

Low-Fat, Low-Cholesterol Confusion
Sugar-laden muffins, nutritionally neutered toast, and insulin-exploding juice are touted as part of a balanced, nutritious breakfast because they are low in fat. We look at any new food and ask ourselves, “Is this low in fat?” If the answer is yes, we think it is healthy. Yet foods that contain fat are not necessarily unhealthy.
Most researchers today agree that our total intake of fat is not a risk factor for cardiovascular disease or cancer. But don’t low-fat diets help us lose weight? The Harvard School of Public Health strongly disagrees. “The low-fat, high-carbohydrate diet recommended by the . . . USDA Food Guide Pyramid may be among the worst eating strategies for someone who is overweight. . . . People on low-fat diets generally lose about two to four pounds after several weeks, but then gain that weight back even while continuing with the diet. Randomized trials of weight loss usually show little net weight changes after a year.”108
Foods containing fat do not make us fat, but we’ve been led to think so because a gram of fat contains more calories than a gram of carbohydrate or protein. Fat has 9 calories per gram while protein and carbohydrate have only 4. But as you’ve learned in earlier chapters, calories are not the primary issue—fat’s higher quantity of calories does not mean eating fat causes us to store body fat. That thinking is rooted in the calorie-counting theory, which we know is wrong. International cholesterol expert Uffe Ravnskov, MD, PhD, puts it well: “The idea that you become fat by eating fat is just as silly as to say that you become green by eating green vegetables.”109
According to the National Academy of Sciences, Harvard Medical School, Harvard School of Public Health, and dozens of other well-respected medical organizations, obesity itself is not associated with dietary fat in either national or international studies. No solid evidence proves that dietary fat or percentage of calories from fat causes weight gain. There is even evidence that lower fat intake correlates with higher obesity rates.
This evidence seems counterintuitive because we’ve been led to believe that eating whole-food fats encourages overeating. We’ve been misinformed.
Think back to Satiety. Water, fiber, and protein play the biggest role in the Satiety of food and Satiety determines how many calories we eat. Notice how there is no mention of fat there. Many water-, fiber-, and protein-packed foods contain fat. For example, seafood, meat, eggs, nuts, and seeds all contain a lot of fat. But when we focus on eating less fat, we replace these high-Satiety foods with low-Satiety but low-fat starches and sweets. Since low-Satiety foods require more calories to fill us up, this swap causes us to eat more—not fewer—calories. So, far from discouraging overeating, avoiding SANE foods that contain fat encourages overeating and hormonal clogging.
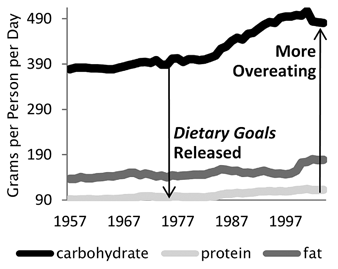
LESS NATURAL FOODS CONTAINING FAT, MORE OVEREATING
LESS NATURAL FOODS CONTAINING FAT, MORE BODY FAT
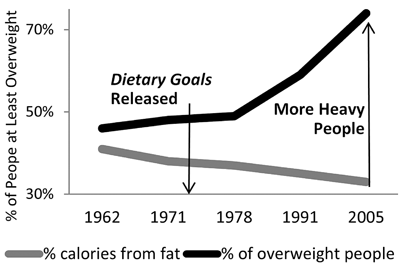
The last four decades of data tell the same story. We were told to avoid eating fat, so we reduced our relative intake of fat, increased our intake of starches and sweets, and were less satisfied. To deal with our increased hunger we increased our total inSANE caloric intake and ended up sicker and heavier—albeit only a tiny fraction heavier relative to what we should have gained thanks to our set-point—as a result.
