Figure 8.1 Anatomy of the chest, showing the key organs lying within the chest cavity. (Ian Brown, Department of Anatomy University of Aberdeen)
Wounds of the chest have been associated with a high mortality throughout the history of war and there had been a general view that there was nothing that could be done to save these casualties. John Hunter, the famous British surgeon with a great experience in war surgery (see Chapter 7), stipulated that the casualty should be laid down on the side of the injury so as to let the blood drain out of the chest through the wound, and this was the only treatment possible. As understanding of the function of the organs in the chest developed and progressed, interest developed in these wounds, allowing the start of a more rational and scientific basis for treatment. Importantly, Patrick Fraser, a surgeon from the Crimean War, realised that fluid within the chest had to be drained and removed because its presence impaired the function of the casualty’s lungs.1 He also noted that it was often better to leave a bullet in the chest if the casualty was reasonably well as there was a possibility that a surgical operation to remove it would potentially cause more damage than leaving it alone.
In the Boer War, penetrating chest wounds were usually caused by a rifle bullet and were managed without surgery and often successfully. In 1914 at the beginning of the Great War, treatment of chest wounds was rudimentary and consisted mainly of trying to drain any fluid within the chest and not to embark on surgical operations within the chest. Perhaps the differing conditions in the Boer War, where wounds were sustained in relatively clean and dry conditions, in stark contrast to wounds sustained in the mud of France and Flanders, contributed to the belief that surgery was not necessary. Indeed surgeons in the Boer War attributed successful result of treatment with only approximately 9% of the wounded and 27% of those with penetrating chest wounds dying to “the climate, the sunshine, and the dry and pure air”.2 Furthermore, a lack of understanding of the physiology and function of the human body led surgeons to believe that it was not possible to operate on the chest without special equipment and that if the lung was touched there would be rapid and unstoppable bleeding.3 These were, of course, erroneous beliefs.
In the early years of the Great War, casualties with chest wounds had a high mortality in the same way that abdominal wounds had, until surgeons challenged the conventional ways of dealing with them. Several surgeons were instrumental in bringing about change, including Major A. Don, and Captains Roberts, Craig, Hathaway and Gask. These surgeons certainly led the way in the medical literature by reporting their experiences treating chest wounds in casualty clearing stations. Major Don, mentioned in Chapter 7 for his work in patients with abdominal wounds, really led the way and stimulated critical thinking because he was concerned by the “impotency” of the non-operative management of severe haemorrhage in casualties with penetrating chest wounds.4 In 1916 he began to manage these casualties by considering the way in which the chest wall and the contents of the chest worked under normal circumstances and decided to undertake an early operation to drain blood from the chest and arrest haemorrhage. This was successful and he published his technique straight away for other surgeons to consider and take forward.
All of these surgeons believed strongly that the management of chest wounds should follow the same principles as for wounds sustained elsewhere in the body. This meant surgery at the earliest possible time, to excise the wound by complete removal of all infected tissues and foreign material, and repair of the tissues by primary closure.5 The results they achieved were an improvement and were an important step towards a more active surgical management policy for casualties with penetrating chest wounds.6 7 8
Chest wounds were seen less commonly than wounds affecting other areas, due to the high risk of death associated with wounds to the vital structures lying within the chest itself. Around one-third of casualties who died on the battlefield either had an isolated chest wound or a combination of wounds including a chest wound. Chest wounds represented approximately 5% of all wounds requiring initial medical care but because of the deaths that occurred during transfer through the evacuation chain only represented approximately 2% of all wounds arriving at the casualty clearing stations.9 However, a specific expertise was needed, and developed, to manage these casualties and by 1918 approximately 70-80% of casualties with a chest wound survived if they reached the casualty clearing station.
Penetrating chest wounds were caused by the same projectiles that caused the abdominal wounds described in the last chapter. These were bullets (pistol and rifle), shrapnel balls, or high explosive shells, bombs and grenades. What caused the wound was extremely important because a bullet or shrapnel ball had the potential to go straight through the chest, penetrating the skin and muscle before entering the chest cavity on one side and coming out of the other. However, if it struck a rib or any other bone around the chest such as the scapula (shoulder blade) then due to the changes in its flight characteristics, as discussed in the last chapter, there was the potential to cause much more damage, with greater likelihood of damage and destruction of both the chest wall and the structures inside. In contrast, high explosives and fragments of metal usually caused more extensive wounds at the sites of entry and exit of the projectile and often the projectile dragged with it into the chest large amounts of clothing, soil and debris. Consequently these were much more serious wounds than those caused by a bullet or shrapnel ball, unless of course it had gone through the heart or a major blood vessel and caused a rapid death.
The importance of chest wounds is because of the damage caused to the function of the vital organs and structures which lie within the chest. The organs are enclosed by a semi-rigid protective cage consisting of skin, muscle and bone. The muscles provide a functional as well as protective layer of tissue lying under the skin but outside the chest cavity. They can firstly be categorised into those which are attached at one end to the chest wall and to the upper limb or shoulder blade at the other and have the principal function of moving the upper limb, for example the large pectoral muscles on the front of the chest wall. The second group of muscles is attached only to the chest wall, and act on the chest wall alone. These are the intercostal muscles which are attached to and between adjacent ribs. There are 12 ribs on each side of the chest in total and their function is concerned with respiratory movements, i.e. breathing in and breathing out, because as they rise and fall, contraction of the intercostals muscles swings the ribs out with a bucket handle type of motion allowing air to move in and out.
Figure 8.1 Anatomy of the chest, showing the key organs lying within the chest cavity. (Ian Brown, Department of Anatomy University of Aberdeen)
Lying directly underneath and on the inside of the chest wall and between the chest wall and the lungs, is a small potential space called the pleural cavity which is lined by a membrane (very thin lining on the surface of the lung and on the chest wall). These two layers normally stick together and this keeps the lung fully expanded. If, however, air gets into this potential space then the lung will collapse and this is called a pneumothorax and if blood gets into this space it is called a haemothorax. The lung(s) cannot then function and expand normally until the air or blood is removed from the pleural space.
