Almost all our suffering is the product of our thoughts. We spend nearly every moment of our lives lost in thought, and hostage to the character of those thoughts. You can break this spell, but it takes training just like it takes training to defend yourself against a physical assault.
—Sam Harris
Your head is where your brain and mind reside, although most of us give our minds more attention. The health of each affects the other, so we don’t want to neglect either. In fact, the perception of your external environment affects the biology of your internal environment, and vice versa. Your thoughts can direct gene expression. So we want to integrate the mind and body, starting with the brain.
This goal is born of necessity because the brain is getting older. I like to think it’s getting better, because I know that the math of a healthy brain involves a better balance between inputs (like drinking green smoothies and meditating) and outputs (such as prioritizing sleep, preventing leaky gut, and even keeping mitochondria in top shape). Part of the challenge for me is that I have a high level of negative self-talk, cognitive dissonance, and distortion, plus a familial tendency toward addictive behavior. If something is worth doing, isn’t doing more of it better? Uh, no, not usually. I’m a recovering workaholic, exercise-aholic, self-fixer-aholic, to-do-list-aholic, and food addict. Or as a friend put it, I’m a type A minus.
Maybe you have one or more of these problems too. You almost certainly experience negative and inconsistent thought patterns, attitudes, and beliefs that influence your choices and behaviors, sometimes irrationally and without your conscious awareness. You may be like me in the way that I overvalue the wrong factors when making decisions, default to an all-or-nothing mentality, or dwell on the negative rather than the positive. While it’s totally human to be slow to acknowledge errors, I know that these tendencies have led to conflict in my marriage, self-righteousness in my parenting and friendships, and sometimes to eating and drinking outside of my personal integrity.
There is an alternative. Each of us can think and act with more awareness, generally doing a better job at this opportunity called life. It requires mental rehabitulation and a recalibration toward what is good for the mind, brain, and nervous system. Without all of those operating at their best function, your choices for a longer healthspan suffer along with your inner clock—that is, you get old before your time. It’s not as hard as you might think, as long as you break it down into baby steps. What you’ve accomplished in the previous six weeks of the protocol is already benefiting your head; now we want to take the improvements to the final level. At this point, you won’t be surprised to see me rattle off the top genes that give a person stinkin’ thinkin’ or hurt your brain function. I am genetically loaded with some, but thankfully not all, of these variations.
• Corporate warrior gene, or COMT, which affects whether you’re a warrior or a worrier (shockingly, I’m a warrior).
• Alzheimer’s and Bad Heart gene, APOE, which raises or lowers your risk of Alzheimer’s disease (I don’t carry the APOE4 risk allele, but many of my patients do); the changes start in the brain decades before symptoms appear.
• Unhelpfully named adrenergic beta-2 surface receptor gene, ADRB2, which gives me a terrible relationship with weight and food over the long haul. When you have this variation, weight loss takes you twice as long as it takes a normal person. It’s like a party crasher for women who want to burn fat. Exercise helps very little; it’s all about wrangling my mind to eat the right types and amounts of food with steady discipline. Gah!
• Klotho, a gene that codes for an antiaging hormone that raises IQ.
• Dopamine receptor D2 (DRD2), which makes me more likely to overeat and behave addictively.
• BDNF, the gene that makes your brain smarter and more neuroplastic (adaptable) over time as you get older.
• FAAH, also known as the Bliss gene, the same one we covered in the last chapter, which codes for the enzyme that acts on anandamide, our natural cannabinoid molecule of bliss.
An extreme example of faulty thinking is Alzheimer’s, a brain disease that affects your mind. Symptomatic of the disease, victims have a total lack of awareness that they’re losing their minds. Two-thirds of Alzheimer’s patients don’t understand that they have it, and my grandmother Helen was a good example. Granny stood out as a beacon of unconditional love when I was young—glamorous, funny, always humming and dancing to big-band songs while she puttered around her home, cooking, cleaning, and showering me with care. I’d clomp around her house wearing her spectator pumps and costume jewelry. While I was growing up in Maryland, she picked me up after school (and camp during the summers) because my mother worked full-time. Granny taught me how to garden, fish, and catch blue crabs. That is, until she developed the early stages of Alzheimer’s in her sixties.
First, Granny would get lost while driving. We’d go grocery shopping and end up on the highway to Baltimore instead of heading toward her home on the Chesapeake Bay. Then she became less articulate and was no longer able to trust her instincts; she developed a vacant stare, like no one was home. Later, her warm and loving personality changed; she would glare at me with fury and probably frustration as her mind slipped away. The smallest decision would render her childlike, paralyzed by pathos, a ghost of her former self. Yet she didn’t die. Instead, she languished in a nursing home for twenty more years, unable to recognize anyone in our family, bedbound and requiring round-the-clock care until her death at age eighty-four. She had a long life span but a painfully short healthspan.
I’ve learned that developing Alzheimer’s may be avoidable. Even if you’re genetically wired to develop it based on your family history or genes, you can prevent or reverse this heartbreaking scourge. I don’t have the gene for Alzheimer’s, but given my experience with my grandmother, I’m extremely motivated to do everything within my power epigenetically to prevent the disease from taking hold.
Why It Matters
Normally, the mind and brain age gradually, if at all, in the absence of injury and disease. When you take care of your brain, vocabulary and language skills can actually increase with age. Older folks may be better at perspective and problem solving; they take their time to carefully craft smart and well-reasoned solutions to problems. They are better at recognizing patterns and being attuned to the effects of their decisions.