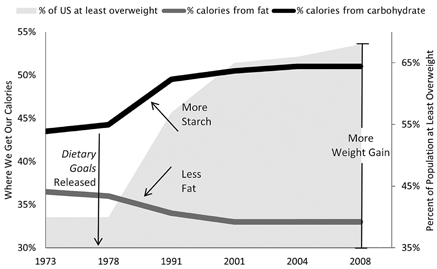
HOW WE EAT VERSUS OUR INCIDENCE OF WEIGHT GAIN
HOW WE EAT VERSUS OUR INCIDENCE OF DIABETES
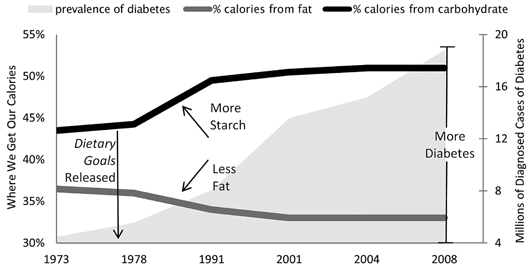
The government knows this too. The Centers for Disease Control and Prevention (CDC) reported, “During 1971–2000, a statistically significant increase in average energy intake occurred. . . . The increase in energy intake is attributable primarily to an increase in carbohydrate intake.”110 Even the authors of the government’s guidelines—with the US Department of Agriculture (USDA)—have gone on record stating that since the 1970s the major dietary trend has been a greatly increased consumption of carbohydrates. They found that starch consumption had increased by nearly sixty pounds per person per year and sweetener consumption had increased by nearly thirty pounds. That is ninety additional pounds of low-quality low-Satiety food—every year.
In the USDA’s Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (the document on which all government and related organizations base their nutrition practices), the government acknowledges: “Compared to higher fat intakes, low fat, high carbohydrate diets may modify the metabolic profile in ways that are considered to be unfavorable with respect to chronic diseases such as coronary heart disease (CHD) and diabetes. . . . This metabolic pattern has been associated with increased risk for CHD and type 2 diabetes. . . . In sedentary populations, such as that of the United States where overweight and obesity are common, high carbohydrate, low fat diets induce changes in lipoprotein and glucose/insulin metabolism in ways that could raise risk for chronic diseases.”111
So if low-fat/high-carb is linked to everything we’re trying to avoid, why is it being recommended to us?
New York University researchers remind us of the sad fact that “dietary guidelines necessarily are political compromises between what science tells us about nutrition and health and what is good for the food industry.”112
The emphasis on low fat leads away from eating SANE whole foods and misses an important point. Long-term health and fat loss do not result from diets low in fat, carbohydrate, or protein. Fat is not evil. Carbohydrates are not bad. And protein is not dangerous. The best way to burn body fat is to be balanced and SANE.
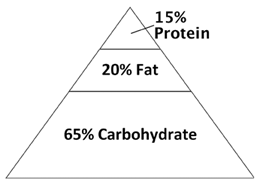
However, when you look at the government’s pyramid and plate, balance is nowhere to be found:
THE FOOD GUIDE PYRAMID/MYPYRAMID |
MYPLATE |
 |
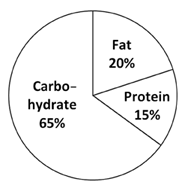 |
How are these balanced diets? They are high in carbohydrate and low in everything else. Consider the high-fat Atkins Diet. It is called “high-fat” because it advises individuals to get 65 percent of their calories from fat. Look at the USDA’s pyramid and plate diets that advise us to get 65 percent of our calories from carbohydrate. Doesn’t that make them high-carbohydrate diets? This could be why USA Today poked fun at the 72 percent of Americans who claimed to eat a balanced diet. The implication: “How could 70 percent of you be overweight if you ate a balanced diet?”113 We could easily be overweight if the “balanced” diet we are told to eat by the government is actually out of balance.
This imbalance exists in other guidelines as well. The American Heart Association Nutrition Committee refers to a diet consisting of 40 percent carbohydrate, 30 percent fat, and 30 percent protein as a “low-carbohydrate/very-high-protein diet.”114 Since when does 40:30:30 indicate that anything is very high?