The two lungs lie on either side of the chest cavity and are spongy in texture comprising thousands of air sacs. Air which is breathed in through the mouth and/or nose passes through the back of the throat into the airway called the trachea (windpipe) which runs inside the chest between the two lungs and then splits into two main branches one to take air to the left and the other to the right lung. The lung is where the air that is breathed in containing oxygen (which is necessary for all the body’s cells), comes into contact with the blood and oxygen diffuses into the blood stream. The blood flowing to the lungs contains a large amount of carbon dioxide, which has been produced by the body’s cells and needs to be removed. This gas diffuses from the blood into the air within the lungs’ air sacs and is breathed out.
Another major organ is the heart, which is simply a mechanical pump for the blood and divided into two halves, each with a different role but still nevertheless each is a pump. Blood returns to the heart having been returned from all the body’s tissue through two main blood vessels which are veins, called the superior and inferior vena cava. This blood needs to be oxygenated so this right side of the heart pumps it to the lungs through the pulmonary arteries where oxygen is taken into the blood and carbon dioxide is removed. The blood then comes straight back from the lungs through the pulmonary veins to the left side of the heart and the left side of the heart pumps this blood out through the aorta, which is the main artery running through the chest and the abdomen (see Chapter 7). Branches from the aorta are numerous and through these blood reaches all the body’s tissues before being returned to the heart through the vena cava as described above.
The oesophagus (gullet) also runs with the trachea from the back of the throat running along the length of the chest cavity at the back and lying behind the heart where it then passes through the diaphragm to enter the abdominal cavity and join with the stomach. The diaphragm separates the abdominal and chest cavities and is actually a thin sheet of muscle which contracts, moving upwards and downwards and helps to draw air into and out of the lungs. The structures in the centre of the chest, i.e. the heart and large blood vessels, the trachea and its branches which enter the lungs (trachea and bronchi) and the oesophagus (gullet) together with a variety of nerves are termed the mediastinum, and this is a commonly used anatomical term.
Very simply, therefore, as a result of trauma to the chest the three most immediate problems that the casualties faced were, lack of oxygen in the blood necessary to supply all the tissues and organs in the body, haemorrhage (bleeding) and failure of the heart to pump adequate amounts of blood around the body. However, a review of the deaths occurring in casualties with chest wounds categorised them as generally falling into one of three groups as shown in Table 8.110 11 and this information was particularly important for developing a rational plan of management for life-threatening and potentially life-threatening wounds (see Table 8.2).
Table 8.1
Causes of death after penetrating wounds of the chest
| Time of death | Cause of death |
| Death on the battlefield or within a few hours of admission to medical facility. | Injury to the large blood vessels in the chest or a massive wound that was too extensive to be treated surgically. |
| Death after 48 hours from sustaining the wound. | Usually infection within the pleural cavity. |
| Deaths at the base hospital seven days or more after the wound occurred. | These were due to infection. |
Taken from Stevenson, W.F., “Notes on surgical experiences of the Boer War”, Journal of the Royal Army Medical Corps 1903; 1: pp.93-8.
Table 8.2
Commonest life-threatening and potentially life-threatening situations
| Life-threatening | Potentially life-threatening |
| Obstruction of the airway Tension pneumothorax “Sucking” pneumothorax Large haemothorax Flail chest segment Cardiac tamponade |
Simple pneumothorax Haemothorax Perforation of the trachea and or bronchi Tears of the oesophagus (gullet) Rupture of the diaphragm |
The approach taken by the surgeons to perforating wounds of the chest was a very simple and understandable one. Wallace and Fraser12 recognised that simplicity was the key in being able to understand and treat the damage that had occurred, and they considered that the wound may be to:
• the chest wall at the site of the penetration,
• the lung underlying the chest wall, and
• the lung on the opposite side of the chest together with the structures in the mediastinum.
Working classifications of the different types of chest wounds evolved during the Great War and were found useful by all the teams in the evacuation pathway chain for management. Commonly, casualties were categorised on being admitted to the casualty clearing station as follows:13
• Type A – closed entrance and exit wounds and no foreign body retained
• Type B – open wounds with entrance and exit wounds or with entrance wounds and a retained foreign body
• Type C – open tangential wounds at the periphery of the chest circumference.
A further refinement was that those with Type A wounds were then categorised into those where the blood within the chest was infected and a second group where it was considered that the blood within the chest was not infected. This formed a basis for clinical management because those casualties in groups B and C proceeded to urgent surgery which had become recognised as the best treatment, whereas the patients in group A in whom it was felt did not have any infection within their chest did well without having to have any surgery performed on them.14 Other surgeons and teams had different ways of classifying chest wounds. An example is shown in Table 8.3 and perhaps this describes not just the structural damage but gives us more information about the effect the wound had on the patient.15 A “sucking” wound was one where air entered the chest through the hole in the chest wall each time the casualty breathed in and air within the chest cavity (air should be within the lungs themselves) then couldn’t get out again due to a tissue flap valve, so that pressure within the chest cavity increased greatly, compressing both lungs and stopping them from functioning. This was a potentially life-threatening wound.
Table 8.3
Alternative classification of penetrating chest injuries
| Class | Description | Occurrence |
| 1 | “Open” or sucking wounds with free air entry. | 19% |
| 2 | “Closed” wounds with large septic laceration of the chest wall. | 16% |
| 3 | “Closed” wounds with early signs of infection of haemothorax. | 10% |
| 4 | “Closed” wounds with no evidence of intraperitoneal infection. | 50% |
Data from Don, A., “Perforating and penetrating wounds of the chest with severe haemorrhage: a suggestion for treatment”, British Medical Journal 1916; 1: pp.816-817.
