Manometric Studies
Overview
Manometric studies evaluate certain areas of the body by using a manometric device to measure and record pressures. These devices can be as familiar to the patient as a blood pressure instrument or as foreign as the one used in oculoplethysmography (OPG) to record eye pressures. Table 6-1 lists the various tests and the areas evaluated.
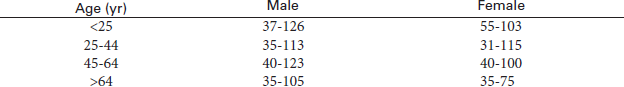
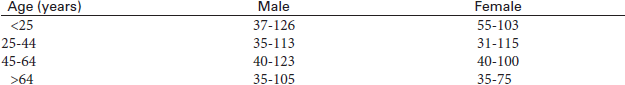
TABLE 6-1
Manometric Studies and Areas Evaluated
| Test | Area Evaluated |
| Cystometry | Bladder |
| Esophageal function studies | Esophagus |
| Oculoplethysmography | Ophthalmic artery |
| Plethysmography | Arterial pressures |
| Tilt-table testing | Blood pressure |
| Urethral pressure profile | Urethra |
Procedural Care for Manometric Studies
Before
• Explain the purpose and procedure to the patient. Patient cooperation is essential in these studies. Many of these studies require informed consent.
• Fasting requirements vary according to the particular study performed. For example, no fasting is required for cystometry. The patient must be fasting for esophageal function studies.
During
• Patient positioning depends on the procedure indicated.
• A particular type of manometer is applied to the patient. For example, blood pressure cuffs are applied to the extremities for arterial plethysmography. A catheter is inserted into the bladder and attached to a pressure monitor for cystometry.
• Patients must remain very still during the procedure. Movement can affect the pressure readings.
Potential Complications of Manometric Studies
There are few complications associated with these tests. The few that do occur vary markedly from test to test. For example, gastric aspiration is a potential complication of esophageal function studies. Conjunctival hemorrhage is a potential complication of OPG.
Cystometry (Cystometrogram [CMG])
Normal Findings
Indications
This test is used to measure pressures within the bladder to identify patients who have bladder dysfunction. It is used in patients with bladder outlet obstruction, urinary incontinence, and questionable neurogenic bladder. It is also used to document progress in treatment of these abnormalities.
Test Explanation
The purpose of cystometry is to evaluate the motor and sensory function of the bladder when incontinence is present or neurologic bladder dysfunction is suspected. A graphic recording of pressure exerted at varying phases of the filling of the urinary bladder is produced. A pressure/volume relationship of the bladder is determined. This urodynamic study assesses the neuromuscular function of the bladder by measuring the efficiency of the detrusor muscle, intravesical pressure and capacity, and the bladder's response to thermal stimulation.
Cystometry can determine whether a bladder function abnormality is caused by neurologic, infectious, or obstructive diseases. Cystometry is indicated to elucidate the causes of bladder outlet obstruction or frequency and urgency, especially before surgery on the urologic outflow tract. Cystometry is also part of the evaluation for the following: incontinence, persistent residual urine, vesicoureteral reflux, motor and sensory disorders affecting the bladder, and the effect of certain drugs on bladder function.
This test is performed by a urologist in approximately 45 minutes and is often performed at the same time as cystoscopy. The only discomfort is that associated with the urethral catheterization. Nocturnal examinations can be performed to evaluate nocturnal incontinence.
Procedure and Patient Care
Before
![]() Explain the purpose and the procedure to the patient.
Explain the purpose and the procedure to the patient.
![]() Tell the patient that no fluid or food restrictions are needed.
Tell the patient that no fluid or food restrictions are needed.
![]() Assure the patient that he or she will be draped to prevent unnecessary exposure.
Assure the patient that he or she will be draped to prevent unnecessary exposure.
• Assess the patient for signs and symptoms of urinary tract infection.
![]() Instruct the patient not to strain while voiding because the results can be skewed.
Instruct the patient not to strain while voiding because the results can be skewed.