We all know elders who are wiser and more accepting of the mixture of joy and sadness in their lives. They are less likely to feel angry, stressed, or worried than younger people. Psychological wellness—roughly, your overall appraisal of your life and mood—reaches a low point at age forty-six.1 After that, with the brain and mind in a better place, the body benefits from improved stress resilience and wiser choices. Gratitude, forgiveness, appreciation, and a sense of calm peak at age seventy and stay high. Other functions—organization, planning, and analysis—are the same in elderly brains as they are in youthful ones. However, it isn’t all rainbows and unicorns. Processing speed tends to slow, and memory becomes weaker in the aging brain. As collagen recedes, joints give out, and more gray hairs keep appearing, these tough situations may breed negative thoughts and depression if you let them get to your head.
My hope is that this won’t happen to you because you’re already on a better track with our protocol! You can prevent deteriorating memory and dementia (and hearing loss!) through regular physical exercise, learning and education, repairing your gut, and even playing video games. You want your hippocampus—the section of your brain that serves as the center of emotion, memory, and the autonomic nervous system—to be lush and connected, like a dense fern growing in a tropical rain forest.
A Simple Way to Create New Neural Pathways
Here is a simple technique based on an exercise from the late Irish poet and philosopher John O’Donohue2 that I’ve adapted with a few more ideas from meditation teacher Tara Brach.3
1. Document. Take a day this week to recognize and document your self-talk. Sometimes I call my thoughts the “members of the committee” who sit in judgment inside my head. Just record the most common thoughts without judgment.
– I’m fat.
– I’m so tired. It’s not normal to feel this tired.
– I’m getting old. My neck hurts.
– I’m a bad mom.
– I deserve chocolate.
– I suck at getting together with my friends.
– I need to call my mom; why am I so bad at calling her regularly?
– Look at that woman in the front row of barre class! She’s got twenty years on me and she’s stronger! I’ll never be like her!
No editing. Simply write down the top five to seven thoughts.
2. Ask. For each thought, inquire: Is it true? Is it helpful? Is it serving me? What’s the tone? How old is the narrator? The idea is to be a dispassionate observer of your thoughts, so that you’re not fused with a limited set of emotions. For instance, maybe I do suck at getting together with my friends, and I need to address it. Note: swearwords are a sure sign that the narrator is a rebellious teenager!
3. Identify the bad, but with kindness. Does it make me feel bad? Explore the downstream emotional consequences of the self-talk. For me, thinking that I’m fat becomes a self-fulfilling prophecy. It’s not helpful or loving, and it keeps me constricted and stuck.
4. Recognize the good. What’s good about the thought? When it comes to Sylvia in the front row of barre class (see chapter 4 for a complete description), comparing myself to her causes me despair, but drawing inspiration and learning from her is great. She is a wonderful model of optimal aging.
5. Reframe. Is there a new way to frame the self-talk so it’s more loving and supportive? As John O’Donohue described in an interview with Krista Tippett,4 you’ve been married to these thoughts for a long time, and you’ve never even flirted with other thoughts. Now’s the time to flirt with a cognitive reframe that suits you—your mind, brain, emotions, spirit—better. Such as Look at Sylvia. She is strong and beautiful. I want to age like her. I think I’ll take a nap today like she does, skip the restaurant for dinner, and make sure I get to bed by ten.
Science of Week 7: Think
If you want to skip the science, go straight to the protocol to start changing your brain for the better.
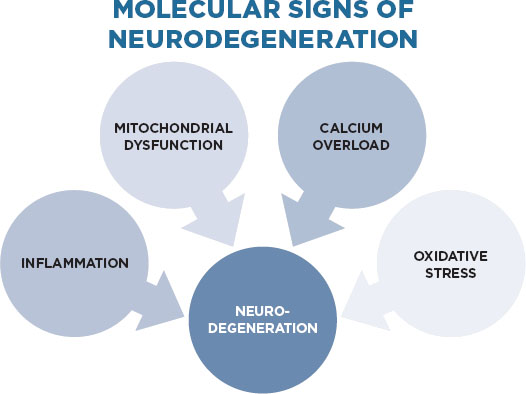
When it comes to the ways that your brain ages and slows down, there are four main pathways in your brain cells: inflammation, mitochondrial dysfunction, intracellular calcium overload, and oxidative stress.5
These molecular events, which often overlap, become toxic to nerve cells in the brain. What’s a girl to do? Your job is to prevent all of these molecular problems or, if just one or two are happening, address those to keep the brain happy, adaptable, and slow to age. I’ll show you how in this week’s protocol.
