CHAPTER 8 NEUROHUMORAL PHYSIOLOGY AND PSYCHONEUROIMMUNOLOGY
NEUROHUMORAL MECHANISMS
The autonomic nervous system (ANS) maintains homeostasis by a series of humoral and nervous system interactions that continually occur on a subconscious, involuntary level. The ANS sends nervous impulses to all parts of the body as directed by the integration of several complex biofeedback mechanisms.
The information from these biofeedback loops is integrated in the central nervous system (CNS), and appropriate neural directives are passed along to the organs of respiration, circulation, digestion, excretion, and reproduction via the ANS.
Thus the body is maintained in a state of dynamic equilibrium, continually responsive to stimuli from internally monitored systems and environmental influences.
The functional anatomy of the ANS has important implications for therapeutics (Table 8-1). The division of the system into two major parts—sympathetic and parasympathetic—provides a series of checks and balances to regulate body functions. This division enables an ongoing dialogue between the two parts to maintain dynamic equilibrium. The opposition of two vital forces may be likened to the Asian concept of the yin and the yang, in which the interaction of these opposing forces maintains the balance and harmony of humans and the universe (see Chapters 1 and 2). Accordingly, each of the two forces may take on some characteristics of the other. An analogy lies in the sympathetic and parasympathetic divisions of the nervous system, which are antagonistic, with a few notable exceptions. Coronary and pulmonary blood vessels are dilated by both divisions of the ANS, whereas the vessels supplying blood to skeletal muscles may be dilated by the sympathetic system in exercise or by the postganglionic parasympathetic neurotransmitter at rest.
TABLE 8-1 Sympathetic and Parasympathetic Divisions of the Autonomic Nervous System
| Sympathetic | Parasympathetic | |
|---|---|---|
| Synonym | Adrenergic | Cholinergic |
| Preganglionic fiber | Short | Long |
| Neurohumoral agent* | Acetylcholine | Acetylcholine |
| Ganglion location | Paravertebral | End organ |
| Postganglionic fiber | Long | Short |
| Neurohumoral agent* | Norepinephrine | Acetylcholine |
| Extraautonomic sites | Adrenal medulla | Neuromuscular junction |
| Evolutionary role | Fight-flight/defense-alarm | Relaxation response, vegetative functions |
| Activators | Multiple | Specific |
| Blockers | Diffuse, nonspecific | Selective, cholinesterase |
| Degradative enzymes | Monoamine oxidase, methyltransferase |
* These compounds are referred to as neurohumoral agents because they are present both in the general circulation and within nervous tissue. They are neurotransmitters because they manifest their activity across presynaptic or postsynaptic junctions during transmission of nerve impulses.
The unique short-term and long-term adaptability of the human organism to environmental stimuli is facilitated by the actions of the ANS. The so-called fight-flight or defense-alarm responses are promulgated by the sympathetic nervous system, which raises blood oxygenation and pressure, regulates blood flow to the musculoskeletal system for activity and to the skin for thermal regulation, and causes retention of fluids and electrolytes in a state of arousal. These acute physiological responses are adaptive in the short term and allow long-term survival of the human organism.
The “relaxation response” is mediated by the dynamic opponent of the sympathetic system—the parasympathetic system. The parasympathetic nervous system directs the normative functions of the organism, allowing development of an ongoing state of well-being and physiological equilibrium. The maintenance of vegetative functions has facilitated human development and cultural evolution. The ability to relax has allowed humans to reserve some portion of physical and mental energy for the pursuit of activities peripheral to primary survival. This ability has given humans their unique cultural attributes, which enable each individual to express the inclination for creativity. The selective responsiveness of the ANS has enabled humans, both as individuals and as a species, to make the successful adaptation to the environment that has characterized human evolution.
The anatomical divisions corresponding to the functional autonomy of the sympathetic and parasympathetic nervous system can be traced along the length of the brain and spinal column (Figure 8-1). The ANS begins with cranial nerve X, the vagus, a single bundle of parasympathetic nerves that originates from the brainstem and courses throughout the body. Cranial nerves III, VII, and IX also send some parasympathetic fibers to the eyes, nose, and salivary glands. Vagus means “wanderer” in Latin, and no other nerve interfaces at so many diverse points along the functional anatomy. Passing down along the spinal cord, the cervical, thoracic, and lumbar divisions send sympathetic nerves throughout the body. Finally, the sacral divisions of the spinal cord send a few parasympathetic nerves to the lower regions of the body.