Perhaps the simplest of all wounds was the bullet (or shrapnel ball) which passed straight through the chest and did not have its flight characteristics altered in any way! However, as already explained, a fragment of metal from a shell or grenade was of variable size and often caused more damage to the chest wall. In addition, often the underlying ribs were broken and fragments of the ribs and the skin and muscle of the chest wall, or large segments, would be lodged inside the chest cavity. Clearly some of these wounds would be instantly fatal or not survivable from the time they were sustained.
The lung is a relatively large structure and with two occupying the majority of the chest these were nearly always damaged to a greater or lesser extent. The physical nature of the lung is very spongy as it comprises sacs containing air as explained above and it is relatively easy for projectiles to pass through causing damage. Damage was not limited to the track that the projectile had followed but there was also often bruising and bleeding of the lung further away and with wounds that had been sustained at a closer range then whole areas of lung could be affected in this way. If the larger blood vessels in the lungs were damaged then bleeding could be substantial and this might accumulate in the pleural cavity. This would compress the lung and impair its function to a varying degree. This is called a haemothorax.
It became apparent that it was not only the lung underlying the damage to the chest wall that was at risk but also the lung on the opposite side of the chest could suffer damage. This varied from a mild bruising to extensive changes throughout the lung which resembled a pneumonia (infection of the lung) when autopsies were performed on those who died. Nowadays, we recognise a condition known as adult respiratory distress syndrome (ARDS), which occurs at 24-48 hours after an injury or major trauma. When this happens there is an inflammation throughout the lung with fluid accumulating in the lung, impaired lung function and impaired exchange of gases within the lung substance which can result in death. Nowadays these patients are managed in an intensive care unit, and frequently need to have a period when they are put on a ventilator, a machine which breathes for a patient when breathing becomes too difficult. This allows the lungs to maintain oxygen levels in the blood stream until the inflammation resolves in the lung, but often these patients also have failure of other organs such as the kidneys and heart. Even today there is a significant mortality rate for such patients and this is probably what was happening to these casualties. The features of ARDS are summarised in Table 8.4 It is likely that many of those soldiers who survived the carnage of the Great War but died of the complications of Spanish flu in 1919 would also have died of ARDS occurring.
Table 8.4
Adult respiratory distress syndrome (ARDS)
| Causes (examples) | What happens in the lung? | Effects on the casualty |
| Major trauma Infections Pneumonia After surgery Drug reactions |
The body releases a variety of chemicals that cause inflammation in the lungs. Cells called macrophages and polymorphs (normally to fight infection) accumulate in the lungs and then release a further series of chemicals. This causes even more inflammation, fluid accumulation and damage to the lung. |
The lungs become swollen and fluid accumulates in the air sac where inspired air would normally be. The patient cannot then take into the body oxygen and so the levels of oxygen in the blood stream fall. The patient will become breathless and struggle to breath and even becomes so exhausted trying to breathe more deeply and more quickly that they stop breathing. The lack of oxygen in the bloodstream may lead to dysfunction in many other organs, leading to death. |
The casualties with penetrating chest wounds were usually in quite a distressed condition by the time they had gone through the chain of evacuation and arrived at the casualty clearing station. Not only were they generally very anxious, but they had varying degrees of respiratory distress and breathlessness due to impaired pulmonary function arising from damage to the chest wall, pleura or lung, or of any combination of these. This leads to a lack of oxygen in the blood stream (hypoxia) and failure to expel carbon dioxide resulting in dysfunction of all the body’s tissues and organs. In addition, they had often sustained blood loss with resultant hypovolaemic shock, which itself could lead to dysfunction of other organs and death (discussed in earlier chapters).
Prior to the casualties arriving at the casualty clearing station where the definitive and life-saving surgery would be undertaken, initial treatment would have been given at the regimental aid posts and advanced dressing station. It was standard practice to begin treatment by warming and resting the patient, and if there was an open wound involving the pleural cavity this was closed either by stitching the skin closed over the hole or by filling the hole with gauze and then applying a strong strapping over the top.
A detailed physical examination of the casualty would have been undertaken to ascertain how severe the chest wound was and to identify any other areas of the body that had been wounded, especially the abdomen and spine. There was awareness that the chest wound might have been caused by a projectile entering the body elsewhere and so this was carefully sought. The physical signs looked for, and detected when present, depended on the type of wound, and were exactly the same signs we would look for today. The casualty then had a chest X-ray taken in the casualty clearing station. This was particularly important to locate the position of any, or multiple, foreign bodies and fragments of bone within the chest. The surgeons could also see if a haemothorax and/or a pneumothorax was present and how severe these were, and also looked at the opposite lung and at the heart to determine if there was any suggestion of damage or displacement of these organs. They also observed how the diaphragm was moving as this could also indicate important features of the wound.16
A well defined plan for treatment after the casualty’s arrival at the casualty clearing station was as follows:17 18
• Casualties were put into a special ward, warmth was provided and they were allowed to rest for about an hour.
• If there was a sucking wound which had not been closed previously, this was covered by a dressing (or temporary stitches) and checked to make sure that air was not being sucked in when the casualty took a breath in.
• If casualties were distressed, which was usual, they were given a small amount of a morphine-like drug (omnopon) by injection under the skin.
• Fluids were given to the casualty by administering one pint of hot coffee with 1 ounce of glucose – given by the rectum (back passage).
• A mixture of camphor, olive oil and ether might also be given by an intramuscular injection – to relieve distress.
• The casualty was positioned in bed sitting up in Fowler’s position (see Chapter 7).
The next step in the management was to decide whether or not the casualty required surgery. There emerged a consensus that the wounds shown in Table 8.5 could be managed without chest surgery.
The casualties who had a relatively small amount of blood lying within the pleural cavity, between the inside of the chest wall and the surface of the lung (fitting into the categories shown in Table 8.5) could have this removed without undergoing an operation. The usual treatment was to aspirate this by inserting a needle between the ribs through the chest wall to suck out the blood, after first rubbing a small amount of bismuth, iodoform and paraffin into the wound and surrounding skin to disinfect the area.19 These casualties were then carefully observed for signs of ongoing bleeding or difficulty in breathing, with regular monitoring of their pulse, blood pressure and respiratory rate. If the casualty’s clinical condition deteriorated, it was clear this conservative management was not working and that surgery was necessary.