What could be the reason for this confusion? The answer lies in another myth that has been proved false: eating foods that contain fat leads to unhealthy cholesterol levels. The fact is that eating the right kinds of whole-food fats is key to improving our cholesterol.
WHOLE-FOOD FAT HELPS CHOLESTEROL
As with other popular misconceptions about how our bodies work, confusion runs rampant about the word “cholesterol.” Ancel Keys played an important role in creating this problem. Along with his other claims, he needed a scientific-sounding explanation for how foods containing fat kill us. Looking at his data, Keys noticed that people eating more foods that contain fat generally had higher total cholesterol. While there was—and still is—no proof that high total cholesterol causes cardiovascular issues, Keys called it the cause of their heart problems.
Even while Keys was touting his new findings, the Federal Register (the official log of the federal government of the United States) was on record with the true scientific data at that time: “The role of cholesterol in heart disease has not been established. A causal relationship between blood cholesterol levels and these diseases has not been proved. The advisability of making extensive changes in the nature of the dietary fat intake of the people of this country has not been demonstrated.”115
Likewise, to this day, no studies have proven high total cholesterol causes heart disease. The American Journal of Medicine reported, “Total cholesterol per se is not a risk factor for coronary heart disease at all.”116 Researcher Uffe Ravnskov, MD, PhD, analyzed twenty-six randomized and controlled trials, which were designed to lower total cholesterol and, theoretically, the risk of heart disease and of death from heart disease. Ravnskov’s analysis divided people into two groups:
Treatment Group: People who ate less food that contains fat and/or took cholesterol-lowering drugs.
Control Group: People who did not eat less food that contains fat and did not take cholesterol-lowering drugs.
Across the studies, the total number of heart attack deaths was equal between the groups, and during the period of the trials more people died overall in the group who ate less fat and/or took cholesterol-lowering drugs.
Average Outcomes across the Twenty-Six Studies
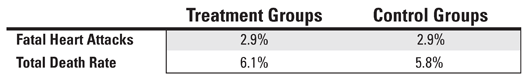
Ravnskov concluded: “Lowering serum cholesterol concentrations does not reduce mortality and is unlikely to prevent coronary heart disease.”117
To prove that our government’s dietary recommendations are helpful, three points must be proved:
1. Eating natural foods that contain fat leads to risky levels of cholesterol.
2. These levels of cholesterol cause heart disease.
3. The diet outlined by government’s guidelines improves these cholesterol levels.
None of these things have been proved.
Eating whole foods containing fat has never been proved to lead to risky levels of cholesterol. The effect of natural dietary fat on cholesterol has never been proved to cause heart disease. Studies have actually shown the opposite. The high-starch, low-fat, and low-protein diet promoted by the government’s guidelines has been proved to worsen the type of cholesterol (high-density lipoprotein, HDL) that decreases the risk of heart disease. For example, a 2009 study published in the New England Journal of Medicine went so far as to call HDL cholesterol “a biomarker for dietary carbohydrate.”118 In other words, the more “low-fat” carbohydrate we eat the lower our levels of the type of cholesterol that is crucial to heart health.
Here is where the confusion about cholesterol comes up: there are different types of cholesterol and most of them are helpful or neutral. The two most commonly discussed are LDL (low-density lipoprotein) and HDL. They are required to produce new cells and hormones. Because of this critical role, even if we never ate any cholesterol, our liver or intestines would produce it as our body works to keep us in balance. Much as unhealthy levels of body fat indicate a disorder in automatic energy balance and unhealthy levels of blood sugar indicate a disorder in automatic insulin balance, unhealthy levels of cholesterol indicate a disorder in automatic lipoprotein balance.
When it comes to predicting heart health, the American Heart Association, the International Diabetes Federation, and the World Health Organization agree that low HDL cholesterol—not high LDL cholesterol—is what matters. Looking at disease and death rates at various levels of LDL and HDL cholesterol, researchers have found that people with low HDL run a much greater risk of heart disease.