During
• Note the following procedural steps:
1. Cystometry, usually performed in a urologist's office or a special procedure room, begins with the patient being asked to void.
2. The amount of time required to initiate voiding and the size, force, and continuity of the urinary stream are recorded. The amount of urine, the time of voiding, and the presence of any straining, hesitancy, or terminal urine dribbling are also recorded. (See the discussion of urine flow studies, p. 701.)
3. The patient is placed in a lithotomy or supine position.
4. A retention catheter is inserted through the urethra and into the bladder.
5. Residual urine volume is measured and recorded.
6. Thermal sensation is evaluated by the instillation of approximately 30 mL of room-temperature saline solution into the bladder followed by an equal amount of warm water. The patient reports any sensations.
7. This fluid is withdrawn from the bladder.
8. The urethral catheter is connected to a cystometer (a machine used to monitor bladder pressure).
9. Sterile water, normal saline solution, or carbon dioxide gas is slowly introduced into the bladder at a controlled rate, usually with the patient in a sitting position. While the bladder is slowly filled, pressures are simultaneously recorded. This is called a cystometrogram.
10. Patients are asked to indicate the first urge to void and then when they have the feeling that they must void. The bladder is full at this point.
11. The pressures and volumes are plotted on a graph.
12. The patient is asked to void around the catheter, and the maximal intravesical voiding pressure is recorded.
13. The bladder is drained for any residual fluid or gas.
14. If no additional studies are to be done, the urethral catheter is removed.
15. For urethral pressures, fluid or gas is instilled through the catheter, which is withdrawn while pressures along the urethral wall are obtained. (See the discussion of the urethral pressure profile, p. 700.)
• Throughout the study, ask the patient to report any sensations, such as pain, flushing, sweating, nausea, bladder filling, and an urgency to void.
• Note that certain drugs may be administered during the cystometric examination to distinguish between underactivity of the bladder because of muscle failure and underactivity associated with denervation. Cholinergic drugs (e.g., bethanechol [Urecholine]) may be given to enhance the tone of a flaccid bladder. Anticholinergic drugs (e.g., atropine) may be given to promote relaxation of a hyperactive bladder. If these drugs are to be given, the catheter is left in place.
After these drugs are given, the examination is repeated 20 to 30 minutes later, using the first test as a control value. The information obtained with the drugs assists in deciding whether drugs will be effective treatment.
After
• Observe the patient for any manifestations of infection (e.g., elevated temperature, chills, or dysuria).
• Examine the urine for hematuria. Notify the physician if the hematuria persists after several voidings.
• Provide a warm sitz bath or tub bath for the patient's comfort if desired.
• Note that pelvic floor sphincter electromyography (p. 576) can be performed to evaluate the urethral sphincter in cases of incontinence.
Test Results and Clinical Significance
Neurogenic bladder: With loss of motor function of the bladder, reduced filling pressures and detrusor pressures are observed. Increased residual volume of urine is also noted. Sensation of fullness and temperature is often diminished or absent. There are several different classifications of neurogenic bladder, some of which are based on the cystometry findings. Spina bifida cord injury, compression, or demyelinating diseases can cause a neurogenic bladder. Diabetic neuropathy, anticholinergics, and alpha-adrenergic antagonists also diminish bladder muscle tone. Extensive pelvic surgery can interrupt the peripheral nerve fibers to the bladder, thereby creating a neurogenic bladder.
Bladder obstruction: Bladder outlet obstruction is evidenced by a reduced urine flow, increased intravesicular pressures while voiding, and residual urine volume. Although congenital causes (e.g., urethral valves, phimosis, meatal stenosis) of bladder outlet obstruction can occur, the most common cause of bladder outlet obstruction is a prostatic pathologic condition (cancer or hypertrophy). In women the most common cause of outlet obstruction is a neoplasm (usually of the cervix) or neurogenic bladder (see previous discussion).
Bladder infection: Urgency and reduced bladder capacity are noted. Discomfort associated with bladder distention may be enhanced.