1. Inflammation. Of course, inflammation is a natural part of your body’s defense system, but problems arise when it doesn’t turn off—for example, when the immune system is chronically on high alert. In the introduction, I referred to this process as inflammaging because unnecessary inflammation accelerates your aging, like a woodstove that keeps burning until the house is torched. Persistent immune activation leads to the flood of noxious chemicals in the body that can trigger neurodegeneration, as seen in Alzheimer’s and Parkinson’s disease.6 When biomarkers of inflammation are elevated, cognitive decline is more likely.7
2. Calcium overload. Normally, calcium levels rapidly rise and fall in a cell as a means of triggering biochemical signals, such as the release of neurotransmitters. You need normal calcium signaling to stay neuroplastic, or adaptive. Calcium and its movements become disturbed in several neurodegenerative disorders, such as Alzheimer’s, Parkinson’s disease, Huntington’s disease, and in the motoneuron disorder amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig’s disease). When calcium levels get disturbed, they can change gene expression, harm the mitochondria (there’s a recurrent theme here and lots of overlapping), reduce neural plasticity, and cause problems with neuron survival.8 Sadly, even small changes in calcium levels can wield big changes in cognitive function.9
3. Oxidative stress. As we covered in chapter 9, oxidative stress is the imbalance between harmful chemicals (free radicals like reactive oxygen species and H2O2) and neutralizing antioxidants (such as glutathione). Oxidative stress is a major player in brain fog and accelerated aging. When you have too many free radicals interacting with your genes, immune system, and endocrine system, this stress generates that foggy feeling. Your hypothalamus, the part of your brain that makes many essential hormones, is most influenced by oxidative stress. This stress accumulates like rust and causes mitochondrial dysfunction, which then leads to more oxidative stress and increased inflammation . . . you can see the vicious cycle.10
4. Mitochondrial dysfunction. When you’re healthy, your mitochondria power your thoughts and actions. Millions of these tiny organelles in your cells work together as a power grid for your body, a bioenergetics hub of energy. Your mitochondria lose their might from various causes that usually overlap: nutritional deficiencies like neutralizing antioxidants, nutritional excesses such as carbohydrates and/or fructose, bad microbes and dysbiosis, xenobiotics (particularly pesticides, herbicides, and substances such as hydrogen sulfide), abnormal mitochondrial DNA, and excess oxidative stress. When your mitochondria don’t work, you age fast throughout your entire body.11 You feel tired and worn out, often because your mitochondria are tired and worn out.12
Our Biggest Fear: Alzheimer’s Disease
Most people consider old age as a progressive decline toward drooling and living in a nursing home, which is one of our greatest fears. By 2050, the number of people age sixty-five and older with the big “A” is expected to have tripled, according to conservative estimates.13 Sadly, after age sixty-five, an individual’s risk of developing Alzheimer’s doubles every five years. After you hit age eighty-five, the risk reaches nearly 50 percent.14
Alzheimer’s is characterized by a decline in memory, language, problem solving, and cognitive ability. It stems from a loss of certain nerve cells and an accumulation of beta-amyloid plaques and neurofibrillary tangles. The plaques result from abnormal protein folding and aggregation, like the misfolded bedsheets I described in chapter 9. Two-thirds of people with Alzheimer’s are women. The best known gene for it is APOE4, which has the strongest impact on your risk. You inherit a copy of the APOE gene—e2, e3, or e4—from each parent.
When you consider most diseases of aging, the issue is usually a problem of imbalance. Take osteoporosis, for example. With this disease, your bones are on the wrong side of the balance; you have too much osteoclast activity (which thins the bone) and not enough osteoblast activity (which builds the bone). A similar problem is occurring in the brains of people with Alzheimer’s, according to neurologist and UCLA professor Dale Bredesen of the Buck Institute for Research on Aging. In the normal brain, certain signals create more nerve connections and make memories, while other signals foster a way to forget irrelevant information, like when you need to do some spring cleaning in your closet to make room for new clothes. In people with Alzheimer’s disease, the balance between opposing signals is off, leading to a net effect of truncated nerve connections (synapses) and lost memories of important information. If you are freaking out and wondering if there’s a solution, yes, almost there!
Greek Myth, Klotho, and Oxidative Stress
Your genes can shift how fast your brain is aging. For instance, the Klotho gene codes for the Klotho protein, which protects cells and tissues from oxidative stress and therefore acts as an age-suppressor gene.15 Klotho takes its name rather poetically from Greek mythology; Klotho is Zeus’s daughter who spins the thread of life.16 Making more Klotho—with exercise and enough vitamin D—regardless of the gene you inherited will help you keep spinning your thread of life and prevent it from being cut too early.
You Can Reverse Cognitive Decline
The latest version of the Alzheimer’s Facts and Figures gets one fact completely wrong: “It’s the only cause of death in the top 10 in America that cannot be prevented, cured, or slowed.”17 Since first described a century ago, Alzheimer’s disease has been without effective treatment. Until now. Dr. Bredesen has pioneered a program that reverses memory loss in nearly all of his patients within three to six months. Yes, reverses. Larger clinical trials need to be done, but this is a rare bright spot in the treatment of Alzheimer’s that you need to know about now, before it’s too late.
Yet the cure is probably not a single drug with one target. Instead, the best solution appears to be a functional medicine approach that addresses multiple root causes. Imagine having a roof with thirty-six holes in it, and a drug that patches only one hole. Dr. Bredesen says that if you seal one hole, you still have a leaky roof with thirty-five other holes. So taking a drug for treatment isn’t helpful. But if you address multiple holes, you may get an additive or even synergistic effect, even if each hole is only modestly affected. You might reduce the leakiness by 90 percent. You haven’t fixed everything, but you’re much better off.
The Best APP for Your Brain . . . Amyloid Precursor Protein
There’s a protein you should know about when it comes to saving your mind: amyloid precursor protein (APP). According to Dr. Bredesen, APP is like the CFO of your company (that is, your body). “APP looks at all the inputs from all the different accountants: are you in the red or the black? Every day, you’re actively remembering what you did this morning or you’re actively forgetting the seventh song that played on the radio on the way to work yesterday. You have this beautiful balance,” he says. One hundred percent of the people with Alzheimer’s disease are on the wrong side of that balance for years. He nicknamed the problem synaptoporosis.