Relative Risk of Heart Disease119
(Total Cholesterol in Parenthesis)
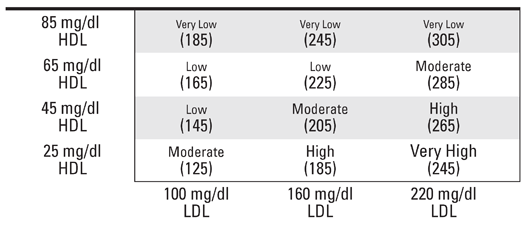
There are two things to note. First, total cholesterol is irrelevant. If people tell you their total cholesterol is 185, what is their risk of heart disease? Looking at the preceding table, it is either very low or high, depending on how much of that 185 consists of HDL cholesterol. Similarly, if people tell you their total cholesterol is 245, they either have a herculean heart or have a hemorrhaging heart, depending on their HDL levels.
Second, note how increasing HDL cholesterol is more important for heart health than decreasing LDL cholesterol. High HDL cholesterol protects us from heart problems more than dropping our LDL levels ever could. Heart-healthy diets are not about lowering total cholesterol. They are about raising HDL cholesterol.
The most effective way to raise our HDL levels through diet is to eat more whole-food fat and less starch. Whole-food fat raises HDL. Starch lowers HDL.
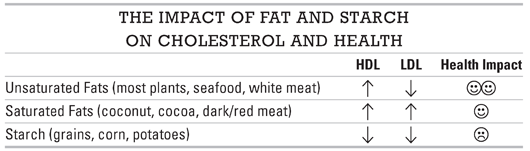
Since lower HDL does more harm than lower LDL does good, any diet that tells us to replace SANE sources of fat with inSANE starch worsens our cholesterol. That’s why many experts, from researchers at Harvard to scientists reporting in the Journal of the American Medical Association, believe our focus on eradicating fat (especially saturated fat) to try to reduce our LDL and total cholesterol may not just have failed to reduce heart disease risk—it may actually have increased it, along with decreasing our health, weakening our blood sugar control, and increasing the prevalence of insulin resistance and obesity.
Even saturated fats, about which so much has been said, are not cholesterol criminals. The American Heart Association found that no well-designed randomized controlled study in the general population has shown that lowering saturated fat intake significantly decreases our risk of coronary heart disease mortality.
Let’s also keep in mind the critical benefits of whole-food fats. Our bodies can’t make much use of vitamins A, D, E, K, and quite a few other helpful substances unless we eat fats. This is why your multivitamin instructs you to “take with a meal.” The manufacturers are hoping your pill will find some natural fats to help the vitamins get where they need to go. Dietary fat also plays a critical role in cell and hormone production as well as brain function. Certain saturated fats known as medium-chain triglycerides (such as those in coconuts) and polyunsaturated fats known as omega-3 fatty acids (such as those in fish, flaxseed, chia seeds, and grass-fed beef) are especially helpful for heart and brain health and have been shown to help us burn body fat. We should see these whole-food fats as health foods rather than the cause of arterial clogs.
Please disregard the performances on commercials and talk shows that demonstrate that saturated fats are solid at room temperature and tell you that this is why they get clogged in our arteries. By that logic spinach, broccoli, and all other vegetables also get clogged in our arteries, as they are also solid at room temperature.
We know the cause of clogs. They do not come from whole-food fats. They come from starches and sweets. The Journal of the American Medical Association summarized the science beautifully: “The proportion of total energy from fat appears largely unrelated to risk of cardiovascular disease, cancer, diabetes, or obesity. Saturated fat—targeted by nearly all nutrition-related professional organizations and governmental agencies—has little relation to heart disease within most prevailing dietary patterns.”120
What is the bottom line? The overwhelming evidence shows that any diet telling you to replace whole-food fats with starches is unhealthy and fattening.
Sadly, the government’s diet tells us to do exactly what science says we should avoid.
If you think this is troubling, wait until you see what happened when big business jumped onto the government bandwagon.