Bladder hypertonicity: Increased pressures are noted with filling. Capacity is reduced. This occurs with some forms of spastic paralysis. This is most common with upper motor neuron disease or injury.
Diminished bladder capacity: This may be the result of post–radiation-therapy fibrosis or an extrinsic tumor compressing the bladder. A fibrotic and inflamed bladder cannot distend adequately. Likewise, when a tumor compresses the bladder, the bladder cannot distend. Capacity is reduced.
Related Tests
Urine Flow Studies (p. 701). This is a measurement of urine flow per unit of time and is used to diagnose bladder outlet obstruction.
Pelvic Floor Sphincter Electromyography (p. 576). This is a measurement of the electrical activity of the periurethral sphincter function.
Cystography (p. 1036). This is an x-ray contrast study of the bladder. Outlet obstruction is evident on this study.
Esophageal Function Studies (Esophageal Manometry, Esophageal Motility Studies)
Indications
This test is used to identify and document the severity of diseases affecting the swallowing function of the esophagus. It is also used to document and quantify gastroesophageal reflux. A wide variety of motor disturbances can be identified. It is commonly used on patients with heartburn, chest pain, or difficulty swallowing.
Test Explanation
Esophageal function studies include the following:
1. Determination of the lower esophageal sphincter (LES) pressure (manometry)
2. Graphic recording of esophageal swallowing waves, or swallowing pattern (manometry)
3. Detection of reflux of gastric acid back into the esophagus (acid reflux)
4. Detection of the ability of the esophagus to clear acid (acid clearing)
5. An attempt to reproduce symptoms of heartburn (Bernstein test)
Manometric Studies
Two manometric studies are used in assessing esophageal function: (1) measurement of LES pressure and (2) graphic recording of swallowing waves (motility). The LES is a sphincter muscle that acts as a valve to prevent reflux of gastric acid into the esophagus. Free reflux of gastric acid occurs when the sphincter pressures are low. An example of such a disorder in adults is gastroesophageal reflux; in children, it is called chalasia (incompetent or relaxed LES).
With increased sphincter pressure, as found in patients with achalasia (failure of the LES to relax normally with swallowing) and with diffuse esophageal spasms, food cannot pass from the esophagus into the stomach. Increased LES pressures are noted on manometry. In achalasia, few if any swallowing waves are detected. In contrast, diffuse esophageal spasm is characterized by strong, frequent, asynchronous, and nonpropulsive waves.
Acid Reflux With pH Probe
Acid reflux is the primary component of gastroesophageal reflux. Patients with an incompetent LES will regurgitate gastric acid into the esophagus. This will then cause a drop in the esophageal pH during esophageal pH monitoring. With the newer and smaller catheters, 24-hour pH monitoring can be performed. Episodes of acid reflux are evident. If they coincide with patient symptoms of chest pain, esophagitis can be incriminated. Transnasal pH catheters can cause discomfort in patients, sometimes resulting in the avoidance of pH testing, which is the “gold standard” for measuring pH levels in the esophagus. This limits the ability to definitively diagnose and ultimately treat gastroesophageal reflux disease (GERD).
With the wireless pH probes, patients can eat and drink normally as well as engage in their usual activities while having their pH levels tested. A wireless pH-probe capsule is now being used with increasing frequency. It collects pH data in the esophagus and transmits it via radio frequency telemetry to an external, pager-sized receiver worn by the patient. This allows patients to maintain regular diet and activities during the monitoring period (24 to 48 hours). This small pH capsule is attached to the wall of the esophagus by esophagoscopy (p. 608). Within days, the capsule spontaneously sloughs off the wall of the esophagus and passes through the patient's gastrointestinal tract. After the study is completed, the patient returns the receiver, and the data is downloaded to a computer for analysis.
Acid Clearing
Patients with normal esophageal function can completely clear hydrochloric acid from the esophagus in less than 10 swallows. Patients with decreased esophageal motility (frequently caused by severe esophagitis) require a greater number of swallows to clear the acid.