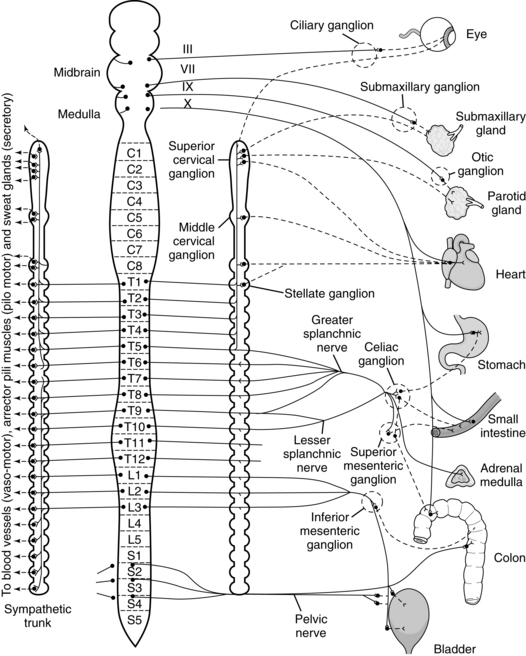
Figure 8-1 Autonomic nervous system and cranial nerves.
(From Williams PL: Gray’s anatomy, Edinburgh, 1995, Churchill Livingstone.)
Each nerve of the ANS has two longitudinal divisions as it passes from the CNS to the end organs. The initial, or preganglionic, nerve fiber originates in the CNS and terminates in a nerve ganglion. Here it synapses with a new continuation—the postganglionic nerve fiber. This postganglionic fiber originates in the ganglion and terminates at a site of action. Autonomic nerve impulses travel in a continuum along the preganglionic fiber, through the synapse, and onto the postganglionic fiber to the site of action. In the sympathetic division, the preganglionic fibers are short and end in nearby ganglia, which occur in chains along the thoracic and lumbar vertebrae. From there, the postganglionic fibers travel to the diverse sites of action. In the parasympathetic system the preganglionic fibers are long and travel into ganglia located near end organs. From there, postganglionic fibers traverse a short distance to the sites of action.
The occurrence of synapses in the ganglia, between the preganglionic and postganglionic fibers, is important to therapy. Local anesthetics affect nerve conduction in the nerve fiber. Otherwise, these nerve impulses may be influenced by activities at the synaptic junction site. The interactions that occur in the synapse are a microcosm of neurophysiology and serve to distinguish the sympathetic system functionally from the parasympathetic system. These distinctions are used extensively in therapy. Each of these systems makes use of characteristic neurohumoral agents for the unique transmission of nervous impulses throughout the body. The preganglionic fibers of both divisions use acetylcholine as the neurotransmitter across the synapse. The postganglionic parasympathetic transmitter is also acetylcholine, but the sympathetic transmitter is norepinephrine. The exclusive postganglionic use of acetylcholine as the parasympathetic and norepinephrine as the sympathetic neurotransmitter holds throughout the ANS, except in the case of sweating of the palms, soles, and axilla, where the autonomic innervation is adrenergic, but the neurotransmitter is acetylcholine. Because these neurohumoral compounds used in the transmission of impulses across the synaptic junction are distinct chemical entities, they tend to accumulate at their sites of release. Such an occurrence would limit effectiveness of the ANS in providing sensitive, instantaneous regulation of body systems. Thus the synaptic sites maintain extensive and sophisticated mechanisms for the reuptake and degradation of released neurohumoral transmitters, and the synaptic junctions are kept clear of accumulated active compounds on an ongoing basis.
Specific enzymes degrade norepinephrine in the sympathetic postganglionic synapses, as well as their metabolic products. The concentration of these metabolites may be increased in certain pathological conditions and detected by analytical chemical techniques.
The enzyme responsible for the breakdown of acetylcholine in the postganglionic parasympathetic synapse is acetylcholinesterase. Although acetylcholine itself cannot practically be administered even when its properties are desired, a “functional dose” may be given through inhibition of its breakdown by cholinesterase. Thus, anticholinesterases form the basis for parasympathetic nervous stimulation in clinical therapeutics. A phenomenon known as denervation hypersensitivity greatly depends on this system of reuptake and degradation. When the autonomic innervation to an organ is anatomically interrupted (denervation), the postganglionic synaptic site loses its induced degradative enzymes, and the synaptic receptor becomes extremely sensitive (hypersensitive) to the neurohumoral agent. Thus any amount of the original neurohumoral agent introduced into the site by the circulation, through administration or otherwise, will have a magnified effect because the activity will not be mitigated by action of its appropriate degradative mechanism.
