year, for example, or more often for people suffering from chronic disruption of the intestinal flora.
PROBIOTICS
Probiotic foods and supplements contain within themselves germs of fermentation that can integrate with the existing intestinal flora and help it rebuild. The germ concentration varies from one product to the next. Once they have been ingested, the germs make their way into the intestines and colonize them.
Probiotics represent a substantial intake of germs. They make it possible in a short time to increase the number of the germs of fermentation, without having to wait for those that are present to multiply in order to rebuild a destroyed flora.
Probiotic Yogurts
This is the preeminent probiotic food. Probiotic yogurt is rich in germs, because they play a significant role in its manufacture. If milk can be transformed into yogurt, it is in fact uniquely thanks to the action of the lactobacilli that cause the milk to curdle and remain in the product once the transformation has been completed.
To be beneficial to the intestinal flora, these germs must remain alive. This is the case when they have not been killed by heat. It so happens that during the preparation of most yogurts, the milk and bacteria blend is heated, which kills everything that is alive in it. The sole yogurts that contain living germs—those that will be able to live in the intestines and multiply there—are those that have not been cooked and that are expressly designated as “probiotic yogurts.” These kinds of yogurts are easy to find today, as their use has become widespread.
One important criterion in the choice of yogurts is the choice of germs used to make them. Some lactobacilli are not found in the intestinal flora of human beings and their ability to survive in the intestines is quite weak. These germs, though they may be used to make yogurt, cannot help regenerate the flora. At best they momentarily take up space and therefore act as a barrier against the bacteria of putrefaction, but only for a short time. This is the case with Lactobacillus bulgaricus, for example.
Lactobacillus acidophilus and Bifidobacterium bifidus, on the other hand, are normal residents of the intestinal flora. They are reasonably resistant to the acidity of the gastric secretions they will encounter during their passage through the stomach and easily get a foothold in the intestinal milieu, where they will remain once they are established. These germs are therefore indicated to rebuild the intestinal flora. Probiotic yogurts have an extremely high concentration of them. To rebuild intestinal flora that has been damaged or to keep it healthy during treatment with conventional antibiotics, you should not hesitate to eat three to five probiotic yogurts a day, or even as many as you like. Of course, it is better if these yogurts do not contain white sugar. For people who do not like plain yogurt, they can sweeten it with raw sugar, honey, or maple syrup, or, even better, lactose, which will offer a combination of prebiotic and probiotic effects.
Dosage
- Intensive cure: 3 to 5 probiotic yogurts daily, spread out over the course of the day
- Maintenance dose: 1 probiotic yogurt a day
Fermented Milk Drinks
Quite similar to yogurt but more concentrated are milk drinks that have been fermented with probiotics. They are sold in small bottles often labeled with names that begin with “acti” (such as Danone’s Actimel and Dannon’s Activia). They have high levels of probiotics; two to three bottles a day is enough to regenerate the intestinal flora. In order for the germs to properly colonize the intestines, it is necessary for the cure to extend over a period of several weeks. One bottle contains around six billion probiotic organisms (compared to the one billion organisms found in probiotic yogurt). This may seem like an enormous number, but it is not a large number for the intestines, as the normal intestinal population borders on several hundred billion germs.
Dosage
- Intensive cure: 2 to 3 bottles of probiotic milk drinks a day
- Maintenance dose: 1 bottle of probiotic milk drink a day
Freeze-Dried Probiotic Supplements
To rebuild the intestinal flora very effectively and rapidly, you might consider pharmaceutical preparations that are made from lyophilized (freeze-dried) probiotic germs. Lyophilization is a process that delicately dries the germs without killing them. When they reach the moist, warm environment of the digestive tract, they rehydrate and emerge from their forced slumber. Active once again, they colonize the intestines and begin to multiply. The content of these products can range from several dozen million to several billion germs.
Their effectiveness is especially easy to observe in the treatment of diarrhea, for which they are often recommended. The massive intake of germs in fact erects a barrier against the proliferation of the germs responsible for the diarrhea, and in this way they eliminate the illness.
The sanitary rules concerning the manufacture of these products are quite strict. The bacteria that are used for these preparations absolutely must be germs that are normal residents of the intestines. They must be held in the formulation alive or in suspended animation, and they must be capable of competitively occupying the intestinal milieu when confronting pathogenic germs and those responsible for putrefaction. Furthermore, the toxins produced by these germs must be harmless to humans but bacteriostatic to pathogenic germs.
Lyophilized bacteria come in the form of a powder to be mixed with water or as capsules.
Dosage
Numerous freeze-dried probiotic preparations are available commercially. Some popular ones include:
Belle + Bella Flora Restore
Bio-Flora
Dr. Mercola Complete Probiotics
Hyperbiotics Pro-15
Natren Bifido Factor
Nature’s Way Primadophilus Bifidus
Now Acidophilus & Bifidus
Pileje Lactibiane
Follow the instructions provided by the manufacturer.
Saccharomyces boulardii
The yeast (Saccharomyces boulardii) that is often recommended for an individual taking conventional antibiotics is not technically a probiotic. This living yeast is not a normal resident of the intestines and does not factor in the normal composition of the intestinal flora. It is not able to really establish a foothold in this environment, either, and will leave it within a certain period of time. Moreover, it does not inhibit the growth of pathogenic bacteria—that is, it does not have an antibiotic effect—and it has no nutritive value like brewer’s yeast. So why use it?
Despite these deficiencies, S. boulardii has the ability to blend in with the intestinal flora and take up space, which puts it in competition with the flora of putrefaction and certain pathogenic germs. In this way it contributes to the barrier effect of the intestinal flora. It is all the more equipped to perform this role because it is resistant to conventional antibiotics (hence its utilization during these treatments). So while it is not a probiotic, this yeast has its uses.
Generally speaking, brewer’s yeast and food yeasts are not probiotics either, but they can be used like S. boulardii if they are living and it is possible to bring them back to an active state. However, they are rarely used for this purpose because the majority of them are heated during their manufacture, and this kills all life. Only the yeasts that are sold specifically with living or lyophilized cultures, such as Arkopharma’s yeasts, can perform this barrier role.
Nevertheless, unlike Saccharomyces boulardii, brewer’s yeast and food yeast have a high nutritional value, which has a prebiotic effect for the germs of the intestinal flora.
REPAIR OF THE INTESTINAL MUCOUS MEMBRANES
In addition to taking prebiotics and probiotics, it is a good idea to encourage the regeneration of the intestinal mucous membranes. If they are in a damaged state, they are receptive to colonization by pathogenic germs; if they are torn or have lesions, they are open doors that allow germs to enter the tissues.
In addition to regenerating the intestinal flora, which will reduce the production of aggressive food toxins, one of the most helpful steps is to supplement with vitamins A and E and with omega-3 and omega-6 fatty acids, all of which have a regenerating effect on the mucous membranes.
Dosage
For omega-3 and -6 supplementation, choose one of the following:
- Flaxseed oil: 2 teaspoons mixed with a fatty food, like cottage cheese or fromage blanc, once a day; if flaxseed oil is unavailable, substitute 2 to 3 tablespoons of sunflower, canola, or safflower oil
- Borage oil: Capsules; follow the manufacturer’s dosage instructions
For vitamin E supplementation:
- Wheat germ oil: 1 to 2 teaspoons mixed with a fatty food, like cottage cheese or fromage blanc, once a day; or take capsules, following the manufacturer’s dosage instructions
For vitamin A:
- Halibut oil: Capsules; follow the manufacturer’s dosage instructions