Bernstein Test (Acid Perfusion)
The Bernstein test is simply an attempt to reproduce the symptoms of gastroesophageal reflux. If the patient suffers pain with the instillation of hydrochloric acid into the esophagus, the test is positive and proves the patient's symptoms are caused by reflux esophagitis. If the patient has no discomfort, a cause other than esophageal reflux must be sought to explain the patient’s discomfort.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
![]() Instruct the patient not to eat or drink anything for at least 8 hours before the test.
Instruct the patient not to eat or drink anything for at least 8 hours before the test.
![]() Allay any fears and allow the patient to verbalize concerns. Be sensitive to the patient's fears about choking during the procedure.
Allay any fears and allow the patient to verbalize concerns. Be sensitive to the patient's fears about choking during the procedure.
![]() Tell the patient that except for some initial gagging when swallowing the tubes, these tests are not uncomfortable.
Tell the patient that except for some initial gagging when swallowing the tubes, these tests are not uncomfortable.
During
• Note the following procedural steps:
1. Esophageal studies are usually performed in the endoscopy laboratory.
2. The fasting, unsedated patient is asked to swallow two or three very tiny tubes. The tubes are equipped so that pressure measurements can be taken at 5-cm intervals (Figure 6-1).
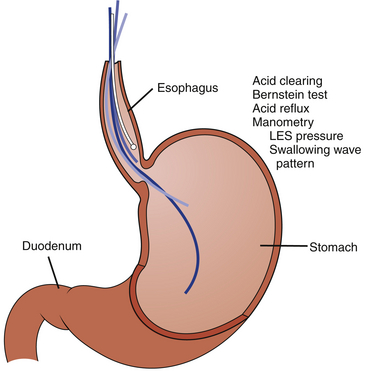
Figure 6-1 Esophageal function studies demonstrating placement of manometry tubes and a pH probe within the esophagus.
3. The outer ends of the tubes are attached to a pressure transducer.
4. All tubes are passed into the stomach; then three tubes are slowly pulled back into the esophagus. A rapid and extreme increase in the pressure readings indicates the high-pressure zone of the LES.
5. The LES pressure is recorded.
6. With all tubes in the esophagus, the patient is asked to swallow. Motility wave patterns are recorded.
7. The pH indicator probe is placed in the esophagus.
8. The patient's stomach is filled with approximately 100 mL of 0.1-N hydrochloric acid. A decrease in the pH of the esophageal pH probe indicates gastroesophageal reflux.
9. Hydrochloric acid is instilled into the esophagus, and the patient is asked to swallow. The number of swallows is counted to determine acid clearing. More than 10 swallows to clear the acid (as determined by the pH probe) indicates decreased esophageal motility.
10. Finally, 0.1-N hydrochloric acid and saline solution are alternately instilled into the esophagus for the Bernstein test. The patient is not told which solution is being infused. If the patient volunteers symptoms of discomfort while the acid is running, the test is considered positive. If no discomfort is recognized, the test is negative.
• Note that these tests are performed by an esophageal technician in approximately 30 minutes.
![]() Inform the patient that the test results are interpreted by a physician and are available in a few hours.
Inform the patient that the test results are interpreted by a physician and are available in a few hours.
Test Results and Clinical Significance
Presbyesophagus: This is a common motility pattern noted among the elderly. It is evident as asynchronous esophageal contractions. As a result, the food is not propelled down the esophagus but, rather, becomes temporarily lodged between the two areas of contraction. This can be quite painful along with causing a functional obstruction to the passage of food.
Diffuse esophageal spasm: Spastic synchronously occurring contractions of the esophagus do not allow the food to be propelled down the esophagus but, rather, lodge it temporarily between the two areas of contraction. This, too, can be quite painful along with causing a functional obstruction to the passage of food.
Chalasia: Absence of tone in the lower esophageal sphincter allows for free reflux of food and gastric juices into the esophagus. This is a common cause of vomiting in newborns.