So Dr. Bredesen set out to understand what’s driving the process—what leads to Alzheimer’s patients being on the wrong side of the balance, and how we can use that information to prevent Alzheimer’s from taking hold, before it’s too late. Dr. Bredesen published the results of his initial small study of a comprehensive functional medicine program to reverse memory loss.22
Alzheimer’s Disease and APOE Gene by the Numbers
• APOE4 is responsible for approximately 20 percent of Alzheimer’s cases.18
• Inheriting one copy (from one parent) of the APOE4 gene triples your risk of developing Alzheimer’s, while inheriting two copies (one from each parent) of the APOE4 gene makes your risk eight to fifteen times higher.19 Approximately 2 percent of the U.S. population inherit two copies of e4.20
• Women who carry the APOE4 gene are more likely to get Alzheimer’s than men.
• Not having the APOE4 gene does not guarantee that you will not get the disease.
• APOE4 causes a profound reduction in SIRT1 and an overproduction of mTOR, two of the longevity genes.21
• If you inherit two copies of the APOE2 gene, you have a lower risk of Alzheimer’s.
• You can test for this important gene in one of the labs listed in the appendix.
One of his first patients was a sixty-seven-year-old woman with two years of progressive memory loss. He referred to her as Patient Zero. She was considering quitting her demanding job, which involved analyzing data and writing reports. By the time she reached the bottom of a page she was reading, she would need to start again at the top, owing to her poor short-term memory. She began to get disoriented driving, and she mixed up the names of her pets.
Patient Zero’s mother had developed similar progressive cognitive decline beginning in her early sixties, had become severely demented, and had died at eighty. When the patient consulted her physician, he told her that she had the same problem as her mother, and he could do nothing about it. He wrote memory problems in her chart, and she was therefore turned down when she applied for long-term care. Knowing that there was still no effective treatment and that she couldn’t get long-term care, she decided to commit suicide. She called a friend to commiserate, who suggested Dr. Bredesen for a second opinion.
She started Bredesen’s program and could adhere to some but not all of the components; she couldn’t convince her local doctor to prescribe bioidentical hormones; she stayed off gluten but kept eating other grains like brown rice, and she had a hard time getting more than seven hours of sleep. Still, after only three months, all of her symptoms abated—she was able to navigate familiar roads again without problems, recall phone numbers, and read and retain information. When she got sick with a cold, she stopped the comprehensive program and relapsed, but when she reinstated the program, she felt normal.
Types of Alzheimer’s Disease
Dr. Bredesen has found three distinct types of Alzheimer’s disease.23 The first is the “hot” or inflammatory type, most commonly found in people with one or two copies of the APOE4 allele. The second is “cold” or non-inflammatory. Women more commonly fall into the type 2 category. Bredesen has found that those with type 1 or type 2 are able to hang on to their jobs for a while because the main problem is memory and they find work-arounds. For instance, they are dentists who can still drill teeth and physicians who can still listen to hearts as long as they have good assistants to guide them. Type 3 or “toxic” results from exposure to specific toxins—most commonly mold—as a manifestation of chronic inflammatory response (CIRS). It affects younger people and the cortex more broadly. They lose the cerebral cortex, which is the folded gray matter in the brain that’s important for consciousness. That means they lose old memories, fall apart in terms of daily functioning and stress coping, and must leave their jobs early.
Behaviors That May Harm Brain and Mind (and Increase Your Risk of Alzheimer’s)
Although 60 to 80 percent of your risk of Alzheimer’s is related to genetic factors, only about half of this risk is through APOE.24 (Other genes such as APP, can cause Alzheimer’s, but they are very rare.25) Furthermore, you can modify your risk with fewer toxic exposures and other lifestyle adjustments, many of which we’ve already introduced in the protocol to date.26 As we covered in the introduction, the five factors contributing to inflammaging also increase your risk of declining cognition and Alzheimer’s.27 Correcting hormone imbalance takes care of the brain, so it can take care of your mind and, by extension, you.
Other culprits include:
Poor sleep
• How it affects your brain: you didn’t get the full shampoo by your glymphatic system (see chapter 6), so you feel leaden and toxic. Blood sugar may be higher than normal, leading to brain fog. You may even feel depressed or anxious. In a national poll from 2005, people diagnosed with depression or anxiety were more likely to sleep fewer than six hours per night.28
• How it affects your mind: you’re groggy, cranky, and have a shorter fuse. Cortisol is higher than normal, allowing stress to take advantage of you.
Lack of stimulation
• How it affects your brain: What you don’t exercise atrophies. It’s true for muscles, and it’s true for your brain.29 The stimulation of adult education reduces the risk of dementia by 75 percent.30 When you stop engaging in cognitively stimulating activities like crossword puzzles, games, baking, gardening, or staying up on current events, your brain can go south. Picking them up again can help reverse mild to moderate symptoms of Alzheimer’s.31 My father-in-law is a great example of ongoing learning: at age eighty-four, he passed multiple Coast Guard exams to become his local flotilla’s commander. Go, Ira!