The functional divisions of the ANS have great pathophysiological and therapeutic significance. For example, the entire gastrointestinal (GI) tract is extensively innervated by nerve fibers from both the sympathetic and the parasympathetic divisions. As previously discussed, the parasympathetic ganglia, where preganglionic fibers synapse with postganglionic fibers, are located near the sites of action in end organs. In the case of the GI tract, the parasympathetic ganglia lie in two areas of the esophageal, gastric, intestinal, and colonic walls: the Auerbach myenteric plexus and Meissner submucous plexus. These ganglia may be congenitally absent, as in Hirschsprung disease, or destroyed by a number of pathogenic agents. The resultant disease depends on the location of the deficiency or insult along the GI tract.
With destruction of the parasympathetic ganglia, there is prolonged, unopposed sympathetic stimulation. The characteristic effect is for the diseased segment to become constricted, with impaired motility and loss of peristaltic action. The segment of the GI tract proximal to the constriction lesion becomes extensively dilated as a pathological response to the event.
Achalasia of the esophagus is such a condition, in which a local area of constriction leads to proximal dilation of the esophagus. It has been thought that achalasia is caused by degenerative disease of the parasympathetic vagus nerve, which innervates this area.
Pyloric stenosis of the gastric outlet is a similar condition. A ganglionic megacolon, or Hirschsprung disease, is caused by a congenital lack of parasympathetic ganglion cells in the intestinal tract.
Chagas disease, or South American trypanosomiasis, caused by the parasitic organism Trypanosoma cruzi, may be associated with both megaesophagus and megacolon resulting from the toxic degeneration of the intraluminal nerve plexus through T. cruzi infection. On the other hand, selective loss of sympathetic activity occurs in Horner syndrome, with the characteristic triad of ptosis, miosis, and anhydrosis (lid lag, pupillary constriction, and loss of sweating). Horner syndrome occurs with injury to the cervical sympathetic trunk and unopposed parasympathetic innervation.
Unfortunately, no autonomic therapeutic agents are available for the effective treatment of disorders such as Horner syndrome or irreversible disorders of the GI tract. However, autonomic agents to treat diseases of the circulatory and respiratory systems are common therapies in medicine. These same neurohumoral mechanisms involved in medical therapeutics may also be used in a nonspecific manner by many of the “mind-body” techniques of complementary, integrative, and alternative medicine.
PSYCHONEUROIMMUNOLOGY
The Romans’ view of mens sanum in corpore sano, “a sound mind in a sound body,” as well as the Greek physician Galen’s observation that women suffering from depression had a predisposition toward developing breast cancer, reflected the early recognition of mind-body interactions and their significance in health and disease. Understanding the connection and functioning of the mind has been the subject of discussions from the ancient era and transcended the Renaissance and modern times. This is witnessed by the philosophical writings of Pythagoras that “the brain served as the organ of the mind and the temple of the soul,” and Anaximander, another Greek philosopher, that “mind gives body a life force” (Cassano, 1996). The European Renaissance was marked by the work of Leonardo da Vinci and Michelangelo. Da Vinci was mostly interested in answering the question of how the brain processes sensory inputs; Michelangelo, an expert in anatomy, painted detailed structures of the human brain (Meshberger, 1990). René Descartes, a post-Renaissance philosopher, declared the connection between the body and the soul to be located in the pineal gland (Lokhorst et al, 2001). The development of electrochemistry in the eighteenth and nineteenth centuries led to the identification of different gases and their role in maintaining life through respiration, which also made the lungs the new indispensable organ to be seriously considered. It is basically what Hippocrates and Avicenna called the “air element” that distributes the spirits inside the body (Tercier, 2005). The importance of breathing started then to occupy the discussion about what animates living beings. The twentieth century was marked by remarkable technological developments, especially imaging, in which the functional brain is visualized and its metabolites measured.
Thus, it was not until studies in the 1950s and 1960s verified the impact of stress on overall health that mind-body connection research started to become a focus of attention. In 1964, Solomon and Moos described the interaction between mind and body as a result of stress exposure. The early work of Rasmussen et al showed (1957) that animals exposed to stress had increased susceptibility to infection. George Engel’s view that genetics is not the only cause of poor health and that social and psychological factors have a direct impact on all biological processes further expanded this new, holistic medical model referred to as “psychoneuroimmunology,” or PNI (Engel, 1977; Lutgendorf et al, 2003). Subsequent research strongly suggested that the higher cognitive and limbic emotional centers are capable of regulating virtually all aspects of the immune system and therefore play a significant role in health and disease (Ader R et al, 1991; Blalock, 1994; Reichlin, 1993). The pioneering work of Besedovsky et al (1975) revealed the role of hormones and cytokines in modulating the brain and immune functions (Besedovsky et al, 1975). The Institute of Medicine issued two reports titled Health and Behavior (1982, 2001) with a special focus on understanding the role and interactions of the biological, behavioral, and social factors in health and disease.