Achalasia: This is the opposite of chalasia and most commonly occurs in young adults. The tone of the LES is significantly increased. No relaxation of the sphincter occurs. As a result, the LES acts as an obstruction to the passage of food through the esophagus.
The presence of gastric contents in the esophagus causes esophagitis. The pathophysiology of gastroesophageal reflux is not completely understood. It is known that the LES tone is reduced. This allows acid to reflux into the esophagus. This is evident during pH monitoring. Esophagitis follows, and acid clearing is prolonged because the swallowing function of the inflamed esophagus is reduced.
Related Tests
Esophagoscopy (p. 608). This is an endoscopic test of the esophagus. Reflux esophagitis, esophageal obstruction, achalasia, and other diseases, can be observed.
Barium Swallow (p. 999). This is an x-ray study of the esophagus. Evidence of diseases of the esophagus as listed for esophagoscopy can be visualized.
Plethysmography, Arterial
Indications
This is a noninvasive method of identifying and monitoring treatment of arterial occlusive disease.
Test Explanation
Plethysmography is usually performed to rule out occlusive disease of the lower extremities; however, it also can identify arteriosclerotic disease in the upper extremities. This test does require one normal extremity against which the other extremities may be compared.
Arterial plethysmography is performed by applying three blood pressure cuffs to the proximal, middle, and distal parts of an extremity. Pressure readings are also taken in the upper arm (brachial) artery. These are then attached to a pulse volume recorder (plethysmograph) that enables each pulse wave to be displayed. A reduction in amplitude of a pulse wave in any of the three cuffs indicates arterial occlusion immediately proximal to the area where the decreased amplitude is noted. Also, measurements of arterial pressures are performed at each cuff site. A difference in pressure of greater than 20 mm Hg indicates a degree of arterial occlusion in the extremity. A positive result is reliable evidence of arteriosclerotic peripheral vascular occlusion. However, a negative result does not definitely exclude this diagnosis, because extensive vascular collateralization can compensate for even a complete arterial occlusion.
An Ankle/Brachial Ratio of <0.9 indicates peripheral vascular disease in the lower extremity. Arterial plethysmography can also be performed immediately after exercise to determine if symptoms of claudication are caused by peripheral vascular occlusive disease.
Although it is not as accurate as arteriography (see p. 988), plethysmography is performed without serious complications and can be done for extremely ill patients who cannot be transported to the arteriography laboratory.
Interfering Factors
• Arterial occlusion proximal to the extremity
• Cigarette smoking, because nicotine can cause transient arterial constriction
Procedure and Patient Care
Before
During
• Note the following procedural steps:
1. The patient is placed in the semirecumbent position.
2. The cuffs are applied to the extremities and then inflated to 65 mm Hg to increase their sensitivity to pulse waves.
3. The pulse waves are recorded on the plethysmographic paper.
4. The amplitudes and form of the pulse wave of each cuff are measured and compared. A marked reduction in wave amplitude indicates arterial occlusive disease.
• Note that this test usually is performed in the noninvasive vascular laboratory or at the patient's bedside by a noninvasive vascular technologist in approximately 30 minutes.
![]() Inform the patient that results are usually interpreted by a physician and are available in a few hours.
Inform the patient that results are usually interpreted by a physician and are available in a few hours.
Test Results and Clinical Significance
Arterial atherosclerotic occlusive disease,
Arterial occlusion is noted by a decreased pressure in the cuff immediately distal to the occlusion.
Small vessel diabetic changes: Little or no change may be noted in this disease. This type of vascular insufficiency is usually seen in diabetics.
Vascular diseases (e.g., Raynaud phenomenon): Arterial occlusion that is episodic is classic for Raynaud phenomenon. This is difficult to identify on plethysmography unless larger vessels of the wrist or hand are involved. Often this diagnosis requires that pressure-sensitive cuffs be placed on the fingers.
Related Tests
Doppler Arterial Flow Studies (p. 900). This ultrasound examination determines blood flow within the artery suspected to be stenotic. This is a very accurate test of arterial patency.