Table 8.5
Casualties with wounds not requiring surgery
| Casualties with chest wounds who did not require surgery |
• If there was a small wound which looked clean and there was no other evidence of there being serious damage in the chest. This included wounds where the projectile had gone straight through the chest. |
• If the missile was still in the chest but of a very small size and the casualty also did not show evidence of serious damage in the chest. |
• If there was a large foreign body in the cavity and it was thought that it would be too difficult and dangerous for the casualty to |
• If there was a haemothorax (blood in the pleural cavity as explained above) without there being infection in it. |
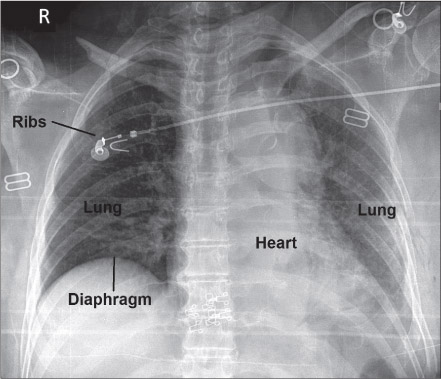
Figure 8.2 Chest X-ray indicating a serious injury to the underlying lungs as a result of chest trauma. The lungs should appear as a uniform black colour (due to air inside the lung) but here there is a “fluffy” white appearance indicating the accumulation of fluid within the lung stopping it from taking in oxygen for the body and possibly resulting in the death of the patient. (Courtesy of Dr Alan Denison)
Figure 8.3 This chest X-ray shows several abnormalities as a result of trauma to the chest. There are fractures ribs on both sides (arrows) and on the right a segment of the ribs has become displaced inwards causing extensive damage. The underlying lung appears a white colour (instead of a uniform black appearance) indicating extensive damage to the lung itself. In addition there is some fluid inside the chest on the right side and on the left side at the uppermost area of the lung (indicated) there is a very black appearance (blacker then normal lung) that indicates that there is some air outside the lung but in the pleural cavity. (Courtesy of Dr Alan Denison)
Although surgery could be avoided in some cases by simply draining the chest, not only did some patients need operating on as outlined above but others, who seemed to settle initially, went on to develop an infection in their chest cavity, because blood was an excellent medium in which bacteria could grow. If the casualty developed a rising pulse rate with a high temperature and the amount of fluid in the chest increased, this was highly suggestive of infection and the fluid from the chest was examined microscopically to detect any bacteria. If it was decided that infection was present, an operation was then necessary to open up the chest and drain the remaining blood and any pus which may have accumulated. This dangerous complication led to the suggestion that all casualties should undergo surgery in order to prevent it happening, but this was not adopted as the standard policy. A strong advocate of immediate surgery was Major George Gask, who believed that it was important to remove any blood from within the chest cavity and thus hopefully prevent infection.
George Gask was one of the most important contributors to the development of chest surgery in casualty clearing stations. He was consulting surgeon to the 4th Army and developed great expertise in the management of casualties with chest trauma. He published his results for treating 500 patients with penetrating gunshot wounds of the chest and these are discussed later.20 After the Great War, he returned to London and became Professor of Surgery at St Bartholomew’s hospital, establishing an academic unit of surgery there.
Whilst the patients described above did not need to undergo surgery initially, the following categories of patients were identified as needing to proceed to immediate surgery in the casualty clearing station:
Table 8.6
Casualties requiring urgent surgery
Taken from Roberts, J.E. & J.G. Craig, “The surgical treatment of severe war wounds of the chest”, British Medical Journal 1917; 2: pp.576-579.
As expertise developed in the management of casualties with chest wounds, there was a growing recognition that a short period of time to begin treatment of “shock” was required (see Chapter 3 where this is explained in detail). Casualties were warmed up and kept quiet. This usually took about an hour but could take up to six hours. There was also recognition that casualties with chest wounds could not be operated on, if as well as having one directly damaged lung, the opposite lung was also collapsed. Operating on such casualties resulted in death.
Surgeons today will spend long periods of time with patients before surgery explaining what the operation will entail and then obtain informed consent before surgery can proceed. Whilst the situation was obviously different almost 100 years ago in the setting of war, the following is an interesting insight into what surgeons might want to tell the casualty before surgery:
… the patient should be warned in a tactful way that he may feel extraordinarily distressed and apprehensive during the operation … but that he should try to lie and breathe quietly, that struggling and excitement will only increase his distress, and that the symptoms will pass off very quickly once the operation is finished.21
The surgeons had priorities of treatment. They had to try to ensure that the lungs were allowed to function as well as possible to provide oxygen to the body. They had to stop bleeding thus preventing hypovolaemic shock and death, and they had to do everything possible to reduce the subsequent risk of infection developing in the pleural cavity and chest. This third factor was the main cause of later death if the casualty survived the initial wound and/or surgery. The reason for the development of infection was the same for any type of wound a casualty might have sustained. It is worth remembering from Chapter 2 that wound excision was the single most important surgical intervention at a casualty clearing station. There was always a high risk of bacteria being carried straight into the wound on the projectile, fragments of bone, or on clothing contaminated with mud and debris. Only by removing all this material completely could the risk of infection be reduced.
While the principles for treatment of chest wounds were the same as any wound, there had to be some specific modifications given the vital nature of the lungs and heart within the chest. Surgeons knew that speed was essential if the patient was to survive because the casualty’s general condition meant that he could not withstand long periods of anaesthesia (Chapter 3). Everything should be planned and an important piece of advice from experienced surgeons was that “the operator must not lose his head when things become alarming”.22 It had been believed that the techniques required for working in the chest were possessed by all experienced surgeons working in the casualty clearing stations and the surgical instruments required were no different from normal instruments for every day purposes.23 Whilst this is true, as in all branches of surgery, specialism in chest surgery and developments in techniques and better instruments enabled surgery to be performed more efficiently and with better results as time progressed.