Autonomic and neuroendocrine processes constitute the mind-body pathways of communication. The ANS innervates the bone marrow, thymus, spleen, and mucosal surfaces, the areas where immune cells develop, mature, and encounter foreign proteins (Felten et al, 1992). This innervation involves sympathetic, parasympathetic, and nonadrenergic noncholinergic fibers. As discussed earlier, signal transduction occurs through epinephrine, norepinephrine, acetylcholine, and neuropeptides. These chemical messengers exert tissue-specific inflammatory or antiinflammatory effects on immune target tissues, and nerves and inflammatory cells mutually influence each other in a time-dependent manner (Watkins, 1995). Development and aging of the immune system and ANS appear to be closely related (Ackerman et al, 1989; Bellinger et al, 1988). Levels of natural killer (NK) cells, considered the first line of immune defense against viral infections, were found dramatically reduced in individuals exposed to chronic life stress as well as in those with major depression. The levels of NK cells were found to return to normal levels after the depression episodes subsided (Irwin and Miller, 2007). Studying 245 patients who had depression and were stratified by smoking habits, Jung and Irwin (1999) found that the combination of depression and smoking caused a more pronounced decline in levels of NK cells than depression or smoking alone. Several studies published in the past 25 years have clearly showed that behavior affects immunity and have deciphered neuroimmune pathways governing the observed effects. The neuroimmune system also affects behavior, functioning as a bidirectional highway of communications involving neuropeptides and cytokines. It has been hypothesized that altered cytokine profiles, including levels of interleukin-1 (IL-1), IL-6, and tumor necrosis factor, might contribute to symptoms of depression, such as insomnia and fatigue (Irwin and Miller, 2007).
The neuroendocrine pathway constitutes the second indirect communication channel involving the hormonal regulation of immune cell function. Immune cells have surface receptors for endorphins, enkephalins, and the various hormones, such as growth hormone, thyroid-stimulating hormone, sex hormone–releasing hormones, vasopressin, and prolactin (Blalock, 1994; Felten et al, 1992). The release of many of these hormones is intimately related to thoughts and emotions and has a profound effect on immune system function. The “molecules of emotion” therefore govern the immune response through the endocrine system, leading to either suppression or enhancement (Pert et al, 1998). The neuroendocrine peptide corticotropin-releasing hormone (CRH) received a special attention, especially after it was found that depressed patients had elevated central CRH levels as measured in the cerebrospinal fluid. Furthermore, acute administration of CRH centrally caused dramatic reduction in innate and cellular immune responses in animal models (Irwin et al, 1987, 1989; Strausbaugh et al, 1992). These studies showed that the central action of this neuropeptide could affect the peripheral immune response. CRH is considered as the major neuroimmunoendocrine integrator.
Because thoughts, feelings, emotions, and perceptions alter immunity (Watkins, 1995), complementary therapies targeted at these areas should affect health and elicit changes in pathological conditions (Watkins, 1994).
Epilepsy illustrates this point (i.e., the effect of the mind on the brain). Epileptic seizures can be triggered by stressful events (Fenwick, 1998), and negative emotions exacerbate the condition. A potential mechanism is the activation of the cytokine network (Hulkkonen et al, 2004), which corresponds to seizure activity, but whether it is cause or effect remains unclear.
The reverse scenario is reflected in a long-term study involving healthy World War II veterans who were asked to write about their war experiences and themselves. The essays were rated on a scale ranging from extreme optimism to extreme pessimism. When the study participants reached the age of 45, health status positively correlated with optimistic scoring at the beginning of the study (Peterson et al, 1993). Recently, a new approach using multiplex immunoassay was applied to assess the relationship of 11 T-cell cytokines and chemokines to behavior. Mommersteeg et al investigated whether cytokine and chemokine profiles correlated to hostility in 304 healthy Dutch military males before deployment. In addition to finding that hostility was related to various clusters of proinflammatory and antiinflammatory cytokines and chemokines and to potential risk factors including age, body mass index, smoking, drinking, previous deployment, early life trauma, and depression, the authors found that “hostility was significantly related to decreased interleukin 6/chemokine secretion and increased pro- and antiinflammatory cytokines” (Mommersteeg et al, 2008).