Tilt-Table Testing
Indications
The tilt-table test is a provocative test used to diagnose vasopressor and vasovagal syncope.
Test Explanation
Patients with this vasomotor syncope syndrome usually demonstrate symptomatic hypotension and syncope within a few to 30 minutes of being tilted upright by approximately 60 to 90 degrees. This test is usually performed with an electrophysiologic study (p. 559). Tilt-table testing is often used to assess the efficacy of prophylactic pacing in some patients with vasopressor syncope. It is also used to evaluate the impact of posture on some forms of tachyarrhythmias. Normally a minimal drop in systolic blood pressure, rise in diastolic blood pressure, and increase in heart rate occur in the tilted position. Patients with vasopressor or vasovagal syncope demonstrate these changes in an exaggerated fashion and become light-headed and dizzy on assuming the tilted position.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
• Obtain intravenous (IV) access in the event emergency drugs are required.
• Note that an arterial line can be placed to accurately monitor blood pressure.
![]() Ask whether the patient has had excessive fluid loss (diarrhea or vomiting) in the previous 24 hours.
Ask whether the patient has had excessive fluid loss (diarrhea or vomiting) in the previous 24 hours.
• Record antihypertensive or diuretic medicines that the patient may be taking.
During
• Have the patient lie supine on a horizontal tilt table.
• Obtain the patient's blood pressure and pulse as baseline values before tilting is carried out.
• Note that the table is progressively tilted to 60 to 80 degrees while the patient is being monitored. Alternatively, the patient is asked to sit or stand.
• Monitor these vital signs during the procedure.
![]() Question the patient about the presence of symptoms of dizziness and lightheadedness.
Question the patient about the presence of symptoms of dizziness and lightheadedness.
Related Test
Electrophysiologic Study (p. 559). This is a method of studying evoked potentials within the heart. It is used to evaluate patients with syncope, palpitations, or arrhythmias.
Tourniquet Test (Capillary Fragility)
Indications
This test evaluates capillary integrity. It is used to aid in the clinical diagnosis of hemorrhagic fever (Dengue fever).
Test Explanation
Petechiae occur as a result of increased capillary fragility (microvessels easily rupture and a small amount of bleeding occurs in the skin) or thrombocytopenia (causing spontaneous bleeding in the skin). There are more accurate tests to indicate platelet count (p. 401) and function (p. 404). Petechiae are small, round nonraised red spots in the skin.
Production of petechiae can be induced in patients who have increased capillary fragility or thrombocytopenia. There are two methods of inducing petechiae. The most common is with positive pressure. A blood pressure cuff is applied to an extremity and inflated above venous pressure. The second way is with negative pressure. A suction cup is applied to an area of skin for a particular period of time. Patients with thrombocytopenia, poor platelet function, or purpura will develop more than 10 petechiae per square inch of skin. The number of petechiae can be graded from few to confluent (1 to 4).
Interfering Factors
• Premenstrual women experience transient episodes of increased capillary fragility.
• Postmenopausal women who do not use hormones experience increased capillary fragility.
• Women, especially those with sun-damaged skin, can have increased capillary fragility.
Test Results and Clinical Significance
Positive: Greater Than 2 Petechiae
Immunologic thrombocytopenia (e.g., idiopathic thrombocytopenic purpura),
Drug-induced thrombocytopenia,
Thromboasthenia (poor platelet function):
Reduced platelets cause spontaneous microbleeding. Nonimmunologic thrombocytopenia is rarely associated with a positive tourniquet test.
Related Tests
Platelet Count (p. 401). This is a direct measurement of platelet number.
Platelet Volume, Mean (p. 407). This is a direct measurement of platelet volume.
Platelet Aggregation (p. 398). This is a direct measurement of platelet function.
Platelet Antibody (p. 399). This test identifies platelet antibodies that destroy the platelet.
