chapter 5: diet – repair your gut first
The first key principle when it comes to restoring good gut health is to focus on repairing it. The following is a straightforward programme, which can help to improve gut health and involves several phases. However, before you embark on this gut health-restoring programme, it can be helpful to keep a food and symptoms journal for seven days, so you can spot any specific foods that may be the cause of your symptoms. Furthermore, if you have an existing medical condition, I advise speaking to a medical practitioner before embarking on this programme.
Phase one – remove
This first phase generally lasts 2–4 weeks, depending on your symptoms. We want to focus on repairing, and the initial step in this phase is to remove any foods and chemicals that you think may be causing you digestive discomfort. This includes foods that disturb the gut microbiota and cause intestinal permeability, a.k.a. leaky gut. It also includes chemicals that harm the beneficial gut bacteria.
Foods that are a common cause of gut issues include dairy, eggs, gluten, soy, shellfish and coffee.
Therefore, in this phase, focus on removing the following foods from your diet:
As you will see, I have recommended the removal of legumes in this phase, since they can cause bloating. In addition, researchers have suggested that the lectins they contain can cause increased gut permeability, and possibly drive autoimmune diseases. However, you are able to re-introduce these after two weeks, and it is important to do so if you are vegan, as legumes are a great plant protein source.
LECTINS are a family of carbohydrate-binding proteins, which occur in nearly all foods, but the highest amounts are found in legumes.
I don’t recommend removing too many foods at once; instead, remove in stages, starting with the food that you suspect is the number-one culprit causing your symptoms.
I have suggested you may wish to remove coffee during this phase. Caffeine can be problematic for some people, as it is a stimulant and can promote the release of the stress hormones cortisol and adrenaline. However, research has shown that your genes have a major influence on your tolerance to it. Some people can consume significantly more than others without negative effects. If you feel jittery after consuming coffee, I would eliminating it during this phase.
This phase also involves removing chemicals, since they are harmful to the gut. These include dietary chemicals, such as artificial sweeteners, additives and preservatives, as well as the chemicals produced by our own bodies, such as excessive cortisol, a.k.a. the stress hormone. Chronic stress, which we will look at further in Chapter 10: how to manage stress effectively, has a significant and adverse impact on our gut health and immunity.
What can we eat in this initial phase?
How much protein do we need?
*However, protein requirements are increased for physically active individuals, as well as in older people, and those recovering from injuries.
During Phase 1, we need to focus on repairing the gut lining and ensuring adequate intake of nutrients, such as vitamins A and D, zinc, omega-3 fatty acids and antioxidants, which is also explored further in Chapter 7: eat to improve your immunity – the micros and phytonutrients. Ensure you get plenty of the following:
Vitamin A – found in sweet potatoes, butternut squash and pumpkin.
Vitamin D – found in wild salmon, sardines, herrings, egg yolks and mushrooms.
Zinc – found in shellfish, hemp seeds, pumpkin seeds, sesame seeds, nuts and eggs.
Antioxidants – found in red, purple, yellow, orange and green fruit and vegetables, and green and white tea.
Nutritional anti-inflammatories – such as omega-3 fatty acids (found in fatty fish, nuts and seeds) and curcumin (the main active ingredient in turmeric), which has powerful anti-inflammatory effects and is also a potent antioxidant.
Bone broth – an excellent restorative for the GI mucosa, it contains collagen and the amino acids glycine and glutamine, which are nutrients that can really help repair the gut lining.
You may feel better after two weeks on this phase, but you may wish to continue for up to four weeks.
Phase two – re-introduce
Once you have completed the initial 2–4-week phase, you can begin to re-introduce the foods you removed in Phase 1. Introduce each food one by one, over the course of three days. If symptoms reappear after you introduce a particular food, eliminate it, leave it a few days, then re-introduce a different food. Remember, you can re-introduce pulses at this point, which are rich in prebiotic fibre, but you must ensure you introduce them slowly.
When it comes to gluten, I suggest starting with sourdough bread, since the wild yeast and lactobacilli in the leaven neutralize the phytic acid, thereby making it a lot easier to digest. Then, introduce the ‘lower’ gluten grains, such as rye, and finally introduce wheat over three days.
With dairy, I would advise starting with live natural yoghurt, cheese, butter and then milk (in that order).
During this phase, you can re-introduce alcohol in moderation. I recommend opting for red wine, as it is loaded with antioxidants, and enjoying a glass with your dinner. The powerful plant compounds in red wine have been associated with numerous health benefits, including reduced inflammation, decreased risk of heart disease and cancer, and even longevity. Furthermore, red wine has been demonstrated to increase the abundance of beneficial gut bacteria, while reducing the number of harmful gut bacteria. This indicates the potentially beneficial prebiotic effects associated with red wine polyphenols45.
Prebiotics and probiotics
At this stage, I recommend you increase your intake of pre- and probiotic foods.
Prebiotics
A prebiotic is a type of dietary fibre that feeds your ‘good’ gut bacteria. Many people think prebiotics and fibre are the same thing, but they’re not! To be classed as a prebiotic, the fibre must:
In addition, prebiotic fibre helps our bacteria make certain nutrients, such as butyrate, for the cells in the large intestine. This then promotes a healthier and balanced gastrointestinal tract.
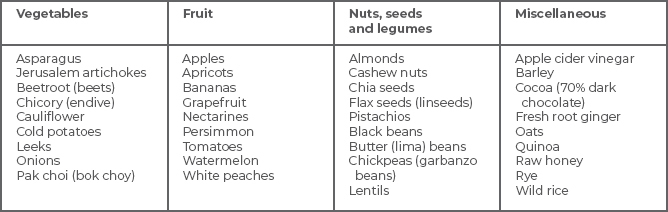
As you will see in Part 3, lots of the prebiotic-rich foods that I highlight in the table over the page feature frequently in the recipes.
Seeds such as flax (linseeds), hemp seeds and chia seeds, which have been sprouted, are also excellent sources of fibre and help ‘feed’ the good bacteria. However, if you have a weakened and damaged gut, you may wish to get your fibre from steamed vegetables and fruit initially. Then, you can introduce sprouted seeds when your gut is feeling stronger.
Probiotics
These are the live bacteria found in certain foods or supplements that can provide numerous health benefits, including promoting digestive health and supporting our immunity. During this phase and going forward, focus on including fermented foods, which contain probiotic bacteria, such as live yoghurt, sauerkraut, kimchi and kefir.
I get asked a lot if it is worth supplementing with probiotics. The main issue when it to comes to probiotics is that research is still in its infancy, and we don’t know as yet which exact strains should be taken and if they are helpful for all individuals. If you are very young, old or very ill, there is a growing body of research that suggests they are beneficial47. However, if this doesn’t apply to you, I would recommend concentrating on promoting your beneficial gut bacteria by consuming a diverse, fibre-rich diet.
Glutamine
This is the most abundant amino acid (building block of protein) in the body, and it plays a vital role in gut health. It encourages immune-cell activity in the gut, helps prevent infection and inflammation, and heals the gut lining. The best food sources of glutamine include beetroot (beets), cabbage, spinach, tofu, lentils, beans, bone broth, chicken and fish.
Digestive Aids
You may find that you need to replace naturally occurring digestive aids, including enzymes, hydrochloric acid and bile acids that support proper digestion. These can be taken in supplement form before eating a meal, but I would suggest seeking advice from a nutritionist or dietician if you suspect you may need them. They can advise you further and ensure you are taking the appropriate digestive aid.