Evidence for Psychoneuroimmunological Mediation of the Effects of Complementary and Alternative Therapies
The use of PNI-related techniques has dramatically increased in the United States. According to a recent survey, one in five adults reported using one or more mind-body therapies during the previous year (Wolsko et al, 2004). Relaxation techniques, guided imagery, hypnosis, and biofeedback are the most frequently used modalities. Patients sought these PNI-related techniques for treatment of chronic diseases such as anxiety (34%), depression (26.5%), headaches (18.5%), back or neck pain (18%), heart problems or chest pain (18%), arthritis (14.8%), digestive disorders (12.4%), and fatigue (12.1%). The authors estimated that the absolute numbers of patients using the modalities listed were as follows: for back and neck pain, 11.2 million; for anxiety, 6.3 million; and for fatigue, 6.8 million. Between 29% and 55% of patients found these therapies “very helpful” for their respective health condition. A recent study on the prevalence of complementary and alternative medicine (CAM) use in the military population showed that 37% of the 1305 individuals in a random sample of active duty and Reserve and National Guard members contacted between December 2000 and July 2002 had used at least one CAM modality in the previous year (Smith et al, 2007).
What is the evidence that complementary, integrative, and alternative therapies work through the previously outlined mind-body pathways? To date, few studies have actually investigated the mechanism of action of these therapies. Some data suggest that the activity of the ANS may be altered by chiropractic intervention (Beal, 1985; Bouhuys, 1963), hypnosis (DeBenedittis et al, 1994; Neild et al, 1985), conditioning (Hatch et al, 1990), and acupuncture (Han et al, 1980; Jian, 1985). Other studies have indicated that the benefit derived from acupuncture (Kasahara et al, 1992) and spinal manipulation (Vernon et al, 1986) might be mediated through endorphin release.
Several studies demonstrate that acupuncture-induced analgesia is blocked by naloxone, an opioid antagonist, which indicates that an opioidergic mechanism mediates the acupuncture analgesic response (Mayer et al, 1977; Sjolund et al, 1979). In electroacupuncture, electrical pulses are applied via acupuncture needles. Opioid and nonopioid pathways govern the antinociceptive effect induced by electroacupuncture. However, the PNI-mediated mechanism in electroacupuncture occurs at the level of neuronal nitric oxide synthase, nitric oxide expression and synthesis in the brain, and the therapeutic response induced by acupoint ST36 (Ma, 2004).
Recently, a new hypothesis on the mechanism of acupuncture involving neutrophins and cytokines has been postulated (Kavoussi et al, 2007). The beneficial effects of acupuncture on inflammatory pain, as well as neurodegenerative and psychiatric diseases, could indeed be mediated by nerve growth factor, brain-derived neurotrophic factor, neurotrophin 3, or neurotrophin 4/5, as well as by IL-1, IL-2, IL-6, tumor necrosis factor α, and transforming growth factor β. The dynamic crosstalk between the central and peripheral nervous systems could shed light on the mechanism of acupuncture (Du, 2008).
Acupuncture has also been used to relieve stress and anxiety, which are known to affect the immune response. In a study investigating the effects of acupuncture in women with anxiety, Arranz et al tested several immune functions: adherence, chemotaxis, phagocytosis, basal and stimulated superoxide anion levels, lymphocyte proliferation in response to phytohemagglutinin A, and NK activity of leukocytes (neutrophils and lymphocytes). Ten 30-minute sessions of manual acupuncture using 19 acupoints were administered to 34 women aged 34 to 60 with anxiety, as assessed by the Beck Anxiety Inventory, and 20 healthy controls. The investigators found that the most positive effects of acupuncture on the immune parameters appear 72 hours after a single session and persist for 1 month after the full treatment regimen. The abnormal immune profiles of women with anxiety were normalized and the immune functions significantly enhanced by acupuncture (Arranz et al, 2007).
Using state-of-the-art technology (e.g., two-dimensional electrophoresis-based proteomics) and an animal model for neuropathic pain, Sung et al (2004) detected 36 proteins that were differentially expressed in the brains of injured animals compared with controls. Most interestingly, normal levels of these proteins were restored after the injured animals were treated with electroacupuncture. Of these proteins, 21 have been characterized as playing a role in inflammation, enzyme metabolism, and signal transduction, and this study undoubtedly will elucidate other pathways triggered by acupuncture (Sung et al, 2004).