• How it affects your mind: While the same study by the Cochrane Collaboration did not find a benefit to mood, it’s clear that lifelong mental engagement keeps your mind sharp. Try humor; it improves memory!32
Lack of community
• How it affects your brain: Interacting with people stimulates the brain and keeps you sharp. Stronger social ties are proven to lower blood pressure and boost longevity. Having no social ties is an independent risk factor for cognitive decline. Talking to another person just ten minutes per day improves memory and test scores.33 The higher the level of social interaction, the greater the cognitive functioning. Researchers found that people with at least five social ties—such as church or social groups, regular visits or phone calls with family and friends—were less likely to experience cognitive decline than those with no social ties.34
• How it affects your mind: Dealing with other people can be challenging, but it’s an important way to create meaning and reduce isolation. In fact, my friend and colleague Mark Hyman, M.D., says, “The power of community to create health is far greater than any physician, clinic, or hospital.” I agree. If having a community of accountability partners doubles to triples your weight loss, imagine what a positive community can do for your healthspan! Socializing is just as effective as other types of mental exercise when it comes to improving memory and intellectual performance. Plus it’s just more fun!
Poor microbiome
• How it affects your brain: There’s a reason that the gut is considered the second brain. Nine meters long, with five hundred million neurons, featuring thirty major neurotransmitters, it is a chief ally in the function of your nervous system. Problems with the microbiome are associated with autism, anxiety, and depression. On the other hand, a good microbiome, rich in lactobacillus and bifidobacteria, may increase BDNF.35
• How it affects your mind: I can’t put it better than The Atlantic: Your gut bacteria want you to eat a cupcake.36 When your gut microbes and their DNA are out of balance, you may crave sugary foods in order to feed the troublemaking microbes, thereby inducing a vicious cycle of more cravings and more bad microbes.
Thinking Ahead
The best news out of all of this scary stuff is that cognitive decline can be fixed with targeted lifestyle changes, and women have an advantage, if they’re not too old, because of the benefit of natural hormone balancing.
Want to know what Patient Zero did? You’ve already been performing a streamlined version of it in previous weeks, and we’ll add a few additional tenets in this week of the protocol.
• Cut out all refined carbohydrates, gluten, and processed and packaged foods.
• Added vegetables, fruit, and wild fish.
• Fasted for three hours between dinner and bedtime, and for a minimum of twelve hours between dinner and breakfast.
• Purchased an electric toothbrush and flosser and used them regularly.
• Started practicing yoga and, ultimately, became a yoga teacher. She practices yoga sixty to ninety minutes a day at least five times per week.
• Added transcendental meditation twice per day for twenty minutes.
• Began taking melatonin at night; sleep went from four or five to seven or eight hours per night. Other supplements: methylcobalamin, 1 mg/day; fish oil, 2,000 mg/day; vitamin D3, 2,000 IU/day; CoQ10, 200 mg/day.
• Exercised aerobically for thirty to forty-five minutes four to six days per week.
Now age seventy, Patient Zero remains without symptoms of cognitive decline and continues to work full-time, sometimes clocking ten-hour days and traveling internationally. She feels better than she did thirty years ago, and even her libido is high. She continues to eat gluten-free with an occasional glass of red wine.
Reversing or preventing cognitive decline demands a change in diet, exercise, stress, sleep, brain stimulation, and supplements. Patients with Alzheimer’s often have poor hygiene, inflammation, insulin resistance, vitamin D abnormalities and hormonal imbalances, and toxic exposures.
Similar to what you’ve found in the previous weeks of the Younger protocol, during week 7 you’ll make the proven changes to modify your genetic or epigenetic risk of Alzheimer’s. The key is to intervene before the window closes—ideally within ten years of the first symptoms (like my granny getting lost on familiar roads), when there’s still time to reverse the imbalanced signals. Or, even better, way before any symptoms start.
Increase the Good Inputs
You want to begin optimizing the inputs for your brain as early as possible, such as now. Don’t wait until you’re having significant difficulties, because that’s been one of the biggest problems in dementia. We could dramatically reduce the global burden of dementia if people would just get going earlier with improving the brain. As Dr. Bredesen indicated, when you address at least thirty-six neurotrophic inputs in aggregate, you can reverse and prevent cognitive decline. They work together to improve signaling in the brain, from calcium to mitochondria to hormones (like estrogen, progesterone, and testosterone) so that you flip APP toward the remembering side of the equation. Think of it as the brain equivalent of preventing osteoporosis; you are preventing synaptoporosis. You just need a plan that’s proven to make a difference.
Epigenetic effects account for one-third to one-half of cases of Alzheimer’s disease.37 The epigenetic effects result from environmental factors that hasten the onset of dementia: traumatic brain injury, aging, diabetes, hypertension, obesity, sedentary lifestyle, smoking, low educational levels, and stroke.38
Now that you’re scared stiff and want to prevent Alzheimer’s from entering your body, here’s the short list of what prevents it.
Summary: Good Inputs to Prevent Alzheimer’s
1. Eat whole, unprocessed food. Consume healthy fats like medium-chain triglycerides and omega-3s.
2. Keep blood sugar in the normal range (fasting 70 to 85 mg/dL).
3. Sleep seven to eight and a half hours per night.
4. Exercise regularly and intensely.
5. Practice yoga (or another method of observing your thoughts and calming down your nervous system).
6. Create hormone balance, getting a prescription for bioidentical hormone therapy as needed. (Read my first book, The Hormone Cure, for greater detail.) Signs that your hormones are in alignment include solid sleep, strong libido, consistent energy, and a lean body.