Urethral Pressure Profile (UPP, Urethral Pressure Measurements)
Indications
This test is often a part of cystometry (p. 688). It is used to document reduced urethral pressures in incontinent patients (e.g., females with stress incontinence or males after prostatectomy). It is also used to indicate the degree of compression applied to the urethra from an abnormally enlarged prostate (which will increase UPP value).
Test Explanation
The UPP indicates the intraluminal pressure along the length of the urethra with the bladder at rest. Indications for this urodynamic investigation include the following:
1. Assessment of prostatic obstruction
2. Assessment of stress incontinence in females
3. Assessment of postprostatectomy sequela of incontinence
4. Assessment of the adequacy of external sphincterotomy
5. Analysis of the effects of drugs on the urethra
6. Analysis of the effects of stimulation on urethral flow
7. Assessment of the adequacy of implanted artificial urethral sphincter devices
This test is usually performed by a urologist in less than 15 minutes. This test is only slightly more uncomfortable than urethral catheterization.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
![]() Because many patients are embarrassed by this procedure, assure the patient that he or she will be draped to ensure privacy.
Because many patients are embarrassed by this procedure, assure the patient that he or she will be draped to ensure privacy.
During
• Note the following procedural steps:
1. A catheter is placed into the bladder and attached to a pressure monitor machine.
2. Fluids (or gas) are instilled through the catheter, which is withdrawn while the pressures along the urethral wall are measured.
3. A constant infusion of the fluids or gas is maintained by a motorized syringe pump.
Related Test
Cystometry (p. 688). This test often includes UPP. This test, which can identify bladder neuromuscular pathologic conditions, is a measure of bladder pressures.
Urine Flow Studies (Uroflowmetry, Urodynamic Studies)
Indications
This test is used to evaluate bladder and urethral dysfunction and/or voiding abnormalities. This test is indicated to investigate dysfunctional voiding or suspicious outflow tract obstruction. It is also done before and after any procedure designed to modify the function of the urologic outflow tract.
Test Explanation
Uroflowmetry is the simplest of the urodynamic techniques, being noninvasive and requiring uncomplicated and relatively inexpensive equipment. This study measures the volume of urine expelled from the bladder per second. If the rate is reduced, outflow obstruction can be documented and measured.
The urine flow depends greatly on the volume of urine voided. Normally, on initiation of urination, flow is slow. However, almost immediately, flow rate rapidly rises until bladder volume quickly decreases. Then the flow decreases rapidly. In patients with outlet obstruction, for example secondary to an enlarged prostate, the flow slowly rises to a level lower than normal. The flow plateaus for a longer time until the bladder volume decreases, and then flow diminishes slowly. The flow rates are highest and most predictable in the urine volume range of 200 to 400 mL. When the bladder contains more than 400 mL of urine, the efficiency of the bladder muscle is greatly decreased. Nomograms of maximal flow versus voided volume may be used for accurate test result interpretation, taking into account the patient's gender and age. If the flow rates are abnormally low, the test should be repeated to check for accuracy.
Modern urine flowmeters provide a permanent graphic recording. If flowmeters are not available, the patient can time the urinary stream with a stopwatch and record the voided volume; from this the average flow is calculated.
In some cases, it is more valuable to analyze several voided volumes and flow rates rather than a single flow rate. If this is to be done, the patient is taught to use a flowmeter. A graph of flow versus volume can be plotted. Together with clinical observation, this provides very valuable information on the severity of outflow obstruction, the likelihood of urinary retention, and the state of compensation or decompensation of the detrusor muscle.
This test is often performed in conjunction with cystometry (p. 688).
Procedure and Patient Care
Test Results and Clinical Significance
Dysfunctional voiding: Flow rates may be normal but intermittent or delayed.
Outflow tract obstruction: Flow rates will be diminished significantly, indicating obstruction caused by urethral stricture, prostatic cancer, or hypertrophy. The flow rate curve will plateau at a lower rate and stay there longer than normal.
Related Test
Cystometry (p. 688). This is a measurement of the pressures within the bladder during filling and micturition. Uroflowmetry may be a part of that study.