Interestingly the surgeons may have begun the operation under local anaesthetic after giving the patient a “premed” (similar to today’s “premeds” as it comprised omnopon and scopolamine designed to reduce the lung and airway secretions). The technique used was designed to anaesthetise the chest wall initially by injecting a local anaesthetic called novocaine (similar to today’s ones which are used in hospitals and by dentists) into the wound and surrounding area and also around the intercostal nerves which run along the under surface of each rib. This provided very good anaesthesia for the chest wall and a similar technique may be used today to relieve pain in patients who have fractured ribs.
When the surgeons got inside the chest cavity, they then needed a general anaesthetic which was nitrous oxide and oxygen. It may have been supplemented with chloroform in some patients. An interesting description in one of the reports of these wounds and written by a surgeon states that the patients may also be given “a few whiffs of chloroform and ether”.24 Other surgeons thought the patients should be “well doped” and “be made very drowsy” although still capable of cooperating with the surgeon’s instructions.25 Perhaps surgeons didn’t fully appreciate the importance of appropriate anaesthesia in the management of their casualties! Nitrous oxide is still used today although in combination with other anaesthetic agents, to provide better and safer general anaesthesia. The specifics regarding the use of anaesthetic agents and developments in anaesthesia has been discussed in more detail in Chapter 3.
First, damaged tissues around the entry wound to the chest wall were excised, being sure to remove all damaged and dead tissue, debris and foreign material, down to the level of the underlying ribs. Surgeons knew that unless this was done there was a high risk of infection developing subsequently in the post-operative period. If there was damage to the underlying ribs this was carefully assessed and any ragged pieces of bone were smoothed off, and loose bits of devitalised bone splinters were removed. If the wound extended into the chest the surgeon would explore this manually, putting his hand into the chest feeling for and removing any bits of bone that had been driven inside the chest, evacuating any blood and inspecting the surface of the lung. Pre-operative chest X-rays were not always available, so the surgeon had to be vigilant in feeling for foreign bodies. If there was bleeding from the lung this was stopped using fine sutures. The surgeon then had to decide whether to open the chest more extensively so as to formally inspect all the structures or whether the exposure undertaken to accomplish wound excision was enough. Some surgeons stopped and closed the wound at this stage if they thought there was no damage to the structures within, although others always thought it necessary to go further and have a really good look inside the chest for unsuspected damage. This, of course, prolonged the surgery and was a bigger operation for the casualty to withstand.26 27
The more severe chest wounds, however, did require more extensive surgery, for example, if there was major bleeding or if there was a large foreign body within the chest and it had been decided that it should be removed (as explained previously). Large fragments of metal nearly always carried fragments of contaminated clothing into the chest, which always gave rise to infection if not removed. Depending on where the pre-operative X-ray indicated the fragments of metal to be, it was sometimes possible for the surgeon to gain access inside the chest by working though the hole in the chest that the projectile had caused. Sometimes, however, this did not provide adequate exposure for the surgeon or the projectile was located some distance away within the chest from where it had entered. This meant that the chest had to be cut open in a different place and in a specific way. This operation is termed a “thoracotomy” and is strategically placed to give optimum access to the area of the chest requiring attention.
The way this was done was to make an incision some 6 inches long along the line of the 5th or 6th ribs and running from the side of the chest towards the front wall of the chest. After cutting through the muscles overlying the chest wall the underlying rib was reached. A 4 to 6-inch segment of rib was removed by cutting it off at the front where it is attached to the cartilages which lie between the rib at its front end and the breast bone (these act like a buffer under normal circumstances) and cutting straight through the rib at the back end of the incision. The lining on the inside of the chest (called the pleura) was then cut open and the surgeon had entered the chest. Alternative techniques were developed by some surgeons to avoid removing a section of rib. These included splitting a rib down the centre and then opening it up like the leaves of a book with an upper and lower half of the rib still being attached to the intercostal muscles on either side.28

Figure 8.5 The incision used in a thoracotomy operation to gain access to the structures within the chest. (Courtesy of Mr George Gibson FRCS)
To see what he was doing, an instrument called a “rib spreader” was then inserted between the ribs (or between the two halves of the rib if it was retained) spreading them well apart giving the surgeon a good view of the lungs and the heart.29
Any foreign body identified using this technique could easily be removed. If however, it lay within the lung tissue itself it would require to be located by touch during a careful examination of the lung. It was removed from the lung either through the hole it had caused on the way in, or by making a new cut in the lung to get it out – a relatively easy procedure. The lung was carefully repaired by stitching it and any bleeding was stopped. If any lung tissue was considered to be too damaged to survive then it was removed and the remaining lung stitched back together. The chest cavity was carefully examined to make sure that there was no further bleeding. Then it could be washed out with saline solution or perhaps even an antiseptic solution, for example Eusol, Dakin’s solution or flavine depending on the surgeon’s preference, to try to reduce the risk of infection developing later.
The layers of the chest would be closed separately just as they had been cut open, pleura being stitched to pleura, muscle to muscle and skin to skin. The surgeons considered that the most important layer to stitch together very precisely was the pleura lying on the inner layer of the chest wall and to do this they used catgut, which is a material still used in present surgical practice. Sometimes, depending on the extent of the damage done to the chest wall or where there was an inadequate amount of muscle to repair, then just the skin was stitched closed. Techniques were also developed to deal with cases where there was insufficient skin left after the chest wall (muscle layers) had been closed.
At the end of the procedure the surgeons recognised that they had to keep the pleural cavity free of blood and/or air as the lung would collapse down if this was not the case. To expel any air lying between the surface of the lung and the inner wall of the chest, if necessary they often aroused the casualty, although there must still have been a degree of anaesthesia present, with the casualty drowsy and hopefully not fully aware of what was happening. The casualty was then told to purse his lips, hold his nose, and make a strong expiratory effort so as to expel the air and so the lung would fully expand just as the last stitch was being tightened!30 This is no longer necessary, the reader will be pleased to know, as the anaesthetist has a tube passed into each lung and can inflate the lung fully when the surgeons are closing the layers of the chest wall and whilst the patient is still anaesthetised.