Exercise Type, Intensity, Duration
In a study conducted at multiple academic centers (among them the University of Maryland and Cleveland Clinic), a group of ninety-seven cognitively intact older adults, ages sixty-five to eighty-nine, were divided into four groups: high genetic risk (APOE4) and low physical activity; low genetic risk (no APOE4) and low physical activity; high genetic risk and high physical activity; and low genetic risk and high physical activity. Low physical activity applied for people who exercised at low intensity (slow walking, light chores) twice per week or less. High physical activity included one or more of the following three or more days per week:
• Brisk walking, jogging, or swimming for fifteen minutes or more
• Moderately difficult chores for forty-five minutes
• Regular jogging, running, bicycling or swimming for thirty minutes or more
• Playing sports such as tennis for an hour or more
After eighteen months, only the group with high genetic risk and low physical activity showed shrinkage of the hippocampus.39
In another fascinating study, this time from the Cooper Clinic in Dallas, Texas, high levels of fitness and intensity decreased the risk of dementia, diabetes, stroke, and all-cause mortality.40 They followed a group of 19,458 people from 1971 to 2009, and those in the highest quintile of fitness had a 36 percent lower risk of dementia.41 That group included 26 percent women, so ladies, let’s get with the exercise program.
7. Intermittently fast, ideally twice per week.
8. Fill nutritional gaps such as missing zinc and B vitamins (including methylated folate).
9. Clean the air at your home and work. Test and remediate mold, a common cause of type 3 Alzheimer’s disease and chronic inflammatory response syndrome (CIRS). Maintain and replace air filters monthly or as needed for optimal function.
10. Take supplements with neurotrophic and antioxidant effects.
11. Stimulate your brain to learn new things.42
12. Restore gut health by repairing leaky gut and eating nourishing foods for the microbiome. (Signs of leaky gut include chronic gas, bloating, constipation, diarrhea, headaches, fatigue, nutritional deficiencies, poor immune system, memory loss, and food intolerances.)
One of the best ways to preserve and improve your brain is to exercise regularly, probably because it upgrades your brain plasticity, neurogenesis, metabolism, and vascular function, which results in the release of growth factors like BDNF and improved memory and learning.43 Physical exercise prevents neurodegeneration and keeps your hippocampus from shrinking and your cognition from declining, even if you are at genetic risk.44
Mind Makeovers for Weight Loss
Alzheimer’s may be the scariest reason to take care of your brain and mind, but other mental-health issues affect aging.
It is time to address the ways that genetics can affect your behavior with food and, consequently, your weight, and to learn how to work around these tendencies. If there are a lot of people in your family who are overweight or obese (or they work tirelessly to prevent it), listen up, because this is a matter of brain function too. (See appendix for full names.)
• ANKK1/DRD2 increases food desire, overeating, and addictive behaviors. Find pleasure in non-food items, like getting a regular massage, smelling fresh flowers in the house, taking hot baths, practicing yoga or meditation, and drinking green tea (which raises dopamine levels in the brain). Keep a food journal to stay on track and not let the inner addict run the show.
• MC4R is a gene variant that leads to over-snacking. Once you start, it can be very difficult to stop, like an avalanche. Those with the genetic variant are nodding along right now. The gene is expressed in the brain’s hunger center and is linked to obesity. This is the way I handle it: I eat my first meal most days around 7:30, followed by lunch four to six hours later, followed by dinner four to six hours after that. Then I fast three hours before I go to bed (I stop eating by 7:00 p.m.). So I eat three times per day, no snacks. (When intermittently fasting, I eat my first meal around noon, and another four to six hours later.)
• The Fatso gene (FTO) as discussed leaves you having a hard time feeling full. For me, it’s as if someone cut the wires between my stomach and my brain, so I don’t know when to stop eating. Intuitive eating just doesn’t work. I have found that the best work-around is to weigh food and commit to the type and quantities in advance, usually the night before. I know, I know, but it can keep you from overeating. The surprising part is that for me and some of my patients, this process provides more peace. No bargaining or wondering if I’m hungry.
• SLCA2 is a gene variant that gives some of my patients a sweet tooth. These women have an increased likelihood of eating more sweets that tend to go straight to their waistlines and cause brain fog. Our work-around is to include sufficient fruits in their meal plans.45
Integration of Mind and Body to Improve Healthspan
The other key to improving your thinking and healthspan is activating the COMT gene. Your goal is to turn off the worrier gene and turn on the warrior gene, start noticing your thoughts, identifying the negative ones on a regular basis. Becoming an objective witness to your thoughts is imperative. The reason why is that self-talk is often negative and self-defeating and can easily become part of a pattern of neuroticism or negative emotionality.46 It’s like the automatic-pilot setting; it just happens.
Self-talk can lead to either neuroticism or healing. That is, it can be harmful or healthful. Neuroticism refers to the tendency to respond with negative emotions to threat, loss, or frustration. For people who are neurotic, that response is frequent and out of proportion to the circumstances. Not surprisingly, neurotic traits increase your risk of poor health- and life span because they can create anxiety, depression, insomnia, and heart disease.47 I used to joke that I could think my way into hormonal imbalance. Insomnia is particularly correlated with internalization, perfectionism, and an anxious or depressive coping style.48
The mind works best as your servant, not your master. Negative thoughts feel familiar, like a security blanket, so we become accustomed to them—but that doesn’t make them good or healthy. It’s like being in love with a terrorist . . . eventually things will go bad.
You need insight in order to work with the emotional, psychological, and spiritual dimensions of your experience, and it starts by addressing the biological basis. When it comes to retraining the mind, very few people are nutritionally and hormonally balanced enough to benefit from psychotherapy or coaching. If you’re deficient in omega-3 fatty acids, B vitamins, sex or thyroid hormones, it will be hard for you to focus on your mind and soul. Reason and revelation together help us understand ourselves. My advice: correct the imbalances first with this week’s protocol, then address your negative thoughts with the meditation approaches covered in chapter 10. It turns out that you have more influence than you may realize over your thoughts and how they affect your healthspan.