A growing body of evidence suggests that meditation alleviates anxiety, fosters a positive attitude, and improves the immune response. A meditation training program known as “mindfulness-based stress reduction” (MBSR), developed by Jon Kabat-Zinn, PhD, in the late 1970s, yielded increased left frontal lobe activation in response to both negative and positive emotion induction. When vaccinated after intervention, the meditation group experienced a significantly increased rise in antibody titers. The correlation between the shift toward left-sided brain activation and the elevated immune response demonstrates the relationship between the PNI system and meditation (Davidson et al, 2003). Similarly, cancer outpatients using the same MBSR technique experienced improved mood, which correlated with a more favorable hormone profile with regard to melatonin, cortisol, dehydroepiandrosterone sulfate (DHEA-S), and the cortisol/DHEA-S ratio, as well as an enhanced immune response (Carlson et al, 2004).
The quasi-experimental study carried out by Robinson et al (2003) using an 8-week structured MBSR intervention in patients with human immunodeficiency virus (HIV) infection showed that NK cell activity and number increased significantly in the MBSR group compared with the controls. In a more recent single-blind randomized controlled trial, Creswell et al assessed the efficacy of an 8-week MBSR meditation program compared with a 1-day control seminar on CD4+ T-lymphocyte counts in stressed HIV-infected adults. Participants in the 1-day control seminar had reduced CD4+ T-lymphocyte counts, whereas counts among participants in the 8-week MBSR program were unchanged from baseline to postintervention. Another study also found an indication that mindfulness meditation training can buffer CD4+ T lymphocyte declines in adults infected with HIV-1 (Creswell et al, 2009).
Beneficial effects of MBSR have also been reported among cancer patients. Quality-of-life, mood, endocrine, immune, and autonomic parameters have been assessed in patients with early-stage breast and prostate cancer enrolled in an MBSR program. In this study the authors carried out preintervention and postintervention as well as 6- and 12-month follow-up measurements of the psychobehavioral and physiological parameters. They found significant general improvements in stress symptoms, which were preserved through the follow-up periods. In addition to a steady decrease in salivary cortisol level throughout the follow-up period, improvements in immune patterns were also maintained as shown by a decrease in the proinflammatory T helper cell type 1 cytokines. Reductions in heart rate and systolic blood pressure were positively correlated with improvements in self-reported stress symptoms. This pilot study data clearly showed the longer-term effects of MBSR on a range of potentially important psychoimmunophysiological biomarkers (Carlson et al, 2007). Another study enrolled women who had been recently diagnosed with early-stage breast cancer and were not currently receiving chemotherapy into an MBSR program. Compared with the levels before MBSR intervention, postintervention and 4-week follow-up assessments in the MBSR group showed an increase in peripheral blood mononuclear NK cell activity and cytokine production accompanied by a decrease in IL-4, IL-6, and IL-10 production, whereas the non-MBSR control group showed reduced NK cell activity and interferon-γ levels and increased IL-4, IL-6, and IL-10 production. Furthermore, the MBSR-intervention group demonstrated reduced cortisol levels, improved quality of life, and improved coping effectiveness (Witek-Janusek et al, 2008).
Among the other mind-body programs is the one developed by Herbert Benson, MD, in the 1970s, in which he emphasized the relaxation response. A large body of evidence has been developed showing its beneficial effects on a wide array of diseases and disorders, and it is only recently that a special interest in its mechanism(s) of action has been developed. Building upon newly developed hypotheses that nitric oxide plays a role in the immune response and in stress-related diseases (Tripathi, 2007), an association between oxygen consumption, through breathing exercises, and nitric oxide production has been elucidated (Dusek et al, 2006). Furthermore, the new technological approaches of high-throughput genomic analyses have been applied to mechanistic investigations of the relaxation response. Thus, genomic counterstress alterations induced by the relaxation response have been detected using whole blood transcriptional profiles. Genomic profiles were compared in 19 long-term practitioners of relaxation, 20 novice individuals who completed an 8-week relaxation program, and 19 healthy controls. Over 2200 genes in the long-term practitioners and 1561 genes in the novice group were differentially expressed compared with the control group. Among these genes, the long-term practitioners and novices shared 433 genes. The gene analysis revealed changes in gene expression related to cellular metabolism, oxidative phosphorylation, and production of reactive oxygen species and regulation of oxidative stress, especially among the relaxation response practitioners (Dusek et al, 2008).
T’ai chi is a Chinese martial art that emphasizes meditative aerobic activity and relaxation. Its practice in the West is witnessing a great development. Several studies using t’ai chi as intervention in subjects who either had their immune response clinically challenged or had immune-related diseases have recently been published. In a prospective randomized controlled trial 112 healthy adults were vaccinated with Varivax (attenuated varicella-zoster virus) and divided to either t’ai chi or health education groups. The t’ai chi group showed a significant improvement in scores on the Short-Form Health Survey (SF-36); in addition, the cell-mediated immune response to the vaccine not only was higher but also increased at a higher rate than in the control group (Irwin, Olmstead et al, 2007).
