3 Who is at Risk of Osteoporosis?
Osteoporosis and osteoporotic fractures are more common in women than men. In each age group, in fact, the fracture risk for women is higher. One of the reasons for this is that men have bigger bones, which in itself seems to protect against fracture. At around the age of 50, women experience the menopause and at this time their ovaries virtually stop producing the hormone oestrogen, which helps to keep bones strong, although HRT can mitigate this (see here). Women also tend to live longer.
According to the Royal Osteoporosis Society (ROS), the risk factors that can affect your bone stress and the possibility of osteoporosis are:
• Excessive drinking
• Smoking. People who smoke put themselves at risk of breaking bones, because smokers tend to have a lower body weight. It’s also thought that smoking has a direct negative effect on the bone-building cells, and women who smoke may have an earlier menopause (before the age of 45). Even some passive smokers – women who live with heavy smokers – have been found to have an earlier-than-average menopause, with risk of greater reduction of bone density
• Heavy caffeine intake
• Slight build, low body weight. If you have a low body weight, you are likely to have less bone tissue overall and also less padding, which is important should you have a fall. A BMI (body mass index) below 19kg/m is considered a risk factor for osteoporosis and painful fractures
• Early menopause before the age of 45
• Family history of osteoporosis, especially in close female relatives (i.e. mother or grandmother)
• Lack of exercise
• Prolonged bed rest or immobility
• Fair skin (people who are black Afro-Caribbean are at lower risk of developing osteoporosis than those who are Caucasian or Asian origin)
• Lack of sufficient calcium in diet throughout life
• Vitamin D deficiency. This reduces the body’s ability to utilise calcium
• Long-course cortisone or thyroid treatment
• Excessive dieting. Anorexia or bulimia sufferers are particularly vulnerable
• Excessive exercise. Women such as marathon runners, who have a low body weight (which can cause periods to diminish), are at risk. The risks are from both the reduction in hormones and the exercise. Excessive exercise produces wear and tear on the mechanical structure of bone, causing stress fractures. Time off between exercising is essential
• Conditions that affect the absorption of food, such as Crohn’s or coeliac disease. This leads to the malabsorption of vitamin D and calcium, a risk factor in reducing bone density
• Conditions that predispose osteoporosis, such as rheumatoid arthritis. This can be due to the treatments given – such as steroids or new bioagents – which cause the loss in bone density
• Taking certain medications. According to the Royal Osteoporosis Society these include glucocorticoids (steroids) taken for more than three months, anti-epileptic drugs and antidepressants. Injectable contraceptives prevent periods, creating false amenorrhoea at the time when there should be peak bone mass gain. Breast cancer treatments, such as aromatase inhibitors, are also a risk – as are prostate cancer drugs, which affect either the production of the male hormone testosterone or the way that it works in the body. More research is needed on other medicines, but if you are concerned talk it over with your doctor
• Low levels of the sex hormone oestrogen in women and low levels of the sex hormone testosterone in men. This may have an effect on bone health, so discuss treatment and management of these conditions with your doctor
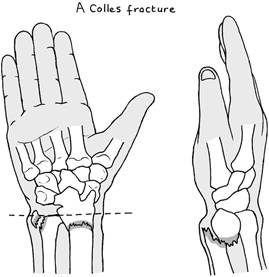
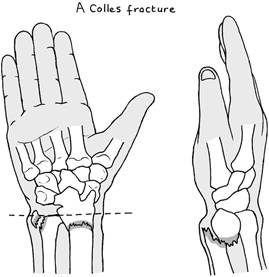
Osteoporotic fractures can occur in various parts of the body, but the most commonly affected sites are the hips, spine and wrists, and a fracture could be the first indication of osteoporosis. Healthy bones should be able to withstand a simple fall. My Colles fracture occurred when I put out my arm to break my fall while ice skating – and, sadly, broke my wrist instead! Fractures that occur because of reduced bone strength are called fragility fractures, and many of them will be caused by osteoporosis. Bones affected by osteoporosis don’t feel painful, but as I know from my own experience broken bones can cause pain and other mobility problems.