Become a Psychoanalyst at Seventy-Four?
Rita Sussman, Ph.D., is a child psychologist and now psychoanalyst who revels in people and stories. She works part-time providing psychotherapy and psychoanalysis to adults and children and focuses on the interplay between emotional development and learning. Dr. Sussman was raising her children, including my close friend Jo, when she went back to school to complete a Ph.D. in 1979. Her dissertation was on curiosity and exploration, “twin pursuits that have been defining currents” in her life and likewise predict longevity.49 At Jo’s home near mine in Berkeley, Dr. Sussman is a frequent visitor who loves to spend time with her grandkids. She completes her patient care on Thursday afternoon and flies to Oakland to hang out for the weekend. While Jo and I freak out about the usual clamor of busy lives as working moms—unruly kids, overwhelming work/family demands, irritation at the impossible volume of work to be done—Dr. Sussman listens quietly and always offers a kind word, a calm presence, and wisdom that reflects her rich inner life.
Last year, at age seventy-four, Dr. Sussman completed the ten-year process of becoming a psychoanalyst. “Dealing with my dreams, the timelessness of the unconscious, and working through so many points of fragmentation in my life, gradually enabled an emerging sense of robustness and vitality. Developing a relationship with my second analyst allowed me to take pleasure in my accomplishments—indeed trumpet them—and allowed me a wonderful opportunity to believe in the development of my own self as a separate, autonomous being, connected to others, but not needing to be controlled by them or how they felt about me.”
Dr. Sussman has no plans to retire. Her commitment to lifelong learning, curiosity, and being of service to her children, grandchildren, and patients keeps her mind sharp and young: “I’m more willing to accept where I am and recognize what I haven’t done, and recognize that now I am living actually who I am, not who I want to be.” Similarly, I hope you can connect to the timelessness of your unconscious. I want you to find the new idea or passion that you can commit to as a means of keeping your mind young and agile.
Protocol for Week 7: Think
It’s time to make your brain and mind your partners. Most of us don’t know which APOE variant we have, so the key is to act as if you do have APOE4 and commit to the lifestyle interventions that will turn it off. It will improve your inputs and may de-age your brain while boosting your healthspan.
Guess what—you’re already doing many of the basics from earlier in the Younger protocol that improve your brain health and function.
• Keep sleeping seven to eight and a half hours per night, and nap if you get less. Sleep prods the glymphatic system to wash away the beta-amyloid plaques and remove other waste.
• Continue to exercise four to six days per week for at least thirty to forty minutes at a moderate pace, working in several high-intensity intervals, in order to raise BDNF, prompt neurogenesis, and lower blood sugar.50
• Are you still flossing twice per day and brushing three times, with an electric toothbrush? Yes, it prevents cognitive decline (see chapter 5).
• Keep improving mitochondrial function by eating more vegetables and repleting your antioxidant stores, avoiding refined carbohydrates, and intermittently fasting to activate longevity genes.
• Keep taking vitamin D3 and fish oil each day.
Next we’re going to add some of the most important actions to enhance the state of your brain.
Basic Rituals
• Food first. Dietary choices directly affect brain function and help stave off the brain enemies of diabetes and Alzheimer’s.
– Cashews are rich in magnesium (which may help sleep and prevent muscle tightness) and zinc (which may help memory). Add a handful as an appetizer daily or throw ten into a green shake as a meal replacement.
– Quinoa is an ancient seed that is another great source of zinc and folate, which may help prevent dementia. Include it in at least two meals this week.
– Turmeric root is anti-inflammatory; chop and add to quinoa in at least two meals this week. If you can’t find turmeric root, use turmeric powder sprinkled on food.
– Coconut oil51—a single serving of medium-chain triglycerides (the primary fat found in coconut oil) improves cognitive function in patients with memory problems.52 A small randomized trial showed improvement in cognitive impairment at a dose of 56 grams per day (about a quarter cup). Use one tablespoon per serving at least twice this week, perhaps when you make quinoa with turmeric.
– Eat probiotic-rich foods such as kefir, yogurt, kimchi, kombucha, and miso in at least two meals this week.
• Skip the restaurant and takeout this week. Eating eleven to fourteen of your meals at home reduces your risk of diabetes and obesity, which clobber the brain!53 The reason is that you have more control over ingredients and quantities; hopefully you don’t use industrial oils while cooking, and you’re more likely to stop when you’re full.
• Create new neural pathways by using your nondominant hand for activities such as eating, writing, and brushing your teeth. The more new neural pathways you create, the more remembering you do in the balance of remembering and forgetting.
• Make bone broth. It helps to seal the leaks in your gut so that you can make the proper amount of happy-brain chemicals. I use it to make simple soups: I’ll bring one quart of chicken bone broth with one head of cauliflower, chopped, to a boil and simmer twenty minutes, then puree with watercress in my blender, add a little sea salt and ground pepper, and garnish with ancho chili powder. See the appendix for recipes.
• Haven’t tried the oil pulling from chapter 5? Here’s your second chance, because it’s so effective. Do it at least once this week to reset the microbiome in your mouth. Extra credit for doing it daily, then revel in well-deserved pride when your dental hygienist asks what you’ve been up to because your gingivitis is gone and there’s very little plaque on your teeth.