Another randomized clinical trial tested whether t’ai chi could improve immune function and psychosocial functioning in 252 HIV-affected individuals compared with a wait-listed control group. Although only modest effects were observed on the psychosocial test results, a significant increase in the lymphocyte proliferation function was found. The investigators concluded that t’ai chi could be considered as an effective alternative intervention in patients with immune-mediated diseases (McCain et al, 2008).
Yoga has become a popular practice in Western culture. Based on the development and balance of psychophysical energies, yoga has proven to be beneficial in pulmonary and cardiovascular conditions, including asthma, chronic bronchitis, and hypertension (Raub, 2002). A study investigating the effects of yoga and meditation on psychological profile, cardiopulmonary performance, and melatonin secretion demonstrated increased well-being, improved performance, and elevated plasma melatonin levels (Harinath et al, 2004).
Yoga has been administered as adjuvant therapy in treatment of other health conditions, in addition to the afore-mentioned disorders. Premenstrual syndrome, or PMS, is considered to be a stress-related psychoneuroendocrine disorder for which the numerous available treatments have not brought satisfactory relief. Fifty healthy women of reproductive age were assigned either to a Hatha Yoga group performing a 61-points relaxation exercise or to a no-intervention control group. Several physiological parameters were measured: heart rate, systolic and diastolic blood pressure, electromyographic activity, electrodermal galvanic activity, respiratory rate, and peripheral temperature. After 10 minutes of Hatha Yoga practice, values of all parameters declined significantly except that temperature increased, which suggests a reduction in sympathetic activity and basal sympathetic tone. Thus, Hatha Yoga could be used as an adjuvant to other medical treatment in alleviating PMS symptoms (Dvivedi et al, 2008).
Psychological outcomes, perceived stress, anxiety, and depression levels as well as radiation-induced DNA damage were assessed in 68 breast cancer patients undergoing radiotherapy and enrolled in an integrated yoga program. The psychological outcomes were significantly improved in the yoga group, but only a slight decrease in DNA damage was seen compared with the no-intervention group (Banerjee et al, 2007).
In another study, 98 outpatients with stage II or III breast cancer were assigned to either yoga or supportive therapy. Data were analyzed only for those who underwent surgery followed by radiotherapy and chemotherapy (n = 38). Subjects were assessed using the State Trait Anxiety Inventory (STAI) before and after 60 minutes of daily yoga sessions. Results showed a general decrease in self-reported STAI scores in the yoga group and a positive correlation of these scores with distress during conventional treatment intervals (Rao et al, 2009).
Looking into the neuroendocrine mechanisms underlying the effect of yoga, Madanmohan et al (2002) approached the question of whether shavasan yoga modulates the stress physiological response from a different angle (yes, the pose is indeed from a different angle). They used the cold pressor test (CPT) to trigger a stress response in 10 healthy subjects who were taught shavasan practice and measured the respiratory rate interval variation, deep breathing difference, and heart rate, blood pressure, and rate-pressure-product response to CPT before and immediately after shavasan. A significant increase in deep breathing difference and a close to significant increase in respiratory rate interval variation were observed, which indicate improved parasympathetic activity. Values of the other parameters mirroring sympathetic activity were blunted, which suggests that yoga practice helps reduce the sympathetic load on the heart (Madanmohan et al, 2002).
Biochemical and genomic approaches have also been undertaken to understand the action mechanisms underlying the stress reduction effects of Sudarshan Kriya Yoga. Whole blood drawn from 42 healthy subjects was used to measure glutathione peroxidase levels, and red blood cell lysate was used for superoxide dismutase activity assay as well as to estimate glutathione levels. White blood cells were separated and processed for gene expression. The results showed a better immune status and antioxidant profile both at the enzyme activity and at the RNA level in the yoga intervention group. A prolonged lymphocyte life span supported by the upregulation of antiapoptotic and survival genes was also observed. All together, these results suggest that Sudarshan Kriya has beneficial effects on immunity, cell death, and stress regulation through transcriptional pathways (Sharma et al, 2008).
Placebo Effect
A placebo is an inert substance or a control method used to evaluate the psychological and physiological effects of a new drug or procedure. The response to the placebo should not exceed that to the experimental drug or method, which would otherwise be considered ineffective. The placebo response is unpredictable, unreliable, and mediated by nonspecific mechanisms that are dismissed as immeasurable and irrelevant.