A broken hip is usually the result of a fall that can happen so suddenly and unexpectedly while doing everyday activities. It can be particularly painful and has an immediate effect on day-to-day living. Most people will require an operation. For a person who was previously fit, the chances are that they will recover well and get back home, which is all-important. With appropriate physiotherapy and possible help from social services, they can look forward to returning to independent living. But for others less fortunate – more often than not in their late 70s or 80s or in frail health – recovery can be difficult. As if this isn’t distressing enough, it is chilling to realise that statistics show that one month after suffering a fracture of the hip, 1 in 14 people will have died – and around half will remain in long-term care.
Spinal or vertebral fractures usually occur in the thoracic (middle) or lumbar (lower) areas of the spine, as a result of bones becoming squashed because of their reduced strength. These are sometimes referred to as crushed, collapsed or wedge fractures, or they are called compression fractures. Back pain is the most common symptom, with pain varying from person to person. Spinal fractures take from 6 to 12 weeks to heal but can persist for a longer period. For the majority of people, spinal fractures do not interfere with the spinal cord or result in paralysis. (This does happen, but only in very unusual cases.) People with very weak bones must be aware that fractures can occur if they move awkwardly, such as when turning quickly, reaching up, or bending down.
When spinal bones heal, they don’t return to their original shape but are often flattened or wedge-shaped. This can cause a loss of height and the spine to tip forwards in an outward curve (kyphosis), which results in a curvature of the spine, unkindly termed ‘dowager’s hump’. As a result of these spinal changes there is a shortage of space for the internal organs, which can cause a protruding tummy, indigestion, breathlessness and possible stress incontinence. These postural changes can be distressing and have a negative effect on body image, sometimes resulting in depression.
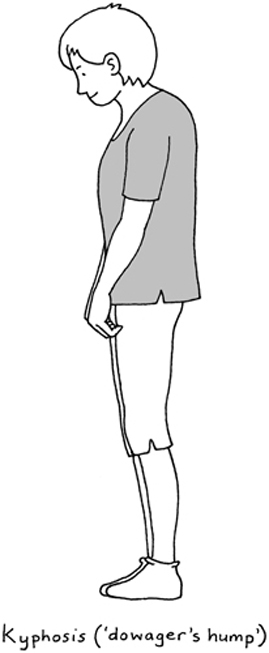
Not all fractures cause problems and disabilities. Keeping fit and active into older age, plus good hospital treatment and aftercare, will help reduce fractures affecting your quality of life. However, for some people a change in posture and shape can prove problematic when it comes to everyday dressing, and can be something of a challenge when it comes to shopping. Finding clothes to suit a changing body shape after vertebral compression fractures can be difficult.
One of the most important things to remember about choosing and buying clothes is to continue to buy what you like. Clothes are the first impression we give people of ourselves and inevitably reflect our personality. For people with significant postural changes, this is easier said than done and the hunt for a suitable outfit can be difficult. Sometimes this means that people have to compromise on style and fashion in order to find a garment that actually fits them and which is comfortable to wear. While there is no perfect solution in terms of finding clothes to fit a changing body shape, there are a number of things that you can do to draw the eye away from the main problem areas. Help is at hand to give you some ideas and pointers of what to look for when buying clothes and advice on garment styles, fabrics and colour. (See ‘Clothing, body image and osteoporosis’ on the Royal Osteoporosis Society’s excellent website for information.)
Bone loss can be gradual, with nothing noticeable at first, but it’s what happens in the long run that counts. A typical sign is the broken wrist (Colles fracture). We know the scenario: a woman slips and falls on an outstretched hand. I use the word ‘woman’ advisedly, because it happens more often to women than to men, and at an average age of 60. Fracture of the femur, the thigh bone, is another indicator that can happen through quite a minor fall. The incidence rises with increased age in both men and women, but again it’s women who are statistically more prone to these injuries. One estimate suggests that about 60 per cent of elderly women will experience wedging of bones in the spine. Hip fractures increase after the age of 70. They are the most serious of the four types of fracture connected with osteoporosis. While the other kinds may cause pain, they rarely need much medical care. But hip fractures are associated with hospitalisation, permanent disability and possible death in old age.
And yet, I say again that some of the fractures associated with osteoporosis are preventable. It pays to find out more about your risk factors because there may be actions you can take to reduce these risks and make fragility fractures less likely. We can all help ourselves to slow down the onset and prevent osteoporosis by changes in lifestyle. If your risk of fracture is high, a drug treatment may be recommended to strengthen your bones and reduce the risk of fracture. Specialised drugs are available to maintain bone density, plus drugs to slow down bone loss, including HRT (hormone replacement therapy).