• Smell something essential. Essential oils are proven to alter the biochemistry of your nervous system in powerful ways. Some oils stimulate while others calm you. If you’re feeling low and unmotivated, try inhaling a stimulating scent such as grapefruit, black pepper, or fennel, which double your sympathetic nervous system activity.54 If you need to calm down, try lavender or rose oil.55 If it’s easier, buy a bunch of fragrant roses and inhale the aroma all week long; smelling roses has been shown to improve physiological and psychological relaxation.56
Supplements
Take enough Methylcobalamin to keep your serum level at about 500 pg/ mL or above—typically a dose of approximately 1 mg/day for most people, including Patient Zero. If you live in Japan or Europe, that’s the recommended serum level (500–550 pg/mL), but here in the United States, the cutoff for deficiency is 200 pg/mL.57 No wonder we have higher rates of dementia. There’s a growing problem of marginal B12 serum levels, with 39 percent of people aged 26 and 83 in the low-normal range where people experience fatigue, memory problems, and other neurological symptoms.58 Rates of low-normal levels are increased among vegetarians and vegans.59 You need it for DNA synthesis,60 to make red blood cells, and for bone strength. Consult with a knowledgeable clinician because many more nuances exist in interpreting your levels and how vitamin B12 is trafficked in your body.
Advanced Projects
Remember, we’re trying to stop the leaks from thirty-six holes in the roof. The more you take on this week, the more likely you’ll prevent or reverse the big “A.”
• Try a new form of exercise this week. Use the Younger protocol to continue breaking out of your old patterns with fitness—it’ll create new neural pathways. Ideas: start jumping rope; go to a spin, barre, or Pilates mat class; sign up with a trainer and learn high-intensity interval training with weights. Quick reminder: higher intensity exercise reduces your risk of Alzheimer’s disease.
• Take more supplements.
– Citicoline (CDP choline), a dietary supplement used commonly in Europe, may help your brain if you’re lower than normal in your mental functioning.61 As little as a single dose can improve processing speed, working memory, verbal learning, and executive function in healthy people with low-baseline cognitive functioning. Despite that, it has no effects in medium-baseline performers and it impairs high-baseline performers. Until we know more, only take it if you have cognitive impairment such as from dementia, acute ischemic stroke, or acute concussion; dose 500 to 1,000 mg. (In acute ischemic stroke, 2,000 mg.62)
– CoQ10 will feed your mitochondria. Take 100 to 200 mg per day.
• Talk to a functional medicine clinician, hormone expert, or gynecologist about whether you’re a good candidate for getting your hormones in balance. In particular, you want your estradiol, progesterone, and testosterone in the healthy range. Under proper care, you may improve memory, libido, and energy while staving off Alzheimer’s disease.
• Pick a new cognitively stimulating activity from the following list and perform the task for around forty-five minutes at least twice this week.
– Learn a new language.
– Bake or cook.
– Take up a new musical instrument.
– Complete a crossword puzzle.
• Test your methylation capacity—your ability to methylate genes to turn them off. You may be methylating too much or too little.
• Assess your microbiome.
• Try NeuroRacer, a therapeutic video game created by Professor Adam Gazzaley of the University of California at San Francisco. Video games are no longer just for teens; Gazzaley designed NeuroRacer to combat age-related mental decline by using neurofeedback and TES (transcranial electrical stimulation) to boost the brain. The game requires that you steer a virtual car while performing other tasks. After playing for twelve hours (not consecutively!), older folks improved so strikingly that they were edging out twenty-year-old novices. The game specifically aids working memory and attention span, and improved skills that were transferable to the real world.63 (See Resources for details.)
• Join a community or build one around your interests. I have a yoga community, a school community around my daughters’ schools, a functional medical community, and, very excitingly, a community growing around the Younger protocol. As you may have read in the science section, community is a powerful lever for remembering and keeping your brain and mind healthy as you age.
• Try nutritional ketosis with high fat (70 percent), moderate protein (20 percent), and low carbohydrates (10 percent). In my opinion, nutritional ketosis works better for men than women and may worsen thyroid and adrenal function. I suggest trying nutritional ketosis in collaboration with a knowledgeable health practitioner who can track your results and help determine if it’s a good fit for you.
What to Take After a Brain Injury
When I experienced a traumatic brain injury in 2015, I had a functional neurologist named Dr. Jay Lombard on speed dial. Here are the immediate treatments that he recommended:
• CDP choline, a supplement that acts as a neurotroph (makes the brain grow)
• Allopregnanolone, a hormonal metabolite of progesterone (You have to take it sublingually because it won’t get into your body if you swallow it.)
• Zofran, if you’re like me and experience nausea as a sign of brain inflammation.
• Depakote, an antiseizure medication that is available by prescription only.
Recap: Benefits of Week 7
Within one week, you may experience improved memory, focus, and mental acuity. Carried out over the long term, you can expect this week’s changes to reduce your risk of accumulated oxidative stress and other bad pathways of neurodegeneration so that you can reverse or prevent cognitive decline and lower your chance of early death.
Bottom Line
Richard Dawkins says that genes created us, body and mind. It’s true that they are the key to your past, present, and future. But they aren’t the only factor. Once you’re born and start making choices, it’s your balance of inputs and outputs that create a brain and mind that are fit for a long healthspan. Yes, your genes are set for life, but you can change how the environment interacts with your genes. Your physical healthspan will never be at its best if your brain, mind, and nervous system aren’t at their best. When you clean out your head space, you’ll be able to create who you want to be in the moment and stay mentally sharp for years, allowing you to consistently choose the best actions that keep the aging process in check.