There was great discussion about whether or not drains should be put into the chest at the end of surgery to allow the drainage of any fluid that might accumulate within the chest after such procedures. Indeed, there was controversy as to whether they should be used anywhere because it was recognised that infections could get into the body through the drainage tube.31 The generally accepted policy for chest wounds was that drains were not used unless the chest wall could not be closed or if there was a well-established infection inside the chest. The drain used was a rubber tube of about a half-inch diameter which was positioned just inside the pleura and attached to a glass bottle containing boric acid which was on the floor. The tube was actually in the boric acid so this allowed a negative pressure to be maintained within the pleural cavity (because as air left the chest cavity it could not be replaced) and so encourage the lung to remain expanded. Such a drainage system is called an “underwater seal” and is used today but usually with water and not boric acid. It has already been pointed out in Chapter 2 that delayed closure was not an option with chest wounds. Not to close the wound would almost certainly mean the death of the patient.
After surgery patients were nursed initially semi-recumbent and then partially sitting up. One of the most important things was to keep their lungs clear of secretions by coughing up sputum. If they could not do this it would accumulate in the lungs and predispose to pneumonia and death. After an operation either on the chest or abdomen, trying to breathe deeply or to cough could be extremely painful unless adequate pain relief was administered. Morphine was used for this and it is still used as the basis of pain relief after surgery today. The substances used to aid coughing and help the patients to get rid of their lung and bronchial secretions included tincture of camphor, syrup of Tolu, ammonium carbonate, creosote and potassium iodide – none of these, however, would be used now.
It was recognised that there might be an accumulation of fluid (or air) in the pleural cavity as detected on clinical examination and/or with a chest X-ray. If this occurred then it was drained by inserting a needle into the chest (called an aspiration) using local anaesthetic for the skin and muscles and using a tube which was large enough to allow the fluid out without blocking. If the fluid re-accumulated, then repeated aspirations were performed. However, if there was blood in the fluid and this had clotted then it was not possible to aspirate and an operation had to be done to open the chest and scoop all the blood clot out manually. This had to be done because it was recognised that clotted blood was an excellent medium for harbouring and growing bacteria leading to serious infections.
Infection developing in the chest after surgery was the most serious complication. Although surgeons believed in “the natural power of the pleura to deal with infection”32, unfortunately this power frequently failed the patient and infection occurred. If the fluid within the chest did become infected (and there was no clotted blood) then a tube was placed into the chest by removing some of the stitches. If it was not possible to drain the infected fluid through the tube then an operation was required to open up the chest and remove all clotted blood and infected material. This is similar to what would be done now although the needle would be positioned very accurately through the chest wall into the fluid lying in the chest using an ultrasound (sound wave) scanner to guide the needle into the correct position and we would also use antibiotics for the infection. Antibiotics were not available during the Great War, and consequently patients with chest wounds complicated by sepsis often died.
The mortality for chest wounds admitted to the casualty clearing station fell to approximately 20%. The surviving casualties would remain at the casualty clearing station for varying periods of time before being transferred back to base hospitals. For example, if the wound was a small haemothorax but they were well, then they would be kept for 72 hours whereas those undergoing major surgery would stay for at least 10 days or until any post-operative complications that occurred had been treated. The reasons for this are that it was just not safe to transfer the casualties unless their clinical situation was stable. The complications of these wounds may result in collapse of the lung with accumulations of air or fluid (pus and/or blood) and these can very quickly become life-threatening without immediate treatment,
The outcomes following surgery depended on the severity of the wound inflicted. Roberts and Craig analysed 199 casualties who were admitted to their casualty clearing station to try to learn more and to improve management. They categorised the deaths according to the severity of the injury as shown in Table 8.7.
Table 8.7
Outcomes of surgery for penetrating chest wounds
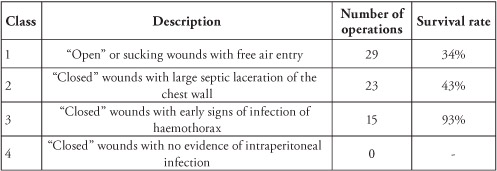
Data from Don, A., “Perforating and penetrating wounds of the chest with severe haemorrhage: a suggestion for treatment”, British Medical Journal 1916; 1: pp.816-817.
They carefully analysed their data and their results, and published it in the medical literature to share and learn from their experiences. Of the 199 casualties who were admitted during the time of their analysis, 108 were evacuated to base hospitals without undergoing an operation, 24 died without having surgery and 67 casualties underwent chest surgery at the casualty clearing station. They described these 67 soldiers as “forlorn hopes” but 34 recovered to be evacuated to base hospitals with the other 33 dying. However, about half of those who died had major “gross” injuries elsewhere, most commonly in the abdomen, and they considered that no deaths were attributable to the chest injury itself.
Another series of 365 casualties with chest wounds who were admitted to the same casualty clearing station between June 7 1916 and August 31 1917 was detailed by Gask and Wilkinson.33 Not only is this a very large experience to learn from but the data they collected gives a fascinating insight into their management of these wounds. Of these casualties 76 died but 45 of these had significant associated wounds of the head, abdomen, spine, heart blood vessels or combinations of these. However, when they specifically focussed on those soldiers with chest wounds only there were 31 deaths out of 320 cases, which gave a mortality rate of only 9.6%. The causes of death were shock and blood loss or infection as had been found previously. The details of the operations undertaken in the 104 casualties who proceeded to surgery are shown in Table 8.8.
Table 8.8
Operative details and mortality for casualties undergoing chest surgery
| Type of operation | Number of operations | Survival rate |
| Excision of wounds of chest wall | 36 | 94% |
| Thoracotomy for repairing the chest wall/ lung with draining haemothorax | 24 | 63% |
| Thoracotomy with removal of foreign body, repair of lung and draining haemothorax | 16 | 81% |
| Thoracotomy for infected haemothorax | 15 | 67% |
| Combined abdominothoracic operations | 12 | 83% |
Date from Roberts, J.E. & J.G. Craig, “The surgical treatment of severe war wounds of the chest”, British Medical Journal 1917; 2: pp.576-579.