How does the psychoneuroimmunological complex relate to the placebo effect? It has been argued that every therapeutic intervention—whether complementary, integrative, and alternative medicine or allopathic medicine—involves a placebo effect. Most allopathic physicians consider it unethical or even deceitful to actively encourage a placebo response. However, in a recent survey of 1200 practicing internists and rheumatologists in the United States that inquired about behaviors and attitudes regarding the use of placebo treatments, among those who responded (n = 679), half reported prescribing placebo treatments on a regular basis in the form of saline, sugar pills, over-the-counter analgesics, and vitamins within the previous year. Most physicians describe these substances to their patients as potentially beneficial or as a treatment not typically used for the patient’s condition, and most physicians believe this practice to be common and ethically allowable (de la Rochefordiere et al, 1996).
PNI research demonstrates that an expectation of recovery can alter subjective feelings of well-being and result in ANS activation and pituitary hormone production. Thus, specific verifiable pathways have been identified by which expectation can alter immunity. However, expectation likely has different effects in different individuals, producing large shifts in autonomic balance and hormonal output in some and negligible changes in others, which explains the unpredictability of the placebo response. Together with the idea that complementary therapies affect merely “subjective” measures of disease activity, these observations have formed the platform on which allopathic physicians argue that complementary practices are fundamentally flawed and of limited benefit.
Although fallacious, defeatist, and ultimately counterproductive, these arguments persist. The expectation of recovery that promotes a placebo response is separate from any subjective improvement and, incidentally, is also different from hope. It is possible to feel subjectively better without expecting a full recovery. Similarly, it is possible to expect recovery without feeling better at all. Complementary therapies cannot be dismissed as mere placebos, and it is becoming increasingly obvious that they produce substantial subjective and objective clinical benefits unrelated to the placebo effect.
Individuals differ in their responsiveness to the various activation stimuli, whether expectancy, subjective sensations, or complementary therapies. This would explain why complementary therapies that are supposedly mediated by placebo mechanisms, as in allopathic arguments, could outperform placebos in a double-blind trial (Reilly et al, 1994). It would also explain the need to combine a number of complementary approaches to ensure that these pathways are fully activated.
There is fortunately a growing body of scientific literature published since 2006 from psychoneurologists and neuroscientists addressing the specific issues of placebo and nocebo, which is the worsening of symptoms due to a nonspecific response, and their potential biological mechanisms. According to Eccles (2007), the placebo response in clinical medicine could be compared to a component of an allergy treatment that possesses “nonspecific effects” (e.g., natural recovery) and a “true placebo effect” represented as the psychological therapeutic effect of the treatment. Intrinsic positive belief in the efficacy of the treatment characterizes the true placebo effect, which can be enhanced by extrinsic factors such as the interaction with physician. Negative belief, however, can engender a nocebo effect that may elucidate some psychogenic diseases (Eccles, 2007). To examine placebo and nocebo symptoms, college students were recruited into what appeared to be a clinical trial evaluating the effectiveness of an herbal supplement on cognitive performance. Subjects received either an herbal supplement or a placebo (both are placebo inactive pills) and a list of positive and adverse effects. Most participants reported symptoms, and those who believed they were ingesting the herbal supplement reported significantly more symptoms than those who thought they were taking a placebo. In this case the belief may exacerbate the placebo response (Link et al, 2006).
SUMMARY
The medical and scientific communities are showing growing interest in the neurohumoral mechanisms underlying PNI responses to complementary therapies.
The latest research in the biomedical sciences and the social sciences is beginning to demonstrate mechanisms of action by which CAM therapies exert their benefits. The studies published to date have been carried out with relatively small groups of subjects and reflect conventional study criteria and design. Although complementary medicine research currently follows the conventional scientific approach to silence critics, evaluation of the efficacy of various complementary, integrative, and alternative modalities may require the development of additional methodologies based on a new paradigm to overcome foreseeable limitations.
It is noteworthy that the criticism of alternative and integrative therapies as being placebos has moved basic and clinical scientists to question the placebo and nocebo response. There is a call to expand the thinking beyond the “expectation and brain reward circuitry” or Pavlovian conditioning to include other pathways and mechanisms that reflect the psychoneuroimmunoendocrine paradigm. The theoretical framework needs to be redefined, and methodological as well as ethical paradigms should be developed to elucidate the placebo-nocebo response.
 Chapter References can be found on the Evolve website at http://evolve.elsevier.com/Micozzi/complementary/
Chapter References can be found on the Evolve website at http://evolve.elsevier.com/Micozzi/complementary/