But perhaps what also gave great insight into the risk of death with chest wounds and how they should be managed were the figures which they provided where wounds were broken down according to their cause. It was clear that the rifle bullet passing through the chest was associated with the very best chance of survival. It must be remembered however, that all these figures refer to a selected group of casualties because these are the ones who made the journey back to the casualty clearing station satisfactorily. Those with more severe injuries died either on the battlefield or during the evacuation pathway.
Table 8.9
Mortality from chest wounds according to cause of the wound
| Cause | Mortality |
| Bullet with entrance wound only (bullet remains in chest) | 17% |
| Bullet with entrance and exit wound (passed through the chest) | 10% |
| Shell fragment with entrance wound only | 21% |
| Shell fragment with entrance and exit wounds | 47% |
| Shrapnel ball | 9% |
Date from Roberts, J.E. & J.G. Craig, “The surgical treatment of severe war wounds of the chest”, British Medical Journal 1917; 2: pp.576-579.
Wounds of the heart were almost universally fatal with casualties dying very quickly on the battlefield due to bleeding – even today they are unlikely to survive. However, there were reports in the medical literature of a small number of casualties from the Great War who survived after undergoing surgery for wounds to the heart! One was alive and well nine months later, the other survived the surgery but died a few days later. These are discussed below in view of their rarity and the surgical skill needed to do this:
A soldier had sustained a wound with a fragment from a bomb penetrating his chest close to the nipple on the side of his breast bone. The casualty was clearly seriously wounded from his general appearance and his pulse and when a small probe was put into the wound it pulsated with a “cardiac rhythm”.34 The surgeon, Captain Fraser, removed a portion of the casualty’s rib and after identifying the lining around the heart called the pericardium (this forms a sac within which the heart is contained), he cut it open and blood came out. He saw that there was a small hole in the muscle of the heart wall of the right atrium and he succeeded in stitching this closed. What was actually happening was that blood was escaping through this hole in the wall of the heart but blood was being contained within the sac surrounding the heart thus putting pressure on the heart and not allowing it to pump blood properly. This casualty recovered well.
The second case was more complex. The casualty had been wounded eight days previously, with a small wound to the right side of the lower part of his breast bone. However, chest X-rays suggested that a bullet was actually in the muscle wall of the heart, as it moved as the heart was beating. The surgeon here was Colonel Henry Gray (later Sir Henry Gray) who had made a hugely significant contribution to the treatment of casualties with wounds of bones, joints, soft tissues and head as discussed in other chapters, contributions which, most importantly, were acknowledged by his surgical colleagues who were operating in the casualty clearing stations.35
Colonel Gray decided to operate under local anaesthetic and made an incision on the front of the chest wall over the breast bone trying to follow the track he thought the bullet would have followed. He operated skilfully, identified the heart and with his finger felt the bullet which was thought to be either in the wall of the right ventricle of the heart or possibly lying in the cavity of the pumping chamber of the heart. With the patient feeling no pain and not in any distress he took hold of the heart and cut into the heart muscle to remove the bullet and then stitched the heart muscle back together whilst holding it between his finger and thumb!36
The casualty was well for four hours after the surgery but then his respiratory rate was observed to be 48 breaths per minute (normally 12-16) and he died almost five days later. At post-mortem examination the heart was well healed, there was no blood in the pericardial sac. However, there were some clots of blood in the cavity of the right heart (probably because of the damage to the heart) and these had become dislodged and travelled to the lungs blocking the lungs’ circulation and causing death. This is called a pulmonary embolism and also occurs when clots of blood from within the veins of the leg (for example, after long aeroplane journeys) become dislodged, travelling to the right ventricle and then to the lungs, as happened in this casualty’s case.
An even more serious wound than either that of the chest or abdomen was the penetrating wound involving both the chest and the abdomen. This occurred in approximately 12% of all abdominal wounds37 and about 9% of all chest wounds38. These wounds were often fatal but when casualties did survive they presented a complex management problem for the surgeons of the Great War, and indeed, this wound is still a very complex one for the surgeons of today, almost 100 years later. Whilst the concern was the damage to the organs in both the abdominal and chest cavities these wounds also involved the diaphragm, which was nearly always damaged on one side, as bilateral injury to the diaphragm was usually fatal.
The diaphragm is not only important in breathing, as explained earlier, but it also acts as a partition between the chest and abdomen. The abdominal organs (most commonly the stomach, small intestine and large intestine) can pass into the chest through any holes in the diaphragm, usually on its left side because on the right side the liver sits under the diaphragm and is immobile and attached in its position. This extrusion of the abdominal viscera into the chest is called a diaphragmatic hernia and can cause major problems for the patient, interfering with breathing or the intra-abdominal organs can become damaged at a later stage. It was crucial, therefore, for the surgeons to try to work out where the projectile had entered the body, where it had gone after entering, and where it had come out, to be able to operate with a chance of success.
Careful planning for surgery was essential and X-rays of the chest and abdomen taken pre-operatively were extremely important to help determine where the damage was most likely to have occurred, and also provide information regarding location of any foreign bodies. Judgement was required in deciding which of the wounds required addressing the most urgently. Wallace and Fraser39 made the following clear and simple recommendations (re-iterated some 20 years later and recommended to surgeons preparing for the Second World War):40 41
• Disregard the thoracic wound if it is small and concentrate on the abdominal wound.
• If there is an “open” sucking wound of the chest then this should be the first priority before attending to the abdomen.
• If the abdominal wound is extensive and there is little damage to the chest the abdomen should be explored through an abdominal incision first.
• In those wounds of the chest which are close to the lower margin of the rib cage then access to the abdomen can be obtained by cutting through the lower part of the rib cage.
• If the foreign body lies higher up and closer to the diaphragm and it is thought that the rest of the abdomen is alright, then the surgeon can gain access to the upper abdomen when working in the chest by working through the hole in the diaphragm.
Generally, if at all possible the diaphragm was repaired by stitching it together, because it improved the casualty’s breathing post-operatively and helped to prevent an immediate, or subsequent, diaphragmatic hernia from developing.
This type of surgery was a major undertaking in the Great War. Even today, with intensive care units providing specialised ways of supporting the functions of the heart, lung and kidneys, these wounds have a substantial risk of death. However, during the Great War, the mortality of thoraco-abdominal wounds fell quite dramatically; this is shown in Table 8.10. Whilst these casualties could be regarded as a very select group, given that they were fit young men who had already survived the journey to the casualty clearing station, nevertheless there had been important developments in surgical techniques, anaesthesia, and pre- and post-operative care which had contributed to the improved survival of these patients. Perhaps the most important development in reducing the mortality was the introduction of blood transfusion in 1917.
Table 8.10
Survival for casualties undergoing combined surgery on the chest and abdomen during the Great War
| Year | Recovery rate |
| 1916 (Battle of the Somme) | 18% |
| 1917 | 49% |
| 1918 | 67% |
Data from Wallace, C., “War surgery of the abdomen” The Lancet 1917; 1: pp.561-568.
In parallel with the changes that were taking place in the management of casualties with all types of wounds during the Great War, there were major developments in the treatment of chest wounds. At the start of the Great War, treatment was based largely on experiences in the Boer War, where a rifle bullet was the main wounding agent. If this had passed straight through the chest and the soldier had not died, there was a reasonably good chance of surviving without further surgery. However, this did not happen in France and Flanders. It was recognised that this was inappropriate treatment given the nature of the wounds and the environment in which the fighting was taking place. Surgical experience resulted in the development of clearly defined categories of casualties depending on whether they did or did not require surgery, and a rational management plan for those with chest wounds was developed. As with abdominal wounds, the increasing success rates were also due very much to the developments in anaesthesia and blood transfusion, which played a critical role in supporting the types of major chest surgery being undertaken in casualty clearing stations.
1 Fraser, P., A Treatise Upon Penetrating Wounds of the Chest. London: John Churchill, 1859.
2 Stevenson, W.F., “Notes on surgical experiences of the Boer War”, Journal of the Royal Army Medical Corps 1903; 1: pp.93-8.
3 Gask, G.E., “Gunshot wounds of the chest”, British Medical Journal 1939; 1(4089): pp. 1043-1045.
4 Don, A., “Perforating and penetrating wounds of the chest with severe haemorrhage: a suggestion for treatment”, British Medical Journal 1916; 1: pp.816-817.
5 Roberts, J.E. & J.G. Craig, “The surgical treatment of severe war wounds of the chest”, British Medical Journal 1917; 2: pp.576-579.
6 Ibid.
7 Gask, G.E. & K.D. Wilkinson, “Remarks on penetrating gunshot wounds of the chest, and their treatment”, British Medical Journal 1917; 2: pp.781-784.
8 Hathaway, F.J., “The early operative treatment of penetrating gunshot wounds of the chest”, British Medical Journal 1917; 2: pp.582-583.
9 Herringham, W., “Penetrating wounds of the chest at the casualty clearing stations”, British Medical Journal 1917; 1: pp.721-722.
10 Gask, op.cit., pp.1043-1045.
11 Gask & Wilkinson, op.cit., pp.781-784.
12 Wallace, C.S. & J. Fraser, Surgery at a casualty clearing station. London: A & C Black, 1918.
13 Ibid.
14 Ibid.
15 Roberts & Craig, op.cit., pp.576-579.
16 Gask & Wilkinson, op.cit., pp.781-784.
17 Roberts & Craig, op.cit, pp.576-579.
18 Anderson, J., “The surgical treatment of severe penetrating wounds of the chest in a casualty clearing station”, British Medical Journal 1917; 2: pp.575-576.
19 Roberts & Craig, op.cit, pp.576-579.
20 Gask & Wilkinson, op.cit., pp.781-784.
21 Roberts & Craig, op.cit, pp.576-579.
22 Ibid.
23 Anderson, op.cit., pp.575-576.
24 Hathaway, op.cit., pp.582-583.
25 Roberts & Craig, op.cit, pp.576-579.
26 Gask, op.cit., pp.1043-45.
27 Hathaway, op.cit., pp.582-583.
28 Cowell, E.M., “Plastic transcostal thoracotomy”, British Medical Journal 1917 Nov 3; 2 (2966): pp.581-582.
29 Hathaway, op.cit., pp.582-583.
30 Roberts & Craig, op.cit, pp.576-579.
31 Hathaway, F., “The abuse of drainage tubes”, British Medical Journal 1918; pp.1718-1720.
32 Hathaway, F.J., “The early operative treatment of penetrating gunshot wounds of the chest”, British Medical Journal 1917; 2: pp.582-583.
33 Gask & Wilkinson, op.cit., pp.781-784.
34 Bowlby, A. & C. Wallace, “The development of British surgery at the front”, British Medical Journal 1917; 1: pp.705-721.
35 Hathaway, F., “The abuse of drainage tubes”, British Medical Journal 1918; pp.1718-1720.
36 Birkbeck, L.H., G.N. Lorimer & H.M. Gray, “Removal of a bullet from the right ventricle of the heart under local anaesthesia”, British Medical Journal 1915; 2: pp.561-562.
37 Wallace, C., “War surgery of the abdomen”, The Lancet 1917; 1: pp.561-568.
38 Gordon-Taylor, G., The abdominal injuries of warfare. Bristol: John Wright and Sons, 1939.
39 Wallace & Fraser, op.cit.
40 Gordon-Taylor, G., “Abdomino-thoracic Injuries I”, British Medical Journal 1941; 1: pp.862-864.
41 Gordon-Taylor, G., “Abdomino-thoracic Injuries II”, British Medical Journal 1941; 1: pp.898-901.